- 1Department of Electrocardiogram, Huanggang Central Hospital, Huanggang, Hubei, China
- 2School of Public Health, Mudanjiang Medical University, Mudanjing, Heilongjiang, China
Aim: Handgrip strength (HGS), a measure of muscle strength, has been reported to be associated with the risk of hypertension in adults. This study intended to assess the relationship of relative HGS (rHGS) and HGS asymmetry ratio with elevated blood pressure and hypertension in children and adolescents.
Methods: This cross-sectional study included children and adolescents aged 6–19 years with HGS and blood pressure measurements in the 2011–2014 National Health and Nutrition Examination Survey (NHANES) dataset. The relationships of rHGS and HGS asymmetry ratio with elevated blood pressure and hypertension were assessed using weighted logistic regression models and described as odds ratio (OR) with 95% confidence interval (CI). Subgroup analysis was conducted according to age (<13, ≥13 years) and gender (male, female).
Results: In total, 3,736 children and adolescents were included in the study, of whom 509 (13.75%) had elevated blood pressure and 188 (4.72%) had hypertension. High rHGS levels were related to lower odds of elevated blood pressure (OR = 0.52, 95%CI, 0.33–0.81) and hypertension (OR = 0.34, 95%CI, 0.18–0.66). In addition, children and adolescents with HGS asymmetry ratio of >30.0% had higher odds of elevated blood pressure (OR = 2.14, 95%CI, 1.27–3.61) and hypertension (OR = 3.02, 95%CI, 1.42–6.42). Subgroup analyses demonstrated that the relationship between high rHGS levels and lower odds of elevated blood pressure and hypertension did not differ by age or sex, whereas the association between HGS asymmetry ratio of >30.0% and higher odds of elevated blood pressure and hypertension was found only in children ≥13 years and males.
Conclusion: High rHGS levels were associated with lower odds of elevated blood pressure and hypertension in children and adolescents, whereas an HGS asymmetry ratio of >30.0% was related to higher odds of elevated blood pressure and hypertension.
Introduction
Hypertension is a major risk factor for the development of cardiovascular disease in people of all ages (1, 2). Exposure to hypertension in childhood and adolescence has been found to be significantly associated with an increased risk of cardiovascular, cerebrovascular, and other chronic diseases in adulthood (3). Epidemiologic studies showed that approximately 14% of U.S. adolescents aged 12–19 had elevated blood pressure or hypertension during 2013–2016 (4). In addition, hypertension is difficult to diagnose in children and adolescents, and its true prevalence may be underestimated (5). Prevention and control of hypertension in children and adolescents is key to primary prevention of cardiovascular disease.
Skeletal muscle, the organ with the largest mass in the body, significantly influences metabolic processes, and skeletal muscle health is an important cardiometabolic marker (6). Handgrip strength (HGS) is a simple and reliable physiologic indicator of skeletal muscle strength in clinical settings (7). Several studies have reported that high HGS may be associated with a reduced risk of hypertension in adults (8, 9). Other studies have found that high HGS may be positively associated or not associated with the risk of hypertension in adults (10, 11). These inconsistent results may be influenced by body mass index (BMI), which has a significant effect on HGS values (10, 12). Relative HGS (rHGS) and HGS asymmetry ratio are both indicators of the level of HGS, with rHGS adjusting for BMI on the basis of absolute HGS and HGS asymmetry ratio responding to the difference in HGS between two hands (13, 14). rHGS and HGS asymmetry ratio have been found to be significantly related to the risk of metabolism-related diseases such as hypertension in adults as well as in the elderly population (8, 15). However, the relationship between HGS-related indicators and the risk of hypertension remains unclear in children and adolescent populations. Therefore, this study intended to investigate the association of rHGS and HGS asymmetry ratio with elevated blood pressure and hypertension in children and adolescents.
Methods
Study design and data sources
The data analyzed for this cross-sectional study were obtained from the National Health and Nutrition Examination Survey (NHANES) dataset from 2011 to 2014. The NHANES survey is conducted by the National Center for Health Statistics (NCHS) to evaluate the health and nutrition status of the United States non-hospitalized population (https://wwwn.cdc.gov/nchs/nhanes/AnalyticGuidelines.aspx). The NHANES survey collects data from participants through interviews and physical examinations in survey cycles every 2 years. Data in NHANES include demographic, dietary, socioeconomic, health-related, medical, physiologic measurements, and laboratory tests. Since HGS measurement data were only available in two survey cycles, 2011–2012 and 2013–2014, only NHANES data from 2011 to 2014 were analyzed in this study. Participants aged 6–19 years with HGS and blood pressure measurements were included. The exclusion criteria were as follows: (1) participants had any pain, aching or stiffness in right/left hand in the past 7 days; (2) participants with missing information on key covariates (e.g., BMI). The NHANES protocols were approved by the NCHS Research Ethics Review Board and written informed consent was obtained from each participant.
Outcomes
The outcomes were elevated blood pressure and hypertension. The diagnosis of elevated blood pressure and hypertension was based on the criteria of the American Academy of Pediatrics (16): (1) for children aged <13 years, elevated blood pressure was defined as systolic blood pressure (SBP) or diastolic blood pressure (DBP) ≥90th percentile blood pressure; hypertension was defined as SBP or DBP ≥95th percentile blood pressure; (2) for children aged ≥13 years, elevated blood pressure was defined as SBP/DBP ≥120/80 mmHg; hypertension was defined as SBP/DBP ≥130/80 mmHg. The 90th and 95th percentiles were derived by using quantile regression on the basis of normal-weight children (BMI <85th percentile).
Measurement of HGS
Muscle strength was measured through a HGS test using a handgrip dynamometer (17). After the examiner explained and demonstrated the test protocol to the participant, adjusted the grip size of the dynamometer, and the participant practiced the test, the participant was asked to squeeze the dynamometer as hard as possible with one hand while exhaling to avoid a buildup of pressure in the chest. This test was then repeated on the other hand. Each hand was tested three times alternately. The combined HGS was calculated as the sum of the maximum readings from each hand. The rHGS was calculated as: the combined HGS/BMI. The HGS asymmetry ratio was calculated as: . The rHGS values were divided into three groups based on tertiles according to male and female, respectively [male: <2.13 (low), 2.13–3.22 (median), ≥3.22 (high); female: <1.86 (low), 1.86–2.4 (median), ≥2.4 (high)]. The HGS asymmetry ratio was categorized into four groups according to previous studies (18): 0%–10%, 10.1%−20.0%, 20.1%−30.0%, and >30.0%.
Data collection
Participant data were collected including age, gender (male, female), race (White, Black, others), education level (below high school, high school, above high school), family poverty-to-income ratio (PIR) (<1.3, ≥1.3, unknown), screen time (<5, ≥5 h), physical activity (non-ideal, ideal), birth weight (<5.5 pounds, ≥5.5 lbs, unknown), household smokers (no, yes, unknown), family education (below high school, high school, above high school, unknown), total cholesterol, direct high density lipoprotein cholesterol (HDL-C), cotinine (<0.05, ≥0.05 μg/L, unknown), Healthy Eating Index (HEI)-2020, HGS, rHGS, and HGS asymmetry ratio.
Statistical analysis
Continuous data were described as mean and standard error (S.E), and weighted t-test was used for comparisons between groups. Categorical data were described as the numbers and composition ratio [N (%)], and the Chi-square test was used for comparisons between multiple groups. Weighted variables (SDMVPSU, SDMVSTRA, WTINT2YR) from the NHANES database were used for statistical analysis.
A few variables (education level, physical activity, direct HDL-C, total cholesterol, and HEI-2020) had missing values, and multiple interpolation method was used to interpolate the missing values. Difference analysis showed no statistically significant differences before and after the interpolation of missing variables (Supplementary Table 1). Weighted univariable logistic regression model was applied to screen for confounders related to elevated blood pressure and hypertension, respectively. Variables with P < 0.05 in the univariable model were adjusted as confounders in the multivariable model (Supplementary Tables 2, 3). The associations of rHGS and HGS asymmetry ratio with elevated blood pressure and hypertension were assessed using weighted univariable and multivariable logistic regression models and expressed as odds ratio (OR) with 95% confidence interval (CI). Moreover, the non-linear relationship of rHGS with elevated blood pressure and hypertension was explored using restricted cubic spline (RCS). Subgroup analysis was conducted according to age (<13, ≥13 years) and gender (male, female). Statistical analyses were completed using SAS 9.4 software (SAS Institute, Cary, NC). Statistical significance was defined as P < 0.05.
Results
Characteristics of populations
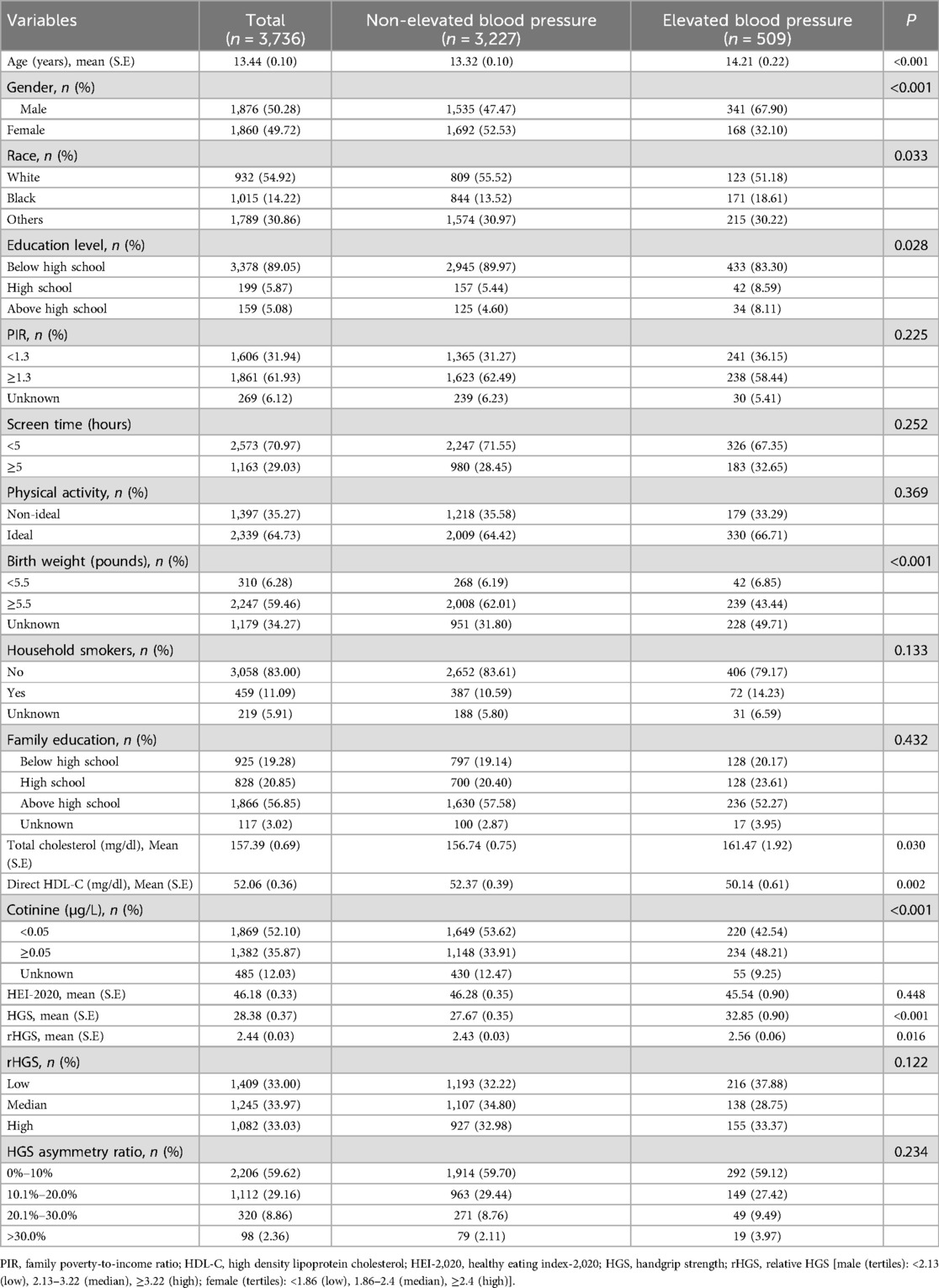
A total of 5,404 children and adolescents aged 6–19 years were recorded in the 2011–2014 NHANES survey. After excluding 1,668 participants, 3,736 participants were included in the analysis (Figure 1). The characteristics of participants according to elevated blood pressure were shown in Table 1. Moreover, the characteristics of participants according to hypertension were presented in Supplementary Table 4. There were 509 (13.75%) participants with elevated blood pressure and 188 (4.72%) participants with hypertension. The mean age was 13.44 (0.10) years and 1,876 (50.28%) participants were male. The mean HGS and rHGS were 28.38 (0.37) kg and 2.44 (0.03), respectively. There were 2,206 (59.62%) participants with HGS asymmetry ratio of 0%–10%, 1,112 (29.16%) with HGS asymmetry ratio of 10.1%–20.0%, 320 (8.86%) with HGS asymmetry ratio of 20.1%–30.0%, and 98 (2.36%) with HGS asymmetry ratio of >30.0%.
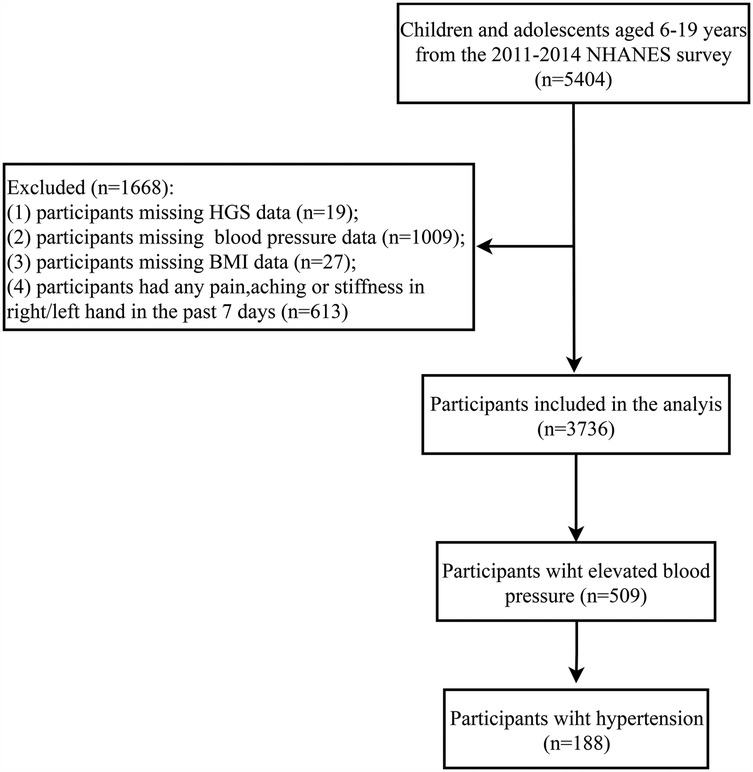
Figure 1. Screening flowchart for the population. NHANES, the National Health and Nutrition Examination Survey; HGS, handgrip strength; BMI, body mass index.
Relationship of rHGS and HGS asymmetry ratio with elevated blood pressure and hypertension in children and adolescents
The associations between HGS and elevated blood pressure and hypertension in children and adolescents were presented in Table 2. Children with median (OR = 0.52, 95%CI, 0.32–0.85) and high (OR = 0.52, 95%CI, 0.33–0.81) rHGS levels were related to lower odds of elevated blood pressure compared with children with low rHGS levels. For hypertension, median (OR = 0.55, 95%CI, 0.34–0.89) and high (OR = 0.34, 95%CI, 0.18–0.66) rHGS levels were also correlated with lower odds of hypertension compared with low rHGS levels. In addition, children with HGS asymmetry ratio of >30.0% had higher odds of elevated blood pressure (OR = 2.14, 95%CI, 1.27–3.61) and hypertension (OR = 3.02, 95%CI, 1.42–6.42) compared with children with HGS asymmetry ratio of 0%–10%, but not for children with HGS asymmetry ratio of 10.1%–20.0% and 20.1%–30.0% (P > 0.05). The RCS curves showed that there were non-linear relationships between rHGS levels and elevated blood pressure and hypertension (Figure 2). The relationship between rHGS levels and elevated blood pressure was “V” shaped, while the relationship between rHGS levels and hypertension was “U” shaped.
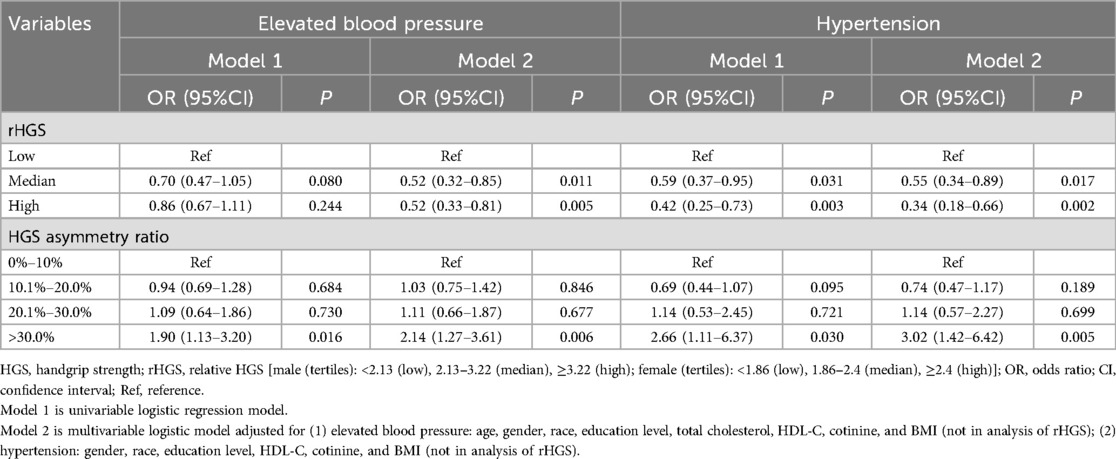
Table 2. Associations between HGS and elevated blood pressure and hypertension in children and adolescents.
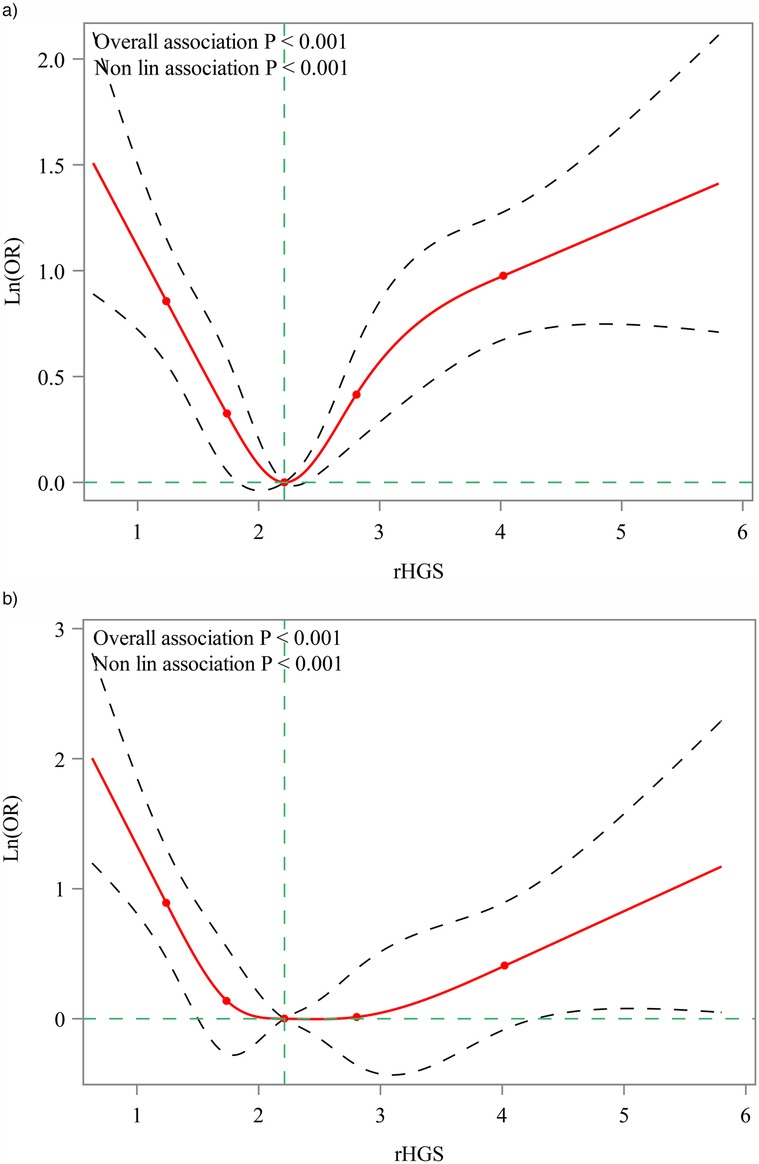
Figure 2. Restricted cubic spline (RCS) for the non-linear relationship of rHGS with elevated blood pressure and hypertension. (a) Association between rHGS and elevated blood pressure; (b) association between rHGS and hypertension. rHGS, relative handgrip strength; OR, odds ratio.
The relationships between HGS and elevated blood pressure and hypertension in children were further analyzed based on age (<13, ≥13 years) and gender (male, female) subgroups (Table 3). For rHGS, high rHGS levels were associated with lower odds of elevated blood pressure in children aged <13 years (OR = 0.34, 95%CI, 0.14–0.83) and ≥13 years (OR = 0.40, 95%CI, 0.23–0.69). High rHGS levels were also related to lower odds of hypertension in children aged <13 years (OR = 0.39, 95%CI, 0.16–0.94) and ≥13 years (OR = 0.26, 95%CI, 0.08–0.85). In the analysis of HGS asymmetry ratio, the association of HGS asymmetry ratio of >30.0% with higher odds of elevated blood pressure (OR = 2.54, 95%CI, 1.29–4.99) and hypertension (OR = 5.48, 95%CI, 1.78–16.87) was found only in children aged ≥13 years.
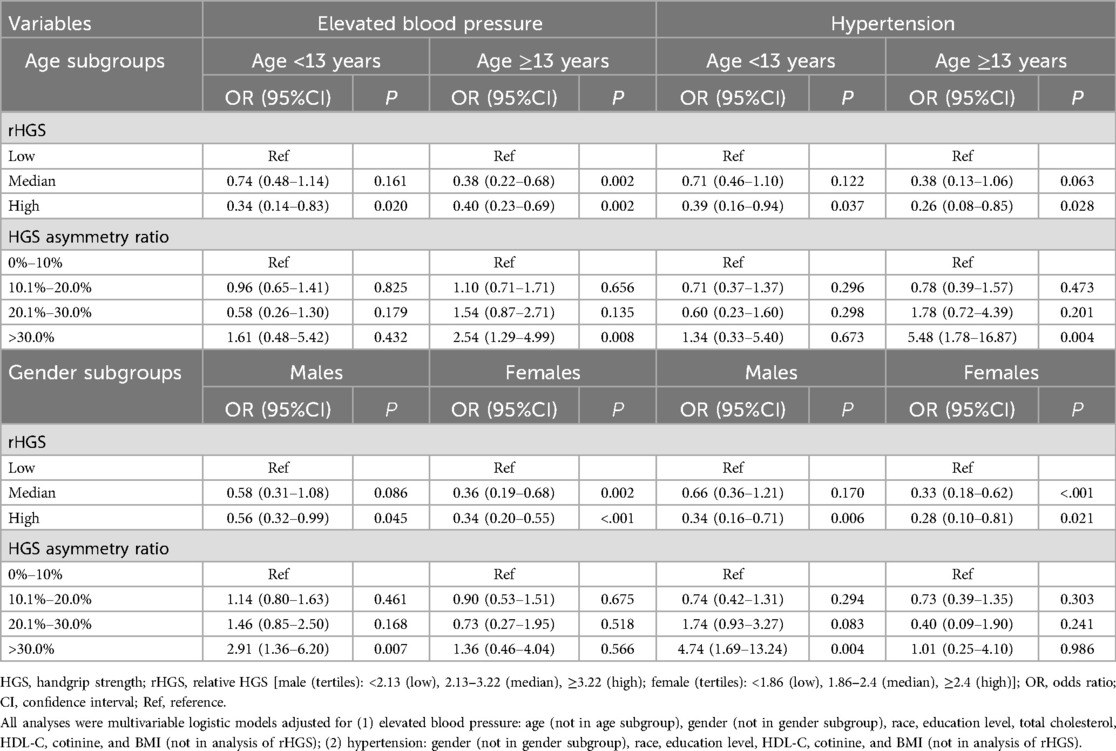
Table 3. Subgroup analysis of the relationships between HGS and elevated blood pressure and hypertension in age and gender subgroups.
In the gender subgroups, high rHGS levels were related to lower odds of elevated blood pressure and hypertension in males [elevated blood pressure: OR = 0.56, 95%CI, 0.32–0.99; hypertension: OR = 0.34, 95%CI, 0.16–0.71] and females [elevated blood pressure: OR = 0.34, 95%CI, 0.20–0.55; hypertension: OR = 0.28, 95%CI, 0.10–0.81]. Moreover, the relationship of HGS asymmetry ratio of >30.0% with higher odds of elevated blood pressure (OR = 2.91, 95%CI, 1.36–6.20) and hypertension (OR = 4.74, 95%CI, 1.69–13.24) was observed only in males.
Discussion
The current study analyzed the relationship between HGS and elevated blood pressure and hypertension in children and adolescents. Our results showed that high rHGS levels were correlated with lower odds of elevated blood pressure and hypertension in children. HGS asymmetry ratio of >30.0% were related to higher odds of elevated blood pressure and hypertension in children. Subgroup analysis found that the relationship between high rHGS levels and lower odds of elevated blood pressure and hypertension was observed in children aged <13 years or ≥13 years and males or females, whereas the association between HGS asymmetry ratio of >30.0% and higher odds of elevated blood pressure and hypertension was found only in children ≥13 years and males.
Muscle strength is a good indicator of overall health, and HGS is a reliable biomarker for assessing muscle strength (19, 20). Previous studies have reported a relationship between HGS and blood pressure in adults (8, 9, 21). Increased HGS was significantly associated with a reduced risk of hypertension in adult women (8). A prospective cohort study showed that high weight-adjusted HGS was associated with a lower risk of hypertension in middle-aged and older adults, but not absolute HGS (9). Several meta-analyses have shown isometric HGS training to be effective in reducing resting blood pressure in adults (22, 23). Some studies have also reported a relationship between HGS and other diseases such as pulmonary hypertension (24), cardiovascular disease (25), and chronic kidney disease (26). HGS decreased with the increase of the level of forebrain natriuretic peptide, a key indicator of pulmonary hypertension monitoring (24). In addition, BMI may affect the role of HGS (12, 27), and the association between blood pressure and handgrip strength in children may be confused by BMI (10). This study assessed the relationship between BMI-adjusted HGS (rHGS) and elevated blood pressure and hypertension in children aged 6–19 years. High rHGS levels were found to be correlated with lower odds of elevated blood pressure and hypertension in children. Our findings suggested that the relationship between HGS and blood pressure in children was consistent with the results of previous studies in adults (8, 9). In addition, an HGS asymmetry ratio of >30.0% was associated with higher odds of elevated blood pressure and hypertension. The HGS asymmetry ratio reflects the difference of HGS between the two hands of an individual, and a large HGS asymmetry ratio may represent a functional deficiency of the neuromuscular system (14). Moreover, subgroup analysis showed that the relationship between HGS asymmetry ratio of >30.0% and higher odds of elevated blood pressure and hypertension was observed only in children ≥13 years and males. A study also showed no difference in HGS between males and females from 6 to 11 years of age, but from 12 years of age onwards, males had higher HGS values in both hands (28).
The exact mechanism by which HGS affects blood pressure in children remains unclear, and several possible explanations have been proposed in previous studies. Possible mechanisms for the effects of HGS training on blood pressure include improvements in conduit and resistance due to endothelium-dependent dilation, oxidative stress, and autoregulation of heart rate and blood pressure (29). HGS training may lower blood pressure by attenuating peripheral sympathetic vasoconstrictor activity (30). HGS training is associated with increased NO-dependent dilation of local ductus arteriosus in hypertensive patients (31). Moreover, HGS training improves the vasodilatory response, and prolonged training may increase vessel diameter and decrease total peripheral resistance, which in turn enhances autonomic vasodilation (32, 33). In addition to representing muscle strength, HGS is also an indicator of muscle mass and even nutritional status (19). Individuals with higher HGS levels are more likely to engage in healthy lifestyle behaviors that affect hypertension risk and overall health. Improved muscle health is associated with the release of cytokines and myokines into the circulation, which may enhance anti-atherosclerotic properties (34, 35). However, the specific mechanisms underlying the effects of HGS on blood pressure in children may depend on subsequent mechanistic studies.
We assessed the relationship between HGS and elevated blood pressure and hypertension in children and adolescents. Unlike previous studies in adults, we used rHGS and HGS asymmetry ratio instead of absolute HGS. rHGS can rule out the effect of BMI on HGS. Nevertheless, several limitations of this study should be considered. First, this study was a cross-sectional study design that did not allow for causal inferences and may be subject to some bias. The association between HGS-related indicators and hypertension in children and adolescents still needs further validation in prospective studies. Second, judgments of elevated blood pressure and hypertension in this study were based on multiple blood pressure measurements taken on a single day, rather than spread over two or more visits, which may have been biased. Third, some potential confounders such as family history of hypertension could not be obtained due to limitations of the NHANES database.
Conclusions
High rHGS levels were related to lower odds of elevated blood pressure and hypertension in children and adolescents, whereas an HGS asymmetry ratio of >30.0% was correlated with higher odds of elevated blood pressure and hypertension. In addition, the association between rHGS and elevated blood pressure and hypertension did not differ by age or sex, whereas the correlation between HGS asymmetry ratio and elevated blood pressure and hypertension was found only in children ≥13 years and males.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: NHANES database, https://wwwn.cdc.gov/nchs/nhanes/.
Ethics statement
The requirement of ethical approval was waived by School of Public Health, Mudanjiang Medical University for the studies involving humans because the NHANES protocols were approved by the NCHS Research Ethics Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
HL: Conceptualization, Project administration, Supervision, Writing – original draft, Writing – review & editing. HG: Data curation, Formal analysis, Investigation, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2025.1559556/full#supplementary-material
References
1. Colafella KMM, Denton KM. Sex-specific differences in hypertension and associated cardiovascular disease. Nat Rev Nephrol. (2018) 14(3):185–201. doi: 10.1038/nrneph.2017.189
2. Dawson JD, Sonka M, Blecha MB, Lin W, Davis PH. Risk factors associated with aortic and carotid intima-media thickness in adolescents and young adults: the muscatine offspring study. J Am Coll Cardiol. (2009) 53(24):2273–9. doi: 10.1016/j.jacc.2009.03.026
3. Khoury M, Urbina EM. Cardiac and vascular target organ damage in pediatric hypertension. Front Pediatr. (2018) 6:148. doi: 10.3389/fped.2018.00148
4. Jackson SL, Zhang Z, Wiltz JL, Loustalot F, Ritchey MD, Goodman AB, et al. Hypertension among youths—United States, 2001–2016. MMWR Morb Mortal Wkly Rep. (2018) 67(27):758–62. doi: 10.15585/mmwr.mm6727a2
5. Khoury M, Urbina EM. Hypertension in adolescents: diagnosis, treatment, and implications. Lancet Child Adolesc Health. (2021) 5(5):357–66. doi: 10.1016/s2352-4642(20)30344-8
6. Ramírez-Vélez R, Correa-Bautista JE, Lobelo F, Izquierdo M, Alonso-Martínez A, Rodríguez-Rodríguez F, et al. High muscular fitness has a powerful protective cardiometabolic effect in adults: influence of weight status. BMC Public Health. (2016) 16(1):1012. doi: 10.1186/s12889-016-3678-5
7. Buigues C, Padilla-Sánchez C, Garrido JF, Navarro-Martínez R, Ruiz-Ros V, Cauli O. The relationship between depression and frailty syndrome: a systematic review. Aging Ment Health. (2015) 19(9):762–72. doi: 10.1080/13607863.2014.967174
8. Feng Q, Jiang C, Wang M, Cai R, Wang H, Wu D, et al. Association between relative handgrip strength and hypertension in Chinese adults: an analysis of four successive national surveys with 712,442 individuals (2000–2014). PLoS One. (2021) 16(10):e0258763. doi: 10.1371/journal.pone.0258763
9. Gu Y, Dong J, Meng G, Zhang Q, Liu L, Wu H, et al. Handgrip strength as a predictor of incident hypertension in the middle-aged and older population: the TCLSIH cohort study. Maturitas. (2021) 150:7–13. doi: 10.1016/j.maturitas.2021.06.002
10. Ji C, Zheng L, Zhang R, Wu Q, Zhao Y. Handgrip strength is positively related to blood pressure and hypertension risk: results from the national health and nutrition examination survey. Lipids Health Dis. (2018) 17(1):86. doi: 10.1186/s12944-018-0734-4
11. Ash GI, Taylor BA, Thompson PD, MacDonald HV, Lamberti L, Chen MH, et al. The antihypertensive effects of aerobic versus isometric handgrip resistance exercise. J Hypertens. (2017) 35(2):291–9. doi: 10.1097/hjh.0000000000001176
12. Dong B, Wang Z, Arnold L, Song Y, Wang HJ, Ma J. The association between blood pressure and grip strength in adolescents: does body mass Index matter? Hypertens Res. (2016) 39(12):919–25. doi: 10.1038/hr.2016.84
13. Byeon JY, Lee MK, Yu MS, Kang MJ, Lee DH, Kim KC, et al. Lower relative handgrip strength is significantly associated with a higher prevalence of the metabolic syndrome in adults. Metab Syndr Relat Disord. (2019) 17(5):280–8. doi: 10.1089/met.2018.0111
14. Fraser BJ, Blizzard L, Tomkinson GR, McGrath R, Dwyer T, Venn AJ, et al. Tracking handgrip strength asymmetry from childhood to mid-life. Acta Paediatr. (2023) 112(11):2408–17. doi: 10.1111/apa.16930
15. Klawitter L, Bradley A, Hackney KJ, Tomkinson GR, Christensen BK, Kraemer WJ, et al. The associations between asymmetric handgrip strength and chronic disease status in American adults: results from the National Health and Nutrition Examination Survey. J Funct Morphol Kinesiol. (2021) 6(4):79. doi: 10.3390/jfmk6040079
16. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. (2017) 140(3):e20171904. doi: 10.1542/peds.2017-1904
17. National Health and Nutrition Examination Survey. Muscle strength-grip test. (2014). Available at: https://wwwn.cdc.gov/Nchs/Nhanes/2011-2012/MGX_G.htm#MGDCGSZ (Accessed January 04, 2025).
18. McGrath R, Clark BC, Cesari M, Johnson C, Jurivich DA. Handgrip strength asymmetry is associated with future falls in older Americans. Aging Clin Exp Res. (2021) 33(9):2461–9. doi: 10.1007/s40520-020-01757-z
19. Bohannon RW. Grip strength: an indispensable biomarker for older adults. Clin Interv Aging. (2019) 14:1681–91. doi: 10.2147/cia.S194543
20. Bohannon RW, Magasi SR, Bubela DJ, Wang YC, Gershon RC. Grip and knee extension muscle strength reflect a common construct among adults. Muscle Nerve. (2012) 46(4):555–8. doi: 10.1002/mus.23350
21. He P, Gan X, Ye Z, Liu M, Zhou C, Wu Q, et al. Combined handgrip strength and walking pace, genetic susceptibility, and incident hypertension: a prospective study in UK biobank. Scand J Med Sci Sports. (2023) 33(6):989–99. doi: 10.1111/sms.14336
22. Kelley GA, Kelley KS. Isometric handgrip exercise and resting blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. (2010) 28(3):411–8. doi: 10.1097/HJH.0b013e3283357d16
23. Jin YZ, Yan S, Yuan WX. Effect of isometric handgrip training on resting blood pressure in adults: a meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. (2017) 57(1–2):154–60. doi: 10.23736/s0022-4707.16.05887-4
24. Kavgacı A, Kula S, Berber Maraşlı E, Zinnuroğlu M, Çelik B, Terlemez S, et al. Evaluation of handgrip strength in children with pulmonary hypertension. Cardiol Young. (2024) 34(7):1482–6. doi: 10.1017/S1047951124000398
25. Lim TS, Kwon S, Bae SA, Chon HY, Jang SA, Kim JK, et al. Association between handgrip strength and cardiovascular disease risk in MASLD: a prospective study from UK biobank. J Cachexia Sarcopenia Muscle. (2025) 16(2):e13757. doi: 10.1002/jcsm.13757
26. He P, Ye Z, Liu M, Li H, Zhang Y, Zhou C, et al. Association of handgrip strength and/or walking pace with incident chronic kidney disease: a UK biobank observational study. J Cachexia Sarcopenia Muscle. (2023) 14(2):805–14. doi: 10.1002/jcsm.13180
27. Díez-Fernández A, Sánchez-López M, Gulías-González R, Notario-Pacheco B, Cañete García-Prieto J, Arias-Palencia N, et al. BMI as a mediator of the relationship between muscular fitness and cardiometabolic risk in children: a mediation analysis. PLoS One. (2015) 10(1):e0116506. doi: 10.1371/journal.pone.0116506
28. Gómez-Campos R, Vidal Espinoza R, de Arruda M, Ronque ERV, Urra-Albornoz C, Minango JC, et al. Relationship between age and handgrip strength: proposal of reference values from infancy to senescence. Front Public Health (2022) 10:1072684. doi: 10.3389/fpubh.2022.1072684
29. Millar PJ, McGowan CL, Cornelissen VA, Araujo CG, Swaine IL. Evidence for the role of isometric exercise training in reducing blood pressure: potential mechanisms and future directions. Sports Med. (2014) 44(3):345–56. doi: 10.1007/s40279-013-0118-x
30. McGowan CL, Visocchi A, Faulkner M, Verduyn R, Rakobowchuk M, Levy AS, et al. Isometric handgrip training improves local flow-mediated dilation in medicated hypertensives. Eur J Appl Physiol. (2006) 98(4):355–62. doi: 10.1007/s00421-006-0282-x
31. Grassi G, Seravalle G, Quarti-Trevano F. The “neuroadrenergic hypothesis” in hypertension: current evidence. Exp Physiol. (2010) 95(5):581–6. doi: 10.1113/expphysiol.2009.047381
32. Baffour-Awuah B, Pearson MJ, Dieberg G, Smart NA. Isometric resistance training to manage hypertension: systematic review and meta-analysis. Curr Hypertens Rep. (2023) 25(4):35–49. doi: 10.1007/s11906-023-01232-w
33. Edwards JJ, Wiles J, O’Driscoll J. Mechanisms for blood pressure reduction following isometric exercise training: a systematic review and meta-analysis. J Hypertens (2022) 40(11):2299–306. doi: 10.1097/hjh.0000000000003261
34. Polo-López A, Calatayud J, Núñez-Cortés R, Andersen LL, Moya-Ramón M, López-Bueno R. Dose-response association between handgrip strength and hypertension: a longitudinal study of 76,503 European older adults. Curr Probl Cardiol. (2023) 48(9):101813. doi: 10.1016/j.cpcardiol.2023.101813
Keywords: handgrip strength, hypertension, HGS asymmetry ratio, children and adolescents, NHANES
Citation: Li H and Gu H (2025) Association between handgrip strength and hypertension in children and adolescents: an analysis of the National Health and Nutrition Examination Survey 2011–2014. Front. Pediatr. 13:1559556. doi: 10.3389/fped.2025.1559556
Received: 13 January 2025; Accepted: 31 March 2025;
Published: 14 April 2025.
Edited by:
Edson Zangiacomi Martinez, University of São Paulo, BrazilReviewed by:
Virginia Weffort, Universidade Federal do Triângulo Mineiro, BrazilAkif Kavgacı, Ankara Etlik City Hospital, Türkiye
Copyright: © 2025 Li and Gu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongmei Gu, Z2hvbmdtZWkzMUAxNjMuY29t
 Huanhuan Li1
Huanhuan Li1 Hongmei Gu
Hongmei Gu