- Department of Anesthesiology, The Third Xiangya Hospital, Central South University, Changsha, Hunan, China
Objective: This study aimed to evaluate the effectiveness of a novel “Time-Segmented-Target” (TST) teaching method compared to traditional approaches for spinal puncture training among first-year resident physicians.
Methods: We conducted a randomized trial with 134 participants equally divided into TST and traditional teaching groups. The TST method broke down the spinal puncture procedure into three distinct phases (pre-operative preparation, operation, and postoperative management along with humanistic compassion). Each phase has clear stage teaching objectives and achievement criteria. A reasonable time limit is set for each stage to require students to complete their assigned tasks within the specified timeframe. The traditional method introduce the operational steps from beginning to end, including the goals and achievement criteria for completing each step of the operation. Both groups received 4 h of training. Outcomes were assessed immediately after training and at 2-month follow-up.
Results: The TST group demonstrated significantly higher competency scores in the pre-operative preparation phase, the operational phase, postoperative management along with humanistic compassion, and total scores (p < 0.01 for each pairwise comparison). Concurrently, the TST group exhibited shorter operational times, and better retention of skills over time (p < 0.01 for each pairwise comparison). Additionally, participants in the TST group reported higher levels of proficiency, willingness, confidence, and satisfaction with teaching (p < 0.01 for each pairwise comparison).
Conclusion: The TST teaching method proves significantly more effective than traditional approaches for spinal puncture training, offering improved skill acquisition, retention, and learner satisfaction. These findings suggest TST’s potential value for enhancing procedural skill education.
1 Introduction
Spinal puncture, a routine medical procedure, is extensively employed in the diagnosis of neurological disorders (Margolis et al., 2021), clinical anesthesia (Gong et al., 2025), and pain management (Fontaine et al., 2024). The procedure’s complexity is compounded by the intricate anatomical structure of the spine, as well as variations in the spinal structure of special patients, including the elderly, the obese, and those with abnormal lumbar spine anatomy (Uyel and Kilicaslan, 2021; Huang et al., 2024). It is challenging to perform spinal puncture, and can potentially result in complications including bleeding, nerve injury, and postdural puncture headache (Pirenne et al., 2023). Thus, the spinal puncture procedure exacts a rigorous requirement for the operator’s theoretical knowledge and technical proficiency, rendering it a daunting skill to master. Presently, the traditional teaching method involves a combination of theoretical lectures and model practice (Carstensen et al., 2022; Ma et al., 2023; Overskott et al., 2024). The objective of traditional teaching method is to master intraspinal puncture, which introduce the operational steps from beginning to end, including the goals and achievement criteria for completing each step of the operation. However, it neither divides complex operations into stage learning nor sets clear stage goals with time limits, often resulting in a prolonged learning curve.
To elevate the learning efficiency of spinal puncture and shorten the learning curve, our team propose the “Time-Segmented-Target” (TST) teaching method. Based on the theory of cognitive load (Zou et al., 2025), the TST method reduces intrinsic cognitive load through dividing the teaching process of spinal puncture into three phases, allowing focused mastery of each step before progression: (1) the pre-operative preparation phase, including preparation of the operator, patient, and supplies, (2) the operational phase, including positioning, disinfection, draping, local anesthesia and puncture, (3) postoperative management along with humanistic compassion. Each phase has clear teaching objectives and achievement criteria. For example, during the pre-operative preparation stage, students need to master the stage goals, including preparation of the operator (dressing, verifying the patient, signing informed consent forms), preparation of the patient (opening venous access, exposing puncture sites), and preparation of supplies (monitoring, disinfection, and puncture supplies, etc) (Appendix 1). In short, the operational objectives of each step are categorized and summarized in this stage, which are different from traditional teaching method. Please refer to Appendix 1 for the teaching objectives and achievement criteria of the operational phase and postoperative management along with humanistic compassion. This method aims to make each stage goal clear and engage in deliberate practice, aligning with Ericsson’s principles of deliberate practice and ensuring competency at each stage (Rajaratnam et al., 2021). Additionally, based on the principle of time-and-motion (Harewood et al., 2008), a reasonable time limit is set for each stage to optimize procedural efficiency, requiring students to complete their assigned tasks within the specified timeframe. Both teaching methods cover the safety measures and preparation (e.g., aseptic principles, informed consent, and patient monitoring, etc). Teachers consistently track the students’ progress, providing essential guidance and constructive feedback. This study aimed to evaluate the effectiveness of the TST teaching method in spinal puncture through comparison between TST and traditional teaching group.
2 Methods
2.1 Study design
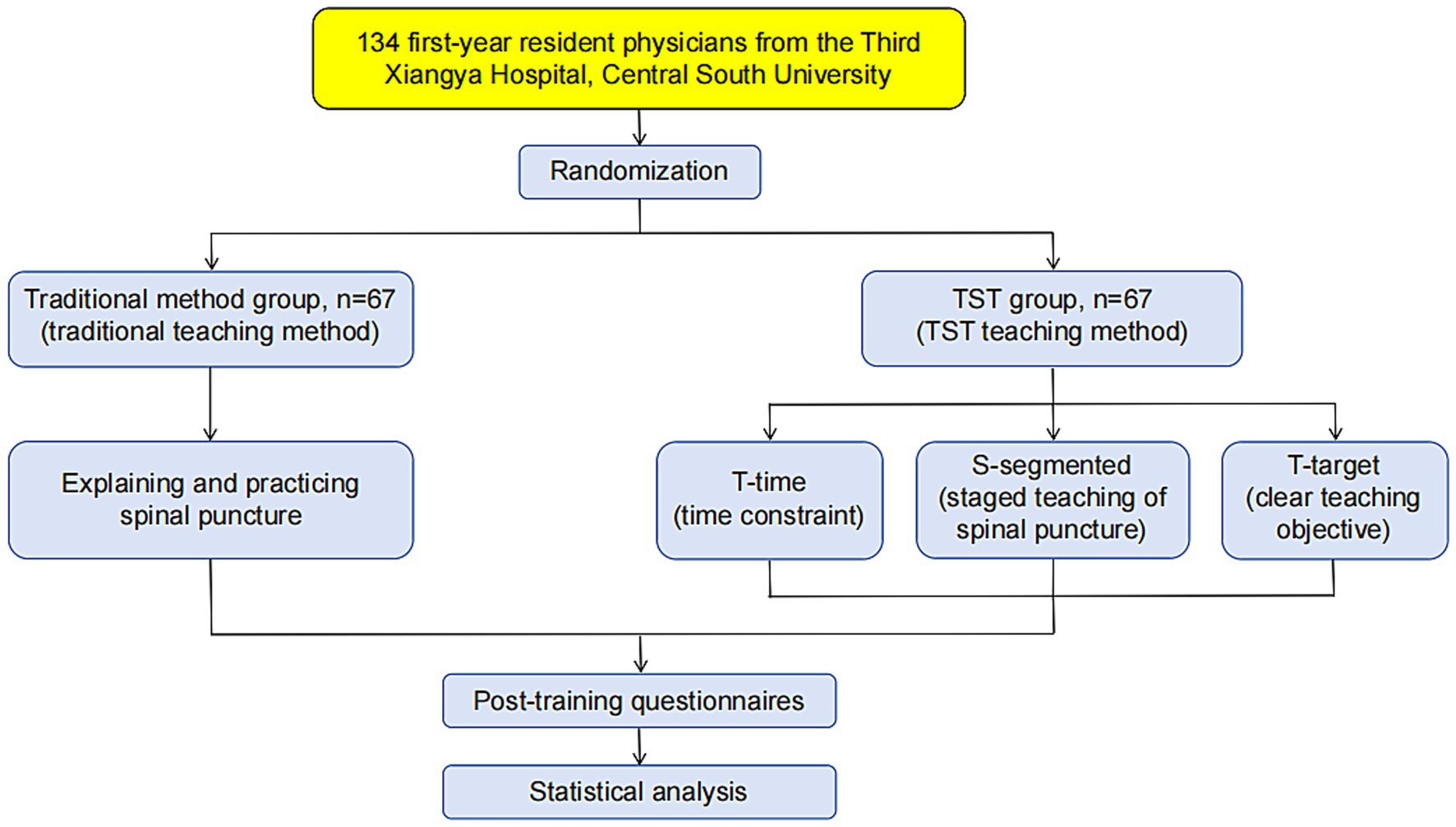
This study was a randomized trial. In this study, we applied the TST teaching method to the teaching of “spinal puncture” in the resident physician training course. All participating resident physicians were randomly assigned to either the traditional method group or the TST group through a random number table approach (Figure 1). The traditional method group was taught using the traditional teaching method, while the TST group was educated utilizing the TST teaching method. Each group was instructed by an experienced anesthesiology teacher. Both teachers had completed the resident physician teacher training, a program certified by the Chinese Medical Doctor Association. Both instructors were supplied with detailed lesson plans to follow. They meticulously prepared the lessons before each class, and actively involved their students through asking questions in class. The teaching courses for both groups of students spanned an identical duration of 4 h. A 10 min intermission was scheduled after every 45 min of instruction. All of these courses were conducted in the science and education building of the Third Xiangya Hospital. Each instructor was responsible for guiding 16 to 17 students per class, resulting in a teacher-to-student ratio of 1:16–17.
To compare the mastery of spinal puncture technique between two groups of students, an assessment via a simulated operation was conducted by another anesthesiology teacher who was blinded to the grouping during the last hour of the course and 2 months post-training (see Appendix 1 for the assessment score table). All participants were instructed not to engage in spinal puncture practice or seek additional training during the two-month period. Access to simulation labs was restricted for study-related practice to prevent unaccounted rehearsal. After the course, a questionnaire survey was administered to the students. In the questionnaire, students were inquired about their proficiency, willingness, and confidence in performing spinal puncture, and satisfaction with teaching. The results of the questionnaire were analyzed to evaluate the effects and satisfaction of the TST teaching method (Appendix 2). The assessment tools were adapted from validated instruments. The simulated operation score table (Appendix 1) was based on the Objective Structured Assessment of Technical Skills (OSATS) and was modified for spinal puncture. Inter-rater reliability (Cohen’s κ = 0.89) was confirmed during piloting. The questionnaire of participant survey (Appendix 2) was pre-tested for internal consistency (Cronbach’s α = 0.82). The trial was registered and approved by the Institutional Review Board of the Third Xiangya Hospital of Central South University (Date: 10/20/2023, Decision No: R23082). No incentives or reimbursements were offered to the participants.
The learner attendance, the materials utilized, the educational strategies employed, and the duration of the educational intervention were evaluated by trained raters. The raters consisted of two doctoral-level students who received their training from senior staff.
In the preliminary study, the average scores for simulated operation assessment in the traditional teaching group and TST group were 77.1 and 82.4, respectively. The standard deviation was 8.3. The sample size was determined based on the following parameters: a two-tailed test, with a significance level (α) of 0.05 and a power level (1-β) of 0.9, ensuring an equal allocation of participants between the two groups. To detect statistically significant differences, 53 participants for each of the two groups were deemed necessary. Accounting for a dropout rate of 20%, we necessitated enrolling 67 participants per group for a total of 134 participants.
2.2 Participants
All participants were first-year resident physicians participating in the residency training program at the Third Xiangya Hospital of Central South University. They had successfully completed a five-year undergraduate program in clinical medicine and/or a three-year master’s program. According to the training contents and standards established by the National Health Commission of China for resident physicians, spinal puncture was identified as a fundamental competency that anesthesiologists and neurologists must possess. Therefore, we had integrated spinal puncture into their training program. We released recruitment information from December 1st, 2023, to February 28th, 2024, inviting first-year resident physicians to volunteer for the trial. In order to ensure that the learning starting points of the two groups of students were consistent, we specifically excluded those physicians who had previously received spinal puncture training due to certain opportunities. All participants in this study had obtained written informed consent.
2.3 Study protocol
For the traditional teaching method of spinal puncture, the instructor first taught the basic theoretical knowledge, including the purpose, significance, indications, contraindications, positioning, and anatomy of the puncture (0.5 h in this section). Subsequently, the instructor meticulously delineated each step of the process and provided a detailed explanation of the technique according to the standards of spinal puncture (0.5 h in this section). Following this, the participants were afforded the opportunity to practiced spinal puncture on the model (2 h in this section).
For the TST teaching method implemented by the experimental group, initially, the instruction followed the conventions of traditional teaching methods by commencing with the acquisition of essential theoretical knowledge (0.5 h in this section). Then, adhering to the established standards for spinal puncture, the instructor meticulously segmented the operation process into three stages: the preoperative preparation phase, the operational phase, the phase of postoperative management and humanistic compassion. During the preoperative preparation phase, the instructor delivered comprehensive elucidations and demonstrations focusing on the preparations required for the operator, the patient, and the necessary supplies. In adherence to the teaching objectives and requirements, the participants were tasked with accomplishing above preparations within a span of 1 min, followed by a dedicated practice (0.5 h in this phase). During the operational phase of spinal puncture, the participants received detailed guidance and demonstrations covering key aspects such as positioning, disinfection, draping, local anesthesia, and the puncture itself. They were expected execute these tasks on the model within 6 min (1.0 h in this phase). After the operation was completed, an explanation regarding “postoperative management and humanistic compassion” was provided. The participants were to perform the above tasks on the model within 1 min (0.5 h in this phase). The segmented time arrangement (1 min preparation, 6 min operation, 1 min post-procedure management) were derived through preliminary observational studies and pilot testing. Adjustments were made after testing with 20 trainees (not part of the main study) to balance feasibility and thoroughness. The instructor highlighted critical steps and precautions at each stage, including patients’ positioning, selection of the puncture site, the scope of disinfection, puncture techniques, and the maintenance of aseptic conditions during the procedure. To consolidate their learning, the participants would practice the entire process again (0.5 h in this section).
Before the end of the course, another instructor who was blinded to the grouping conducted an evaluation, assigning a score to each participant based on their demonstrated skill level.
2.4 Statistical analysis
Statistical analysis was conducted using IBM SPSS Statistics version 26.0. The Kolmogorov– Smirnov test was applied to verify the normality of the continuous variables. Data were presented as means ± standard deviations for normally distributed continuous variables, as medians and interquartile ranges for those with a non-normal distribution, and as frequencies for enumeration data. To assess the differences between the two groups of continuous variables, the unpaired t test was used for data with a normal distribution, while the Mann–Whitney U test was employed for non-normally distributed data. Enumeration data were analyzed using the χ2 test. A p-value of less than 0.05 was deemed statistically significant.
3 Results
3.1 Demographic characteristics of participants
A total of 134 participants took part in the study. Following the spinal puncture course, all participants independently filled out a questionnaire. There were no significant statistical differences in demographic characteristics, including age, gender, and educational level between the traditional method group and the TST method group (p > 0.05) (Table 1). Additionally, Table 1 illustrates the participants’ prior knowledge of spinal puncture techniques. A majority of 80.60% (108/134) had never observed an spinal puncture procedure, while 19.40% (26/134) had witnessed it 1 to 2 times prior to the training. None of the participants had any hands-on experience with spinal puncture procedures. There was no record of any specific adaptations made to educational intervention.
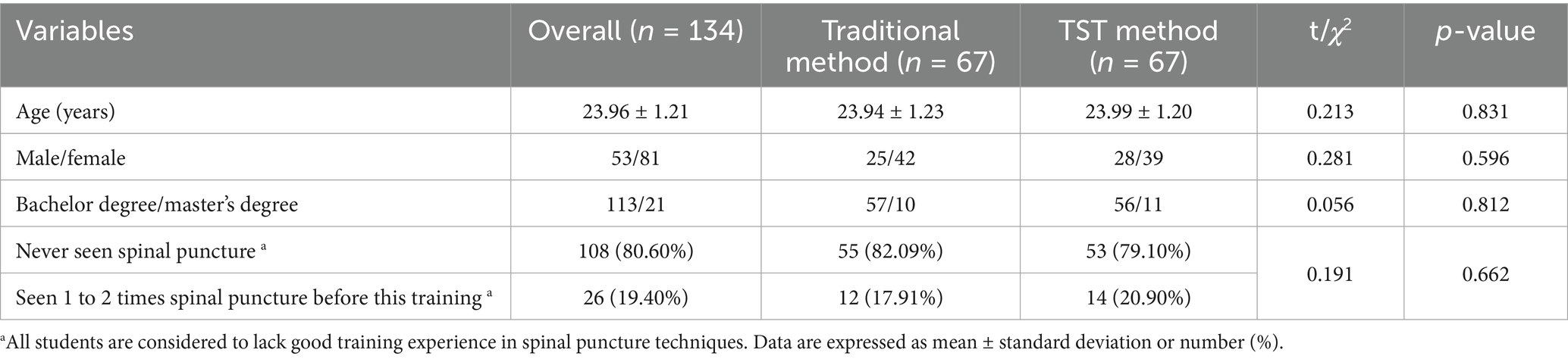
3.2 Mastery level of spinal puncture skills
An assessment through a simulated operation was conducted by another anesthesiology teacher during the last hour of the course. The mastery level of spinal puncture skills between two groups of students are presented in Table 2. Participants who received TST teaching demonstrated significantly higher competency scores on the spinal puncture skill assessment compared to those in the traditional teaching group. Specifically, the average scores of the pre-operative preparation phase, the operational phase, postoperative management along with humanistic compassion and total scores in the TST method group were higher than those in the traditional method group (all p < 0.01), but the operational time was shorter than that in the traditional method group (p < 0.001). There was no significant difference in the aseptic principle scores between the two groups of participants (p = 0.839) (Table 2). No record was retained of any modifications made throughout the course of the educational intervention.
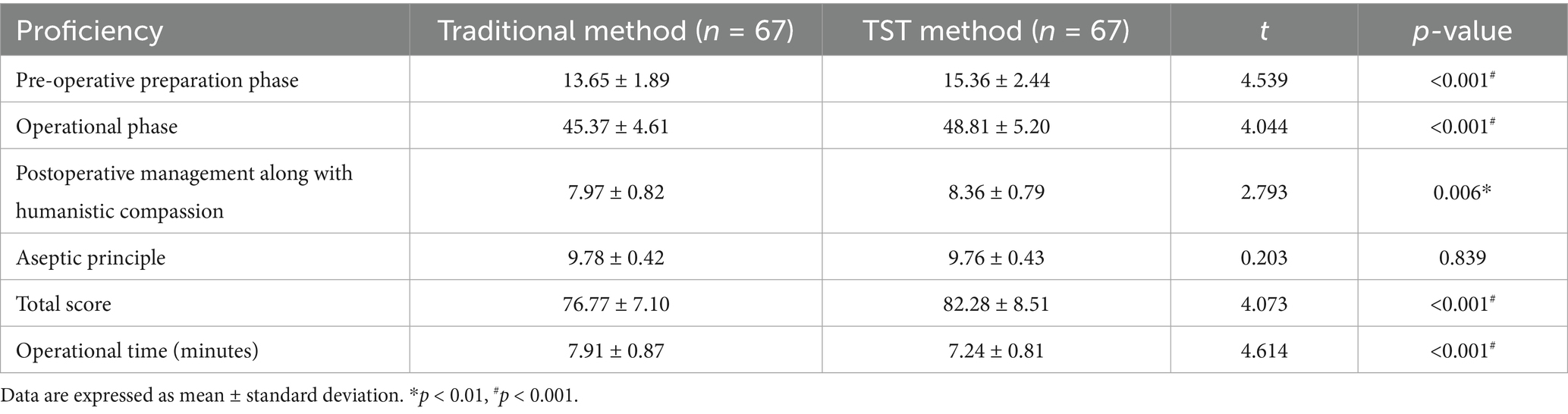
3.3 Knowledge and skills retention
An assessment through a simulated operation was conducted by another anesthesiology teacher at 2 months after the training. All participants did not receive training on spinal puncture within the 2 months. The TST group retained a higher level of knowledge and skills related to spinal puncture. Specifically, compared to the traditional method group, participants in the TST method group demonstrated significantly higher scores in the pre-operative preparation phase, the operational phase, postoperative management along with humanistic compassion, and total scores (all p < 0.001), but the operational time was shorter (p < 0.001) (Table 3). In contrast, the difference in scores between 2 months after the training and immediately after the training in the TST group, including the pre-operative preparation phase, the operational phase, postoperative management along with humanistic compassion, and total scores were lower than those of the traditional method group (all p < 0.01). There was no significant difference in the aseptic principle scores between the two groups of participants at 2 months after the training (p = 0.860). Moreover, the difference in aseptic principle scores between 2 months after the training and immediately after the training exhibited no significant discrepancy between the two groups (p = 0.730) (Table 3). No record of any modifications was kept throughout the course of the educational intervention process.
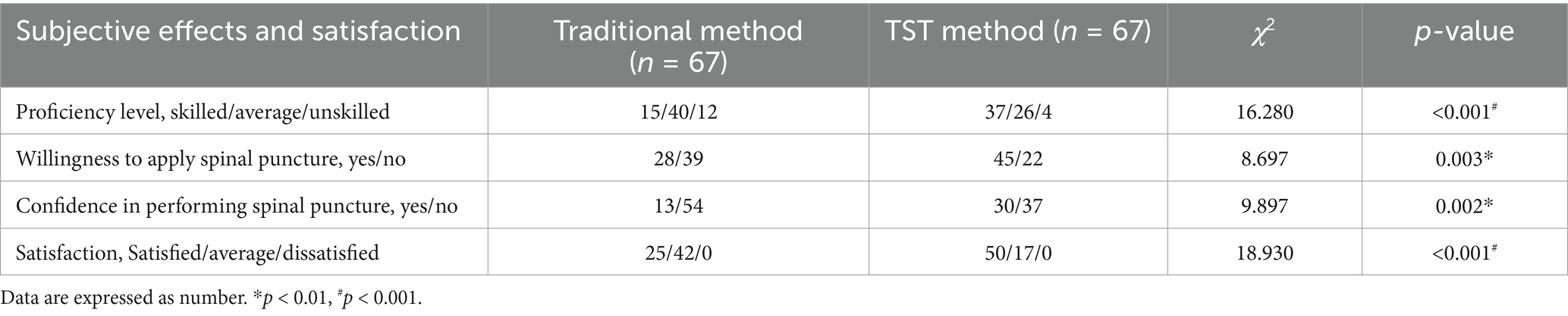
3.4 Participants subjective effects and satisfaction evaluation of the TST method and the traditional method
Evaluation of participants subjective effects of the TST method and the traditional method based on three indicators, including proficiency, willingness, and confidence in performing spinal puncture, are presented in Table 4. The TST course participants believed their proficiency, willingness, and confidence in performing spinal puncture were stronger than those of participants in traditional courses (all p < 0.01). In addition, the satisfaction of participants in the TST method group was higher than that in the traditional method group (p < 0.001) (Table 4).
4 Discussion
The present study aimed to compare the efficacy of TST and traditional teaching methods in improving spinal puncture skills. Our findings indicated that TST was a more effective teaching method for enhancing participants’ performance and overall satisfaction in spinal puncture compared to traditional teaching approaches.
Our results revealed that participants who received TST teaching method demonstrated significantly higher scores and less operational time in spinal puncture skill assessments immediately after training and at the 2-month follow-up compared to those in the traditional teaching method group. These suggest that TST teaching method not only facilitates immediate skill acquisition but also promotes retention of the skills over time. The segmented teaching of TST can better organize the learning process, with time constraints allowing subjects to be more focused on tasks during specific time periods. Consistent with reports of Hardeland and Peluso, clear learning objectives enable learners to effectively focus on key aspects of the procedure, leading to better mastery and retention (Hardeland et al., 2017; Peluso et al., 2018). The reduction in operational time is a critical advantage, as efficiency in performing medical procedures is often associated with better patient outcomes and increased satisfaction among healthcare providers (Witmer et al., 2022). The TST teaching method enables subjects to efficiently and proficiently master spinal puncture. It may contribute to reducing the operational time.
Furthermore, participants in the TST group subjectively reported higher levels of proficiency, willingness, and confidence in performing spinal puncture compared to their counterparts in the traditional teaching group. This finding is significant as proficiency, willingness and confidence to perform medical procedures are crucial for safe and effective practice (Meffe et al., 2012; Chuan, 2020; Yu et al., 2021; Kohli et al., 2022; Wang and Shen, 2022). The targeted nature of TST, which allows learners to practice repeatedly with clear objectives, may improve their proficiency and confidence to perform the procedure successfully. This is similar to the clear educational goals observed in virtual reality simulations (Plotzky et al., 2021). Our study also showed that participants in the TST group had higher satisfaction compared to those in the traditional teaching group. This increased satisfaction could be attributed to the ease of mastering TST teaching content, which may make the learning process easier and less intimidating. Previous studies have also shown that the higher the availability and acceptability of technology, the higher the satisfaction of subjects (Rossetto et al., 2023). Moreover, the ability to see immediate progress through targeted practice and feedback may contribute to higher satisfaction (Cooney et al., 2014; Nielsen et al., 2023).
It is worth noting that aseptic principle scores showed no significant differences between the TST and traditional groups, which may be related to standardized foundational training and repetitive reinforcement. Aseptic technique is a universally mandated competency in medical education, rigorously emphasized across all procedural training. Both groups received identical foundational instruction in sterile protocols during their core curriculum, which may have overshadowed any incremental improvements from TST’s phase-specific segmentation. Furthermore, unlike procedural steps unique to spinal puncture, aseptic practices (e.g., hand hygiene, sterile field maintenance) are reinforced across diverse clinical contexts, making them less susceptible to variation between teaching methods. This consistency highlights that TST’s advantages lie in optimizing procedural-specific skills rather than universal competencies like asepsis.
These findings have important implications for medical education. The adoption of TST as a teaching method for spinal puncture could lead to improved operational proficiency, willingness and confidence, and satisfaction with teaching.
This study has several limitations. First, it was conducted at a single academic medical center with first-year resident physicians, which may limit the generalizability of the findings to other institutions or more experienced learners. Second, each group was instructed by an experienced anesthesiology teacher in this study; although both instructors were experienced and followed detailed lesson plans, some variability in teaching style is unavoidable. This could introduce a slight degree of bias. Third, the primary outcome was assessed in a simulated environment; while this controls for confounding variables, it does not fully capture performance in real-world clinical settings with actual patients. The last but not the least, the follow-up period was limited to 2 months; a longer-term assessment is needed to evaluate the durability of skill retention.
Future research should aim to validate these findings through multi-center studies involving a more diverse learner population. Investigating the transfer of skills from simulation to clinical practice is a critical next step. Furthermore, long-term follow-up studies at 6 months or 1 year would provide valuable insights into the persistence of the TST method’s benefits. Finally, exploring the application of the TST framework to other complex procedural skills in medicine would determine the broader utility of this educational approach.
5 Conclusion
TST is a superior teaching method for spinal puncture compared to traditional teaching methods. It not only improves immediate and long-term skill acquisition but also enhances operational proficiency, willingness and confidence, and satisfaction with teaching. These findings support the potential benefits of incorporating TST into medical education curricula for spinal puncture and other procedural skills.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
Ethics statement
The studies involving humans were approved by Institutional Review Board of the Third Xiangya Hospital of Central South University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
WQ: Methodology, Writing – original draft. HS: Writing – review & editing. CC: Writing – review & editing. RY: Supervision, Writing – review & editing. ZH: Supervision, Writing – review & editing. XL: Project administration, Writing – review & editing. MC: Investigation, Writing – review & editing. SC: Writing – review & editing. FZ: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the Nature Science Foundation of Hunan Province (#2023JJ30825 and #2025JJ60698), and Undergraduate education and teaching reform research project of Central South University (2024JY154).
Acknowledgments
We would like to extend our sincere gratitude to all those who have contributed to the completion of this research. First and foremost, we are grateful to Professor Xiaohong Tang, for their invaluable guidance, unwavering support, and encouragement throughout the entire research process. Her expertise and profound knowledge have been instrumental in shaping the direction and quality of this article. We would also like to thank the Third Xiangya Hospital of Central South University for providing us with the necessary resources and facilities to conduct this research. Lastly, we would like to extend our heartfelt appreciation to the participants who took part in our study. Their willingness to contribute their time and experiences has made it possible for us to gather the data required for this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2025.1665203/full#supplementary-material
Abbreviations
TST, Time-Segmented-Target; OSATS, Objective Structured Assessment of Technical Skills.
References
Carstensen, S. M. D., Velander, M. J., Konge, L., Ostergaard, M., Pfeiffer Jensen, M., Just, S. A., et al. (2022). Training and assessment of musculoskeletal ultrasound and injection skills-a systematic review. Rheumatology 61, 3889–3901. doi: 10.1093/rheumatology/keac119
Chuan, A. (2020). Education and training in ultrasound-guided regional anaesthesia and pain medicine. Curr. Opin. Anaesthesiol. 33, 674–684. doi: 10.1097/ACO.0000000000000908
Cooney, C. M., Redett, R. J. 3rd, Dorafshar, A. H., Zarrabi, B., and Lifchez, S. D. (2014). Integrating the NAS milestones and handheld technology to improve residency training and assessment. J. Surg. Educ. 71, 39–42. doi: 10.1016/j.jsurg.2013.09.019
Fontaine, C., Libert, I., Echterbille, M. A., Bonhomme, V., Botterman, J., Bourgonjon, B., et al. (2024). Evaluating pain management practices for cancer patients among health professionals in cancer and supportive/palliative care units: a Belgian survey. Support Care Cancer 32:811. doi: 10.1007/s00520-024-08984-4
Gong, C., Ye, X., Liao, Y., Ye, P., Zheng, T., and Zheng, X. (2025). Hypotension after unilateral versus bilateral spinal anaesthesia: a systematic review with meta-analysis. Eur. J. Anaesthesiol. 42, 203–223. doi: 10.1097/EJA.0000000000002098
Hardeland, C., Skare, C., Kramer-Johansen, J., Birkenes, T. S., Myklebust, H., Hansen, A. E., et al. (2017). Targeted simulation and education to improve cardiac arrest recognition and telephone assisted CPR in an emergency medical communication Centre. Resuscitation 114, 21–26. doi: 10.1016/j.resuscitation.2017.02.013
Harewood, G. C., Chrysostomou, K., Himy, N., and Leong, W. L. (2008). A "time-and-motion" study of endoscopic practice: strategies to enhance efficiency. Gastrointest. Endosc. 68, 1043–1050. doi: 10.1016/j.gie.2008.03.1116
Huang, C., Zhang, Y., Diedrich, D. A., Li, J., Luo, W., Zhao, X., et al. (2024). A horizontal and perpendicular interlaminar approach for intrathecal nusinersen injection in patients with spinal muscular atrophy and scoliosis: an observational study. Orphanet J. Rare Dis. 19:268. doi: 10.1186/s13023-024-03278-8
Kohli, R., Replogle, K., Gough-Goldman, A., Taylor, B., Maughan, B., Sehgal, H. S., et al. (2022). Launching an innovative educational model addressing substance use disorders and dental pain management (project ECHO(R) in dentistry). BMC Oral Health 22:402. doi: 10.1186/s12903-022-02417-6
Ma, J., Wang, Q., Xia, X., Guo, Z., Feng, Q., Zhou, Y., et al. (2023). Inclusion of the workshop model in the standardized training of emergency medicine residents. Heliyon 9:e15942. doi: 10.1016/j.heliyon.2023.e15942
Margolis, M. S., DeBusk, A. A., Moster, M. L., Falardeau, J. M., Eggenberger, E. R., Sergott, R. C., et al. (2021). Lumbar puncture for diagnosis of idiopathic intracranial hypertension in typical patients. J. Neuroophthalmol. 41, 375–378. doi: 10.1097/WNO.0000000000001319
Meffe, F., Claire Moravac, C., and Espin, S. (2012). An interprofessional education pilot program in maternity care: findings from an exploratory case study of undergraduate students. J. Interprof. Care 26, 183–188. doi: 10.3109/13561820.2011.645089
Nielsen, C., Katz, S., Parker, M., Trefsgar, J., Bcharah, H., Kalin, J., et al. (2023). A student-driven mindfulness curriculum for first-year osteopathic medical students: a pilot study. J Osteopath Med 123, 485–492. doi: 10.1515/jom-2022-0246
Overskott, H. L., Markholm, C. E., Sehic, A., and Khan, Q. (2024). Different methods of teaching and learning dental morphology. Dent J 12:114. doi: 10.3390/dj12040114
Peluso, M. J., Tapela, N., Langeveldt, J., Williams, M. E., Mochankana, K., Motseosi, K., et al. (2018). Building health system capacity through medical education: a targeted needs assessment to guide development of a structured internal medicine curriculum for medical interns in Botswana. Ann. Glob. Health 84, 151–159. doi: 10.29024/aogh.22
Pirenne, V., Dewinter, G., and Van de Velde, M. (2023). Spinal anaesthesia in obstetrics. Best Pract. Res. Clin. Anaesthesiol. 37, 101–108. doi: 10.1016/j.bpa.2023.03.006
Plotzky, C., Lindwedel, U., Sorber, M., Loessl, B., Konig, P., Kunze, C., et al. (2021). Virtual reality simulations in nurse education: a systematic mapping review. Nurse Educ. Today 101:104868. doi: 10.1016/j.nedt.2021.104868
Rajaratnam, V., Rahman, N. A., and Dong, C. (2021). Integrating instructional design principles into surgical skills training models: an innovative approach. Ann. R. Coll. Surg. Engl. 103, 718–724. doi: 10.1308/rcsann.2020.7132
Rossetto, F., Borgnis, F., Isernia, S., Foglia, E., Garagiola, E., Realdon, O., et al. (2023). System integrated digital empowering and teleRehabilitation to promote patient activation and well-being in chronic disabilities: a usability and acceptability study. Front. Public Health 11:1154481. doi: 10.3389/fpubh.2023.1154481
Uyel, Y., and Kilicaslan, A. (2021). Preprocedural ultrasonography versus landmark-guided spinal anesthesia in geriatric patients with difficult anatomy: a prospective randomized trial. Eurasian J. Med. 53, 9–14. doi: 10.5152/eurasianjmed.2020.20215
Wang, Z., and Shen, J. (2022). Simulation training in spine surgery. J. Am. Acad. Orthop. Surg. 30, 400–408. doi: 10.5435/JAAOS-D-21-00756
Witmer, H. D. D., Dhiman, A., Jones, A. D., Laffan, A. M., Adelman, D., and Turaga, K. K. (2022). A systematic review of operative team familiarity on metrics of efficiency, patient outcomes, cost, and team satisfaction. Ann. Surg. 276, e674–e681. doi: 10.1097/SLA.0000000000005531
Yu, J. H., Chang, H. J., Kim, S. S., Park, J. E., Chung, W. Y., Lee, S. K., et al. (2021). Effects of high-fidelity simulation education on medical students' anxiety and confidence. PLoS One 16:e0251078. doi: 10.1371/journal.pone.0251078
Keywords: time-segmented-target teaching, time limit, segmented teaching, spinal puncture, procedural skills training
Citation: Qing W, Su H, Cheng C, Yu R, Hu Z, Liu X, Chen M, Cao S and Zhang F (2025) Comparison of time-segmented-target teaching and traditional teaching methods for spinal puncture: a randomized trial. Front. Educ. 10:1665203. doi: 10.3389/feduc.2025.1665203
Edited by:
Asmaa Abdelnasser, Ibn Sina National College for Medical Studies, Saudi ArabiaReviewed by:
Amira Farghaly, Prince Sattam Bin Abdulaziz University, Saudi ArabiaErini Efat, Faculty of Medicine Suez Canal University, Egypt
Copyright © 2025 Qing, Su, Cheng, Yu, Hu, Liu, Chen, Cao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fan Zhang, emhhbmctZmFuMTk4NkBxcS5jb20=
 Wenxiang Qing
Wenxiang Qing Han Su
Han Su Cancan Cheng
Cancan Cheng Rili Yu
Rili Yu Minghua Chen
Minghua Chen Fan Zhang
Fan Zhang