- Department of Audiology, School of Human and Community Development, University of the Witwatersrand, Johannesburg, South Africa
Background: The COVID-19 pandemic precipitated a global shift in education and healthcare delivery, including the field of audiology. In South Africa, the sudden transition to remote learning and tele-healthcare posed unique challenges, particularly given existing resource constraints and technological inequities. This review synthesizes the current literature on the use of technological advancements for clinical teaching and learning in audiology, identifying the opportunities and challenges introduced by the pandemic.
Aim: This paper aims to explore the evidence on how advances in technology were embraced for clinical teaching and learning in audiology, with a focus on the South African academic context following the onset of COVID-19.
Methods: A narrative review methodology was employed to explore and synthesize a broad range of literature, including peer-reviewed articles, gray literature, and reports on technological advancements in audiology education and clinical practice. The review involved iterative cycles of searching, analysis, and interpretation of available evidence. Themes were identified related to the use of tele-audiology, virtual simulations, and online platforms for professional development, with a focus on the South African context.
Results: Five key themes emerged from the analysis: (1) Embracing tele-audiology for clinical training and service delivery, (2) Utilization of virtual simulations to compensate for in-person clinical training, (3) Challenges and inequalities in access to technology, (4) Shifting to online platforms for continuing professional development (CPD), and (5) The potential for hybrid models in audiology education. While technology offered flexibility and continued learning, significant barriers such as digital infrastructure gaps and regulatory constraints were highlighted.
Conclusion: The COVID-19 pandemic accelerated the adoption of technological tools in audiology education and practice in South Africa. Tele-audiology, virtual simulations, and online platforms for CPD were pivotal in maintaining clinical education and service delivery during the pandemic. However, challenges related to access, infrastructure, and training must be addressed to ensure the equitable and sustainable use of these technologies in the future.
Introduction
The COVID-19 pandemic has had a transformative impact on the global education sector, compelling institutions to pivot to remote learning modalities to ensure continuity in education (Legon et al., 2020; Gelles et al., 2020). The sudden shift to online learning, driven by the need for social distancing and lockdown measures, has brought about significant changes in the way education is delivered. In South Africa, this transition has posed unique challenges and opportunities, particularly in the field of audiology, where clinical teaching and learning are heavily reliant on in-person interaction and hands-on experience, where clinical training and hands-on experience are crucial components of the curriculum (Mandke, 2021; Khoza-Shangase et al., 2021a; Kgare et al., 2024). Audiology students, who represent a vulnerable population due to the intensive nature of their training, faced unprecedented disruptions (Balton et al., 2022; Khoza-Shangase and Mophosho, 2018). The pandemic highlighted the necessity for innovative solutions to maintain the quality and effectiveness of clinical education.
Audiology students in South Africa, particularly the previously disadvantaged groups which are increasing in numbers in training programs, constitute a vulnerable population due to a confluence of historical, socioeconomic, cultural, and systemic factors (Moonsamy et al., 2017; Khoza-Shangase and Mophosho, 2018, 2021; Mophosho et al., 2022; Abrahams et al., 2023; Mtimkulu et al., 2023). South Africa’s history of apartheid has left a legacy of profound socioeconomic disparities, disproportionately affecting Black communities. Many Black students come from under-resourced educational backgrounds, which can impact their academic preparedness and access to higher education opportunities. These disparities often translate into challenges in accessing quality education and support services necessary for successful academic progression in demanding fields like audiology (Albertus, 2019; Gukurume and Maringira, 2022). This is compounded by limited access to resources.
Vulnerable audiology students may face limited access to essential resources, such as high-speed internet, computers, and specialized audiology equipment, especially those from rural or low-income areas. This digital divide became even more pronounced during the COVID-19 pandemic, when remote learning became the norm (Sife et al., 2007; Rashid et al., 2020; Bakhov et al., 2021). Lack of access to these resources can hinder their ability to participate fully in online classes, access educational materials, and complete clinical training requirements. This challenge is worsened by financial constraints that many of these students experience, which can impact their ability to afford tuition, textbooks, and other educational expenses (Seabi et al., 2014; Pillay and Sebothoma, 2021); unless they have financial aid. Financial difficulties may also necessitate part-time employment, which can detract from study time and academic performance. The stress and uncertainty associated with financial instability further contribute to their vulnerability. Additionally, language and cultural differences documented in South African training programs can pose significant challenges for Black audiology students who do not speak English/Afrikaans as their first language, the only languages used in university level audiology programs in South Africa (Khoza-Shangase and Kalenga, 2023, 2024a; Abrahams et al., 2023). Many may speak English as a second language or come from diverse linguistic and cultural backgrounds. This can affect their comprehension of complex audiology concepts taught in English and their ability to communicate effectively with patients from different linguistic backgrounds during clinical training (Khoza-Shangase and Kalenga, 2024b).
Addressing these vulnerabilities requires targeted interventions, such as providing financial aid such as the National Student Financial Aid Scheme (NSFAS), ensuring access to essential resources, fostering an inclusive and supportive academic environment, and implementing mentorship programs (Chiramba and Ndofirepi, 2023; Woldegiorgis and Chiramba, 2024; Yende, 2024). However, the COVID-19 crisis also presented a unique opportunity to explore and integrate advanced technologies in clinical teaching and learning (Tabatabai, 2020; Gaur et al., 2020; Karimian et al., 2022). Technologies such as tele-audiology, virtual simulations, and online collaborative platforms emerged as vital tools to bridge the gap created by the absence of in-person interactions (Coco et al., 2020; Khoza-Shangase et al., 2021a; Morgan et al., 2022; Nagdee et al., 2022; Maluleke and Khoza-Shangase, 2023). The pandemic’s introduction of barriers to traditional learning methods and necessitating rapid adaptation to new technological tools and platforms also catalyzed innovation and the adoption of advanced technologies, presenting opportunities to enhance clinical education in ways previously unimagined. Such opportunities require the audiology community to embrace advances in technology for clinical teaching and learning.
The adoption of advanced technologies in audiology education offers numerous benefits, particularly in the context of a pandemic. These include: (1) increased accessibility and flexibility, where the use of online platforms and virtual simulations can allow students to access learning materials and clinical training modules from any location, providing flexibility in their schedules and accommodating diverse learning needs (Nagdee et al., 2022); (2) enhanced learning experiences, where virtual simulations and tele-audiology can enable students to engage in realistic clinical scenarios, enhancing their practical skills and decision-making abilities without the need for physical presence (Khoza-Shangase et al., 2021b); (3) broader reach, where technology can bridge geographical barriers, enabling institutions to offer high-quality education to students in remote or underserved areas particularly in the African context where only a few training programs exist and are localized in only a few countries such as South Africa and Morocco; (Sebothoma and Khoza-Shangase, 2018; Chong-White et al., 2023; Khoza-Shangase et al., 2021a; Sebothoma et al., 2022) (4) innovative teaching methods, where the use of multimedia resources, interactive modules, and real-time feedback through online platforms can enhance engagement and improve learning outcomes (Kgare et al., 2024); and (5) continuity of education, where during disruptions like the COVID-19 pandemic, technology can ensure that education and training can continue without significant interruptions, maintaining the progression of students through their programs (Maluleke and Khoza-Shangase, 2023).
Despite the numerous benefits, several challenges and barriers exist in integrating advanced technologies into audiology education, especially within the South African context. These include (1) digital divide, where a significant disparity in access to technology and reliable internet among students has been documented, particularly those from rural or low-income backgrounds, which can hinder their ability to participate fully in online learning (Khoza-Shangase et al., 2021b; Govender, 2022); (2) technical difficulties, where both students and educators may face challenges related to the technical aspects of using new technologies, including software issues, hardware limitations, and lack of technical support (Leonard et al., 2020; Khoza-Shangase et al., 2021a); (3) cost, where implementing advanced technologies can be costly, and not all institutions or students may have the financial resources to invest in the necessary infrastructure and tools (Govender, 2022); (4) training and adaptation, where educators may need adequate training to effectively use new technologies in their teaching, and students may require support to adapt to these new learning methods (Leonard et al., 2020; Pillay and Sebothoma, 2021); (5) quality assurance, where measures to ensure that the quality of education and clinical training is maintained in an online or virtual format can be challenging, particularly in terms of providing hands-on experience and direct patient interaction (Khoza-Shangase, 2021); and (6) adherence to regulations for clinical training as dictated by regulators, such as the Health Professions Council of South Africa (HPCSA), and these may include ethical and privacy concerns as well as hands-on clinical hours requirements (Swanepoel, 2020; Khoza-Shangase et al., 2021b).
This narrative review aims to explore the evidence on how advances in technology were embraced for clinical teaching and learning in audiology during and after the COVID-19 pandemic, with a specific focus on the South African context. The research question guiding this review is: What evidence has been published on the use of technological advancements in audiology education and clinical practice, particularly within South Africa, following the COVID-19 pandemic? By mapping the existing literature, identifying gaps, and highlighting the opportunities created by the pandemic, this review seeks to inform future educational strategies and support the ongoing development of resilient and effective audiology training programs.
Methodology
This research adopted a narrative review methodology. The decision to conduct a narrative review for this study is based on the broad and evolving nature of the research question, which aims to explore the use of advances in technology for clinical teaching and learning in audiology, particularly within the South African context, following the COVID-19 pandemic. Narrative reviews are well-suited for synthesizing a wide and heterogenous body of literature from diverse sources with varying methodologies, conceptual frameworks, and conceptual settings, offering a rich interpretation of the current state of knowledge without the constraints of rigid inclusion/exclusion criteria inherent in systematic reviews (Sukhera, 2022). A narrative review enables the integration of empirical studies, theoretical discussions, and gray literature, which aligns with the study’s objective and allows for the flexibility needed to assess how the pandemic catalyzed changes in teaching and learning methodologies in audiology, and to explore various technological advancements implemented during this period.
Literature search strategy
The literature search for this narrative review was iterative and involved multiple cycles of searching, analysis, and interpretation. While adhering to the recommendations by Levac et al. (2010), the search strategy was planned to be clear, transparent, comprehensive, while ensuring feasibility. The literature search was conducted in September 2024 across several electronic databases, including ScienceDirect, CINAHL, EBSCOHost, MEDLINE, ProQuest, PubMed, Scopus, and African Journals Online (AJOL). The search aimed to identify peer-reviewed articles from January 2020 to current, a timeframe that aligned with the pandemic. The search terms and keywords were carefully selected to align with the research question. These terms combined with Boolean operators included: ‘COVID-19’ OR ‘coronavirus’ OR ‘SARS-CoV-2…AND (‘technology’ OR ‘digital learning’ OR ‘online learning’ OR ‘e-learning’ OR ‘virtual learning’ OR ‘virtual simulation’ OR ‘tele-education’ OR ‘tele-learning’ OR ‘remote learning’ OR ‘digital education’)…AND (‘clinical teaching’ OR ‘clinical education’ OR ‘clinical training’ OR ‘clinical practice’ OR ‘hands-on training’ OR ‘practical training’)…AND (‘audiology’ OR ‘hearing disorders’ OR ‘hearing healthcare’ OR ‘audiology education’ OR ‘audiology training’ OR ‘hearing science’ OR ‘hearing rehabilitation’)…AND (‘students’ OR ‘learners’ OR ‘educators’ OR ‘teachers’ OR ‘faculty’ OR ‘academic staff’)…AND (‘Africa’ OR ‘South Africa’) (Aliyu, 2017). Aliyu (2017) stresses that utilizing a combination of keywords improves the search strategy’s effectiveness by expanding the probability of discovering pertinent articles while excluding inappropriate ones.
Study selection
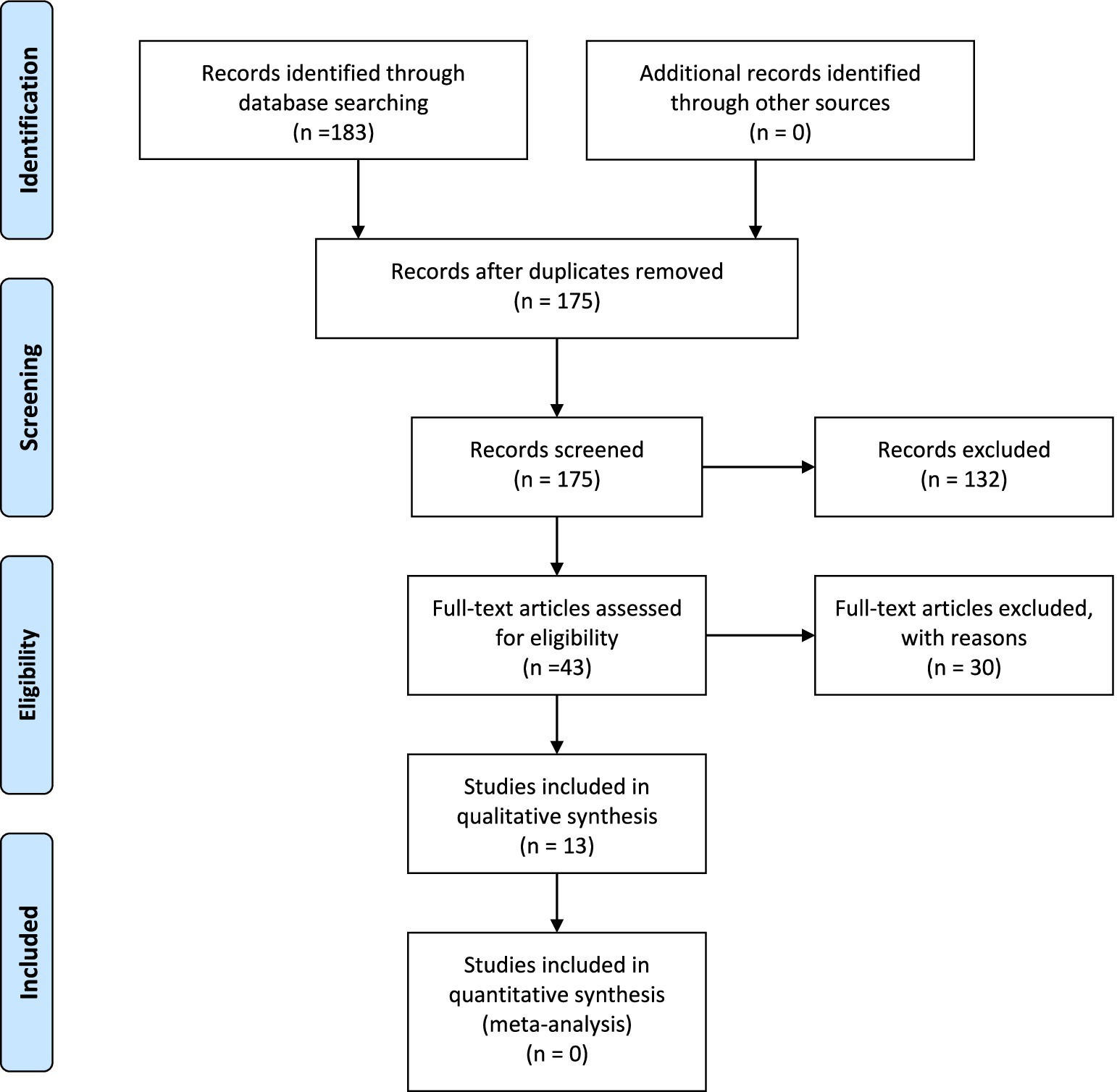
Studies were included if they focused on the use of technological advancements for clinical teaching and learning in audiology, particularly those implemented or adapted in response to the COVID-19 pandemic. The focus was on the South African context, though relevant studies from other regions were also included for relevant comparative insights. Studies that explicitly discussed the use of digital technologies, such as tele-audiology, virtual simulations, or online CPD; were published between 2020 and 2024; and were accessible in English were included. Studies that focused exclusively on traditional, face-to-face (in-person interventions) teaching methodologies with no reference to technological interventions, as well as studies unrelated to audiology or clinical education were excluded. Additionally, opinion pieces, commentaries or editorials without empirical or theoretical or conceptual analysis; and studies that fell outside the scope of audiology or closely related speech-language professions were excluded. A total of 183 studies were identified through the initial search process. After screening titles and abstracts, 43 full-text articles were reviewed for relevance, of which 13 met the inclusion criteria and were included in the qualitative synthesis. Studies were excluded if they did not address technological advances in audiology education or clinical practice during/following covid-19, if they lacked sufficient detail on outcomes, or if they focused solely on face-to-face interventions. A PRISMA-style flow diagram (Figure 1) summarizes the study selection process.
Data extraction and synthesis
Applying guidelines by Peters et al. (2015), data were charted in accordance with the review’s aims, utilizing a standardized data extraction form. A total of 13 studies formed the final evidence data used in the review and are summarized and presented in Table 1. The review process involved extracting key information from each identified source, including:
• Study characteristics: Author(s), year of publication, country of origin, and study design.
• Context and objectives: The specific context in which the study was conducted and the primary objectives.
• Technological interventions: Types of technologies used for clinical teaching and learning in audiology (e.g., tele-audiology, virtual simulations, online platforms, tele-supervision).
• Key findings and outcomes: The main findings of the studies, including the effectiveness, challenges, and benefits of the technological interventions used.
• Challenges and opportunities: Identified barriers to the implementation of these technologies and opportunities for future improvements.
• Recommendations: Suggestions for future research, practice, and policy development related to the integration of technology in audiology education.
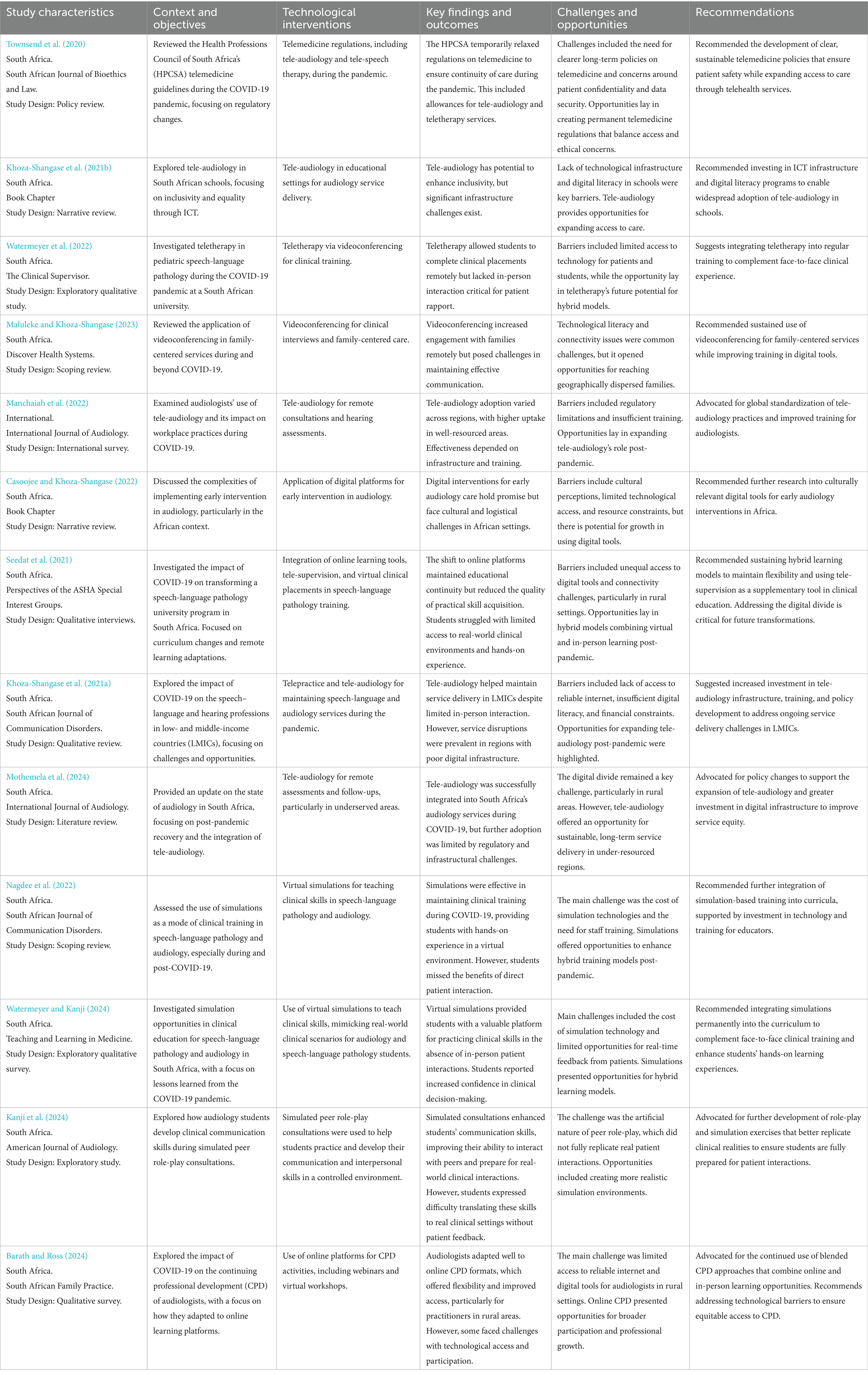
Table 1. Summary of evidence on the use of technology for clinical teaching and learning in audiology.
Data analysis
A narrative approach to analysis was adopted, allowing for an in-depth interpretation of the findings in the context of the research question. Thematic analysis was conducted through an iterative process involving close reading, extraction, and coding of relevant information from each source. Initially, data from each article were summarized using a structured evidence Table 1 capturing study design, setting, technology used, key findings, challenges, and recommendations. Descriptive codes were applied to recurrent concepts (e.g., tele-supervision, access limitations, simulation effectiveness). These codes were then grouped inductively into broader themes that reflected the cross-cutting issues emerging from the literature (Peters et al., 2015; Schiller and Malouf, 2000). The themes included the effectiveness of different technological interventions, the challenges and barriers faced by students and educators, and the broader implications for audiology education in a post-pandemic world. In the context of this narrative review, saturation was reached when the inclusion of additional studies no longer provided new insights or themes related to the research question (Sukhera, 2022). As the review process progressed, it became clear that key themes—such as the role of tele-audiology, virtual simulations, and the digital divide—were consistently emerging across multiple sources. At this point, the iterative search and analysis cycles did not reveal any substantially new information, indicating thematic sufficiency. Therefore, saturation was considered achieved, ensuring that the literature reviewed provides a comprehensive understanding of the topic. Thematic saturation was determined when no new themes emerged after the review of the first 10 included studies. The remaining studies served to confirm, elaborate, or provide nuance to these themes without introducing fundamentally new categories. This approach is consistent with qualitative synthesis methodology, where saturation is reached once additional data do not add substantive new insights.
Quality and rigor
Although narrative reviews are not as rigid as systematic reviews, steps were taken to ensure the rigor and quality of the review (Johnson et al., 2020). These included:
• Transparent documentation of the search strategy and selection process.
• Iterative refinement of the research question and scope based on the emerging literature.
As far as critical appraisal was concerned, while formal scoring tools were not applied due to the narrative nature of the review, all included studies were appraised for their relevance, clarity, and conceptual contribution to the research question. Studies were retained based on their alignment with the focus on technological responses to COVID-19 in audiology education and practice, particularly within the African context. Where possible, thematic findings were triangulated across multiple sources to enhance trustworthiness.
Reflexivity and interpretation
Throughout the review, reflexivity was maintained to ensure that the interpretation of the literature was informed by the researcher’s perspectives, the historical context of the pandemic, and the unique challenges faced by South African educational institutions. This approach recognizes the subjectivity inherent in narrative reviews and aims to provide a thoughtful synthesis of the literature that acknowledges different points of view.
Ethical considerations
As this study involved a review of existing literature, ethical approval was not required. However, ethical considerations related to the integrity, transparency, and accuracy of the review process were strictly adhered to. This included ensuring that all sources were appropriately cited, findings were presented objectively, and any potential conflicts of interest were disclosed (Thomas et al., 2020; Vergnes et al., 2010; Suri, 2020).
Results and discussion
Of the 13 manuscripts analyzed, all (100%) focused on adaptations and considerations within South Africa, highlighting the unique challenges and opportunities in this context. Additionally, five (38%) of the studies concerned specifically academic institutions, while eight (62%) were focused mainly on clinical environments. This distribution highlights the dual impact of technological advancements on both educational and service delivery settings during the pandemic.
The studies included in this narrative review represent a diverse range of methodologies, settings, and populations, providing a comprehensive perspective on the use of technological advancements in audiology education and practice during the COVID-19 pandemic. The evidence spans qualitative reviews, scoping reviews, literature reviews, and policy reviews, reflecting both empirical and theoretical approaches to understanding the impact of these technologies. Most studies were conducted in South Africa, with a focus on the South African academic and healthcare systems, but a few extended their scope to include insights from other low- and middle-income countries (LMICs) (Khoza-Shangase et al., 2021b; Mothemela et al., 2024). The evidence base also includes insights from health policy reviews, such as the one conducted by Townsend et al. (2020), which focused on regulatory frameworks for telemedicine in South Africa during the pandemic. The settings of these studies primarily involved academic institutions and clinical service delivery environments, particularly those utilizing tele-audiology, virtual simulations, and online platforms for professional development.
The populations targeted in these studies varied. While several studies focused on audiology students undergoing clinical training (Watermeyer and Kanji, 2024; Nagdee et al., 2022), others examined professional audiologists and speech-language pathologists adapting to the rapid shift toward tele-health and tele-education during the pandemic (Manchaiah et al., 2022; Khoza-Shangase et al., 2021b). The age groups of the populations ranged from pediatric to adult patients receiving tele-audiology services, though specific demographic data such as gender and socioeconomic background were less commonly emphasized. However, many of the studies did highlight rural and underserved communities, particularly when discussing access challenges related to tele-audiology.
The variation in study designs and populations included in this review reflects the wide-ranging impact of COVID-19 on both audiology education and clinical practice. The inclusion of qualitative and scoping reviews provided deep, interpretive insights into the challenges and opportunities brought by technological interventions, while literature and policy reviews offered a critical analysis of existing guidelines and theoretical frameworks. The studies’ focus on South Africa and other LMICs underscores the unique resource constraints and infrastructural challenges faced in these contexts, particularly regarding access to reliable internet, digital tools, and technical support. This geographical and socioeconomic focus adds depth to the analysis, highlighting the disparities in access to technology between urban and rural populations, and between high-income and low-income areas. The heterogeneity in populations—ranging from students to professionals, and from pediatric to adult patients—indicates that technological interventions in audiology during COVID-19 had a broad and far-reaching impact. This diversity in the evidence base allows for a nuanced understanding of how different stakeholders within the audiology field were affected by the pandemic and the technological changes it necessitated. However, the lack of specific demographic data such as gender or socioeconomic characteristics in some studies points to gaps in the literature, suggesting a need for future research to explore how these factors influence access to and success in tele-audiology and online learning platforms.
The thematic analysis of the data in Table 1 and the article summaries identified five key themes that address the research question: “What evidence has been published on the embracing of advances in technology for clinical teaching and learning in audiology following COVID-19 to benefit the South African academy?”: (1) Embracing tele-audiology for clinical training and service delivery, (2) Utilization of virtual simulations to compensate for in-person clinical training, (3) Challenges and inequalities in access to technology, (4) Shifting to online platforms for continuing professional development (CPD), and (5) The potential for hybrid models in audiology education.
Theme 1: embracing tele-audiology for clinical training and service delivery
Tele-audiology emerged as a critical tool during the COVID-19 pandemic, allowing for the continuation of audiology services and clinical training when in-person interaction was not possible. Tele-audiology was used for remote consultations, hearing assessments, and service delivery. Tele-audiology helped audiologists provide care despite social distancing restrictions, particularly in underserved areas where face-to-face interaction was not possible. Telepractice tools were also used in audiology education to deliver clinical teaching remotely, enabling students to participate in tele-supervision, conduct virtual consultations, and learn through online clinical scenarios. Studies such as Khoza-Shangase et al. (2021a) and Manchaiah et al. (2022) highlighted the use of tele-audiology for hearing assessments and consultations, particularly in rural and underserved areas of South Africa. This technology allowed students to observe and participate in real-time remote consultations, offering a practical learning environment despite restrictions on physical interaction. The success of tele-audiology in bridging the gap in service delivery, including delivery of clinical teaching, suggests that it can be permanently integrated into the healthcare system as well as education and training sectors, especially in areas with limited access to audiology services. In education, tele-audiology offers opportunities for extending clinical placements to students in remote locations and allows for greater flexibility in training, and within the African context where limited training programs exist across the continent, opportunities for cross-country training are significant. However, there is a need for structured tele-supervision training for both students and educators to maximize its benefits.
While tele-audiology has emerged as a valuable tool for remote consultations and training, it is important to acknowledge its limitations. Accurate assessments of auditory function, particularly those requiring calibrated tools in sound-attenuating environments, remain dependent on in-person appointments in dedicated clinical facilities. Remote assessments may lack the precision needed for tasks such as pure-tone audiometry or speech-in-noise testing, and these limitations must be addressed through hybrid approaches that complement tele-audiology with in-person sessions. Similarly, while tele-audiology can facilitate follow-up consultations and device troubleshooting, tasks such as mapping cochlear implants, programming hearing aids, or performing detailed device calibration are challenging to conduct remotely. These procedures necessitate hands-on adjustments in controlled environments, underscoring the need for hybrid service models that integrate tele-audiology with scheduled in-person appointments.
Theme 2: utilization of virtual simulations to compensate for in-person clinical training
Virtual simulations played a pivotal role in audiology training during the pandemic, providing students with hands-on learning experiences in a controlled, virtual environment. Virtual simulations were utilized as a teaching tool to replace in-person clinical training during lockdowns. These simulations allowed students to engage in interactive clinical scenarios and decision-making processes in a virtual environment. Simulations included virtual patients, scenarios mimicking real-life clinical interactions, and collaborative problem-solving exercises. Virtual simulations provided practical exposure and helped maintain skills development when direct patient interaction was not feasible. Nagdee et al. (2022) described the use of virtual simulations to teach clinical skills, with Watermeyer and Kanji (2024) recently described students engaging in decision-making and diagnostic exercises mimicking real-life scenarios through the use of simulations. ‘Real-life scenarios’ in remote learning refer to structured virtual simulations and tele-audiology cases where students interact with simulated or recorded diagnostic data that mimics patient assessments. For instance, students can learn to interpret audiometric results, perform speech discrimination tests, and analyze tympanometry or otoacoustic emissions recordings through remote platforms. These activities provide an opportunity to engage with diagnostic processes in controlled environments. While remote platforms cannot replicate all aspects of in-person diagnostics, they can effectively teach students how to assess and interpret data in cases such as unilateral hearing loss, auditory neuropathy, or otitis media. Accurate remote diagnostic training depends on high-quality, pre-calibrated data sets and guided tele-supervision from experienced educators to ensure students develop diagnostic proficiency. While simulations provided valuable learning opportunities, students reported that these technologies could not fully replicate the benefits of interacting with real patients (Kanji et al., 2024). The use of virtual simulations is likely to become a standard component of audiology education, complementing in-person clinical placements. Hybrid models combining virtual and real-world training can create a more holistic educational experience. Institutions will need to invest in advanced simulation software and hardware, e.g., in the form of mannequins, and ensure that educators are trained in how to effectively incorporate these technologies into the curriculum. Mannequins, often designed with anatomically accurate ear canals and tympanic membranes, can be used in audiology education to simulate real-world procedures. These tools allow students to practice skills such as otoscopy, cerumen removal, and earmold impressions in a safe and controlled environment. Advanced mannequins equipped with embedded sensors can also simulate auditory responses, enabling students to conduct air- and bone-conduction audiometry. By using mannequins, students can gain hands-on experience and build confidence before transitioning to working with real patients. This approach complements remote learning by offering a tactile and interactive component to audiology training.
The effectiveness of virtual simulations for clinical training is influenced by the technological resources and learning environments of individual students. Disparities in access to high-performance devices and stable internet connections can create unequal learning experiences within the same program. Students with limited resources may struggle to engage fully with simulations, which could affect the overall quality and consistency of their clinical training. Addressing these inequities requires institutional support, such as providing standardized devices or access to equipped simulation labs, to ensure equitable training experiences.
Theme 3: challenges and inequalities in access to technology
Challenges with regards to digital divide, technological literacy, cost, and regulatory and ethical concerns were found. One of the biggest barriers to the widespread adoption of these technologies was the digital divide (Khoza-Shangase et al., 2021a). Many students and patients faced challenges with reliable internet access, availability of devices, and technical support. Additionally, both students and educators often struggled with the technological aspects of using new tools (Maluleke and Khoza-Shangase, 2023). The lack of digital and technological literacy among patients also hindered the adoption of tele-audiology services (Seedat et al., 2021). Furthermore, implementing tele-audiology and virtual simulation technologies was costly for many institutions, limiting their ability to fully embrace these advancements (Mothemela et al., 2024). Lastly, there were concerns around patient confidentiality and data security in tele-audiology, as well as ethical considerations when using telehealth platforms for sensitive clinical interactions, all pointing toward regulatory and ethical concerns. There is a need to develop clear regulatory frameworks to guide the use of tele-audiology, addressing issues such as patient confidentiality, data protection, and ethical practice. Global standardization of tele-audiology practices should be pursued to ensure consistent quality of care across different regions.
A recurring challenge across studies was the issue of unequal access to digital tools, reliable internet, and technological infrastructure, particularly for students and patients in rural or low-income areas. Studies like Seedat et al. (2021) and Manchaiah et al. (2022) identified the digital divide as a major barrier to the successful implementation of tele-audiology and online learning. The lack of technological access impeded participation in virtual clinical placements, CPD, and patient consultations, creating inequities in learning and service delivery. Addressing the digital divide is critical for ensuring equitable access to education and healthcare. Governments and educational institutions must prioritize investment in digital infrastructure, especially in rural and underserved areas. Subsidizing technology and internet access for students and patients in need could help bridge the gap and ensure that everyone can benefit from advancements in tele-audiology and online learning platforms (Reddy et al., 2022).
Theme 4: shifting to online platforms for continuing professional development (CPD)
The pandemic led to a significant increase in the use of online platforms for training and CPD activities, allowing audiologists to engage in professional development remotely. Videoconferencing tools such as Zoom and Microsoft Teams were employed for both educational and clinical purposes (Watermeyer and Kanji, 2024; Maluleke and Khoza-Shangase, 2023). For teaching, videoconferencing enabled lectures, group discussions, and tele-supervision sessions. Clinically, it was used for teletherapy and patient consultations, allowing students to observe or participate in live case discussions and treatment planning with patients. This technology was particularly valuable in delivering family-centered care and speech-language therapy to children with hearing impairments (Maluleke and Khoza-Shangase, 2023). Collaborative platforms such as Moodle, Google Classroom, and Blackboard were used for hosting course content, assessments, and facilitating discussions (Seedat et al., 2021). These platforms allowed students and educators to stay connected, share resources, and engage in continuous learning despite physical restrictions. These platforms also supported peer-to-peer learning and asynchronous learning, providing flexibility for students.
Studies like Barath and Ross (2024) found that online CPD courses and webinars were effective in maintaining professional standards during the pandemic. Audiologists in remote locations benefited from the flexibility and accessibility of online platforms, which allowed them to participate in CPD without the need for travel. Online CPD is likely to remain a popular and flexible option for audiologists, particularly those in rural areas. Institutions should continue offering blended CPD models that combine online and in-person opportunities to cater to different needs and preferences, and to extend the reach of CPD initiatives. Expanding the range of topics covered in online CPD programs, including tele-audiology and virtual supervision, can enhance the relevance of these platforms for practitioners adapting to new technologies in clinical practice.
Theme 5: the potential for hybrid models in audiology education
A key opportunity identified in several studies is the development of hybrid models that combine online learning with in-person clinical placements. Virtual simulations, tele-supervision, and online collaborative platforms proved valuable during the pandemic, but they were often limited by the absence of real-world patient interactions. As the pandemic subsides, hybrid models that integrate the best aspects of both virtual and in-person training can provide a more comprehensive and flexible learning experience for audiology students. Hybrid learning models offer an opportunity to enhance the audiology curriculum by providing students with more diverse training experiences. Institutions should focus on refining these models to ensure they strike the right balance between virtual and in-person learning and align with HPCSA minimum standards and training regulations. The success of hybrid models will depend on the availability of adequate resources, including simulation technologies, trained supervisors, and infrastructure that supports both remote and face-to-face interactions. By incorporating hands-on experiences alongside tele-supervision and virtual simulations, hybrid models can ensure that future clinicians receive the comprehensive training needed to manage complex patient cases effectively. This approach also aligns with regulatory requirements for clinical competency, such as those outlined by the HPCSA.
While telehealth and virtual simulations offered critical solutions during the COVID-19 pandemic, they should not be construed as full replacements for in-person clinical education or service delivery. Instead, these technologies served as temporary substitutions during a unique and unprecedented global crisis. As the field moves forward, hybrid approaches that combine these advancements with traditional in-person methods will be essential to ensure the development of fully competent clinicians and the delivery of high-quality care to patients. This perspective highlights the need for ongoing evaluation of telehealth’s long-term impact on audiology practice and education.
Integrating simulations and tele-supervision into audiology training can be guided by established pedagogical and competency-based frameworks. Models such as Miller’s Pyramid (“knows,” “knows how,” “shows how,” “does”) can be applied to support a phased approach skill development (Miller, 1990). Tele-simulations align with the “shows how” level, allowing students to demonstrate clinical competencies in a safe, monitored virtual environment before progressing to real-patient interactions. In parallel, the World Health Organization’s (WHO) global competency framework for universal health coverage (World Health Organization, 2022) emphasizes core domains such as person-centered care, communication, ethics, and digital health proficiency—all of which are relevant to training in tele-audiology and simulation-based education. Incorporating these competencies into formal curricula can ensure that students acquire the skills needed for digital practice, while aligning training programs with global health workforce standards. Tele-supervision practices can further be informed by Vygotsky’s zone of proximal development (Kantar et al., 2020), where supervision through video or live feedback helps students bridge the gap between what they can do independently and what they can do with guided support; where structured, remote guidance supports students’ progression from assisted to independent practice. Formalizing these approaches within curricula ensures that remote learning is not merely a temporary response to crisis but a structured component of long-term competency development. It also will help ensure that hybrid education models are rigorous, equitable, and sustainable.
Conclusion and implications
The findings from this narrative review reveal that the COVID-19 pandemic served as a catalyst for embracing technological advancements in audiology education and clinical practice. Tele-audiology, virtual simulations, and online platforms for CPD transformed how audiologists are trained and how services are delivered across South Africa. These technologies offered critical solutions to continue education and patient care during the pandemic, particularly in contexts where in-person interactions were restricted. However, the adoption of these innovations also underscored persistent challenges, especially regarding access to technological infrastructure, digital literacy, and the digital divide—challenges that disproportionately affected vulnerable populations in rural and underserved areas. For students and patients in these contexts, adapting to remote learning and telehealth services proved difficult due to limited access to reliable internet, digital devices, and technical support. The themes emerging from this review highlight the paradox of technology: while it presents significant opportunities for improving audiology education and service delivery, it also risks deepening existing inequalities if not implemented equitably. Vulnerable populations, particularly in low- and middle-income countries like South Africa, face greater barriers to accessing the benefits of these advancements, further marginalizing students and patients in rural and underserved areas.
This review underscores the critical need to prioritize equity in the implementation of technological solutions. While technology has the potential to democratize access to education and healthcare, its success will depend on addressing the systemic barriers faced by vulnerable populations, including economic disparities, limited infrastructure, and socio-cultural challenges. Implications for policymakers, educators, and researchers are advanced by current findings. For policymakers, the findings call for urgent action to expand digital infrastructure in rural and underserved areas. Governments and institutions need to increase funding and create policies that ensure equitable access to tele-audiology and online learning platforms, particularly for vulnerable populations who are most affected by the digital divide. This includes investments in broadband access, affordable digital devices, and digital literacy programs tailored to the specific needs of students and patients in resource-constrained settings. Additionally, policies should focus on long-term sustainability of telehealth and online education beyond the pandemic, ensuring that these technologies continue to serve vulnerable communities even as in-person services resume. For educators, audiology and speech-language pathology education must adopt hybrid learning models that combine virtual and in-person training to ensure a flexible, inclusive approach that addresses the diverse needs of students. In particular, students from rural and economically disadvantaged backgrounds should receive support, such as access to digital devices and internet subsidies, to ensure they are not left behind. Training programs should also focus on building digital competencies among both students and educators to effectively utilize tele-audiology and virtual simulations. Furthermore, culturally responsive training tools should be developed to ensure that the content delivered via these technologies is relevant to the unique contexts and challenges faced by students and patients in African countries. Lastly, for researchers, further research is needed to evaluate the long-term impact of tele-audiology, virtual simulations, and hybrid education models on both student learning outcomes and patient care, particularly within vulnerable and underserved populations. Researchers should examine how these technologies can be optimized for resource-constrained settings and explore best practices for integrating them into audiology education and clinical practice. Additionally, research should focus on the development of culturally relevant digital tools that address the specific needs of African populations, ensuring that these technologies are not only accessible but also culturally appropriate. This includes studying the impact of language, cultural norms, and healthcare access on the effectiveness of tele-audiology and virtual education.
In addition to broad policy and infrastructure recommendations, this review suggests the need for concrete, actionable frameworks to support the sustainable use of technology in audiology education and practice. A hybrid training model could, for example, consist of a minimum percentage of in-person supervised clinical hours combined with remote tele-simulations, tele-supervision, and online case discussions. Universities could be required to adopt minimum technological standards for students and staff participation, including access to stable internet, headphones with specified frequency response, and access to simulation software licenses. In terms of ethical practice, contextual tele-audiology protocols should be developed to address issues of informed consent, data security, patient confidentiality, and culturally appropriate communication—particularly in rural or multilingual communities.
Building on these general frameworks, more specific and contextualized recommendations can be proposed to guide policy and practice in South Africa. The Health Professions Council of South Africa (HPCSA) should consider mandating that a minimum of 30% of clinical training hours incorporate tele-simulations or remote supervision to ensure all graduates develop digital health competencies. The National Student Financial Aid Scheme (NSFAS) could subsidize student data bundles and support device acquisition for learners from low-income backgrounds to reduce digital inequities. Universities could be required to implement minimum technological standards, such as ensuring access to stable internet connections, headphones with specified frequency response, and simulation software licenses for all students. The National Department of Health, in partnership with professional bodies, could develop ethical tele-audiology protocols to safeguard issues of informed consent, patient privacy, and culturally appropriate communication. These actions would help operationalize the broader recommendations discussed above and provide a more sustainable, equitable pathway for the integration of technology into audiology education and practice.
This thematic analysis underscores the transformative potential of technology in audiology education and clinical service delivery, particularly in the context of the COVID-19 pandemic. However, it also highlights the importance of equity and inclusivity in ensuring that the benefits of these advancements reach all members of society, particularly vulnerable populations in African countries. Without strategic investments and thoughtful policy interventions, technological advancements may further marginalize those already disadvantaged. Therefore, a concerted effort is needed to ensure that the digital divide is addressed, that cultural considerations are integrated into technological solutions, and that the voices of vulnerable populations are centered in future developments in audiology education and clinical practice. A key limitation of this narrative review is the relatively small number of included studies (n = 13). This may limit the generalisability of the findings, particularly in relation to global trends in audiology education and service delivery. Additionally, this relatively small sample size may not fully capture the breadth of adaptations made by educational and clinical facilities globally during the COVID-19 pandemic. However, the aim of this narrative review was to explore developments primarily within the South African context — and, where applicable, other African or low- and middle-income country settings. The iterative review process was guided by the principle of thematic saturation, where further searching no longer yielded novel insights. While this review focuses primarily on the South African context, the findings should be interpreted cautiously, as they may not be generalizable to all settings. Nevertheless, future research that expands the regional scope and includes additional global perspectives is encouraged to validate and extend these findings. Future studies with a broader scope and more extensive dataset are recommended to provide a comprehensive understanding of the technological adaptations in audiology education and clinical practice.
Author contributions
KK-S: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author declares that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abrahams, F., Moroe, N. F., and Khoza-Shangase, K. (2023). Transformation of higher learning in South Africa: perceptions and understanding of speech-language therapy and audiology undergraduate students. Educ. Change 27, 1–26. doi: 10.25159/1947-9417/11648
Albertus, R. W. (2019). Decolonisation of institutional structures in south African universities: a critical perspective. Cogent Soc. Sci. 5:403. doi: 10.1080/23311886.2019.1620403
Aliyu, M. B. (2017). Efficiency of Boolean search strings for information retrieval. Am. J. Eng. Res. 6, 216–222.
Bakhov, I., Opolska, N., Bogus, M., Anishchenko, V., and Biryukova, Y. (2021). Emergency distance education in the conditions of COVID-19 pandemic: experience of Ukrainian universities. Educ. Sci. 11:364. doi: 10.3390/educsci11070364
Balton, S., Vallabhjee, A. L., and Pillay, S. C. (2022). When uncertainty becomes the norm: the Chris Hani Baragwanath academic hospital’s speech therapy and audiology department’s response to the COVID-19 pandemic. S. Afr. J. Commun. Disord. 69:913. doi: 10.4102/sajcd.v69i2.913
Barath, S., and Ross, A. J. (2024). Impact of COVID-19 on continuing professional development: perspectives of audiologists. S. Afr. Fam. Pract. 66, 1–7. doi: 10.4102/safp.v66i1.5963
Casoojee, A., and Khoza-Shangase, K. (2022). Complexities and challenges with implementation of communication therapeutic approaches to early intervention in audiology in the African context. Ed. K. Khoza-Shangase. Complexifies and challenges in prevenfive audiology: An African perspecfive, Cape Town: AOSIS, 41–54.
Chiramba, O., and Ndofirepi, E. S. (2023). Access and success in higher education: disadvantaged students’ lived experiences beyond funding hurdles at a metropolitan south African university. S. Afr. J. High. Educ. 37, 56–75. doi: 10.20853/37-6-6021
Chong-White, N., Incerti, P., Poulos, M., and Tagudin, J. (2023). Exploring teleaudiology adoption, perceptions and challenges among audiologists before and during the COVID-19 pandemic. BMC Digit. Health 1:24. doi: 10.1186/s44247-023-00024-1
Coco, L., Davidson, A., and Marrone, N. (2020). The role of patient-site facilitators in teleaudiology: a scoping review. Am. J. Audiol. 29, 661–675. doi: 10.1044/2020_AJA-19-00070
Gaur, U., Majumder, M. A. A., Sa, B., Sarkar, S., Williams, A., and Singh, K. (2020). Challenges and opportunities of preclinical medical education: COVID-19 crisis and beyond. SN Compr. Clin. Med. 2, 1992–1997. doi: 10.1007/s42399-020-00528-1
Gelles, L. A., Lord, S. M., Hoople, G. D., Chen, D. A., and Mejia, J. A. (2020). Compassionate flexibility and self-discipline: student adaptation to emergency remote teaching in an integrated engineering energy course during COVID-19. Educ. Sci. 10:304. doi: 10.3390/educsci10110304
Govender, S. (2022). “Tele-audiology within the African school context: opportunities, challenges and proposed solutions” in Preventive audiology: an African perspective. ed. K. Khoza-Shangase (Cape Town: AOSIS Books).
Gukurume, S., and Maringira, G. (2022). “Confronting legacies of apartheid” in Youth-led social movements and peacebuilding in Africa. ed. S. Gukurume (London: Routledge).
Johnson, J. L., Adkins, D., and Chauvin, S. (2020). A review of the quality indicators of rigor in qualitative research. Am. J. Pharm. Educ. 84:7120. doi: 10.5688/ajpe7120
Kanji, A., Watermeyer, J., and Hassim, A. (2024). Audiology students' clinical communication during simulated peer role play consultations: an exploratory study. Am. J. Audiol. 33, 575–585. doi: 10.1044/2024_AJA-23-00197
Kantar, L. D., Ezzeddine, S., and Rizk, U. (2020). Rethinking clinical instruction through the zone of proximal development. Nurse Educ. Today 95:104595. doi: 10.1016/j.nedt.2020.104595
Karimian, Z., Farrokhi, M. R., Moghadami, M., Zarifsanaiey, N., Mehrabi, M., Khojasteh, L., et al. (2022). Medical education and COVID-19 pandemic: a crisis management model towards an evolutionary pathway. Educ. Inf. Technol. 27, 3299–3320. doi: 10.1007/s10639-021-10697-8
Kgare, K., Maepane, C., Mabusela, G., Mphahlele, M., and Rinae, R. (2024). Speech-language pathology and audiology students’ expectations and experiences of academic and clinical experiences of online learning. In University of Fort Hare Teaching and Learning Conference (UFHTL 2023) (pp. 130–149). Atlantis Press: Beijing.
Khoza-Shangase, K., and Kalenga, M. (2023). Influence of social inclusion and institutional culture on students’ interactions in clinical settings. S. Afr. J. Commun. Disord. 70:991. doi: 10.4102/sajcd.v70i1.991
Khoza-Shangase, K., and Kalenga, M. (2024a). English instruction experiences of native south African speech-language and/or hearing (SLH) undergraduate students: an exploratory study. J. Psychol. Afr. 34, 59–64. doi: 10.1080/14330237.2023.2290426
Khoza-Shangase, K., and Kalenga, M. (2024b). English additional language undergraduate students’ engagement with the academic content in their curriculum in a south African speech-language and hearing training program. Front. Edu. 9:1258358. doi: 10.3389/feduc.2024.1258358
Khoza-Shangase, K. (2021). “Confronting realities to early hearing detection in South Africa” in Early detection and intervention in audiology: An African perspective. eds. K. Khoza-Shangase and A. Kanji (Johannesburg: Wits Press), 66–68.
Khoza-Shangase, K., and Mophosho, M. (2018). Language and culture in speech-language and hearing professions in South Africa: the dangers of a single story. S. Afr. J. Commun. Disord. 65, 1–7. doi: 10.4102/sajcd.v65i1.594
Khoza-Shangase, K., and Mophosho, M. (2021). Language and culture in speech-language and hearing professions in South Africa: re-imagining practice. S. Afr. J. Commun. Disord. 68, 1–9. doi: 10.4102/sajcd.v68i1.793.
Khoza-Shangase, K., Moroe, N., and Neille, J. (2021a). Speech-language pathology and audiology in South Africa: clinical training and service in the era of COVID-19. Int. J. Telerehabil. 13:e6376. doi: 10.5195/ijt.2021.6376
Khoza-Shangase, K., Sebothoma, B., and Moroe, N. F. (2021b). “Teleaudiology as part of efforts to enhance inclusivity and equality through ICT in south African schools: some considerations” in Empowering students and maximising inclusiveness and equality through ICT. eds. M. Maguvhe, R. S. Mphahlele, and S. Moonsamy (Boston: Brill), 223–243.
Legon, R., Garrett, R., Fredericksen, E. E., and Simunich, B. (2020). “CHLOE 5: the pivot to remote teaching in spring 2020 and its impact” in The changing landscape of online education. ed. B. Simunich (Texas: Encoura).
Leonard, E., de Kock, I., and Bam, W. (2020). Investigating the barriers and facilitators to implementing an eHealth innovation into a resource-constrained setting: a south African case study. In 2020 IEEE international conference on engineering, technology and innovation (ICE/ITMC) (pp. 1–7). IEEE. Cardiff
Levac, D., Colquhoun, H., and O’Brien, K. K. (2010). Scoping studies: advancing the methodology. Implement. Sci. 5:69. doi: 10.1186/1748-5908-5-69
Maluleke, N. P., and Khoza-Shangase, K. (2023). Embracing videoconferencing interview applications beyond COVID-19: scoping review-guided implications for family centered services in South Africa. Discov. Health Sys. 2:20. doi: 10.1007/s44250-023-00033-x
Manchaiah, V., Eikelboom, R. H., and Bennett, R. J., and Swanepoel, D. W. (2022). International survey of audiologists during the COVID-19 pandemic: effects on the workplace. International journal of audiology, 61, 265–272. doi: 10.1080/14992027.2021.1937348
Mandke, K. N. (2021). Challenges and opportunities for speech and hearing programs: Covid-19 and beyond. J. India Inst. Speech Hearing 40, 18–22. doi: 10.4103/jose.JOSE_1_22
Miller, G. E. (1990). The assessment of clinical skills/competence/performance. Acad. Med. 65, S63–S67. doi: 10.1097/00001888-199009000-00045
Moonsamy, S., Mupawose, A., Seedat, J., Mophosho, M., and Pillay, D. (2017). Speech-language pathology and audiology in South Africa: reflections on transformation in professional training and practice since the end of apartheid. Perspect. ASHA Spec. Interest Groups 2, 30–41. doi: 10.1044/persp2.SIG17.30
Mophosho, M., Masuku, K. P., and Khoza-Shangase, K. (2022). “Complexities with context: cultural and linguistic diversity challenges in preventive audiology in Africa” in Complexities and challenges in preventive audiology: an African perspective. ed. K. Khoza-Shangase (Cape Town: AOSIS Books).
Morgan, S. D., Zeng, F. G., and Clark, J. (2022). Adopting change and incorporating technological advancements in audiology education, research, and clinical practice. Am. J. Audiol. 31, 1052–1058. doi: 10.1044/2022_AJA-21-00215
Mothemela, B., Manchaiah, V., Mahomed-Asmail, F., and Knoetze, M., and Swanepoel, D. W. (2024). Factors influencing hearing aid use, benefit and satisfaction in adults: a systematic review of the past decade. International Journal of Audiology, 63, 661–674.
Mtimkulu, T. K., Khoza-Shangase, K., and Petrocchi-Bartal, L. (2023). Barriers and facilitators influencing hearing help-seeking behaviors for adults in a peri-urban community in South Africa: a preventive audiology study. Front. Public Health 11:1095090. doi: 10.3389/fpubh.2023.1095090
Nagdee, N., Sebothoma, B., Madahana, M., Khoza-Shangase, K., and Moroe, N. (2022). Simulations as a mode of clinical training in healthcare professions: a scoping review to guide planning in speech-language pathology and audiology during the COVID-19 pandemic and beyond. S. Afr. J. Commun. Disord. 69:905. doi: 10.4102/sajcd.v69i2.905
Peters, M., Godfrey, C., McInerney, P., Soares, C. B., Khalil, H., and Parker, D. (2015). Methodology for JBI scoping reviews. In the Joanna Briggs institute reviewers manual 2015. Adelaide: The Joanna Briggs Institute.
Pillay, D., and Sebothoma, B. (2021). “Educational audiology within the classroom: the use and importance of information and communication technologies” in Empowering students and maximising inclusiveness and equality through ICT. ed. B. Sebothoma (Leiden: Brill), 244–259.
Rashid, M. F. N. B., Quar, T. K., Chong, F. Y., and Maamor, N. (2020). Are we ready for teleaudiology? Data from Malaysia. Speech Lang. Hear. 23, 146–157. doi: 10.1080/2050571X.2019.1622827
Reddy, H., Joshi, S., Joshi, A., and Wagh, V. (2022). A critical review of global digital divide and the role of technology in healthcare. Cureus 14:e29739. doi: 10.7759/cureus.29739
Schiller, E. P., and Malouf, D. B. (2000). “Research syntheses: implications for research and practice” in Contemporary special education research. eds. D. W. Moore and T. Glynn (London: Routledge), 251–262.
Seabi, J., Seedat, J., Khoza-Shangase, K., and Sullivan, L. (2014). Experiences of university students regarding transformation in South Africa. Int. J. Educ. Manag. 28, 66–81. doi: 10.1108/IJEM-01-2012-0017
Sebothoma, B., and Khoza-Shangase, K. (2018). A comparison between video otoscopy and standard tympanometry findings in adults living with human immunodeficiency virus (HIV) in South Africa. S. Afr. J. Commun. Disord. 65, 1–7. doi: 10.4102/sajcd.v65i1.591
Sebothoma, B., Khoza-Shangase, K., Masege, D., and Mol, D. (2022). The use of tele practice in assessment of middle ear function in adults living with HIV during the COVID-19 pandemic. Indian J. Otolaryngol. Head Neck Surg. 74, 3118–3125. doi: 10.1007/s12070-021-02836-x
Seedat, J., Adams, S. N., Coutts, K., Kater, K. A., Sher, J., and Sawasawa, C. (2021). The impact of COVID-19 on transformation in a speech-language pathology university program in South Africa. Perspect. ASHA Spec. Interest Groups 6, 1299–1304. doi: 10.1044/2021_PERSP-21-00086
Sife, A., Lwoga, E., and Sanga, C. (2007). New technologies for teaching and learning: challenges for higher learning institutions in developing countries. Int. J. Educ. Develop. ICT 3, 57–67.
Sukhera, J. (2022). Narrative reviews: flexible, rigorous, and practical. J. Grad. Med. Educ. 14, 414–417. doi: 10.4300/JGME-D-22-00480.1
Suri, H. (2020). “Ethical considerations of conducting systematic reviews in educational research” in Systematic reviews in educational research. eds. O. Zawacki-Richter, M. Kerres, S. Bedenlier, M. Bond, and K. Buntins (Berlin: Springer Nature).
Swanepoel, D. W. (2020). eHealth technologies enable more accessible hearing care. Semin. Hear. 41, 133–140. doi: 10.1055/s-0040-1708510
Tabatabai, S. (2020). Simulations and virtual learning supporting clinical education during the COVID 19 pandemic. Adv. Med. Educ. Pract. 11, 513–516. doi: 10.2147/AMEP.S257750
Thomas, A., Lubarsky, S., Varpio, L., Durning, S. J., and Young, M. E. (2020). Scoping reviews in health professions education: challenges, considerations and lessons learned about epistemology and methodology. Adv. Health Sci. Educ. 25, 989–1002. doi: 10.1007/s10459-019-09932-2
Townsend, B. A., and Thaldar, D. W. (2020). Navigating uncharted waters: Biobanks and informational privacy in South Africa. South African Journal on Human Rights. 35, 329–350. doi: 10.1080/02587203.2020.1717366
Vergnes, J. N., Marchal-Sixou, C., Nabet, C., Maret, D., and Hamel, O. (2010). Ethics in systematic reviews. J. Med. Ethics 36, 771–774. doi: 10.1136/jme.2010.039941
Watermeyer, J., and Kanji, A. (2024). Lessons from an exploratory qualitative survey on simulation opportunities for clinical education in speech-language pathology and audiology in South Africa. Teach. Learn. Med. 37, 430–440. doi: 10.1080/10401334.2024.2362878
Watermeyer, J., and Kater, K. A., and Khumalo, G. (2022). Experiences of a pediatric speech-language teletherapy practical at a South African university training site during COVID-19: an exploratory qualitative study. The Clinical Supervisor, 41,149–166. doi: doi: 10.1080/07325223.2022.2114567
Woldegiorgis, E. T., and Chiramba, O. (2024). Access and success in higher education: fostering resilience in historically disadvantaged students in South Africa. J. Appl. Res. High. Educ. 17, 759–771. doi: 10.1108/JARHE-05-2023-0217
World Health Organization (2022). Global competency framework for universal health coverage. Geneva: World Health Organization.
Keywords: audiology education, tele-audiology, virtual simulations, COVID-19, clinical teaching, South Africa, narrative review, technological advancements
Citation: Khoza-Shangase K (2025) Narrative review on embracing advances in technology for clinical teaching and learning in audiology: opportunities delivered by COVID-19 to the South African academy. Front. Educ. 10:1551800. doi: 10.3389/feduc.2025.1551800
Edited by:
Jie Hou, Chongqing University of Posts and Telecommunications, ChinaReviewed by:
Noble Lo, Lancaster University, United KingdomOpeoluwa I. Akinradewo, University of the Free State, South Africa
Copyright © 2025 Khoza-Shangase. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Katijah Khoza-Shangase, S2F0aWphaC5LaG96YS1TaGFuZ2FzZUB3aXRzLmFjLnph
†ORCID: Katijah Khoza-Shangase, orcid.org/0000-0002-6220-9606
 Katijah Khoza-Shangase
Katijah Khoza-Shangase