- 1Department of Oncology, Chendu Second People’s Hospital, Chengdu, China
- 2Tha Academy of Chinese Health Risks, West China Hospital, Sichuan University, Chengdu, China
A 51-year-old man with perianal Bowen’s diseases, treated with tislelizumab and capecitabine chemotherapy, the tumor was significantly reduced and Improved quality of life.
Background
Primary cutaneous malignancies are among the most common cancer types globally, with Bowen’s disease having an age-standardized incidence rate of 5.8% (1). Bowen’s disease, also known as squamous cell carcinoma in situ of the skin, typically affects the epidermal layer without often invading deeper skin tissues. Characteristically, it presents as a single, well-demarcated, irregular red patch in sun-exposed areas such as the head, neck, and extremities (2). However, in this particular case, the lesion occurred peri-anally, an area typically shielded from sunlight, and it exhibited an exceedingly rare, massive, cauliflower-like growth pattern.
Treatment
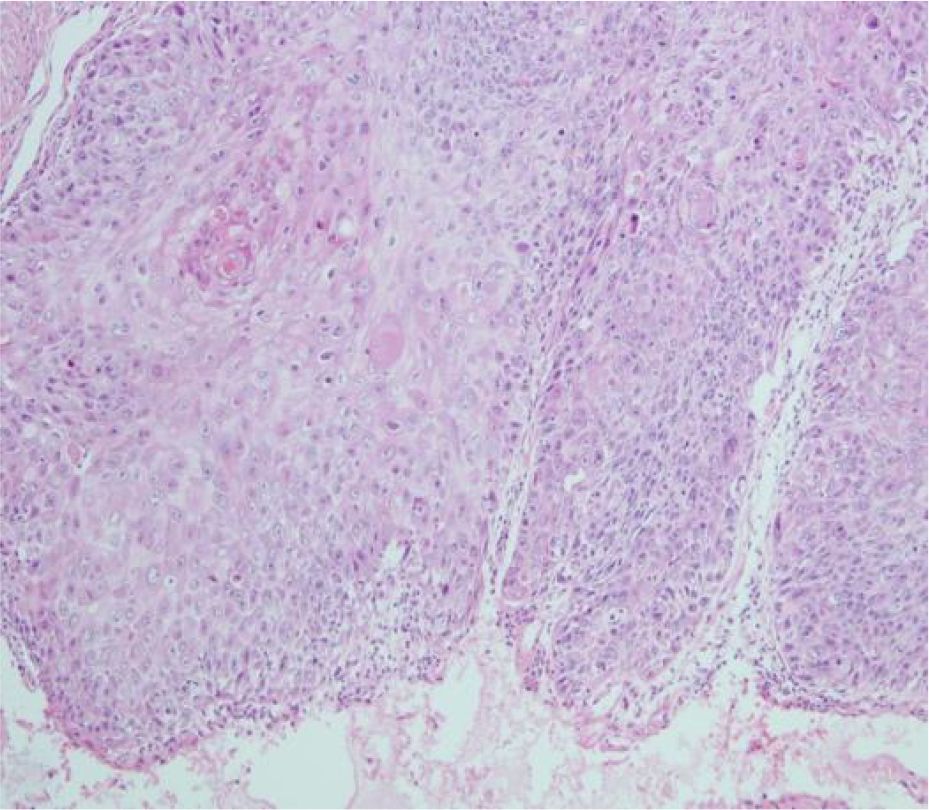
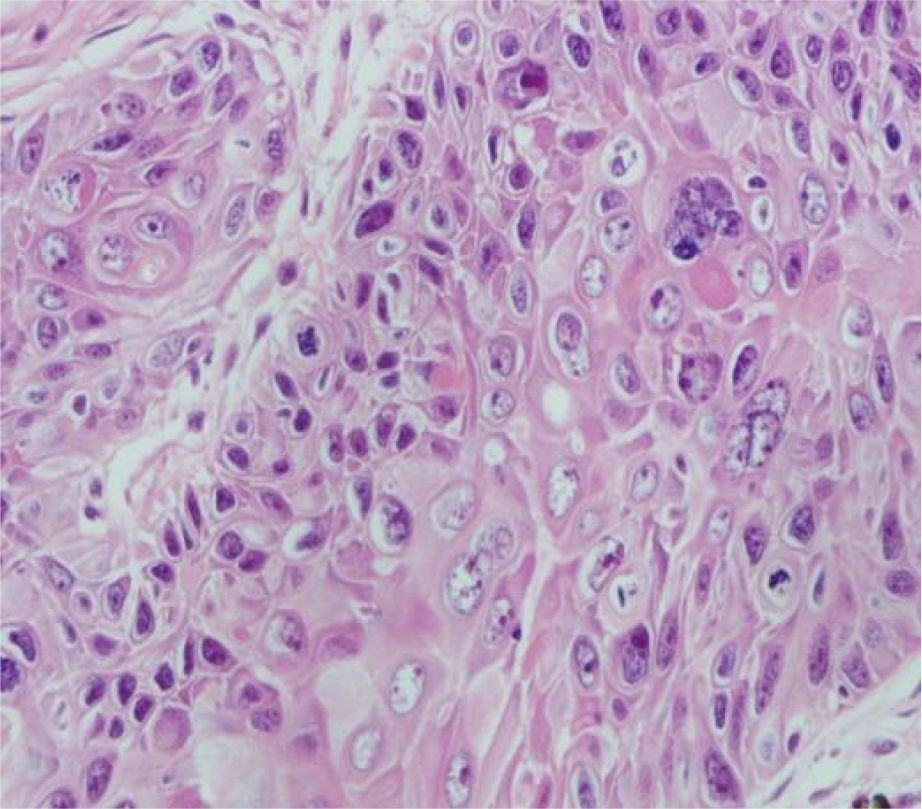
A 51-year-old middle-aged man inadvertently noticed a soybean-sized swelling on the perianal skin, without obvious symptoms such as itching, pain, or bleeding and discharge. Three months later, the swelling gradually increased in size, accompanied by itching and discharge (Figure 1). A pathological biopsy revealed “perianal” Bowen’s disease (Figures 2, 3), with suspected focal infiltration. After consultation with a surgical team, it was determined that the patient’s perianal tumor had grown significantly, involving the scrotum and perineum, with poor mobility, making radical resection impossible. Following departmental discussion, the patient was treated with tislelizumab and capecitabine chemotherapy, along with topical application of fluorouracil ointment on the tumor. After two cycles of treatment, the tumor was significantly reduced, and the third cycle of treatment was continued (Figure 4). However, the patient did not proceed with the fourth cycle of treatment due to personal reasons. Subsequent follow-ups have shown that the patient has survived for two years since then.
Discussion
The exact etiology of Bowen’s disease remains unclear, but research has demonstrated that chronic exposure to ultraviolet radiation, arsenic exposure, various strains of HPV, chemical carcinogens, immunosuppression, and chronic irritation are considered to be some of the risk factors contributing to the development of Bowen’s disease (3). In this case, the patient experienced rapid and substantial growth of the lesion, which was also attributed to long-term scratching due to perianal itching, confirming that prolonged chronic irritation is one of the significant risk factors for the development of Bowen’s disease.
This is the first instance of treating Bowen’s disease with a combination of immune checkpoint inhibitors and 5-fluorouracil. The patient was a 51-year-old single man without employment or a stable income, so his treatment budget was tightly constrained. The tumor had grown to an exceptionally large size, infiltrating the scrotum, perianal area, and perineum, exhibiting poor mobility. Therefore, radical resection was impossible and any local modality was expected to yield only limited benefit. After multidisciplinary discussion, systemic therapy was chosen.Guidelines list the recommended options for inoperable Bowen’s disease in the following order: photodynamic therapy (PDT, grade A), topical fluorouracil, and cryotherapy (4). Although PDT is the preferred first-line modality, its efficacy is constrained by factors such as photosensitizer type, limited depth of cytotoxic effect, tumor hypoxia, and technical complexity; moreover, the shallow tissue penetration of light markedly reduces its activity against deeper tumor components (5).Numerous studies and guidelines have affirmed the role of 5-fluorouracil in squamous cell carcinoma (6, 7). The programmed cell death protein 1 (PD-1) inhibitors are monoclonal antibodies that block the interaction between PD-1 and its ligands, thereby restoring the immune system’s ability to attack tumor cells. They have become a cornerstone of immunotherapy for multiple advanced solid and hematologic malignancies (8). PD-1 inhibitor cemiplimab has been approved as a first-line treatment for patients with metastatic or locally advanced cutaneous squamous cell carcinoma (cSCC) (9), but considering the accessibility and cost of the medication, we ultimately opted for another PD-1 inhibitor, tislelizumab, in combination with 5-fluorouracil for treatment. Historical data indicate that topical fluorouracil is less effective than surgery and slightly inferior to photodynamic therapy, while robust evidence for immunotherapy in Bowen’s disease is still lacking. Nevertheless, for extensive lesions it represents a novel strategy worth investigating and may signal a future direction. In this case, evaluation after two cycles revealed marked tumor shrinkage, an outcome that is both encouraging and promising.
Conclusion
In the era of immunotherapy, the combination of PD-1 inhibitors with 5-fluorouracil has proven effective in treating patients with Bowen’s disease who are not suitable candidates for local therapies, offering a systemic treatment approach for future management of patients with extensive Bowen’s disease.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Chengdu Second People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XX: Formal Analysis, Writing – original draft. QC: Writing – original draft, Data curation. JZ: Writing – review & editing, Visualization. XP: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kwon SH, Choi S, Kim JS, Kim SS, Jue MS, Seo SH, et al. Incidence and survival rates of primary cutaneous Malignancies in Korea, 1999-2019: A nationwide population-based study. J Dermatol. (2024) 51(4):532–8. doi: 10.1111/1346-8138.17118
2. Manivannan L, Swaminathan T, Rengarajan M, and Vadivelu S. A case series of bowen’s disease in a tertiary care centre in South India IJCED. IP Indian Journal of Clinical and Experimental Dermatology. (2024) 10(3):340–7. doi: 10.18231/j.ijced.2024.060
3. Sebaratnam D. Rook’s textbook of dermatology, 4 volume set, 10th edition. Edited by christopher E.M. Griffiths, jonathan barker, tanya O. Bleiker, walayat hussain, rosalind C. Simpson brit J dermatol. Brit J Dermatol. (2024). doi: 10.1093/bjd/ljae320
4. Sharma A, Birnie AJ, Bordea C, Seau Tak C, Jasmine M, Colin A, et al. British Association of Dermatologists guidelines for the management of people with cutaneous squamous cell carcinoma in situ (Bowen disease) 2022. Brit J Dermatol. (2023) 188(2):186–194. doi: 10.1093/bjd/ljac042
5. Gunaydin G, Gedik ME, and Ayan S. Photodynamic therapy-current limitations and novel approaches. Front Chem. (2021) 9:691697. doi: 10.3389/fchem.2021.691697
6. Saeed A, Hameem ZU, Modi D, Park R, and Saeed A. Cutaneous paraneoplastic syndrome associated with anal squamous cell carcinoma: a rare presentation of an uncommon cancer. Curr Oncol. (2020) 27:e433–5. doi: 10.3747/co.27.6557
7. Gil S, Yébenes M, Luelmo J, Alsina M, and Sabés M. A comparative study of the effectiveness of cisplatin and 5-fluorouracil on cutaneous squamous human carcinoma cell line: Potential chemotherapy alternative to surgery. Dermatol Ther. (2016) 29(5):341–4. doi: 10.1111/dth.12373
8. Alsaab HO, Sau S, Alzhrani R, Tatiparti K, Bhise K, Kashaw SK, et al. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. (2017) 8:561. doi: 10.3389/fphar.2017.00561
Keywords: Bowen’s disease, PD-1 inhibitor, chemotherapy, 5-fluorouracil, cutaneous squamous cell carcinoma
Citation: Xie X, Chen Q, Zhang J and Peng X (2025) Case Report: Bowen’s disease treated with PD-1 inhibitor and chemotherapy. Front. Oncol. 15:1654431. doi: 10.3389/fonc.2025.1654431
Received: 26 June 2025; Accepted: 08 September 2025;
Published: 25 September 2025.
Edited by:
Simona Kranjc Brezar, Institute of Oncology Ljubljana, SloveniaReviewed by:
Maria Guadalupe Moreno Treviño, University of Monterrey, MexicoBing Yang, Krirk University, Thailand
Copyright © 2025 Xie, Chen, Zhang and Peng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaodong Peng, eGRwZW5nMTk3M0AxMjYuY29t
†These authors have contributed equally to this work
 Xiaohui Xie1†
Xiaohui Xie1† Xiaodong Peng
Xiaodong Peng