- 1Department of Paediatrician, Women’s and Children’s Hospital of Ningbo University, Ningbo, China
- 2Department of Paediatrician, Yuyao Maternal and Child Health Centre, Yuyao, China
- 3Department of Scientific Research, Women’s and Children’s Hospital of Ningbo University, Ningbo, China
Background: Pediatric renal abscesses is a severe infectious disease with a long treatment period. Due to atypical symptoms, there is a risk of delayed diagnosis, missed diagnosis, and misdiagnosis. Inadequate or incomplete treatment can lead to prolonged hospital stays, even Irreversible kidney damage. This study aimed to analyze the clinical characteristics of pediatric renal abscesses, aiming for early diagnosis and timely, appropriate treatment.
Methods: A retrospective analysis was conducted on clinical manifestations, laboratory tests, imaging studies, and treatment data of 12 pediatric renal abscess cases treated in the Nephrology Department of our hospital from October 2018 to March 2023.
Results: Among the 12 cases, there were 3 males and 9 females, aged between 7 months to 12 years. All cases were from urban areas, with fever being the primary symptom (100%), accompanied in some by abdominal pain and urinary frequency/pain. Clinical symptoms were atypical, with 91% showing elevated white blood cell count(WBC), a significant rise in neutrophil percentage, C-reactive protein (CRP), and a marked increase in procalcitonin (100%). significant elevation of urinary white blood cells in 83.3% of cases. Both urine and blood cultures were negative. All 12 cases underwent abdominal CT or Magnetic Resonance Urography (MRU), showing abscesses, all less than 3 cm. Treatment included third-generation cephalosporins, with the addition of linezolid in cases where the initial treatment was ineffective. Hospital stays ranged from 10 to 21 days. Follow-up MRU showed the disappearance of abscesses.
Conclusion: Clinical symptoms of pediatric renal abscesses are atypical. Children with fever, accompanied by abdominal pain, and significant elevation in white blood cells, CRP, and PCT should be considered for renal abscess, and abdominal CT or MRU is recommended for early diagnosis. Conservative anti-infection treatment can yield good results for abscesses smaller than 3 cm.
Backgroud
Pediatric renal abscess is an acute localized purulent lesion of the renal parenchyma, which is very rare in children. Due to atypical symptoms, there is a risk of delayed diagnosis, missed diagnosis, and misdiagnosis. Inadequate or incomplete treatment can lead to prolonged hospital stays, even irreversible kidney damage,and endangering life. Compared with urinary tract infection, which is characterized by typical urinary tract irritation symptoms such as frequent urination, urgency, and painful urination, renal abscess has no specific clinical manifestations. Literature reports indicate that early diagnosis can be misidentified as respiratory infections, and even ultrasound may show localized masses mistaken for tumors. The infection pathways of renal abscess primarily involve ascending urinary tract infection or hematogenous spread, with Escherichia coli being the most common pathogen, followed by Staphylococcus in some cases. Regarding treatment, literature mainly recommends conservative management. This study aimed to analyze the clinical characteristics of pediatric renal abscesses, aiming for early diagnosis and timely, appropriate treatment.
Materials and methods
General information
This study is a retrospective analysis. The study was approved by the Hospital's Medical Ethics Committee (approval number: EC2023-011). Guardians of the children involved in the study were fully informed, consented to the research, and signed informed consent forms. Clinical data of 12 pediatric patients with renal abscesses treated in the Pediatric Nephrology Department of our hospital from October 2018 to March 2023 were collected.
Methods
Clinical data of the pediatric patients were collected through the hospital's electronic medical record system. This included a range of information such as basic details (gender, age, living environment), clinical presentations, and laboratory tests (white blood cells, neutrophil percentage, C-reactive protein, calcitonin, erythrocyte sedimentation rate, serum creatinine, urine white blood cells, urine red blood cells, urine microprotein, urine culture, blood culture). Imaging studies like MRU, abdominal CT, urinary system ultrasound, and retrograde ureterography were also reviewed, along with treatment details. Patient outcomes were gathered through telephone follow-ups and outpatient medical record systems.
Statistical analysis
Descriptive analysis was employed. Quantitative data such as age, white blood cells, neutrophil ratio, and serum creatinine were represented using the median (M) and range.Results are presented as mean ± standard deviation for continuous variables.
Results
Basic information
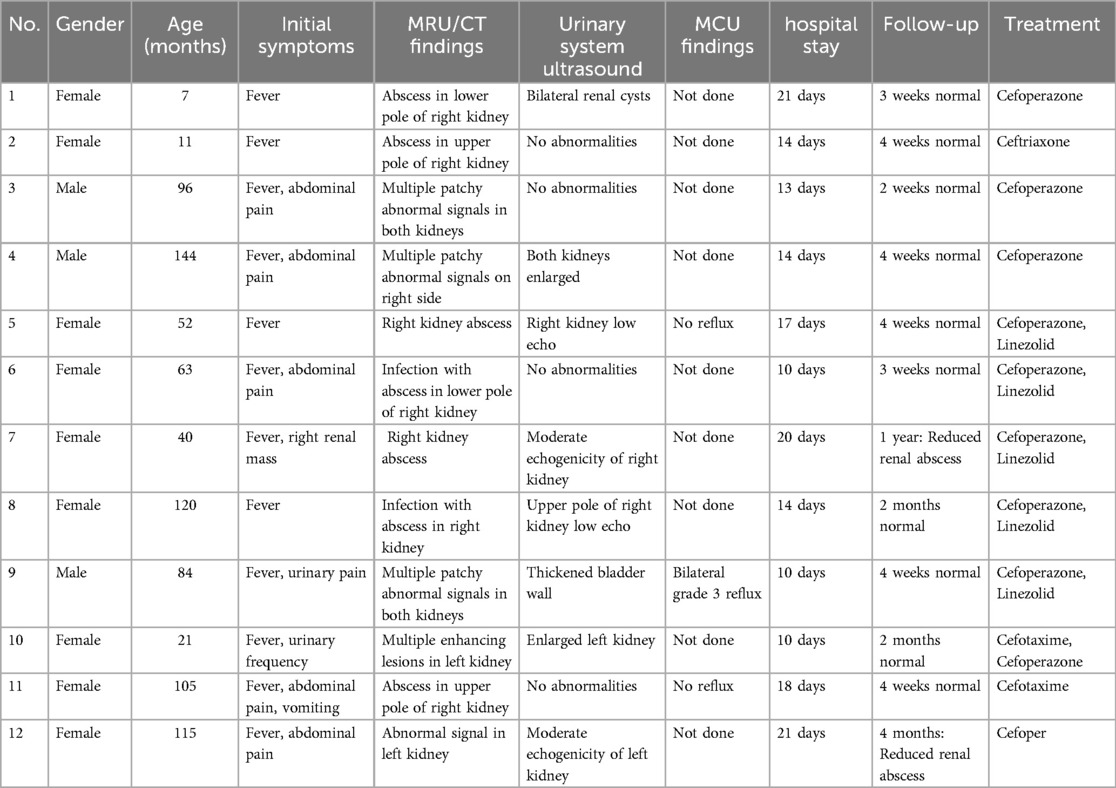
Among the 12 pediatric patients, there were 3 males and 9 females; ages ranged from 7 months to 12 years (median age 6 ± 3.86 years), including 2 cases under 1 year old (Table 1). Residential Environment: All patients came from urban areas with parents having a college degree or higher education.
Clinical symptoms
All patients primarily presented with fever (100%), predominantly high fever (body temperature ≥39°C). The duration of illness before admission was 1–8 days (median course 4 ± 0.11 days), with no history of preceding infections. Five cases were accompanied by abdominal pain, two cases exhibited urinary frequency or urinary pain, one case had a right renal mass, three cases were transferred from the gastroenterology department, and one case from the surgery department. Only one child presented with renal percussion pain (Table 1).
Laboratory and imaging examinations
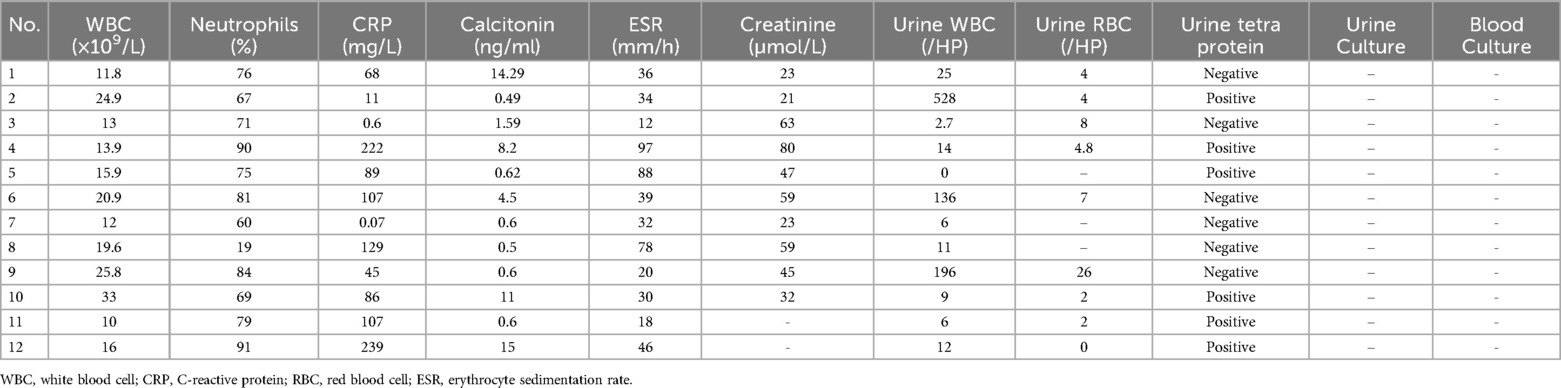
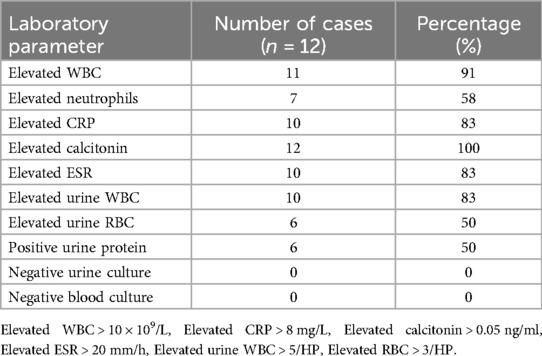
Renal ultrasound was performed on all patients upon admission, with only 4 cases (33.33%) showing renal abscesses. All 12 patients underwent abdominal CT or MRU, revealing abscesses (8 on the right side (66.67%), 2 bilateral (16.67%), and 2 on the left side (16.67%), all less than 3 cm in size). Three patients underwent Micturating Cystourethrography (MCU), of which 2 showed no reflux, and 1 exhibited bilateral grade 3 reflux (Table 1). Peripheral blood WBC ranged from (11.8 to 33) × 109/L, neutrophil percentage (N) from 67 to 91%, CRP from 11 to 239 mg/L, and calcitonin from 0.49 to 15 ng/ml. Kidney function tests showed no abnormalities. Urinalysis indicated red blood cells (RBC) ranging from 4 to 26 per HP, white blood cells (WBC) from 0 to 528 per HP, and urinary red blood cells from 0 to 26 per HP. Both urine and blood cultures were negative (Table 2). Laboratory data showed that 91% of the children had elevated white blood cell counts, with a significant increase in the proportion of neutrophils. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were markedly elevated in 66% of the cases. Calcitonin levels were significantly increased in all cases (100%). Urinalysis revealed that 83.3% of the patients had a notable increase in urinary white blood cells. Hematuria was present in 50% of the cases, and the rate of positive urinary protein was 50% (Table 3).
Treatment
Upon admission, patients were treated with third-generation cephalosporin antibiotics. This treatment was effective in 7 cases, while 5 cases showed no response and were subsequently treated with linezolid. All patients received conservative treatment. The length of hospital stay ranged from 10 to 21 days. Within 2–10 days of treatment, the children's body temperature normalized. At 2 weeks to about 1 month post-discharge, a follow-up renal MRU in 8 cases showed the disappearance of renal abscesses (Figure 1). In 2 cases, abscesses completely resolved after continued medication for 2 months post-discharge. And the total duration of palliative antibiotic therapy was 14–60 days (median course 28 ± 7.30 days).In 1 case, the abscess size reduced after 4 months, and in 1 child, a small lesion was detected during a 1-year follow-up ultrasound (with normal urinalysis). One child with reflux underwent surgical treatment and was normal at the 1-year follow-up (Table 1).
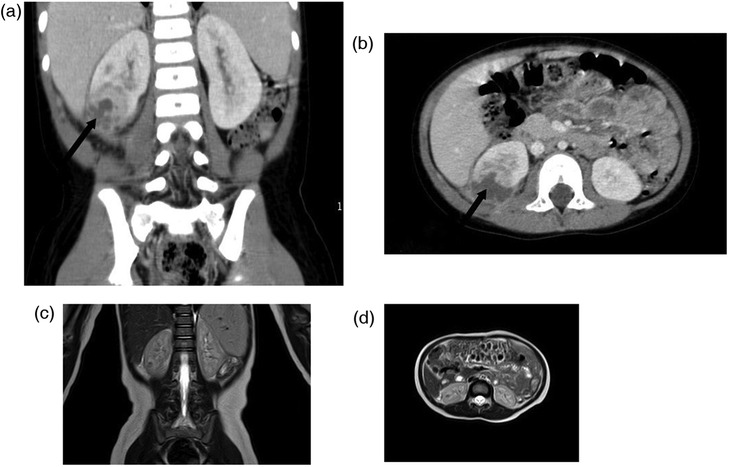
Figure 1. The changes of CT before treatment (a,b), and MRU after about 1 month of treatment (c,d) in case five. (a,b) The abscesses in lower pole of the right kidney were measured as about 2.4 × 2.7 cm (arrow), (c,d) The abscesses was largely disappeared.
Discussion
Intra-abdominal abscesses are relatively rare in children, with renal abscesses being even rarer. A retrospective analysis study found that among approximately 200,000 pediatric emergency department visits, there were only 17 cases of renal abscesses. The incidence rate is about 0.007% (1). However, it is a severe infectious disease with a long treatment period and significant damage to renal parenchyma. Due to atypical symptoms, there is a risk of delayed diagnosis, missed diagnosis, and misdiagnosis. Inadequate or incomplete treatment can lead to prolonged hospital stays (2, 3). Literature review reveals no related guidelines; diagnosis and treatment are based on adult and small-sample data, with limited case information and no unified diagnostic and therapeutic strategies (4).
Children of all ages can be affected. An 11-year literature retrospective study found that the age of onset ranged from 1 month to 18 years, more common in girls (2, 4, 5), though some reports indicate a higher proportion in boys (6, 7). Our data show that the age of affected children in our group ranged from 7 months to 12 years (median age 6 ± 3.86 years), with a higher proportion in girls. This suggests that renal abscesses may not have a significant gender difference. Additionally, whether the incidence of renal abscesses is related to residential areas and living environments is unclear. Our group of children all came from urban areas, with parents having college-level education or higher, and living in good environmental conditions. This suggests that the occurrence of renal abscesses may not be related to living environments, but further accumulation of clinical data is needed for observation.
The clinical presentation of pediatric renal abscesses lacks specificity. Most cases present with fever as the main clinical manifestation, while some children experience back pain, abdominal pain, and abdominal masses (8, 9). Thus, patients are not initially admitted to nephrology or urology departments but are dispersed in other departments, such as initially being admitted to gastroenterology, general surgery, or other pediatric departments, diagnosed with “surgical diseases such as appendicitis, digestive system diseases, sepsis”, etc. (2, 5, 10). Our data show that 3 cases were transferred from surgery, gastroenterology, and other pediatric departments, and even one child was only accurately diagnosed during a second hospitalization. All children in our study had fever, 5 with accompanying abdominal pain and vomiting, only 2 with frequent urination and dysuria, and 1 child was hospitalized due to renal occupation.
In terms of laboratory data, our study found that the children's infection indicators were significantly elevated, such as peripheral blood white blood cell count, C-reactive protein, and procalcitonin, consistent with literature reports (4). Surprisingly, unlike acute pyelonephritis where urinary white blood cells are significantly higher than normal, we found that most children with renal abscesses had only a small amount of white blood cells in the urine, no pyuria, and a slight increase in urinary red blood cells. As literature reports, if the abscess does not break through the renal pelvis and calyces, and the pus does not enter the collecting system, obvious pyuria may not be present. Therefore, the presence and size of a renal abscess cannot be denied based on the degree of increase in urinary white blood cells and the presence or absence of pyuria (5, 7, 11).
Renal abscesses occur via different pathways, including ascending urinary tract and hematogenous infections, as well as inflammation spreading from adjacent organs. Ascending infections are often related to urogenital system malformations or recurrent urinary tract infections. The main pathogens are Gram-negative bacteria, predominantly Escherichia coli. Staphylococcal infections are the most common cause of hematogenous spread (12, 13). Lin Xiaoliang et al. reported a case of a child with a renal abscess where cultures were negative, and the pathogen was identified through metagenomic sequencing after ineffective treatment with third-generation cephalosporins. Urine and blood cultures in our group of children were all negative, which may be related to the abscesses being confined to the renal parenchyma and not breaking through the renal pelvis and calyces (7). Adult renal abscess patients often have underlying conditions such as diabetes, cirrhosis, female reproductive system infections, stress urinary incontinence, etc. (14, 15). It has been reported that children often have recurrent urinary tract infections, some of which are accompanied by urinary tract malformations (6) but children without underlying diseases can also develop renal abscesses (8). A Chinese study of 5 pediatric renal abscess cases found none with urogenital malformations, and 2 without recurrent urinary tract infections (16). Our group of children had no history of recurrent urinary tract infections, normal prenatal urinary system checks, and no history of urinary tract malformations or reflux. After infection control, cystourethrography was performed on 3 children, with one child found to have bilateral grade 3 reflux.
Due to the atypical clinical symptoms and lack of ultrasound, CT, and other imaging studies, it is difficult to make a definitive diagnosis based solely on clinical presentation and physical examination (13). Ultrasound, being simple to operate, radiation-free, non-invasive, affordable, and widely accepted by families, is often the first choice for initial examination. All 12 of our cases underwent ultrasound, but only 3 children showed abnormalities, suggesting that abscesses are hard to detect before abscess cavity formation and when the abscess is small, leading to missed diagnoses. After hospitalization, all children in our group completed CT or MRU scans. Due to the radiation of CT, children initially admitted to our department preferred magnetic resonance imaging, which showed good imaging results. Whether MRU will be preferred in the future requires further large-sample validation. Additionally, due to its simplicity, ultrasound can be used for clinical follow-up and assessment during the treatment of renal abscesses.
Based on acute pyelonephritis and previous literature reports of renal abscesses predominantly involving Gram-negative bacteria (2, 3, 5), treatment for our group of children upon admission initially involved third-generation cephalosporins. Since the children's blood and urine cultures were all negative, those whose temperature still fluctuated after 3–5 days of treatment were additionally treated with linezolid, achieving good results, with no similar reports in previous literature. Foreign literature reports the use of aminoglycoside antibiotics, which are almost never used in Chinese children (4, 12). There is still controversy regarding the treatment approach of conservative treatment vs. surgical intervention. Previous studies have shown that abscesses smaller than 3 cm can be treated with conservative anti-infection therapy, while those larger than 3 cm can be treated with percutaneous abscess puncture (2–4). A Chinese study showed significant therapeutic effects with conservative treatment for abscesses up to 4.7 cm in diameter (16). For cases 5 and 7, we initially considered abscess drainage. However, after adjusting antibiotics, the body temperature returned to normal, renal area tenderness was negative, and follow-up ultrasound showed the abscess had reduced in size. Therefore, abscess drainage was not performed, and conservative antibiotic treatment continued with good results, consistent with this study in our country.A Russian study retrospectively found that abscesses larger than 3 cm were treated with percutaneous abscess puncture and drainage (17). All 12 children in our group were treated conservatively, with a hospital stay of 10 days to 3 weeks and were discharged smoothly. 11 children were cured after 1–3 months of follow-up, the child with grade 3 reflux underwent surgical treatment for reflux, and 1 child showed a small abscess on ultrasound but had no clinical symptoms and normal urine routine.
This study highlights the atypical presentation and diagnostic challenges of pediatric renal abscesses. Fever, accompanied by non-specific abdominal or renal symptoms, should raise suspicion. The role of imaging, especially CT or MRU, is crucial in early diagnosis. Our findings suggest that conservative treatment with antibiotics is effective for small abscesses, while larger abscesses may require additional interventions.
Conclusion
In summary, pediatric renal abscesses, though rare, should be considered in children presenting with fever and abdominal or renal symptoms. Early imaging and appropriate antibiotic treatment can lead to favorable outcomes, reducing the risk of complications.
This paper has some limitations: it is a single-center study with a small number of cases. Cultures were negative, and further metagenomic testing was not performed. Only some children underwent cystourethrography.
Author contributions
JS: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Writing – original draft. LS: Data curation, Formal analysis, Investigation, Resources, Writing – original draft. LY: Data curation, Investigation, Writing – original draft. YX: Conceptualization, Data curation, Investigation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Medical and Health Science and Technology Programme of Zhejiang Province (NO. 2023KY1114); Ningbo Top Medical and Health Research Program (NO. 2022020405); Ningbo Medical Key Disciplines (NO. 2022-B17); Ningbo Medical Clinical Research Centre (NO. 2019A21002).
Acknowledgments
The authors would like to thank Yulin Kang of the Nephrology Department of Children's Hospital of Shanghai Jiao Tong University for helpful discussions on topies related to this work. We also thank the associate editor and the reviewers for their useful feedback that improved this paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chen CY, Lin MJ, Yang WC, Chang YJ, Gao FX, Wu HP. Clinical spectrum of intra-abdominal abscesses in children admitted to the pediatric emergency department. J Microbiol Immunol Infect. (2020) 53(2):283–91. doi: 10.1016/j.jmii.2018.07.003
2. Chen CY, Kuo HT, Chang YJ, Wu KH, Yang WC, Wu HP. Clinical assessment of children with renal abscesses presenting to the pediatric emergency department. BMC Pediatr. (2016) 16(1):189. doi: 10.1186/s12887-016-0732-5
3. Seguias L, Srinivasan K, Mehta A. Pediatric renal abscess: a 10-year single-center retrospective analysis. Hosp Pediatr. (2012) 2(3):161–6. doi: 10.1542/hpeds.2012-0010
4. Buschel H, Leung P, Stalewski H, Carroll D, Mariyappa-Rathnamma B. Renal abscesses in children: an 11-year retrospective study and review of the literature. ANZ J Surg. (2022) 92(12):3293–7. doi: 10.1111/ans.17943
5. Linder BJ, Granberg CF. Pediatric renal abscesses: a contemporary series. J Pediatr Urol. (2016) 12(2):99.e1–5. doi: 10.1016/j.jpurol.2015.05.037
6. Zhang X, Xie Y, Huang G, Fu H. Analysis of 17 children with renal abscess. Int J Clin Exp Pathol. (2019) 12(9):3179–84.31934162
7. Zhang X, Zhang BL, Wang WH, Song SN, Jiang Y. Clinical analysis of renal abscess in children. Chin J Appl Clin Pediatr. (2019) 34(15):1191–2. doi: 10.3760/cma.j.issn.2095-428X
8. Cheng CH, Tsai MH, Su LH, Wang CR, Lo WC, Tsau YK, et al. Renal abscess in children: a 10-year clinical and radiologic experience in a tertiary medical center. Pediatr Infect Dis J. (2008) 27(11):1025–7. doi: 10.1097/INF.0b013e31817b617b
9. Jiménez M, Gajardo M, Bolte L, Lazcano A, Salgado I. Pediatric renal abscesses: a diagnostic challenge. Andes Pediatr. (2022) 93(2):222–8. doi: 10.32641/andespediatr.v93i2.3765
10. Comploj E, Cassar W, Farina A, Gasparella P, Trenti E, Palermo S, et al. Conservative management of paediatric renal abscess. J Pediatr Urol. (2013) 9(6 Pt B):1214–7. doi: 10.1016/j.jpurol.2013.05.016
11. Tsukagoshi D, Dinkovski B, Dasan S, Jethwa J. Perinephric abscess secondary to a staghorn calculus presenting as a subcutaneous abscess. CJEM. (2006) 8(4):285–8. doi: 10.1017/s1481803500013889
12. Rubilotta E, Balzarro M, Lacola V, Sarti A, Porcaro AB, Artibani W. Current clinical management of renal and perinephric abscesses: a literature review. Urologia. (2014) 81(3):144–7. doi: 10.5301/urologia.5000044
13. Zhan Z, Lin X, Li G, Zeng J, Su D, Liao J, et al. Renal abscess complicating acute pyelonephritis in children: two cases report and literature review. Medicine (Baltimore). (2023) 102(48):e36355. doi: 10.1097/MD.0000000000036355
14. Yen DH, Hu SC, Tsai J, Kao WF, Chern CH, Wang LM, et al. Renal abscess: early diagnosis and treatment. Am J Emerg Med. (1999) 17(2):192–7. doi: 10.1016/s0735-6757(99)90060-8
15. Hung CH, Liou JD, Yan MY, Chang CC. Immediate percutaneous drainage compared with surgical drainage of renal abscess. Int Urol Nephrol. (2007) 39(1):51–5. doi: 10.1007/s11255-006-9033-5
16. Luo TH, Zhang XH, Meng QM, Sun YF, Wang W. Conservative management of pediatric renal abscess. Chin J Pediatr Surg. (2021) 42(10):903–6. doi: 10.3760/cma.j.cn421158-20210104-00006
Keywords: renal, abscess, pediatric, management, review
Citation: Sun J, Shi L, Ye L and Xu Y (2025) Pediatric renal abscess: clinical analysis and literature review. Front. Pediatr. 13:1407437. doi: 10.3389/fped.2025.1407437
Received: 26 March 2024; Accepted: 14 April 2025;
Published: 28 April 2025.
Edited by:
Orkun Tolunay, University of Health Sciences, TürkiyeReviewed by:
O. P. Mishra, Heritage Institute of Medical Sciences, IndiaRainer Büscher, Essen University Hospital, Germany
Merve Kılıç Çil, Ministry of Health, Türkiye
Copyright: © 2025 Sun, Shi, Ye and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanan Xu, eHludHQxMjcxMTE2QG91dGxvb2suY29t
†These authors have contributed equally to this work
 Jianxin Sun
Jianxin Sun Lina Shi
Lina Shi Lezhen Ye1
Lezhen Ye1