- 1Dr. v. Hauner Children’s Hospital, Pediatric Intensive Care Unit, Ludwig-Maximilians-University Munich, Munich, Germany
- 2Division of Pediatric Intensive Care, Department of Pediatrics, University Hospital Carl Gustav Carus, Dresden, Germany
Background: Vascular access is essential for the efficient treatment of critically ill children, but it can be difficult to obtain. Our study was conducted to analyze the feasibility and short-term safety of intraosseous access (IO) use as well as factors influencing its success and the incidence of complications in pediatric emergencies and resuscitation. This dataset of systematically documented intraosseous access attempts constitutes one of the largest published in the literature.
Methods: Two-year nationwide prospective surveillance study in Germany from July 2017 to June 2019. Pediatric hospitals anonymously reported the case data of all children aged 28 days to 18 years who arrived with or were treated with an intraosseous access to the German Pediatric Surveillance Unit (GPSU). The main outcomes were the occurrence of complications, overall success and success at the first attempt. The influence of individual factors on outcomes was evaluated using multivariate regression models.
Results: A total of 417 patients underwent 549 intraosseous access attempts. The overall rates of success and success at the first attempt were 98.3% and 81.9%, respectively. Approximately 63.6% of patients were successfully punctured within 3 min from the time of indication. Approximately 47.7% of IO access attempts required patient resuscitation. Dislocation [OR 17.74 (5.32, 59.15)] and other complications [OR 9.29 (2.65, 32.55)] occurred more frequently in the prehospital environment. A total of 22.7% of patients experienced minor complications, while 2.5% of patients experienced potentially severe complications.
Conclusion: We conclude that intraosseous access is a commonly used method for establishing emergency vascular access in children, being associated with a low (age-dependent) rate of severe complications and providing mostly reliable vascular access despite a relatively high rate of dislocation.
Introduction
Vascular access is paramount for the efficient treatment of critically ill children. Because multiple attempts to establish intravenous access increase mortality rates due to prolonged on-scene times or delayed application of drugs, choosing the best site for quick and reliable vascular access plays an important role in increasing the chances of survival (1, 2).
Establishing a conventional intravenous line in a critically ill pediatric patient is challenging and fails in almost 1/3 of patients treated in the prehospital environment (3). According to several guidelines, the intraosseous route should be considered in the early stage of life-threatening pediatric emergencies, and, as a result of such recommendation, the intraosseous access has been increasingly used in past decades, especially in the prehospital setting (4–7). As many as 1 in 4 critically ill children arrive at a hospital with an intraosseous cannula (3). However, time constraints associated with pediatric emergencies and anatomic challenges, such as a thickened subcutaneous layer and small target structures, pose challenges even for experienced providers (7).
Although intraosseous access is widely regarded as facilitating fast and reliable vascular access to administer drugs and fluids, there are only a few studies on success rates in children and long- and short-term safety in terms of adverse outcomes. Furthermore, it remains unclear whether findings from adult patient studies can be translated to pediatric patients. Studies with a large sample size have yet to be published (7).
This study aims to evaluate the safety and success rates and influencing factors of the use of intraosseous devices in children being treated in the hospital and the prehospital setting.
Methods
Study population and case reporting
The present study includes the clinical data of all pediatric patients who are included in the GPSU database and who received IO access in a clinical or/and an out-of-hospital setting in Germany between their first month of life and adulthood. The data of patients who met the case definition were reported monthly to GPSU, from 1 July 2017 to 30 June 2019. GPSU is a well-established hospital-based nationwide prospective surveillance system for rare pediatric diseases covering 345 pediatric hospitals and departments in Germany. Regular analysis of its capture rates showed that reporting completeness of the GPSU surveillance system consistently exceeds 95% (8).
Ethical approval and consent to participate
All surveillance studies of the GPSU are based on a common study and data protection protocol. The local ethics committee of the Rhineland-Palatinate Medical Association and the state representative for data protection in Rhineland-Palatinate have approved this protocol. A waiver of written informed consent was granted by the Ethics Committee of the State Medical Association of Rhineland-Palatinate (Number 2020-15400_1) and the state representative for data protection in Rhineland-Palatinate as participants were not subjected to any study-related procedures and data were collected in a completely anonymous form.
All analyzed data involving human participants were collected in accordance with the ethical standards outlined in the 1964 Helsinki declaration and its later amendments or comparable ethical standards. In addition to the general ethical approval of the GPSU, the study was approved by the data protection office and the ethics committee of the medical faculty of the Ludwig-Maximilians-University, Munich Nr. 641-16 (19-12-2016).
Data collection
In this prospective, population-based surveillance study, all the involved German pediatric hospitals and departments received a monthly reminder to report the data of all patients with IO access, including the data of patients who were punctured in their center and the data of those who were transferred with IO access from another center or prehospital setting, as far as known in the receiving center. The report of a case prompted the dissemination of a study-specific pseudonymized questionnaire that was designed by a consensus panel of pediatric emergency specialists of the German Society for Neonatology and Pediatric Intensive Care Medicine (GNPI) and German Interdisciplinary Society for Intensive Care and Emergency Medicine (DIVI).
The questionnaire was completed by the attending pediatrician and then returned with anonymized patient information to GPSU in Mainz (formerly Düsseldorf), Germany. The questionnaire included details on demographic data (age, sex, gestational age), medical indication for the use of an IO needle and diagnosis, IO access use (number of attempts, anatomical location of needle placement, system used, qualification of attending physician, retrospectively estimated time to first access, alternative vascular access routes attempted, infused/applied substances, complications, and time to removal), and the course of the disease and outcome. The overall response rate to the distributed questionnaires after report of a case was 94.4%. All reports were checked for plausibility of data by 2 pediatric intensivists.
Overall success was defined as a patient who received an IO access that facilitated the application for an appropriate amount of time to administer necessary drugs to treat the patient, regardless of the number of attempts.
Statistical analysis
Data were entered into a Microsoft Office Access 2003 (Version 11.0) database and transferred to the R statistical package, version 3.6.2, for group comparisons. We compared patient groups by analyzing criteria at the patient level as well as on an individual IO attempt basis using Student's t test, χ2 test and Fisher's exact test as appropriate.
Results
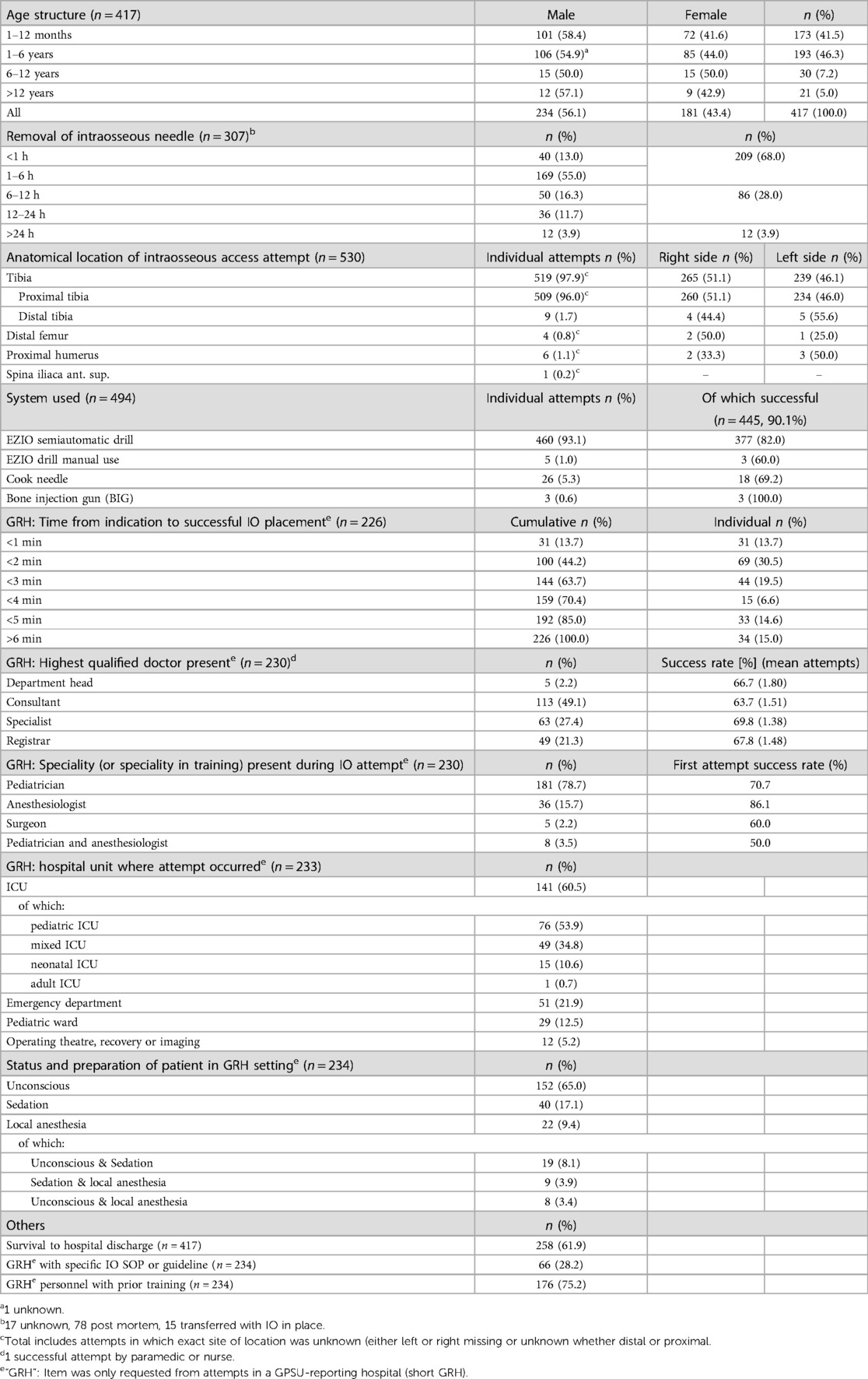
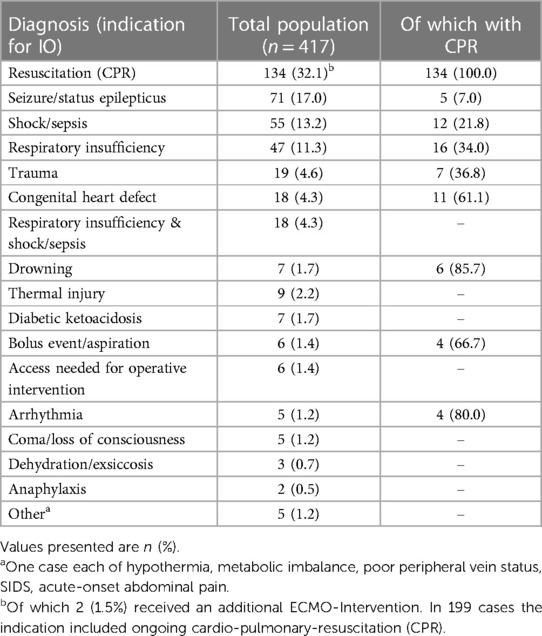
Over the study period of two years, the clinical data of 417 patients who underwent 549 attempts to establish intraosseous access were included in the analysis. More than 1 access attempt was made in 110 patients (26.4%). A total of 87.8% were between 1 month and 6 years old. In 199 patients (47.7%), the indication included ongoing cardiopulmonary resuscitation (CPR).
Table 1 provides an overview of the basic characteristics of the study population.
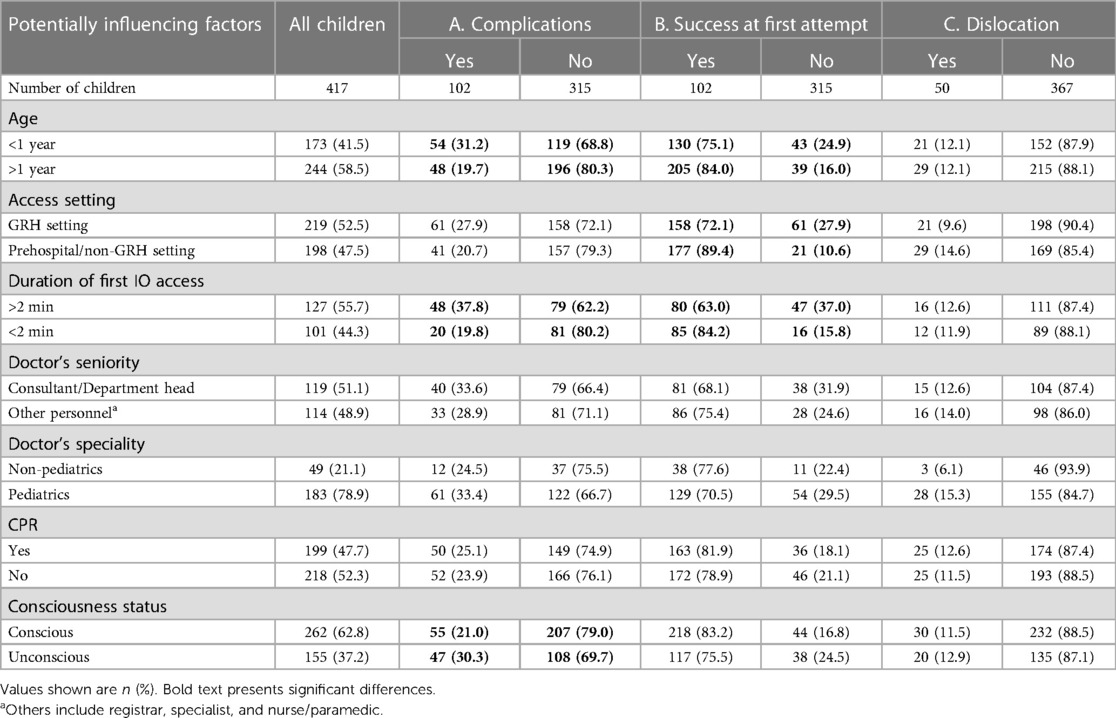
A total of 81.9% of all IO attempts worked at the first attempt, while 98.3% of patients had at least one working access for a long enough period to give necessary drugs (classified as overall success). First attempt success was achieved significantly more often in children older than 1 year of age (p = 0.034), in a prehospital setting (p = 0.000017) and when first attempts took less than 2 min (p = 0.00067). An overview of success rates and complication dynamics by age group can be found in Supplementary Figure S1 Content section.
Almost 3/4 of patients (74.4%) had no complications during their hospitalization related to the establishment of intraosseous access. In 92 patients (22.7%), minor complications, classified as extra or paravasation, misplacement into soft tissue or local swelling, occurred. Ten patients (2.5%) experienced at least one potentially severe complication, including compartment syndrome (n = 4), necrosis (n = 5), soft tissue infections (n = 2), poor perfusion of the foot (n = 1) and potential piercing of the tibial bone (n = 1). In 0.5% of attempts, technical difficulties caused by insufficient charges in the battery due to old equipment or frequent testing in the equipment check routine were encountered. In children younger than 1 year of age, significantly more complications were encountered (p = 0.009).
In terms of indicators of correct placement, out of all attempts with complete information that were successful at the first attempt (n = 169), 76.9% had a firm fit in the bone, and 77.5% showed no signs of paravasation. In 53.8% of cases, aspiration of blood/bone marrow was reported. A total of 11.7% of initially successful IO accesses dislocated after some time of use.
The proportions of potentially influencing factors on IO access outcomes are detailed in Table 2. The effects of individual factors are displayed in Supplementary Figure S2–S4 Content section.
The success or failure of an IO attempt in our data does not significantly depend on which system was used (p = 0.2096).
Analyzing the effect of individual factors on the occurrence of moderate and severe patient-side complications, a univariate model identified unconsciousness, age <1 year and prolonged insertion times (>2 min) as proxies for a difficult placement setting. In a multivariate model using stepwise backward selection, a prolonged insertion time (OR 2.58) and prehospital/non-GRH (GPSU-reporting Hospital) setting (OR 9.29) significantly increased the occurrence of complications. We further investigated the factors that influenced first-time success. The multivariate backward selection model identified only a time >2 min to first working access as a significant positive influencing factor on first attempt success. In a similar fashion, the effect of a set of factors on dislocation was assessed. A highly significant OR of 17.74 was identified for dislocations occurring in a prehospital/non-GRH setting.
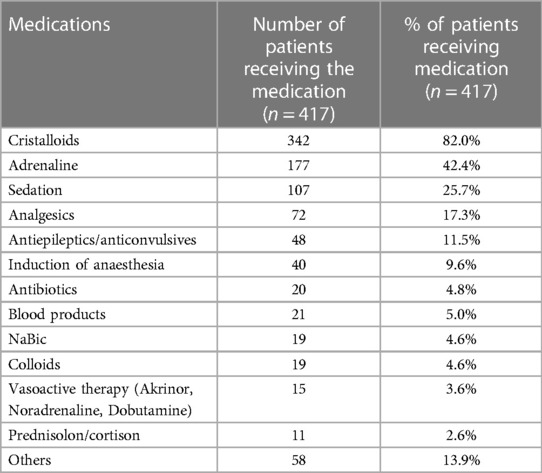
Additional data on diagnoses leading to intraosseous access attempts, medications applied via the intraosseous route as well as success rates and complication occurrence by age group can be found in Tables 3–5 respectively.
Discussion
To our knowledge, this dataset of systematically documented intraosseous access attempts constitutes one of the largest published in the literature.
Our study found that both the chance of success at the first attempt and the overall success rate increased significantly with the age of the child. In parallel, the overall rate and rate of severe complications decreased sharply as the size and age of the child increased, which were consistent with Capobianco et al.'s (9) study in that a higher risk of incorrect positioning was found in smaller target structures. Schwindt et al. (10) found that this trend continues in patients receiving an IO in their first 24 h of life, with higher gestational age increasing the overall success rate.
By comparing the success rates in our study with those in other studies, we found that the success rate for all attempts in our cohort was higher at 81.2% than the 65.0% success rate in the cohort of 4,270 pediatric patients in the study by Rosetti et al. (11) and that the mean number of attempts in our cohort was lower at 1.31 vs. 1.54 and the EZIO-specific (the product name of the most frequently-used intraosseous access drill by the company Arrow) success rate in our cohort was higher at 81.2% vs. 70.0% (12). Myers et al. reported the results of 62 patients, which are in line with the findings of our study, with a first attempt success rate for EZIO devices of 83.9% vs. 81.9% (12). Sunde et al. published a 96% overall success rate for the EZIO system, which is higher than the 82.0% (n = 460) achieved in this cohort, while 55% for the Cook needle is below our estimate of 68.0% (n = 25) for Cook needles (13). Helm et al. (14) even found a 100% overall and 87.5% first try success rate in children smaller 7 years of age in a prehospital setting. Our data suggests a significant difference in first attempt success rate between children smaller 1 year of age and children older 1 year of age of 75.1% and 84.0% respectively.
Individual cases of manual EZIO placement were reported in children less than 12 months of age. This represents a possible alternative for placement in small children, as also shown for the neonatal cohort by Schwindt et al. (10).
The proximal tibia is the preferred location for IO access due to its ease of identification, thin layer of subcutaneous tissue and relatively large target area, which is well reflected in our data.
Somewhat counterintuitively, prolonged placement of the first IO access increases the risk for complications by 2.58 and the rate for success on the 1st attempt by 3.3. We attribute these increases to prolonged placement and preparation (e.g., time spent for optimal positioning).
According to Leidel et al., the first-time success rate of IO access during resuscitation in a level 1 trauma center in adults was 85% and that of central venous catheter (CVC) placement was 60% (15).
A very early study from Rosetti et al. (16) in 1985 found a very low rate of potentially severe complications of only 0.9%, of which 0.6% were osteomyelitis. The low rate of potentially severe complications in our cohort was 2.5%, which constitutes a justifiable risk in terms of the urgent need for quick vascular access in life-threatening emergencies. No cases of osteomyelitis were observed in our cohort. The relatively high rate of minor complications of 22.1% seems acceptable in life-threatening emergency situations and, if detected early, usually does not lead to long-term complications. Mori et al. found a comparable rate of minor complications of 21.6% (17 extravasations of fluid and 4 dermal abrasions) in a pediatric emergency department cohort (17). In the few articles on long-term complications, there are no relevant long-term effects of intraosseous infusion on tibial bone growth (18).
Our study found a strong difference in the rate of complications between children younger and children older than 1 year of age. While the overall rate of complications is 19.7% above 1 year of age, IO access attempts in children younger than 1 year of age encounter complications in almost every third patient (31.2%).
The significantly decreased occurrence of complications and lower failure rate of IO attempts in a prehospital setting might be due to underreporting of additional attempts which were unknown to the admitting center and/or complications at the handover or might be due to prehospital staff being more familiar and experienced with IO devices.
Initially, successfully placed needles dislocated at a relatively high rate of 11.7%, often leading to a necessary second attempt. According to user comments, this was often due to poor fixation in children, although dislocation through high intramedullary pressure by fluid bolus application or other causes might be possible. A sufficient amount of time is needed to precisely fix the cannula, especially in a prehospital environment where dislocations were observed in almost every 7th patient and almost twice as frequently compared to an intrahospital setting (13.3% vs. 7.4%).
Almost two-thirds of patients (61.6%) received alternative access attempts before IO access was attempted. In 248 patients a peripheral venous line, in 21 patients a central venous line and in 1 patient a port puncture was attempted. In the prehospital setting, the percentage of patients receiving alternative access attempts across all indications was 44.9%. Only 47.1% (97/206) of patients with indications for resuscitation in the prehospital setting and in a GPSU-reporting hospital (short GRH) underwent an alternative access attempt before IO access was attempted. In 9 cases, an IO was attempted with an alternative access already in place due to the need for a higher inflow of drugs and/or a further vascular access. According to the ERC guidelines at that time, IO access should be attempted 60 s after attempts to create intravenous access were unsuccessful; thus, because of the low rate of successful IV placement in critically ill children, IO access should be the primary access method (4, 7). Lee et al. (19), however, discovered that providers might still be hesitant to use IO in non-CPR settings.
Interestingly, frequent use of IO accesses during seizures (n = 66, 15.8%) as a means of infusing anti-epileptic/convulsive drugs was reported. This is surprising due to the existence of a less invasive application method, such as intranasal, buccal or intramuscular routes of antiepileptic drug application. Bhattacharyya et al. (20) identified a mean time from arrival at the emergency to the administration of intranasal midazolam of 50.6 +/− 14.1 s, which was shorter than the average IO insertion time by almost 2 min, while Mahmoudian (21) found no significant side effects of intranasal drug application. Another alternative form is intramuscular application of midazolam, which could help to prevent the need for IO access (22).
With almost two-thirds (64.8%) of all IO needles being removed within 12 h of placement and only a small fraction (3.0%) remaining in place for more than 24 h, our data confirm that intraosseous access is mainly used to establish quick emergency access to bridge emergency situations until a more permanent access, such as a central or peripheral venous catheter, can be established. This finding is also in accordance with guidelines (7) in which the maximum use time is 24 h and the ideal removal time is 2 h after arrival at the hospital and replacement with another access method. Suominen et al. (23) suggests aiming for early removal of the IO needle and ensuring vigilant and frequent monitoring of perfusion in the affected extremity. In contrast, Philbeck et al. (24) demonstrated that it might be safe to maintain the EZIO in place for up to 48 h in an adult cohort. The German guideline on intraosseous infusion, however, recommends interpreting these results with great care and only as preliminary findings (7).
Pediatricians and anesthesiologists performed 97.9% of all access attempts in a GRH setting, with a board qualified physician being present in 78.4% of cases and a consultant or department head in 51.1% of cases. Intensified training efforts on IO indication, handling and placement would be well advised for those two specialties, and more generally, all medical personnel, doctors, nurses and paramedics treating children (25) should have timely access to and be familiar with and well trained in the use of intraosseous drills and access methods (7).
Regular training is important and leads to high success rates, as demonstrated by a simulation-based IO-training study using manikins. Thus, it is reasonable to conclude that six months after a single training session, the success rates for correct identification of the puncture site as well as successful puncture at the first attempt are high (26, 27).
Limitations
Multiple limitations apply to our data. Data being acquired via German hospitals only might limit the applicability of the data in settings where training, SOPs, and operating circumstances might differ widely. Evaluating details of an emergency situation, often filling out the questionnaire sometime after the event, might have led to misinformation or lost details. Time to establish the io access was estimated, not measured. Reconstructing the chain of events and their success rate from a retrospective questionnaire posed some significant challenges that might have also introduced some discrepancies in how events truly occurred. GPSU might have introduced a significant underreporting bias. Children who did not arrive at a GRH, for example, because resuscitation was discontinued in a prehospital setting, were not reported to GPSU and are not included in our data. The lack to follow-up this population might introduce a significant bias as there might potentially be significant discrepancies in malpositioning rates in the post-mortem cohort as suggested by Maxien et al. (28) There is a possibility of an underreporting bias of critical incidence, as reporting was voluntary. There was no further information on the extent or area of the complications available.
Conclusion
This study supports the recommendations of international guidelines regarding intraosseous access use. First attempt and overall success increase significantly with the age of the child, while the rate of minor and severe complications decrease significantly in children older one year of age. Given the paramount need for quick vascular access in emergency situations the rate of severe complications is low, while the chance of achieving successful emergency access is high. Dislocations occur in almost 1 out of 10 cases and twice as frequently in the prehospital environment. We conclude that intraosseous access is a frequently used and reliable method for the establishment of vascular access in an emergency situation.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation upon reasonable request.
Ethics statement
The studies involving humans were approved by the ethics committee of the medical faculty of the Ludwig-Maximilians-University, Munich Nr. 641-16 (19-12-2016), the Ethics Committee of the Rhineland-Palatinate Medical Association as well as the state representative for data protection in Rhineland-Palatinate. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because participants were not subjected to any study-related procedures and data were collected in a completely anonymous form.
Author contributions
DP: Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review & editing. MO: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing. SB: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing. DG: Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review & editing. VL: Funding acquisition, Supervision, Writing – review & editing. FH: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This project was financially supported by the “German Interdisciplinary Society for Intensive Care and Emergency Medicine” (DIVI) and the BINZ Foundation.
Acknowledgments
This project was supported by the “German Society for Neonatology and Pediatric Intensive Care” (GNPI) and the “German Interdisciplinary Society for Intensive Care and Emergency Medicine” (DIVI). We thank the Erhebungseinheit für Seltene Pädiatrische Erkrankungen in Deutschland (GPSU, German Pediatric Surveillance Unit) and Beate Heinrich for their exceptional cooperation and collaboration. The authors thank all participating hospitals and physicians involved in data collection.
Conflict of interest
FH is president-elect of the German Interdisciplinary Society for Intensive Care and Emergency Medicine (DIVI) and was involved in the guideline process for the European Resuscitation Councils 2021 Pediatric Life Support Guidelines and the Pediatric Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. MO is spokesperson for the DIVI department Pediatric Intensive-Care and Emergency Medicine. SB is committee member in the DIVI presidium for Pediatric and Adolescent Medicine.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1294322/full#supplementary-material
References
1. Hansen M, Schmicker RH, Newgard CD, Grunau B, Scheuermeyer F, Cheskes S, et al. Time to epinephrine administration and survival from nonshockable out-of-hospital cardiac arrest among children and adults. Circulation. (2018) 137(19):2032–40. doi: 10.1161/CIRCULATIONAHA.117.033067
2. Banerjee P, Ganti L, Stead TG, Vera AE, Vittone R, Pepe PE. Every one-minute delay in EMS on-scene resuscitation after out-of-hospital pediatric cardiac arrest lowers ROSC by 5. Resusc Plus. (2021) 5:100062. doi: 10.1016/j.resplu.2020.100062
3. Sommer A, Weiss M, Deanovic D, Dave M, Neuhaus D. Einsatz der intraossären infusion im pädiatrischen notarztdienst. Analyse von notarzteinsätzen 1990–2009. Anaesthesist. (2011) 60(2):125–31. doi: 10.1007/s00101-010-1802-y
4. van de Voorde P, Turner NM, Djakow J, de Lucas N, Martinez-Mejias A, Biarent D, et al. Lebensrettende maßnahmen bei kindern (paediatric life support, PLS): leitlinien des European resuscitation Council 2021 [Paediatric Life Support]. Notf Rett Med. (2021) 24(4):650–719. German. doi: 10.1007/s10049-021-00887-9
5. Maconochie IK, Aickin R, Hazinski MF, Atkins DL, Bingham R, Couto TB, et al. Pediatric life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. (2020) 156:A120–55. doi: 10.1016/j.resuscitation.2020.09.013
6. Maconochie IK, Bingham R, Eich C, López-Herce J, Rodríguez-Núñez A, Rajka T, et al. European Resuscitation council guidelines for resuscitation 2015: section 6. Paediatric life support. Resuscitation. (2015) 95:223–48. doi: 10.1016/j.resuscitation.2015.07.028
7. Helm M, Gräsner JT, Gries A, Fischer M, Böttiger B, Eich C, et al. S1-leitlinie 001-042: die intraossäre infusion in der notfallmedizin: aktualisierte handlungsempfehlungen des wissenschaftlichen arbeitskreises kinderanästhesie (WAKKA) der deutschen gesellschaft für anästhesiologie und intensivmedizin (DGAI).
8. Göbel U, Heinrich B, Krauth KA, Steingrüber H-J, von Kries R. Evaluation der prozess- und ergebnisqualität der erhebungseinheit für seltene pädiatrische erkrankungen in deutschland (ESPED). Klin Padiatr. (2010) 222(2):92–7. doi: 10.1055/s-0030-1247587
9. Capobianco S, Weiss M, Schraner T, Stimec J, Neuhaus K, Neuhaus D. Checking the basis of intraosseous access-radiological study on tibial dimensions in the pediatric population. Paediatr Anaesth. (2020) 30(10):1116–23. doi: 10.1111/pan.13979
10. Schwindt E, Pfeiffer D, Gomes D, Brenner S, Schwindt J-C, Hoffmann F, et al. Intraosseous access in neonates is feasible and safe—an analysis of a prospective nationwide surveillance study in Germany. Front Pediatr. (2022) 10:952632. doi: 10.3389/fped.2022.952632
11. Pifko EL, Price A, Busch C, Smith C, Jiang Y, Dobson J, et al. Observational review of paediatric intraosseous needle placement in the paediatric emergency department. J Paediatr Child Health. (2018) 54(5):546–50. doi: 10.1111/jpc.13773
12. Myers LA, Russi CS, Arteaga GM. Semiautomatic intraosseous devices in pediatric prehospital care. Prehosp Emerg Care. (2011) 15(4):473–6. doi: 10.3109/10903127.2011.598611
13. Sunde GA, Heradstveit BE, Vikenes BH, Heltne JK. Emergency intraosseous access in a helicopter emergency medical service: a retrospective study. Scand J Trauma Resusc Emerg Med. (2010) 18:52. doi: 10.1186/1757-7241-18-52
14. Helm M, Haunstein B, Schlechtriemen T, Ruppert M, Lampl L, Gäßler M. EZ-IO(®) intraosseous device implementation in German helicopter emergency medical service. Resuscitation. (2015) 88:43–7. doi: 10.1016/j.resuscitation.2014.12.015
15. Leidel BA, Kirchhoff C, Bogner V, Braunstein V, Biberthaler P, Kanz K-G. Comparison of intraosseous versus central venous vascular access in adults under resuscitation in the emergency department with inaccessible peripheral veins. Resuscitation. (2012) 83(1):40–5. doi: 10.1016/j.resuscitation.2011.08.017
16. Rosetti VA, Thompson BM, Miller J, Mateer JR, Aprahamian C. Intraosseous infusion: an alternative route of pediatric intravascular access. Ann Emerg Med. (1985) 14(9):885–8. doi: 10.1016/S0196-0644(85)80639-9
17. Mori T, Takei H, Sasaoka Y, Nomura O, Ihara T. Semi-automatic intraosseous device (EZ-IO) in a paediatric emergency department. J Paediatr Child Health. (2020) 56(9):1376–81. doi: 10.1111/jpc.14940
18. Fiser RT, Walker WM, Seibert JJ, McCarthy R, Fiser DH. Tibial length following intraosseous infusion: a prospective, radiographic analysis. Pediatr Emerg Care. (1997) 13(3):186–8. doi: 10.1097/00006565-199706000-00003
19. Lee SH, Frey M, Kerrey BT, Zhang Y, Byczkowski T, Geis GL. A video-based, case-control study of factors associated with intraosseous catheterization during pediatric resuscitation. Ann Emerg Med. (2020) 75(6):755–61. doi: 10.1016/j.annemergmed.2019.09.005
20. Bhattacharyya M, Kalra V, Gulati S. Intranasal midazolam vs rectal diazepam in acute childhood seizures. Pediatr Neurol. (2006) 34(5):355–9. doi: 10.1016/j.pediatrneurol.2005.09.006
21. Mahmoudian T, Zadeh MM. Comparison of intranasal midazolam with intravenous diazepam for treating acute seizures in children. Epilepsy Behav. (2004) 5(2):253–5. doi: 10.1016/j.yebeh.2004.01.003
22. Glauser T, Shinnar S, Gloss D, Alldredge B, Arya R, Bainbridge J, et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the guideline committee of the American epilepsy society. Epilepsy Curr. (2016) 16(1):48–61. doi: 10.5698/1535-7597-16.1.48
23. Suominen PK, Nurmi E, Lauerma K. Intraosseous access in neonates and infants: risk of severe complications—a case report. Acta Anaesthesiol Scand. (2015) 59(10):1389–93. doi: 10.1111/aas.12602
24. Philbeck TE, Puga TA, Montez DF, Davlantes C, DeNoia EP, Miller LJ. Intraosseous vascular access using the EZ-IO can be safely maintained in the adult proximal humerus and proximal tibia for up to 48 h: report of a clinical study. J Vasc Access. (2022) 23(3):339–47. doi: 10.1177/1129729821992667
25. Olaussen A, Williams B. Intraosseous access in the prehospital setting: literature review. Prehosp Disaster Med. (2012) 27(5):468–72. doi: 10.1017/S1049023X12001124
26. Szarpak L, Ladny JR, Dabrowski M, Ladny M, Smereka J, Ahuja S, et al. Comparison of 4 pediatric intraosseous access devices: a randomized simulation study. Pediatr Emerg Care. (2020) 36(10):e568–72. doi: 10.1097/PEC.0000000000001587
27. Bielski K, Szarpak L, Smereka J, Ladny JR, Leung S, Ruetzler K. Comparison of four different intraosseous access devices during simulated pediatric resuscitation. A randomized crossover manikin trial. Eur J Pediatr. (2017) 176(7):865–71. doi: 10.1007/s00431-017-2922-z
Keywords: critical care, pediatric emergency care, pediatric intensive care, vascular access, intraosseous access, resuscitation, pediatric
Citation: Pfeiffer D, Olivieri M, Brenner S, Gomes D, Lieftüchter V and Hoffmann F (2023) Factors influencing the success and complications of intraosseous access in pediatric patients—a prospective nationwide surveillance study in Germany. Front. Pediatr. 11:1294322. doi: 10.3389/fped.2023.1294322
Received: 14 September 2023; Accepted: 14 November 2023;
Published: 29 November 2023.
Edited by:
Thomas Schaible, University Medical Centre Mannheim, University of Heidelberg, GermanyReviewed by:
Frank Eifinger, University Hospital of Cologne, GermanyDominique Singer, University Medical Center Hamburg-Eppendorf, Germany
© 2023 Pfeiffer, Olivieri, Brenner, Gomes, Lieftüchter and Hoffmann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Florian Hoffmann Zmxvcmlhbi5ob2ZmbWFubkBtZWQudW5pLW11ZW5jaGVuLmRl
 Daniel Pfeiffer
Daniel Pfeiffer Martin Olivieri
Martin Olivieri Sebastian Brenner
Sebastian Brenner Delphina Gomes
Delphina Gomes Victoria Lieftüchter1
Victoria Lieftüchter1 Florian Hoffmann
Florian Hoffmann