- 1Department of Obstetrics & Gynecology, Baylor College of Medicine, Houston, TX, United States
- 2McGovern Medical School, University of Texas Health Science Center, Houston, TX, United States
- 3Department of Gynecologic Oncology and Reproductive Medicine, University of Texas Medical Doctor (MD) Anderson Cancer Center, Houston, TX, United States
- 4Department of Anatomical Pathology, University of Texas Medical Doctor (MD) Anderson Cancer Center, Houston, TX, United States
Objective: Mucinous ovarian carcinomas (mOC) often harbor unique molecular alterations differentiating them from other epithelial ovarian carcinoma subtypes. We sought to characterize the somatic genomic mutation patterns in mOC and elucidate their associations with oncologic outcomes.
Methods: All patients with mOC treated at a single institution between 2005–2023 were identified, and those with validated tumor molecular profiling (TMP) using next-generation sequencing of somatic variants were included. Progression-free survival (PFS) and overall survival (OS) were calculated on a Kaplan-Meier estimator. Multivariable analysis was performed using Cox regression models.
Results: Forty patients were included in this retrospective cohort; 34 (85%) had at least 1 genomic alteration on TMP, with a median of 3 mutations (range 0-30). TP53 (68%) and KRAS (63%) were most frequently altered, and 21 patients (53%) had tumors with TP53/KRAS co-mutations. Patients with TP53/KRAS co-mutations were younger (median 27.9 vs 54.1 y, p=0.01) and were more likely to have early-stage disease (86% vs 47%, p=0.02) than patients without these co-mutations. On multivariable analysis, TP53/KRAS co-mutations were associated with decreased PFS (adjusted hazard ratio [aHR] 4.02, 95% confidence interval [CI] 1.46-12.5, p=0.01) and OS (aHR 21.4, 95% CI 4.28-156, p<0.001). On subgroup analysis of stage I tumors (N=27), the presence of TP53/KRAS co-mutations remained independently associated with worse OS (aHR 8.66, 95% CI 1.50-93.8, p=0.03).
Conclusion: A substantial proportion of mOCs have concurrent TP53 and KRAS alterations on TMP, and this may portend worse survival, even for patients with early-stage disease. TMP could be a useful tool for prognostication and can be considered for patients with mOC at the time of diagnosis.
Introduction
Ovarian cancer is a leading cause of mortality in patients with gynecologic malignancies and the second most common type of gynecologic malignancy in the United States (1). Mucinous ovarian carcinoma (mOC) is a rare subtype of epithelial ovarian carcinoma that accounts for less than 5% of all ovarian cancer cases (2, 3). Traditionally, the mainstay of treatment is surgery followed by chemotherapy for patients with advanced-stage or higher-risk disease. The 5-year overall survival of patients who present with early-stage disease usually exceeds 80% but drastically decreases for those with advanced-stage disease (3). When compared to high-grade serous ovarian carcinomas, mOC is less responsive to traditional cytotoxic chemotherapy; additionally, there is a lack of consensus on the preferred treatment regimen (4).
Due to these challenges and the unique behavior of mOC, researchers and clinicians have sought to characterize its distinct molecular profile in the hopes of better understanding its pathogenesis and identifying possible therapeutic targets. KRAS and TP53 gene mutations are commonly implicated in many types of cancer, including epithelial ovarian cancer (5). KRAS is a proto-oncogene that functions as a key mediator of the RAS signaling pathway, which drives cell growth and proliferation; specifically, codon 12 is recognized as a mutational “hotspot” across many cancer types. TP53 is a tumor suppressor gene commonly mutated in a variety of cancers; its mutation leads to a variety of genetic aberrations that can lead to cancer formation and progression. The most common alterations in TP53 include missense and nonsense mutations, many of which impair its DNA binding and transactivation functions (6, 7). In this study, we sought to characterize the mutational landscape of mOCs from patients treated at our institution and to examine potential associations of TP53 and KRAS mutations with patient outcomes.
Methods
Following IRB approval, a retrospective cohort study of all patients diagnosed with mOC between 2005–2023 at a single comprehensive cancer center was performed. Study subjects were identified as part of an institutional internal rare cancers’ registry, and histology was confirmed by central pathology review. Patients were included if they had tumor molecular profiling (TMP) via next-generation sequencing (NGS). Patients were excluded if surgery was not performed at some point during their treatment, if they had mixed histology or mOC from a separate site, a synchronous malignancy, or an incomplete medical record available for review (Supplementary Figure 1.1).
Basic demographic information was extracted from the electronic medical record. Cancer-specific data were also abstracted, including stage, grade, surgical records, all TMP and genomic data, as well as dates of diagnosis, treatment, recurrence, and death. TMP and genomic data were obtained from either internal or external sequencing panels, which were ordered either at initial diagnosis or at the time of recurrence, based on the discretion of the primary treating oncologist. All pathogenic variants identified through these panels were recorded (Supplementary Table 1.2). Individual mutations in TP53 and KRAS were then independently cross-referenced with ClinVar and the NCI’s TP53 Database to assess and validate their functional significance. Study data were collected and managed using REDCap (Research Electronic Data Capture) hosted at our institution. Staging was based on FIGO 2014 criteria, and all cases diagnosed prior to 2014 were “re-staged” for the purposes of this study. Primary outcomes included progression-free survival (PFS) and overall survival (OS). PFS was defined as the length of time from the date of diagnosis to the date of disease recurrence, and OS was defined as the length of time from the date of diagnosis to the date of death. Patients were censored if they did not experience disease recurrence or death by the end of data collection (December 31, 2023).
Demographic and clinical characteristics were analyzed and compared using t-tests and chi-square/Fisher exact tests. Survival indices were calculated on a Kaplan-Meier estimator using the log-rank method. Multivariable analyses were performed using Cox regression models. All statistical analyses were performed using GraphPad Prism 10.2.1 (Dotmatics; Boston, MA, USA). Statistical significance was set at p ≤ 0.05.
Results
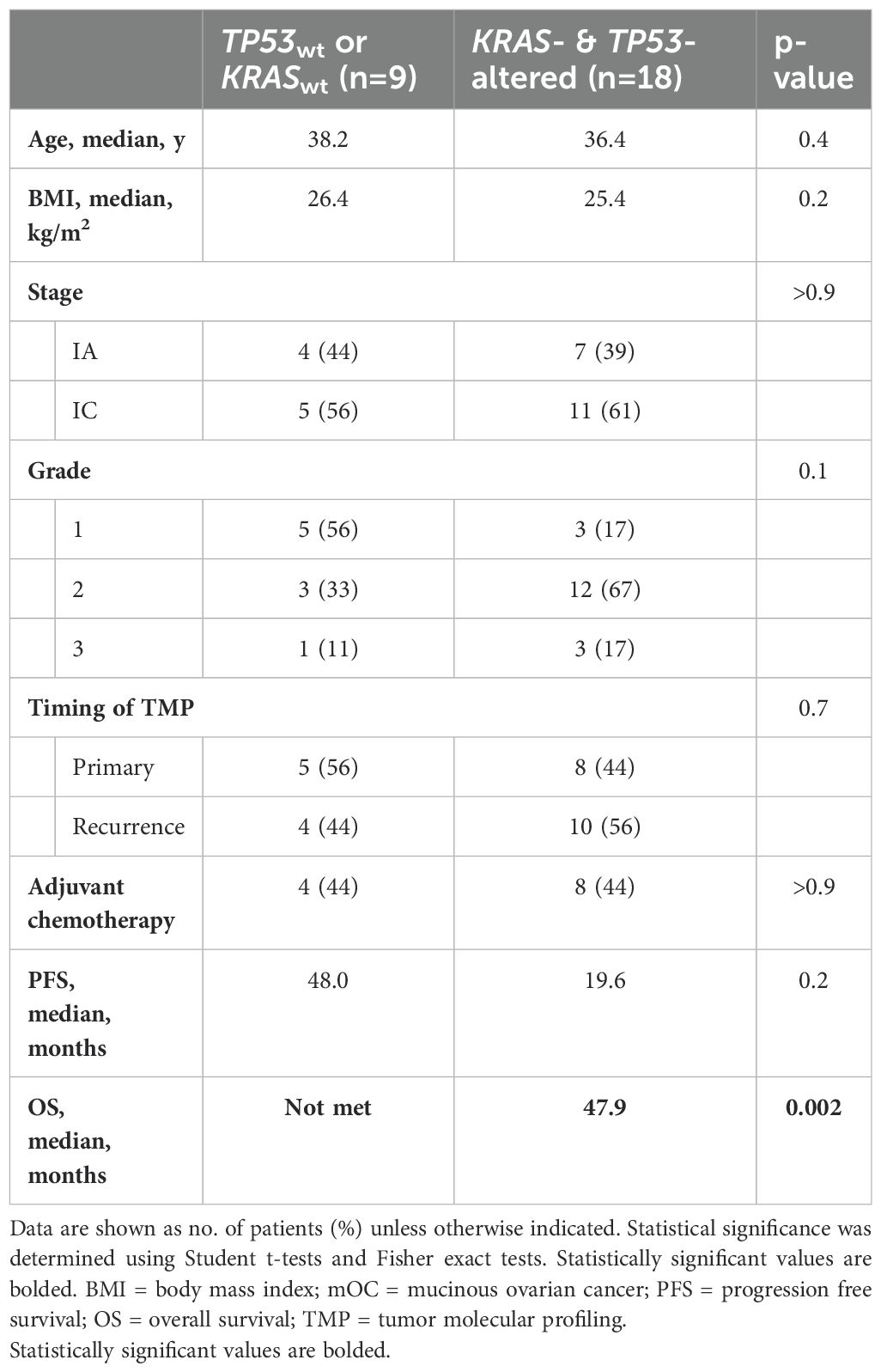
A total of 40 patients were included in the final cohort (Supplementary Table 1.1). All patients underwent primary surgery, and 25 (63%) received adjuvant systemic chemotherapy. At least 1 genomic alteration was identified on TMP in 34 patients (85%), with a median of 3 mutations (range 0-30). In total, 148 alterations in 73 different genes were found, with missense mutations being the most common (55.9%), followed by amplification (10.5%) and deletion (8.6%) (Figure 1). TP53 (67.5%) and KRAS (62.5%) were the most frequently altered genes; 21 patients (53%) had tumors with TP53/KRAS co-mutations. Most KRAS mutations occurred at codon 12, with G12D (44%) and G12V (32%) being the most prevalent. TP53 mutations were more diverse, with 23 distinct variants identified (Supplementary Table 1.3).
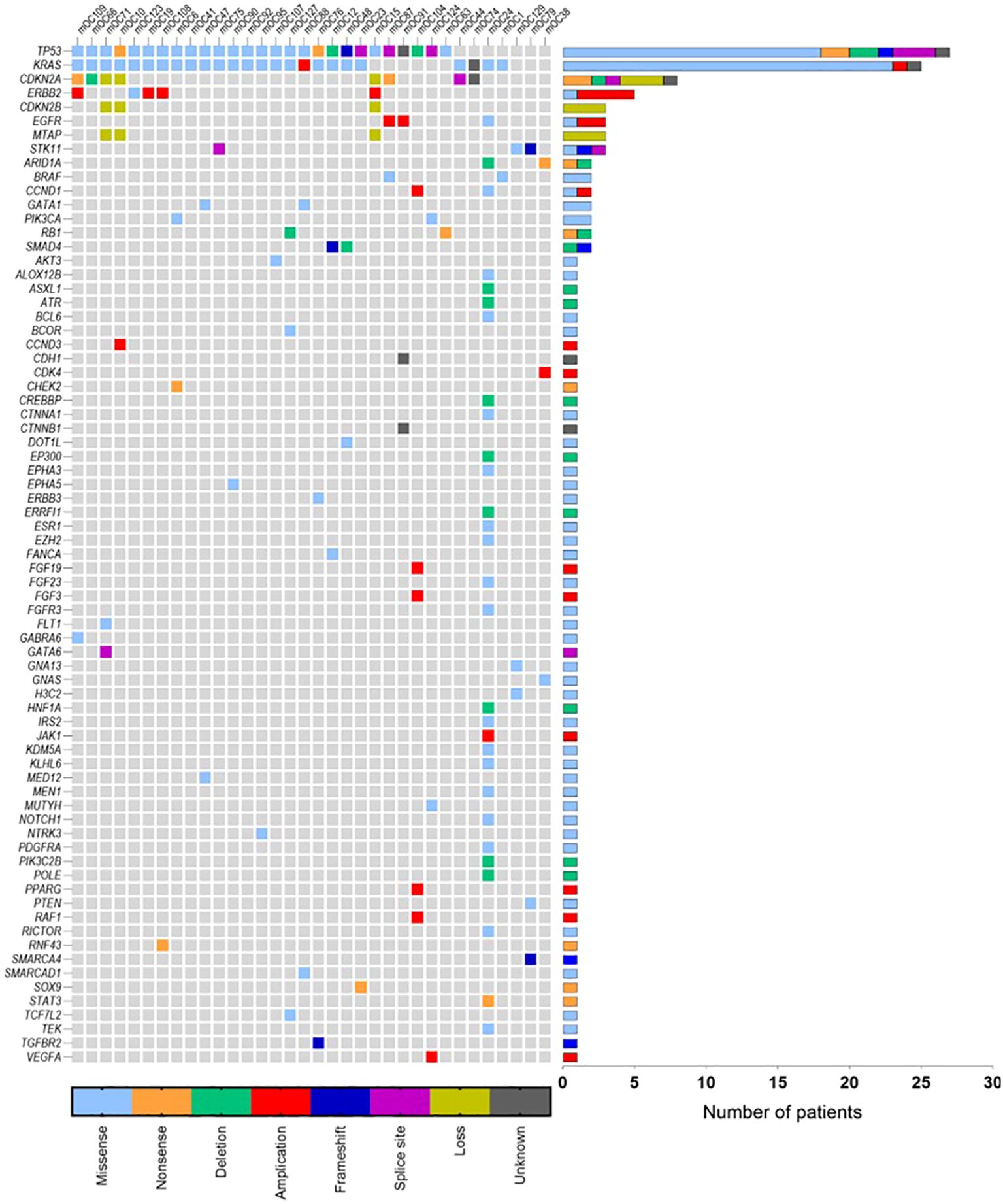
Figure 1. Oncoplot of mOC patients with alterations (N=34) identified on NGS. Six patients without any identifiable mutations are not included. TP53 (N=27) and KRAS (N=25) were the most frequently identified genes with alterations. Missense mutations were the most common detected type (56.4%), followed by amplifications (10.7%) and deletions (9.4%).
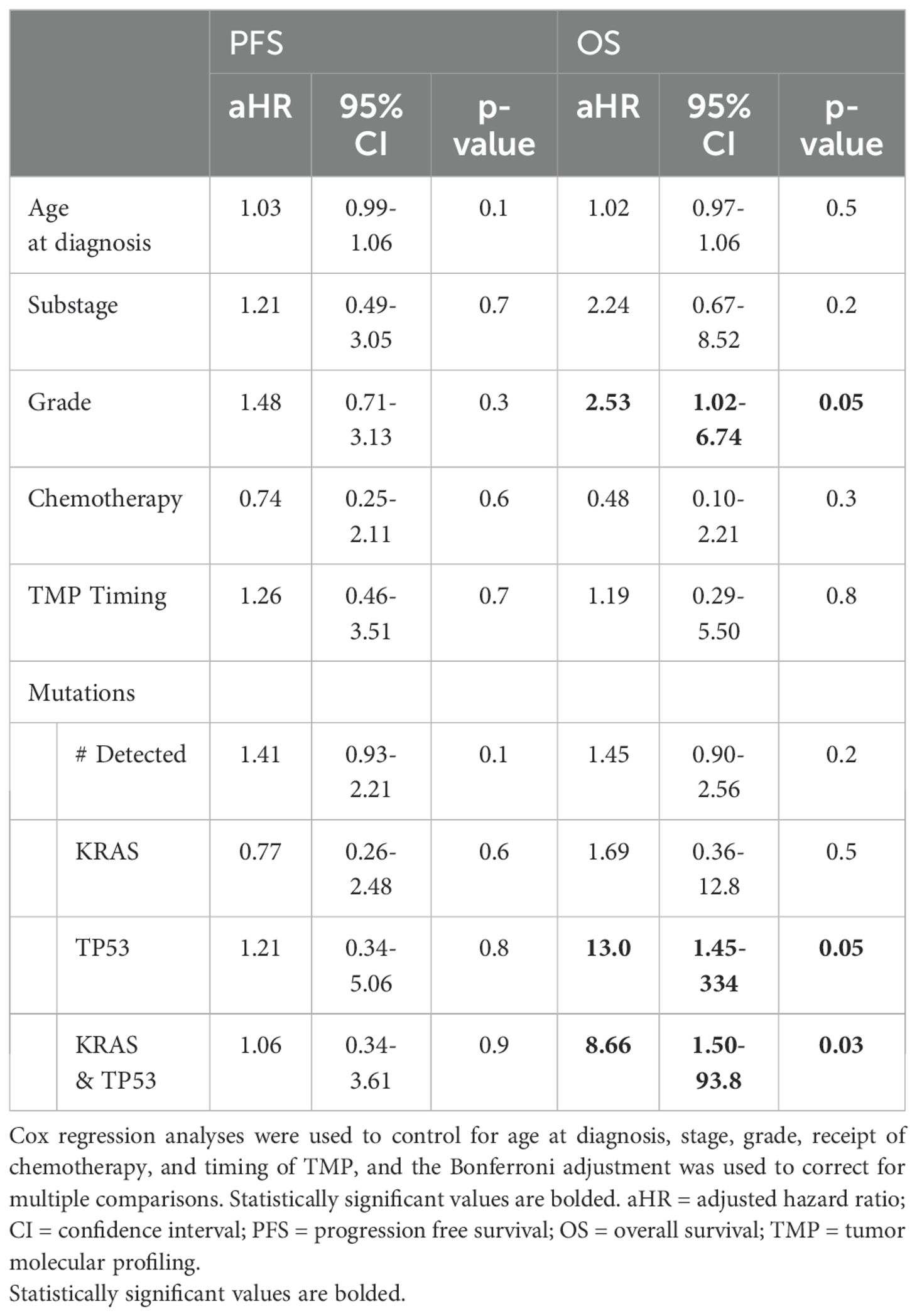
Patients with TP53/KRAS co-mutations were younger (median 27.9 vs 54.1 y, p=0.01) and were more likely to have stage I disease (86% vs 47%, p=0.02) than patients without TP53/KRAS co-mutations (Table 1A). There were no differences in body mass index (BMI), tumor grade, or chemotherapy administration between the 2 groups. Samples collected from recurrent tumors demonstrated more TP53/KRAS co-mutations than did primary tumor samples (62% vs 38%), but this difference was not significant (p=0.07). On subgroup analysis of patients with stage I disease, there were no differences in age at diagnosis, BMI, tumor grade, chemotherapy administration, or TMP timing (Table 1B). There were also no differences in the proportion of patients with stage IA or IC disease at diagnosis (p>0.9). In this analysis, stage IC included IC1 (N=8), IC2 (N=1), and IC3 (N=7); there were no patients with stage IB disease at diagnosis. In the overall cohort, patients with TP53/KRAS co-mutations and those without did not have significantly different median PFS (18.9 vs 19.8 months, p=0.6) or OS (46.5 vs 54.0 months, p=0.3); however, among patients with stage I disease, those with TP53/KRAS co-mutated tumors had significantly shorter median OS compared to those without the co-mutation (47.9 months vs median not met, p=0.02) (Figure 2). No significant differences in survival curves were observed when stratifying by individual mutations in either KRAS or TP53 alone (Supplementary Figures 1.2 & 1.3).
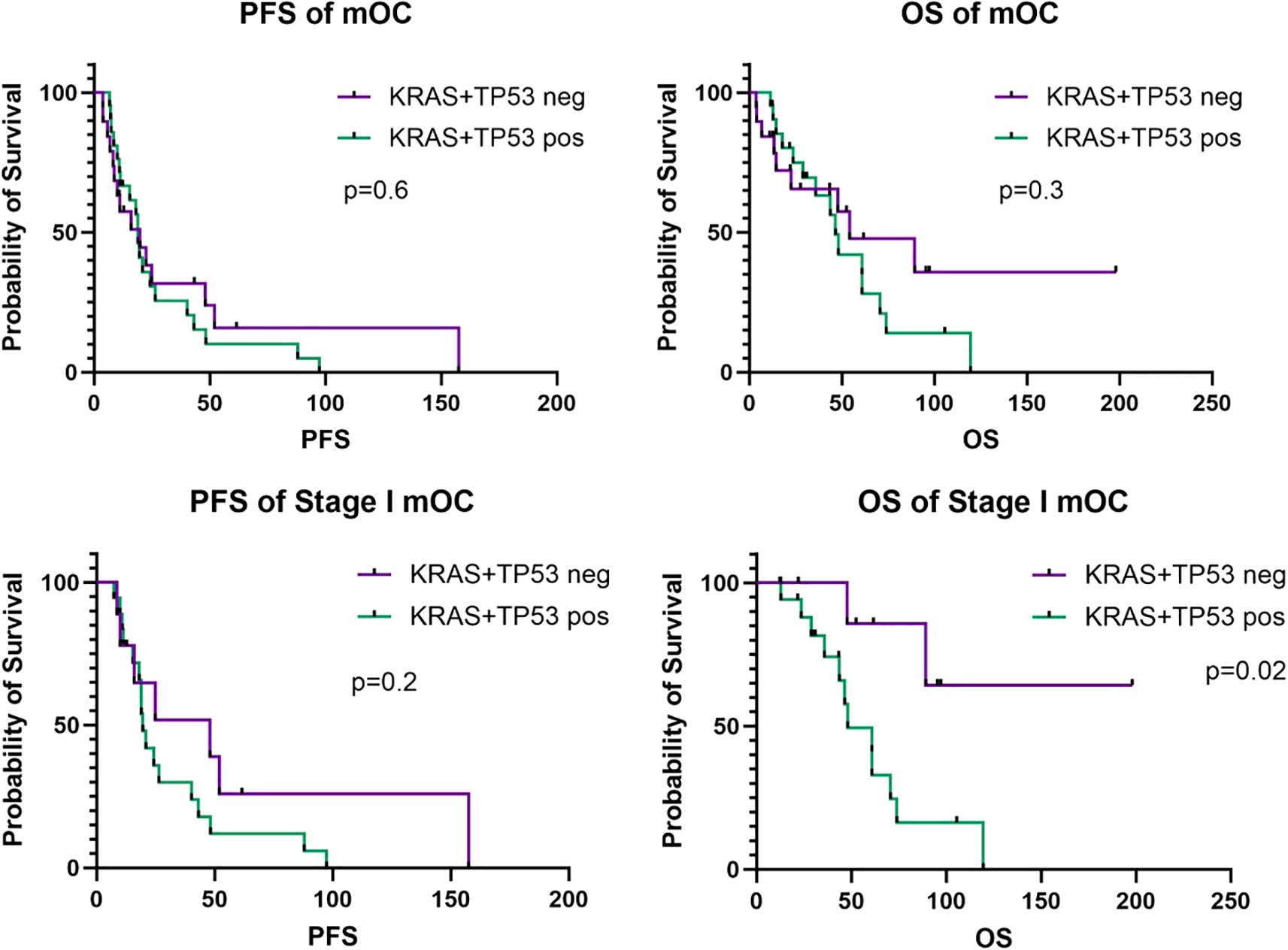
Figure 2. Progression-free survival (PFS) and overall survival (OS) curves for the entire study cohort (N=40) and the stage I subgroup (N=27). Survival analyses were calculated on a Kaplan-Meier estimator using the log-rank method. Y-axis (probability of survival) is quantified by percentages. X-axis (PFS or OS) is quantified by number in months. mOC, mucinous ovarian cancer.
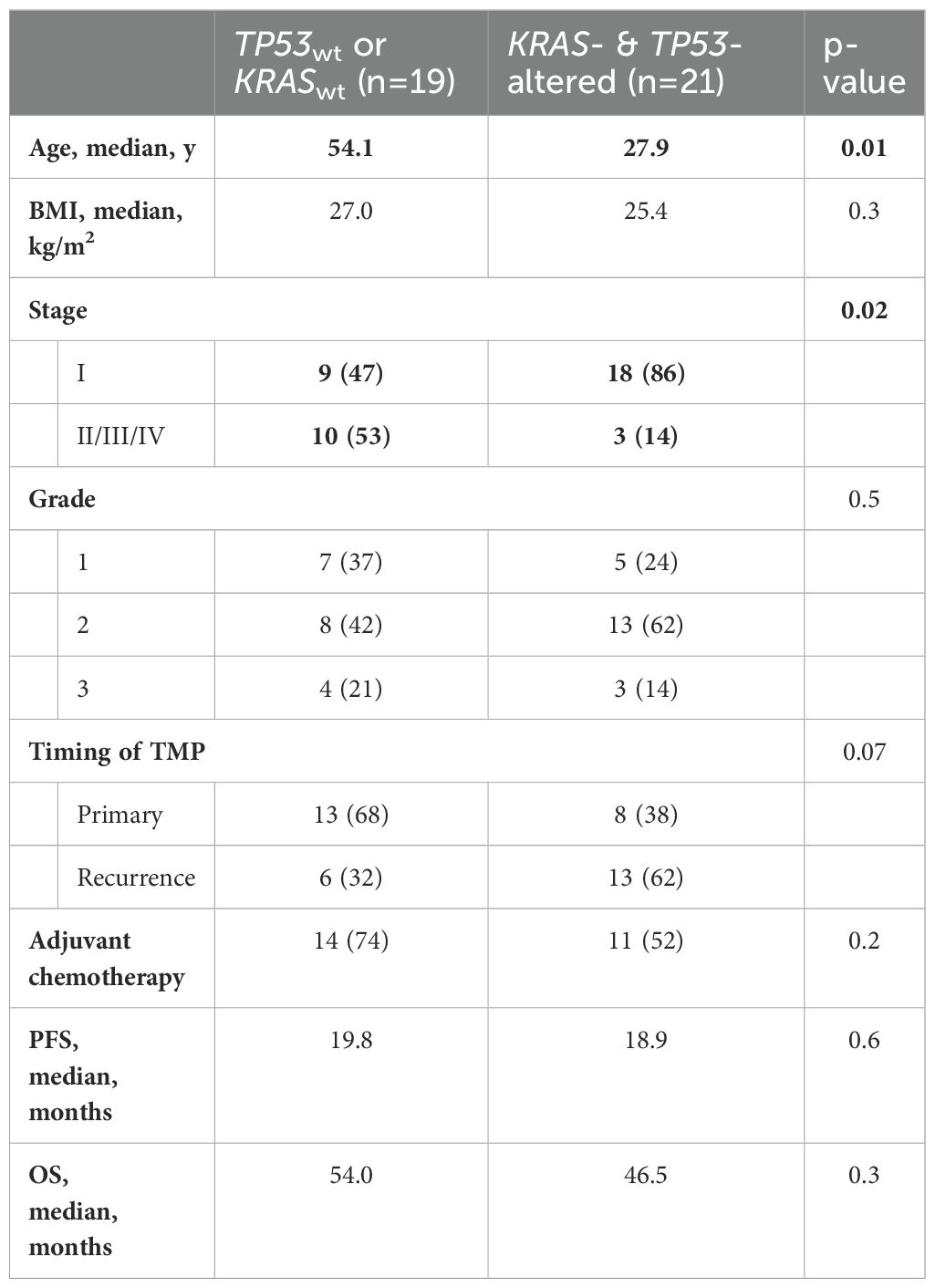
Table 1A. Comparison of demographic and clinical characteristics between patients with and without KRAS/TP53 co-mutations.
Clinically relevant variables were selected as potential confounders. After adjusting for stage and age, as well as grade, chemotherapy, and timing of TMP collection, multivariable analyses demonstrated that the presence of TP53/KRAS co-mutations was associated with both lower PFS (aHR 4.02, 95% CI 1.46-12.5, p=0.01) and OS (aHR 21.4, 95% CI 4.28-156, p<0.001) (Table 2A). Other independent associations found were tumor grade with worse OS (adjusted hazard ratio [aHR] 2.19, 95%CI 1.10-4.29, p=0.02), and stage with both worse PFS (aHR 7.42, 95% CI 2.55-23.1, p<0.001) and OS (aHR 11.6, 95% CI 3.12-50.0, p<0.001). On subgroup analysis of stage I tumors (N=27), the presence of TP53/KRAS co-mutations remained independently associated with worse OS (aHR 8.66, 95% CI 1.50-93.8, p=0.03) (Table 2B). High-grade disease was also independently associated with worse OS (aHR 2.53, 95% CI 1.02-6.74, p=0.05). Substage (stage IA vs IC) was not associated with changes in either PFS or OS.
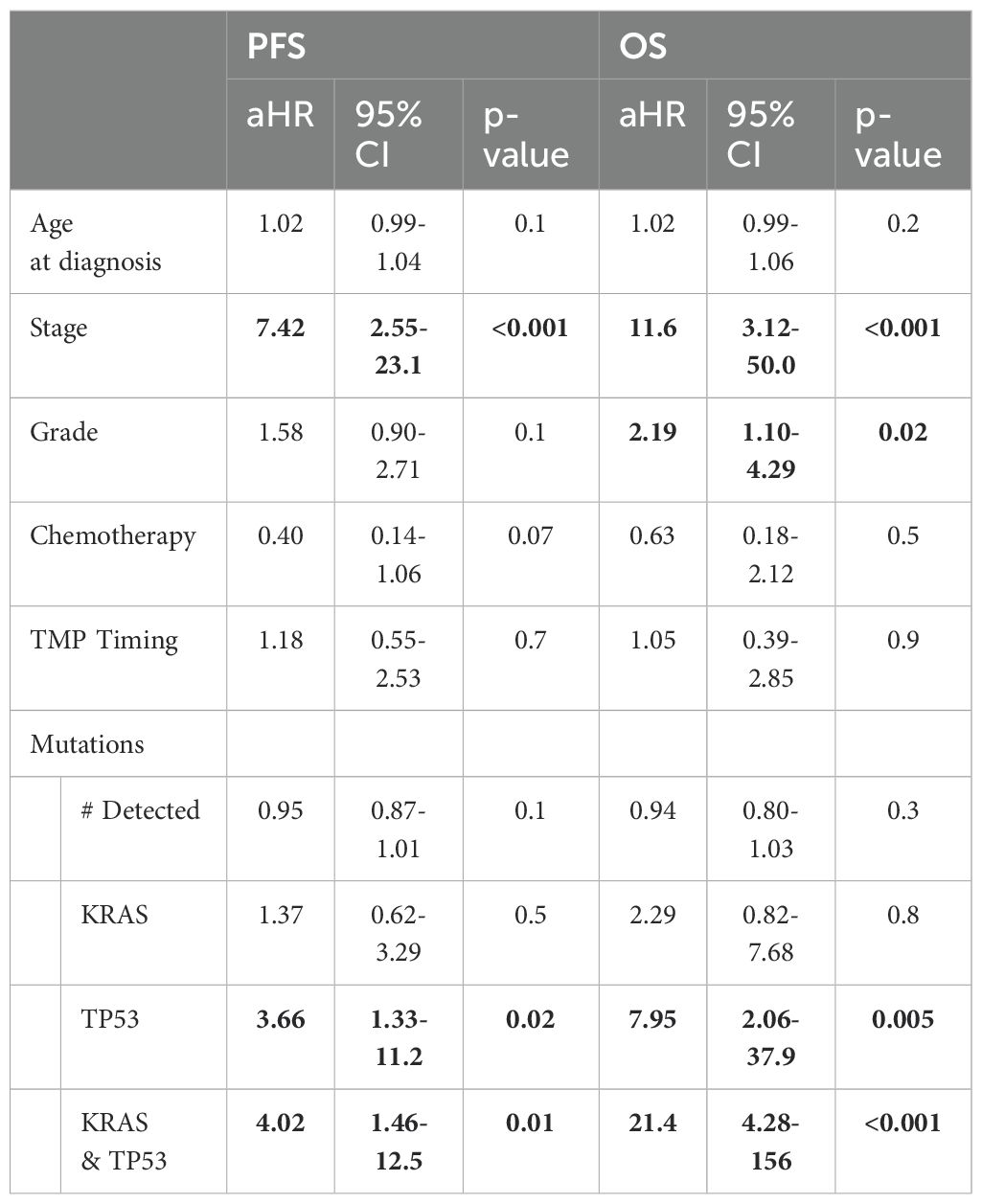
Table 2. Multivariable analyses of independent associations of clinical factors and KRAS/TP53 mutation status with survival.
Table 2A. Full study cohort (N=40).
Discussion
For early-stage mOC, comprehensive surgery can be curative without the need for adjuvant treatment, with reported 5-year survival rates of 86-90% (8, 9). For patients with advanced-stage or recurrent disease, however, there is a paucity of evidence to guide treatment owing to the rarity of this tumor. There is also no clear consensus on how to appropriately risk-stratify patients with early stage mOC for the need for adjuvant chemotherapy. Current guidelines are extrapolated from historical trials dominated by other histological subtypes of high-grade epithelial carcinomas (10). There is growing evidence that, much like low-grade serous ovarian cancer, mucinous tumors represent a separate and distinct entity from other epithelial ovarian malignancies with respect to their pattern of invasion, recurrence, and response to therapy (11, 12).
At present, the extent of disease warranting adjuvant treatment for stage I mOC is up for debate, with some groups advocating more aggressive treatment starting with stage IB rather than stage IC disease (13, 14). There is less dispute about the management of stage IA disease with surgery alone, though some recent evidence suggests that consideration of adjuvant treatment for patients with infiltrative subtypes may be reasonable given the potentially higher risk of recurrence (15–17). Retrospective cohorts have shown that patients with infiltrative stage I disease demonstrate increased rates of recurrence when compared to those with expansile histology, especially after fertility-sparing surgery, and that survival outcomes were comparable to patients with stage I high grade serous carcinomas (18, 19).
Furthermore, the choice of specific adjuvant therapies remains unsettled. Following the early closure of GOG241 due to poor accrual, some retrospective data have suggested the use of a gastrointestinal-based regimen of oxaliplatin, capecitabine, and 5-fluorouracil over the traditional ovarian cancer-based carboplatin and paclitaxel regimen, but clear survival benefit has not been consistently demonstrated (20–22).
Our data suggest that tumor mutational status could be an important step in risk stratification, as patients with TP53/KRAS co-mutations had significantly shorter OS than did patients without co-mutations, particularly among those with stage I disease at diagnosis. Given that both stage I subgroups had otherwise similar clinical and demographic features, it is possible that the distinct genetic profiles could be driving their disparate outcomes. These results may warrant consideration of collecting TMP for patients with mOC.
In addition to determining who needs adjuvant treatment, there is also a need for targeted treatment options more suited to the distinct molecular profile of mOC. As TMP becomes more widely implemented in oncology, specific actionable genetic targets have been identified. In KRAS-altered carcinomas and adenocarcinomas, codon 12 is the most frequently mutated, and the G12D mutation is generally the most prevalent (23). Its favorable structural conformation and downstream targeting has been shown to create protein expression profiles distinct from other KRAS mutations, contributing to its high oncogenic potential as well as unique clinical outcomes (24). In our cohort, the G12D mutation was present in most of the KRAS-altered tumors, consistent with its reported prevalence in other KRAS-altered cancer types. In contrast, TP53 mutations exhibit a much wider heterogeneity in mOC, making therapeutic targeting more challenging in this population (Supplementary Table 1.3).
Recent breakthroughs in targeting the RAS oncogene began with KRAS-G12C inhibition, which has shown some promise in phase I/II clinical trials for metastatic lung, pancreatic, and colorectal carcinomas (25–28). Small molecules with anti-KRAS-G12D activity have shown remarkable response in preclinical models, and several first-in-human trials are currently in recruitment, with clinical data anticipated as early as this year (NCT05533463, NCT05737706, NCT06040541, NCT05382559) (29–34). It is important to note that though these trials are open to patients with all solid tumors with the KRAS-G12D mutation, their supporting preclinical data rarely include gynecologic cancer models. As underscored by our cohort, a substantial proportion of mOCs harbor KRAS mutations. The negative associations of KRAS mutations with recurrence and survival are not limited to mOC and are evident in other subtypes of epithelial ovarian cancers as well (35, 36). Additionally, somatic mutational analysis comparing mOC with mucinous carcinomas of other primary origins showed significant parallels between mOC and pancreatic carcinomas, especially with respect to specific KRAS and TP53 mutations (37). This may represent a potential alternative or subsequent therapy to traditional chemotherapy for patients with mOC, especially in the contemporary era of increasing approvals for mutation-driven, tumor-agnostic treatment options (38–40).
This study is limited by its retrospective and single-institutional nature. Though this work represents one of the largest single institutional retrospective cohorts reported for mOC, statistical associations should be carefully interpreted in the context of the relatively small sample size and limited power, especially evident in some of the wide confidence intervals in this analysis. Furthermore, the 18-year duration of the study coincided with significant advances in sequencing technology, including improvements in accessibility, sensitivity, and throughput, both within our institution and across commercial platforms. However, specific details regarding the evolution of “generations” of testing used by external companies are not publicly available (Supplementary Table 1.2). Although the availability of molecular profiling was clearly beneficial for patient care, the use of heterogeneous sequencing platforms introduces the potential for unrecognized confounding variables, particularly in a retrospective study where testing methodologies varied over time.
In this cohort, the histologic distinction between infiltrative and expansile patterns was only available for a small portion of our patients, and thus not included in the analysis; recent retrospective survival data suggest that this classification may be a major confounding variable and should remain an active area of focus in future studies.
While our findings demonstrated a survival difference, the current data are not of sufficient quality to support changes in the treatment paradigm for patients with early-stage mOC. We hope that our genomic data contribute meaningfully to the existing literature and may assist clinicians in risk-stratification when counseling patients who have undergone tumor molecular profiling. However, we emphasize that the evidence remains insufficient to justify treatment decisions based solely on mutational status. Larger-scale prospective studies are needed to validate these associations, though their feasibility is limited by the rarity of this disease. Ongoing and future tumor-agnostic biomarker-driven trials offer more immediate clinical relevance for the mOC treatment landscape.
The broader implementation of TMP for patients with mOC is not without significant challenges. Despite substantial advances in sequencing technology and gradual improvements in accessibility and insurance coverage over the past two decades, molecular profiling remains underutilized, especially outside of major academic centers. In the United States, many initial surgeries are performed by general gynecologists for presumed benign masses, and patients are referred to oncologists only after cancer is found on final pathology. For patients whose original tissue blocks are not available for testing, circulating tumor DNA (ctDNA) could serve as a proxy for any minimal residual disease left after primary surgery. CtDNA-based genomic sequencing has shown potential for predicting recurrence and guiding adjuvant therapy decisions in several solid tumors, including breast, colorectal, and lung cancers (41). Moreover, multiple studies have demonstrated that ctDNA is a viable marker for identifying specific mutations, estimating disease burden at diagnosis, and monitoring treatment response in epithelial ovarian cancer (42–44). Although further validation is needed, ctDNA remains a promising adjunct—and in some cases, a potential alternative—to traditional TMP in mOC and other gynecologic malignancies.
Our study underscores the importance of molecular profiling in mOCs, especially in patients with early-stage disease. We propose that universal TMP should be considered for all cases of mOC—when available and financially accessible—given its potential prognostic value and possibility of informing future shifts in treatment strategies. While large-scale, prospective trials in mOC will continue to pose logistical challenges due to the rarity of the disease, they may become feasible through coordinated multi-institutional collaboration.
Author’s note
This abstract was presented at the Society for Gynecologic Oncology Annual Meeting for Women’s Cancer: March 16-18, 2024, San Diego, California, USA.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by MD Anderson IRB and Human Research Protection Program (HRPP). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because Minimal risk, review of existing medical records.
Author contributions
YZ: Data curation, Formal analysis, Investigation, Software, Visualization, Writing – original draft, Writing – review & editing. SB: Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. PK: Data curation, Investigation, Writing – review & editing. AL: Methodology, Project administration, Writing – review & editing. DG: Writing – review & editing. PR: Writing – review & editing. MF: Conceptualization, Writing – review & editing. AS: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. We thank A. Ninetto (Research Medical Library, The University of Texas MD Anderson Cancer Center, Houston, Texas, USA) for editorial assistance. This research was supported, in part, by the MD Anderson Ovarian Cancer SPORE (P50 CA281701), grants R35 CA209904, American Cancer Society, Rhonda’s Award, Ovarian Cancer Research Alliance, the LeBert Suess Family Endowment for Ovarian Cancer, the Gordon Fund, the Dunwoody Fund, the Blanton-Davis Ovarian Cancer Research Program, Judy’s Mission, and the Frank McGraw Memorial Chair in Cancer Research.
Conflict of interest
DG declares the following competing financial or non-financial interests: consultant for Verastem Oncology; royalties from Elsevier, UpToDate; equity interest in Bristol Myers Squibb, Johnson & Johnson, Procter & Gamble. AS declares the following competing financial or non-financial interests: consultant for Onxeo, Ivlon, Kaida, Starpharma; DSMB for Advenchen and Mural Oncology.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1573801/full#supplementary-material
References
1. Siegel R, Giaquinto AN, and Jemal A. Cancer statistics, 2024. CA Cancer J Clin. (2024) 74:12–49. doi: 10.3322/caac.21820
2. Seidman J, Kurman RJ, and Ronnett BM. Primary and metastatic mucinous adenocarcinomas in the ovaries: incidence in routine practice with a new approach to improve intraoperative diagnosis. Am J Surg Pathol. (2003) 27:985–93. doi: 10.1097/00000478-200307000-00014
3. Peres LC, Cushing-Haugen KL, Köbel M, Harris HR, Berchuk A, Rossing MA, et al. Invasive epithelial ovarian cancer survival by histotype and disease stage. J Natl Cancer Inst. (2019) 111:60–8. doi: 10.1093/jnci/djy071
4. Hess V, A’Hern R, Nasiri N, King DM, Blake PR, Barton DPJ, et al. Mucinous epithelial ovarian cancer: a separate entity requiring specific treatment. J Clin Oncol. (2004) 22:1040–4. doi: 10.1200/JCO.2004.08.078
5. Rechsteiner M, Zimmermann AK, Wild PJ, Caduff R, von Teichman A, Fink D, et al. TP53 mutations are common in all subtypes of epithelial ovarian cancer and occur concomitantly with KRAS mutations in the mucinous type. Exp Mol Pathol. (2013) 95:235–41. doi: 10.1016/j.yexmp.2013.08.004
6. Kato S, Han SY, Liu W, Otsuka K, Shibata H, Kanamaru R, et al. Understanding the function-structure and function-mutation relationships of p53 tumor suppressor protein by high-resolution missense mutation analysis. Proc Natl Acad Sci U S A. (2003) 100:8424–9. doi: 10.1073/pnas.1431692100
7. Strandgren C and Wiman KG. Therapeutic targeting of TP53 nonsense mutations in cancer. Upsala J Med Sci. (2024) 129:10–48101. doi: 10.48101/ujms.v129.10719
8. Vergote I, De Brabanter J, Fyles A, Bertelsen K, Einhorn N, Sevelda P, et al. Prognostic importance of degree of differentiation and cyst rupture in stage I invasive epithelial ovarian carcinoma. Lancet. (9251) 2001:357. doi: 10.1016/S0140-6736(00)03590-X
9. Nasioudis D, Haggerty AF, Giuntoli RL 2nd, Burger RA, Morgan MA, Ko EM, et al. Adjuvant chemotherapy is not associated with a survival benefit for patients with early stage mucinous ovarian carcinoma. Gynecol Oncol. (2019) 154:302–7. doi: 10.1016/j.ygyno.2019.05.009
10. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Ovarian Cancer Including Fallopian Tube Cancer and Primary Peritoneal Cancer Version 2.2023. Available online at: https://www.nccn.org/professionals/physician_gls/pdf/ovarian.pdf (Accessed January 10, 2024).
11. Groen RS, Gershenson DM, and Fader AN. Updates and emerging therapies for rare epithelial ovarian cancers: one size no longer fits all. Gynecol Oncol. (2015) 136:373–83. doi: 10.1016/j.ygyno.2014.11.078
12. Yoshihara M, Emoto R, Kitami K, Iyoshi S, Uno K, Mogi K, et al. A large-scale multi-institutional study evaluating prognostic aspects of positive ascites cytology and effects of therapeutic interventions in epithelial ovarian cancer. Sci Rep. (2021) 11:15154. doi: 10.1038/s41598-021-93718-3
13. Crane EK and Brown J. Early stage mucinous ovarian cancer: a review. Gynecol Oncol. (2018) 149:598–604. doi: 10.1016/j.ygyno.2018.01.035
14. Matsuo K, Rau AR, Machida H, Roman LD, and Wright JD. Intraoperative rupture and chemotherapy use in stage I ovarian cancer. Eur J Obstet Gynecol Reprod Biol. (2023) 284:200–2. doi: 10.1016/j.ejogrb.2023.03.015
15. Gouy S, Saidani M, Maulard A, Bach-Hamba S, Bentivegna E, Leary A, et al. Characteristics and prognosis of stage I ovarian mucinous tumors according to expansile or infiltrative type. Int J Gynecol Cancer. (2018) 28:493–9. doi: 10.1097/IGC.0000000000001202
16. Gorringe KL, Cheasley D, Wakefield MJ, Ryland G, Allan PE, Alsop K, et al. Therapeutic options for mucinous ovarian carcinoma. Gynecol Oncol. (2020) 156:552–60. doi: 10.1016/j.ygyno.2019.12.015
17. Kurnit KC and Frumovitz M. Primary mucinous ovarian cancer: options for surgery and chemotherapy. Int J Gynecol Cancer. (2022) 32:ijgc–2022-003806. doi: 10.1136/ijgc-2022-003806
18. Algera MD, Van de Vijver KK, van Driel WJ, Slangen BF, Lof FC, van der Aa M, et al. Outcomes of patients with early stage mucinous ovarian carcinoma: a Dutch population-based cohort study comparing expansile and infiltrative subtypes. Int J Gynecol Cancer. (2024) 34:722–9. doi: 10.1136/ijgc-2023-004955
19. Hada T, Miyamoto M, Ishibashi H, Matsuura H, Kakimoto S, Iwahashi H, et al. Comparison of clinical behavior between mucinous ovarian carcinoma with infiltrative and expansile invasion and high-grade serous ovarian carcinoma: a retrospective analysis. Diagn Pathol. (2022) 17:12. doi: 10.1186/s13000-022-01195-7
20. Gore ME, Hackshaw A, Brady WE, Penson RT, Zaino RJ, McCluggage WG, et al. Multicentre trial of carboplatin/paclitaxel versus oxaliplatin/capecitabine, each with/without bevacizumab, as first line chemotherapy for patients with mucinous epithelial ovarian cancer (mEOC). J Clin Oncol. (2015) 33:5528. doi: 10.1200/jco.2015.33.15_suppl.5528
21. Schlappe BA, Zhou QC, O’Cearbhaill R, Iasonos A, Soslow RA, Abu-Rustum NR, et al. A descriptive report of outcomes of primary mucinous ovarian cancer patients receiving either an adjuvant gynecologic or gastrointestinal chemotherapy regimen. Int J Gynecol Cancer. (2019) 29:ijgc–2018-000150. doi: 10.1136/ijgc-2018-000150
22. Kurnit KC, Sinno AK, Fellman BM, Varghese A, Stone R, Sood AK, et al. Effects of gastrointestinal-type chemotherapy in women with ovarian mucinous carcinoma. Obstet Gynecol. (2019) 134:1253–9. doi: 10.1097/AOG.0000000000003579
23. Cook JH, Melloni GEM, Gulhan DC, Park PJ, and Haigis KM. The origins and genetic interactions of KRAS mutations are allele-and tissue-specific. Nat Commun. (2021) 12:1808. doi: 10.1038/s41467-021-22125-z
24. Zeissig MN, Ashwood LM, Kondrashova O, and Sutherland KD. Next batter up! Targeting cancers with KRAS-G12D mutations. Trends Cancer. (2023) 9:955–67. doi: 10.1016/j.trecan.2023.07.010
25. Skoulidis F, Li BT, Dy GK, Price TJ, Falchook GS, Wolf J, et al. Sotorasib for lung cancers with KRAS p.G12C mutation. N Engl J Med. (2021) 384:2371–81. doi: 10.1056/NEJMoa2103695
26. Jänne PA, Riely GJ, Gadgeel SM, Heist RS, Ou SHI, Pacheco JM, et al. Adagrasib in non–small-cell lung cancer harboring a KRASG12C mutation. N Engl J Med. (2022) 387:120–31. doi: 10.1056/NEJMoa2204619
27. Strickler JH, Satake H, George TJ, Yaeger R, Hollebecque A, Garrido-Laguna I, et al. Sotorasib in KRAS p. G12C–mutated advanced pancreatic cancer. N Engl J Med. (2023) 388:33–43. doi: 10.1056/NEJMoa2208470
28. Yaeger R, Weiss J, Pelster MS, Spira AI, Barve M, Ou SHI, et al. Adagrasib with or without cetuximab in colorectal cancer with mutated KRAS G12C. ”N Engl J Med. (2023) 388:44–54. doi: 10.1056/NEJMoa2212419
29. Hallin J, Bowcut V, Calinisan A, Briere DM, Hargis L, Engstrom LD, et al. Anti-tumor efficacy of a potent and selective non-covalent KRASG12D inhibitor. Nat Med. (2022) 28:2171–82. doi: 10.1038/s41591-022-02007-7
30. Kemp SB, Cheng N, Markosyan N, Sor R, Kim IK, Hallin J, et al. Efficacy of a small-molecule inhibitor of KrasG12D in immunocompetent models of pancreatic cancer. Cancer Discov. (2023) 13:298–311. doi: 10.1158/2159-8290.CD-22-1066
31. Nagashima T, Inamura K, Nishizono Y, Suzuki A, Tanaka H, Yoshinari T, et al. ASP3082, a First-in-class novel KRAS G12D degrader, exhibits remarkable anti-tumor activity in KRAS G12D mutated cancer models. Eur J Cancer. (2022) 174:S30. doi: 10.1016/S0959-8049(22)00881-4
32. Zhou C, Li W, Song Z, Zhang Y, Zhang Y, Huang D, et al. LBA33 a first-in-human phase I study of a novel KRAS G12D inhibitor HRS-4642 in patients with advanced solid tumors harboring KRAS G12D mutation. Ann Oncol. (2023) 34:S1273. doi: 10.1016/j.annonc.2023.10.025
33. Menard MJ, Chow C, Chen K, Blaj C, Shifrin NT, Courtney H, et al. RMC-9805, a first-in-class, mutant-selective, covalent and orally bioavailable KRASG12D (ON) inhibitor, promotes cancer-associated neoantigen recognition and synergizes with immunotherapy in preclinical models. Cancer Res. (2023) 83:3475. doi: 10.1158/1538-7445.AM2023-3475
34. Zhou C, Li C, Luo L, Li X, Jia K, He N, et al. Anti-tumor efficacy of HRS-4642 and its potential combination with proteasome inhibition in KRAS G12D-mutant cancer. Cancer Cell. (2024) 42:1286–300. doi: 10.1016/j.ccell.2024.06.001
35. Ratner ES, Keane FK, Lindner R, Tassi RA, Paranjape T, Glasgow M, et al. A KRAS variant is a biomarker of poor outcome, platinum chemotherapy resistance and a potential target for therapy in ovarian cancer. Oncogene. (2012) 31:4559–66. doi: 10.1038/onc.2011.539
36. Therachiyil L, Anand A, Azmi A, Bhat A, Korashy HM, and Uddin S. Role of RAS signaling in ovarian cancer. F1000Res. (2022) 11:1253. doi: 10.12688/f1000research.126337.1
37. Mueller JJ, Schlappe BA, Kumar R, Olvera N, Dao F, Abu-Rustum N, et al. Massively parallel sequencing analysis of mucinous ovarian carcinomas: genomic profiling and differential diagnoses. Gynecol Oncol. (2018) 150:127–35. doi: 10.1016/j.ygyno.2018.05.008
38. Meric-Bernstam F, Makker V, Oaknin A, Oh DY, Banerjee S, González-Martín A, et al. Efficacy and safety of trastuzumab deruxtecan in patients with HER2-expressing solid tumors: primary results from the DESTINY-PanTumor02 phase II trial. J Clin Oncol. (2024) 42:47–58. doi: 10.1200/JCO.23.02005
39. Kummar S and Lassen UN. TRK inhibition: a new tumor-agnostic treatment strategy. Target Oncol. (2018) 13:545–56. doi: 10.1007/s11523-018-0590-1
40. Ko HC, Strickland KC, Jaggessarsingh D, Dillard A, Green M, Newburn E, et al. From tissue-specific to tissue-agnostic: HER2 overexpression and the rise of antibody-drug conjugates. Front Oncol. (2025) 15:1565872. doi: 10.3389/fonc.2025.1565872
41. Zhu L, Xu R, Yang L, Shi W, Zhang Y, Liu J, et al. Minimal residual disease (MRD) detection in solid tumors using circulating tumor DNA: a systematic review. Front Genet. (2023) 14:1172108. doi: 10.3389/fgene.2023.1172108
42. Parkinson CA, Gale D, Piskorz AM, Biggs H, Hodgkin C, Addley H, et al. Exploratory analysis of TP53 mutations in circulating tumour DNA as biomarkers of treatment response for patients with relapsed high-grade serous ovarian carcinoma: a retrospective study. PloS Med. (2016) 13:e1002198. doi: 10.1371/journal.pmed.1002198
43. Kim YM, Lee SW, Lee YJ, Lee HY, Lee JE, and Choi EK. Prospective study of the efficacy and utility of TP53 mutations in circulating tumor DNA as a non-invasive biomarker of treatment response monitoring in patients with high-grade serous ovarian carcinoma. J Gynecol Oncol. (2019) 30:e32. doi: 10.3802/jgo.2019.30.e32
44. Vanderstichele A, Busschaert P, Smeets D, Landolfo C, Van Nieuwenhuysen EV, Leunen K, et al. Chromosomal instability in cell-free DNA as a highly specific biomarker for detection of ovarian cancer in women with adnexal masses. Clin Cancer Res. (2017) 23:2223–31. doi: 10.1158/1078-0432.CCR-16-1078
Keywords: mucinous adenocarcinoma, ovarian cancer, TP53, molecular sequencing, NGS, genomic sequencing, tumor mutation
Citation: Zhang Y, Barkdull S, Kontoyiannis PD, Legarreta AF, Gershenson DM, Ramalingam P, Frumovitz MM and Sood AK (2025) TP53 and KRAS co-mutations are associated with worse outcomes in mucinous ovarian carcinomas. Front. Oncol. 15:1573801. doi: 10.3389/fonc.2025.1573801
Received: 09 February 2025; Accepted: 07 July 2025;
Published: 14 August 2025.
Edited by:
Caiyue Li, Louisiana State University, United StatesReviewed by:
Beatrice D’Orsi, National Research Council (CNR), ItalyCheng-Yao Chiang, The Ohio State University, United States
Copyright © 2025 Zhang, Barkdull, Kontoyiannis, Legarreta, Gershenson, Ramalingam, Frumovitz and Sood. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anil K. Sood, YXNvb2RAbWRhbmRlcnNvbi5vcmc=
 Yingao Zhang
Yingao Zhang Savannah Barkdull
Savannah Barkdull Panayiotis D. Kontoyiannis
Panayiotis D. Kontoyiannis Alejandra Flores Legarreta3
Alejandra Flores Legarreta3 Michael M. Frumovitz
Michael M. Frumovitz Anil K. Sood
Anil K. Sood