- 1Dessie Comprehensive Specialized Hospital, Dessie, Ethiopia
- 2Department of Pediatrics and Child Health Nursing, School of Nursing and Mid-Wifery, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
- 3Department of Medical Laboratory Sciences, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Background: Neonatal mortality rate is high in sub-Saharan Africa than high-income countries in relation to the growing wealth disparity. Different factors are linked with neonatal mortality in Ethiopia. Identification of the causes of death is the first step in reducing mortality rates. Thus, the aim of this study was to assess the magnitude of neonatal mortality and associated factors among neonates admitted in Neonatal Intensive Care Unit (NICU) in Dessie Comprehensive Specialized Hospital, Northeast Ethiopia.
Methods: A retrospective cohort study was conducted among 1,598 neonates admitted in Neonatal intensive care unit of Dessie Comprehensive Specialized Hospital from 28/06/2022 to 30/03/2023. Demographic and clinical data were abstracted from admission/discharge registration books; perinatal facility-based data abstraction form and patient medical records using data extraction checklist. Bivariable and multivariable analyses were conducted to determine the factors associated with neonatal mortality and variables with an adjusted relative risk (ARR) and its P-value < 0.05 were considered statistically significant. Model fitness was computed using Hosme-Lemeshow Goodness of fitness (P = 0.847).
Results: Among 1,598 neonates who were admitted in NICU were included in this study of which 914 (57.2%) were males. The magnitude of neonatal mortality was 10.2%. Prematurity (ARR = 2.58, 95% CI: 1.39–4.87, P < 0.009), sepsis (ARR = 1.47 95% CI: 1.02–2.11, P < 0.036), birth asphyxia (3.59 = 4.36, 95% CI: 2.40–6.87, P < 0.008), and respiratory distress syndrome (ARR = 2.93, CI: 1.47–5.30, P = 0.011) were independent predictors of neonatal mortality.
Conclusion: The magnitude of neonatal mortality was 10.2% which alarms the need of immediate collaborative actions for reduction of the burden particularly tackling on the causal factors such as prematurity, sepsis and birth asphyxia which leads adverse birth outcomes. Therefore, maternal counseling, giving focused ante natal care as well as behavior change communications might be considered to promote positive behaviors are recommended to avoid the leading causes of neonatal mortality.
1 Introduction
Neonatal mortality, which is defined as death within the first 28 days of life, is a crucial indicator for the health and wellbeing of newborns and is increasingly playing a significant role in the total under-five mortality rate. As a result, health officials are paying special attention to neonatal deaths (1). It can be further classified into late newborn fatalities (7–27 days) and early neonatal deaths (0–6 days), which occur after the seventh day but before the 28th day of life (2). The neonatal period, which lasts for the first 28 days of a neonate's existence, is the most dangerous stage of life because a baby is especially prone to making many of the physiological changes required for life outside the uterus at this time (3). The neonatal period is associated with an average global rate of 18 deaths per 1,000 live births (4) and 3–4 million global deaths per year where 99% of them was in low to middle income countries (5).
Despite a continuous decline in under-five mortality, approximately 7,000 newborns die each day, according to a 2017 WHO report (6, 7). However, the global neonatal mortality has significantly decreased from 5 million in 1990 to 2.4 million in 2019, newborn death still accounts for 47% of all deaths among children under the age of 5, with nearly one-third dying on the day of birth and nearly three-quarters dying within the first week of life (8). Furthermore, the evidence from Inter-Agency Group for Child Mortality Estimation reported that around 30 million neonates will die before their fifth birthday between 2017 and 2030 (9).
The burden of neonatal mortality is high in low- and middle-income countries (LMICs) than high-income countries. sub-Saharan Africa and Asia have the highest mortality rates. In the WHO Regions of Africa (28%) and South-East Asia (36%), neonatal mortality rates are two thirds higher (10). From sub-Saharan African countries, Ethiopia had the fifth-highest rate of neonatal deaths in 2016 (90/1,000) (11). Nearly 1 and 2 million deaths occur on the day of delivery and in the first week of life, respectively, and neonatal deaths account for 40% of all mortality of children under the age of 5 (12). When compared to the remainder of the month, where 50% of deaths occur and 75% occur throughout the first 7 days of life, a newborn has a 500 times higher chance of dying within the first 24 h (13). The rate of neonatal mortality is intrinsically linked to the health of the mother and the care she receives before, during and immediately after giving birth. Asphyxia and birth injuries usually result from poorly managed labor and delivery and lack of access to obstetric services (14, 15).
Preterm, prenatal asphyxia, and infections like sepsis, meningitis, and pneumonia account for more than 80% of newborn deaths (16). Particularly in Ethiopia, preterm birth, intrapartum problems, and infections account for roughly 90% of all fatalities. For 31% of neonatal deaths in Ethiopia, neonatal infection is the major contributing factor (17). Neonatal illnesses are challenging to treat with a single therapeutics or clinical interventions but it requires a systematic approach (16). Moreover, offering a continuum of care from pregnancy through birth and the immediate postpartum period, immediate causal factors could be readily avoided (18, 19). In addition, reduced newborn morbidity and mortality can be achieved through skilled care during pregnancy, labour, and the postpartum period (20).
The number of deaths and the percentage of neonatal deaths are predicted to increase to 69 million deaths and 52%, respectively, by 2030. Target 3.2 of the Sustainable Development Goals (SDGs) 3 shifts the focus to newborn health, with the goal of bringing the rate of neonatal mortality below 12 per 1,000 live births by 2030 (21, 22). But, on the basis of current trends more than 60 nations will fall short of SDG target by 2030. Similarly, by 2050 over half of them won't have accomplished the goal (23). Furthermore, the Mini-Ethiopian Demographic and Health Survey (EDHS) report states that Ethiopia has a neonatal mortality rate of 30% per 1,000 live births (4). Neonatal mortality increased from 28 per 1,000 live births in 2016 to 30 per 1,000 live births in 2019 according to a report from EDHS-2019 indicating NMR is still a big public health problem in Ethiopia (24).
Despite a significant reduction in maternal and child mortality in Ethiopia, neonatal deaths are still occurring in substantial numbers. A piece of evidence has also tried to indicate the problem of NMR, but the problem is quite different due to ecological factors. Additionally, previous studies were performed using a small sample size, which might lack generalizability. Thus, evidence with a cohort study design and higher sample size can provide more reliable evidence for scientific communities, as well as policy makers and decision makers. Therefore, the aim of this study was to assess the magnitude of neonatal mortality and to identify associated factors among neonates admitted in Neonatal intensive care unit in Dessie Comprehensive Specialized Hospital, Northeast Ethiopia.
2 Methods and materials
2.1 Study area, design, period and population
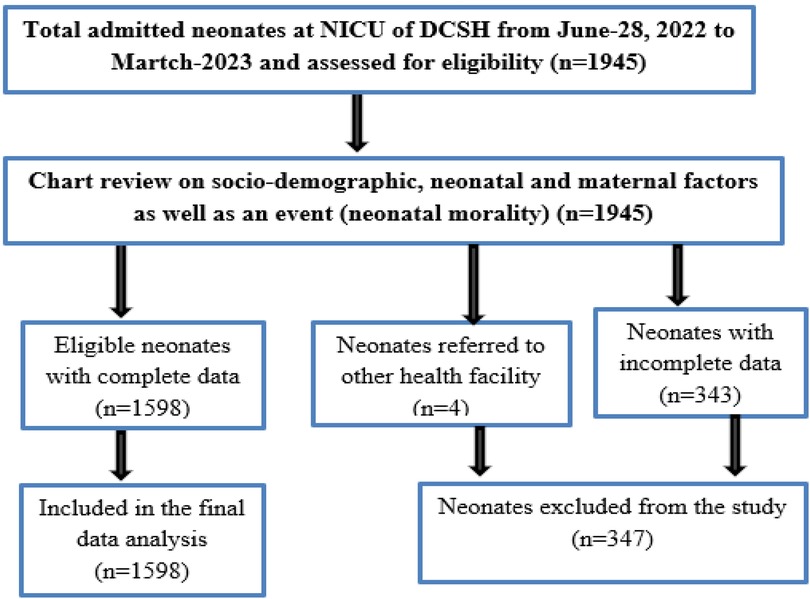
A retrospective cohort study of neonatal death was conducted from 28/06/2022 to 30/03/2023 among a total of 1,598 neonates admitted in Neonatal intensive care unit (NICU) of Dessie Comprehensive Specialized Hospital (DCSH) (Supplementary Data Sheet 1). The DCSH neonatal care unit has a 38-bed capacity with sections of term, preterm and septic/postop sections and equipped with 04 incubators, 07 phototherapy, 13 radiant warmers, 04 CPAP machine, 04 concentrators and 01 pulse oximetry. The unit is headed by senior consultant pediatricians together with a team of 4 general practitioners, interns, 11 neonatal nurses, 12 BSc nurse and other paramedical staff. Chart review of this study was carried-out from 01/05/2023 to 30/05/2023. Neonates chart with missing data for socio-demographic, clinical and epidemiological variables were excluded from the study analysis.
2.1.1 Eligibility criteria
All neonates who were admitted in NICU of Dessie Compressive Specialized hospital from June-28, 2022 to March-2023 were included. However, neonates who were referred to other health facilities and those had incomplete medical records were excluded from the study (Figure 1).
2.1.2 Variables
The dependent variable was neonatal mortality while socio-demographic factors (age of the neonate in days and the mother, sex of the neonates, and place of residence), neonatal factors (birth weight, medical illnesses, danger signs, length of stay on admission and body temperature) and maternal factors (ANC service, feeding type to their neonate, breast feeding initiation time, place of delivery, mode of delivery, birth order, gravidity, history of neonatal death, HIV status of the mother, chronic disease of the mother, multiple pregnancies and gestational age) were considered as explanatory variables.
2.1.3 Operational definitions
• Neonatal death: Death of a neonate within the first 28 completed days of life that was born alive
• Early neonatal death: The death of neonate that occur with in the first 7 days of life
• Late neonatal death: Death of a neonate that occur between 7 and 28 completed days of life
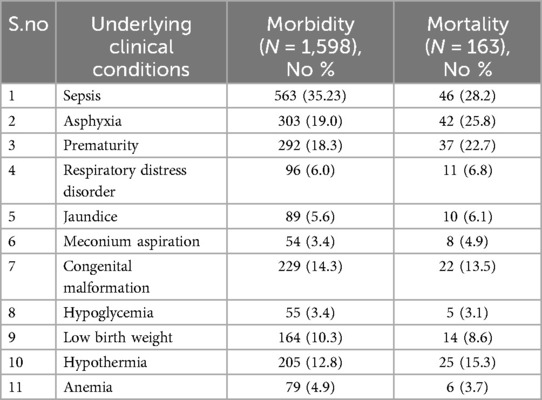
• Morbidity: is defined as the presence of confirmed medical conditions in a neonate within the first 28 days of life such as sepsis, asphyxia, prematurity, respiratory distress disorder, jaundice, meconium aspiration, congenital malformation, hypoglycemia, low birth weight, hypothermia and anemia etc.
2.1.4 Data collection
Data were abstracted during June-2022–March,2023 from the medical records of the neonates, NICU register book, and Facility based data abstraction form of Perinatal Death Surveillance and Response (PDSR) retrospectively using pre-prepared and pre-tested data extraction checklist containing socio-demographic factors (age of the neonate in date and the mother, sex of the neonates, and place of residence), neonatal factors (birth weight, medical illnesses, danger signs, length of stay on admission and body temperature), and maternal factors of neonatal deaths (ANC service, feeding type to their neonate, breast feeding initiation time, place of delivery, mode of delivery, birth order, gravidity, history of neonatal death, HIV status of the mother, chronic disease of the mother, multiple pregnancies and gestational age). The data was collected by 4 health care workers (1 neonatal nurse and 3 BSc nurse) with a close supervision by senior Maternal neonatal and child health (MNCH) supervisor who had an experience in NICU. Only one person did the data checking and recording per neonate.
2.1.5 Statistical analysis
Patient data were registered into Microsoft excel and analyzed using SPSS version 25 software (SPSS Inc., Chicago, IL, USA). Categorical variables were summarized by frequencies and percentages, and continuous variables were summarized by mean ± standard deviation (SD). Bivariable logistic regression analyses were performed to assess predicting factors associated with neonatal mortality. Variables that were found to be significant in bivariable analysis (P < 0.25) were included in the multivariable backward stepwise logistic regression model to identify factors independently associated with neonatal mortality. Model fitness was computed using Hosme-Lemeshow Goodness of fitness (P = 0.847). Finally, variables with an adjusted relative risk (ARR) with a P-values < 0.05 were considered significant.
3 Result
3.1 Socio demographic, neonatal and maternal characteristics
A total of 1,598 neonates who were admitted in NICU had complete medical records and included in the study. Majority of the neonates were male (57.2%). Almost tenfold of the neonates were admitted in the age of 1–7 days with the maximum age of 20 days and the median age of 1 day. Around two thirds of (65.7%) of the neonates were from rural residence. Furthermore, around 2/3rd (67.3%) of neonates were delivered from mothers of gestational age 37–42 weeks. Regarding maternal and neonatal factors, nearly half (47.9%) of the neonates were delivered from mothers had history of four and above visits of ANC. With regard to place of delivery, majority 1,085 (67.9%) were delivered at same heath facility. Similarly, majority of neonates 1,309 (81.9%) were also delivered by SVD and 1,594 (99.7%) were single on births. However, more than half of (60.6%) neonates were delivered from mothers with history of 2–4 parity (Table 1).
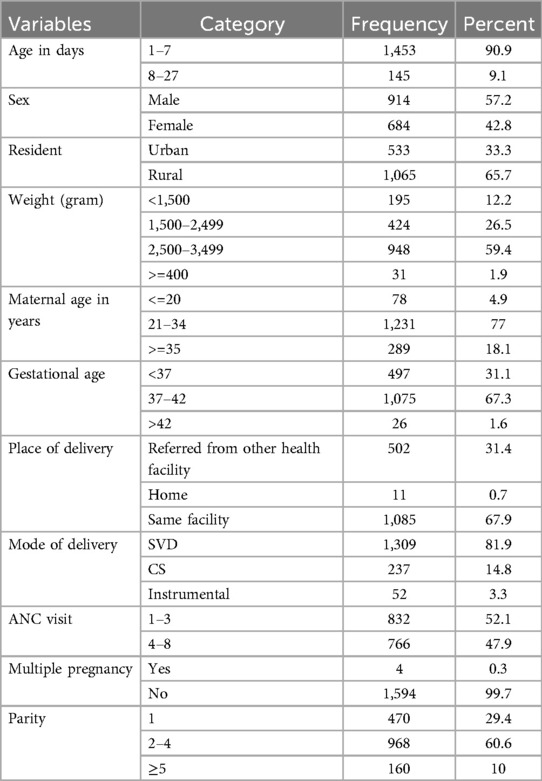
Table 1. Socio demographic, neonatal and maternal characteristics of neonates from June 2022 to March 2023 at Dessie comprehensive specialized hospital.
3.2 Magnitude of neonatal mortality
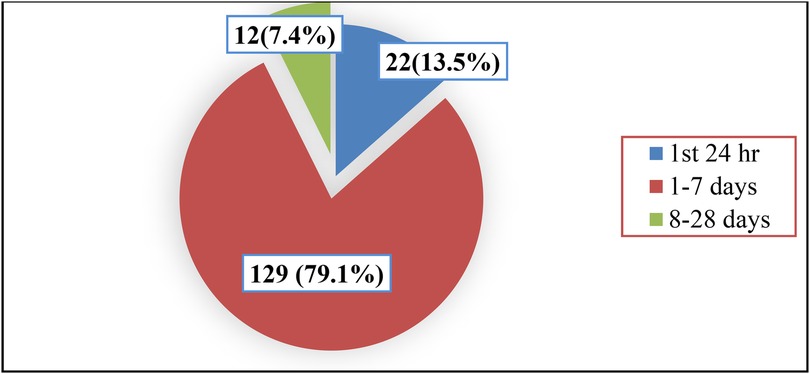
Out of the total 1,598 neonates, 1,435 were improved and discharged alive; however, 10.2% (n = 163; 95%CI: 8.8–11.7) of the neonates were died. About 79.1% (129/163) of neonates were died within 1–7 days of birth while 13.5% (22/163) were died within the first 24 h. Totally, the magnitude of neonatal mortality within the first week of birth was nearly 93% (151/163) (Figure 2).
The top three predominant causes of neonatal morbidity or causes of neonatal admission were sepsis (35.2%, asphyxia (19%), and prematurity (18.2%). Likewise, the predominant causes of morbidity were also reported as a causes of neonatal mortality (Table 2).
3.3 Factors associated with neonatal death among neonates admitted at NICU
The magnitude of neonatal mortality was assessed in the current study using a variety of risk factors. In bivariable and multivariable analysis, Preterm new borns (prematurity of neonates) who had higher risk of death than those who born term babies (ARR = 2.586, 95%CI 1.392–4.877, P = 0.009), and those newborn babies who had sepsis with sepsis developed new borns were 1.470 times at risk to die than those non sepsis developed babies (ARR = 1.470, 1.025–2.110, P = 0.036). Neonates faced birth asphyxia were 3.595 times at risk to die than those who were non asphyxiated newborns had non asphyxia new borns (ARR = 3.595, CI: 2.405–6.874, P = 0.008). Moreover, the risk of neonatal death was about 2.9 times higher in neonates who had respiratory distress syndrome (ARR = 2.932, CI: 1.475–5.301, P = 0.011) than their counter parts (Table 3).
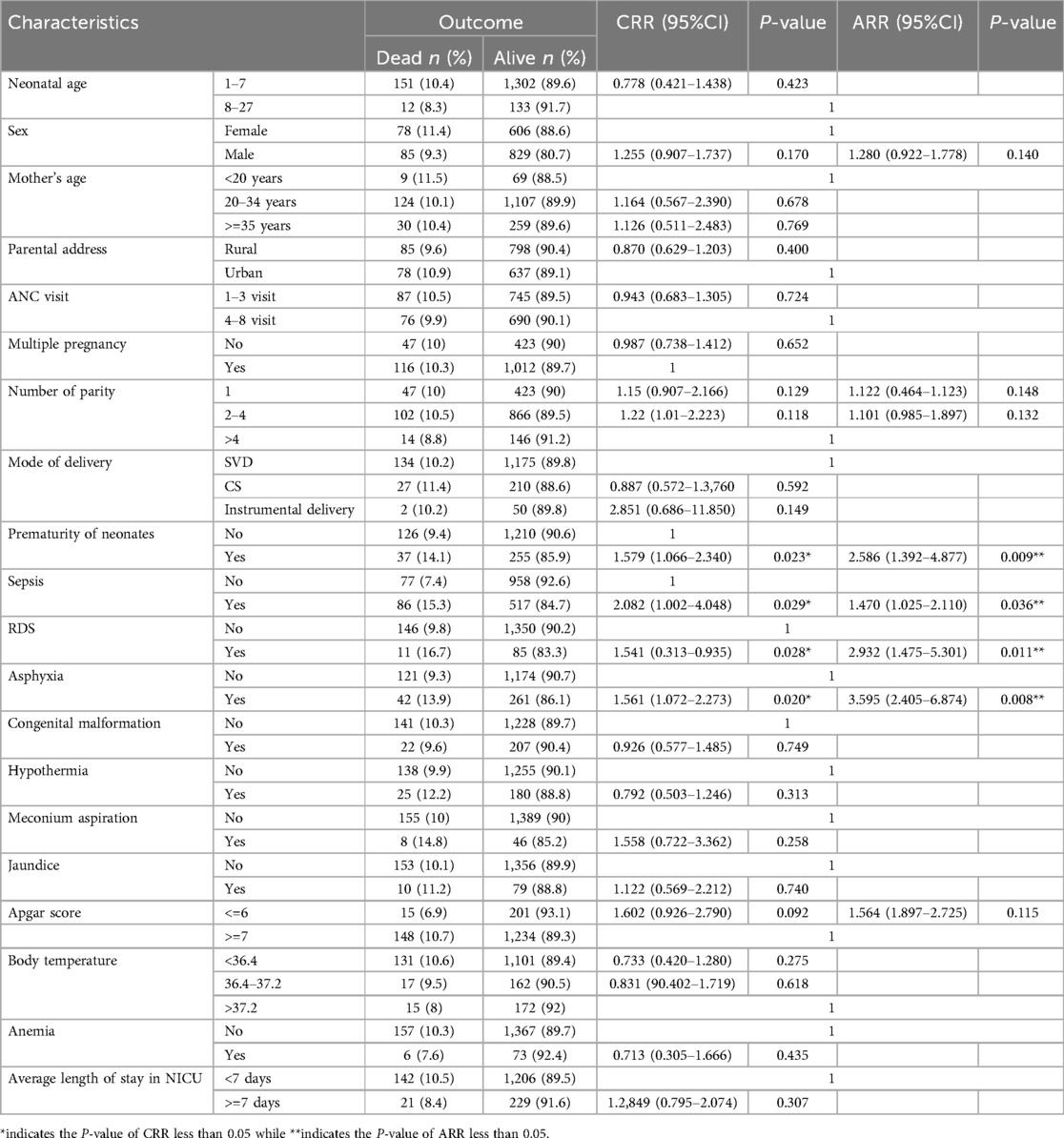
Table 3. Bivariable and multivariable analysis of risk factors associated with neonatal mortality among admitted neonates in NICU at Dessie comprehensive specialized hospital June 2022–March, 2023.
4 Discussion
Neonatal mortality remains a severe public health issue, especially in low- and middle-income countries like Ethiopia, despite numerous advancements and treatments made to increase the survival of babies. Thus, the aim of the current study was to identify magnitude and associated factors of neonatal mortality at Dessie Comprehensive Specialized Hospital, Northern Ethiopia. The magnitude of neonatal mortality among NICU admitted neonates was 10.2% (95% CI: 8.8–11.7) which was comparable with previous findings reported from 11.4% prevalence in Ethiopia (25). On the other hand, the finding of the current study was lower than the finding of previous Ethiopian studies reported (16.7%) (13) and (18.34%) (26).
Moreover, it was higher than 4.37% neonatal death reported from Ethiopia (27). The variations might be due to study setting such as this study was conducted among neonates in NICU who have high risk of death than their counterparts. In addition, the variation can be explained by differences in skill of health professionals, presence of sociocultural and socioeconomic differences across regions of Ethiopia as well as the difference in sample sizes (9, 28) and economic disparities among study participants (9, 29, 30). Moreover, difference in health seeking behavior and health service utilization such as institutional delivery by skilled care providers and health seeking for sick neonates. As the quality of care can be affected by the availability of equipment and skilled professionals, the higher magnitude of neonatal death found in this study can be claimed to be explained by this condition.
The magnitude of early neonatal death in this study was 93% which was consistent with previous finding reported from northeastern Ethiopia. This is in line with other prior studies done in Diredewa (30) and Mizan- Tapi (9). However, the finding was higher than studies in Jimma and Bahir Dar (15, 31). The possible reason of higher magnitude of early neonatal death could be due to the fact that the first few hours of age after birth are very critical to adapt the environment, simple and inexpensive measures can decrease neonatal mortality in the first 24 h of life. Likewise, high number of prematurity-related deaths (majority of which are secondary to respiratory distress syndrome), where maximum deaths occurred in the first 72 h of age. In addition, it could be due to majority of neonatal mortality in developing countries are related to conditions of labor, intra- partum and the immediate newborn care practices which could be further associated with prematurity, sepsis, respiratory distress syndrome and birth asphyxia. This again clearly pointed out that neonatal survival interventions have to target the intra-partum as well as immediate and early neonatal periods.
The risk of neonatal mortality was significantly associated with clinical characteristics of neonatal factors which aggravates neonatal mortality. In our study, the risk of neonatal mortality was observed to rise as complication of prematurity advances, it was significantly associated with the magnitude of neonatal death (P < 0.009). Of 18.3% of the study subjects who were complication of prematurity, 14.5% of neonates were dead, this is due to the fact that, premature neonates are at higher risk of dying due to complications such as respiratory problems, feeding difficulties, poor regulation of body temperature and recurrent infections (32).
Neonates admitted to neonatal intensive care unit with birth asphyxia had 3.595 time at risk of dying than their counterpart. This could be due to the fact that oxygen deficit at delivery (birth asphyxia) can lead to severe hypoxic ischemic organ damage in newborns followed by a fatal outcome or severe life-long pathologies. This finding is consistent with a study done in Somalia region (33). This difference might be due to health service utilization, study period and sample size variations. In premature neonates’ organs are not enough matured and one organ is likely to also affect the function of other organ, as a result of this the outcome of neonates was evolving and death.
The findings of this study indicate that the risk of neonatal death is significantly higher among neonates diagnosed with neonatal sepsis compared to those without sepsis. This may because of sepsis can rapidly progress in neonates, causing severe systemic inflammation and multi-organ failure, which can overwhelm their ability to cope. Moreover, the subtle symptoms of sepsis may be mistaken for other conditions, leading to delayed recognition and treatment, ultimately resulting in worse outcomes. Additionally, these findings align with existing literature that identifies neonatal sepsis as a significant contributor to neonatal mortality (34–36).
Moreover, the risk of neonatal death was significantly higher in neonates who had respiratory distress syndrome (P = 0.011) than neonates who haven't respiratory distress syndrome. This could be due to the fact that, respiratory distress significantly increases neonatal mortality due to factors like insufficient surfactant, leading to lung collapse, and impaired gas exchange. These issues can cause severe hypoxemia, acidosis, and multi-organ dysfunction, ultimately increasing the risk of death, especially in premature infants. The study was identified based on the documented data and could not display all factors that were not documented in the patient's files such as parents’ educational status, wealth index, training and educational status of health professional providing services, infection prevention practices. Thus, variations in physicians' clinical diagnosis, completeness and quality of the recorded information were limitations of the study.
5 Conclusion and recommendation
The study revealed that the magnitude of neonatal mortality was high which alarms the need of immediate collaborative actions for reduction of the burden particularly avoiding on the causal factors such as prematurity, sepsis and birth asphyxia which leads adverse birth outcomes. The majority of neonatal mortality was occurred in the first week of life. Therefore, maternal counseling, giving focused ante natal care as well as behavior change communications might be considered to promote positive behaviors are recommended to avoid the leading causes of neonatal mortality.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Institutional Review Board of the College of Medicine and Health Sciences, Wollo University. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because the data is retrospective were the participants couldn't be directly participated.
Author contributions
BA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. RA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. GM: Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation. HE: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. EM: Writing – original draft, Writing – review & editing. AS: Writing – original draft, Writing – review & editing. AbM: Writing – original draft, Writing – review & editing. NF: Writing – original draft, Writing – review & editing. BB: Writing – original draft, Writing – review & editing. AdM: Writing – original draft, Writing – review & editing. MN: Writing – original draft, Writing – review & editing. FG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by Dessie Comprehensive Specialized Hospital.
Acknowledgments
The authors thank the study participants and data collectors for their support and unreserved cooperation in making this study to be a fruitful work. We would like to also thank Dessie Comprehensive Specialized Hospital for financial support for this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2025.1466599/full#supplementary-material
References
1. You D, Hug L, Ejdemyr S, Beise J, Perez-Escamilla R, Moran V, et al. Levels and trends 317 in child mortality. Estimates developed by the UN Inter-agency Group for Child Mortality 318 Estimation (IGME). Report 2015. Matern Child Nutr. (2016) 52(3):1–6.
2. WHO U, Mathers C. Global strategy for women's, children's and adolescents' health (2016-320 2030). Organization. (2016) 201:4–103.
3. Gunasekhar R, Somasekhara R. A study of neonatal morbidity and mortality in government general hospital, Srikakulam Andhra Pradesh, India. Int J Contemp Pediatrics. (2019) 6:1485–90. doi: 10.18203/2349-3291.ijcp20192573
4. Fabian C. Un-chained: experiments and learnings in crypto at UNICEF. Innovations: 325 Technology, Governance, Globalization. (2018) 12(1–2):30–45.
5. Victora CG, Barros AJ, França GV, da Silva IC, Carvajal-Velez L, Amouzou A. The contribution of poor and rural populations to national trends in reproductive, maternal, newborn, and child health coverage: analyses of cross-sectional surveys from 64 countries. Lancet Glob Health. (2017) 5(4):e402–7. doi: 10.1016/S2214-109X(17)30077-3
6. Organization WH. World Health Statistics 2016 [OP]: Monitoring Health for the Sustainable Development Goals (SDGs). Geneva: World Health Organization (2016).
7. Arunda M, Emmelin A, Asamoah BO. Effectiveness of antenatal care services in reducing neonatal mortality in Kenya: analysis of national survey data. Glob Health Action. (2017) 10(1):1328796. doi: 10.1080/16549716.2017.1328796
8. Organization WH. Newborns: Improving Survival and Well-being. (2020). Available online at: https://www.who.int/westernpacific/newsroom/fact-sheets/detail/newborns-reducing-mortality (Accessed June 10, 2025).
9. Mekonnen T, Tenu T, Aklilu T, Abera T. Assessment of neonatal death and causes among admitted neonates in neonatal intensive care unit of Mizan Tepi University teaching hospital, Bench Maji zone, south-west Ethiopia, 2018. Clin Mother Child Health. (2018) 15(4):2. doi: 10.4172/2090-7214.1000305
10. Cresswell JA, Campbell OM, De Silva MJ, Filippi V. Effect of maternal obesity on neonatal death in sub-Saharan Africa: multivariable analysis of 27 national datasets. Lancet. (2012) 380(9850):1325–30. doi: 10.1016/S0140-6736(12)60869-1
11. Organization WH. Roadmap Towards Ending TB in Children and Adolescents. 3rd edn. Geneva: World Health Organization (2023).
12. Gentile A, Bhutta Z, Bravo L, Samy AG, Garcia RDJ, Hoosen A, et al. Pediatric disease burden and vaccination recommendations: understanding local differences. Int J Infect Dis. (2010) 14(8):e649–58. doi: 10.1016/j.ijid.2009.11.006
13. Hadgu FB, Gebretsadik LG, Mihretu HG, Berhe AH. Prevalence and factors associated with neonatal mortality at ayder comprehensive specialized hospital, northern Ethiopia. A cross-sectional study. Pediatric Health Med Ther. (2020) 11:29–37. doi: 10.2147/PHMT.S235591
14. Bryce J, Boschi-Pinto C, Shibuya K, Black RE. WHO estimates of the causes of death in children. Lancet. (2005) 365(9465):1147–52. doi: 10.1016/S0140-6736(05)71877-8
15. Debelew GT, Afework MF, Yalew AW. Determinants and causes of neonatal mortality in Jimma Zone, Southwest Ethiopia: a multilevel analysis of prospective follow up study. PLoS One. (2014) 9(9):e107184. doi: 10.1371/journal.pone.0107184
16. Hug L, Mishra A, Lee S, You D, Moran A, Strong KL, et al. A Neglected Tragedy the Global Burden of Stillbirths: Report of the UN Inter-Agency Group for Child Mortality Estimation (UN IGME). New York, NY: United Nations Children’s Fund (2020).
17. Berhan Y, Berhan A. Perinatal mortality trends in Ethiopia. Ethiop J Health Sci. (2014) 24:29–40. doi: 10.4314/ejhs.v24i0.4S
18. Weldearegawi B, Melaku YA, Abera SF, Ashebir Y, Haile F, Mulugeta A, et al. Infant mortality and causes of infant deaths in rural Ethiopia: a population-based cohort of 3684 births. BMC Public Health. (2015) 15(1):1–7. doi: 10.1186/s12889-015-2090-x
19. Kokeb M, Desta T. Institution based prospective cross-sectional study on patterns of neonatal morbidity at Gondar University Hospital Neonatal Unit, North-West Ethiopia. Ethiop J Health Sci. (2016) 26(1):73–9. doi: 10.4314/ejhs.v26i1.12
20. Mengesha HG, Sahle BW. Cause of neonatal deaths in Northern Ethiopia: a prospective cohort study. BMC Public Health. (2017) 17(1):1–8. doi: 10.1186/s12889-016-3979-8
21. You D, Hug L, Ejdemyr S, Idele P, Hogan D, Mathers C, et al. Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN inter-agency group for child mortality estimation. Lancet. (2015) 386(10010):2275–86. doi: 10.1016/S0140-6736(15)00120-8
22. Gelband H, Sankaranarayanan R, Gauvreau CL, Horton S, Anderson BO, Bray F, et al. Costs, affordability, and feasibility of an essential package of cancer control interventions in low-income and middle-income countries: key messages from disease control priorities. Lancet. (2016) 387(10033):2133–44. doi: 10.1016/S0140-6736(15)00755-2
23. Organization WH. Global Strategy for Women’s, Children’s and Adolescents’ Health 2016–2030. Geneva: WHO (2015).
24. Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF. 2021. Ethiopia Mini Demographic and Health Survey 2019: Final Report. Rockville: EPHI and ICF (2019).
25. Thomas G, Demena M, Hawulte B, Eyeberu A, Heluf H, Tamiru D. Neonatal mortality and associated factors among neonates admitted to the neonatal intensive care unit of Dil Chora referral hospital, Dire Dawa City, Ethiopia, 2021: a facility-based study. Front Pediatr. (2022) 9:793160. doi: 10.3389/fped.2021.793160
26. Abera T, Bayisa L, Bekele T, Dessalegn M, Mulisa D, Gamtessa LC. Neonatal mortality and its associated factors among neonates admitted to Wollega University referral hospital neonatal intensive care unit, East Wollega, Ethiopia. Glob Pediatr Health. (2021) 8:2333794X211030157. doi: 10.1177/2333794X211030157
27. Kebede B, Gebeyehu A, Sharma HR, Yifru S. Prevalence and associated factors of neonatal mortality in North Gondar Zone, Northwest Ethiopia. Ethiop J Health Dev. (2012) 26(2):66–71.
28. David N, Ezechi O, Wapmuk A, Gbajabiamila T, Ohihoin A, Herbertson E, et al. Child sexual abuse and disclosure in south western Nigeria: a community based study. Afr Health Sci. (2018) 18(2):199–208. doi: 10.4314/ahs.v18i2.2
29. Alebel A, Wagnew F, Petrucka P, Tesema C, Moges NA, Ketema DB, et al. Neonatal mortality in the neonatal intensive care unit of Debre Markos referral hospital, Northwest Ethiopia: a prospective cohort study. BMC Pediatr. (2020) 20:1–11. doi: 10.1186/s12887-020-1963-z
30. Woday Tadesse A, Mekuria Negussie Y, Aychiluhm SB. Neonatal mortality and its associated factors among neonates admitted at public hospitals, pastoral region, Ethiopia: a health facility based study. PLoS One. (2021) 16(3):e0242481. doi: 10.1371/journal.pone.0242481
31. Tewabe T, Mehariw Y, Negatie E, Yibeltal B. Neonatal mortality in the case of Felege Hiwot referral hospital, Bahir Dar, Amhara regional state, north west Ethiopia 2016: a one year retrospective chart review. Ital J Pediatr. (2018) 44:1–5. doi: 10.1186/s13052-018-0498-5
32. Jain K, Sankar MJ, Nangia S, Ballambattu VB, Sundaram V, Ramji S, et al. Causes of death in preterm neonates (<33 weeks) born in tertiary care hospitals in India: analysis of three large prospective multicentric cohorts. J Perinatol. (2019) 39(Suppl 1):13–9. doi: 10.1038/s41372-019-0471-1
33. Mohamed HA, Shiferaw Z, Roble AK, Kure MA. Neonatal mortality and associated factors among neonates admitted to neonatal intensive care unit at public hospitals of Somali regional state, eastern Ethiopia: a multicenter retrospective analysis. PLoS One. (2022) 17(5):1–16. doi: 10.1371/journal.pone.0268648
34. Desalew A, Sintayehu Y, Teferi N, Amare F, Geda B, Worku T, et al. Cause and predictors of neonatal mortality among neonates admitted to neonatal intensive care units of public hospitals in eastern Ethiopia: a facility-based prospective follow-up study. BMC Pediatr. (2020) 20:1–11. doi: 10.1186/s12887-020-02051-7
35. Alemu AY, Belay GM, Berhanu M, Minuye B. Determinants of neonatal mortality at neonatal intensive care unit in northeast Ethiopia: unmatched case-control study. Trop Med Health. (2020) 48:1–10. doi: 10.1186/s41182-020-00232-9
Keywords: associated factors, Ethiopia, magnitude, neonate, neonatal intensive care unit, neonatal mortality
Citation: Adugna B, Asaminew R, Maru GS, Eshetie HA, Mohammed E, Samuel A, Mekonnnen A, Fentaw N, Belay B, Mekonen A, Nigussie M, Getaneh FB and Gedefie A (2025) Magnitude and associated factors of neonatal mortality among neonates admitted at Dessie comprehensive specialized hospital, Northeast, Ethiopia. Front. Pediatr. 13:1466599. doi: 10.3389/fped.2025.1466599
Received: 18 July 2024; Accepted: 27 May 2025;
Published: 10 July 2025.
Edited by:
Molla Yigzaw Birhanu, Debre Markos University, EthiopiaReviewed by:
Mselenge Hamaton Mdegela, University of Greenwich, United KingdomAgize Asfaw, Wolkite University, Ethiopia
Copyright: © 2025 Adugna, Asaminew, Maru, Eshetie, Mohammed, Samuel, Mekonnnen, Fentaw, Belay, Mekonen, Nigussie, Getaneh and Gedefie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alemu Gedefie, YWxlbXVnZWRlZmllQGdtYWlsLmNvbQ==
 Berhanu Adugna1
Berhanu Adugna1 Robel Asaminew
Robel Asaminew Abdulmelik Mekonnnen
Abdulmelik Mekonnnen Fekadeselassie Belege Getaneh
Fekadeselassie Belege Getaneh Alemu Gedefie
Alemu Gedefie