- 1Department of Obstetrics and Gynecology, The First Affiliated Hospital of Dalian Medical University, Dalian, China
- 2Department of Obstetrics and Gynecology, Shanghai Putuo District Central Hospital, Shanghai, China
- 3Department of Obstetrics and Gynecology, Women and Children’s Hospital of Tibet Autonomous Region, Lhasa, China
Objective: Building on our previous study of obstetrics and gynecology outpatients, this study examined inpatients’ acceptance of medical student participation by gender and nationality, and compared findings with outpatient data, attempting to identify potential factors that can balance the patient’s experience and the learning outcomes of medical students.
Methods: Selected patients hospitalized in the obstetrics and gynecology wards of a tertiary teaching hospital in China from October 2023 to June 2024 were surveyed and statistically analyzed through the distribution of questionnaires. A total of 750 inpatient questionnaires were distributed, and ultimately 692 usable questionnaires were obtained. Acceptance rates were compared across four groups: Chinese female, Chinese male, international female, and international male medical students. Multivariate analysis identified factors associated with acceptance.
Results: Among inpatient respondents, acceptance rates for clinical participation by Chinese female, international female, Chinese male, and international male medical students were 71.7%, 70.5%, 51.4%, and 45.7%, respectively. Overall, the acceptance rate is higher than that of outpatients. Regardless of being outpatients or inpatients, the main reason for refusing international medical students is “language barriers.” The analysis shows that physicians sharing more information about the disease is an independent influencing factor affecting inpatients’ acceptance of medical students of all types.
Conclusion: Promoting the hospital’s teaching role and fostering a sense of altruism, alongside medical students increasing communication with patients, sharing more medical knowledge, and especially international students improving their Chinese language and interpersonal skills, may increase acceptance of medical student participation in obstetrics and gynecology internships by Chinese patients.
1 Introduction
Clinical internships, as an important component of medical talent training, provide essential opportunities for developing clinical skills and enhancing doctor-patient communication (Coleman and Murray, 2002). Obstetrics and gynecology (Ob/Gyn) present unique challenges compared to other clinical specialties, with the patient population exclusively female. They may be less comfortable due to the private and sensitive nature of the field. This discomfort can create obstacles for medical students in clinical internships, especially for males (Nguyen et al., 2022). A study at the University of Brasilia indicated that 18.3% of Ob/Gyn patients were willing to have only female students participate in their care (Wanderley et al., 2019). Similarly, research in China showed that only 30.1% of patients accepted student involvement during gynecological physical examinations (Ling et al., 2010). Attitudes toward student involvement are particularly negative in obstetrics compared to gynecology (Jiang, 2016). Concerns about potential risks associated with student participation are also prevalent among instructors at Chinese teaching hospitals (Li et al., 2007). Cultural factors play a significant role in this resistance. In the article from the preliminary survey, we have detailed the origins of Chinese traditional culture. Such cultural beliefs might make Chinese patients less comfortable with male medical students, particularly in the Ob/Gyn field.
In addition to domestic students, a large proportion of international students must also participate in clinical clerkships. Under the influence of educational globalization and the “Belt and Road” initiative, talent exchange between countries is becoming increasingly frequent. China has seen a rising number of international medical students enrolling in its universities. According to the latest data update in China, in the academic year of 2023–2024, domestic medical institutions alone admitted a total of 3,048 international students (China general office of the ministry of education, 2024). Because of purely English-speaking clinical settings, language barriers may heighten patient discomfort and lead to higher refusal rates (Wang et al., 2022). However, research from other countries suggests that patient acceptance of medical students may be higher than expected (Mwaka et al., 2022; Woolner and Cruickshank, 2015). This negative expectation makes medical students lack a sense of identification with the profession of obstetrician-gynecologist. Therefore, we need to gain an in-depth understanding of patients’ acceptance of different types of students and the influencing factors, in order to further improve the effectiveness of internships.
Quantitative research on this topic in China remains very limited. Previously, our team conducted a study on patient acceptance of student participation in Ob/Gyn outpatient settings. Among the 501 patients who were surveyed with questionnaires, the acceptance rates for the four groups of students (Chinese female, international female, Chinese male, and international male) were 59.7%, 55.9%, 32.1%, and 25.9%, respectively. Regardless of nationality, patients in Ob/Gyn were more likely to accept female students than males, with the lowest acceptance rate for international male students (Xiao et al., 2020). However, during a single outpatient visit, the communication time between doctors and patients is limited, which is a significant difference from the ample communication during hospitalization. This increased interaction may affect patients’ attitudes. On the basis of previous work, this study again used a questionnaire based on relevant international survey models (Hartz and Beal, 2000; Rizk et al., 2002; Mavis et al., 2006; Saeed et al., 2007; Koh et al., 2010; Gil-Santos et al., 2022), adapted to the Chinese healthcare context. A cross-sectional survey was conducted with Ob/Gyn inpatients at a teaching hospital to compare and summarize the data obtained from outpatient surveys in previous work, to obtain more comprehensive data and conclusions.
2 Materials and methods
2.1 Background
The First Affiliated Hospital of Dalian Medical University is a teaching hospital where medical students complete Ob/Gyn rotations involving both outpatient and inpatient settings. Students acquire skills in history-taking, pelvic and obstetric examinations, and assist in surgeries and post-operative care. At the end of the rotation, students are evaluated through written and skill-based exams. Upon completion, students are expected to demonstrate proficiency in the fundamental principles, knowledge, and skills related to common Ob/Gyn conditions.
2.2 Study design
This study is a cross-sectional survey targeting Ob/Gyn inpatients in our hospital. Two graduate students in Ob/Gyn received unified training in the research protocol. After obtaining patient consent, they distributed copies of the survey questionnaire to the patients and guided them to fill it out independently. For patients who were unable to read or write, the survey was conducted face-to-face and the responses were recorded. Ethical approval for this study was obtained from the Ethics Committee of the First Affiliated Hospital of Dalian Medical University (Record No. YJ-KY-FB-2023-01).
2.3 Participants and sample size
This follow-up study targeted inpatients rather than outpatients. The two groups operate in distinct clinical environments and exhibit different psychological characteristics; building on our earlier outpatient data, the aim was to obtain more comprehensive information and enhance comparability.
The respondents were selected through simple random sampling based on their hospital admission numbers. Using the hospital’s daily admission list, we first compiled a complete roster of all eligible inpatients each day to form the sampling frame. We then employed a random-number table to draw the required sample without replacement until the predetermined target of 750 participants was reached.
Inclusion criteria: Age >18 years; mentally competent; hospitalized for more than 3 days; patients’ health status allows them to communicate. A total of 750 surveys were distributed between October 2023 and June 2024. Of these, thirty-three were incomplete, and twenty-five were invalid due to patient withdrawal. The final sample size was 692, with a response rate of 92%.
2.4 Questionnaire design and content
The questionnaire was adapted from international survey models, modified to fit the Chinese healthcare setting, and combined with our team’s previous investigation of outpatients in Ob/Gyn.
The first part of the questionnaire consists of basic demographic information. The second part focuses on the patients’ experiences with medical student participation during their current hospital stay. Since this survey targets inpatients, the questionnaire includes additional closed-ended questions about whether there are any different communication behaviors between doctors and patients during hospitalization. This section focuses more on exploring the impact of different in-hospital communication behaviors on the acceptance of medical students by Ob/Gyn inpatients. The third part explores the possible reasons why respondents accept or refuse medical students. The questionnaire lists various potential factors that may influence patients’ acceptance or refusal, allowing for one or multiple selections, with blank options for patients to add their own reasons. At the end of the questionnaire, there is a section on the acceptance of different types of medical students, based on communication and experiences with medical students during the current hospital stay. Since previous studies have shown that patients have different acceptance levels for male and female students, the questionnaire mainly investigates patients’ acceptance of the following four specific types of medical students (i.e., Chinese females, Chinese males, international females, international males). A subset of items employed a 5-point Likert scale, and the questionnaire asked patients to rate their level of acceptance on a sequential scale from 1 to 5 (1 = Strongly Agree, 2 = Agree, 3 = Neutral, 4 = Disagree, 5 = Strongly Disagree).
The preliminary survey questionnaire was first pre-tested among 50 Ob/Gyn inpatients, and we conducted reliability and validity analyses for the subset of items designed with a Likert scale. Based on feedback, the questionnaire was revised to form the final version. The questionnaire demonstrated excellent internal consistency (Cronbach’s α = 0.874). The KMO value was 0.642 (likely attributable to the limited number of items). Bartlett’s test of sphericity was significant (χ2 = 1706.933, df = 6, p < 0.001). A single factor explained 72.813% of the variance, with all factor loadings exceeding 0.82, indicating stable construct validity.
The translated questionnaire can be found in the Supplementary materials.
2.5 Statistical analysis
Most data were analyzed using descriptive statistics. Categorical data were analyzed using chi-square tests. Statistical significance was set at p < 0.05. Variables that were statistically significant in the univariate analysis were entered into a multinomial logistic regression model. Adjusted odds ratios (ORs) with corresponding 95% confidence intervals were calculated for each independent variable, and model fit was assessed using standard goodness-of-fit procedures. All analyses were performed with SPSS (Version 27.0).
3 Results
3.1 Sociodemographic characteristics of patients
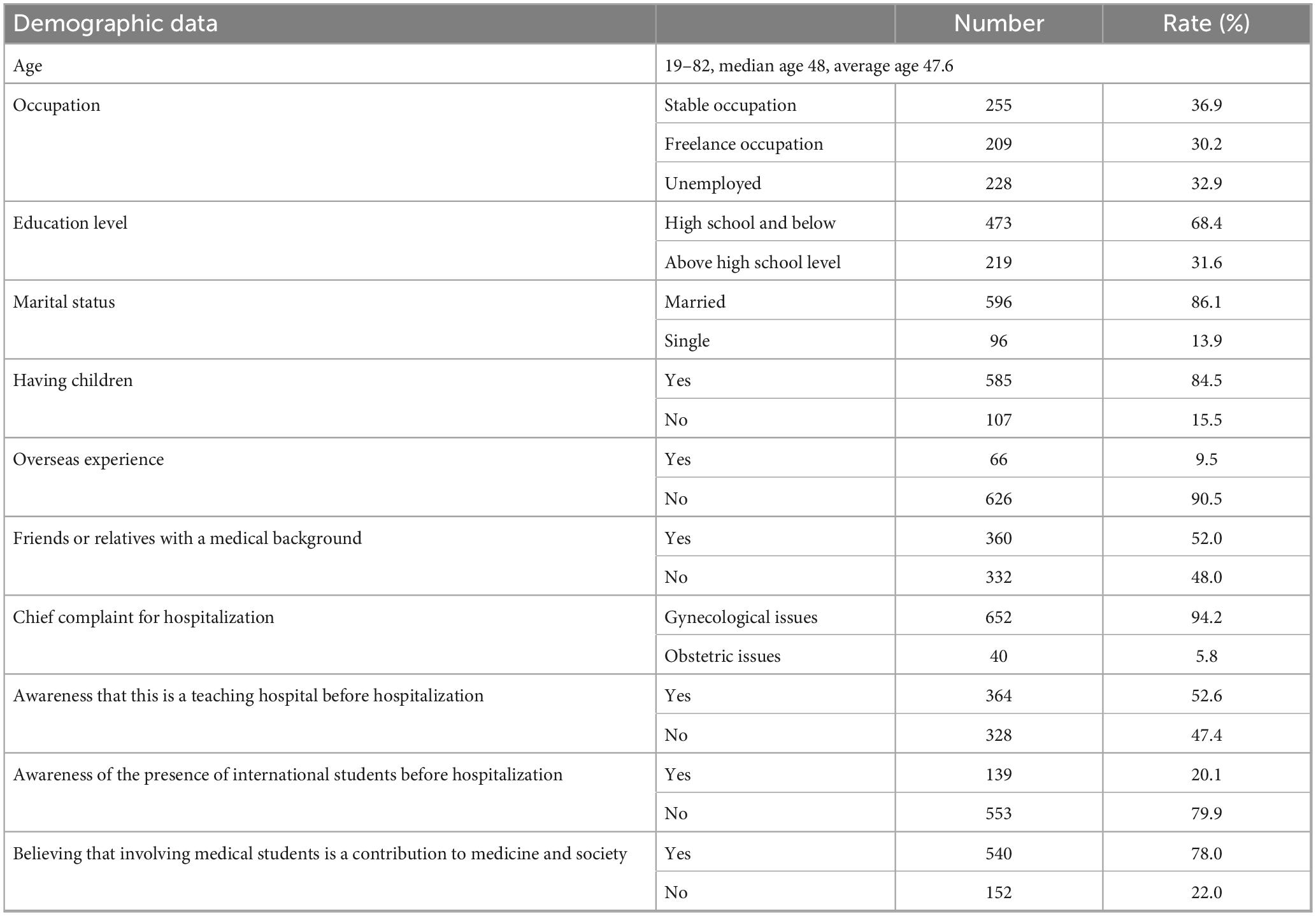
The sociodemographic information of the 692 Ob/Gyn inpatient respondents is summarized in Table 1. The median age of the patients was 48 years old, with the majority being married and having given birth, and the current hospitalization was due to gynecological issues. Over half of the respondents had a high level of education and a career, with a minority having overseas experience. About half of the patients had friends or relatives with a medical background, and approximately half of the patients were aware that medical students might be present before this hospitalization, but only 20.1% knew that the hospital also had international students. Most patients (78.0%) viewed their acceptance of medical student involvement as a contribution to society and medicine.
3.2 Patient attitudes toward different medical students
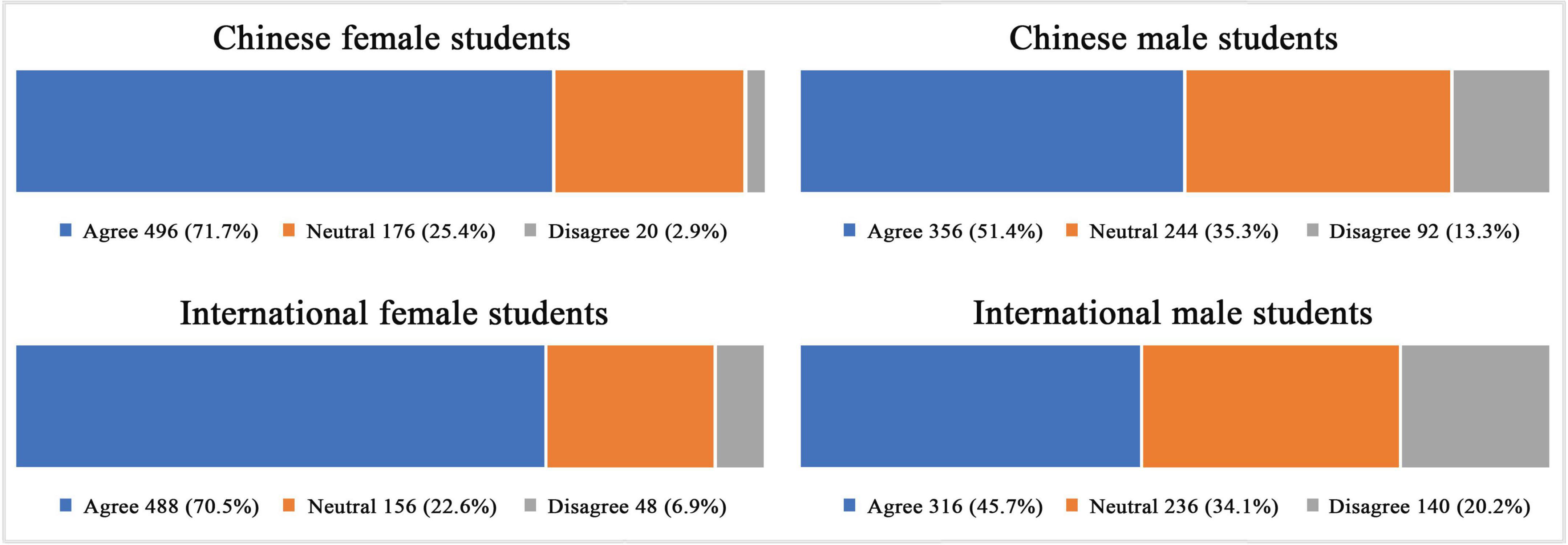
The different attitudes of patients toward medical students of different nationalities and genders are shown in Figure 1. For ease of analysis, responses indicating “Strongly agree” and “Agree” were combined into “Agree,” while “Strongly disagree” and “Disagree” were combined into “Disagree,” the “Neutral” option remains unchanged. Statistical analysis revealed that approval of Chinese female students was highest at 71.7%, followed closely by international female students at 70.5%, with no statistically significant difference between these groups. Among all categories of students, international males faced the lowest acceptance rate at 45.7%. However, acceptance of Chinese male students was slightly higher at 51.4%, with a statistically significant difference (p < 0.05).
3.3 Potential reasons for acceptance and refusal
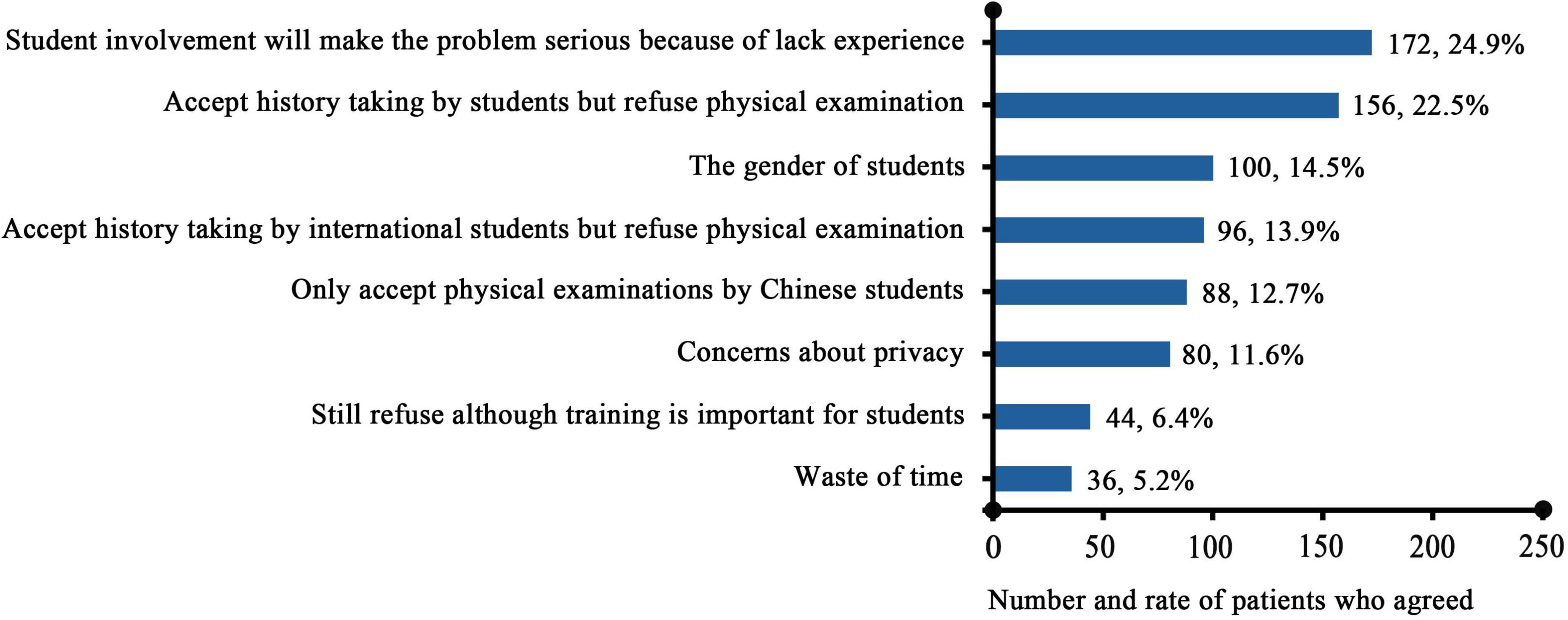
Among the reasons that patients accept medical student participation, the leading ones include viewing it as a contribution to medicine and society (68.8%), a willingness to allow participation if it is non-harmful (53.8%), and concerns about future healthcare availability (48.6%), the remaining reasons are shown in Figure 2. In contrast, the main reason for rejection (Figure 3) was the perception that students lack experience and may worsen conditions (n = 172, 24.9%). Additionally, 22.5% of inpatients (n = 156) were comfortable with medical students taking medical histories but rejected their involvement in physical contact procedures. The primary reason for rejecting international students was language barriers (n = 316, 45.7%) (Figure 4).
3.4 Factors that may promote the acceptance of student participation by Ob/Gyn patients
Results in Table 2 indicate that the acceptance of male students was significantly increased in patients who had given birth, regardless of nationality (χ2 = 6.240–14.569, p < 0.05). Patients who perceive student participation as beneficial to medicine and society are more likely to accept medical students, except for international females (χ2 = 6.651–15.894, p < 0.05). In addition, prior awareness that the hospital is a teaching institution was associated with greater acceptance of only Chinese male students, while being aware in advance that the hospital has international students increases the acceptance of international female students.
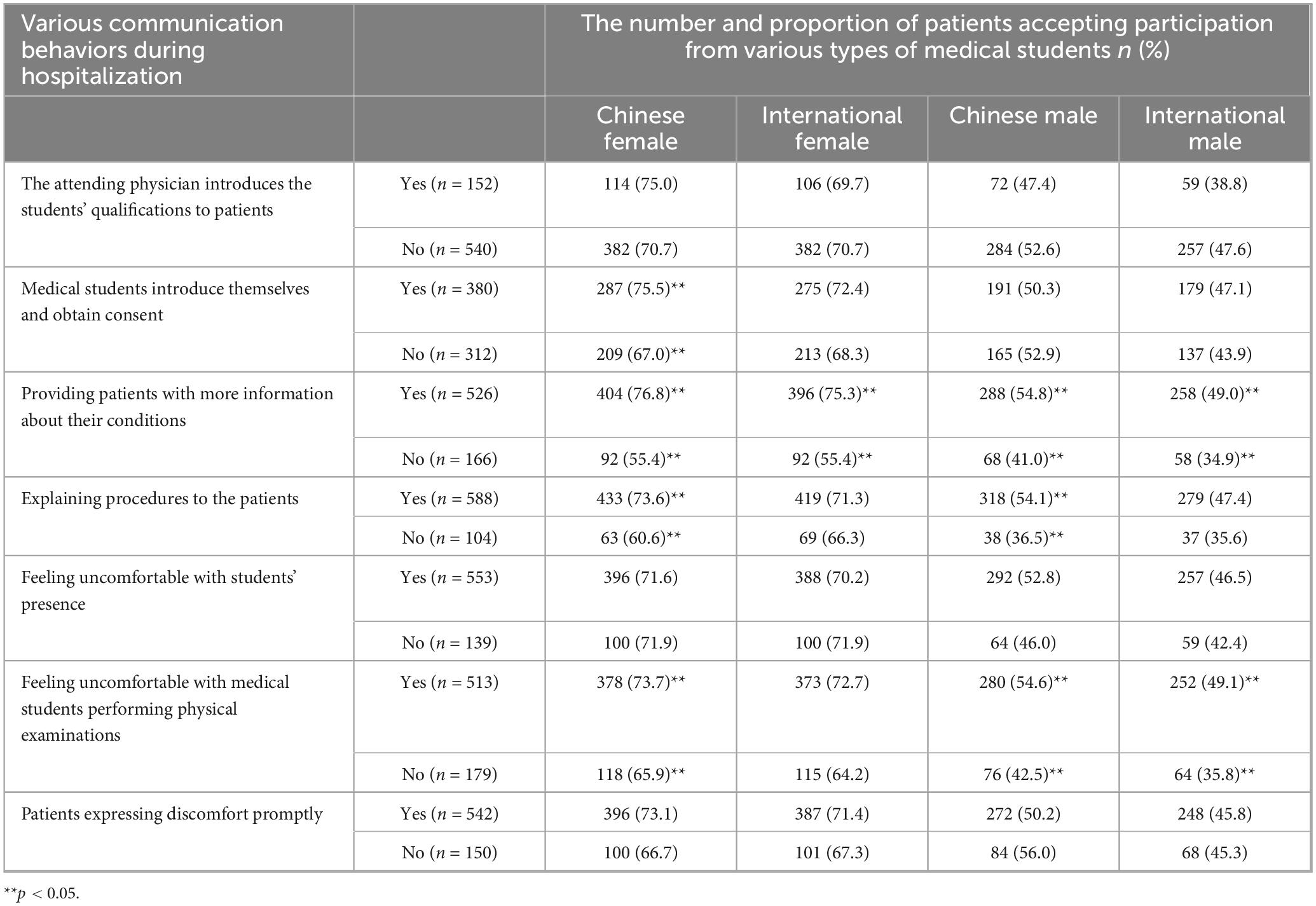
During hospitalization, patients have more opportunities to communicate with doctors and students than in a single outpatient visit. We found that certain in-hospital communication behaviors may affect patients’ acceptance of medical students (As shown in Table 3). For all students, providing patients with more information about their conditions increased acceptance rates (χ2 = 11.019–30.433, p < 0.05). In all cases except for international female students, the critical factor affecting acceptance was whether patients felt uncomfortable with medical students performing physical examinations (χ2 = 8.078–11.414, p < 0.05). The key in-hospital communication behaviors that improved acceptance of Chinese students included students explaining procedures to the patients (χ2 = 9.507–12.697, p < 0.05). In addition, medical students introducing themselves and obtaining consent can increase the acceptance of Chinese female students.
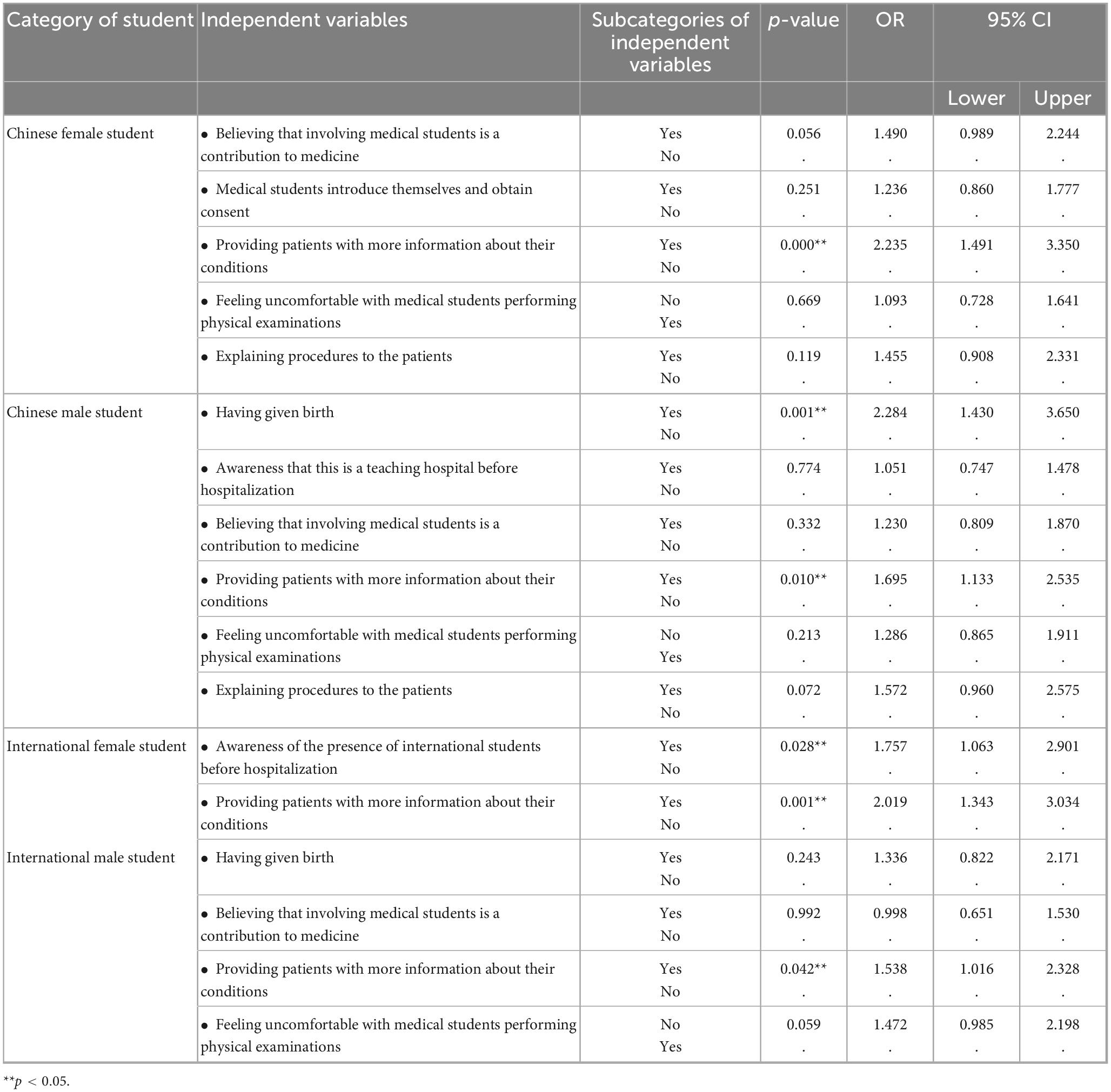
3.5 Multinomial logistic regression analysis
A multinomial logistic regression analysis was performed to examine the potential interactions between the univariate factors listed in Tables 2, 3. Patient attitudes toward the four types of medical students (1 = Agree, 2 = Neutral, 3 = Disagree) were set as the dependent variable, and the factors identified in the univariate analysis (p < 0.05) were included as independent variables. In the model-fit tests, the omnibus χ2 tests (comparing the null with the final models) were significant (p < 0.001) across the four models. Nagelkerke R2 values were 0.079, 0.111, 0.061 and 0.046 for Chinese female, Chinese male, international female and international male students, respectively. Goodness-of-fit Pearson/Deviance tests yielded p = 0.010/0.012 for the international female model, while the other three models had p < 0.001; this is likely due to the large-sample sensitivity. Regardless, our models are statistically significant and offer meaningful, albeit limited, explanatory power over the null models. The analysis demonstrated that physicians sharing more disease-related information during the encounter was an independent predictor of inpatients’ willingness to accept medical student participation, irrespective of the students’ nationality or gender. The adjusted odds ratios (95% confidence intervals) were 2.235 (1.491–3.350) for Chinese female students, 1.695 (1.133–2.535) for Chinese male students, 2.019 (1.343–3.034) for international female students, and 1.538 (1.016–2.328) for international male students (As shown in Table 4).
4 Discussion
Our current study follows up on the attitudes of Ob/Gyn outpatients by examining the attitudes and influencing factors of inpatients toward medical student participation in internships. In this survey, we found some similarities and significant differences in the attitudes of inpatients and outpatients. We discovered that inpatients’ acceptance rates for the four types of students (Chinese female, international female, Chinese male, international male) are 71.7%, 70.5%, 51.4%, and 45.7%, respectively, which are significantly higher than the acceptance rates of outpatients (59.5%, 55.7%, 31.9%, 25.8%) (Xiao et al., 2020), this is the research data from our team’s previously published study. Additionally, since inpatients have more opportunities to communicate with attending physicians and medical students than during a single outpatient visit, we have made some other discoveries regarding factors that affect patient acceptance. Using multinomial logistic regression analysis, we found that if physicians share more knowledge about the disease during the medical student participation, more patients would choose to accept, regardless of their nationality and gender.
Inpatients are more likely to accept the involvement of various types of students compared to outpatients. This is due to the differences in diagnostic and treatment content and the characteristics of the areas between outpatient and inpatient settings. On one hand, during hospitalization, the frequency of communication between patients, doctors, and medical students increases, allowing for the establishment of a good trust relationship. Moreover, when students are involved, patients receive more explanations about their conditions, as the teaching process itself is a sharing of medical knowledge. Previous studies have also shown similar situations (Woolner and Cruickshank, 2015; Esguerra et al., 2014). When the attending physician conducts bedside teaching, more than two-thirds (67.55%) of the participants understand their conditions better than before and consider it a pleasant experience (Mohamed et al., 2024). On the other hand, patients are more psychologically vulnerable in a hospital setting, making them more dependent on and trusting of medical staff. A study from the King Edward Memorial Hospital in Western Australia found similar results, with women in both gynecology and obstetrics wards showing significantly higher overall satisfaction with medical student involvement in their care compared to outpatients (Carmody et al., 2011). It is also possible that inpatients have more severe conditions, focusing more on their health and less on the medical students, thus increasing acceptance rates.
Another difference compared to outpatients is that the main reason for inpatients to refuse students is the concern that the students’ lack of experience might exacerbate the problem, which is understandable. Given the severity of inpatients’ conditions, people often prefer “experts” for diagnosis and treatment. This may also stem from distrust of students or young doctors or previous unpleasant experiences. A recent study in Saudi Arabia also mentioned that when patients were asked whether they would allow students to be in the operating room during surgical interventions, the refusal rate increased dramatically. They worry that students might participate in surgical operations, leading to unexpected outcomes (Iqbal et al., 2020). Medical students are often perceived as immature doctors who are still learning and growing, with professional skills that cannot be assessed, leading to concerns that their involvement might affect communication and normal treatment with doctors.
As previously stated, inpatients and outpatients share similarities. First, acceptance rates for female students were significantly higher than for males, which aligns with expectations and mirrors findings from other studies (Rizk et al., 2002; Mohamed et al., 2024; Iqbal et al., 2020; Subki et al., 2018). This is largely attributed to cultural norms. Gynecological conditions often involve privacy, and some conditions are difficult to discuss, making female patients more likely to refuse male students. In a survey from the United Arab Emirates, some patients even considered male students to be malicious individuals (McLean et al., 2010). Patient biases regarding gender may hinder male students’ participation in clinical practice, potentially diminishing their confidence and interest in Ob/Gyn and possibly deterring them from pursuing this specialty in the future (Wanderley et al., 2019; Wanderley and Sobral, 2017; Riedel et al., 2022). According to the “China Health Statistics Yearbook 2022,” in 2021, among maternal and child health care institutions in China, the percentage of male practicing (assistant) physicians was 26.5%, while for females it was 73.5%. However, among the national practicing (assistant) physicians, the male-to-female ratio was 52.5 to 47.5% (China Health Statistical Yearbook, 2022). Additionally, over the past two decades, there has been a significant decrease in the number of male graduates choosing to become obstetric and gynecological residents in Brazil (p 0.002), while there has been no significant change among female graduates (Wanderley et al., 2019; Wanderley and Sobral, 2017).
0.002), while there has been no significant change among female graduates (Wanderley et al., 2019; Wanderley and Sobral, 2017).
Secondly, both inpatients and outpatients attribute the refusal of international students to communication barriers. Most of them are visiting China for the first time, and they have been studying in English in their home countries without exposure to Chinese. Their learning of Chinese began only after enrollment, and the rarity of all-English scenarios during internships prevents smooth and successful communication with patients, thus becoming a key factor in the refusal of international students. 45.7% of patients believe that if communication with international students were as smooth as with students whose first language is Chinese, they would accept them. Australian research found that whether medical students have English as their first language significantly affects patient satisfaction with student involvement in Ob/Gyn internships, as well as their ratings of the medical students’ professional skills (Carmody et al., 2011). Helping international students improve their Chinese proficiency not only aids in their learning of professional skills but also allows them to understand more about Chinese culture. Communicating smoothly with patients in a manner that is familiar to the Chinese people can increase their acceptance. The exchange of talent is not only about professional skills but also includes the exchange and promotion of culture.
Not only the language barrier, but also due to differences in geographical and cultural backgrounds, international students find it difficult to gain patients’ acceptance. Generally, they are more accepted during medical history inquiries, but less so during specialized examinations (Hamza et al., 2020). To address the difficulties, we have undertaken several initiatives. These include offering Chinese language courses (including medical Chinese), courses on Chinese culture, personalized teaching, simulation-based instruction, and pairing international and domestic students in a “1 + 1” arrangement during their internships. This allows them to reduce communication barriers and increasing patient acceptance. However, it is also crucial for the students themselves to make efforts. In this study, 23.7% of patients indicated that they would accept international students if their demeanor were more friendly. During the internship process, medical students should introduce themselves appropriately, and provide clear explanations before performing procedures, which does not necessarily lead to rejection due to revealing their student status. On the contrary, they will gain more acceptance. In a qualitative study conducted in Ireland using semi-structured interviews, some patients even expressed a preference for dealing with younger doctors, as they felt older doctors causing them to feel nervous. If they feel uncomfortable or the students are disrespectful in their approach, they will be rejected (Carty et al., 2020). Studies have also suggested that these findings indicate future training should place more emphasis on cultivating students’ confidence, communication skills, and professionalism so that patients show a more tolerant attitude toward medical students (Iqbal et al., 2020).
The similarities and differences in attitudes toward medical students between Ob/Gyn outpatients and inpatients, as found in related studies and this study, are summarized in Table 5.

Table 5. Similarities and differences in the attitudes of outpatients and inpatients toward student internships.
The main strength of this study is that, building on the previous survey of Ob/Gyn outpatients, we conducted a cross-sectional survey on a considerable scale of inpatients, providing a good basis for comparison and reference. This allows for a more comprehensive understanding of the situation of both outpatients and inpatients in Ob/Gyn in China, obtaining quantified research data and offering a certain reference for the planning of medical education policies.
Limitations of the present study are as follows. First, the data were collected from a single tertiary teaching hospital. The attitudes of inpatients at this institution may not reflect the broader cultural or regional diversity of the country. Future studies should incorporate multiple centers to enhance generalizability. Second, social-desirability bias is a potential confounder, as patients surveyed within the hospital may feel pressured to respond positively, which could inflate reported acceptance of medical-student involvement. Third, we did not control for prior exposure to medical students, a factor that may also influence patients’ attitudes. In addition, although the questionnaire was pre-tested in a small group, its predominantly closed-ended format may have overlooked other reasons for acceptance or refusal. Future research could combine qualitative methods (such as in-depth interviews or open-ended surveys) to achieve more comprehensive findings. Finally, this study treated all international students as a homogeneous group. In reality, patient responses may vary according to students’ language fluency, appearance, or cultural behavior. These variables were not measured, and future studies are encouraged to perform subgroup analyses to yield more nuanced data.
5 Conclusion
The acceptance of clinical practice involvement by different types of medical students is higher among Ob/Gyn inpatients compared to outpatients. Based on the analysis of factors affecting patient acceptance, the following targeted efforts can be made to improve patient acceptance of medical student: 1) Strengthen the promotion of the attributes of teaching hospitals and medical ethics, advocating that there is no gender distinction in front of a physician, while also enhancing the cultural and educational propaganda of altruistic thinking across society. 2) Medical students should improve their communication skills, engage more with inpatients, and share more medical knowledge, encourage international medical students to understand and learn about Chinese culture and to improve their proficiency in the Chinese language to communicate with patients in a manner familiar to the Chinese. 3) Teaching administrators and instructors need to make reasonable internship arrangements based on the different situations of patients and medical students to enhance acceptance.
Data availability statement
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Committee of the First Affiliated Hospital of Dalian Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LB: Data curation, Investigation, Writing – review & editing. MZ: Writing – review & editing, Conceptualization, Visualization. CL: Methodology, Software, Writing – review & editing. MT: Supervision, Writing – review & editing. NG: Supervision, Writing – review & editing. Deqiong: Conceptualization, Writing – review & editing. ZX: Writing – review & editing, Formal analysis.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The research was supported by the corresponding author Zhen Xiao’s personal funding, the Xingliao Talent Program (Project No. YXMJ-QN-14), the University-level Teaching Reform Research Project of Dalian Medical University (Project No. DYLX24003), and the Lhasa Science and Technology Program (Project No. LSKJ202505).
Acknowledgments
All the authors wish to express their gratitude to the participants who volunteered for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2025.1660085/full#supplementary-material
References
Carmody, D., Tregonning, A., Nathan, E., and Newnham, J. P. (2011). Patient perceptions of medical students’ involvement in their obstetrics and gynaecology health care. Aust. N. Z. J. Obstet Gynaecol. 51, 553–558. doi: 10.1111/j.1479-828X.2011.01362.x
Carty, M., O’Riordan, N., Ivers, M., and Higgins, M. F. (2020). Patient perspectives of bedside teaching in an obstetrics, Gynaecology and neonatology hospital. BMC Med. Educ. 20:111. doi: 10.1186/s12909-020-02016-5
China general office of the ministry of education (2024). List of Universities Admitting Undergraduate Clinical Medicine Program (Taught in English) for International Students in the 2023-2024 Academic Year and Admission Plans. Available online at: http://www.moe.gov.cn/srcsite/A20/moe_850/202305/t20230530_1061988.html (accessed September 12, 2024).
China Health Statistical Yearbook (2022). National Health Commission Statistics and Information Center. Available online at: https://www.nhc.gov.cn/mohwsbwstjxxzx/tjtjnj/tjsj_list.shtml (accessed February 20, 2024).
Coleman, K., and Murray, E. (2002). Patients’ views and feelings on the community-based teaching of undergraduate medical students: A qualitative study. Fam. Pract. 19, 183–188. doi: 10.1093/fampra/19.2.183
Esguerra, R., Toro, J., Ospina, J. M., Porras, A., Diaz, C., and Reyes, S. (2014). The transition to a teaching hospital: Patient satisfaction before and after the introduction of medical students. Med. Teach. 36, 710–714. doi: 10.3109/0142159X.2014.907877
Gil-Santos, I., Santos, C. C., and Duarte, I. (2022). Medical education: Patients’ perspectives on clinical training and informed consent. Int. J. Environ. Res. Public Health 19:7611. doi: 10.3390/ijerph19137611
Hamza, A., Warczok, C., Meyberg-Solomayer, G., Takacs, Z., Juhasz-Boess, I., Solomayer, E. F., et al. (2020). Teaching undergraduate students gynecological and obstetrical examination skills: The patient’s opinion. Arch. Gynecol. Obstet. 302, 431–438. doi: 10.1007/s00404-020-05615-1
Hartz, M. B., and Beal, J. R. (2000). Patients’ attitudes and comfort levels regarding medical students’ involvement in obstetrics-gynecology outpatient clinics. Acad. Med. 75, 1010–1014. doi: 10.1097/00001888-200010000-00018
Iqbal, M. Z., Bukhamsin, E. Y., Alghareeb, F. Y., Almarri, N. M., Aldajani, L. M., and Busaleh, H. A. (2020). Participation of medical students in patient care: How do patients perceive it? J. Family Med. Prim Care 9, 3644–3651. doi: 10.4103/jfmpc.jfmpc_130_20
Jiang, N. (2016). Investigation of Clinical Teaching and Doctor-Patient Relationship in Obstetrics and Gynecology. Mauranipur: Knowledge Library.
Koh, G. C., Wong, T. Y., Cheong, S. K., Lim, E. C., Seet, R. C., Tang, W. E., et al. (2010). Acceptability of medical students by patients from private and public family practices and specialist outpatient clinics. Ann. Acad. Med. Singap. 39, 555–510. doi: 10.47102/annals-acadmedsg.V39N7p555
Li, C. M., Pan, X. L., Ouyang, Y. W., and Xu, L. Z. (2007). Survey of the psychological status of patients on clinical clerkship in obstetrics and gynaecology. China High. Med. Educ. 14:35. doi: 10.3969/j.issn.1002-1701.2007.04.008
Ling, J. W., Chen, M. L., Deng, Y., and Wang, Z. L. (2010). Investigation on the patients’ attitudes towards medical students in obstetrics and gynecology department. Chin. J. Med. Educ. 30, 265–267. doi: 10.3760/cma.j.issn.1673-677X.2010.02.041
Mavis, B., Vasilenko, P., Schnuth, R., Marshall, J., and Jeffs, M. C. (2006). Medical students’ involvement in outpatient clinical encounters: A survey of patients and their obstetricians-gynecologists. Acad. Med. 81, 290–296. doi: 10.1097/00001888-200603000-00023
McLean, M., Al Ahbabi, S., Al Ameri, M., Al Mansoori, M., Al Yahyaei, F., and Bernsen, R. (2010). Muslim women and medical students in the clinical encounter. Med. Educ. 44, 306–315. doi: 10.1111/j.1365-2923.2009.03599.x
Mohamed, E. R., Almulhem, M. A., AlElq, A. H., Zeeshan, M., Alharbi, R. S., Almuhanna, A. E., et al. (2024). Obstetrics and gynecology patients’ perceptions about bedside teaching at a Saudi teaching hospital. J. Family Commun. Med. 31, 168–175. doi: 10.4103/jfcm.jfcm_229_23
Mwaka, A. D., Taremwa, S., Adoch, W., Achan, J., Ainembabazi, P., Walego, G., et al. (2022). Patients’ attitudes towards involvement of medical students in their care at university teaching hospitals of three public universities in Uganda: A cross sectional study. BMC Med. Educ. 22:519. doi: 10.1186/s12909-022-03576-4
Nguyen, B. T., Streeter, L. H., Reddy, R. A., and Douglas, C. R. (2022). Gender bias in the medical education of obstetrician-gynaecologists in the United States: A systematic review. Aust. N. Z. J. Obstet Gynaecol. 62, 349–357. doi: 10.1111/ajo.13511
Riedel, M., Hennigs, A., Dobberkau, A. M., Riedel, C., Bugaj, T. J., Nikendei, C., et al. (2022). The role of gender-specific factors in the choice of specialty training in obstetrics and gynecology: Results from a survey among medical students in Germany. Arch. Gynecol. Obstet. 305, 129–137. doi: 10.1007/s00404-021-06232-2
Rizk, D. E., Al-Shebah, A., El-Zubeir, M. A., Thomas, L. B., Hassan, M. Y., and Ezimokhai, M. (2002). Women’s perceptions of and experiences with medical student involvement in outpatient obstetric and gynecologic care in the United Arab Emirates. Am. J. Obstet Gynecol. 187, 1091–1100. doi: 10.1067/mob.2002.126284
Saeed, F., Kassi, M., Ayub, S., Rehman, R., Kasi, P. M., and Rizvi, J. H. (2007). Factors influencing medical student participation in an obstetrics and gynaecology clinic. J. Pak. Med. Assoc. 57, 495–498.
Subki, A. H., Algethami, M. R., Addas, F. A., Alnefaie, M. N., Hindi, M. M., and Abduljabbar, H. S. (2018). Women’s perception and attitude to medical students’ participation in obstetrics and gynecology care. Saudi Med. J. 39, 902–909. doi: 10.15537/smj.2018.9.22668
Wanderley, M. D. S., and Sobral, D. T. (2017). Ob-Gyn gender preferences of gynecology ambulatory patients and students’ choice of the specialty. Rev. Bras. Ginecol. Obstet. 39, 645–646. doi: 10.1055/s-0037-1606840
Wanderley, M. D. S., Sobral, D. T., Lima, B. A. O., Freire, M. E. B., Campos, D. S. M. A., Goncalves, R. M. P. S., et al. (2019). Attitudes and personal attributes regarding patient receptivity towards the participation of medical students in gynecological consultations: A cross-sectional study. Rev. Bras. Ginecol. Obstet. 41, 613–620. doi: 10.1055/s-0039-1697984
Wang, S. Y., Lei, H., Yu, M. X., Liu, C. A., and Wang, H. L. (2022). Investigation on the approaches to enhance the quality of clinical internship for MBBS international students. China High. Med. Educ. 1:40. doi: 10.3969/j.issn.1002-1701.2022.01.017
Woolner, A., and Cruickshank, M. (2015). What do pregnant women think of student training? Clin. Teach. 12, 325–330. doi: 10.1111/tct.12312
Keywords: Clinical internship, patient acceptance, medical students, international students, Chinese inpatients
Citation: Bai L, Zhao M, Lu C, Tao M, Gao N, Deqiong and Xiao Z (2025) Gender but not nationality matters: acceptance of international and domestic medical student participation in obstetrics and gynecology practice in China based on a cross-sectional study. Front. Educ. 10:1660085. doi: 10.3389/feduc.2025.1660085
Received: 05 July 2025; Accepted: 25 August 2025;
Published: 16 September 2025.
Edited by:
Shavi Fernando, Monash University, AustraliaReviewed by:
Linda Aljunaid, Tawam Hospital, United Arab EmiratesMade Violin Weda Yani, Udayana University, Indonesia
Copyright © 2025 Bai, Zhao, Lu, Tao, Gao, Deqiong and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Na Gao, Z2FvbmEyMDAxQDE2My5jb20=; Deqiong, MTU1MjM2MjcyQHFxLmNvbQ==; Zhen Xiao, c2VyaW91c2RvY0AxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Lina Bai
Lina Bai Mengmeng Zhao1†
Mengmeng Zhao1† Zhen Xiao
Zhen Xiao