- 1Department of Pediatrics and Child Health Nursing, School of Nursing, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 2Department of Emergency and Critical Care Nursing, School of Nursing, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 3Department of Comprehensive Nursing, School of Nursing, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Introduction: Globally, there is consensus that traditional medicine (TM) has its benefit in solving health-related issues; however, a challenge lies in the lack of standardized scientific criteria to guide its appropriate use. Evidence suggests that, in some cases, traditional medicine may exacerbate health problems and lead to complications. Although many studies have explored traditional medicine use among adults, there is limited research on parental use of traditional medicine for children, particularly in Harar City. Therefore, the aim of this study was to determine the prevalence and associated factors of parental traditional medicine use for children in Harar City, Eastern Ethiopia.
Research methods: A cross-sectional study was carried out in the community of Harar City between 15 October and 15 November 2024. A multistage sampling procedure was used to obtain 348 parents. The required data were assembled through in-person interviews. The data that assembled were analyzed using Stata statistical software, version 16.0. To determine the associated factors with the outcome variable, multivariable logistic regression was applied via adjusted odds ratio (aOR) with a 95% confidence interval (CI). Independent variables with p < 0.05 were declared as significantly associated variables with the outcome variable.
Results: Approximately 348 parents were sampled for the study with a response rate of 100%. The proportion of parental TM use for children was 76.15% (95% CI: 71.8–80.5). Parents with more than four children (aOR = 3.24, 95% CI: 1.13–9.28), with a good attitude toward TM (aOR = 1.98, 95% CI: 1.02–3.86), and who were members of community-based health insurance (aOR = 0.34, 95% CI: 0.19–0.63) were independent variables associated with parental traditional medicine use for children.
Conclusion: Approximately three-quarters of parents reported using traditional medicine for their children. This practice was influenced by modifiable factors. Therefore, stakeholders in the health sector should give focused attention to the key factors influencing parental use of traditional medicine for children.
Introduction
Traditional medicine (TM) encompasses the therapeutic practices rooted in traditional knowledge and culturally specific beliefs that have been developed over generations within various societies, including indigenous communities, before the advent of modern science (1, 2). It refers to the knowledge, skills, and practices based on the theories, beliefs, and experiences indigenous to different cultures—whether scientifically explained or not—used for maintaining health as well as for the prevention, diagnosis, and treatment of physical and mental illnesses (3, 4).
In the previous decade, the development and mass production of chemically synthesized drugs have revolutionized healthcare in most parts of the world (5). However, large sections of the population in developing countries still depend on traditional medicine for their primary healthcare needs (6). The global disease burden is growing rapidly; as a result, indigenous African medicine offers an alternative and affordable remedy that is accessible to millions who cannot afford or access modern healthcare due to its high cost and limited availability (7, 8).
Various forms of traditional medicine are practiced across different cultures, reflecting their diversity. These include bone setting, puncture-induced bleeding, cupping, cauterization, scarification, tooth extraction (9), use of mineral substances, herbal remedies, animal products, and spiritual therapies like tsebel (holy water). Manual techniques are also applied, either alone or in combination (10), through non-invasive or invasive procedures (11). People depend on traditional medicine because it is easily accessible, affordable, and low cost, particularly in contexts marked by poverty, illiteracy, and limited access to modern healthcare services (12, 13).
Globally, approximately 80% of the population relies on TM for their primary healthcare needs, with most remedies derived from natural products, animals, and plants (14, 15). In developing countries, specifically in Asia and Africa, the use of TM is in the range of 70%–95% (16). In Africa, especially sub-Saharan countries, approximately 90% of the population depends on TM (17, 18). In Ethiopia, more than 80% of the population depends on TM for their primary healthcare needs (19). Approximately 71%–90.3% of Ethiopian parents have used different types and forms of TM for their children (20). The most commonly practiced traditional therapies include herbal remedies (66.9%), religious treatments (52.8%), massage (22.8%), bone setting (21.8%), and cutaneous cauterization (43.6%) (20, 21).
Even though traditional medicine offers benefits for human health, a major concern lies in the lack of scientifically proven standards—particularly regarding appropriate usage, dosage, and route of administration (22). Studies have shown that some traditional medicine therapies used in children by their parents have had adverse outcomes (23). More than half of all TMs are prescribed, dispensed, and sold illegally by traditional healers and approximately half of all users use TM incorrectly (24).
Many patients are hospitalized due to the adverse effect of and complications associated with TM (21, 25). The secretive nature of some traditional healers creates barriers to effective treatment and prevention of such complications (26). Invasive traditional herbal medicines result in a wide range of complications, from mild allergic reactions and gastrointestinal issues to severe outcomes such as respiratory problems, blood clotting disorders, blood pressure issues, liver toxicity, renal failure, and multi-organ dysfunction syndrome (27). Among children who receive invasive traditional herbal medicine, approximately 30.96% develop multi-organ dysfunction syndrome (28). In addition, the most commonly affected organs include the kidney (renal failure, 17.74%), nervous system (neurological failure, 15.16%), and heart (heart failure, 14.52%), with nearly one-third of them dying in intensive care units (29). Over 25% of children admitted to the pediatric intensive care units were suspected of experiencing toxicity due to traditional herbal medicine use (30, 31).
Traditional cutaneous cauterization results in a wide variety of complications, including wound infection, abscess, septic shock, deep skin burn, disfigurement from contractures, scars, hair loss, keloids, carcinoma, oral complications, aspiration, edema, and viral transmission, including hepatitis, HIV, and tetanus (32, 33).
Children, being dependent on their parents, are more vulnerable to TM, which can compromise their health rights and hinder progress toward achieving Millennium Development Goal 4 (MDG4) (34, 35). Providing evidence-based information on parental use of TM in children is crucial. This can inform the development of appropriate control measures to ensure the quality and safety of these practices. As a result, this will help improve child health outcomes and reduce TM-related morbidity and mortality among children (36).
There have been many studies conducted on adult TM use; however, there are limited studies conducted on parental use of TM for children, particularly in Harar City. Therefore, the objective of this study was to determine the prevalence and associated factors of parental traditional medicine use for children in Harar City, Eastern Ethiopia.
Research methods and materials
Study design, area, and period
A cross-sectional study was carried out in the community of Harar City, Harari regional state, in the eastern part of Ethiopia. Harar is the principal city of Harari regional state and is one of the most ancient and historic cities of Ethiopia, located approximately 526 km away from the capital city of Addis Ababa. The Harari region is entirely surrounded by the neighboring Oromia region. According to the 2007 report from the National Central Statistical Agency, Harari region had a total population of 183,415, with 92,316 men and 91,099 women. Regarding health facilities in the region, there are 6 hospitals (3 governmental, 2 private, and 1 non-governmental or fistula center), 8 health centers, 29 private clinics, 26 health posts, and 1 regional laboratory. These facilities are supposed to provide health services to the population in this region. These data were obtained from the Harari Regional Health Bureau. Harar City is divided into 9 woredas and 26 localities (kebeles). The study was conducted between 15 October and 15 November 15 2024.
Source and study population
In this study, the population source include all parents with children who live in Harar City. The study population in this research include all parents with children live in randomly chosen kebeles.
Inclusion and exclusion criteria
All parents with children who have lived for at least 6 months in randomly selected kebeles were included in the study. Parents who were seriously ill while data were being gathered were excluded.
Sample size calculation
The sample size for this study was calculated using Epi info statistical software version 7.2.6.0, based on several assumptions. These included 95% confidence interval (CI), 80% power, and an odds ratio (OR) of 2.49 for a variable significantly associated with the outcome in a previous study. The proportion of the outcome in the unexposed group was assumed to be 32%, with an unexposed-to-exposed ratio of 1:1, as the study used a cross-sectional design. In addition, a 10% non-response rate was factored in, and the resulting was multiplied by a design effect of 2 to account for the sampling procedure. The final calculated sample size for the study was 348 participants.
Sampling techniques/procedure
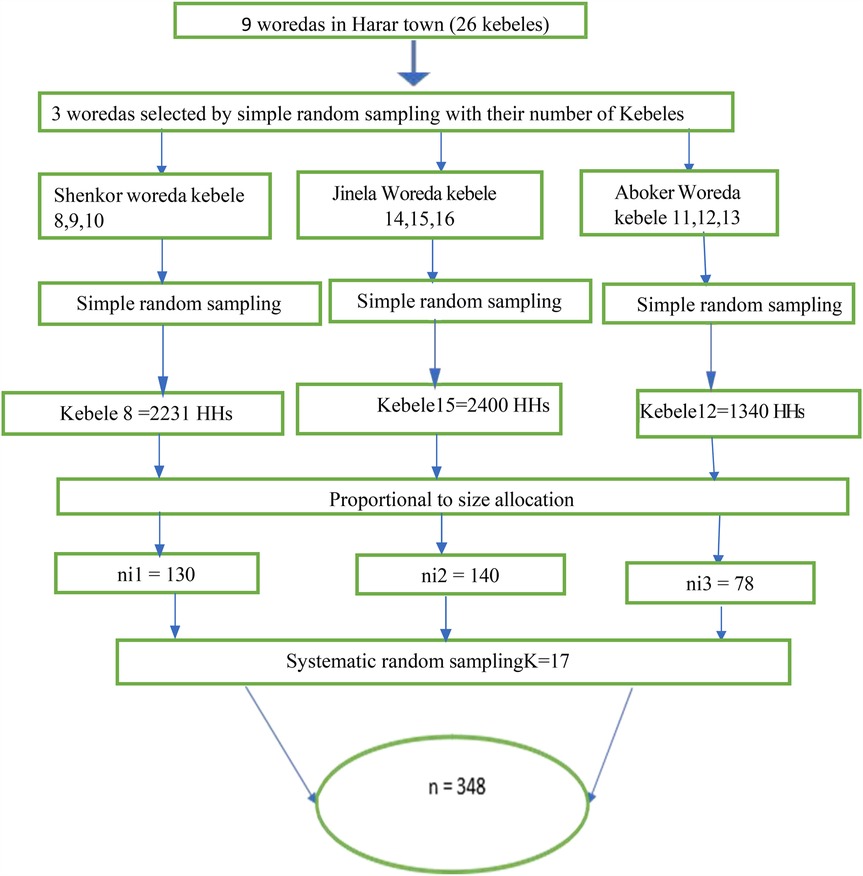
In the present study, a multistage sampling technique was employed to recruit participants. Harar City is composed of 9 woredas and 26 kebeles. Initially, three woredas were selected using the lottery method. From each of the selected woredas, one kebele was randomly chosen, also using the lottery method. The total sample size of 348 participants was then allocated proportionally to the population size of each selected kebele. Thereafter, respondents from each selected kebele were chosen using a systematic random sampling technique. The first respondent was chosen at random, and subsequent participants were selected at regular intervals thereafter (Figure 1).
Data collection method
A structured questionnaire with in-person interviews was used to gather the required data from the study participants. The questionnaire used in this study was modified into our research context from preceding research works that were conducted on similar topics in Ethiopia. The questionnaire consisted of sociodemographic characteristics of the parents, traditional medicine use by parents for children and themselves, the attitude of parents toward TM, factors related to parental healthcare experience, factors that enabled parents to use TM, and need factors. The data collection tool (questionnaire) was primarily prepared in the English language; we then translated it into the local languages of the community (Affan Oromo and Amharic) and back into English by another person who was fluent in both languages to check for consistency and equivalency. Five Bachelor of Science (BSc) nurses were the data collectors and three Master of Science (MSc) graduates were the supervisors in the data collection process.
Data quality control
Before initiating the data collection process, the data collection tool (questionnaire) was pretested in a similar setting outside the study area to ensure the authenticity and quality of the collected data. Based on pretest findings, necessary corrections were made, and the final version of the corrected questionnaire was approved for use. The internal consistency of the tool was checked using reliability analysis, yielding a Cronbach's alpha value of 0.82, which falls within the acceptable range. Both data collectors and supervisors were thoroughly trained on the entire data collection process before commencement. During data collection, trained supervisors closely monitored the process to ensure coherence and completeness. During data management, storage, and analysis, the collected data were extensively checked for completeness and coherence.
Definitions
The term “parent” in our study refers to the mother, father, or legal guardian who cares for the child.
The term “child” refers to individuals aged under 18 years.
Traditional medicine use refers to anything that is not considered a part of contemporary modern medicine (MM) even though it is acknowledged in the community and the community used it for the treatment and prevention of illness as well as to promote health. Traditional medicine is neither ordered by the healthcare provider nor utilized normally as a diet in that specific community.
In this study traditional healers are individuals providing healthcare without being trained in modern medical science.
A bone settler is a traditional practitioner who has no training in modern medical science but provides therapy for bone dislocations or fractures, such as balancing the dislocated bone and helping in the manipulation of joints and muscles.
The term “herbal medicine” refers to culturally acceptable traditional medicines that are prepared from plants to cure illness.
Religious therapy is the treatment and prevention of illness as well as health promotion with the help of the healing presence of God or Allah.
A massage is the relief of pain and tension by placing mild or strong pressure on the joints and muscles of a person and applied by a locally known traditional healer.
Data processing and analysis
After the data collection process was finalized, the data were entered into Epi data statistical software version 4.6 and exported to Stata version 16 statistical software for coding, editing, cleaning, and analyzing.
To describe continuous variables, descriptive statistics such as means and standard deviations (SDs) were used. Categorical variables were described using frequencies and percentages. To identify factors associated with parental TM use, a bi-variable logistic regression analysis was conducted. Initially, bi-variable logistic regression analysis was conducted to screen potential candidate variables. Independent variables with p ≤ 0.25 were then included in the multivariable logistic regression analysis to avoid possible confounding effects.
The association between the independent variables and the outcome variable was assessed using a multivariable logistic regression analysis. The model's goodness of fit was evaluated using the Hosmer and Lemeshow test (p = 0.56). To check for multicollinearity, a variance inflation factor (VIF) analysis was performed, and no evidence of multicollinearity was found. Independent variables with p < 0.05 and adjusted odds ratio (aOR) with 95% confidence intervals were considered statistically significant. The results were presented in the form of text, figures, and tables.
Ethical consideration
Ethical clearance for this study was obtained from the Institutional Health Research Ethics Review Committee of Haramaya University, College of Health and Medical Sciences (reference no. IHRERC/286/2024). A formal letter of cooperation was submitted to the Harari Region Health Bureau. Before data collection, written informed consent was obtained from all participants. Participation was voluntary, and each participant was assured that their responses during the in-person interview would remain strictly confidential.
Results
Sociodemographic characteristics
A total of 348 parents were sampled for the study, with a response rate of 100%. In our study, more than half (n = 217, 62.40%) of the study participants were women. The mean age of the participants was 33 ± 9.4 years. Regarding the religion of the study participants, 172 (49.40%) were followers of the Orthodox religion. The majority of the participants (n = 323, 92.80%) were married. Regarding the educational status of the respondents, 52 (14.90%) participants could not read and write. Of the participants, 125 (35.90%) listed their occupation as housewife. Most of the parents (n = 144, 41.40%) have three to four children (mean 3.15 ± 1.5). In our findings, the majority of the participants (n = 237, 68.10%) had a monthly income of more than 2,000 Ethiopian Birr (ETB) (Table 1).
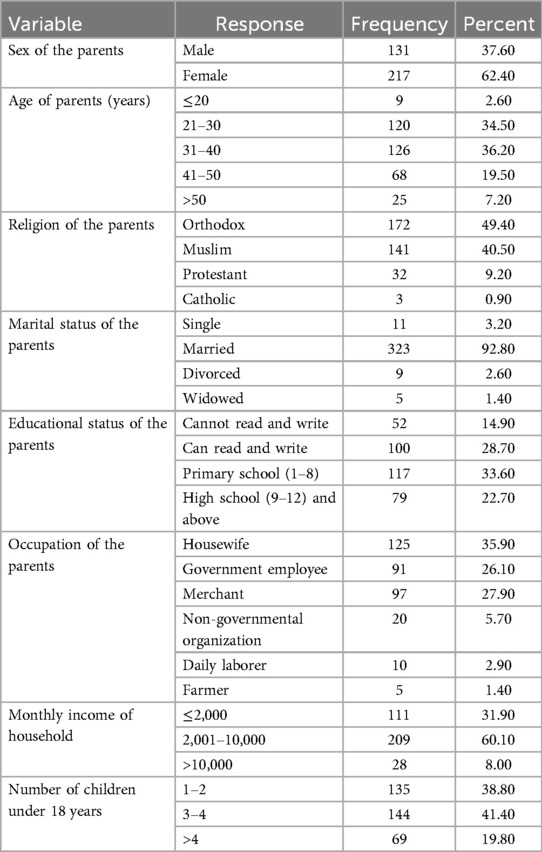
Table 1. Sociodemographic characteristics of parents in Harar City, Eastern Ethiopia, 2024 (n = 348).
Proportion of parental traditional medicine used for children
The proportion of parental TM use for children was 76.15% (95% CI: 71.8–80.5). Regarding the types of TM used by parents for their children, the majority (n = 154, 58.10%) had applied herbal treatments. Regarding the type of TM utilized for children by their parents, most of the parents (n = 168, 63.40%) used a drinkable form of TM (Table 2).
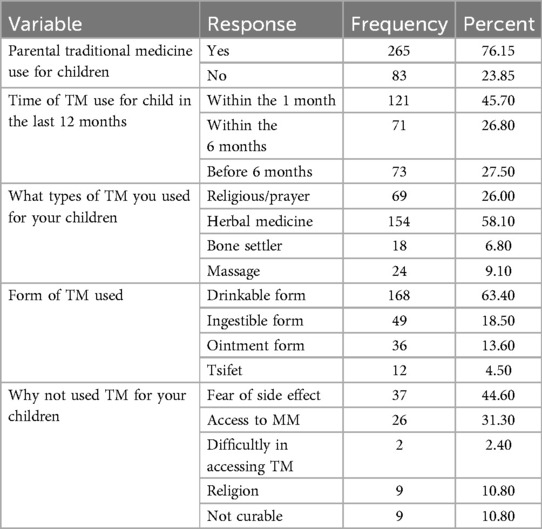
Table 2. Parental use of traditional medicine for children in Harar City, Eastern Ethiopia, 2024 (n = 348).
Parental enabling and need factors to use TM for children
We asked the study participants to tell us the main reasons for using TM for their children. Of them, 108 (40.80%) responded that TM was easily accessible in their environment. Similarly, the participants were asked about the source of information for using TM for their children; of them, 116 (43.80%) replied that a family member was the source of information. Most of the parents (n = 157, 59.20%) used TM for their children as a disease treatment. Of the parents, 64 (24.20%) used TM as a treatment for respiratory disease and 43 (16.20%) used TM to treat gastrointestinal problems (Table 3).
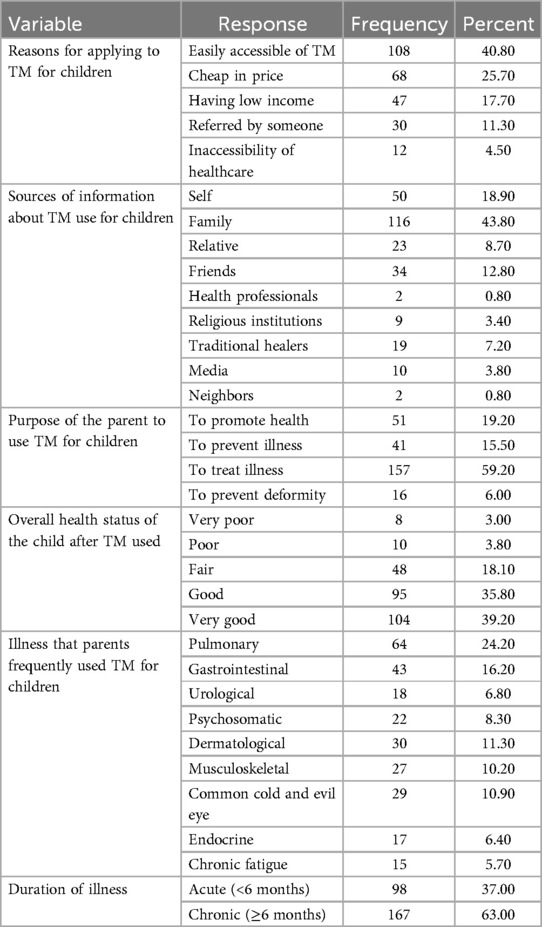
Table 3. Enabling and need factors for parental use of traditional medicine for children in Harar City, Eastern Ethiopia, 2024 (n = 265).
Parental healthcare experience and their attitudes toward TM
We asked the parents whether they used TM for themselves and learned that 165 (47.40%) were self-TM users. Among those users, 111 (67.30%) were women (mothers). The study participants were requested to rate their level of satisfaction with TM, with 36 (21.80%) replying they were satisfied. In total, 158 (45.40%) participants replied that TM has good efficacy. Of the participants, 230 (66.10%) had a good attitude toward TM. More than half of the participants (n = 261, 75.00%) had future plans to use TM. A total of 238 (68.40%) study participants encouraged others to use TM. Approximately 218 (62.60%) participants said that modern medicine cannot cure certain diseases. In our study findings, half of the participants were members of the community-based health insurance (CBHI) plan (Table 4).
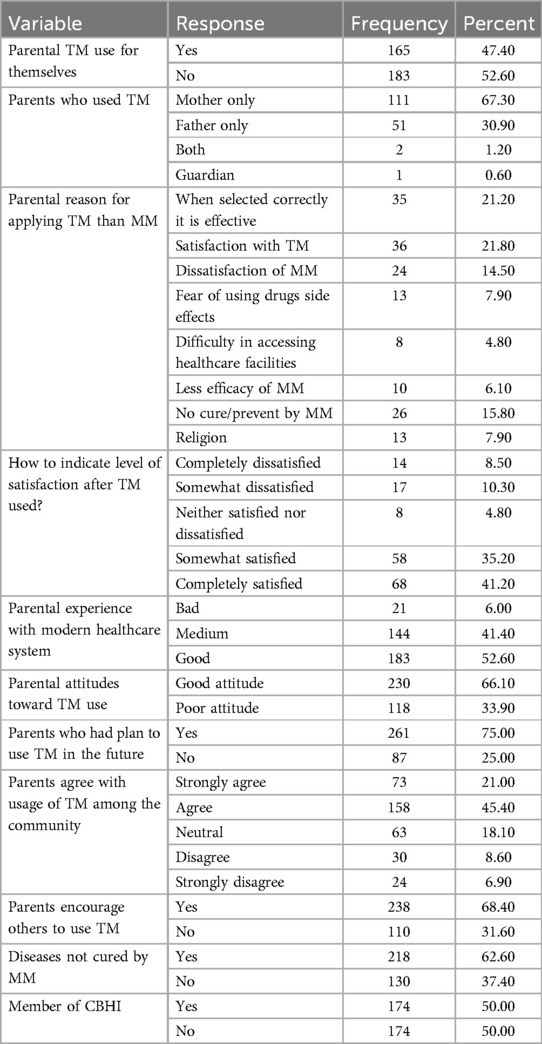
Table 4. Parental healthcare experience and attitudes toward use of traditional medicine for children in Harar City, Eastern Ethiopia, 2024 (n = 348).
Parental use of traditional medicine for children and associated factors
The results of the multivariable logistic regression analysis revealed that the number of children, parental attitudes toward TM, and membership in the community-based health insurance plan were significantly associated with parental use of traditional medicine for children. Parents with more than four children were three times more likely to use TM for their children compared to those with less than four children (aOR = 3.24, 95% CI: 1.13–9.28). Similarly, parents who had a positive attitude toward TM were twice as likely to use it for their children compared to those with a negative attitude (aOR = 1.98, 95% CI: 1.02–3.86). Finally, CBHI was also significantly associated with TM use; parents who were members of CBHI were 66% less likely to use TM for their children compared to non-members (aOR = 0.34, 95% CI: 0.19–0.63) (Table 5).
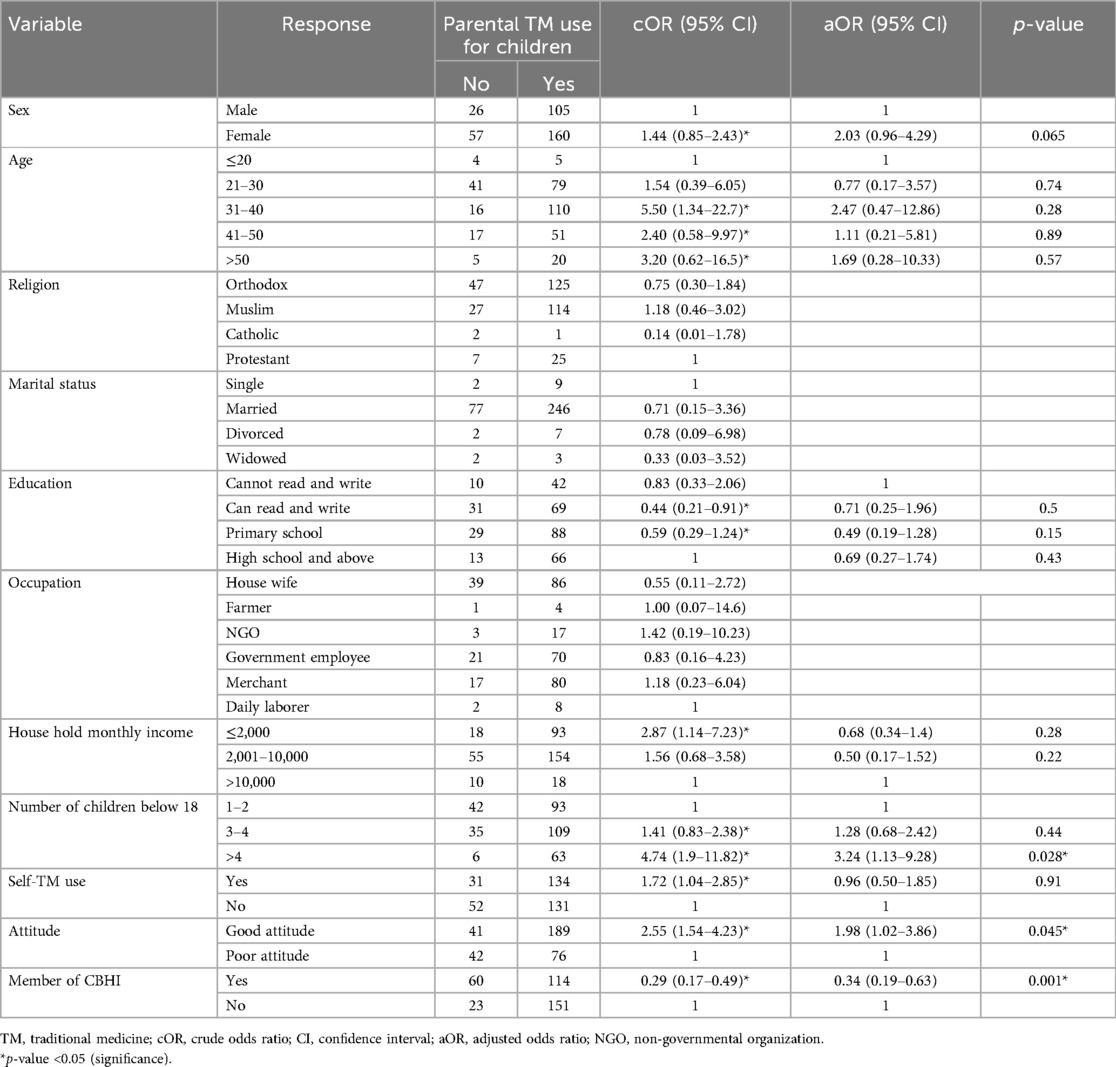
Table 5. Factors associated with parental use of TM for children in Harar City, Eastern Ethiopia, 2024 (n = 348).
Discussion
Traditional medicine practice has its own benefit in solving health-related problems in society; however, there is a problem related to the lack of scientifically proven standards for deciding its appropriate use, including the dose of medicine and route of administration (37). Studies have shown that most patients who used traditional medicine experienced a worsening of their condition and developed new complications (38). Identifying risk factors and implementing safety measures are vital to reducing child morbidity and mortality related to traditional medicine use. The objective of this research was to assess the proportion of parental TM use for their children and its associated factors in Harar City, Eastern Ethiopia.
In our study, the proportion of parental TM use for their children was 76.15% (95% CI: 71.8–80.5). The multivariable analysis identified the number of children parents had, their attitude toward TM, and membership in CBHI as factors associated with parental traditional medicine use for children.
The results of this study were almost consistent with those of previous studies conducted in Fagita Lekoma woreda, Ethiopia (71.0%) (20). Similarly, the findings of this study were almost aligned with the study conducted in the Oromia region of Ethiopia (79.4%) (39).
On the other hand, the results of this study were lower than findings in previous studies conducted in Motta Town, Ethiopia (88.2%) (11), Axum Town (87.8%) (40), North Mecha District (90.3%) (19), and East Wollega (94.2%) (41). This lower prevalence of parental TM use for children in the study area might be due to differences in the availability of modern health facilities or their distance from the villages. In areas where modern healthcare facilities are scarce or located far from the community, the use of TM tends to increase (42). Another possible explanation for this difference may be variations in how much attention is given to child health by health sector stakeholders. This includes differences in public health education, awareness campaigns, and the commitment of community health extension workers to educate communities about the adverse complications of TM use (43). In this regard, since Harai Regional State is the smallest in Ethiopia in terms of both land mass and population, health sector stakeholders may have had a better opportunity to raise awareness about the risks of using unproven traditional medicine. Consequently, TM use may be lower in this area. Lastly, differences in cultural and religious beliefs regarding TM use across regions may also contribute to the variation (44, 45).
In the same fashion, this study's result was lower than findings from studies conducted in Shendi Town, Sudan (92%) (46), Nigeria (84%) (47), and Ghana (86.1%) (12). This discrepancy might be due to cultural, behavioral, health policy, and monitoring differences across countries.
However, the results of the present study were higher than those reported in Korea (65.3%) (48), Australia (68.5%) (49), the UK (38%) (50), and Europe (52%) (51). The higher prevalence of TM use observed in our study may be due to limited access to modern healthcare facilities in the area (52, 53), as well as historical and sociocultural ties to TM (54, 55). Another possible reason could be the lower cost of TM compared to modern treatments, its ease of accessibility in the local environment, and the high price of modern medicines. In addition, differences in health policies and controlling measures surrounding TM use may also be reasons (56–58). Moreover, the high proportion of TM use might be linked to the unavailability of scientifically proven modern treatments for certain conditions, including both non-communicable and communicable diseases (59–61).
Regarding the factors influencing parental use of TM for their children, this study found that several variables played a role. In our findings, there were increased odds of using TM for children among parents who had more than four children compared with those with fewer than four. This finding is supported by a study conducted in Uganda (56). The possible explanation for this association is that parents with larger families may be unable to afford the medical fees associated with modern healthcare services (62). In contrast, TM is often more accessible at lower costs. In addition, traditional healers may accept alternative forms of payment, such as goods, labor, or credit (63). When treating personalistic illnesses, traditional healers often involve the extended kin group, and there may be strong social pressure from family elders to comply with traditional practice, which can include providing financial support (63). On the other hand, in modern health facilities, the medical fees are typically covered by the patient or other relatives (64).
Parental attitude toward traditional medicine use in children plays a key role in determining its utilization. In this study, parents with a positive attitude toward TM were more likely to use it for their children compared to those with a negative attitude. This finding is supported by studies conducted in Plateau State, Nigeria (13), in the University of Karbala, Iraq (65), East Wollega Zone (41), and Mecha District, Ethiopia (19). One possible explanation is that parents who think TM is a preferred form of healthcare are more inclined to use it over modern medicine (15).
Another enabling factor that that affects parental use of traditional medicine in children is membership in CBHI. Participants who were being members of community-based health insurance were less likely to use traditional medicine for their children compared to those who were not members. This finding is consistent with studies conducted in Ethiopia and Tanzania (20, 66). An explanation is that CBHI helps solve financial barriers to accessing modern medical services (67).
Study limitations
In this study, we applied a cross-sectional design, which may not establish a cause-and-effect relationship when assessing factors associated with the outcome variable.
Conclusion
Approximately three-quarters of parents reported using TM for their children. This practice was influenced by modifiable factors. Therefore, stakeholders in the health sector should give specific attention to these influencing factors to address the use of traditional medicine in children more effectively.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Haramaya University, College of Health and Medical Sciences, Institutional Health Research Ethics Review Committee (reference number: IHRERC/286/2024). Written informed consent from the parents/participants OR parents/participants legal guardian/next of kin was obtained to participate in this study.
Author contributions
AA: Conceptualization, Writing – original draft, Formal analysis. FM: Conceptualization, Formal analysis, Writing – original draft. MK: Writing – original draft, Formal analysis, Writing – review & editing. FW: Writing – original draft, Formal analysis, Writing – review & editing. HL: Writing – review & editing, Formal analysis, Writing – original draft. YM: Writing – review & editing, Formal analysis, Writing – original draft. TT: Formal analysis, Writing – original draft, Writing – review & editing. ET: Resources, Writing – original draft, Formal analysis, Writing – review & editing. DT: Writing – original draft, Formal analysis, Writing – review & editing. TA: Writing – review & editing, Formal analysis, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to thank the study supervisors, data collectors, and Harar Town community for their collaboration.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
TM, traditional medicine; MM, modern medicine; aOR, adjusted odds ratio; MDG, Millennium Development Goal; CI, confidence interval; NGO, non-governmental organization; BSc, Bachelor of Science; ETB, Ethiopian Birr; MSc, Master of Science; VIF, variance inflation factor; SD, standard deviation; IHRERC, Institutional Health Research Ethics Review Committee; CBHI, community-based health insurance.
References
1. Cohen MH, Kemper KJ. Complementary therapies in pediatrics: a legal perspective. Pediatrics. (2005) 115(3):774–80. doi: 10.1542/peds.2004-1093
2. Kassaye KD, Amberbir A, Getachew B, Mussema Y. A historical overview of traditional medicine practices and policy in Ethiopia. Ethiop J Health Dev. (2006) 20(2):127–34. doi: 10.4314/ejhd.v20i2.10023
3. Oyebode O, Kandala NB, Chilton PJ, Lilford RJ. Use of traditional medicine in middle-income countries: a WHO-SAGE study. Health Policy Plan. (2016) 31(8):984–91. doi: 10.1093/heapol/czw022
4. Pan S-Y, Litscher G, Gao S-H, Zhou S-F, Yu Z-L, Chen H-Q, et al. Historical perspective of traditional indigenous medical practices: the current renaissance and conservation of herbal resources. Evid Based Complement Alternat Med. (2014) 2014(1):525340. doi: 10.1155/2014/525340
5. Birhan W, Giday M, Teklehaymanot T. The contribution of traditional healers’ clinics to public health care system in Addis Ababa, Ethiopia: a cross-sectional study. J Ethnobiol Ethnomed. (2011) 7:1–7. doi: 10.1186/1746-4269-7-39
6. Franco de Sá R, Nogueira J, De Almeida Guerra V. Traditional and complementary medicine as health promotion technology in Brazil. Health Promot Int. (2019) 34(Supplement_1):i74–81. doi: 10.1093/heapro/day087
7. Okaiyeto K, Oguntibeju OO. African herbal medicines: adverse effects and cytotoxic potentials with different therapeutic applications. Int J Environ Res Public Health. (2021) 18(11):5988. doi: 10.3390/ijerph18115988
8. Bopape M, Mothiba T, Malema R. Indigenous practices of traditional health practitioners (THPs) methods by mothers of children admitted to the Polokwane/Mankweng hospital complex, Limpopo province, South Africa. Afr J Phys Health Educ Recreat Dance. (2013) 19(sup-1):147–58.
9. Sadik EA, Gobena T, Mengistu B. Community medicine & health education. Medicine (Baltimore). (2013) 5:6.
10. Okoronkwo I, Onyia-Pat J-L, Okpala P, Agbo M-A, Ndu A. Patterns of complementary and alternative medicine use, perceived benefits, and adverse effects among adult users in Enugu urban, southeast Nigeria. Evid Based Complement Alternat Med. (2014) 2014(1):239372. doi: 10.1155/2014/239372
11. Melesse TG, Ayalew Y, Getie GA, Mitiku HZ, Tsegaye G. Prevalence and factors associated with parental traditional medicine use for children in Motta town, Amhara regional state, Ethiopia, 2014. Altern Integr Med. (2015) 4(179):2. doi: 10.4172/2327-5162.1000179
12. Gyasi RM, Siaw LP, Mensah CM. Prevalence and pattern of traditional medical therapy utilisation in Kumasi metropolis and Sekyere south district, Ghana. J Ethnopharmacol. (2015) 161:138–46. doi: 10.1016/j.jep.2014.12.004
13. Ohemu TL, Shalkur D, Ohemu BO, Daniel P. Knowledge, attitude and practice of traditional medicine among people of Jos south local government area of Plateau state, Nigeria. J Pharm Bioresour. (2021) 18(2):147–54. doi: 10.4314/jpb.v18i2.7
14. Tuasha N, Fekadu S, Deyno S. Prevalence of herbal and traditional medicine in Ethiopia: a systematic review and meta-analysis of 20-year studies. Syst Rev. (2023) 12(1):232. doi: 10.1186/s13643-023-02398-9
15. Chali BU, Hasho A, Koricha NB. Preference and practice of traditional medicine and associated factors in Jimma town, southwest Ethiopia. Evid Based Complement Alternat Med. (2021) 2021(1):9962892. doi: 10.1155/2021/9962892
16. Mahomoodally MF. Traditional medicines in Africa: an appraisal of ten potent African medicinal plants. Evid Based Complement Alternat Med. (2013) 2013:617459. doi: 10.1155/2013/617459
17. Gruca M, van Andel TR, Balslev H. Ritual uses of palms in traditional medicine in Sub-Saharan Africa: a review. J Ethnobiol Ethnomed. (2014) 10:60. doi: 10.1186/1746-4269-10-60
18. Che CT, Zhang H. Plant natural products for human health. Int J Mol Sci. (2019) 20(4):830. doi: 10.3390/ijms20040830
19. Tizazu D, Workineh Y, Ayalew Y. Parental traditional medicine use for children and associated factors in north Mecha district, north west Ethiopia. Pediatric Health Med Ther. (2020) 11:505–12. doi: 10.2147/PHMT.S275249
20. Asrat D, Alle A, Kebede B, Dessie B. Factors associated with parental traditional medicine use for children in Fagita Lekoma Woreda northwest Ethiopia: a cross-sectional study. SAGE Open Med. (2020) 8:2050312120978008. doi: 10.1177/2050312120978008
21. Mudonhi N, Nunu WN. Traditional medicine utilisation and maternal complications during antenatal care among women in Bulilima, Plumtree, Zimbabwe. Matern Health Neonatol Perinatol. (2021) 7:1–9. doi: 10.1186/s40748-021-00130-w
22. Adeleye OA, Femi-Oyewo MN, Bamiro OA, Bakre LG, Alabi A, Ashidi JS, et al. Ethnomedicinal herbs in African traditional medicine with potential activity for the prevention, treatment, and management of coronavirus disease 2019. Futur J Pharm Sci. (2021) 7(1):72. doi: 10.1186/s43094-021-00223-5
23. Kidane B, van Andel T, van der Maesen LJ, Asfaw Z. Use and management of traditional medicinal plants by Maale and Ari ethnic communities in southern Ethiopia. J Ethnobiol Ethnomed. (2014) 10:46. doi: 10.1186/1746-4269-10-46
24. Dessie AM, Anley DT, Zemene MA, Gebeyehu NA, Adella GA, Kassie GA, et al. Trend, determinants, and future prospect of child marriage in the Amhara region, Ethiopia: a multivariate decomposition analysis. Front Public Health. (2023) 11:1132148. doi: 10.3389/fpubh.2023.1132148
25. Esan DT, Muhammad F, Ogunkorode A, Obialor B, Ramos C. Traditional beliefs in the management and prevention of neonatal jaundice in Ado-Ekiti, Nigeria. Enferm Clin (Engl Ed). (2022) 32(Suppl 1):S73–6. doi: 10.1016/j.enfcli.2021.09.014
26. Adjei B. Utilization of traditional herbal medicine and its role in health care delivery in Ghana: the case of Wassa Amenfi West District. (2013).
27. Tesfai B, Debesai A, Mekonnen S, Girmay F, Kibreab F, Hussien L, et al. Knowledge, attitude, practice and prevalence of traditional cauterization among patients in Massawa hospital, Eritrea: a cross-sectional study. Pan Afr Med J. (2020) 36(1):36–230. doi: 10.11604/pamj.2020.36.230.21349
28. Teshager NW, Amare AT, Tamirat KS, Zeleke ME, Taddese AA. Traditional herbal medicine use doubled the risk of multi-organ dysfunction syndrome in children: a prospective cohort study. PLoS One. (2024) 19(2):e0286233. doi: 10.1371/journal.pone.0286233
29. Usure RE, Kebebe D, Mekasha YT, Hasen G, Chura Waritu N, Dubale S, et al. Traditional herbal medicine regulatory implementation in Ethiopia: a qualitative study. Front Pharmacol. (2024) 15:1392330. doi: 10.3389/fphar.2024.1392330
30. Sarmiento I, Zuluaga G, Andersson N. Traditional medicine used in childbirth and for childhood diarrhoea in Nigeria’s cross river state: interviews with traditional practitioners and a statewide cross-sectional study. BMJ open. (2016) 6(4):e010417. doi: 10.1136/bmjopen-2015-010417
31. Kumar S, Mittal A, Babu D, Mittal A. Herbal medicines for diabetes management and its secondary complications. Curr Diabetes Rev. (2021) 17(4):437–56. doi: 10.2174/18756417MTExfMTQ1z
32. Tuncer AA, Erten EEA. Examination of short and long term complications of thermocautery, plastic clamping, and surgical circumcision techniques. Pak J Med Sci. (2017) 33(6):1418–23. doi: 10.12669/pjms.336.13640
33. Farid MK, El-Mansoury A. Kaiy (traditional cautery) in Benghazi, Libya: complications versus effectiveness. Pan Afr Med J. (2015) 22(1):22–98. doi: 10.11604/pamj.2015.22.98.6399
34. Díaz-Martínez E, Gibbons ED. The questionable power of the Millennium Development Goal to reduce child mortality. J Hum Dev Capabil. (2014) 15(2-3):203–17. doi: 10.1080/19452829.2013.864621
35. Ruducha J, Mann C, Singh NS, Gemebo TD, Tessema NS, Baschieri A, et al. How Ethiopia achieved Millennium Development Goal 4 through multisectoral interventions: a countdown to 2015 case study. Lancet Glob Health. (2017) 5(11):e1142–51. doi: 10.1016/S2214-109X(17)30331-5
36. Timmermans K. Intellectual property rights and traditional medicine: policy dilemmas at the interface. Soc Sci Med. (2003) 57(4):745–56. doi: 10.1016/S0277-9536(02)00425-2
37. Waldram JB. The efficacy of traditional medicine: current theoretical and methodological issues. Med Anthropol Q. (2000) 14(4):603–25. doi: 10.1525/maq.2000.14.4.603
38. Niggemann B, Grüber C. Side-effects of complementary and alternative medicine. Allergy. (2003) 58(8):707–16. doi: 10.1034/j.1398-9995.2003.00219.x
39. Hailu F, Cherie A, Gebreyohannis T, Hailu R. Determinants of traditional medicine utilization for children: a parental level study in Tole district, Oromia, Ethiopia. BMC Complement Med Ther. (2020) 20:1–11. doi: 10.1186/s12906-020-02928-1
40. Gebrekirstos K, Abebe M, Fantahun A. A cross sectional study on factors associated with harmful traditional practices among children less than 5 years in Axum town, north Ethiopia, 2013. Reprod Health. (2014) 11:1–7. doi: 10.1186/1742-4755-11-46
41. Gari A, Yarlagadda R, Wolde-Mariam M. Knowledge, attitude, practice, and management of traditional medicine among people of Burka Jato Kebele, west Ethiopia. J Pharm Bioallied Sci. (2015) 7(2):136–44. doi: 10.4103/0975-7406.148782
42. Samuel O. Under Utilization of Modern Health Facilities and the Practice of Alternative Medicine in Rural Areas of Rivers State. Available at SSRN 2187770. (2012).
43. Desta SH, Basha SY. The role of health extension workers in primary health care in AsgedeTsi'mbla district: a case of Lim'at T'abya health post. Int J Soc Sci Manag. (2017) 4(4):248–66. doi: 10.3126/ijssm.v4i4.18504
44. Espinoza Giacinto R, Castañeda SF, Perez RL, Nodora JN, Gonzalez P, Lopez EJ, et al. Diabetes cultural beliefs and traditional medicine use among health center patients in Oaxaca, Mexico. J Immigr Minor Health. (2016) 18:1413–22. doi: 10.1007/s10903-015-0323-9
45. Unge C, Ragnarsson A, Ekström AM, Indalo D, Belita A, Carter J, et al. The influence of traditional medicine and religion on discontinuation of ART in an urban informal settlement in Nairobi, Kenya. AIDS care. (2011) 23(7):851–8. doi: 10.1080/09540121.2010.534432
46. Elnageeb MM, Mohmmed SA, Alhadi LE, Mohammed AS. Awareness and attitude of mothers about herbal medicine used to treat children aged under 5 years in Shendi City, Sudan. (2019).
47. Oshikoya KA, Senbanjo IO, Njokanma OF, Soipe A. Use of complementary and alternative medicines for children with chronic health conditions in Lagos, Nigeria. BMC Complement Altern Med. (2008) 8:1–8. doi: 10.1186/1472-6882-8-66
48. Kim J-H, Nam C-M, Kim M-Y, Lee D-C. The use of complementary and alternative medicine (CAM) in children: a telephone-based survey in Korea. BMC Complement Altern Med. (2012) 12:1–9. doi: 10.1186/1472-6882-12-46
49. Frawley JE, Anheyer D, Davidson S, Jackson D. Prevalence and characteristics of complementary and alternative medicine use by Australian children. J Paediatr Child Health. (2017) 53(8):782–7. doi: 10.1111/jpc.13555
50. Crawford NW, Cincotta DR, Lim A, Powell CV. A cross-sectional survey of complementary and alternative medicine use by children and adolescents attending the university hospital of Wales. BMC Complement Altern Med. (2006) 6:1–10. doi: 10.1186/1472-6882-6-16
51. Zuzak TJ, Boňková J, Careddu D, Garami M, Hadjipanayis A, Jazbec J, et al. Use of complementary and alternative medicine by children in Europe: published data and expert perspectives. Complement Ther Med. (2013) 21:S34–47. doi: 10.1016/j.ctim.2012.01.001
52. Bazie GW, Adimassie MT. Modern health services utilization and associated factors in north east Ethiopia. PLoS One. (2017) 12(9):e0185381. doi: 10.1371/journal.pone.0185381
53. Bitew Workie S, Mekonen N, Michael MW, Molla G, Abrha S, Zema Z, et al. Modern health service utilization and associated factors among adults in southern Ethiopia. J Environ Public Health. (2021) 2021(1):8835780. doi: 10.1155/2021/8835780
54. Abel AO, Imarenezor EPK, Alloysius OC, Ahamefula AA. Socioeconomic and cultural factors influencing traditional medicine (tm) use in Nigeria: a systematic mixed method review. Eur J Integr Med. (2025) 74:102436. doi: 10.1016/j.eujim.2025.102436
55. Stanifer JW, Patel UD, Karia F, Thielman N, Maro V, Shimbi D, et al. The determinants of traditional medicine use in northern Tanzania: a mixed-methods study. PLoS One. (2015) 10(4):e0122638. doi: 10.1371/journal.pone.0122638
56. Logiel A, Jørs E, Akugizibwe P, Ahnfeldt-Mollerup P. Prevalence and socio-economic factors affecting the use of traditional medicine among adults of Katikekile Subcounty, Moroto district, Uganda. Afr Health Sci. (2021) 21(3):1410–7. doi: 10.4314/ahs.v21i3.52
57. Kim JK, Kim KH, Shin YC, Jang B-H, Ko S-G. Utilization of traditional medicine in primary health care in low-and middle-income countries: a systematic review. Health Policy Plan. (2020) 35(8):1070–83. doi: 10.1093/heapol/czaa022
58. Fitriah R, Hidayati R, Muthia RH. Comparison of public’s interest in selecting traditional and modern medicine therapy. Int J Appl Pharm. (2022) 14(2):17–21. doi: 10.22159/ijap.2022.v14s2.44744
59. Levene D, Phillips DI, Alemu S. Medical traditions and chronic disease in Ethiopia: a story of wax and gold? Trop Dr. (2016) 46(3):122–5. doi: 10.1177/0049475516655060
60. Beykaso G, Teklehaymanot T, Mulu A, Berhe N, Alemayehu DH, Giday M. Medicinal plants in treating hepatitis B among communities of central region of Ethiopia. Hepat Med. (2023) 15:265–77. doi: 10.2147/HMER.S440351
61. Yenet A, Nibret G, Tegegne BA. Challenges to the availability and affordability of essential medicines in African countries: a scoping review. Clinicoecon Outcomes Res. (2023) 15:443–58. doi: 10.2147/CEOR.S413546
62. Heck KE, Parker JD. Family structure, socioeconomic status, and access to health care for children. Health Serv Res. (2002) 37(1):171. doi: 10.1111/1475-6773.99190
63. Eshete MA, Molla EL. Cultural significance of medicinal plants in healing human ailments among Guji semi-pastoralist people, Suro Barguda district, Ethiopia. J Ethnobiol Ethnomed. (2021) 17:1–18. doi: 10.1186/s13002-021-00487-4
64. Muela SH, Mushi AK, Ribera JM. The paradox of the cost and affordability of traditional and government health services in Tanzania. Health Policy Plan. (2000) 15(3):296–302. doi: 10.1093/heapol/15.3.296
65. Chyad Abdulzahra N. Attitude of mothers toward herbal treatment of their children. Kerbala J Med. (2012) 5(11):1384–9.
66. Chomi EN, Mujinja PG, Enemark U, Hansen K, Kiwara AD. Health care seeking behaviour and utilisation in a multiple health insurance system: does insurance affiliation matter? Int J Equity Health. (2014) 13:1–11. doi: 10.1186/1475-9276-13-25
Keywords: parental, traditional medicine, children, Harar, Ethiopia
Citation: Alemu A, Meseret F, Keneni M, Wondimneh F, Legesse H, Mossie Y, Teshager T, Tamiru E, Tizau D and Asfaw T (2025) Parental traditional medicine use for children and associated factors in Harar City, Harari Regional State, Eastern Ethiopia: a community-based cross-sectional study. Front. Pediatr. 13:1546455. doi: 10.3389/fped.2025.1546455
Received: 16 December 2024; Accepted: 16 May 2025;
Published: 9 June 2025.
Edited by:
Maxine Deborah Gossell-Williams, University of the West Indies, JamaicaCopyright: © 2025 Alemu, Meseret, Keneni, Wondimneh, Legesse, Mossie, Teshager, Tamiru, Tizau and Asfaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ayichew Alemu, YXlpY2hld2FsZW11NzQxQGdtYWlsLmNvbQ==
 Ayichew Alemu
Ayichew Alemu Fentahun Meseret
Fentahun Meseret Mulualem Keneni
Mulualem Keneni Fenta Wondimneh
Fenta Wondimneh Henok Legesse
Henok Legesse Yalew Mossie
Yalew Mossie Tilahun Teshager2
Tilahun Teshager2 Diribsa Tizau
Diribsa Tizau