- 1Pediatric Cardiac Critical Care Division, Hadassah University Medical Center, Jerusalem, Israel
- 2Division of Pediatric Critical Care Medicine, Children's Hospital of Richmond at VCU, Richmond, VA, United States
- 3Pediatric Critical Care Medicine, NY Presbyterian Hospital–Weill Cornell Medicine, New York, NY, United States
Clinically significant bleeding complicates up to 20% of admissions to the intensive care unit in adults and is associated with severe physiologic derangements, requirement for significant interventions and worse outcome. There is a paucity of published data on bleeding in critically ill children. In this manuscript, we will provide an overview of the epidemiology and characteristics of bleeding in critically ill children, address the association between bleeding and clinical outcomes, describe the current definitions of bleeding and their respective limitations, and finally provide an overview of current knowledge gaps and suggested areas for future research.
Introduction
Clinically relevant bleeding can commonly affect critically ill patients, either as an admission diagnosis or as a complication of underlying critical disease. In one large, prospective cohort of critically ill adults, approximately one-fifth had significant bleeding during their admission to the ICU (1). One-tenth of critically ill children were reported to be bleeding on admission in a retrospective study in the PICU. In addition, a similar number developed clinically relevant bleeding during their stay (2).
Physiologically, clinically relevant bleeding (CRB) may lead to reduced oxygen delivery in two ways: (1) decreased blood oxygen content due to lower red blood cell mass and (2) decreased cardiac output due to hypovolemia. Poorer clinical outcomes have been associated with bleeding in subpopulations of critically ill patients. These include increased mortality in bleeding adults with acute coronary syndrome (3) and in those following bone marrow transplant (4). Adults who undergo cardiac surgery and have significant post-operative bleeding are more likely to be mechanically ventilated longer and stay longer periods in the ICU (5). Likewise, poorer clinical outcomes have been observed in critically ill children who bleed including more exposure to vasoactive medications and longer lengths of stay in both the ICU and the hospital as compared to those who do not bleed (2). Nevertheless, until recently, there was no published definition accurately describing the severity of bleeding in critically ill children. We lack large epidemiologic studies documenting prevalence of CRB, as well as risk factors and effective prevention.
In this review, we will provide an overview of the existing evidence regarding the epidemiology and characteristics of bleeding in critically ill children, describe the association between bleeding and clinical outcomes, discuss the current definitions of bleeding and their respective limitations, and, in doing so, provide an overview of current knowledge gaps and suggestions for areas of future research.
Epidemiology of Bleeding in The General PICU Population: Incidence, Identified Risk Factors, and Outcome
Despite the potential morbidity of CRB for critically ill children, less than a handful of studies depict the epidemiology and potential risk factors of CRB in the general Pediatric Intensive Care Unit (PICU) population. Current epidemiologic studies are typically limited to certain subsets of critically ill patients, such as those undergoing cardiac repair with cardiopulmonary bypass (6–8), or to specific anatomical locations of bleeding, such as chest tubes (6–8) or the gastrointestinal tract (9–11). None of the published studies to date used a validated pediatric definition of CRB and all of the definitions varied.
In a single-center retrospective cohort study conducted over 6 months in a tertiary care children's hospital, Moorehead et al. reported CRB occurring in 9% (19/214) of their patients (12). The authors defined CRB in relation to hematoma formation, the development of hemorrhagic shock, a defined drop in hemoglobin concentration, the cessation of anticoagulant medication due to bleeding CRB, or fluid resuscitation with either crystalloid or red blood cell (RBC) transfusions to control bleeding. Thrombocytopenia (platelet count < 100 × 109/L), mechanical ventilation, the use of either antibiotic or antacid medications, and cardiac surgery were patient factors that were each associated with increased risk of CRB. The study was limited by significant disagreement between those reviewing the charts as to which patients met their defined criteria for CRB (kappa statistic = 0.26).
To follow up on this study and account for its limitations, Moorehead et al. applied their definition of CRB to a prospective cohort of critically ill children (13). In particular, they reported on the associations between laboratory values and CRB. Two hundred and thirty-four children were enrolled and a similar incidence of CRB was reported. There was a suggestion of decreasing platelet count being associated with increased bleeding. However, the association was not significant when accounting for confounders. Irregularities in other measures of coagulation, such as international normalized ratio (INR) and activated partial thromboplastin time (aPTT), were not associated with increased bleeding. The study was limited by incomplete laboratory data for each patient enrolled.
In a cohort study in a single-center PICU, White et al. reported CRB in 9% (37/405) of the children admitted to the PICU (14). They modified a previously developed tool from the International Society on Thrombosis and Hemostasis (ISTH) and characterized bleeding as either major, clinically relevant non-major, or minor. The majority of children, ~80%, had only one bleeding event. Children receiving invasive mechanical ventilation or stress ulcer prophylaxis were more likely to have CRB. Though mortality was no different, those with CRB had longer lengths of stay both in the ICU and the hospital as a whole.
Pinto et al. used the same bleeding tool (known as the ISTH-BAT) to assess the epidemiology of CRB in critically ill adolescents with increased risk for venous thromboembolism (VTE) (15). The frequency of CRB was 30% (95% CI, 20–40%). The high incidence of CRB reported in this study probably reflects the inclusion of bleeding events occurring on the day of admission that were excluded from the previous studies discussed. As a result, the proportion of surgical and trauma patients in this study was also higher. CRB was more commonly seen in adolescents with VTE, likely reflecting increased risk of bleeding due to anticoagulation. Younger age, higher predicted risk of mortality score, and admission for trauma or surgery were also associated with increased risk for CRB.
In conclusion, there is limited data on the epidemiology of CRB in the general PICU population. Reported incidence of bleeding in single center studies was 9–30%, depending on inclusion criteria and based on different bleeding assessment scales. Risk factors identified were admission due to cardiac surgery or trauma, young age, mechanical ventilation, receipt of antacid medications and thrombocytopenia. Patients with CRB had longer ventilation days, increased requirement for vasoactive drugs and blood products, and longer PICU length of stay.
Bleeding in Selected High Risk Populations of Critically Ill Infants and Children: Characteristics and Etiologies
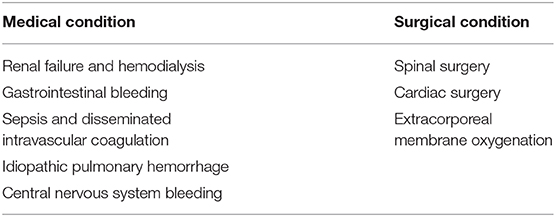
Several subsets of critically ill children may be particularly prone to bleeding complications. ICU diagnoses associated with increased frequency of bleeding include trauma, cardiac surgery, orthopedic surgery, hematologic malignancies, sepsis, respiratory failure (requiring invasive mechanical ventilation), renal failure requiring renal replacement therapy, and extracorporeal membrane oxygenation (ECMO) (16, 17).
As seen in epidemiologic studies, younger age is associated with an increased risk of bleeding. This may be secondary to the characteristics of the normal development of the coagulation system in infancy. Prior to 6 months of age, infants have lower concentrations of vitamin K–dependent pro-coagulant clotting factors and reduced thrombin potential (18), ~70% of the levels as compared to adults. Prothrombin levels are also significantly lower as compared with that in adults (19). It is unclear whether these lower levels are actually associated with more episodes of CRB.
In addition to patient characteristics, there are several physiologic derangements that occur during critical illness that may worsen bleeding. These include hypothermia, acidosis, excessive fibrinolysis, and consumption of coagulation factors and platelets (20). The activity of coagulation factors, as well as necessary enzymes, are inhibited during these physiologic states (21).
We will further discuss selected groups of PICU patients who may be particularly prone to medical and surgical CRB (see Table 1).
Medical Bleeding
Renal Failure and Hemodialysis
Acute kidney injury (AKI) is a common complication of critical illness, affecting almost 30% of the children admitted to pediatric intensive care units (22). Many of these patients develop significant enough AKI to require dialysis, often secondary to fluid overload. In prospective studies in adults, bleeding has been reported in 14–50% of patients with dialysis-dependent AKI, and is described as a major risk factor for mortality (23, 24). Similar to previously mentioned populations, there is very little published data concerning dialysis-dependent AKI and bleeding in the pediatric population.
Kreuzer et al. published a retrospective study of bleeding in nearly 200 children with dialysis-dependent acute kidney injury (25). Slightly over a quarter of the children had bleeding events with 62% of the episodes considered life-threatening. Several factors were independently associated with a higher risk of bleeding including the underlying primary disease leading to AKI, presence of multiorgan dysfunction syndrome (MODS), recent surgery or bleeding prior to the onset of AKI, and hemodialysis or continuous veno-venous hemofiltration (as compared to peritoneal dialysis). In addition, the presence of bleeding was independently associated with mortality in this patient population.
Patients with uremia may be more prone to bleed due to several factors including platelet dysfunction, vitamin K deficiency, and/or slower clearance of unfractionated or low molecular weight heparin which is usually given during dialysis (26). Children with dialysis-dependent AKI are an understudied population in hemostatic research.
Upper Gastrointestinal Bleeding
Although perceived as a prevalent complication in the PICU, there is limited data on the incidence, risk factors and outcome of upper gastrointestinal bleeding in critically ill children. In a single-center prospective study, Chaibou et al. reported upper GI bleeding in 10% (103/1006) of their cohort, with only two percent (16/1006) considered CRB (9). CRB was adjudicated by three authors and had to be associated with significant hemoglobin drop, RBC transfusion, hypotension, development of MODS, surgery, or death. Three independent risk factors for clinically relevant upper GI bleeding were respiratory failure, coagulopathy, and pediatric risk of mortality score >10.
In a more recently published retrospective study, Sahin et al. reviewed records of 136 eligible children consecutively admitted to their tertiary care PICU. The overall incidence of upper GI bleeding was 15%. However, the study was limited by small sample size in that only one child developed what was considered significant bleeding. Approximately 30% of the children who received antacid prophylaxis developed any upper GI bleeding. Mechanical ventilation, trauma, coagulopathy, thrombocytopenia, higher severity score at admission, renal and hepatic failure, hypotension, heart failure, and arrhythmia were found to be associated with the development of any upper GI bleeding (27).
Sepsis and Disseminated Intravascular Coagulation (DIC)
Sepsis is commonly associated with the development of thrombocytopenia, hypofibrinogenemia, and prolongation of prothrombin time (28) which may manifest as multisite bleeding including petechiae, hematomas, and pulmonary hemorrhage. However, sepsis can also trigger the extrinsic coagulation cascade and result in microthrombi (29). In a recently published small cohort of children with septic shock, the incidence of DIC was estimated to be 42–66% (depending on the definition of DIC applied) (30). Though the presence of DIC in children with septic shock has been associated with higher mortality (31), the incidence of bleeding vs. clotting with DIC in these children is not clear. The incidence of bleeding and thrombotic complications in one cohort of Thai children with gram negative sepsis and DIC was 59 and 20%, respectively (32).
Idiopathic Pulmonary Hemorrhage (IPH)
Bleeding into the lower respiratory tract can occur acutely (diffuse alveolar hemorrhage) or more chronically (idiopathic pulmonary hemosiderosis). IPH is a diagnosis of exclusion and other causes, such as gastrointestinal bleeding, cows' milk allergy, cystic fibrosis, or vasculitis must be excluded. The incidence of both acute and chronic IPH is rare. In a 10-years retrospective study of infants at Boston Children's Hospital, only 157 cases were identified (33). Those infants most commonly had associated congenital heart disease, chronic lung disease of prematurity, congenital or acquired lung disorders, or congenital or acquired coagulopathies.
Central Nervous System (CNS) Bleeding
The etiologies of bleeding into the central nervous system of children is varied and includes trauma (both accidental and non-accidental), prematurity, underlying congenital or acquired coagulopathies, idiopathic thrombocytopenia purpura, rupture of arteriovenous aneurysms, or hemorrhage into CNS tumors. Given the diverse pathologies, the incidence of and risk factors for CNS bleeding in pediatrics varies.
Surgical Bleeding
Pediatric Spinal Surgery
Children undergoing spinal surgery, most often correction of scoliosis, are at high risk of bleeding given the length of surgery and the surgical technique required (involving bone dissection and possible disruption of vertebral blood vessels) (34). It is not uncommon for children to lose their entire circulating blood volume. In a large database analysis of blood utilization during spinal surgery from 2000 to 2009, nearly one-third of children required RBC transfusion (35). Survey studies have suggested that the rate of massive bleeding has decreased over time (36), though these studies may be confounded by response bias. The use of antifbrinolytics during surgery (such as tranexamic acid or aminocaproic acid) may have driven the trend of decreased bleeding and decreased post-operative blood product exposure in children undergoing spinal repair (37).
Cardiac Surgery
Children undergoing cardiac repair are also at significant risk of perioperative and post-operative bleeding. Several pre-operative factors may contribute to the bleeding risk. These repairs are often performed during the first year of life. At baseline, infants with congenital heart disease may have lower levels of clotting factors (38). Additionally, cyanotic heart disease has been associated with thrombocytopenia and platelet dysfunction (39–41). Intra-operative blood loss may be pronounced due to coagulopathy induced by the cardiopulmonary bypass circuit, as well as induced hypothermia, use of high dose anticoagulation, and hemodilution (42–47).
Post-operative bleeding is a common complication in pediatric patients undergoing cardiopulmonary bypass (CPB) and is associated with increased morbidity and mortality (46–48). The receipt of post-operative blood products is independently associated with longer lengths of mechanical ventilation and length of PICU stay (49). Post-operative bleeding may be predicted by several factors including thrombocytopenia and hypofibrinogenemia (6, 8).
The Network for the Advancement of Patient Blood Management, Haemostasis, and Thrombosis (NATA) recently published guidelines to minimize blood product exposure in these vulnerable children (50). Their recommendations include the diagnosis and treatment of peri-operative anemia, prophylactic use of either tranexamic acid or aminocaproic acid in the operating room, priming of the cardiopulmonary bypass pump with colloid (as opposed to crystalloid), use of modified ultrafiltration and cell salvage during bypass, and the development of institution-specific transfusion algorithms.
Outside of the post-operative period, critically ill pediatric patients with heart disease can also experience CRB. Patients receiving any form of anti-coagulation (e.g., unfractionated heparin [UFH], low molecular weight heparin [LMWH], and warfarin) are at risk for bleeding secondary to decreased thrombin generation. Acquired von Willebrand disease (vWD) should be considered in patients with excessive mucosal bleeding and the presence of a vascular lesion that creates high shear stress, such as aortic stenosis or a left ventricular assist device (VAD). Definitive treatment of acquired vWD is the correction of the underlying cardiac abnormality, but this is not always possible. Alternatively, treatment with a von Willebrand factor (vWF) containing replacement product can be considered (51).
Extracorporeal Membrane Oxygenation (ECMO)
ECMO may be used to rescue children with profound respiratory and/or heart failure and its use in pediatrics is increasing (52). Like CPB, ECMO is associated with bleeding and is multifactorial secondary to hemodilution, circuit induced coagulopathy, and platelet dysfunction, among other causes. Bleeding and thrombosis, including intracranial hemorrhage and stroke, are frequent and challenging complications in the management of pediatric ECMO patients and associated with increased risk for mortality (53–55). Dalton et al. conducted the first multicenter prospective observational study of children on ECMO examining the incidence, risk factors and associated outcomes of bleeding and clotting (56). Bleeding complications were defined as those requiring RBC transfusion and those occurring in the intracranial space. In a cohort of 514 children followed over 28 days, the incidence of bleeding was 70% (16% of which were intracranial) and the incidence of thrombosis was 38%. Age, indication for ECMO, organ failure at the time of ECMO initiation, and clinical site were all independent predictors of bleeding. Two of three discharge functional status scales were worse in patients who experienced bleeding in comparison to those who did not.
We conducted a secondary analysis of this cohort to evaluate the association between quantifiable bleeding (as measured from chest tubes) and clinical outcomes in children supported by ECMO (57). Over half of the patients had bleeding documented from the chest tube. The median amount of bleeding from the entire population over the course of ECMO was slightly over 120 mL/kg [interquartile range 47–319 mL/kg]. A “dose-dependent” response was observed in the independent association between amount of bleeding and mortality, as well as PICU length of stay. Whereas, some coagulation measures, such as fibrinogen level, were independently associated with chest tube bleeding, other measures, such as platelet count, were not.
Bleeding Scales Applicable to Critically Ill Children—Where are We Today?
As we portrayed thus far, bleeding represents a common complication in the critically ill child, with significant morbidity. In addition, the interventions used to treat CRB, such as blood product, medication administration, and/or surgical procedures, may also be associated with worsened outcomes. Research is needed to guide the clinician as to the correct situations when interventions are needed to treat CRB. However, a standardized definition is needed to conduct these studies.
There are certainly common elements within many of the currently published definitions of bleeding. Definitions often include the amount and site of bleeding (58–61), physiologic or laboratory effects of bleeding (60, 62) and the need for transfusion or other medical intervention to treat the bleeding (59–62). The latter criteria, the need for transfusion or intervention, can add significant variability to the measurement of bleeding incidence as these measures are subjective and may be based on clinician preference. Most definitions have been developed to be specifically applicable to certain patient populations including those with cancer (58, 59, 62), receiving anticoagulation (60) or with inherited bleeding disorders (61). These do not address the specific risk factors for and characteristics of bleeding in critically ill children (e.g., bleeding from an endotracheal tube). Until quite recently, the HEmorrhage MEasurement (HEME) score was the only diagnostic criteria developed to evaluate CRB in critically ill patients (1) and included specific physiologic (such as heart rate) and laboratory (such as hemoglobin) measures. However, it was developed for critically ill adults, and therefore cannot be applied to critically ill children due to different age specific norms.
We conducted a systematic review in order to identify current bleeding scales and their validity to assess bleeding in critically ill children (63). Studies were included if they contained a bleeding score, bleeding measurement tool or clinical measurement of hemorrhage. Of the 18 studies identified, only two described critically ill children. As with previously mentioned scales in adults, the majority of identified bleeding scales included the need for medical or surgical intervention as a part of the definition. In addition, the majority of scales did not report measures of reliability or validation to clinical outcomes. This review highlighted the need for the development of an objective, validated, operational definition that included characteristics of bleeding particular to critically ill children. The National Institute of Health, National Heart, Lung and Blood Institute (NHLBI) and the Biomedical Excellence for Safer Transfusion (BEST) Collaborative recognized this need as well and identified the development of a validated bleeding measurement scale in critically ill children (as well as other vulnerable patient populations) as a high priority (64, 65).
As the next step in the development of a definition of bleeding in critically ill children, we performed a web-based international survey to qualify the clinical significance of different bleeding characteristics in critically ill children (66). We identified four domains of bleeding (site, amount, severity, and progression) and asked pediatric intensivists what they considered clinically relevant vs. irrelevant. Two hundred and twenty-five pediatric intensivists from 16 countries responded. They identified the following characteristics as clinically relevant: bleeding in critical locations (such as the pericardium, pleural space, central nervous system, and lungs), bleeding requiring interventions (such as chest tube insertion or the administration of blood products), bleeding leading to physiologic repercussions (such as organ failure or hypoperfusion); and bleeding lasting more than 6 h. In particular, quantifiable bleeding of more than 5 mL/kg/h for more than 1 h was frequently considered clinically relevant. In addition, providers identified several specific clinical scenarios of bleeding as being clinically irrelevant, including streaks of blood in the endotracheal tube and non-coalescing petechiae.
Based on these identified and characterized bleeding elements, we conducted a Delphi consensus process with over 30 multidisciplinary experts in bleeding and hemostasis in order to design a standard definition for CRB in critically ill children (67). The results of the process, the Bleeding Assessment Scale in Critically Ill Children (BASIC), are presented in Table 2. The experts divided bleeding into severe, moderate and minimal and described clinical characteristics of each category. Qualifiers were made to describe fatal and progressive bleeding. In order to incorporate clinically relevant physiologic consequences of bleeding into the scale, the experts used organ dysfunction as measured by the Pediatric Logistic Organ Dysfunction (PELOD)-2 score (68). Given the PELOD-2 scale includes physiologic derangements within nearly every system, the experts chose not to include each and every possible location of bleeding within the definition. Instead, they only included three sites (intraspinal, intraorbital and intraarticular) that though rare, would not be reflected in the PELOD-2 scoring system. In addition, changes in heart rate, blood pressure and hemoglobin were described by proportional differences, as opposed to whole numbers, in order to account for age-related standards. Lastly, the experts chose to exclude clinical interventions within the definition, based on both the subjectivity of clinical decision-making, as well as retaining the ability of the use of the definition in studies to assess the value of such interventions.
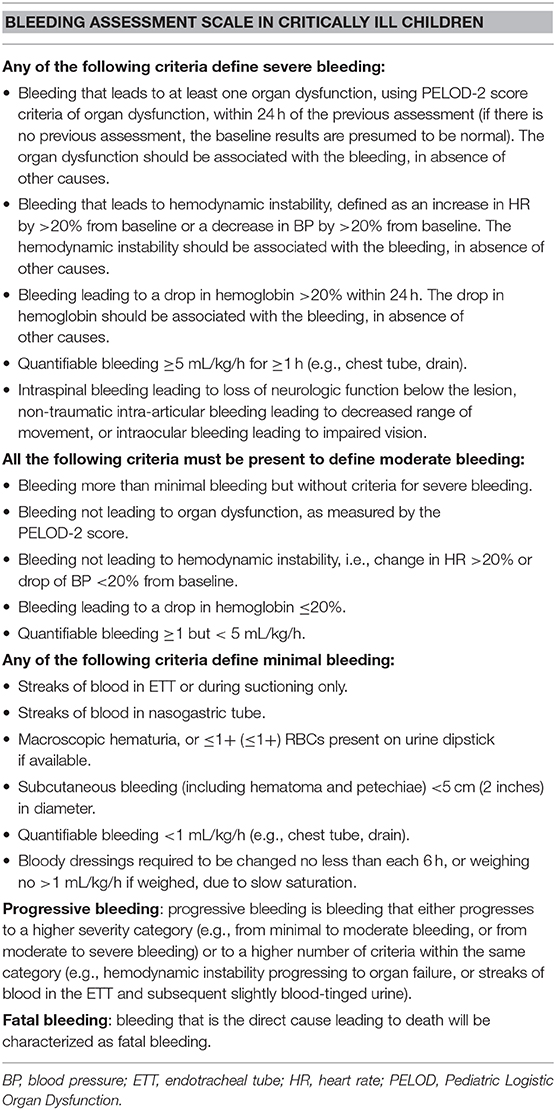
Table 2. Consensus definition of clinically relevant bleeding (59).
The BASIC definition underwent preliminary internal validity testing as it was applied to 40 critically ill children with 46 distinct bleeding episodes in a single center (67). When comparing the application of the definition to describe the bleeding episodes by two independent observers, there was substantial inter-rater reliability [kappa statistic 0.74 (95% CI, 0.6–0.9)]. The BASIC definition represents the first diagnostic criteria for bleeding derived via expert consensus applicable to critically ill children. It must be further validated, both in larger patient cohorts and in relation to clinical outcomes, in order to be applied in clinical trials.
Conclusions and Future Directions
Pediatric intensivists will encounter bleeding on a relatively frequent basis in their patient population. In critically ill children, bleeding has been associated with significant morbidity and mortality. There is paucity of data on CRB acquired in PICU patients, stemming in part from the lack of a standardized pediatric bleeding score. The BASIC definition should be validated to clinical outcomes. This will facilitate the accurate identification of subpopulations of critically ill children at risk for CRB. The data generated from large scale epidemiologic studies can be used to development a numerical bleeding score which includes patient characteristics and laboratory values. This can be used, in turn, to plan monitoring strategies and prevention measures. A standardized and well-validated score can be used to define inclusion criteria or outcome and will aid in the development of large multicenter clinical trials to test current hemostatic interventions, such as platelet or plasma transfusion thresholds in children who are prone to bleed, such as those treated with anticoagulation, those in DIC or supported on ECMO and test new and investigational therapies, such as anti-fibrinolytics, factors replacements, use of whole blood and cold stored platelets.
Author Contributions
AA, OK, and MN conceived of the format of the review and contributed to its writing. All authors reviewed the manuscript and edited it prior to submission.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Arnold DM, Donahoe L, Clarke FJ, Tkaczyk AJ, Heels-Ansdell D, Zytaruk N, et al. Bleeding during critical illness: a prospective cohort study using a new measurement tool. Clin Invest Med. (2007) 30:E93–102. doi: 10.25011/cim.v30i2.985
2. White LJ, Fredericks R, Mannarino CN, Janofsky S, Faustino EVS. Epidemiology of bleeding in critically ill children. J Pediatr. (2017) 184:114–9. doi: 10.1016/j.jpeds.2017.01.026
3. Eikelboom JW, Mehta SR, Anand SS, Xie C, Fox KAA, Yusuf S. Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation. (2006) 114:774–82. doi: 10.1161/CIRCULATIONAHA.106.612812
4. Nevo S, Swan V, Enger C, Wojno KJ, Bitton R, Shabooti M, et al. Acute bleeding after bone marrow transplantation (BMT)-incidence and effect on survival. A quantitative analysis in 1,402 patients. Blood. (1998) 91:1469–77. doi: 10.1182/blood.V91.4.1469
5. Christensen MC, Krapf S, Kempel A, von Heymann C. Costs of excessive postoperative hemorrhage in cardiac surgery. J Thorac Cardiovasc Surg. (2009) 138:687–93. doi: 10.1016/j.jtcvs.2009.02.021
6. Williams GD, Bratton SL, Riley EC, Ramamoorthy C. Coagulation tests during cardiopulmonary bypass correlate with blood loss in children undergoing cardiac surgery. J Cardiothorac Vasc Anesth. (1999) 13:398–404. doi: 10.1016/S1053-0770(99)90210-0
7. Williams GD, Bratton SL, Ramamoorthy C. Factors associated with blood loss and blood product transfusions: a multivariate analysis in children after open-heart surgery. Anesth Analg. (1999) 89:57–64. doi: 10.1213/00000539-199907000-00011
8. Miller BE, Mochizuki T, Levy JH, Bailey JM, Tosone SR, Tam VK, et al. Predicting and treating coagulopathies after cardiopulmonary bypass in children. Anesth Analg. (1997) 85:1196–202. doi: 10.1213/00000539-199712000-00003
9. Chaïbou M, Tucci M, Dugas MA, Farrell CA, Proulx F, Lacroix J. Clinically significant upper gastrointestinal bleeding acquired in a pediatric intensive care unit: a prospective study. Pediatrics. (1998) 102:933–8. doi: 10.1542/peds.102.4.933
10. López-Herce J, Dorao P, Elola P, Delgado MA, Ruza F, Madero R. Frequency and prophylaxis of upper gastrointestinal hemorrhage in critically ill children: a prospective study comparing the efficacy of almagate, ranitidine, and sucralfate. The Gastrointestinal Hemorrhage Study Group. Crit Care Med. (1992) 20:1082–9. doi: 10.1097/00003246-199208000-00003
11. Nithiwathanapong C, Reungrongrat S, Ukarapol N. Prevalence and risk factors of stress-induced gastrointestinal bleeding in critically ill children. World J Gastroenterol. (2005) 11:6839–42. doi: 10.3748/wjg.v11.i43.6839
12. Moorehead PC, Cyr J, Klaassen R, Barrowman NJ, Menon K. An evidence-based threshold for thrombocytopenia associated with clinically significant bleeding in pediatric intensive care unit patients. Pediatr Crit Care Med. (2012) 13:e316–22. doi: 10.1097/PCC.0b013e31824ea28d
13. Moorehead PC, Barrowman NJ, Cyr J, Ray J, Klaassen R, Menon K. A prospective study of the association between clinically significant bleeding in PICU patients and thrombocytopenia or prolonged coagulation times. Pediatr Crit Care Med. (2017) 18:e455–62. doi: 10.1097/PCC.0000000000001281
14. Fasulo MR, Biguzzi E, Abbattista M, Stufano F, Pagliari MT, Mancini I, et al. The ISTH bleeding assessment tool and the risk of future bleeding. J Thromb Haemost. (2018) 16:125–30. doi: 10.1111/jth.13883
15. Pinto MG, Shabanova V, Li S, Trakas E, Miksa M, Gertz S, et al. Epidemiology of clinically relevant bleeding in critically ill adolescents. Pediatr Crit Care Med. (2019) 20:907–13. doi: 10.1097/PCC.0000000000002018
16. Kenet G, Strauss T, Kaplinsky C, Paret G. Hemostasis and thrombosis in critically ill children. Semin Thromb Hemost. (2008) 34:451–8. doi: 10.1055/s-0028-1092875
17. Bateman ST, Lacroix J, Boven K, Forbes P, Barton R, Thomas NJ, et al. Anemia, blood loss, and blood transfusions in North American children in the intensive care unit. Am J Respir Crit Care Med. (2008) 178:26–33. doi: 10.1164/rccm.200711-1637OC
18. Williams MD, Chalmers EA, Gibson BE. The investigation and management of neonatal hemostasis and thrombosis. Br J Haematol. (2002) 119:295–309. doi: 10.1046/j.1365-2141.2002.03674.x
19. Andrew M, Paes B, Milner R, Johnston M, Mitchell L, Tollefson DM, et al. Development of the human coagulation system in the full-term infant. Blood. (1987) 70:165–72. doi: 10.1182/blood.V70.1.165.165
20. Zimmerman LH. Causes and consequences of critical bleeding and mechanisms of blood coagulation. Pharmacotherapy. (2007) 27:45S−56S. doi: 10.1592/phco.27.9part2.45S
21. Meng ZH, Wolberg AS, Monroe DM III, Hoffman M. The effect of temperature and pH on the activity of factor VIIa: implications for the efficacy of high-dose factor VIIa in hypothermic and acidotic patients. J Trauma. (2003) 55:886–91. doi: 10.1097/01.TA.0000066184.20808.A5
22. Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, AWARE Investigators. Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med. (2017) 376:11–20. doi: 10.1056/NEJMoa1611391
23. Mataloun SE, Machado FR, Senna APR, Guimaraes HP, Amaral JLG. Incidence, risk factors and prognostic factors of acute renal failure in patients admitted to an intensive care unit. Braz J Med Biol Res. (2006) 39:1339–47. doi: 10.1590/S0100-879X2006001000010
24. Van de Wetering J, Westendorp RG, van der Hoeven JG, Stolk B, Feuth JD, Chang PC. Heparin use in continuous renal replacement procedures: the struggle between filter coagulation and patient hemorrhage. J Am Soc Nephrol. (1996) 7:45–50.
25. Kreuzer M, Ehrich JH, Pape L. Haemorrhagic complications in paediatric dialysis-dependent acute kidney injury: incidence and impact on outcome. Nephrol Dial Transplant. (2010) 25:1140–6. doi: 10.1093/ndt/gfp596
26. DeLoughery TG. Critical care clotting catastrophies. Crit Care Clin. (2005) 21:531–62. doi: 10.1016/j.ccc.2005.05.003
27. Sahin S, Ayar G, Yazici MU, Koksal T, Akman AO, Gunduz RC, et al. Stress induced gastrointestinal bleeding in a pediatric intensive care unit: which risk factors should necessitate prophylaxis? Minerva Pediatr. (2016) 68:19–26.
28. Toh CH, Hoots WK. SSC on Disseminated Intravascular Coagulation of the ISTH. The scoring system of the Scientific and Standardisation Committee on disseminated intravascular coagulation of the International Society on Thrombosis and Haemostasis: a 5-year overview. J Thromb Haemost. (2007) 5:604–6. doi: 10.1111/j.1538-7836.2007.02313.x
29. Carey MJ, Rodgers GM. Disseminated intravascular coagulation: clinical and laboratory aspects. Am J Hematol. (1998) 59:65–73. doi: 10.1002/(SICI)1096-8652(199809)59:1<65::AID-AJH13>3.0.CO;2-0
30. Jhang WK, Ha E, Park SJ. Evaluation of disseminated intravascular coagulation scores in critically ill pediatric patients with septic shock. J Crit Care. (2018) 47:104–8. doi: 10.1016/j.jcrc.2018.06.017
31. Khemani RG, Bart RD, Alonzo TA, Hatzakis G, Hallam D, Newth CJ. Disseminated intravascular coagulation score is associated with mortality for children with shock. Intensive Care Med. (2009) 35:327–33. doi: 10.1007/s00134-008-1280-8
32. Chuansumrit A, Hotrakitya S, Sirinavin S, Supapanachart S, Khowsathit P, Chantarojanasiri T, et al. Disseminated intravascular coagulation findings in 100 patients. J Med Assoc Thai. (1999) 82:S63–8.
33. Welsh SK, Casey AM, Fishman MP. Pulmonary hemorrhage in infancy: a 10-year single-center experience. Pediatr Pulmonol. (2018) 53:1559–64. doi: 10.1002/ppul.24142
34. Lykissas MG, Crawford AH, Jain VV. Complications of surgical treatment of pediatric spinal deformities. Orthoped Clin N Am. (2013) 44:357–70 (ix). doi: 10.1016/j.ocl.2013.03.007
35. Yoshihara H, Yoneoka D. Trends in the utilization of blood transfusions in spinal fusion in the United States from 2000 to 2009. Spine. (2014) 39:297–303. doi: 10.1097/BRS.0000000000000122
36. Sugawara R, Takeshita K, Takahashi J, Arai Y, Watanabe K, Yamato Y, et al. The complication trends of pediatric spinal deformity surgery in Japan—the Japanese Scoliosis Society Morbidity and Mortality survey from 2012 to 2017. J Orthop Sci. (2020). doi: 10.1016/j.jos.2020.07.007. [Epub ahead of print].
37. Eisler LD, Lenke LG, Sun LS, Li G, Kim M. Do antifibrinolytic agents reduce the risk of blood transfusion in children undergoing spinal fusion? A propensity score-matched comparison using a national database. Spine. (2020) 45:1055–61. doi: 10.1097/BRS.0000000000003455
38. McEwan A. Aspects of bleeding after cardiac surgery in children. Paediatr Anaesth. (2007) 17:1126–33. doi: 10.1111/j.1460-9592.2007.02265.x
39. Wedemeyer AL, Edson JR, Krivit W. Coagulation in cyanotic congenital heart disease. Am J Dis Child. (1972) 124:656–60. doi: 10.1001/archpedi.1972.02110170034005
40. Ekert H, Gilchrist GS, Stanton R, Hammond D. Hemostasis in cyanotic congenital heart disease. J Pediatr. (1970) 76:221–30. doi: 10.1016/S0022-3476(70)80166-4
41. Mauer HM, McCue CM, Caul J, Still WJ. Impairment in platelet aggregation in congenital heart disease. Blood. (1972) 40:207–16. doi: 10.1182/blood.V40.2.207.207
42. Petäjä J, Lundström U, Leijala M, Peltola K, Siimes MA. Bleeding and use of blood products after heart operations in infants. J Thorac Cardiovasc Surg. (1995) 109:524–9. doi: 10.1016/S0022-5223(95)70284-9
43. Agarwal HS, Barrett SS, Barry K, Xu M, Saville BR, Donahue BS, et al. Association of blood products administration during cardiopulmonary bypass and excessive post-operative bleeding in pediatric cardiac surgery. Pediatr Cardiol. (2015) 36:459–67. doi: 10.1007/s00246-014-1034-z
44. Oliver WC Jr., Beynen FM, Nuttall GA, Schroeder DR, Ereth MH, Dearani JA, et al. Blood loss in infants and children for open heart operations: albumin 5% versus fresh-frozen plasma in the prime. Ann Thorac Surg. (2003) 75:1506–12. doi: 10.1016/S0003-4975(02)04991-3
45. Székely A, Cserép Z, Sápi E, Breuer T, Nagy CA, Vargha P, et al. Risks and predictors of blood transfusion in pediatric patients undergoing open heart operations. Ann Thorac Surg. (2009) 87:187–97. doi: 10.1016/j.athoracsur.2008.09.079
46. Guzzetta NA, Allen NN, Wilson EC, Foster GS, Ehrlich AC, Miller BE. Excessive postoperative bleeding and outcomes in neonates undergoing cardiopulmonary bypass. Anesth Analg. (2015) 120:405–10. doi: 10.1213/ANE.0000000000000531
47. Wolf MJ, Maher KO, Kanter KR, Kogon BE, Guzzetta NA, Mahle WT. Early postoperative bleeding is independently associated with increased surgical mortality in infants after cardiopulmonary bypass. J Thorac Cardiovasc Surg. (2014) 148:631–6. doi: 10.1016/j.jtcvs.2013.10.050
48. Chambers LA, Cohen DM, Davis JT. Transfusion patterns in pediatric open-heart surgery. Transfusion. (1996) 36:150–4. doi: 10.1046/j.1537-2995.1996.36296181928.x
49. Closson R, Mauer E, Stock A, Dayton JD, LaPar DJ, Walline MA, et al. The use of hemostatic blood products in children following cardiopulmonary bypass and associated outcomes. Crit Care Explor. (2020) 2:e0172. doi: 10.1097/CCE.0000000000000172
50. Faraoni D, Meier J, New HV, Van der Linden PJ, Hunt BJ. Patient blood management for neonates and children undergoing cardiac surgery: 2019 NATA guidelines. J Cardiothorac Vasc Anesth. (2019) 33:3249–63. doi: 10.1053/j.jvca.2019.03.036
51. Giglia TM, Witmer C. Bleeding and thrombosis in pediatric cardiac intensive care. Pediatr Crit Care Med. (2016) 17:S287–95. doi: 10.1097/PCC.0000000000000814
52. Barbaro RP, Paden ML, Guner YS, Raman L, Ryerson LM, Alexander P, et al. Pediatric extracorporeal life support organization registry international report 2016. ASAIO J. (2017) 63:456–63. doi: 10.1097/MAT.0000000000000603
53. Paden ML, Conrad SA, Rycus PT, Thiagarajan RR, ELSO Registry. Extracorporeal Life Support Organization Registry report 2012. ASAIO J. (2013) 59:202–10. doi: 10.1097/MAT.0b013e3182904a52
54. Zangrillo A, Landoni G, Biondi-Zoccai G, Greco M, Greco T, Frati G, et al. A meta-analysis of complications and mortality of extracorporeal membrane oxygenation. Crit Care Resusc. (2013) 15:172–8.
55. Sy E, Sklar MC, Lequier L, Fan E, Kanji HD. Anticoagulation practices and the prevalence of major bleeding, thromboembolic events, and mortality in venoarterial extracorporeal membrane oxygenation: a systematic review and meta-analysis. J Crit Care. (2017) 39:87–96. doi: 10.1016/j.jcrc.2017.02.014
56. Dalton HJ, Garcia-Filion P, Holubkov R, Moler FW, Shanley T, Heidemann S, et al. Association of bleeding and thrombosis with outcome in extracorporeal life support. Pediatr Crit Care Med. (2015) 16:167–74. doi: 10.1097/PCC.0000000000000317
57. Nellis ME, Dalton H, Karam O, PediECMO Investigators. Quantifiable bleeding in children supported by extracorporeal membrane oxygenation and outcome. Crit Care Med. (2019) 47:e886–92. doi: 10.1097/CCM.0000000000003968
58. Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer. (1981) 47:207–14. doi: 10.1002/1097-0142(19810101)47:1<207::AID-CNCR2820470134>3.0.CO;2-6
59. Rebulla P, Finazzi G, Marangoni F, Avvisati G, Gugliotta L, Tognoni G, et al. The threshold for prophylactic platelet transfusions in adults with acute myeloid leukemia. Gruppo Italiano Malattie Ematologiche Maligne dell'Adulto. N Engl J Med. (1997) 337:1870–5. doi: 10.1056/NEJM199712253372602
60. Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. (2009) 361:1139–51. doi: 10.1056/NEJMoa0905561
61. Schulman S, Angerås U, Bergqvist D, Eriksson B, Lassen MR, Fisher W, et al. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. J Thromb Haemost. (2010) 8:202–4. doi: 10.1111/j.1538-7836.2009.03678.x
62. Slichter SJ, Kaufman RM, Assmann SF, McCullough J, Triulzi DJ, Strauss RG, et al. Dose of prophylactic platelet transfusions and prevention of hemorrhage. N Engl J Med. (2010) 362:600–13. doi: 10.1056/NEJMoa0904084
63. Nellis ME, Levasseur J, Stribling J, Faustino EVS, Zantek ND, Sheth S, et al. Bleeding scales applicable to critically ill children: a systematic review. Pediatr Crit Care Med. (2019) 20:603–7. doi: 10.1097/PCC.0000000000001943
64. Heddle NM, Cook RJ, Webert KE, Sigouin C, Rebulla P. Methodologic issues in the use of bleeding as an outcome in transfusion medicine studies. Transfusion. (2003) 43:742–52. doi: 10.1046/j.1537-2995.2003.00418.x
65. Koreth R, Weinert C, Weisdorf DJ, Key NS. Measurement of bleeding severity: a critical review. Transfusion. (2004) 44:605–17. doi: 10.1111/j.1537-2995.2004.03153.x
66. Karam O, Nellis ME, Zantek ND, Lacroix J, Faustino, BloodNet and the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network. Criteria for clinically relevant bleeding in critically ill children: an international survey. Pediatr Crit Care Med. (2019) 20:e137–44. doi: 10.1097/PCC.0000000000001828
67. Nellis ME, Tucci M, Lacroix J, Spinella PC, Haque KD, Stock A, et al. Bleeding assessment scale in critically ill children (BASIC): physician-driven diagnostic criteria for bleeding severity. Crit Care Med. (2019) 47:1766–72. doi: 10.1097/CCM.0000000000004025
Keywords: bleeding, hemorrhage, scale, epidemiology, critical ill children
Citation: Aran AA, Karam O and Nellis ME (2021) Bleeding in Critically Ill Children—Review of Literature, Knowledge Gaps, and Suggestions for Future Investigation. Front. Pediatr. 9:611680. doi: 10.3389/fped.2021.611680
Received: 29 September 2020; Accepted: 04 January 2021;
Published: 27 January 2021.
Edited by:
John McGuire, University of Washington, United StatesReviewed by:
Jhuma Sankar, All India Institute of Medical Sciences, IndiaMartin Kneyber, University Medical Center Groningen, Netherlands
Copyright © 2021 Aran, Karam and Nellis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marianne E. Nellis, bWFuOTAyNkBtZWQuY29ybmVsbC5lZHU=
 Adi Avniel Aran
Adi Avniel Aran Oliver Karam
Oliver Karam Marianne E. Nellis
Marianne E. Nellis