- 1Department of Oral Medicine and Radiology, Manipal College of Dental Sciences Mangalore, Manipal Academy of Higher Education, Manipal, India
- 2Department of Respiratory Medicine, Kasturba Medical College Mangalore, Manipal Academy of Higher Education, Manipal, India
- 3Department of Medical Education, Kasturba Medical College Mangalore, Manipal Academy of Higher Education, Manipal, India
- 4College of Medicine and Health Sciences, National University of Science and Technology, Muscat, Oman
- 5Department of Community Medicine, Kasturba Medical College Mangalore, Manipal Academy of Higher Education, Manipal, India
- 6University of British Columbia, Vancouver, BC, Canada
- 7WHO Collaborating Centre on Health Workforce Planning and Research, Dalhousie University, Halifax, NS, Canada
- 8University of Technology, Sydney, NSW, Australia
- 9Department of Psychiatry, Kasturba Medical College Mangalore, Manipal Academy of Higher Education, Manipal, India
- 10Department of Social Work, School of Social Work, Roshni Nilaya (Autonomous), Mangalore, India
Background: To address the challenges in the early diagnosis and prevention of oral cancer, it is essential to include clinical psychology and social care professionals in interprofessional healthcare teams. In this context, a needs assessment study was conducted to inform the development of an interprofessional education and collaborative practice (IPECP) course focused on oral cancer for students in clinical psychology and social care. The objectives of this study were to develop a tool for assessing the knowledge, attitudes, and practices (KAPs) related to oral cancer prevention and early detection among these students and to evaluate the current KAP levels within this student cohort. Additional objectives were to estimate the likelihood that students would demonstrate strong KAP scores related to oral cancer prevention and early detection and to assess their readiness for interprofessional learning and collaborative practice.
Methods: Two questionnaires were employed in this study: (1) a custom-designed questionnaire was developed, validated, and administered to assess KAP related to the early detection and prevention of oral cancer and (2) the Readiness for Interprofessional Learning Scale (RIPLS). For data analysis, both descriptive and inferential statistical methods were applied. These included the Mann–Whitney U test, ordered logistic regression, and probit analysis. A significance level of p < 0.05 was set for all the statistical tests.
Results: A total of 220 clinical psychology students and 226 social care students were included in the study. The mean scores related to KAP were 11.04 ± 1.782, 5.28 ± 1.292, and 4.56 ± 1.583, respectively, and the mean score for RIPLS was 82.23 ± 10.961 among clinical psychology students. Among the social care students, the KAPs were 10.46 ± 2.688, 5.36 ± 1.626, and 5.86 ± 1.806, respectively, and the mean RIPLS score was 46.58 ± 9.705.
Conclusion: The analysis revealed that both the clinical psychology and social care student cohorts presented low scores in knowledge and practices related to the prevention and early detection of oral cancer. However, the Readiness for Interprofessional Learning Scale (RIPLS) results indicated a more positive attitude toward interprofessional learning among clinical psychology students than among their social care counterparts.
Background
Oral cancer is considered a preventable malignancy with specific and well-established risk factors that help identify at risk population (Bouvard et al., 2022). Oral screening methods are relatively easy to implement and need minimal armamentarium and technical skills. Despite the nature of this disease, delays in the diagnosis of oral cancer are common in South Asian countries (Dwivedi et al., 2023), especially India, where the prevalence of this disease has increased (Bray et al., 2018). A recent article highlights the burden of disease with significant variations in oral cancer patterns observed across different Indian states between 1990 and 2021, with key observations that included a 31% increase in age-standardized incidence and an 11.18% increase in age-standardized mortality. These trends are closely linked to ongoing high-risk behaviors such as tobacco use, alcohol intake, and betel quid consumption (Zahiruddin et al., 2024). Thus, it is essential to implement targeted interventions that focus on minimizing these risk factors, promoting early diagnosis, and improving treatment accessibility. Furthermore, addressing the underlying socioeconomic inequalities that contribute to the cancer burden remains a critical priority. Currently, oral cancer poses a considerable psychological and socioeconomic burden in India, which is largely attributable to delays in diagnosis. The factors contributing to delay in diagnosis are complex and include person/community-related factors, health professional-related factors and health system-related factors (Sujir et al., 2024; Zahiruddin et al., 2024). Thus, to address this issue at all levels of the healthcare ecosystem, the model of an interprofessional collaborative person-centered approach holds significant promise. Interprofessional practice and care have had a remarkable impact on people's and community-related health outcomes. There is now evidence from longitudinal studies that shows the benefit of interprofessional education in contributing to collaborative care (World Health Organization, 2010; Reeves et al., 2016). Considering this and the complexities associated with oral cancer, collaboration and coordination among health and social care professionals is critical for reducing and managing the burden of oral cancer.
One of the main preventive measures for oral cancer is the cessation of habits such as tobacco and alcohol use. Since the majority of oral cancers can be attributed to such risk factors, habit cessation is key in oral cancer prevention. However, these habits can be addictive and require appropriate psychological intervention for a successful intervention (Bouvard et al., 2022). Targeted habit cessation in an unprofessional setting has multiple challenges. For example, the adoption of habit cessation services in the dental care setting has presented several challenges, such as limited training, limited time for treatment, and a lack of awareness regarding smoking cessation protocols and referral pathways (Chan et al., 2023). Thus, the role of clinical psychologists is crucial in oral cancer prevention. Additionally, considering the scope of practice of clinical psychologists, the frequent interaction of these specialists with individuals seeking to quit such deleterious habits is common. This provides an impetus for clinical psychologists to work in collaboration with oral health professionals and promote oral cavity screening, which requires frequent and long-term follow-up.
In addition to the role of clinical psychologists, the role of social care professionals in the prevention and early detection of oral cancer has been less explored. Oral cancer is known to affect individuals from lower socioeconomic strata. This demographic also has an increased prevalence of tobacco consumption (Babu et al., 2023). The increasing burden of this disease has highlighted the intricate influence of lifestyle choices and socioeconomic conditions (Zahiruddin et al., 2024). Addressing these social determinants of health for early diagnosis and prevention of oral cancer is crucial. There are frameworks in place for health professions to address social determinants of health (Andermann, 2016). However, considering the burden of disease in India, tackling such complex issues within the community would require significant time and expertise, the burden of which could be reduced by including social care professionals on the interprofessional team. In India, several studies have employed social care workers, e.g., ASHA (Accredited Social Health Activists) workers, for screening for oral cancer, and these studies have shown successful results (Thampi et al., 2022). Thus, we considered an interprofessional team that included social care professionals and clinical psychologists for the prevention and early detection of oral cancer. The primary objectives of this study were (1) to establish a tool to assess knowledge attitudes and practices (KAPs) related to the prevention and early detection of oral cancer for clinical psychology and social care students and (2) to assess the same KAP among this cohort. These findings will contribute to the development of an interprofessional education module for the early diagnosis and prevention of oral cancer.
Materials and methods
This study was conducted after obtaining clearance from the Institutional Ethics Committee (Protocol No: 22099) following the STROBE checklist. Informed consent was obtained prior to recruiting participants. The study duration was 8 months. Considering these objectives, two survey tools were utilized for the study. The first was the prevalidated questionnaire i.e., “Readiness for Interprofessional Learning Scale (RIPLS)” (Parsell and Bligh, 1999), and the second was a questionnaire to assess KAP related to the early diagnosis of oral cancer and its prevention. The second questionnaire was developed by modifying and adapting a previously developed questionnaire (Sujir et al., 2024). Considering the target population, certain questions that were outside the scope of practice of social care and clinical psychology, which included clinical examination of the lymph nodes and clinical examination of the oral cavity, were deleted. The clinical terms were modified for comprehensibility (e.g., “oral cancer” was rephrased as “mouth cancer”), and a 34-item questionnaire was finalized. The content validity ratio was assessed by distributing the modified questionnaire among a panel of eight expert members belonging to the specialties of oral medicine, oral pathology, community medicine, public health dentistry, clinical psychology, and social care, and each expert with more than 10 years of academic/clinical experience was chosen for validation. They assessed each item on the basis of its relevance, clarity, simplicity, and lack of ambiguity. The content validity ratio (CVR) for each item was calculated via the method proposed by Ayre and Scally (2014). All the items achieved a CVR of 1, indicating unanimous agreement on their essentiality. Additionally, reliability methods and statistics were also measured. The questionnaire was pilot tested among 20 participants via the test-retest method. The first part of the questionnaire included demographic details. Items 1–17 and 23 were used to assess knowledge; items 18–21, 26, and 33 were used to assess attitudes; and items 22, 24, 25, 27, and 31 were used to assess practices. These were dichotomous questions with yes or no responses, and correct responses were given a score of 1. Thus, the maximum scores of the knowledge, attitudes and practices domains were 18 points, 6 points, and 6 points, respectively. The average score was computed, and good or poor outcomes were defined on the basis of the results. The last three items of the questionnaire were used to assess the willingness of students to learn about the early diagnosis of oral cancer and its prevention.
The sample size was calculated with the Zpower formula for multiple linear regression. The sample size was calculated on the basis of pilot testing conducted with 20 interprofessional participants. Using an alpha error of 0.05, a delta of 0.1765, and an R2 value of 0.15 with 80% statistical power, the required sample size was estimated to be 179 participants. To account for a potential 20% non-response rate, the final sample size was rounded to 220 students. The inclusion criterion was postgraduate students enrolled in clinical psychology and social care programs. The exclusion criteria were students who did not provide informed consent and those who had participated in the pilot study. Data collection was conducted via self-administered questionnaires. Clinical psychology students received the survey via a Microsoft Forms link shared through WhatsApp, whereas social care students were provided with printed copies. A non-probability, convenience sampling method was employed for participant recruitment. The statistical analysis was performed via STATA statistical software (STATA CORP, COLLEGE STATION, TEXAS, USA; VERSION 17). Descriptive statistics, reliability statistics (Cronbach's alpha), the Mann–Whitney U test, ordered logistic regression and probit analysis were performed. A p value < 0.05 was considered significant.
Results
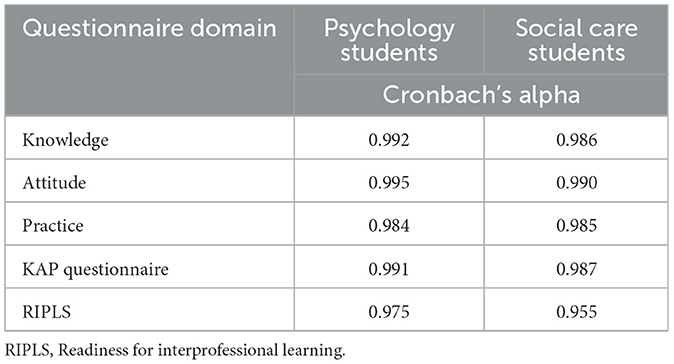
The questionnaire was distributed to 300 postgraduate clinical psychology students and 250 social work students, and the total number of responses recorded was 226 and 220, respectively. Among those recruited, 213 (94.2%) clinical psychology students and 141 (64%) social care students were females. The mean age (standard deviation) was 21.5 ± 2.02 years and 23 ± 1.6 years among the clinical psychology and social care students, respectively. The reliability statistics revealed excellent internal consistency and are summarized in Table 1. The mean scores, standard deviations and standard errors are summarized in Table 2. Mann–Whitney U test comparing the KAP scores and the RIPLS scores between males and females showed no significant difference.
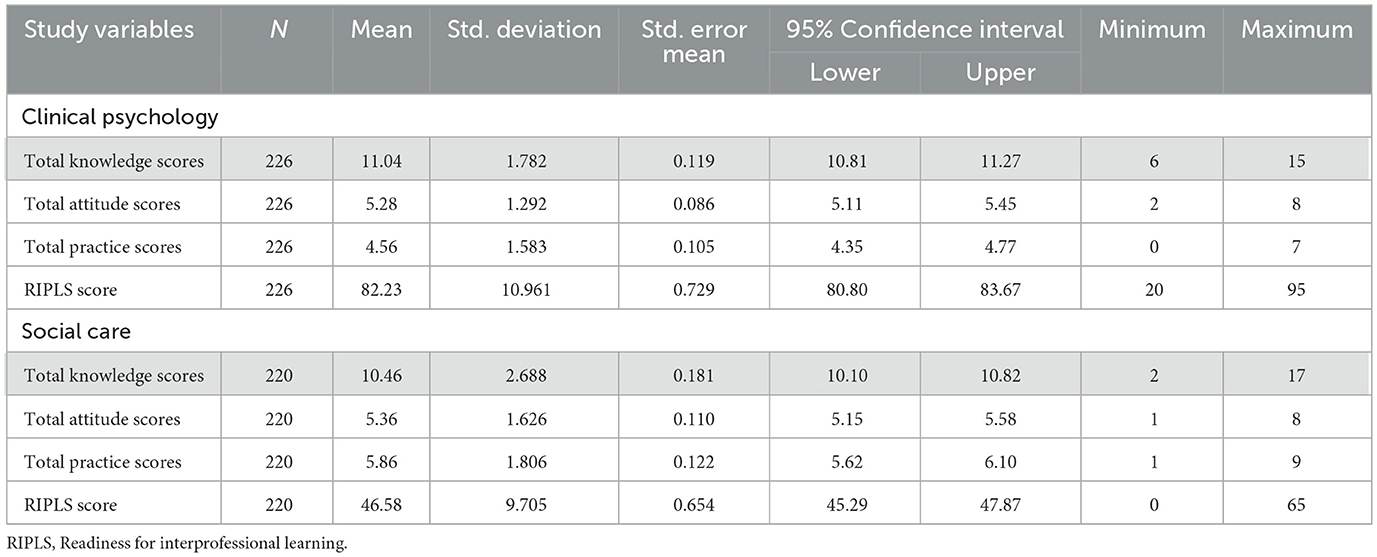
Table 2. Descriptive statistics for the overall sample (knowledge score, attitude score, practice score, and RIPLS score).
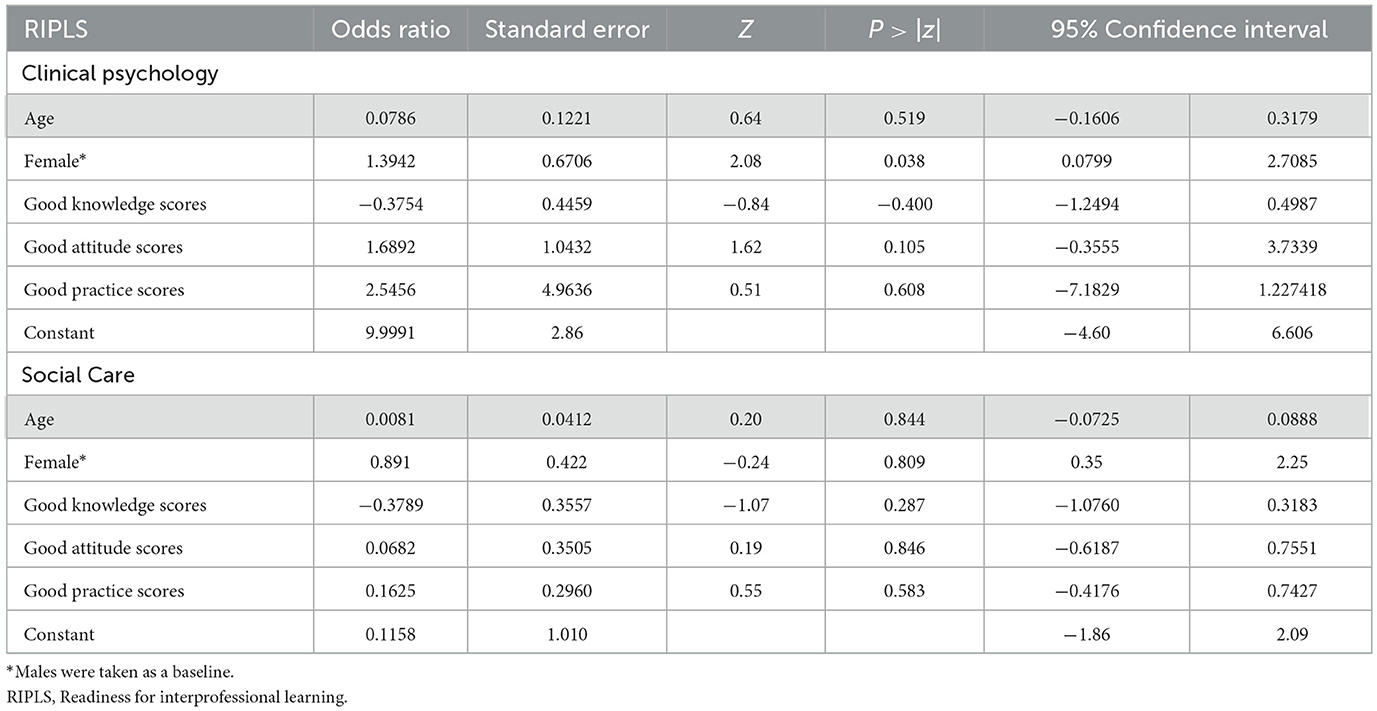
The scores were classified as favorable or unfavorable, and the percentage of students with favorable scores is summarized in Table 3. Ordered logistic regression revealed that sex was a significant covariate influencing the RIPLS score among clinical psychology students (p=0.038); however, for social care students, sex had no significant influence on any factors, such as age, sex, categories of knowledge, attitudes, or practice scores (Table 4).
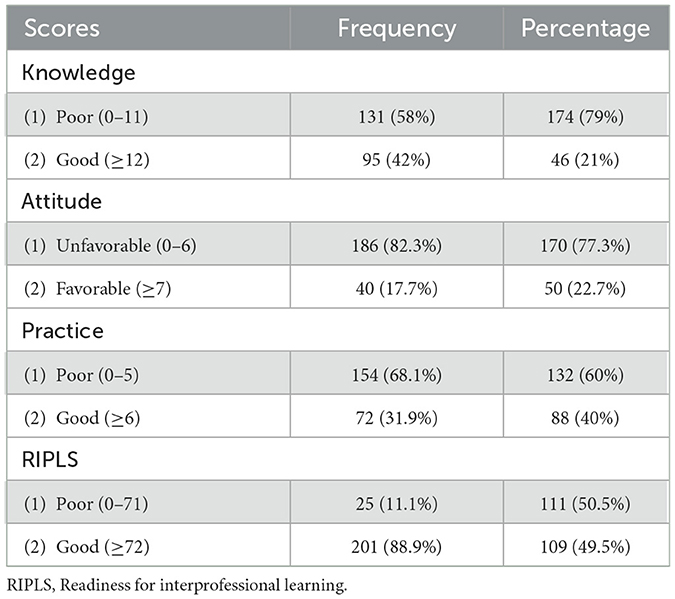
Table 3. Frequency and percentage distributions of students (knowledge, attitudes, practices, and RIPLS scores).
For clinical psychology students, the probability of those with poor knowledge scores achieving good RIPLS scores was approximately 0.91, whereas those with good knowledge scores had a slightly higher probability of approximately 0.97 (Figure 1). When examining attitudes, students with unfavorable attitudes had a 0.87 probability of obtaining good RIPLS scores, whereas those with favorable attitudes had a 0.98 probability (Figure 2). In terms of practice, the probability of students with poor practice scores achieving good RIPLS scores was 0.97, whereas those with good practice scores had a probability of 0.91 (Figure 3). With respect to gender, male students had a 0.72 probability of scoring well on the RIPLS, whereas female students had a notably higher probability of approximately 0.97 (Figure 4). Among social care students, the probability of those with poor knowledge scores achieving good RIPLS scores was approximately 0.53, whereas those with good knowledge scores had a slightly lower probability, ranging between 0.40 and 0.45 (Figure 1). Similarly, students with unfavorable attitudes had a 0.53 probability of obtaining good RIPLS scores, whereas those with favorable attitudes had a 0.50 probability (Figure 2). In terms of practice, students with poor practice scores had a 0.48 probability of scoring well on the RIPLS, whereas those with good practice scores had a higher probability of 0.58 (Figure 3). With respect to gender, male students had a 0.54 probability of achieving good RIPLS scores, whereas female students ranged between 0.45 and 0.50 (Figure 4).
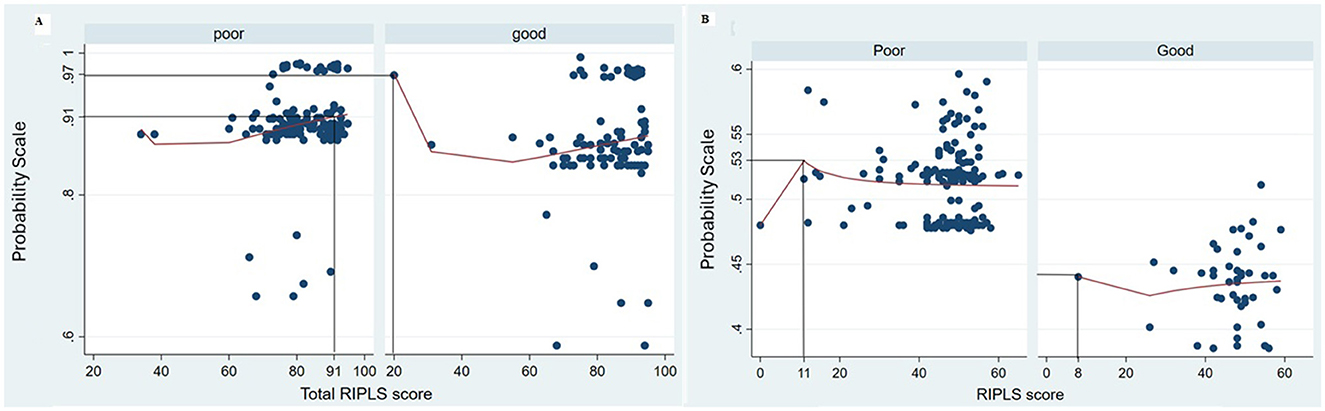
Figure 1. Probit graph showing the probability of the RIPLS score in relation to the knowledge score for (A) clinical psychology students and (B) social care students.
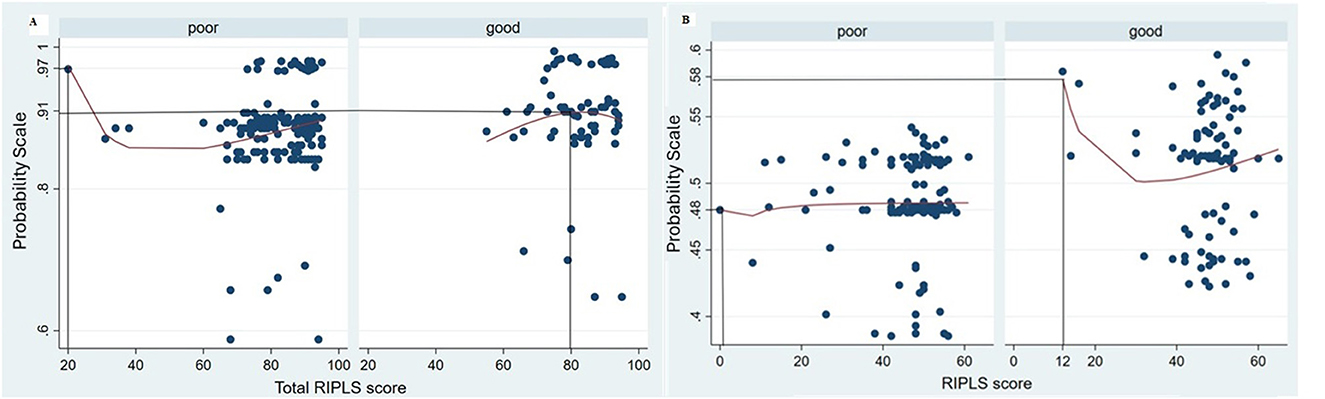
Figure 2. Probit graph showing the probability of the RIPLS score in relation to the practice score for (A) clinical psychology students and (B) social care students.
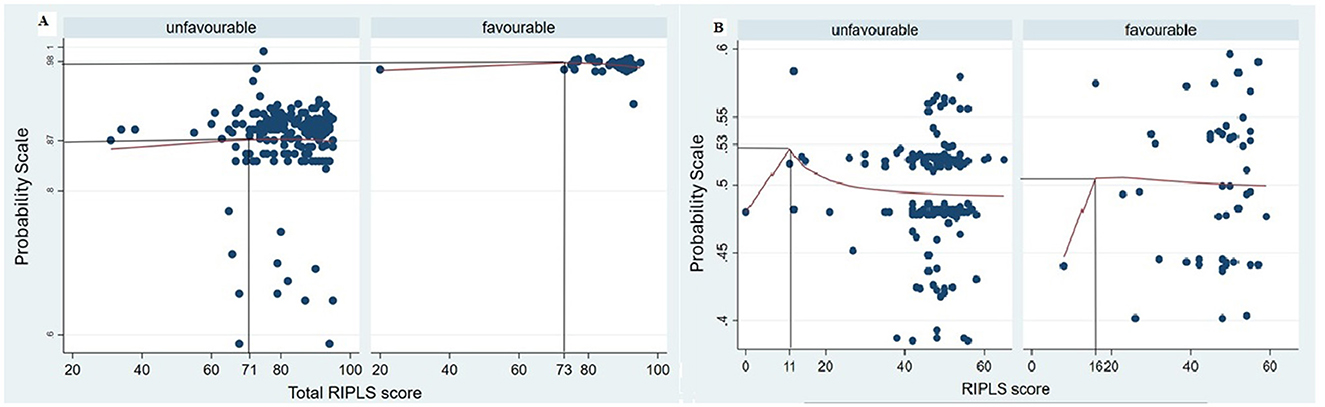
Figure 3. Probit graph showing the probability of the RIPLS score in relation to the attitude score for (A) clinical psychology students and (B) social care students.
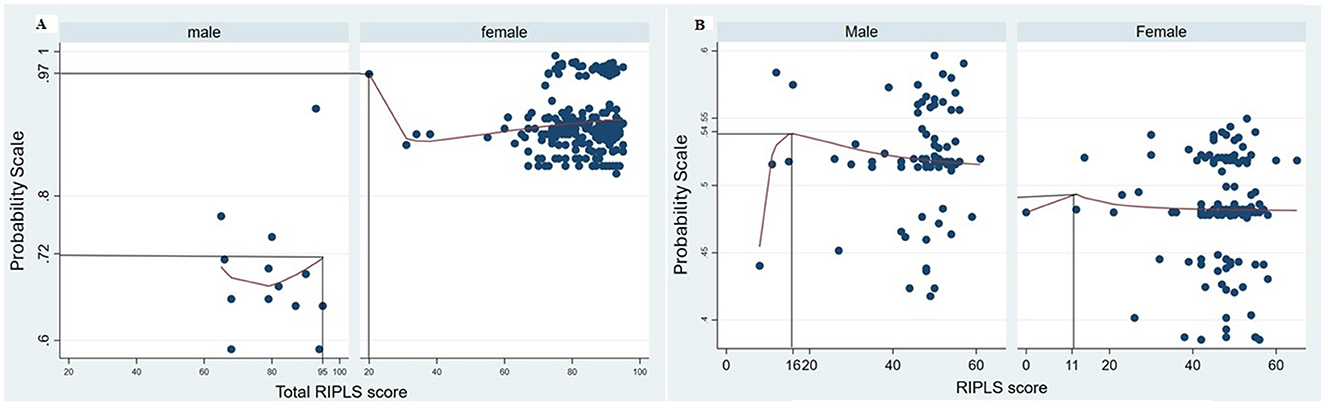
Figure 4. Probit graph showing the probability of the RIPLS score in relation to gender for (A) clinical psychology students and (B) social care students.
Discussion
The primary objectives of this study were to develop a tool to assess KAP related to the prevention and early detection of oral cancer and to evaluate these aspects among postgraduate students in clinical psychology and social care. Additionally, the study explored the relationship between KAP scores and readiness for interprofessional collaborative learning, aiming to understand the potential for integrating these students into oral health initiatives. This needs assessment was conducted with the broader goal of informing the development of an interprofessional education (IPE) module. The findings are presented collectively for both cohorts, acknowledging that the curricula of clinical psychology and social care programs typically do not emphasize diseases of the oral cavity. The participants had no exposure to oral cancer-related aspects in their curriculum. This highlights the importance of targeted educational interventions to bridge existing knowledge gaps and foster collaborative practices in oral cancer prevention and early detection.
Postgraduate clinical psychology students and social care students were selected on the basis of the scope of their disciplinary practice and their contribution to strengthening interprofessional collaborative health care. Additionally, postgraduate students were selected on the basis of their potential client exposure. Unlike other health professionals, e.g., dentistry, where clinical work is part of the undergraduate curriculum, clinical psychology and social care students have better exposure to the clinical environment during their postgraduate education. Thus, keeping in mind the need for experiential learning, during the intended IPE course, postgraduate students were selected from these disciplines to be part of the IP team. The reliability of the survey tools used for this study is a good indicator that the results of the survey contribute to the objective of the study for the cohort of students. The developed questionnaire had high internal consistency, which could indicate high interrelatedness of the items. It could also indicate redundancy of items in the questionnaire (Tavakol and Dennick, 2011). The process of questionnaire development was rigorous (Sujir et al., 2024), and the specific items included were deemed necessary considering the basic knowledge and practice-related questions required for oral cancer prevention and early detection as determined by experts. Two different modes of questionnaire distribution methods were utilized per the permission issued by the school authorities.
Among the clinical psychology students, the majority of survey participants were female, reflecting the gender distribution commonly observed in postgraduate admissions in this field. In contrast, the social care student cohort showed a more balanced distribution of participants by sex, aligning with current enrolment trends in that discipline. Importantly, no statistically significant differences were found in any of the assessed scores—knowledge, attitudes, practices, or readiness for interprofessional learning—based on sex. Overall, the KAP scores related to the early diagnosis and prevention of oral cancer among both cohorts of students were largely unfavorable. This would be expected, as their respective speciality curriculum does not focus on disorders of the oral cavity. However, more than 90% of the students indicated their willingness to learn more about early diagnosis and prevention of oral cancer as well as tobacco and alcohol cessation. This indicates a need to orient this cohort to the basic concepts of oral cancer and its prevention and their role in an interprofessional team contributing to this effort. To the best of our knowledge, this is the first study to report KAP related to oral cancer among clinical psychology and social care students. All the students identified relevant specialists for the diagnosis of oral cancer and were willing to participate in additional training related to oral cancer and habit cessation.
Notably, clinical psychology students had better RIPLS scores than social care students, with a greater proportion of students having good scores. Compared with our previous study, clinical psychology students also had better scores among dental students (Sujir et al., 2024). The readiness for interprofessional collaborative learning among students has been linked to two theories, i.e., role theory (RT) and social identity theory (SIT; Merton et al., 1956; Turner, 1978; Roopnarine and Boeren, 2020). According to RT, behavior is shaped by societal norms associated with a particular role, in this case, a clinical psychology or a social care professional. SIT adds to the concept of shaping behavior through norms exhibited by members of the same group. Thus, professional educational experiences and the environment shape professional identities, which influence collaborative learning readiness. Notably, clinical psychologists most often work closely with at least one other medical health professional, such as a psychiatrist, owing to the complimentary nature of the profession, and are exposed to clinical settings within a hospital for a longer period of time than social care students. Therefore, significant exposure to and interaction with other health professionals during their educational journey may enhance their readiness for collaborative learning. However, this may not be the case among social care professionals. Although hospital postings constitute a small part of the curriculum, the main educational experience among social care professionals is in the community. Thus, their educational environment is comparatively siloed from that of other health professionals. Notably, in the literature, the training of social care professionals to work in an integrated environment has lagged, as it is still centered around traditional roles. Social workers play a crucial role in supporting individuals with complex and multifaceted needs across all stages of life. Their work is especially important for those whose health and wellbeing are shaped by psychosocial challenges or systemic and organizational influences hindering care delivery. These factors also apply to the issues associated with oral cancer. Thus, considerable work is needed to ensure that other health professionals understand the importance of social care professionals for the early diagnosis and prevention of oral cancer. Additionally, social care educational experiences should make space for interprofessional learning opportunities (Barr et al., 2024).
Students' preparedness for interprofessional education (IPE), along with their openness to learning from other disciplines as they share their own expertise, plays a vital role in achieving successful outcomes in IPE initiatives (Mohammed et al., 2021). The RIPLS score was influenced by sex among clinical psychology students, with females having a better probability of obtaining good scores than males do. A previous study in Sweden examined gender differences in the RIPLS score. It demonstrated that females were more likely to have a positive attitude toward teamwork (Wilhelmsson et al., 2011). However, in our study, the intergroup comparisons did not reveal any significant score differences between males and females. This variation could be attributed to the predominance of females among clinical psychology students. Probit analysis contributed to predicting the probability of having a good RIPLS score considering KAP scores and gender. Success of an interprofessional learning module depends on the readiness of the students to actively participate in an interprofessional educational environment, which could be influenced by their overall confidence related to the subject matter. Among clinical psychology students, the probability of having a good RIPLS score was relatively greater than that of social care students. This could indicate a need for additional orientation sessions among social care students concerning the concept of oral cancer and the role of interprofessional collaboration for better outcomes in this disease process. Thus, an additional orientation for social care students toward the concept of a team-based health care delivery model may be beneficial prior to induction into an interprofessional learning environment.
The literature has shown that psychology students are less prepared for interprofessional learning compared to our study (Flato et al., 2022; Hertweck et al., 2012; de Oliveira et al., 2018; Roberts and Forman, 2015). This could be related to context-specific variations in the curriculum (Flato et al., 2022). Additionally, psychology is a broad profession, and for the present study, we included the specialty of clinical psychology, as this discipline would substantially contribute to delivering care for oral cancer patients. Acquavita et al. (2014) included a total of 29 professional students, including law, medicine, nursing, pharmacy, and social work, and reported no significant differences in RIPLS scores among the groups. A call to include social care professions in interprofessional teams has been identified in the past (Barr, 1999). There have been several context-specific interprofessional education programs that have included social care professions (Barett and Greenwood, 2003; Machin et al., 2018; Blacker et al., 2016; Lindqvist et al., 2025). Similarly, the inclusion of psychologists in IP teams has been recognized to be essential for enhancing the understanding of psychological influences on patient care, highlighting the discipline's role in clinical settings, expanding trainees' knowledge of psychology, and fostering effective interdisciplinary collaboration (Ward et al., 2018). A recent systematic review identified 37 articles that included clinical psychology professionals in IP teams and concluded that there is a paucity of literature that describes the role of clinical psychologists in IP teams (Lamparyk et al., 2022). Despite such IP initiatives in the literature, no studies have evaluated the role of clinical psychologists and social professionals in the early diagnosis and prevention of oral cancer.
The results show that when given an opportunity, the students were willing to participate in an interprofessional course on oral cancer prevention and early detection. However, the course design should consider the basic knowledge, attitudes, and practices of individual disciplines of students and their readiness for interprofessional education. Additional orientation programs and educational resources prior to exposure to interprofessional learning could enhance the educational experience of students belonging to various disciplines. Additionally, case-based learning and team-based learning strategies should be employed to ensure sufficient role clarity and teamwork among the interprofessional cohort. However, several limitations related to this study need to be considered. The results of this study represent the findings from three institutions in southern India for social care students and five institutions for clinical psychology students; thus, the results may be context specific. Additionally, such surveys are associated with self-reporting bias, and as the internal consistency values are high, they could indicate redundancy in items. Further studies may be planned to distinguish between the two learning environments and the differences in readiness for interprofessional learning.
Conclusion
This study aimed to develop and validate a tool to assess KAP related to the prevention and early detection of oral cancer among postgraduate students in clinical psychology and social care. Additionally, it explored the potential of these students to demonstrate strong KAP scores, which would reflect their readiness for interprofessional collaborative learning. The findings revealed unfavorable KAP scores across both cohorts, indicating significant gaps in awareness and preparedness for oral cancer prevention and early detection. The next steps include designing a curriculum that caters to deficient knowledge, attitudes and practice-related content for oral cancer prevention and early detection among the student cohort to better orient them to their role in an interprofessional practice-related setting. As the RIPLS scores mostly showed a positive attitude toward interprofessional learning among students, this would indicate their readiness to learn, with, from and about students from other professions that constitute the IP team. Overall, these results underscore the need for targeted educational interventions and provide a valuable baseline for designing future IPE programs focused on oral cancer prevention and early detection. This article is also the first attempt to include allied and social care professionals systematically within the health care delivery network for early diagnosis and prevention of oral cancer, which would require multifaceted inquiries to inform policy.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Ethics Committee, Manipal College of Dental Sciences Mangalore. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Visualization, Writing – original draft, Writing – review & editing. JA: Conceptualization, Formal analysis, Investigation, Supervision, Methodology, Resources, Visualization, Writing – original draft, Writing – review & editing. A: Conceptualization, Formal analysis, Investigation, Supervision, Methodology, Visualization, Writing – original draft, Writing – review & editing. CA: Conceptualization, Formal analysis, Investigation, Methodology, Resources, Visualization, Validation, Writing – original draft, Writing – review & editing. BU: Conceptualization, Formal analysis, Methodology, Resources, Visualization, Validation, Writing – review & editing. JG: Conceptualization, Methodology, Validation, Writing – review & editing. VG: Data curation, Formal analysis, Investigation, Resources, Project administration, Writing – review & editing. MM: Data curation, Formal analysis, Investigation, Resources, Project administration, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor [AS] declared a past co-authorship with the author [BU].
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Acquavita, S. P., Lewis, M. A., Aparicio, E., and Pecukonis, E. (2014). Student perspectives on interprofessional education and experiences. J. Allied Health 43, e31–e36.
Andermann, A. (2016). Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ 188, E474–E483. doi: 10.1503/cmaj.160177
Ayre, C., and Scally, A. J. (2014). Critical values for Lawshe's content validity ratio: revisiting the original methods of calculation. Measure. Eval. Counsel. Dev. 47, 79–86. doi: 10.1177/0748175613513808
Babu, A., Mathew, R. T., and Shetty, R. (2023). Pattern of oral cancer in India: an analysis of hospital based cancer registry data. J. Indian Acad. Oral Med. Radiol. 35, 497–500. doi: 10.4103/jiaomr.jiaomr_145_23
Barett, G., and Greenwood, R. (2003). Integrating interprofessional education into 10 health and social care programmes. J. Interprof. Care 17, 293–301. doi: 10.1080/1356182031000122915
Barr, H. (1999). Integrating health and social care. J. Interprof. Care 13, 205–206. doi: 10.3109/13561829909010363
Barr, H., Anderson, E. S., Fenge, L. A., and Hutchings, M. (2024). Social work in integrated care. J. Interprof. Care 38, 997–1007. doi: 10.1080/13561820.2024.2405552
Blacker, S., Head, B. A., Jones, B. L., Remke, S. S., and Supiano, K. (2016). Advancing hospice and palliative care social work leadership in interprofessional education and practice. J. Soc. Work End Life Palliat. Care 12, 316–330. doi: 10.1080/15524256.2016.1247771
Bouvard, V., Nethan, S. T., Singh, D., Warnakulasuriya, S., et al. (2022). IARC perspective on oral cancer prevention. N. Engl. J. Med. 387, 1999–2005. doi: 10.1056/NEJMsr2210097
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., and Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424. doi: 10.3322/caac.21492
Chan, H. L., Chan, A. K., Chu, C. H., and Tsang, Y. C. (2023). Smoking cessation in dental setting: a narrative review on dental professionals' attitude, preparedness, practices and barriers. Front. Oral Health 4:1266467. doi: 10.3389/froh.2023.1266467
de Oliveira, V. F., Bittencourt, M. F., Navarro Pinto, Í. F., Lucchetti, A. L. G., da Silva Ezequiel, O., and Lucchetti, G. (2018). Comparison of the readiness for interprofessional learning and the rate of contact among students from nine different healthcare courses. Nurse Educ. Today 63, 64–68. doi: 10.1016/j.nedt.2018.01.013
Dwivedi, P., Lohiya, A., Bahuguna, P., Singh, A., Sulaiman, D., Singh, K., et al. (2023). Cost-effectiveness of population-based screening for oral cancer in India: an economic modelling study. Lancet Regional Health Southeast Asia 16:100224. doi: 10.1016/j.lansea.2023.100224
Flato, U. A. P., Nemer, P., Donega, C. R., Vieira, A. A. C., Rubira, C., Serva, F. M., et al. (2022). Awareness of interprofessional learning as a tool to improve a Brazilian university curriculum. J. Interprof. Care 36, 670–675. doi: 10.1080/13561820.2021.1965559
Hertweck, M. L., Hawkins, S. R., Bednarek, M. L., Goreczny, A. J., Schreiber, J. L., and Sterrett, S. E. (2012). Attitudes toward interprofessional education: comparing physician assistant and other health care professions students. J. Phys. Assis. Educ. 23, 8–15. doi: 10.1097/01367895-201223020-00003
Lamparyk, K., Williams, A. M., Robiner, W. N., Bruschwein, H. M., and Ward, W. L. (2022). Interprofessional education: current state in psychology training. J. Clin. Psychol. Med. Settings. 29, 20–30. doi: 10.1007/s10880-021-09765-5
Lindqvist, S., Wilsher, S. H., Vasset, F., Almås, S. H., Willumsen, E., Iversen, H. P., et al. (2025). Integrating interprofessional education in health and social care curricula to equip our future workforce–qualitative findings from senior leaders. Soc. Sci. Human. Open 12:101734. doi: 10.1016/j.ssaho.2025.101734
Machin, L. L., Bellis, K. M., Dixon, C., Morgan, H., Pye, J., Spencer, P., et al. (2018). Interprofessional education and practice guide: designing ethics-orientated interprofessional education for health and social care students'. J. Interprof. Care 33, 608–618. doi: 10.1080/13561820.2018.1538113
Merton, R. K., Bloom, S., and Rogoff, N. (1956). Columbia–Pennsylvania: studies in the sociology of medical education. Acad. Med. 31, 552–565.
Mohammed, C. A., Narsipur, S., Vasthare, R., Singla, N., Yan Ran, A. L., and Suryanarayana, J. P. (2021). Attitude towards shared learning activities and interprofessional education among dental students in South India. Euro. J. Dental Educ. 25, 159–167. doi: 10.1111/eje.12586
Parsell, G., and Bligh, J. (1999). The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Med. Educ. 33, 95–100. doi: 10.1046/j.1365-2923.1999.00298.x
Reeves, S., Fletcher, S., Barr, H., Birch, I., Boet, S., Davies, N., et al. (2016). A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39′. Med. Teach. 38, 656–668. doi: 10.3109/0142159X.2016.1173663
Roberts, L. D., and Forman, D. (2015). Interprofessional education for first-year psychology students: career plans, perceived relevance and attitudes. J. Interprof. Care 29, 188–194. doi: 10.3109/13561820.2014.967754
Roopnarine, R., and Boeren, E. (2020). Applying the Readiness for Interprofessional Learning Scale (RIPLS) to medical, veterinary and dual degree Master of Public Health (MPH) students at a private medical institution. PLoS ONE 15:e0234462. doi: 10.1371/journal.pone.0234462
Sujir, N., Ahmed, J., Ramakrishna, A., Mohammed, C. A., Unnikrishnan, B., and Gilbert, J. H. (2024). Needs assessment for interprofessional education module on prevention and early detection of oral cancer among dental interns: a cross-sectional survey. BMC Oral Health 24:1351. doi: 10.1186/s12903-024-05123-7
Tavakol, M., and Dennick, R. (2011). Making sense of Cronbach's alpha. Int. J. Med. Educ. 27, 53–55. doi: 10.5116/ijme.4dfb.8dfd
Thampi, V., Hariprasad, R., John, A., Nethan, S., Dhanasekaran, K., Kumar, V., et al. (2022). Feasibility of training community health workers in the detection of oral cancer. JAMA Netw. Open 5:e2144022. doi: 10.1001/jamanetworkopen.2021.44022
Ward, W., Zagoloff, A., and Rieck, C. (2018). Interprofessional education: opportunities and challenges for psychology. J. Clin. Psychol. Med. Settings 25, 250–266. doi: 10.1007/s10880-017-9538-3
Wilhelmsson, M., Ponzer, S., Dahlgren, L. O., Timpka, T., and Faresjö, T. (2011). Are female students in general and nursing students more ready for teamwork and interprofessional collaboration in healthcare? BMC Med. Educ. 11:1. doi: 10.1186/1472-6920-11-15
World Health Organization (2010). Framework for Action on Interprofessional Education and Collaborative Practice. Geneva: Health Professions Network of Nursing and Midwifery, Department of Human Resources. Available online at: http://www.who.int/hrh/resources/framework_action/en/ (Accessed December 10, 2024).
Zahiruddin, Q. S., Jena, D., Ballal, S., Kumar, S., Bhat, M., Sharma, S., et al. (2024). Burden of oral cancer and associated risk factors at national and state levels: a systematic analysis from the global burden of disease in India, 1990–2021. Oral Oncol. 159:107063. doi: 10.1016/j.oraloncology.2024.107063
Keywords: interprofession education, oral cancer, prevention and early detection, social care professionals, clinical psychology
Citation: Sujir N, Ahmed J, Anand Ramakrishna, Ali Mohammed C, Unnikrishnan B, Gilbert JHV, Gangadhara VK and Monteiro MJ (2025) Integrating clinical psychology and social care in oral cancer prevention & early detection: a needs assessment for interprofessional education. Front. Educ. 10:1696403. doi: 10.3389/feduc.2025.1696403
Received: 31 August 2025; Accepted: 30 October 2025;
Published: 27 November 2025.
Edited by:
Afeez Abolarinwa Salami, University of Puthisastra, CambodiaReviewed by:
Emeka Okeke, Cephas Health Research Initiative Inc, NigeriaAbhishek Banerjee, Kolhan University, India
Copyright © 2025 Sujir, Ahmed, Anand Ramakrishna, Ali Mohammed, Unnikrishnan, Gilbert, Gangadhara and Monteiro. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junaid Ahmed, SnVuYWlkLmFobWVkQG1hbmlwYWwuZWR1
 Nanditha Sujir
Nanditha Sujir Junaid Ahmed
Junaid Ahmed Anand Ramakrishna
Anand Ramakrishna Ciraj Ali Mohammed
Ciraj Ali Mohammed Bhaskaran Unnikrishnan
Bhaskaran Unnikrishnan John H. V. Gilbert
John H. V. Gilbert Vasudha Kadikadka Gangadhara
Vasudha Kadikadka Gangadhara Meena Juliet Monteiro10
Meena Juliet Monteiro10