- 1Department of Counselling, Tehran North Branch, Islamic Azad University, Tehran, Iran
- 2Department of Psychology, Norwegian University of Science and Technology, Trondheim, Norway
- 3Department of Psychology, Faculty of Humanities and Social Sciences, Istinye University, Istanbul, Türkiye
- 4Department of Psychology, Tehran North Branch, Islamic Azad University, Tehran, Iran
- 5Department of Psychology and Educational Sciences, Yazd University, Yazd, Iran
- 6Department of Psychiatry and the Behavioral Sciences, Keck School of Medicine, University of Southern California, Los Angeles, CA, United States
Introduction: Childhood stressors and adverse experiences can increase the likelihood of children developing mental disorders. The development of mindfulness-based cognitive therapy for children (MBCT-C) offers opportunities to improve emotional resiliency and reduce these children's vulnerabilities. The current study introduces the framework of a future clinical trial that seeks to examine the level of satisfaction and the efficacy of MBCT-C on anxiety, attentional control, and emotional regulation in children.
Method: This research protocol outlines a quasi-experimental design that compares MBCT-C with an active control group. The intervention group will participate in a 12-session MBCT-C program, while the active control group will receive a 12-session program of life skills training (LST). Eighty children aged between 8 and 12 years will be randomly assigned to the intervention or the control group. Data using the Mindful Attention Awareness Scale for Children (MAAS-C), the Emotion Regulation Checklist (ERC), the State-Trait Anxiety Inventory for Children (STAI-CH), and the Attentional Control Scale for Children (ACS-C) will be collected at three times: baseline, post-intervention, and six months following the intervention. The Mindfulness Program Satisfaction Questionnaire (MPSQ) will assess participant satisfaction with the program. The effectiveness of MBCT-C will be evaluated using a conditional mixed regression model in STATA-18.
Discussion: Providing a research protocol to conduct a clinical trial on MBCT-C before the intervention phase provides a precise evaluation of the goals and hypotheses, study method, assessment tools, and treatment outcomes.
Introduction
Children frequently experience emotional problems, such as anxiety disorders (e.g., generalized anxiety disorder, separation anxiety), depression, obsessive-compulsive disorder, and disruptive mood regulation disorder in middle and late childhood (1, 2). Approximately 11.63% of children and adolescents worldwide meet the established criteria for a mental disorder (3), although it is essential to note that the prevalence of subclinical problems, particularly anxiety, is considerably greater (4). Mental problems experienced during childhood are often persistent and frequently continue into adulthood (5). Hence, it is imperative to consider the implementation of psychological interventions that enhance childhood resiliency and reduce the risk of subsequent internalizing and externalizing disorders (6, 7). Along with the contributing role of anxiety, emotion regulation (1, 8, 9) and attentional control (10) have been proposed as underlying factors in the psychopathology of children's emotional problems.
Anxiety is a future-oriented response to perceived threatening situations that are often characterized by ambiguity and uncertainty. Anxiety is a common, sometimes uncomfortable emotional experience. Only when it becomes severe is it considered a manifestation of psychological problems (11, 12). Chronic, uncontrollable anxiety can result in clinical distress and impaired performance (13, 14). Children often experience anxiety due to a wide range of transient or long-term stressors, which can be exacerbated by a limited capacity to effectively cope with such challenges (15, 16). When anxiety becomes severe, it impairs daily functioning, including social and school achievements (14, 17). For example, some children experience separation anxiety when they begin attending school, as they are separated from their parents and enter an unfamiliar environment (18). Others may feel socially anxious, fearing observation and negative judgements from others in social settings, which can lead to avoidance of many situations that require interpersonal interactions (19). Specific phobias also lead to avoidance of the source of fear and inability to tolerate the associated anxiety (20). Along with math (21) and test anxieties (22), which result in low grades and academic failure in children, these are common anxieties impair children's development.
Emotion regulation (ER) is an adaptive manner of managing emotions and feelings (8). ER capacity affects the interpretation of experiences, emotional expression, and responses to the emotions of others (23). Maladaptive coping strategies can disrupt emotion processing and aggravate emotional disturbances (8, 24, 25). Inadequate ER has received increasing attention as an underlying factor in childhood and adolescent mental disorders (26). Children who develop adaptive emotion regulation skills are more likely to have a better quality of life and are at lower risk for mental disorders (27). Strengthening ER skills is considered a preventive approach and a treatment goal to address emotional problems in children (26, 28). In one study, an ER-focused preventive intervention resulted in significant increases in emotional awareness, reductions in negative emotions, and reductions in internalizing problems in preschool children at risk for psychological problems (29). A recent meta-analysis found that a variety of psychosocial interventions were moderately effective in improving ER in children, adolescents, and transition-age youth (30).
Information processing in the human cognitive system takes place through the mechanism of attention control (AC). AC mechanisms facilitate the ability to direct and shift attention between stimuli and situations (31), selectively focusing on task-relevant information while ignoring irrelevant information (32). Difficulties managing attention to emotional and non-emotional stimuli have been associated with anxiety disorders and depression (33).
Cognitive processing deficits, especially the inability to shift attention from distressing thoughts, contribute to the persistence and exacerbation of worry and rumination (34, 35). Evidence supports the correlation of anxiety and depression with lower AC in children (36). The role of AC deficits is apparent in attention deficit hyperactivity disorder (ADHD) and some developmental problems (e.g., autism spectrum disorder) (37). A systematic review has provided evidence suggesting that enhancing attention capabilities contributes to a decrease in anxiety and depression (38).
The development of effective psychotherapies aimed at addressing emotional problems in children has made significant progress (14, 16, 39). Mindfulness-based interventions, in particular, are of growing interest. Mindfulness is an approach to life experiences that emphasizes attention to the present moment and with an attitude of non-judgment (40). Mindfulness, cultivated through meditation, involves bringing awareness to one's thoughts, emotions, and bodily sensations without engaging reactively to them (41, 42). Mindfulness-based interventions, which have been influential in evolving the third wave of cognitive-behavioral therapies, were developed initially for adults, but have now been adapted for children (43).
Mindfulness-based cognitive therapy (MBCT) was developed for relapse prevention in adult patients with recurrent depressive episodes (44, 45), and was later adapted for other problems and populations (46). One of these adaptations, MBCT-C, employs the same methodology as the adult program and shares analogous goals and objectives; however, it has been specifically tailored for children, which includes modifications to the duration of the sessions and the incorporation of child-friendly language and content (47). MBCT-C may be an effective intervention in mitigating emotional difficulties among children and adolescents (48, 49). A study conducted to investigate the effectiveness of MBCT-C on children and adolescents suffering from anxiety disorders who were at risk of bipolar disorder revealed that MBCT-C is effective in reducing clinical symptoms. Additionally, improvements in mindfulness were associated with improvements in anxiety and emotion regulation (50). The effectiveness of MBCT-C has been repeated in other clinical samples, including children with math anxieties (51), cancer (39), and internalizing disorders (52). The results of a meta-analysis, which compiled results from 3,977 child and adolescent mindfulness-based interventions, showed that the effect size of these interventions is small to moderate, and that the effectiveness appears to vary based on two factors: the type of facilitator and the characteristics of the program (53). Therefore, mindfulness-based interventions for children and adolescents in both clinical and non-clinical populations need further evaluation.
Children's clinical intervention programs should not be limited to clinical populations; their prophylactic effectiveness should also be examined in non-clinical populations. These programs may have significant benefits in preventing childhood problems (54). The primary aim of the present study protocol is to outline the theoretical framework and methodology of a quasi-experimental study to investigate the effectiveness of MBCT-C in managing non-clinical anxiety, emotion regulation, and attentional control in children. Five hypotheses are proposed:
Primary hypothesis
1. Following a 12-session MBCT-C program, children in this group will report significantly increased mindfulness compared to children attending a 12-session Life Skills Training (LST) program, as measured by the Mindful Attention Awareness Scale for Children (MAAS-C).
Secondary hypotheses
2. Following a 12-session MBCT-C program, children in this group will report the MBCT-C group will report significant decreases in state and trait anxiety as compared to children attending a 12-session LST program, as measured by the State-Trait Anxiety Inventory for Children (STAI-CH).
3. Following a 12-session MBCT-C program, children in this group will report a significant increase in emotion regulation as compared to children attending a 12-session LST program, as measured by the Emotion Regulation Checklist (ERC).
4. Following a 12-session MBCT-C program, participants in this cohort will report a significant increase in attentional control when compared to children participating in a 12-session LST program, as measured by the Attention Control Scale for Children (ACS-C).
5. The MBCT-C program will be acceptable to children and their parents as measured by recruitment, attendance, drop-out rates, and the Mindfulness Program Satisfaction Questionnaire (MPSQ).
Method
Study design
This is a quasi-experimental study that comparing an MBCT-C program to an active control groupthe. Demographic data will be collected at baseline. Assessment data will be collected at baseline (T1), post-intervention (T2), and 6-month follow-up (T3) (Figure 1). Participants will be randomly assigned to either MBCT-C or LST using a software-generated random sequence. A stratified block randomization method will ensure balanced distribution by gender and age. A comparison of attendance and drop-out rates between the MBCT-C and LST groups will be one marker of program acceptability. Participants' adherence to the intervention will be evaluated via session attendance, group activity participation, and homework assignment compliance. To reduce potential bias, assessors will be blind to group allocation.
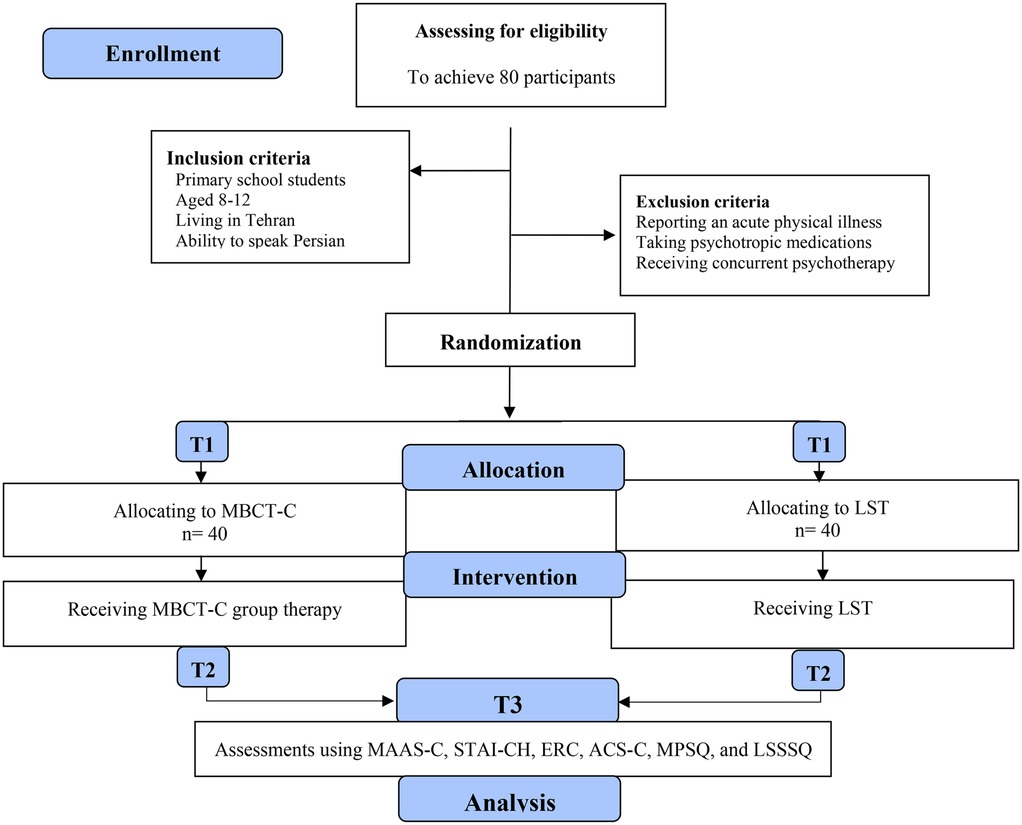
Figure 1. CONSORT diagram illustrating the study phases. T1: baseline; T2: Post-intervention; T3: 6-Month follow-up; MBCT-C: Mindfulness-based Cognitive Therapy for Children; MAAS-C-: Mindful Attention Awareness Scale- Adolescents; STAI-CH: State-Trait Anxiety Inventory for Children; ERC: Emotion regulation checklist; ACS-C: Attentional Control Scale for Children; MPSQ: Mindfulness Program Satisfaction Questioner (MPSQ).
Sample size
According to Thibault & Pedder (55) and Treves et al. (56), the required sample size for this study to achieve sufficient statistical power was determined using G*Power software (57). In this calculation, we used a priori power analysis with the following parameters: significance level α = .05; effect size = .5 (58); power (1-β).95; with two groups, corresponding to the study design. A minimum of 64 participants was estimated to detect hypothesized effects reliably. Recognizing the possibility of participant attrition, we incorporated a buffer to protect the power of the study. Specifically, we estimated a dropout rate of 20%, increasing the sample by an additional 14 participants (calculated as 20% of 64, rounded). This adjustment resulted in a total sample size of 77 (rounded to 80) participants. However, we acknowledge that this sample size limits our ability to detect smaller effect sizes. We have adjusted our expectations accordingly, focusing on larger effects as suggested by prior research (e.g., Goldberg et al. (59), for mindfulness interventions on stress.
Recruitment and randomization procedures
In this study, our sampling framework encompasses four schools (two female-only and two male-only institutions) randomly selected from diverse districts across Tehran to ensure appropriate population representation. The target population comprises all middle school students in Tehran who, according to Iran's educational system, attend gender-segregated schools.
The necessary research permits will be obtained from Tehran's Education Department through the university's Research Vice-Chancellor's office. Group intervention sessions will be conducted after regular school hours in the counseling rooms of the participating schools, providing a quiet and appropriate environment for group therapeutic activities. This approach facilitates student access to the program while avoiding interference with their academic schedules.
Furthermore, school counselors will explain the research and introduce interested parents and students to the research team. Should these recruitment techniques be insufficient to obtain the desired sample size within a reasonable time, we will extend recruitment to additional schools within the Tehran education district.
Potential participants who contact the research assessment team will undergo an in-person screening to determine their eligibility. Inclusion criteria include: (a) primary school students, (b) age between 8 and 12 years old, (c) living in Tehran, and (d) ability to speak Persian. Exclusion criteria comprise (a) reporting an acute physical illness, (c) receiving psychotropic medications, and (e) receiving concurrent psychotherapy. Children who meet the criteria for this study and agree to participate will be enrolled with the consent of a parent or caregiver. Once the desired sample size is enrolled, participants will be randomized to the MBCT-C or LST group using online random allocation software (https://miniwebtool.com/de/number-randomizer/). The allocation will be made in a 1:1 ratio, ensuring equal representation of participants in each group.
Procedure
Participants will be recruited from public elementary schools in Tehran. We will employ a staged recruitment approach, enrolling four cohorts of 20 children each (80 total). As each cohort of 20 children is recruited, they will be randomly assigned to either intervention or control groups (10 per group), and the 12-week programs will begin. While the first cohort undergoes treatment, recruitment for subsequent cohorts will continue.
Interested children will participate in a brief eligibility screening. Eligible students and their parents will receive comprehensive information about the study. Participation requires written informed consent from a parent or guardian and verbal assent from the child. Participants assigned to the intervention group will attend weekly 90-minute MBCT-C sessions for 12 weeks. The control group will participate in a 12-week LST program. Each program will be facilitated by separate instructors trained and invested in their respective models to prevent potential bias.
Protocol adherence will be monitored using the MBCT-C adherence scale and an equivalent measure for LST. A trained supervisor will review recorded sessions and provide feedback to facilitators to ensure standardized protocol implementation. Participants will complete the T2 assessment battery at the end of the intervention and the T3 follow-up assessment six months later. The Client Satisfaction Questionnaire (CSQ-8) will measure participant satisfaction with both programs.
Mindfulness-based cognitive-behavioral therapy-children (MBCT-C)
MBCT-C (47) is a manualized 12-week treatment protocol that focuses on addressing attentional problems and anxiety-spectrum disorders in children. This protocol is designed for children between 8 and 12 years old and includes a variety of meditation and mindfulness techniques to improve cognitive, emotional, and physical awareness.
MBCT-C consists of three sequential steps to improve mindfulness. In the first phase (Sessions 1–3), in addition to preparing participants to overcome the obstacles ahead and how to do the tasks, exercises for conscious breathing, body awareness, and mindfulness will be presented. The second step of MBCT-C (sessions 4–10), which constitutes the principal portion of interventions, is aimed at thoughts, emotional experiences, and physical sensations in a more adept manner ways. Participants will engage in exercises designed to enhance mindfulness in each of their five senses. Additionally, based on informed and non-judgmental observations, they will examine various alternative ways of responding to challenging thoughts, emotions, and external events. In the final stage of the program (sessions 11 and 12), participants are taught to integrate mindfulness practices into their daily routines. Participants will discuss maintaining a daily practice of mindfulness and discuss benefits that may have been experienced during the program. Three months after the end of the program, each participant will receive a letter written by themselves in session 11 to motivate themselves to continue a consistent daily practice. At each session, written session summaries, homework assignments, poems, or stories related to that session, are provided to the participants (Table 1).
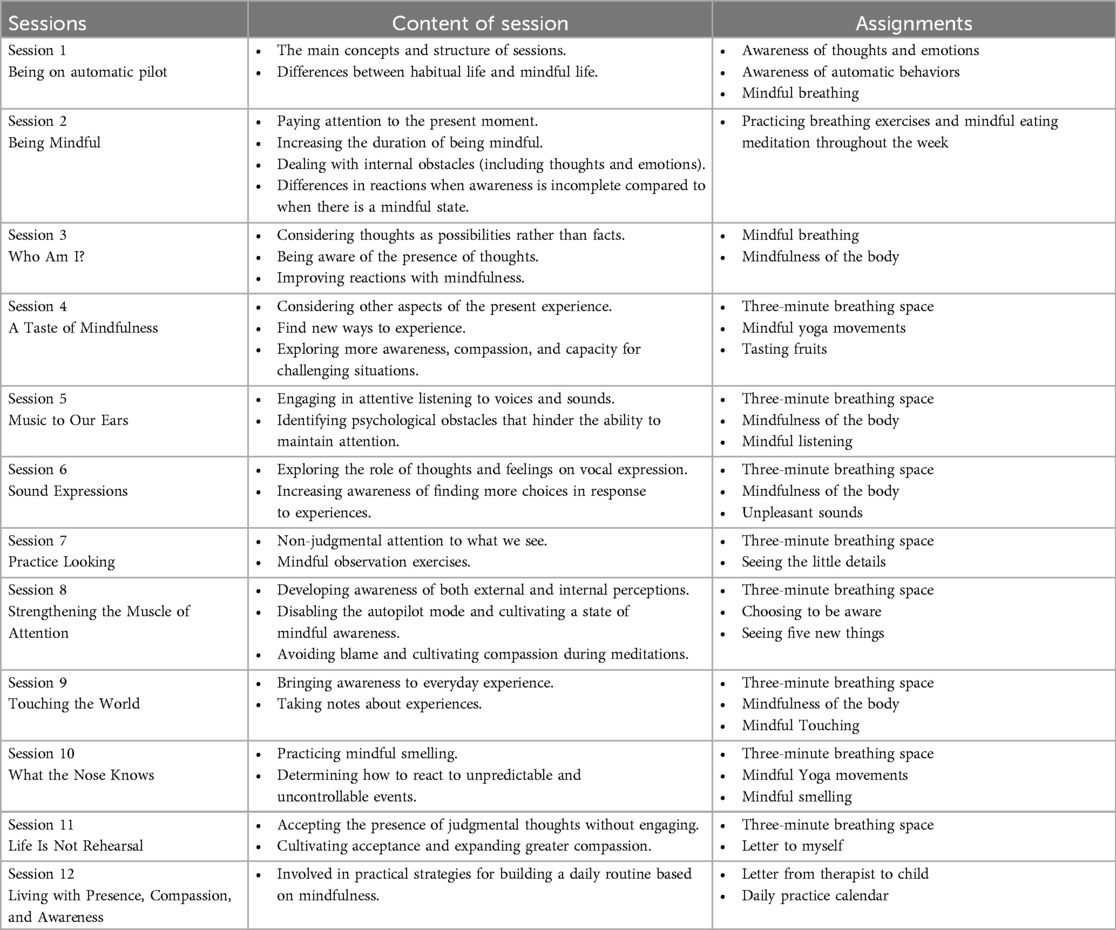
Table 1. The session-to-session content of the MBCT-C protocol [Semple and Lee, (47)].
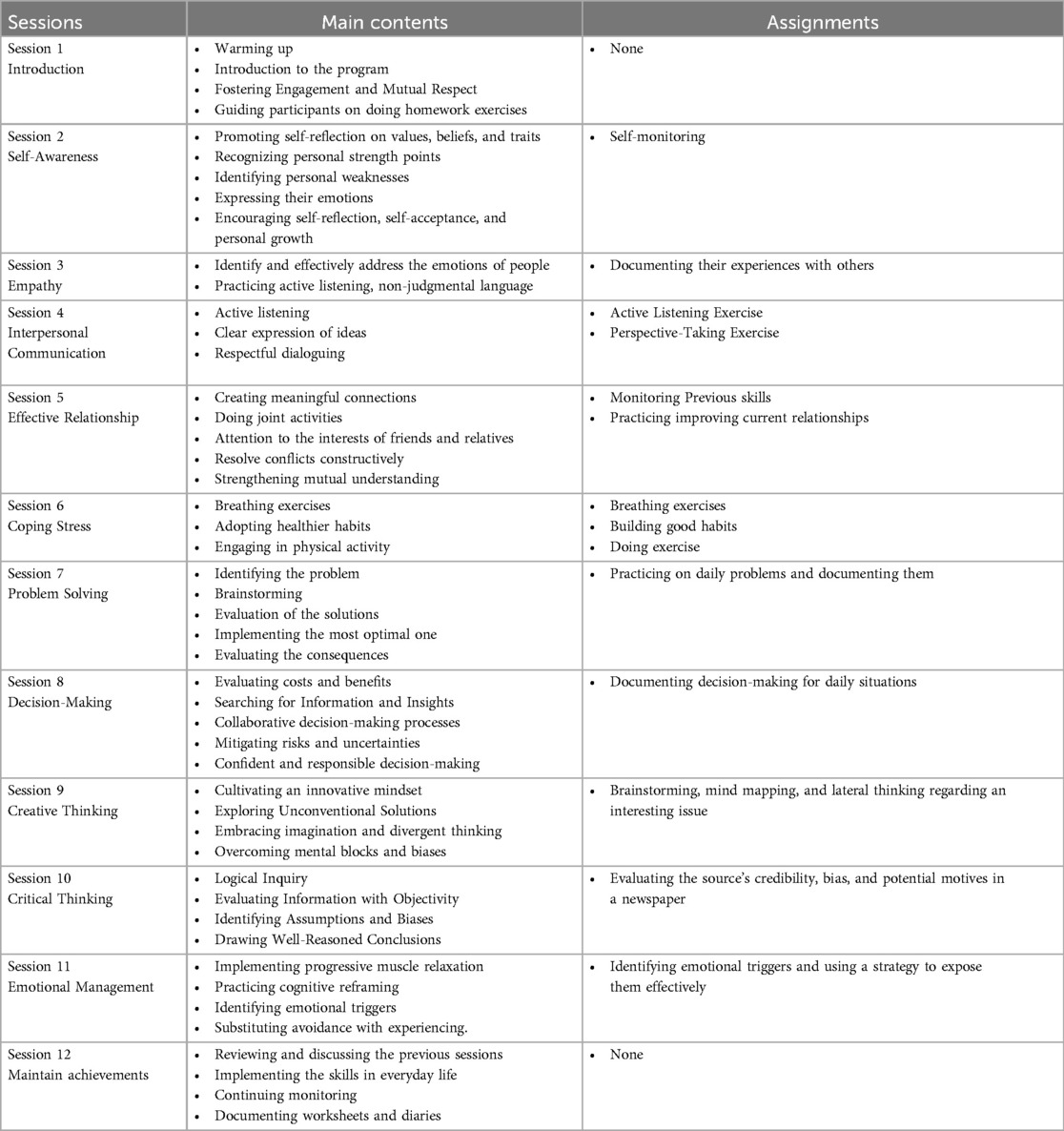
Life skills training (LST)
LST is a comprehensive 12-week group program, developed by GJ Botvin and KW Griffin (60) developed to help participants practice ten essential life skills. The skills covered include self-awareness, empathy, interpersonal communication, coping with stress, decision-making, problem-solving, emotional management, creative thinking, critical thinking, and effective communication. Like the MBCT-C program, LST incorporates practice during sessions and assigns homework. Based on the sessions' practices, upon learning each skill, participants reflect on a recent challenging situation in their lives and utilize the skills acquired to reevaluate that situation, developing appropriate responses. During each session, a facilator elucidates the skills to the participants and facilitate their learning through constructive feedback. As part of their homework, participants are encouraged to effectively implement the skills they have acquired to manage various situations encountered throughout the week. In each session, the homework from the previous session is collectively reviewed in a shared space (Table 2). Two distinct therapists will facilitate the LST and MBCT-C group sessions. We have selected therapists with specialized training and experience in their respective programs. This approach mitigates the risk of bias if a single individual were to conduct both programs, particularly given varying levels of expertise or personal preference.
Protocol adherance
The study supervisor monitors protocol adherence through multiple methods. First, they review video recordings of all sessions. Second, they hold supervision meetings with the therapist every two weeks. Third, they complete standardized fidelity assessments after each session.
For MBCT-C sessions, the supervisor uses the validated MBCT-C Adherence Scale. This tool measures how closely the therapist follows the established protocol. For LST sessions, the supervisor uses the Life Skills Training Fidelity Monitoring Checklist developed by Botvin and colleagues. Both assessment tools evaluate content delivery, participant engagement, and implementation of core techniques.
The supervisor provides feedback to facilitators immediately after reviewing each session. This allows facilitators to address any protocol deviations quickly. Such close monitoring ensures consistent program delivery across all four cohorts of participants.
Measures
Mindful attention awareness scale-children (MAAS-C)
This unpublished self-report tool consists of 15 items to measure mindfulness in children (61). Participants will respond to the questions using a Likert scale ranging from 1 (almost never) to 6 (almost always). All 15 items are phrased negatively and reversely scored. This scoring approach means individuals receiving elevated scores demonstrate stronger mindfulness capabilities. The original MAAS-C has a good internal consistency among children (α = .84) (62).
State-trait anxiety inventory for children (STAI-Ch)
The STAI-CH is a self-report measure of anxiety levels in children (63). Two independent scales of this inventory are state anxiety (S anxiety) and trait anxiety (T anxiety). S anxiety assesses anxiety as a temporary emotional condition, and T anxiety evaluates anxiety as a trait of personality. Both scales consist of 20 items, each rated on a 3-point Likert scale from 1 (rarely) to 3 (often). The overall score for each variable ranges from 20 to 60. The State-Trait Anxiety Inventory for Children (STAI-CH) has exhibited strong psychometric properties. The internal consistency coefficients for both scales surpassed.80 (63). In addition, it has been shown that the psychometric properties of the Persian version of STAI-CH have good levels of internal consistency (α = .89) (64).
Emotion regulation checklist (ERC)
ERC is a commonly employed other-report (e.g., completed by parents or teachers) utilized to evaluate the emotion regulation capacities of children and adolescents (65). ERC includes 24 items scored on a 4-point Likert scale, from 1 (never) to 4 (almost always). Items are categorized into two subscales, Lability/Negativity and Emotion Regulation. Lability/Negativity evaluates how individuals encounter negative emotions and exhibit emotional instability. Emotion Regulation evaluates the capacity to regulate emotional reactions and engage in self-soothing actions. Numerous research investigations showed the ERC's robust psychometric characteristics. The internal consistency of ERC has been determined to be satisfactory for the Lability/Negativity (α = .96) and the Emotion Regulation subscale (α = .83). The ERC exhibits strong convergent validity when compared to other assessments of behavioral problems and social skills (66). The capacity to detect changes has also been evidenced in intervention studies, wherein enhancements in the aptitude to regulate emotions were correlated with a reduction in negative emotional states and an elevation in positive emotional states. The present study will use the Persian version of the ERC. This checklist has high internal consistency (α = .90) in an Iranian population and has convergent validity and acceptable discriminant validity (67).
Attentional control scale for children (ACS-C)
ACS-C is a 20-item self-report scale (68) to assessing attentional control among children. Each item is rated on a five-point Likert scale that ranges from 1 (almost never) to 4 (always). Items evaluate three distinct aspects of attentional control: focusing, shifting, and flexibility. The internal consistency of ACS-C has been reported to be good in different studies [α = .78 and .74 (69, 70)]. The present research will utilize the Persian adaptation of the ACS-C. As this version has not yet been standardized for use in Iran, the internal consistency of the questionnaire will be evaluated during the study's second phase.
Satisfaction and adherence measures
Mindfulness program satisfaction questionnaire (MPSQ)
MPSQ was developed by Semple (2016) using the items of the original version of the Client Satisfaction Questionnaire [CSQ (71)]. It includes 8 items rated on a 4-point Likert scale. Half of the items are scored directly (including 5, 4, 2, and 8), and the other half is scored in reverse (1, 3, 6, and 7). Scores range from 8 to 32, and higher scores indicate higher satisfaction with the MBCT-C program.
Life skills training satisfaction questionnaire (LSTSQ)
We will use an adapted version of the Client Satisfaction Questionnaire [CSQ-8 (71)] to measure participant satisfaction in the LST group. This adapted questionnaire maintains the original 8-item structure with a 4-point Likert scale, with modifications to reflect LST-specific content. Scores range from 8 to 32, with higher scores indicating greater satisfaction with the LST program.
Ethical standards
We registered the present study in the Iranian Registry of Clinical Trials (IRCT; IRCT20230922059488N1). We will follow the ethical guidelines related to human experiments. In addition, we will adhere to the principles outlined in the Declaration of Helsinki in 1975, which was subsequently revised in 2008, in all study phases. Given that the research will be conducted with children under age 18, a formal informed consent document must be signed by a guardian or parent of everyone included in the study. Children will provide verbal assent to participate. Participants may discontinue the intervention at any point during the research voluntarily.
Participant anonymity will be maintained through the assignment of unique identification codes in place of personal information. Names and contact details will be replaced with pseudonyms during data collection. Each participant will receive a distinct identifier that will prevent direct linkage to individual identities. The coding key will be stored separately from the main dataset in a secure location. Data storage will follow standard security protocols. An encrypted database will house all collected information, with access restricted to designated research team members.
The research director, ethics committee, and IRCT will be duly informed of any probable modifications made to the study, and these changes will be subsequently documented in the IRCT. This study protocol received approval from the local ethics council at the Azad University- North Tehran Branch (ethics code: IR.IAU.TNB.REC.1402.067).
Statistical strategy
The study results will adhere to the guidelines established by the SPIRIT guidelines (72). The analysis will be conducted using the STATA-18 software. After data collection and curation, to determine data consistency, we assess the status of outliers by calculating both the average and a 5% reduced average (p < .05). We shall also analyze demographic differences in the baseline utilizing independent t-tests and chi-square tests. Furthermore, an intention-to-treat (ITT) analysis will be conducted should any participant miss more than three intervention sessions. This approach ensures that missing data does not significantly bias the study's primary analysis, remaining below 5% of the total data. In such instances, multiple imputations will replace missing values with alternative ones.
To evaluate the study outcomes, we will use a conditional mixed regression model to simultaneously compare the fixed and random effects of two groups (MBCT-C vs. LST) at the three assessment times (T1, T2, T3). The fixed effects will include group, time, and the group-by-time interaction, enabling the assessment of changes in the main outcomes across time and between groups. Participant ID will be treated as a random effect to account for repeated measurements within individuals. Where appropriate, baseline variables such as age and gender will be included as additional fixed effects to examine their potential role in moderating intervention outcomes. All analyses in the present study will evaluate the results at a significant level (p < .05). The Reliable Change Index (73) will be applied to examine clinically significant changes in primary and secondary outcomes before and after MBCT-C. A statistically significant difference will be represented by an RCI greater than 1.96.
Result
This research is a part of the doctoral thesis of the first author of this article, whose proposal was approved in February 2023 at North Tehran Azad University. The ethical code of this study was presented by the ethics committee of the corresponding university on September 1, 2023. The initial screening of participants is currently underway. The seating required for this intervention and the prerequisites for the sessions are fully provided. When sampling and screening of participants is finished, the interventions will begin.
Discussion
Recent findings regarding doubts about the effectiveness of mindfulness interventions for adolescents have raised concerns about the efficacy of these interventions for younger individuals (53, 74). This study protocol focuses on a younger age group, specifically children aged 8–12. According to this issue, the research explores whether early intervention can enhance mindfulness, reduce anxiety, improve emotional regulation, and boost attention control. The significance of these characteristics is well-established in a diverse array of childhood emotional and behavioral disorders. If MBCT-C can address these problems efficiently, the participants will likely experience positive outcomes.
In this study, it is assumed that anxiety is a prevalent issue among children, demanding intervention when it develops into a functionally impairing disorder. Untreated anxiety issues in children increase their susceptibility to future occurrences of depression, substance abuse, and further emotional difficulties (75–77). The MBCT-C program in this study provides activities and skills training designed to enable children to manage anxiety and overcome emotional avoidance more effectively. Children who include these meditation techniques in their daily routines may feel enhanced psychological well-being, resulting in reduced psychological distress when confronted with anxiety-inducing situations. Moreover, they may be more inclined to face anxiety-provoking situations rather than avoiding them (78).
The absence of proficient emotion regulation skills often results in exacerbated difficulties when attempting to cope with anxiety and stress (79). Children who rely on avoidance or maladaptive coping strategies, such as excessive worry, are at an increased risk of developing anxiety disorders and depression (80, 81). Enhancing emotion regulation skills, especially improved awareness, non-judgmental acceptance, and cognitive reappraisal, is a potential benefit of MBCT-C. Consequently, providing children with these strategies can effectively equip them to cope with emotional challenges. Children who employ adaptive emotion regulation strategies to cope with anxiety can decrease their susceptibility to internalizing and externalizing disorders (82). The development and maturation of adolescents is also facilitated by the cultivation of emotion regulation skills in children (83).
MBCT-C utilizes mindfulness to improve attentional control through sensory-focused activities with children during sessions (taste, hearing, seeing, touch, and smelling), which increases ongoing awareness and attention to non-distracting sensations (84). This study protocol aims to evaluate MBCT-C's efficacy and satisfaction. Children need to develop attentional control, which facilitates the regulation of related emotions/thoughts/behaviors and may improve social-emotional and academic performance (85). This study protocol establishes a controlled framework to assess the efficacy of MBCT-C in children, which will enhance our ability to debate and make conclusions on the effect size and the generalizability of the findings within Iranian children. The study design exhibits two significant limitations requiring careful consideration when interpreting and extrapolating the findings. First and foremost, due to constraints in both financial and human resources, it was unfeasible to carry out the study with a larger sample size. Furthermore, given that the study's sampling is conducted within educational institutions, the potential exists for transmitting session-related information from the intervention group to the control group. If the findings of the present study demonstrate substantial efficacy in these interventions, further research should investigate their effectiveness and participant satisfaction across diverse samples of Iranian children. Additionally, it is advised that future research endeavors encompass a comparative analysis of the efficacy of the treatment program relative to other established treatment programs.
Future research should prioritize larger-scale studies if this study demonstrates MBCT-C's efficacy. Longitudinal studies are also needed to investigate the sustained effects of MBCT-C on children's mental health and academic outcomes over time. Similarly, future comparative studies between MBCT-C and other well-established treatments (e.g., cognitive-behavioral therapy or other mindfulness-based programs) could provide a more comprehensive understanding of its efficacy and cost-effectiveness. Examining participant satisfaction and program feasibility in different Iranian settings, including rural or underserved areas, would provide additional empirical support for the scalability of MBCT-C across diverse populations. Moreover, qualitative methods (e.g., child and parent interviews) would also provide further interpretation of the intervention's acceptability and mechanisms of change.
Ethics statement
The studies involving humans were approved by Ethics Committee of Islamic Azad University, North Tehran branch. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
HK: Conceptualization, Investigation, Project administration, Resources, Writing – original draft, Writing – review & editing. MH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KA: Conceptualization, Investigation, Project administration, Writing – review & editing. FD: Investigation, Project administration, Validation, Writing – review & editing. RS: Conceptualization, Methodology, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study received financial support from the Norwegian University of Science and Technology (NTNU) to facilitate open access publication.
Acknowledgments
We express our gratitude to each school that agreed to take part in this research project.
Conflict of interest
The authors declare that the research was conducted without commercial or financial relationships that could create a conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Habibi Asgarabad M, Steinsbekk S, Wichstrøm L. Social skills and symptoms of anxiety disorders from preschool to adolescence: a prospective cohort study. J Child Psychol Psychiatry. (2023) 64(7):1045–55. doi: 10.1111/jcpp.13787
2. Barlow DH, Ellard KK, Sauer-Zavala S, Bullis JR, Carl JR. The origins of neuroticism. Perspect Psychol Sci. (2014) 9(5):481–96. doi: 10.1177/1745691614544528
3. Kieling C, Buchweitz C, Caye A, Silvani J, Ameis SH, Brunoni AR, et al. Worldwide prevalence and disability from mental disorders across childhood and adolescence: evidence from the global burden of disease study. JAMA Psychiatry. (2024) 81:347–56. doi: 10.1001/jamapsychiatry.2023.5051
4. Donnelly CL, Rhoads JC. Anxiety disorders in childhood and adolescence. In: Klykylo WM, Kay J, editors. Clinical Child Psychiatry. Hoboken, NJ: John Wiley & Sons, Ltd. (2012). p. 215–242. doi: 10.1002/9781119962229.ch13
5. Otto C, Reiss F, Voss C, Wüstner A, Meyrose A-K, Hölling H, et al. Mental health and well-being from childhood to adulthood: design, methods and results of the 11-year follow-up of the BELLA study. Eur Child Adolesc Psychiatry. (2021) 30(10):1559–77. doi: 10.1007/s00787-020-01630-4
6. Tolan PH, Dodge KA. Children’s mental health as a primary care and concern: a system for comprehensive support and service. American Psychologist. (2005) 60(6):601–14. doi: 10.1037/0003-066X.60.6.601
7. Wakschlag LS, Roberts MY, Flynn RM, Smith JD, Krogh-Jespersen S, Kaat AJ, et al. Future directions for early childhood prevention of mental disorders: a road map to mental health, earlier. J Clin Child Adolesc Psychol. (2019) 48(3):539–54. doi: 10.1080/15374416.2018.1561296
8. Cludius B, Mennin D, Ehring T. Emotion regulation as a transdiagnostic process. Emotion. (2020) 20(1):37–42. doi: 10.1037/emo0000646
9. Fard ZG, Schneider S, Hudson JL, Habibi M, Pooravari M, Heidari ZH. Early maladaptive schemas as predictors of child anxiety: the role of child and mother schemas. Int J Appl Behav Sci. (2014) 1(2):9–18. doi: 10.22037/ijabs.v1i2.7564
10. Feurer C, Jimmy J, Bhaumik R, Duffecy J, Medrano GR, Ajilore O, et al. Anterior cingulate cortex activation during attentional control as a transdiagnostic marker of psychotherapy response: a randomized clinical trial. Neuropsychopharmacology. (2022) 47(7):1350–7. doi: 10.1038/s41386-021-01211-2
11. Creswell C, Waite P, Hudson J. Practitioner review: anxiety disorders in children and young people—assessment and treatment. J Child Psychol Psychiatry. (2020) 61(6):628–43. doi: 10.1111/jcpp.13186
12. Heshmati R, Seyed Yaghoubi Pour N, Haji Abbasoghli P, Habibi Asgarabad M. Adverse childhood experience, parental bonding, and fatherhood as parenting vulnerabilities to social anxiety severity. Eur J Investig Health Psychol Educ. (2024) 14(7):2057–73. doi: 10.3390/ejihpe14070137
13. Clark DA, Beck AT. Cognitive theory and therapy of anxiety and depression: convergence with neurobiological findings. Trends Cogn Sci (Regul Ed). (2010) 14(9):418–24. doi: 10.1016/j.tics.2010.06.007
14. Edrissi F, Havighurst SS, Aghebati A, Habibi M, Arani AM. A pilot study of the tuning in to kids parenting program in Iran for reducing preschool children’s anxiety. J Child Fam Stud. (2019) 28(6):1695–702. doi: 10.1007/s10826-019-01400-0
15. Silverman WKF, Andy P. Anxiety Disorders in Children and Adolescents. 2nd ed. Cambridge: Cambridge University Press (2011).doi: 10.1017/CBO9780511994920
16. Ahadianfard P, Gharraee B, Aghebati A, Asgarabad MH. Effectiveness of unified protocol for trans diagnostic treatment in children with anxiety disorders: a randomized control trial. J Educ Health Promot. (2023) 12(1):1–2. doi: 10.4103/jehp.jehp_1578_22
17. Chiu A, Falk A, Walkup JT. Anxiety disorders among children and adolescents. FOCUS. (2016) 14(1):26–33. doi: 10.1176/appi.focus.20150029
18. Caporino NE, Wong JX, O’Brien Cannon A. Separation anxiety disorder in children and adolescents. In: McKay D, Storch EA, editors. Handbook of Child and Adolescent Anxiety Disorders. Cham: Springer International Publishing (2023). p. 249–69. doi: 10.1007/978-3-031-14080-8_17
19. Detweiler MF, Comer JS, Crum KI, Albano AM. Chapter 10 - social anxiety in children and adolescents: biological, developmental, and social considerations. In: Hofmann SG, DiBartolo PM, editors. Social Anxiety (Third Edition). San Diego: Academic Press (2014). p. 253–309. doi: 10.1016/B978-0-12-394427-6.00010-8
20. Davis TE, Guidry J, Ollendick TH. Specific phobias in children and adolescents. In: McKay D, Storch EA, editors. Handbook of Child and Adolescent Anxiety Disorders. Cham: Springer International Publishing (2023). p. 235–48. doi: 10.1007/978-3-031-14080-8_16
21. Szczygieł M, Pieronkiewicz B. Exploring the nature of math anxiety in young children: intensity, prevalence, reasons. Mathemat Think Learn. (2022) 24(3):248–66. doi: 10.1080/10986065.2021.1882363
22. Roos A-L, Goetz T, Voracek M, Krannich M, Bieg M, Jarrell A, et al. Test anxiety and physiological arousal: a systematic review and meta-analysis. Educ Psychol Rev. (2021) 33(2):579–618. doi: 10.1007/s10648-020-09543-z
23. Gross JJ, Jazaieri H. Emotion, emotion regulation, and psychopathology: an affective science perspective. Clin Psychol Sci. (2014) 2(4):387–401. doi: 10.1177/2167702614536164
24. Brehl A-K, Schene A, Kohn N, Fernández G. Maladaptive emotion regulation strategies in a vulnerable population predict increased anxiety during the COVID-19 pandemic: a pseudo-prospective study. J Affect Disord Rep. (2021) 4:100113. doi: 10.1016/j.jadr.2021.100113
25. Jaso BA, Hudiburgh SE, Heller AS, Timpano KR. The relationship between affect intolerance, maladaptive emotion regulation, and psychological symptoms. Int J Cogn Ther. (2020) 13(1):67–82. doi: 10.1007/s41811-019-00061-7
26. Paulus FW, Ohmann S, Möhler E, Plener P, Popow C. Emotional dysregulation in children and adolescents with psychiatric disorders. A narrative review. Front Psychiatry. (2021) 12:628252. doi: 10.3389/fpsyt.2021.628252
27. Xue M, Cong B, Ye Y. Cognitive emotion regulation for improved mental health: a chain mediation study of Chinese high school students. Front Psychol. (2023) 13:1041969. doi: 10.3389/fpsyg.2022.1041969
28. Loevaas MES, Sund AM, Lydersen S, Neumer S-P, Martinsen K, Holen S, et al. Does the transdiagnostic EMOTION intervention improve emotion regulation skills in children? J Child Fam Stud. (2019) 28(3):805–13. doi: 10.1007/s10826-018-01324-1
29. Finlon KJ, Izard CE, Seidenfeld A, Johnson SR, Cavadel EW, Ewing ESK, et al. Emotion-based preventive intervention: effectively promoting emotion knowledge and adaptive behavior among at-risk preschoolers. Dev Psychopathol. (2015) 27(4pt1):1353–65. doi: 10.1017/S0954579414001461
30. Espenes K, Tørmoen AJ, Rognstad K, Nilsen KH, Waaler PM, Wentzel-Larsen T, et al. Effect of psychosocial interventions on children and youth emotion regulation: a meta-analysis. Admin Pol Ment Health Ment Health Serv Res. (2024):2–7. doi: 10.1007/s10488-024-01373-3
31. Muris P, Mayer B, Cv L, Hofman S. Attentional control and psychopathological symptoms in children. Pers Individ Dif. (2008) 44(7):1495–505. doi: 10.1016/j.paid.2008.01.006
32. Eysenck MW, Derakshan N. New perspectives in attentional control theory. Pers Individ Dif. (2011) 50(7):955–60. doi: 10.1016/j.paid.2010.08.019
33. Shi R, Sharpe L, Abbott M. A meta-analysis of the relationship between anxiety and attentional control. Clin Psychol Rev. (2019) 72:101754. doi: 10.1016/j.cpr.2019.101754
34. DeJong H, Fox E, Stein A. Does rumination mediate the relationship between attentional control and symptoms of depression? J Behav Ther Exp Psychiatry. (2019) 63:28–35. doi: 10.1016/j.jbtep.2018.12.007
35. Hasani M, Ahmadi R, Saed O. Psychometric properties and factor structure of the repetitive thinking questionnaire: persian versions of the RTQ-31 and RTQ-10. Trends Psychiatry Psychother. (2022) 44:e20200058. doi: 10.47626/2237-6089-2020-0058
36. Waszczuk MA, Brown HM, Eley TC, Lester KJ. Attentional control theory in childhood: enhanced attentional capture by non-emotional and emotional distractors in anxiety and depression. PLoS One. (2015) 10(11):e0141535. doi: 10.1371/journal.pone.0141535
37. Hendry A, Jones EJH, Bedford R, Andersson Konke L, Begum Ali J, Bölte S, et al. Atypical development of attentional control associates with later adaptive functioning, autism and ADHD traits. J Autism Dev Disord. (2020) 50(11):4085–105. doi: 10.1007/s10803-020-04465-9
38. Edwards EJ, Zec D, Campbell M, Hoorelbeke K, Koster EHW, Derakshan N, et al. Cognitive control training for children with anxiety and depression: a systematic review. J Affect Disord. (2022) 300:158–71. doi: 10.1016/j.jad.2021.12.108
39. Abedini S, Habibi M, Abedini N, Achenbach TM, Semple RJ. A randomized clinical trial of a modified mindfulness-based cognitive therapy for children hospitalized with cancer. Mindfulness (N Y). (2021) 12(1):141–51. doi: 10.1007/s12671-020-01506-3
40. Creswell JD. Mindfulness interventions. Annu Rev Psychol. (2017) 68(1):491–516. doi: 10.1146/annurev-psych-042716-051139
41. Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychol. (2006) 62(3):373–86. doi: 10.1002/jclp.20237
42. Ahmadi R, Ahmadizadeh R, Hasani M, Saed O. Transdiagnostic versus construct-specific cognitive behavioural therapy for emotional disorders in patients with high anxiety sensitivity: a double-blind randomised clinical trial. Behav Change. (2021) 38(3):177–92. doi: 10.1017/bec.2021.6
43. Perrier M-F, Gurgel-Juarez N, Flowers HL, McCormick A, Short SJ. Mindfulness-based interventions for children and adolescents across all settings: a scoping review protocol. Syst Rev. (2020) 9(1):286. doi: 10.1186/s13643-020-01548-7
44. Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based Cognitive Therapy for Depression: A new Approach to Preventing Relapse. New York, NY: Guilford Press (2002).
45. Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based Cognitive Therapy for Depression. 2nd ed. New York, NY: The Guilford Press (2013). p. xix, 451.
46. Ni Y, Ma L, Li J. Effects of mindfulness-based stress reduction and mindfulness-based cognitive therapy in people with diabetes: a systematic review and meta-analysis. J Nurs Scholarsh. (2020) 52(4):379–88. doi: 10.1111/jnu.12560
47. Semple RJ, Lee J. Mindfulness-Based Cognitive Therapy for Anxious Children: A Manual for Treating Childhood Anxiety. Oakland, CA: New Harbinger Publications (2011).
48. Semple RJ, Lee J, Rosa D, Miller LF. A randomized trial of mindfulness-based cognitive therapy for children: promoting mindful attention to enhance social-emotional resiliency in children. J Child Fam Stud. (2010) 19(2):218–29. doi: 10.1007/s10826-009-9301-y
49. Bakhtiari M, Habibi Asgarabad M, Dehghani F, Alhosseini KA, Semple RJ. Effectiveness and satisfaction of mindfulness-based cognitive therapy for children on anxiety, depression, and internet addiction in adolescents: study protocol for a randomized control trial. PLoS One. (2025) 20(4):e0317824. doi: 10.1371/journal.pone.0317824
50. Cotton S, Kraemer KM, Sears RW, Strawn JR, Wasson RS, McCune N, et al. Mindfulness-based cognitive therapy for children and adolescents with anxiety disorders at-risk for bipolar disorder: a psychoeducation waitlist controlled pilot trial. Early Interv Psychiatry. (2020) 14(2):211–9. doi: 10.1111/eip.12848
51. LaGue A, Eakin G, Dykeman C. The impact of mindfulness-based cognitive therapy on math anxiety in adolescents. Preventing School Failure: Alternative Education for Children and Youth. (2019) 63(2):142–8. doi: 10.1080/1045988X.2018.1528966
52. Wright KM, Roberts R, Proeve MJ. Mindfulness-Based cognitive therapy for children (MBCT-C) for prevention of internalizing difficulties: a small randomized controlled trial with Australian primary school children. Mindfulness (N Y). (2019) 10(11):2277–93. doi: 10.1007/s12671-019-01193-9
53. Carsley D, Khoury B, Heath NL. Effectiveness of mindfulness interventions for mental health in schools: a comprehensive meta-analysis. Mindfulness (N Y). (2018) 9(3):693–707. doi: 10.1007/s12671-017-0839-2
54. Werner-Seidler A, Perry Y, Calear AL, Newby JM, Christensen H. School-based depression and anxiety prevention programs for young people: a systematic review and meta-analysis. Clin Psychol Rev. (2017) 51:30–47. doi: 10.1016/j.cpr.2016.10.005
55. Thibault RT, Pedder H. Excess significance and power miscalculations in neurofeedback research. NeuroImage: Clinical. (2022) 35:103008. doi: 10.1016/j.nicl.2022.103008
56. Treves IN, Li CE, Wang KL, Ozernov-Palchik O, Olson HA, Gabrieli JDE. Mindfulness supports emotional resilience in children during the COVID-19 pandemic. PLoS One. (2023) 18(7):e0278501. doi: 10.1371/journal.pone.0278501
57. Faul F, Erdfelder E, Lang A-G, Buchner A. G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) 39(2):175–91. doi: 10.3758/BF03193146
58. Cohen J. The Effect Size. Statistical Power Analysis for the Behavioral Sciences. Abingdon: Routledge (1988). p. 77–83.
59. Goldberg SB: A common factors perspective on mindfulness-based interventions. Na Rev Psychol. (2022) 1(10):605–19. doi: 10.1038/s44159-022-00090-8
60. Botvin GJ, Griffin KW. Life skills training: empirical findings and future directions. J Prim Prev. (2004) 25(2):211–32. doi: 10.1023/B:JOPP.0000042391.58573.5b
61. Goodman MS, Madni LA, Semple RJ. Measuring mindfulness in youth: review of current assessments, challenges, and future directions. Mindfulness (N Y). (2017) 8(6):1409–20. doi: 10.1007/s12671-017-0719-9
62. Lawlor MS, Schonert-Reichl KA, Gadermann AM, Zumbo BD. A validation study of the mindful attention awareness scale adapted for children. Mindfulness (N Y). (2014) 5(6):730–41. doi: 10.1007/s12671-013-0228-4
63. Spielberger CD, Edwards CD, Montouri J, Lushene R. State-trait anxiety inventory for children (STAI-CH). APA PsycTests. (1973):2–8. doi: 10.1037/t06497-000
64. Habibi M, Tahmasian K, Ferrer-Wreder L. Self-Efficacy in Persian adolescents: psychometric properties of a Persian version of the self-efficacy questionnaire for children (SEQ-C). Int Perspect Psychol. (2014) 3(2):93–105. doi: 10.1037/a0036059
66. Reis AH, de Oliveira SES, Bandeira DR, Andrade NC, Abreu N, Sperb TM. Emotion regulation checklist (ERC): preliminary studies of cross-cultural adaptation and validation for use in Brazil. Temas em Psicologia. (2016) 24(1):77–96. doi: 10.9788/TP2016.1-06
67. Pezeshki P, Doos Ali Vand H, Aslzaker M. Psychometric properties of children’s emotional regulation checklist in preschool children in Tehran. Zanko J Med Sci. (2021) 22(74):36–49. Available online at: http://zanko.muk.ac.ir/article-1-566-en.html
68. Muris P, de Jong PJ, Engelen S. Relationships between neuroticism, attentional control, and anxiety disorders symptoms in non-clinical children. Pers Individ Dif. (2004) 37(4):789–97. doi: 10.1016/j.paid.2003.10.007
69. van Son D, Marin CE, Boutris P, Rey Y, Lebowitz ER, Pettit JW, et al. Attending to the attentional control scale for children: confirming its factor structure and measurement invariance. J Anxiety Disord. (2021) 80:102399. doi: 10.1016/j.janxdis.2021.102399
70. Melendez R, Bechor M, Rey Y, Pettit JW, Silverman WK. Attentional control scale for children: factor structure and concurrent validity among children and adolescents referred for anxiety disorders. J Clin Psychol. (2017) 73(4):489–99. doi: 10.1002/jclp.22346
71. Attkisson CC, Zwick R. The client satisfaction questionnaire: psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann. (1982) 5(3):233–7. doi: 10.1016/0149-7189(82)90074-X
72. Butcher NJ, Monsour A, Mew EJ, Chan A-W, Moher D, Mayo-Wilson E, et al. Guidelines for reporting outcomes in trial protocols: the SPIRIT-outcomes 2022 extension. JAMA. (2022) 328(23):2345–56. doi: 10.1001/jama.2022.21243
73. Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. (1991) 59(1):12–9. doi: 10.1037//0022-006x.59.1.12
74. Willem K, Susan B, Catherine C, Poushali G, Benjamin J, Jesus M-M, et al. Effectiveness and cost-effectiveness of universal school-based mindfulness training compared with normal school provision in reducing risk of mental health problems and promoting well-being in adolescence: the MYRIAD cluster randomised controlled trial. Evid Based Ment Health. (2022) 25(3):1–3. doi: 10.1136/ebmental-2021-300396
75. Hill C, Waite P, Creswell C. Anxiety disorders in children and adolescents. Paediatr Child Health (Oxford). (2016) 26(12):548–53. doi: 10.1016/j.paed.2016.08.007
76. Chavira DA, Stein MB, Bailey K, Stein MT. Child anxiety in primary care: prevalent but untreated. Depress Anxiety. (2004) 20(4):155–64. doi: 10.1002/da.20039
77. Kendall PC, Safford S, Flannery-Schroeder E, Webb A. Child anxiety treatment: outcomes in adolescence and impact on substance use and depression at 7.4-year follow-up. J Consult Clin Psychol. (2004) 72(2):276–87. doi: 10.1037/0022-006X.72.2.276
78. Crescentini C, Capurso V, Furlan S, Fabbro F. Mindfulness-oriented meditation for primary school children: effects on attention and psychological well-being. Front Psychol. (2016) 7:00805. doi: 10.3389/fpsyg.2016.00805
79. Aghamohammadi F, Saed O, Ahmadi R, Kharaghani R. The effectiveness of adapted group mindfulness-based stress management program on perceived stress and emotion regulation in midwives: a randomized clinical trial. BMC Psychol. (2022) 10(1):123. doi: 10.1186/s40359-022-00823-7
80. Zhang Q, Zhou Y, Ho SMY. Active and avoidant coping profiles in children and their relationship with anxiety and depression during the COVID-19 pandemic. Sci Rep. (2022) 12(1):13430. doi: 10.1038/s41598-022-15793-4
81. Compas BE, Jaser SS, Bettis AH, Watson KH, Gruhn MA, Dunbar JP, et al. Coping, emotion regulation, and psychopathology in childhood and adolescence: a meta-analysis and narrative review. Psychol Bull. (2017) 143(9):939–91. doi: 10.1037/bul0000110
82. Cai RY, Hardan AY, Phillips JM, Frazier TW, Uljarević M. Brief report: emotion regulation influences on internalizing and externalizing symptoms across the normative-clinical Continuum. Front Psychiatry. (2021) 12:693570. doi: 10.3389/fpsyt.2021.693570
83. Silvers JA. Adolescence as a pivotal period for emotion regulation development. Curr Opin Psychol. (2022) 44:258–63. doi: 10.1016/j.copsyc.2021.09.023
84. Malinowski P. Neural mechanisms of attentional control in mindfulness meditation. Front Neurosci. (2013) 7:00008. doi: 10.3389/fnins.2013.00008
Keywords: adolescents, anxiety, attentional control, children, cognitive therapy, emotion regulation, mindfulness, mindfulness-based cognitive therapy for children
Citation: Kholghi H, Habibi Asgarabad M, Abolmaali Alhosseini K, Dehghani F and Semple RJ (2025) The effectiveness of mindfulness-based cognitive therapy for children on anxiety, attentional control, and emotion regulation in children: a study protocol. Front. Pediatr. 13:1459434. doi: 10.3389/fped.2025.1459434
Received: 4 July 2024; Accepted: 30 June 2025;
Published: 25 July 2025.
Edited by:
Tim S. Nawrot, University of Hasselt, BelgiumReviewed by:
Julia Kalmar, Heidelberg University, GermanyDaphne Berden, University of Hasselt, Belgium
Copyright: © 2025 Kholghi, Habibi Asgarabad, Abolmaali Alhosseini, Dehghani and Semple. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mojtaba Habibi Asgarabad, bW9qdGFiYS5oLmFzZ2FyYWJhZEBudG51Lm5v
†These authors have contributed equally to this work and share first authorship
‡This author shares senior authorship
§ORCID:
Habibeh Kholghi
orcid.org/0000-0002-0782-5254
Mojtaba Habibi Asgarabad
orcid.org/0000-0002-5011-2823
Khadijeh Abolmaali Alhosseini
orcid.org/0000-0002-9714-1816
Fahimeh Dehghani
orcid.org/0000-0002-9890-7430
Randye J. Semple
orcid.org/0000-0001-6469-2032
 Habibeh Kholghi1,†,§
Habibeh Kholghi1,†,§ Mojtaba Habibi Asgarabad
Mojtaba Habibi Asgarabad Randye J. Semple
Randye J. Semple