- Department of Breast and Thyroid Surgery, Lingnan Hospital, The Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, China
Background: Endoscopic thyroidectomy (ET) has become increasingly popular globally, but its application in young children remains largely unexplored. This study reports a 6-year-old girl with a neck mass who underwent ET via total areola approach.
Methods: After ultrasonographic (ACR TI-RADS 4) and cytological (TBSRTC 4) confirmation, the patient underwent endoscopic right and isthmic thyroidectomy with inferior parathyroid auto-transplantation under general anesthesia. The procedure utilized 3 mm pediatric instruments, intraoperative neuromonitoring and near-infrared auto fluorescent parathyroid monitoring.
Results: The procedure achieved complete resection with 215 min operative time and minimal blood loss. The pathological diagnosis was thyroid follicular adenoma. At 3-month follow-up, no complications and excellent cosmetic outcomes were observed.
Conclusion: ET via total areola approach proves highly suitable for young children because of its safety and cosmetic advantages. Experienced surgeons, small-size special surgical instruments and auxiliary monitoring techniques are helpful to improve the safety of pediatric ET.
1 Introduction
Thyroidectomy is one of the main treatments for thyroid diseases in children. In recent years, the number of pediatric patients requiring thyroidectomy has been increasing. Currently, the indications, techniques and complications of thyroidectomy in pediatric patients are similar to those in adults (1).
Thyroidectomy includes open thyroidectomy (OT), which is performed through a neck incision, and endoscopic thyroidectomy (ET), which is performed through concealed incisions in the areola, axilla, mouth floor, and post aurem. Compared to ET, the main disadvantage of OT is visible neck scarring. For pediatric patients, especially female, these scars are more likely to impair their mental health and quality of life. Besides, ET possesses other advantages such as high-definition visual field and less hemorrhage during operation.
At present, the safety and efficacy of thyroidectomy in pediatric patients is acceptable, but the operation volume is far less than that in adults. Therefore, we need more cases for clinical reference. This paper describes a 6-year-old girl with thyroid follicular adenoma who underwent ET via the total areola approach. According to our search, she is the youngest patient to have undergone this approach to date.
2 Case description
2.1 Patient
On July 30, 2024, a 6-year-old girl was hospitalized in the Department of Thyroid and Breast Surgery in our center for a neck mass found more than 2 years ago without any symptoms such as pain and fever. She had a palpable, oval, soft-textured, well-defined, non-tender mass measuring approximately 2*1.5 cm in diameter in the right anterior cervical triangle. No treatment had been conducted prior to this operation. Results of preoperative examinations such as thyroid function, parathyroid function, electrocardiogram, and fiberoptic laryngoscopy were normal. Ultrasonography revealed a thyroid nodule in the right lobe, classified as ACRTI-RADS Grade 4. Fine-needle aspiration biopsy suggested that it might be a follicular tumor with TBSRTC Grade 4. There is no family history of genetic diseases or mental disorders.
2.2 Surgical techniques
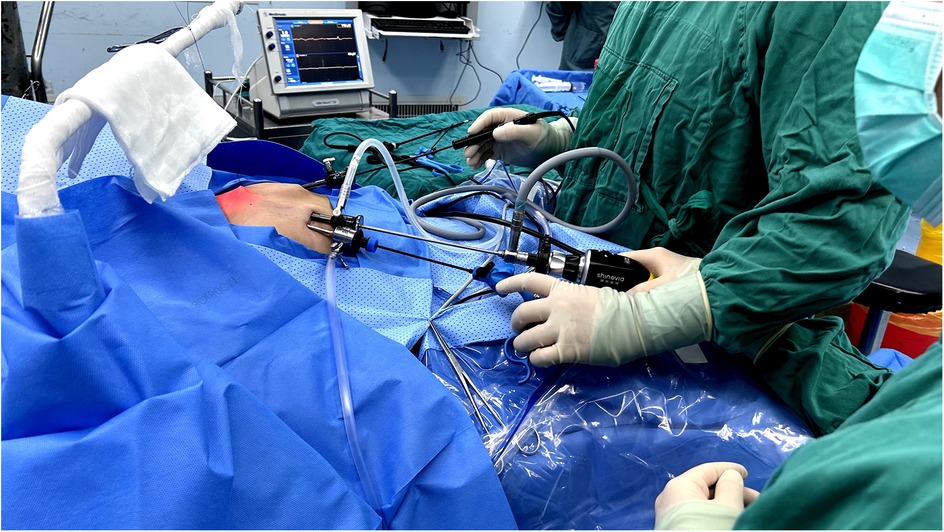
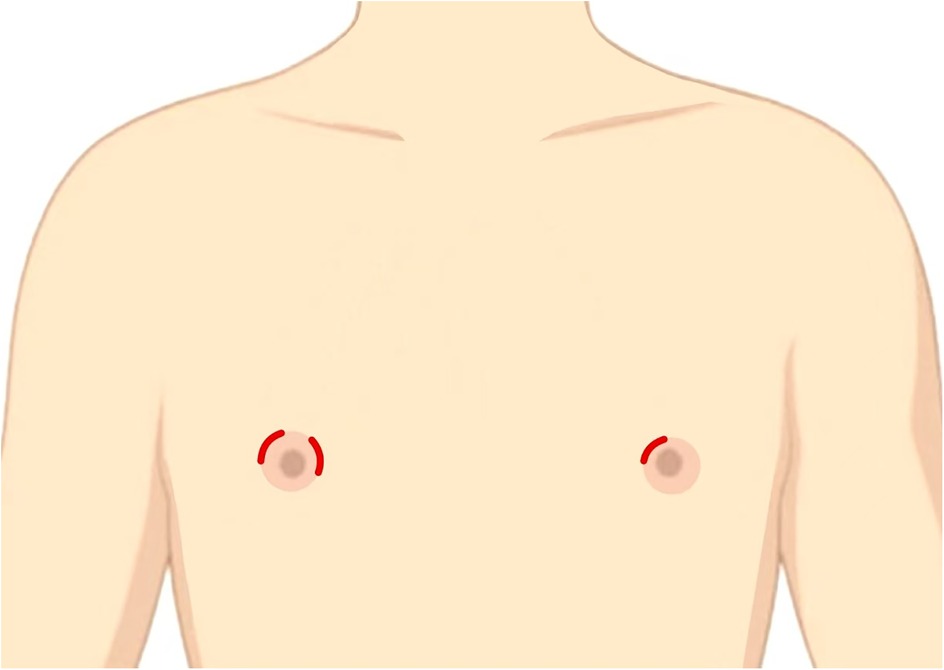
The patient underwent endoscopic right and isthmic thyroidectomy with inferior parathyroid auto-transplantation under general anesthesia on August 1, 2024. The patient was placed in the supine split-leg position, and the laparoscopic system, the ultrasonic scalpel, the suction pump, and intraoperative neuromonitoring (IONM) device was connected. The surgeons made curved incisions with a length of 5–8 mm respectively in the 11 o'clock direction of the bilateral areola and in the 3 o'clock direction of the right areola (Figures 1, 2). Then they chose the 3 mm and 5 mm diameter trocars, which were more suitable for pediatric patients. The subcutaneous tissue was separated up to the anterior neck region with a 3 mm grasping forceps and the ultrasonic scalpel, and the linea alba was cut layer by layer to expose the right lobe and the lesion. The thyroid capsule was carefully dissected to identify recurrent laryngeal nerve (RLN) and parathyroids. Two parathyroids were located and confirmed by a near-infrared auto fluorescent (NIRAF) detector. The superior parathyroid was preserved, while the inferior parathyroid with insufficient blood supply was transplanted into the right sternocleidomastoid muscle. The RLN and vagus nerve were detected by the IONM, which determines the location and conduction of nerves by stimulating and receiving the electrical signals. Eventually, the right thyroid lobe, isthmus, and lesion was completely resected and pulled out with a specimen bag. The surgical field was thoroughly stanched and irrigated, and a drainage tube was placed.
2.3 Results
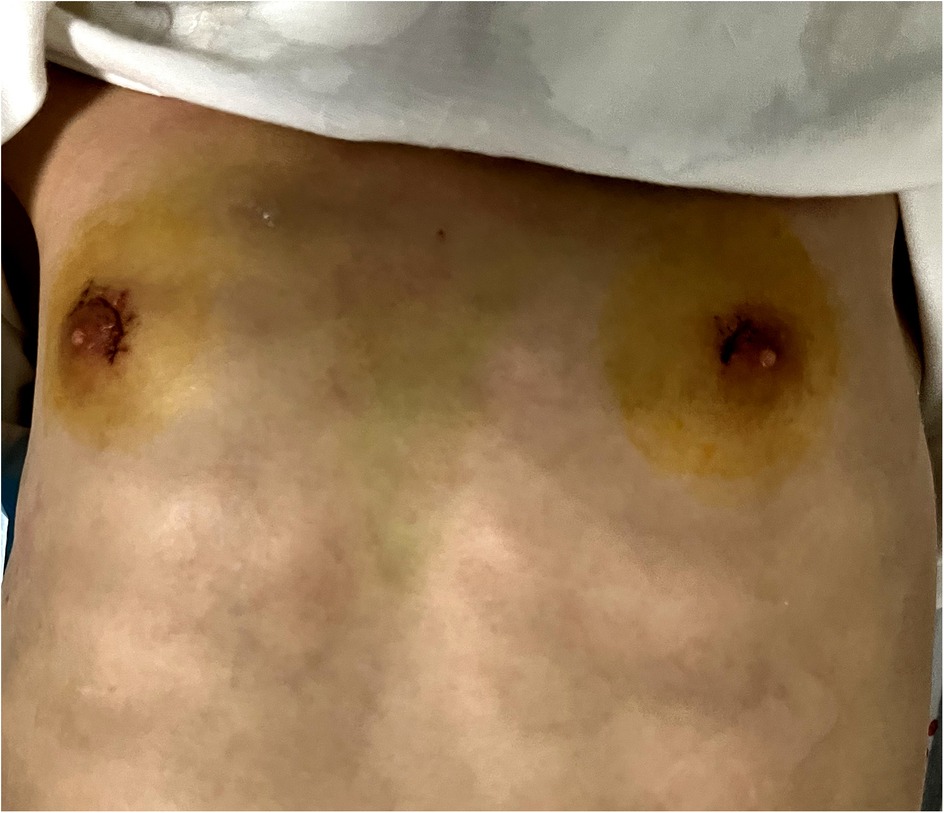
The operation was successfully finished without conversion to OT and the blood loss was about 20 ml. The operative time was 215 min. After the operation, the patient reported mild pain in the neck and fully cooperated with the postoperative treatments which included electrocardiographic monitoring, low-flow oxygen therapy, analgesia, nebulization, intravenous fluids and calcium supplementation. On the 2nd postoperative day, the patient was able to ambulate and received a liquid diet and oral levothyroxine sodium. Within 3 days after surgery, the drainage tube discharged 35 ml, 10 ml, and 8 ml of light red fluid, respectively. On the 3rd postoperative day, the drainage tube was removed and the patient was discharged without any complication. The surgical incisions healed well without local infection or dehiscence (Figure 3). And the diagnosis of thyroid follicular adenoma was confirmed by the pathological result. The patient was followed up for 3 months after discharge, without any surgical complications occurred. Re-examination of neck ultrasonography and thyroid function showed no abnormality. The patient and her family members expressed their contentment with both the surgical efficacy and the post-operative cosmetic outcome.
3 Discussion
During the operation, we found that the parathyroids were more difficult to recognize in children. And the cervical region VI was covered by the larger thymus. Besides, the volume of thyroid is age dependent, the average volume of 7-year-old children is less than 4 cm3 (2), which is much smaller than that of adults, and the same is true for the vessels and parathyroid. As a result, the risk of complications for thyroidectomy is higher in children. Existing studies have shown that the incidence of postoperative permanent hypocalcemia in adults and pediatric patients is 0.87% (3) and 1.16% (1), respectively. In addition, the RLN palsy, wound infection, keloid formation, hemorrhage, and chylous leakage are also complications of thyroidectomy in children. Therefore, it is necessary for surgeons to pay more attention to the protection of parathyroid glands, nerves and blood vessels, especially for children aged 0–6 years.
The application of ET provides a good solution to this issue. The endoscope has a high-definition field of view and the ability to zoom, which allows close-up presentation of important anatomical structures within the surgical field. During the ET in pediatric patients, surgeons can distinguish the small-size parathyroids and blood vessels and even the smaller structures which were difficult to achieve with naked eye. In addition, endoscopic modified instruments, such as 3 mm grasping forceps, improve the delicacy of the surgeon's manipulation, making ET in children safer and more efficient. Due to the unique anatomical and physiological features, thyroidectomy in pediatric patients requires more expertise and experience than in adults. A study revealed that children treated by higher-volume surgeons (more than 30 cases per year) tend to have fewer complications following thyroidectomy (4). As the thyroid gland is highly vascularized, meticulous hemostasis is essential to ensure surgical safety. As demonstrated by Sengul et al. (5) and Aydin et al. (6), the combined use of energy-based devices and IONM in thyroidectomy significantly facilitates surgical procedures, reduces blood loss, and enhances recurrent RLN preservation. This technical combination proves particularly advantageous for pediatric cases, as exemplified by our 6-year-old patient. Furthermore, Benmiloud et al. (7) established that near-infrared autofluorescence (NIRAF) detection improves parathyroid identification accuracy and reduces postoperative transient hypocalcemia rates from 21.7% to 9.1%. In the present case, we achieved optimal outcomes through conducting hemostasis and dissection with ultrasonic scalpel complemented by IONM and NIRAF, resulting in minimal blood loss (10 ml) and no incidence of RLN injury or hypocalcemia during the 3-month follow-up period. In summary, we recommend that high-volume surgeons perform pediatric ET with the assistance of small-sized modified instruments, IONM, and NIRAF detectors to further reduce the incidence of surgical complications.
At present, there are far fewer reports of ET in pediatric patients than in adults. A retrospective clinical study evaluated 31 children who underwent the trans-axillary endoscopic head and neck endocrine surgery, but 8 of them suffered transient minor complications (2). The other 2 case reports described pediatric patients who underwent trans-oral ET (8, 9). However, these papers did not emphasize differences between pediatric and adult ET and offer insights on how to further reduce the incidence of surgical complications.
Another advantage of ET is the cosmetic effect of a scarless neck. Children with head or neck scars are at increased risk of depression and the scars may adversely affect childhood psychosocial functioning (10). Scars resulting from OT can be noticeable and have a significant impact on one's day-to-day routines and emotion (11). The neck scar following OT was found to be associated with a lower quality of life in the pediatric patients (12). A questionnaire survey revealed that psychological distress immediately after operation and during surveillance period was higher in OT than in bilateral axillo-breast approach robotic thyroidectomy (13). In our case, the patient demonstrated high satisfaction with the scarless outcome during the 3-month follow-up. This further supports the cosmetic value of ET in pediatric populations with increasing thyroid diseases.
Among all ET approaches, the total areola approach has several advantages as follows. Firstly, the natural pigmentation of the areola helps to conceal the incisions, resulting in better cosmetic results. Second, compared to the trans-oral approach, the total areola approach takes a lower risk of infection due to its class I incision and provides a more intuitive and classic surgical perspective. Third, compared to the trans-axillary approach and the post-aurem approach, the total areola approach takes a lower risk of serious complications such as neurovascular injury. In addition, compared to robotic thyroidectomy, ET has a shorter learning curve, lower cost, and shorter operation time (14). To sum up, our experience suggests that ET via total areola approach may be a highly suitable option for pediatric patients with thyroid diseases. This paper is a useful reference for selecting surgical approaches for pediatric thyroidectomy.
This case provides evidence supporting the safety and feasibility of endoscopic resection for benign thyroid tumors. However, the applicability of ET in pediatric malignant thyroid disease warrants cautious consideration. Recent data indicate that the malignancy rate of thyroid nodules in children is higher than 60% (15), necessitating rigorous evaluation of ET's role in malignant cases. For patients with malignancy confined to the thyroid without radiologically evident lymph node metastasis, total thyroidectomy with central lymph node dissection (CND) remains standard. The study by Jiang et al. demonstrated that the tumor recurrence rates and the level of surgical completeness in ET are comparable to those in OT (16). However, pediatric-specific long-term follow-up data on recurrence and survival rates are still lacking. Notably, the areolar approach provides adequate exposure for CND in our experience, as the endoscopic magnification facilitates meticulous dissection of central compartment structures. For patients requiring lateral neck dissection due to radiologically confirmed lymph node metastasis, ET's limitations become apparent. The restricted operative field and technical challenges in accessing lateral nodal stations may compromise oncologic completeness. This highlights the need for individualized surgical planning and multidisciplinary evaluation when malignancy is suspected.
While ET offers numerous advantages, this approach is not without significant limitations and shortcomings. Initially, the prolonged operative time must be acknowledged. As evidenced by Cao et al. in their comparative study of benign thyroid tumors, ET required substantially longer operative durations for both unilateral lobectomy (79.9 ± 20.10 vs. 45.4 ± 11.90 min, P < 0.001) and bilateral total thyroidectomy (89.9 ± 14.60 vs. 60.0 ± 8.44 min, P < 0.001) (17). This temporal disparity primarily stems from additional subcutaneous tunnel creation time and the technical constraints of operating within a restricted visual field. Importantly, these temporal demands may be further exacerbated in pediatric populations due to their characteristically reduced anatomical working space. Moreover, ET demands greater surgical expertise and incurs higher economic costs. Furthermore, ET carries unique procedure-related complications, as illustrated by Lobe et al.'s pediatric series where 1 of 31 cases (3.2%) developed postoperative subcutaneous hematoma (18). Other potential endoscopic-specific complications include subcutaneous tunnel paresthesia, flap perforation or necrosis, tumor implantation or recurrence around subcutaneous tunnel and so on.
4 Conclusion
ET via total areola approach demonstrates safety and feasibility in pediatric patients, offering advantages over OT through reduced surgical complications and superior cosmetic outcomes, minimizing physical and psychological trauma. Furthermore, ET performed by experienced surgeons utilizing pediatric-specific miniature instruments and auxiliary monitoring techniques can further improve its efficacy and safety. Further multicenter studies are warranted to validate these findings and refine technical protocols.
Data availability statement
The datasets presented in this article are not readily available because. The dataset cannot be shared with third parties without prior written consent. Any modification to the dataset is strictly prohibited without proper authorization. Requests to access the datasets should be directed to Kunpeng Hu,aHVrcGVuZ0BtYWlsLnN5c3UuZWR1LmNu.
Ethics statement
The study involving human participants was approved by the Institutional Review Board of the Third Affiliated Hospital of Sun Yat-sen University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
QC: Writing – original draft, Writing – review & editing. YK: Writing – review & editing, Methodology. WL: Writing – review & editing, Investigation. PZ: Writing – review & editing, Resources. JW: Data curation, Writing – review & editing. KH: Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by Guangzhou Science and Technology Planning Project (2024A03J0986), the National Natural Science Foundation Cultivation Project of the Third Hospital Affiliated with Sun Yat-sen University (2023GZRPYMS08) and the joint fund of the Third Affiliated Hospital of Sun Yat-sen University and Chaozhou Central Hospital, Project (LH202209).
Acknowledgments
This study is supported by the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, China. The authors also acknowledge the patient and her family for participating in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Vouchara A, Chorti A, Tzikos G, Menni A, Ntouma S, Giza S, et al. Thyroidectomy in children and adolescents: a systematic review. Gland Surg. (2024) 13:697–712. doi: 10.21037/gs-24-16
2. Lobe TE, Wright SK. The transaxillary, totally endoscopic approach for head and neck endocrine surgery in children. J Laparoendosc Adv Surg Tech. (2011) 21:97–100. doi: 10.1089/lap.2010.0163
3. Puzziello A, Rosato L, Innaro N, Orlando G, Avenia N, Perigli G, et al. Hypocalcemia following thyroid surgery: incidence and risk factors. A longitudinal multicenter study comprising 2,631 patients. Endocrine. (2014) 47:537–42. doi: 10.1007/s12020-014-0209-y
4. Drews JD, Cooper JN, Onwuka EA, Minneci PC, Aldrink JH. The relationships of surgeon volume and specialty with outcomes following pediatric thyroidectomy. J Pediatr Surg. (2019) 54:1226–32. doi: 10.1016/j.jpedsurg.2019.02.033
5. Sengul D, Sengul I, Ozturk T. Sutureless thyroidectomy with intraoperative neuromonitoring and energy-based device without sternotomy for symptomatic substernal goiter harboring thyroiditis of gland parenchyma. Cureus (2021) 13:e16258. doi: 10.7759/cureus.16258
6. Aydin I, Sengul I, Sengul D. Sutureless total thyroidectomy for substernal goiter: amending versus unnecessary. Cureus (2021) 13:e12720. doi: 10.7759/cureus.12720
7. Benmiloud F, Godiris-Petit G, Gras R, Gillot J-C, Turrin N, Penaranda G, et al. Association of autofluorescence-based detection of the parathyroid glands during total thyroidectomy with postoperative hypocalcemia risk: results of the PARAFLUO multicenter randomized clinical trial. JAMA Surg. (2020) 155(2):106–12. doi: 10.1001/jamasurg.2019.4613
8. Ngo DQ, Le DT, Hoang GN, Ngo QX, Le QV. Case report: transoral endoscopic thyroidectomy via vestibular approach in pediatric thyroid cancer. Front Pediatr. (2021) 9:765278. doi: 10.3389/fped.2021.765278
9. Cohen O, Tufano RP, Anuwong A, Russell JO, Assadi N, Dionigi G, et al. Trans-oral endoscopic thyroidectomy vestibular approach (TOETVA) for the pediatric population: a multicenter, large case series. Surg Endosc. (2022) 36:2507–13. doi: 10.1007/s00464-021-08537-4
10. Kinahan KE, Sharp LK, Seidel K, Leisenring W, Didwania A, Lacouture ME, et al. Scarring, disfigurement, and quality of life in long-term survivors of childhood cancer: a report from the childhood cancer survivor study. JCO. (2012) 30:2466–74. doi: 10.1200/JCO.2011.39.3611
11. Liao D, Ishii LE, Chen LW, Chen J, Juarez M, Darrach HM, et al. Transoral neck surgery prevents attentional bias towards the neck compared to open neck surgery. Laryngoscope. (2020) 130:1603–8. doi: 10.1002/lary.28305
12. Choi Y, Lee JH, Kim YH, Lee YS, Chang H-S, Park CS, et al. Impact of postthyroidectomy scar on the quality of life of thyroid cancer patients. Ann Dermatol. (2014) 26 (6):693–9. doi: 10.5021/ad.2014.26.6.693
13. Koo DH, Kim DM, Choi JY, Lee KE, Cho SH, Youn Y-K. In-depth survey of scarring and distress in patients undergoing bilateral axillo-breast approach robotic thyroidectomy or conventional open thyroidectomy. Surg Laparosc Endosc Percutan Tech. (2015) 25:436–9. doi: 10.1097/SLE.0000000000000187
14. Razavi CR, Khadem MGA, Fondong A, Clark JH, Richmon JD, Tufano RP, et al. Early outcomes in transoral vestibular thyroidectomy: robotic versus endoscopic techniques. Head Neck. (2018) 40:2246–53. doi: 10.1002/hed.25323
15. Pino C, Dominguez JM, Solar A, Zoroquiain P, Cruz F, García C, et al. Two Decades of Thyroid Nodule Cytology in Children: Malignancy Risk Assessment at a Tertiary Care Center. Horm Res Paediat. (2023):1–8. doi: 10.1159/000541134
16. Jiang W-J, Yan P-J, Zhao C-L, Si M-B, Tian W, Zhang Y-J, et al. Comparison of total endoscopic thyroidectomy with conventional open thyroidectomy for treatment of papillary thyroid cancer: a systematic review and meta-analysis. Surg Endosc. (2020) 34:1891–903. doi: 10.1007/s00464-019-07283-y
17. Cao F, Xie B, Cui B, Xu D. Endoscopic vs. conventional thyroidectomy for the treatment of benign thyroid tumors: a retrospective study of a 4-year experience. Exp Ther Med. (2011) 2:661–6. doi: 10.3892/etm.2011.267
Keywords: thyroidectomy, endoscopic surgical procedures, areola, child, age factors, thyroid nodule, adenoma, follicular
Citation: Cai Q, Ke Y, Li W, Zhang P, Wu J and Hu K (2025) Case Report: endoscopic thyroidectomy via total areola approach in a six-year-old patient with thyroid follicular adenoma. Front. Pediatr. 13:1549049. doi: 10.3389/fped.2025.1549049
Received: 20 December 2024; Accepted: 11 April 2025;
Published: 29 April 2025.
Edited by:
Nikolaos Zavras, University General Hospital Attikon, GreeceReviewed by:
Ilker Sengul, Giresun University, TürkiyeDavide Inversini, University of Insubria, Italy
Marina Minafra, Ospedale civile “Lorenzo Bonomo”, Italy
Copyright: © 2025 Cai, Ke, Li, Zhang, Wu and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kunpeng Hu, aHVrcGVuZ0BtYWlsLnN5c3UuZWR1LmNu
 Qingqing Cai
Qingqing Cai Yifan Ke
Yifan Ke Wenchao Li
Wenchao Li Peng Zhang
Peng Zhang Kunpeng Hu
Kunpeng Hu