- 1Department of Microbiology, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran
- 2Wellcome-Wolfson Institute for Experimental Medicine, Queen’s University Belfast, Belfast, United Kingdom
- 3Neonatal and Children’s Hospital Research Centre, Golestan University of Medical Sciences, Gorgan, Iran
- 4Department of Pediatric and Adolescent Health, University of Botswana, Gaborone, Botswana
- 5Division of Paediatric and Adolescent Medicine, Institute of Clinical Medicine, University of Oslo, Oslo, Norway
- 6Infectious Diseases Research Center, Golestan University of Medical Sciences, Gorgan, Iran
Acute respiratory tract infection (ARTI) remains a major health threat to children under five, contributing to significant morbidity and mortality worldwide. According to the World Health Organization (WHO), ARTI leads to the hospitalization of over 12 million children annually, with approximately one million fatalities, one-third of which occur in low-income countries. The respiratory tract hosts diverse microorganisms, among which pathogenic viruses and bacteria are the leading causes of ARTI. Several risk factors—including age, gender, living conditions, seasonality, and underlying diseases—can influence disease severity. Documenting detailed case series that highlight the clinical characteristics and outcomes of pediatric ARTI, particularly in children with complex underlying conditions, is essential for understanding its impact and guiding clinical decision-making. This manuscript presents a case series of eight pediatric patients from Taleghani Children's Hospital in Gorgan, northern Iran, who tragically succumbed to respiratory viral infections, offering insights into the challenges of managing severe ARTI in children.
Introduction
Acute respiratory tract infection (ARTI) is a significant health concern for children under five, causing illness and deaths worldwide (1). According to WHO, more than 12 million children are hospitalized annually due to ARTI, and around one million die. A third of the fatalities occur in low-income countries (2–4). The respiratory tract hosts a variety of microorganisms, with pathogenic respiratory viruses and bacteria being the primary causes of ARTI (5, 6). The most prevalent viruses linked to ARTIs are respiratory syncytial virus (RSV), human metapneumovirus (HMPV), influenza viruses, human parainfluenza viruses (HPIVs), human rhinovirus (HRV), and human coronaviruses (HCoVs) (7). Among them, RSV is widespread and can cause a range of clinical symptoms and manifestations, including life-threatening illnesses, particularly in high-risk cases such as infants with chronic lung disease or congenital heart disease, prematurity, and children with weakened immune systems (8).
Multiple risk factors, such as age, gender, living environment, seasonality, and underlying diseases, can significantly affect the severity of the disease (9). Publishing detailed case series, including characteristics and outcomes of ARTI in children, particularly those with complex underlying diseases, is important for describing the impact and outcomes of ARTI among children and assisting clinicians in managing complicated cases. Here, we report a case series of eight pediatric patients from Taleghani Children's Hospital in Gorgan, northern Iran, who tragically succumbed to viral respiratory infections. As all cases presented symptoms suspected to the viral respiratory infections, so the cases have been tested for respiratory viruses. This showed that infections other than RSV, such as HMPV, HRV, HPIV, and SARS-CoV-2, can lead to severe respiratory failure and fatalities in children with underlying health conditions.
Case 1
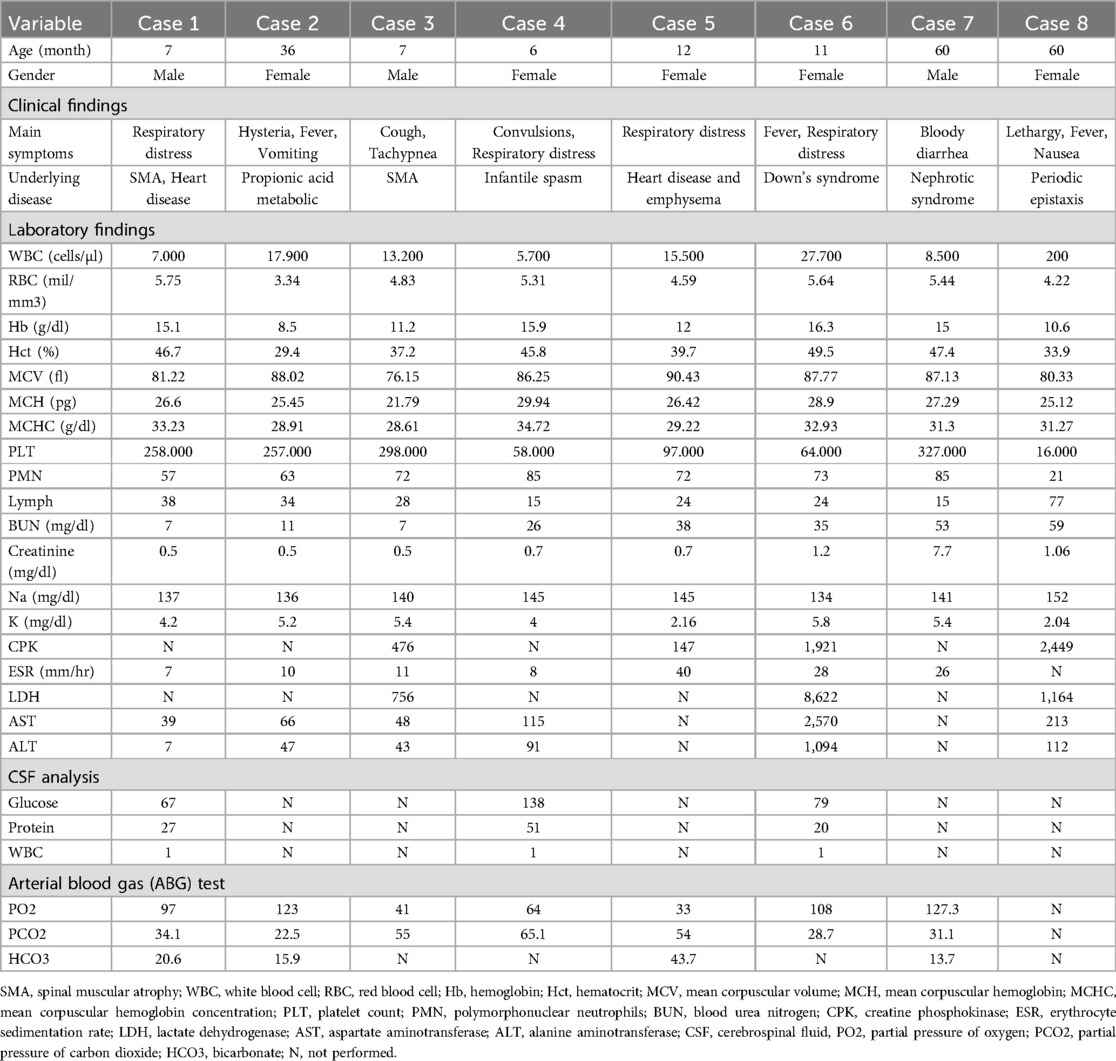
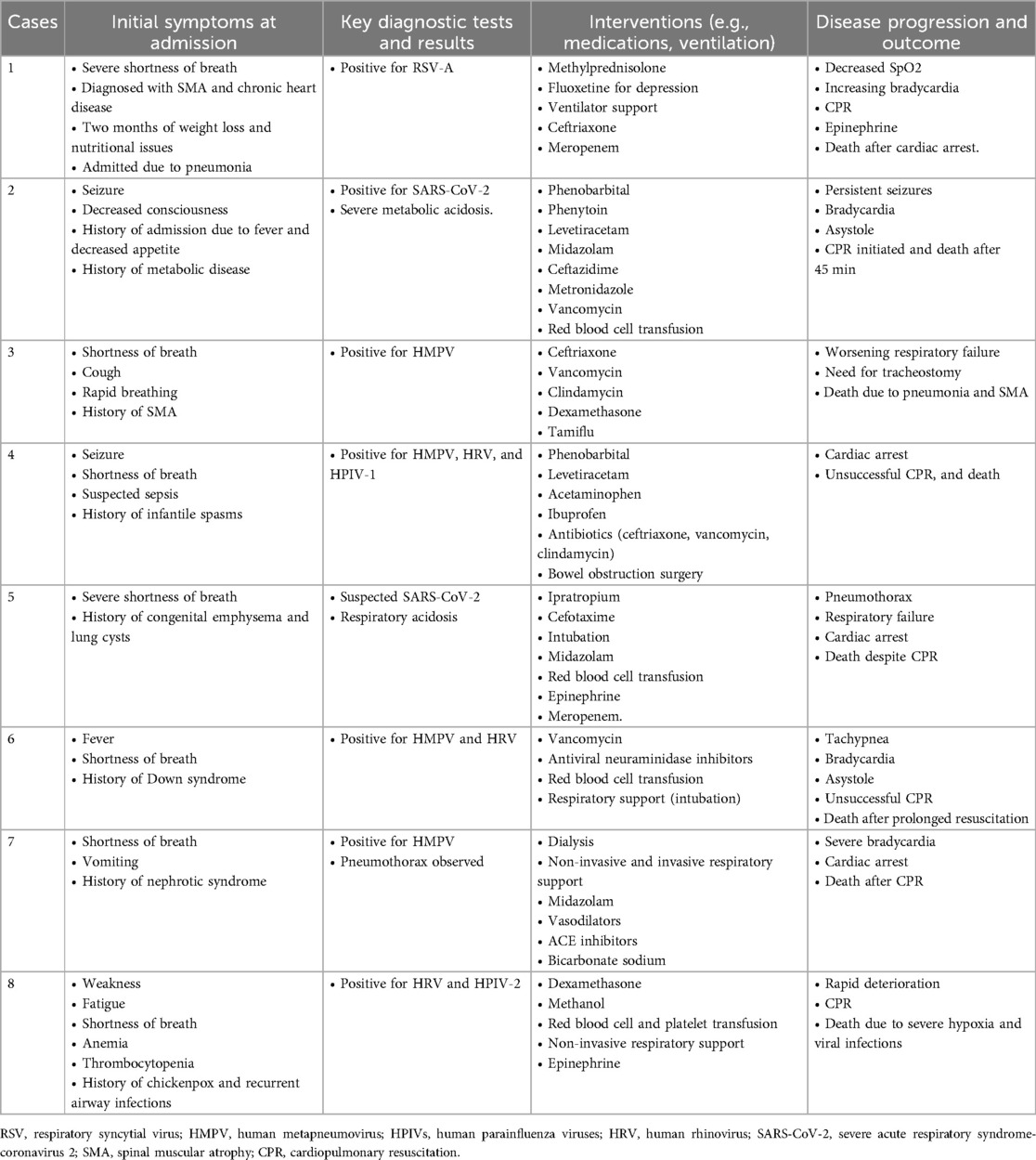
A 7-month-old boy was referred with severe respiratory distress symptoms, needing an oxygen hood. This patient was diagnosed with underlying diseases such as spinal muscular atrophy (SMA) and chronic heart disease, along with a two-month history of weight loss, feeding difficulties, and swallowing challenges. Upon admission, clinical pneumonia was diagnosed based on symptoms such as fever, cough, chest pain and weakness. His declining blood oxygen saturation (SpO2 = 90%) necessitated his transfer to the pediatric intensive care unit (PICU). On the second day, bilateral infiltration was diagnosed, after which methylprednisolone was administered, and fluoxetine was initiated for depression and panic attacks. The test results of SARS-CoV-2 and influenza were negative. Four days later, he experienced renewed respiratory distress, with SpO2 dropping to 95% and presenting a mild fever. Consequently, he was placed on a ventilator. The patient was treated with ceftriaxone, meropenem, and fluoxetine spray to reduce inflammation and mucus production in the lungs and improve breathing and oxygenation, along with 7% saline to help clear mucus and sputum from the airways. The use of fluoxetine was based on the infant's severe irritability and panic-like episodes, which were difficult to diagnose in such a young child. While fluoxetine is not FDA-approved for infants, it was prescribed off-label due to the absence of suitable alternatives and expert clinical judgment. The risks, including potential side effects, were closely monitored, and the decision was made after careful evaluation of the symptoms and treatment needs. On the eighth day of his hospitalization, his symptoms abated, and he regained alertness. Three days later, he developed a fever, and meropenem was continued, and vancomycin was added. His SpO2 was now 95%. Two days later, his oxygen levels and hemoglobin (Hb = 8 g/dl) decreased, and he received a blood transfusion. On the 14th day, he deteriorated, needing mask and bag resuscitation and administration of five doses of epinephrine due to bradycardia. Despite undergoing cardiopulmonary resuscitation (CPR), the patient ultimately passed away after a gradual decline in SpO₂, worsening bradycardia, and subsequent cardiac arrest. Of note, the nasopharyngeal swab tested positive for RSV-A. Further information and laboratory findings are shown in Table 1.
Case 2
A 3-year-old girl with propionic acid metabolic disease and speech problems was admitted with symptoms of convulsions, bilateral eyelid twitching, and decreased level of consciousness. This admission occurred after a previous hospital stay nine days earlier, during which she exhibited symptoms including fever and diminished appetite. At admission, the patient experienced increasing upper limb tremors, unresponsive pupils, fever, and frequent vomiting, which was controlled by subsequently prescribing phenobarbital, phenytoin, and levetiracetam during the second to third days of hospitalization. She then experienced frequent seizures despite continuous midazolam infusion for 5 days. On the fourth day, the patient developed respiratory distress with oxygen desaturation. Her respiratory rate increased (at 35 breaths per minute) with severe recessions, and the arterial blood gas analysis revealed a diagnosis of severe metabolic acidosis (values for HCO3− 4.2 mEq/L, PH 7.07, BE −26 mEq/L, PCO2 14.6 mmHg). Bicarbonate infusion was administered, and the O2 saturation increased to 98%. A test for SARS-CoV-2 came back positive, and treatment with ceftazidime was continued. The following day, a central venous catheter was placed, and the patient began treatment with metronidazole and vancomycin, along with a packed red blood cell transfusion. Seizures and decreased level of consciousness continued during the next 4 days. On the 10th day of hospitalization, the patient received a regimen that included fresh frozen plasma, vitamin K, continued meropenem, amikacin, ceftriaxone, and a dopamine infusion to prevent complications and secondary infections. On the next day, the patient's general condition did not change, and she was intubated. The next day, the patient had bleeding from the mouth, and fresh frozen plasma was prescribed. On the 15th day of the hospital stay, the patient was severely bradycardic (at 34 breaths per minute), and CPR was initiated. After 45 min, resuscitation was stopped due to a lack of return of spontaneous circulation (ROSC).
Case 3
A 7-month-old boy with an underlying condition of SMA was admitted to the hospital due to symptoms of shortness of breath, cough, and rapid breathing that had persisted for the past four days without outpatient treatment response. The child had received vaccinations up to the age of two months but had displayed unfavourable growth and developmental patterns. On the first day of hospitalization, ceftriaxone, vancomycin, clindamycin and dexamethasone were provided to treat bacterial infection and reduce inflammation. On the second day, the SpO2 decreased to 84%, and he was transferred to PICU, where oxygen supplementation via an oxygen hood resulted in an increase in oxygen saturation to 95%. Clindamycin and cefotaxime treatments were continued. The following day, productive coughs developed as well as bradycardia [Respiratory Rate (RR) = 60, Puls Rate (PR) = 170, and temperature (Tm) = 37]. CPR with cardiac massage was performed, and the patient was revived. On the seventh hospital day, due to further deterioration, the patient's treatment plan was adjusted to include clindamycin and an antiviral neuraminidase inhibitor (Tamiflu). Within a few days, the patient was still breathing with the help of an oxygen hood. On the 18th hospital day, a culture from the endotracheal tube (ETT) returned positive for Pseudomonas aeruginosa, which was sensitive to ciprofloxacin, prompting a resumption of treatment with ciprofloxacin and meropenem, and amikacin and ciprofloxacin was stopped. Ten days later, the patient's condition severely deteriorated, mask-bag ventilation was ineffective, a tracheostomy was placed, and the patient received another transfusion of red blood cells. Notably, the nasopharyngeal swab became positive for HMPV. Four days later, the patient died due to pneumonia, hospital-acquired infection, and the underlying SMA disease.
Case 4
A 6-month-old female was admitted with convulsions and respiratory distress; fever and sepsis were suspected. The patient had a history of infantile spasms three weeks before admission and episodes of staring and eye rotation 5–6 times daily, worsening in frequency since age two months. At age 4 months, the patient was hospitalized because growth and developmental milestones were delayed and routine vaccinations were incomplete. Upon admission, phenobarbital and levetiracetam were prescribed to control seizures. She experienced fever, runny nose, and decreasing SpO2 which improved to 90% with oxygen supplementation. On the second day of hospitalization, her condition worsened, with significant respiratory distress and a decrease in oxygen saturation. She tested positive for HMPV, HRV and HPIV-1, and anti-inflammatory medication was started (Acetaminophen and Ibuprofen). The patient exhibited significant rectal bleeding, prompting an abdominal ultrasound and computed tomography (CT) scan that showed intestinal obstruction and intussusception. The next day, the patient underwent surgery. Two days postsurgery, infectious secretions were seen on the surgical site, and the culture test was positive for Pseudomonas aeruginosa, so antibiotic therapy with ceftriaxone, vancomycin, and clindamycin was commenced. Then the patient experienced a SpO2 decrease, the severity of respiratory symptoms, and cardiac arrest was noted. CPR was unsuccessful, and the patient died due to pneumonia and simultaneous infection of three viruses.
Case 5
A one-year-old girl was admitted with a history of left congenital emphysema and a right lung cyst. One week prior to admission, the patient experienced severe respiratory distress, and SARS-CoV-2 infection was suspected with no test performed. She was on continuous oxygen therapy for the past four months prior to admission, and shortly before admission, she experienced enhanced cyanosis. She was born prematurely, and her growth was stunted despite being nourished with formula milk. On the day of admission, the patient presented as pale, with tachypnea, cyanosis, and a runny nose. Ipratropium (Etruvent) and cefotaxime spray were provided, but due to a gasping breathing pattern and metabolic acidosis, she was intubated and transferred to the PICU. CPR was performed after a few hours because of poor perfusion with non-measurable blood pressure, so dopamine and midazolam infusions were initiated, as well as transfusion of red blood cells and fresh frozen plasma. In the following hours, SpO2 decreased to 65%. She developed a fever (Tm 39℃), and vancomycin was initiated. Her acidotic condition worsened (values for HCO3− 15.2 mEq/L, PH 7.27, PCO2 33.1 mmHg). The next day, meropenem was added as well as epinephrine, to improve perfusion and her haemodynamic condition. On the fourth hospital day, she deteriorated with pneumothorax and air was evacuated with pleural drainage. Then, SpO2 declined to 30%. She developed bradycardia followed by cardiac arrest. After admission, respiratory viral test were negative. CPR did not result in ROSC, and she demised.
Case 6
An 11-month-old girl diagnosed with trisomy 21 was admitted with fever (T = 39.5°C) and respiratory distress with influenza-like sympthoms. She had experienced fever for the past six days and productive coughing for the last two days before admission. She had been provided with acetaminophen to reduce fever for five days before admission. At admission, she was hypoxic (SpO2 = 78, PR = 150, Tm = 39.5), was intubated, put on a ventilator, and vancomycin was provided. The fever and tachypnea persisted, an antiviral neuraminidase inhibitor was added on the second day, and anaemia (transfused with red blood cells), leukocytosis, thrombocytopenia, and elevated lactate dehydrogenase (LDH) levels were noted. Then, bradycardia and asystole developed. Notably, the nasopharyngeal swab became positive for HMPV and HRV. Her respiratory condition deteriorated rapidly, with persistent fever, tachypnea, and hypoxia. The infections exacerbated her symptoms, resulting in bradycardia, asystole, and eventual death despite prolonged resuscitation attempts. During CPR, administration of epinephrine and bicarbonate were done every 3–5 min, but ROSC was not achieved, and she demised.
Case 7
A 5-year-old boy was admitted with respiratory distress and vomiting. The patient had a history of nephrotic syndrome and underwent dialysis 3 times a week. Ultrafiltration dialysis was performed on the first day of hospitalization and repeated 2 days later. Non-invasive respiratory support and oxygen supplementation were administered due to cardiorespiratory depression. He was persistently hypoxic (SpO2 77%) and, therefore, was put on invasive respiratory support. Pneumothorax was also observed in the requested graphs. Subsequently, midazolam was prescribed to treat respiratory depression. To relieve his hypertension (BP 139/99) and to help relax the blood vessels, a vasodilating drug (hydralazine), an ACE inhibitor (enalapril), and a Ca2+ blocker were provided, as well as sodium bicarbonate due to respiratory acidosis (HCO3− 12.2 mEq/L, PH 7.33, PO2 113 mmHg, PCO2 23.4 mmHg). The nasopharyngeal swab became positive for HMPV. The following day, he experienced severe bradycardia, leading to cardiac arrest, and unfortunately, he passed away 45 min after CPR was initiated.
Case 8
A 5-year-old girl was admitted due to weakness, lethargy, respiratory distress, nausea and vomiting. She was anaemic and thrombocytopenic and was transfused with red blood cells and platelets. Prior to admission, she had the experience of periodic epistaxis that was not satisfactorily investigated, as well as poor growth and development. At age 1.5 years, she had chicken pox and then experienced frequent upper airway infections. At admission, she deteriorated, became unconscious and was transferred to the PICU for further monitoring and treatment. An emergency brain CT revealed herniation and an occipital mass. Dexamethasone and a course of methanol were initiated to relieve intracranial pressure. She required respiratory support and supplementation of oxygen; thus, non-invasive ventilation was initiated. On the second day, she received FFP and platelets due to the drop in haemoglobin (7 g/dl) and platelets (5,000 μl). She developed hypotension (blood pressure 98/54) and received an epinephrine infusion. Subsequently, severe hypoxia (SpO2 60%) occurred the following day. The patient's test results came back positive for HRV and HPIV-2. The infections led to the rapid deterioration of her condition, culminating in severe hypoxia and the need for resuscitation. The following day, her condition deteriorated significantly. CPR was initiated but was unsuccessful, and she passed away.
Discussion
Acute respiratory infections are a significant health concern for infants and children under five, primarily caused by respiratory viruses such as RSV, HMPV, SARS-CoV-2, HRV, and influenza (10–12). These infections manifest in a range of symptoms, from mild cold-like illness to severe bronchiolitis and pneumonia (10, 13), often necessitating hospitalization (13). WHO estimated that 1.9–2.2 million infants and children die due to respiratory infections every year worldwide (14). The severity of the infection can vary depending on the specific virus, the child's age, and any underlying health conditions (13). Among the various respiratory viruses linked to complications in infants and young children, RSV emerges as the predominant cause of bronchiolitis and pneumonia within the first year of life (15). While most children are infected by age two, it can cause severe lower respiratory tract infections, especially in infants (16). HMPV infections often present with similar symptoms to RSV, including cough, nasal congestion, and wheezing, and can also lead to pneumonia (17). It is an important cause of lower respiratory tract infections in children (18). While many children experience mild illness, HMPV can cause severe disease, especially in premature infants and children with underlying health conditions (19). HRVs is a common cause of the common cold and upper respiratory tract infections (12). While typically mild, it can sometimes lead to lower respiratory tract infections, especially in infants and young children (18). Influenza can cause a range of respiratory illnesses, from mild to severe (10). While generally less severe than RSV in very young children, influenza can still lead to serious complications like pneumonia (18).
The COVID-19 pandemic has ushered in profound shifts in human behaviour and society, which has influenced the incidence of non-SARS-CoV-2 respiratory viruses (20). Recent studies indicate that public health measures implemented during the COVID-19 pandemic significantly impacted the circulation patterns of these viruses, leading to altered seasonal distributions and potentially affecting long-term immunity patterns in vulnerable populations (21). Despite the diversity of pathogens associated with acute respiratory infections, the clinical presentation often appears strikingly similar across cases (14). Therefore, the precise identification of causative factors becomes paramount in guiding effective treatment strategies. The purpose of this study is to investigate the causes of respiratory failure in children under 5 years old who have presented with respiratory symptoms. The study aims to identify the underlying causes of respiratory failure in these children, with a focus on viral infections, pneumothorax, and other factors that may contribute to respiratory failure (Table 2). The study also aims to provide insights into the clinical presentation of respiratory failure in children under 5 years old and to identify potential strategies for prevention and treatment.
This investigation scrutinized eight pediatric cases of children below 5 who presented with acute respiratory symptoms necessitating hospitalization, culminating in fatalities over 5 months from October 2021 to March 2022 in a northern city in Iran. All cases, including three boys and five girls, had underlying diseases, which serve as risk factors for fatal outcomes due to severe respiratory disease, as outlined in Table 1. According to recent research, gender and age significantly influence the risk and severity of respiratory infections in children under five years. Male infants are notably more susceptible, being 55% more likely to develop severe respiratory infections compared to female infants (22). Regarding age distribution, infants under 11 months bear the highest risk, comprising approximately 83% of RSV-positive cases, while children aged 1–2 years account for 9.2% of infections. The clinical manifestations also vary by age, with bronchiolitis (57.5%) and pneumonia (30.8%) being the most common presentations requiring intensive care unit admission (23). Of note, a 7-month-old boy (case 1) was RSV infected, while another was diagnosed with SARS-CoV-2 (case 2), and one had a suspected SARS-CoV-2 infection a week before admission (case 5). This underlines the significance of diagnosing respiratory viral infections in pediatric patients, in line with previous studies (24, 25). Importantly, HMPV (cases 3, 4, 6, and 7), HRV (cases 4, 6, and 8) and HPIV-1 and 2 infections were diagnosed for cases 4 and 8, respectively. Three cases (cases 4, 6, and 8) had co-infections with two viruses. Co-infections can exacerbate disease severity by increasing viral load, triggering excessive immune responses, and impairing the host's ability to control the infection. Additionally, interactions between viruses could enhance viral replication or suppress immune defenses, further worsening clinical outcomes. Co-infections can exacerbate inflammation in the respiratory tract, potentially leading to increased symptom severity, prolonged illness, and a higher risk of complications like pneumonia (26). The interaction between different viruses can also alter immune responses, making the body more susceptible to secondary bacterial infections (26). Further research is needed to fully understand the complex interplay of viruses in co-infections and their precise effects on the body (27). Also, a clinically suspected infection (case 7) led to pneumothorax, and a history of chickenpox virus infection (case 8) that subsequently experienced multiple episodes of respiratory disease. It seems that many symptom-oriented interventions were being carried out in the cases while the aetiology of the disease remained unclear. So, several of these interventions may exacerbated the already disrupted homeostasis of the body.
Among these patients, information regarding the mode of delivery (vaginal birth or cesarean section) was only available for cases 1, 3, 4, and 7, all of which were delivered by cesarean section, while data on this aspect was insufficient for the remaining cases. Cesarean section may increase the risk of respiratory infections in newborns due to the lack of exposure to the mother's vaginal microbiome, which is crucial for immune system development. Additionally, cesarean-born infants may experience impaired lung fluid clearance, leading to respiratory issues. Studies have shown a higher incidence of respiratory diseases, such as bronchiolitis and asthma, in cesarean-delivered infants compared to those born vaginally (28). Two cases had incomplete routine vaccine coverage, emphasizing the role of vaccination in bolstering the immune system, reducing infection rates, and mitigating symptom severity (29). In accordance with previous papers, being born prematurely influences the occurrence and severity of symptoms (30). Children with underlying diseases, including congenital heart disease (cases 1 and 5), SMA (cases 1 and 3), a history of infantile spasms (case 4), trisomy 21 (case 6), underlying nephrotic syndrome needing regular dialysis (case 7), and metabolic disease (case 2), were all Immunocompromised with an inability to clear respiratory tract infections and therefore at increased risk of fatal outcome.
Overally, a total of 411 infants and young children under five years of age presenting with acute respiratory infections were admitted between October 2021 and March 2022. Among these cases, eight patients passed away. Notably, this sample population was drawn exclusively from the single specialized pediatric hospital serving the metropolitan area. This investigation coincided with the post-COVID-19 pandemic era, which potentially influenced circulating respiratory virus patterns and immune system responses. Our analysis revealed that beyond RSV, various other respiratory viruses, including HMPV, HRV, HPIV, and SARS-CoV-2, contributed significantly to disease severity and mortality in neonatal populations.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was approved by the science and bioethics committee of Golestan University of Medical Sciences (IR.GOUMS.REC.1401.023). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the minor(s)' legal guardian for the publication of any potentially identifiable images or data included in this article.
Author contributions
MR: Data curation, Investigation, Writing – original draft, Writing – review & editing. SS: Writing – original draft, Writing – review & editing. ME: Writing – original draft, Writing – review & editing. LB: Data curation, Writing – original draft, Writing – review & editing. BN: Writing – original draft, Writing – review & editing. AT: Conceptualization, Investigation, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors appreciate the support of the Research Deputy at Golestan Medical University (112519).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ARTI, acute respiratory tract infection; RSV, respiratory syncytial virus; HMPV, human metapneumovirus; HPIVs, human parainfluenza viruses; HRV, human rhinovirus; HCoVs, human coronaviruses; SARS-CoV-2, severe acute respiratory syndrome-coronavirus 2; SMA, spinal muscular atrophy; PICU, pediatric intensive care unit; CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation; ETT, endotracheal tube; CT, computed tomography; LDH, lactate dehydrogenase.
References
1. Tahamtan A, Samadizadeh S, Rastegar M, Nakstad B, Salimi V. Respiratory syncytial virus infection: why does disease severity vary among individuals? Expert Rev Respir Med. (2020) 14(4):415–23. doi: 10.1080/17476348.2020.1724095
2. Niu H, Wang R, Jia Y-t, Cai Y. Pidotimod, an immunostimulant in pediatric recurrent respiratory tract infections: a meta-analysis of randomized controlled trials. Int Immunopharmacol. (2019) 67:35–45. doi: 10.1016/j.intimp.2018.11.043
3. Organization WH, UNICEF. Ending Preventable Child Deaths from Pneumonia and Diarrhoea by 2025 the Integrated Global Action Plan for Pneumonia and Diarrhoea (GAPPD). Geneva, Switzerland: WHO (2013). Available at: http://www who int/maternal_child_adolescent/documents/global_action_plan_pneumonia_diarrhoea/en. 2019
4. Tazinya AA, Halle-Ekane GE, Mbuagbaw LT, Abanda M, Atashili J, Obama MT. Risk factors for acute respiratory infections in children under five years attending the Bamenda Regional Hospital in Cameroon. BMC Pulm Med. (2018) 18(1):7. doi: 10.1186/s12890-018-0579-7
5. Echavarría M, Marcone DN, Querci M, Seoane A, Ypas M, Videla C, et al. Clinical impact of rapid molecular detection of respiratory pathogens in patients with acute respiratory infection. J Clin Virol. (2018) 108:90–5. doi: 10.1016/j.jcv.2018.09.009
6. Meskill SD, Bryant O, C S. Respiratory virus co-infection in acute respiratory infections in children. Curr Infect Dis Rep. (2020) 22(1):3. doi: 10.1007/s11908-020-0711-8
7. Principi N, Bosis S, Esposito S. Human metapneumovirus in paediatric patients. Clin Microbiol Infect. (2006) 12(4):301–8. doi: 10.1111/j.1469-0691.2005.01325.x
8. Walsh EE, Hall CB. Respiratory syncytial virus (RSV). In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. Elsevier (2015). p. 1948–60.e3. doi: 10.1016/B978-1-4557-4801-3.00160-0
9. Dagne H, Andualem Z, Dagnew B, Taddese AA. Acute respiratory infection and its associated factors among children under-five years attending pediatrics ward at University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia: institution-based cross-sectional study. BMC Pediatr. (2020) 20(1):93. doi: 10.1186/s12887-020-1997-232111196
10. Hon K-L, Leung AK. Severe childhood respiratory viral infections. Adv Pediatr. (2009) 56(1):47. doi: 10.1016/j.yapd.2009.08.019
11. da Silva RP, Thomé BL, da Souza APD. Exploring the immune response against RSV and SARS-CoV-2 infection in children. Biology (Basel). (2023) 12(9):1223. doi: 10.3390/biology12091223
12. Tregoning JS, Schwarze J. Respiratory viral infections in infants: causes, clinical symptoms, virology, and immunology. Clin Microbiol Rev. (2010) 23(1):74–98. doi: 10.1128/CMR.00032-09
13. Simões EA, Bont L, Manzoni P, Fauroux B, Paes B, Figueras-Aloy J, et al. Past, present and future approaches to the prevention and treatment of respiratory syncytial virus infection in children. Infect Dis Ther. (2018) 7:87–120. doi: 10.1007/s40121-018-0188-z
14. Bhuyan GS, Hossain MA, Sarker SK, Rahat A, Islam MT, Haque TN, et al. Bacterial and viral pathogen spectra of acute respiratory infections in under-5 children in hospital settings in Dhaka city. PLoS One. (2017) 12(3):e0174488. doi: 10.1371/journal.pone.0174488
15. Diaz-Diaz A, Garcia-Maurino C, Jordan-Villegas A, Naples J, Ramilo O, Mejias A. Viral bacterial interactions in children: impact on clinical outcomes. Pediatr Infect Dis J. (2019) 38(6S):S14–S9. doi: 10.1097/INF.0000000000002319
16. Baker RE, Mahmud AS, Wagner CE, Yang W, Pitzer VE, Viboud C, et al. Epidemic dynamics of respiratory syncytial virus in current and future climates. Nat Commun. (2019) 10(1):5512. doi: 10.1038/s41467-019-13562-y
17. Mullins JA, Erdman DD, Weinberg GA, Edwards K, Hall CB, Walker FJ, et al. Human metapneumovirus infection among children hospitalized with acute respiratory illness. Emerg Infect Dis. (2004) 10(4):700. doi: 10.3201/eid1004.030555
18. Pavia AT. Viral infections of the lower respiratory tract: old viruses, new viruses, and the role of diagnosis. Clin Infect Dis. (2011) 52(suppl_4):S284–S9. doi: 10.1093/cid/cir043
19. Pancham K, Sami I, Perez GF, Huseni S, Kurdi B, Rose MC, et al. Human metapneumovirus infection is associated with severe respiratory disease in preschool children with history of prematurity. Pediatr Neonatol. (2016) 57(1):27–34. doi: 10.1016/j.pedneo.2015.03.008
20. Chow EJ, Uyeki TM, Chu HY. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat Rev Microbiol. (2023) 21(3):195–210. doi: 10.1038/s41579-022-00807-9
21. Maglione M, Tipo V, Barbieri E, Ragucci R, Ciccarelli AS, Esposito C, et al. Changes in respiratory viruses’ activity in children during the COVID-19 pandemic: a systematic review. J Clin Med. (2025) 14(4):1387. doi: 10.3390/jcm14041387
22. Korsun N, Trifonova I, Madzharova I, Alexiev I, Uzunova I, Ivanov I, et al. Resurgence of respiratory syncytial virus with dominance of RSV-B during the 2022–2023 season. Front Microbiol. (2024) 15:1376389. doi: 10.3389/fmicb.2024.1376389
23. Jallow MM, Diagne MM, Sagne SN, Tall F, Diouf JBN, Boiro D, et al. Respiratory syncytial virus in pediatric patients with severe acute respiratory infections in Senegal: findings from the 2022 sentinel surveillance season. Sci Rep. (2023) 13(1):20404. doi: 10.1038/s41598-023-47015-w
24. Cheraghali F, Barati L, Amanian D, Shahkar L, Najafinejad M, Naziri H, et al. A case series of pediatric COVID-19 with complicated symptoms in Iran. Future Virol. (2021) 16(10):649–56. doi: 10.2217/fvl-2021-0091
25. Ramzali M, Salimi V, Cheraghali F, Hosseini SD, Yasaghi M, Samadizadeh S, et al. Epidemiology and clinical features of respiratory syncytial virus (RSV) infection in hospitalized children during the COVID-19 pandemic in Gorgan, Iran. Health Sci Rep. (2024) 7(1):e1787. doi: 10.1002/hsr2.1787
26. Crotty MP, Meyers S, Hampton N, Bledsoe S, Ritchie DJ, Buller RS, et al. Impact of antibacterials on subsequent resistance and clinical outcomes in adult patients with viral pneumonia: an opportunity for stewardship. Critical Care. (2015) 19:1–11. doi: 10.1186/s13054-015-1120-5
27. Asner S, Rose W, Petrich A, Richardson S, Tran D. Is virus coinfection a predictor of severity in children with viral respiratory infections? Clin Microbiol Infect. (2015) 21(3):264. e1–. e6. doi: 10.1016/j.cmi.2014.08.024
28. Sevelsted A, Stokholm J, Bønnelykke K, Bisgaard H. Cesarean section and chronic immune disorders. Pediatrics. (2015) 135(1):e92–e8. doi: 10.1542/peds.2014-0596
29. Piot P, Larson HJ, O’Brien KL, N’kengasong J, Ng E, Sow S, et al. Immunization: vital progress, unfinished agenda. Nature. (2019) 575(7781):119–29. doi: 10.1038/s41586-019-1656-7
Keywords: case series, viral respiratory infections, pediatric failure, acute respiratory tract infection, Iran
Citation: Ramzali M, Samadizadeh S, Ebrahimi M, Barati L, Nakstad B and Tahamtan A (2025) Case Report: Pediatric respiratory viral infection failure: a case series of eight fatalities in children under 5 years old in Iran. Front. Pediatr. 13:1396142. doi: 10.3389/fped.2025.1396142
Received: 5 March 2024; Accepted: 22 April 2025;
Published: 9 May 2025.
Edited by:
Ramos Amador Jose T., Complutense University of Madrid, SpainReviewed by:
Hadi Ghaffari, Semnan University of Medical Sciences, Semnan, IranHamed Naziri, Thomas Jefferson University, United States
Copyright: © 2025 Ramzali, Samadizadeh, Ebrahimi, Barati, Nakstad and Tahamtan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alireza Tahamtan, RHIudGFoYW10YW5AZ291bXMuYWMuaXI=; QWxpcmV6YS50bW5AZ21haWwuY29t
 Mahnaz Ramzali
Mahnaz Ramzali Saeed Samadizadeh2
Saeed Samadizadeh2 Britt Nakstad
Britt Nakstad Alireza Tahamtan
Alireza Tahamtan