- Department of Orthopedics, Shanghai Children’s Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
Aim: To understand, comprehensively, care experiences of caregivers for children with developmental dislocation of the hip in Tibet, China.
Background: Postoperative rehabilitation for children with developmental dislocation of the hip (DDH) may last for several months to years. Even after discharge, recovery is often partial. It is important to note that despite optimal surgical treatment, lifelong residual issues may persist, such as limping, chronic pain, or early-onset osteoarthritis. Home care is critical in postoperative recovery. Family as the basic unit of home-based care for patients, many measures are inevitably carried out in the family environment and rely on family caregivers to provide. This requires caregivers to pay long-term and high attention, posing significant challenges to caregiving capacity.
Design: A convergent mixed-methods.
Methods: Caregivers (n = 76) completed the Chinese version of the Family Caregiver Care Ability Scale, the Zarit Caregiver Burden Scale and 12 participated in semi-structured interviews from September, 2023 to February 2024. Descriptive statistics and Pearson correlation analysis were used for quantitative analysis, thematic analysis for qualitative analysis. Both quantitative and qualitative data were merged and integrated for mixed-methods analysis.
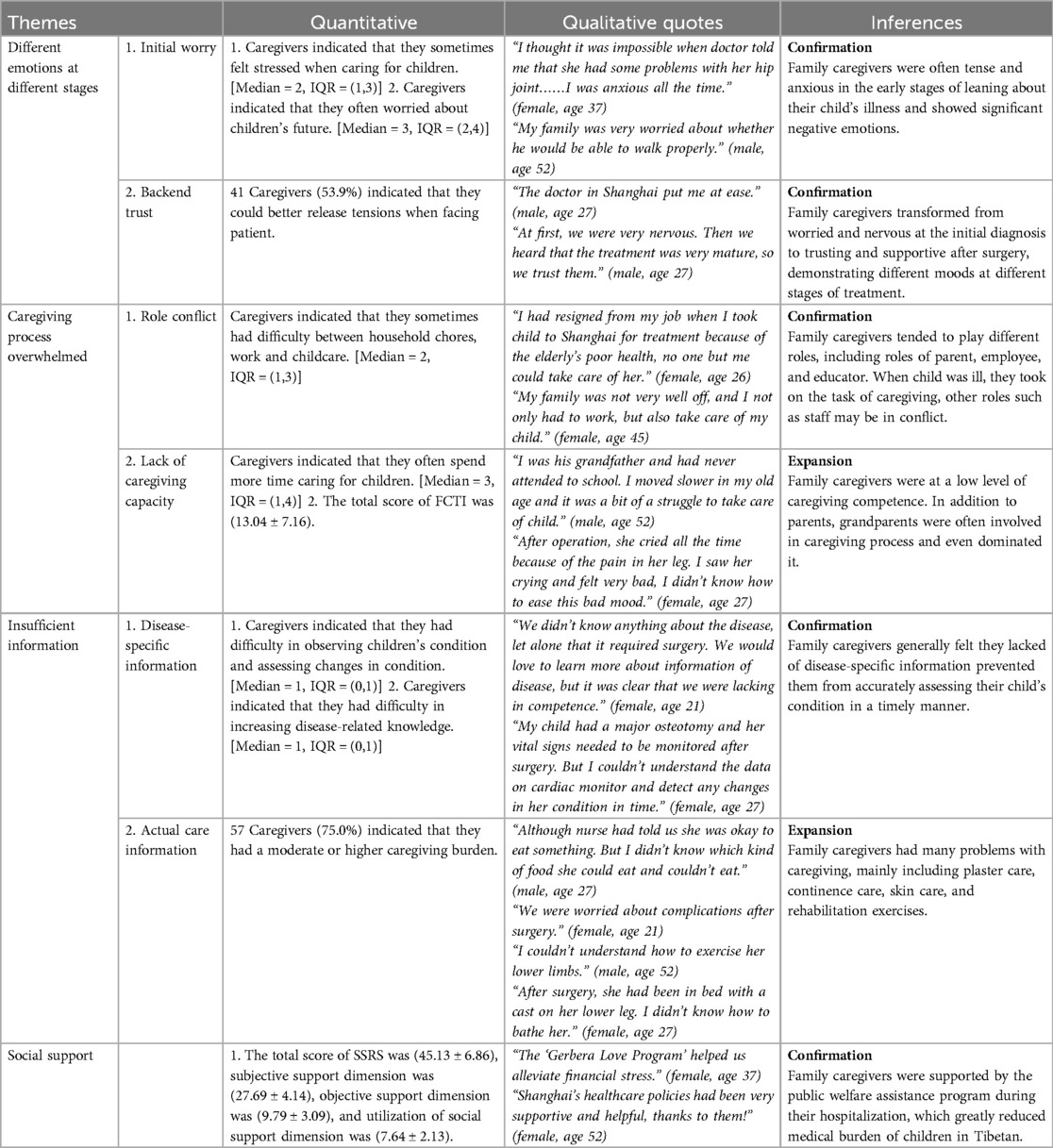
Results: Low caregiver capacity and moderate caregiver burden scores were reported. Four themes emerged from care experiences: different emotions at different stages (initial worry, backend trust), caregiving process overwhelmed (role conflict, lack of caregiving capacity), insufficient information (disease-specific information, actual care information), and social support.
Conclusion: This study is the first to use this mixed-methods design to analyze the current state of care and burden among family caregivers of children with developmental dislocation of the hip in Chinese highland region-Tibet. The combined results showed that qualitative results converged with quantitative results in terms of emotional changes, role burden, lack of disease-specific information, and social support; qualitative results complemented quantitative results in terms of caregiving capacity deficits and lack of actual care information to explain the quantitative results. The quantitative findings also emphasized the link between social support in terms of caregiving capacity and caregiving burden. These results guide future research to promote rehabilitation and improve quality of life for affected children and families.
Introduction
Developmental dysplasia of the hip (DDH) represents a spectrum of disorders affecting the development of the hip joint and is one of the most common congenital malformation in pediatric orthopedics (1). Clinically, it mostly occurs in infants and young children, and will gradually develop symptoms such as limitation of hip joint movement and pain during growth (2). The pathogenesis of DDH is not well understood, and it is currently believed that disease progression intertwines genetic susceptibility with external mechanical forces on the developing hip (3). Such forces affect the developmental window in utero and shortly after birth and may distort the alignment of femoral head with acetabulum. DDH is influenced by a variety of factors and the etiology involves both genetic and non-genetic factors. Literatures reported that positive family history, gender (often female), breech birth were risk factors contributed to development of this disorder (4). In addition, the “bundled” swaddling position with legs extended, hips extended and adducted can deteriorate the immature hip joint and increase the risk of DDH (5). Maternal hormones (e.g., estrogen) may contribute to development of DDH, but perinatal hormones (e.g., “relaxin”) are more likely to contribute to DDH (6). Some studies have shown the incidence of DDH is related to race, with higher rates in Canda and North America, followed by Africa and China (7). The prevalence of DDH had been reported to be about 1% in worldwide (8) and about 0.09%–0.30% in China (9, 10). This rate varied by region, for example, in Shanghai, a coastal city in eastern China, the prevalence of DDH was nearly 0.91% (11), while in Shigatse-Tibet, a high-altitude city in western China, the prevalence was as high as 32.4% (12). Currently, the occurrence of late primary diagnosis of DDH has been greatly reduced by early neonatal hip ultrasound screening in developed countries and in cities such as Shanghai and Beijing in China. But in western part of China, especially in underdeveloped areas such as Tibet, many children with late primary diagnosis of DDH existed due to weakness of healthcare base. Therefore, growth and development of Tibetan children deserve attention of medical professionals.
DDH involves ligaments, femoral head and joint capsule, resulting in loss of normal relationship between bone and acetabulum in joint capsule, making joint dislocated or subluxated. It includes three types of acetabular dysplasia, subluxation and dislocation. Main manifestations are limping, swaying, limitation of limb movement, etc., which affecting development and growth of children (13). At present, there are still controversies internationally regarding the treatment and duration of DDH in children. The Graf method for ultrasound diagnosis and grading are currently the most used and accepted method for DDH diagnosis and grading (14, 15). This method can be used to guide the selection of intervention methods as well as predict treatment outcomes. Early diagnosis and timely treatment are key points of DDH. At present, surgery combined with plaster fixation was mostly used to achieve purpose of treatment (16). However, there remains a risk of complications, such as avascular necrosis (AVN), which may occur not only after surgery but also folloeing treatment with the Pavlik harness. This complication can impair the growth of the femoral head or acetabulum, potentially compromising long-term outcomes (16, 17). Some researchers found recovery of hip function in children with DDH has a direct impact on efficacy of surgery, and the guarantee of surgical efficacy depends on continuous postoperative care, rehabilitation exercises, daily mobility exercises and prevention of complications (18). Inadequate caring may result in trauma to hip joint and surrounding soft tissues or adhesions within joint due to hematoma, which even lead to serious consequences such as joint re-dislocation, joint stiffness, and so on (19). Therefore, good postoperative care and rehabilitation is quite crucial.
Based on characteristics of disease, most children will return home to carry out rehabilitation training on their own after a period of treatment in hospital. Due to the young age of children, most of their caring and rehabilitation training was done with assistance of family caregivers, which put corresponding demands on caregiving ability of family caregivers. It has been shown that active involvement of family caregivers in caregiving can shorten days of hospitalization and promote recovery (20). However, good home care was more effective in preventing complications, promoting improvement of limb function, daily ability and quality of life. Relevant studies have confirmed that family caregivers of children with DDH are not sufficiently knowledgeable about disease awareness and caregiving skills (20–22). Many caregivers lack various types of information during treatment, such as disease information (etiology, clinical manifestations, etc.); preoperative information (preoperative preparations, surgical procedures, etc.); postoperative information (pain control measures, skin care, dietary management, etc.) and discharge information (time of review, care measures during immobilization in a cast or brace, functional limb exercises, etc.). Furthermore, researchers concluded family caregivers were less capable of providing home care in four areas of living care, plaster care, skin care, and exercise guidance (21). This showed family caregivers need to improve their knowledge and skills in caring for their children.
Scholars have focused on analysis of home care for children with DDH in low altitude areas, there is a lack of research on caregiving experiences of family caregivers of children with DDH in high altitude areas. Therefore, a need exists to further understand family caregivers’ experiences and feelings to evaluate their caring attitude and skills.
This study
Aims
To gain an in-depth understanding of the caregiving burden and caregiving experience felt by family caregivers accompanying children with DDH during hospitalization after surgical treatment in the highland region of western China-Tibet, as an indicator of family caregiving management. This study focused on a few specific questions:
1. What are the caregiving burdens perceived by family caregivers when administering care to children with DDH during hospitalization?
2. What is the family caregiver's ability to provide care to the children with DDH during hospitalization?
3. What are the family caregivers’ perceptions of the caregiving experience? To what extent are these perceptions consistent with their experiences?
Design
A convergent mixed-methods design was used in this study, where the quantitative and qualitative components had equal, and separate, simultaneous status in the study. Data was compared, contrasted, transformed, and correlated when analyzing.
Setting
This study was conducted in the orthopedic ward of a tertiary pediatric hospital in Shanghai, China. Many children with DDH come to here every year for treatment because this hospital is running a public assistance program, “Love of Gesang Flower”, for children with DDH in Tibet, a high-altitude region in western China. DDH families usually stayed in hospital for 10–14 days until their vital signs were stabilized, then staff arranged for a train to take them back to Tibet. Caregivers lived with child during treatment. The orthopedic ward set up with beds for caregivers to accompany their children, making it easy for caregivers to check on their child's status at any time. All costs for the treatment were covered by that public assistance program at no additional costs.
Sample
Inclusion criteria included: (a) being the primary caregiver of the child, providing care without compensation; (b) caring for a child diagnosed with DDH by x-ray (unilateral or bilateral) and treatment of hip joint open reduction + pelvic + femoral osteotomy; (c) having good language skills (if the caregiver was an ethnic minority who was unable to speak Mandarin, an interpreter or a translator should be provided) and agreeing to participate in the study. The exclusion criteria included: (a) mental abnormality; (b) those who were unable to fill out the questionnaire completely or answers to entries were consecutively the same; and (c) those who participated in other research projects during the research period.
During the quantitative study, a total of 80 questionnaires were distributed and 80 were recovered, of which 4 had the phenomenon of consecutively identical responses, thus 76 questionnaires were valid, with an overall validity rate of 95%. During the qualitative phase of the study, 12 family caregivers were recruited through convenience sampling. A small qualitative sample size is justified as it provides a deeper understanding of the phenomenon under study (23).
Data collection
Data collection period was from September 2023 to June 2024. The same researcher was responsible for data collection to ensure consistency. Prior to data collection, participants were provided with complete information about the study and signed a written informed consent form. The researcher stayed with participants during the administration of scale and answered their questions. They were reminded of their right to withdraw. After completing the questionnaire, participants were asked if they were willing to join in a 10–30 minutes semi-structured interview. Interviews were generally scheduled on the 3rd day after surgery. The reasons for conducting the interview were explained to those family members who were willing to be interviewed, and then they were asked to be interviewed in a quiet place. The whole interview process avoided using induced cues, summarized responses of family caregivers at the right time, and recorded the interviewee's true and comprehensive experiences, views, opinions, knowledge and attitudes after obtaining his or her consent. The orthopedic demonstration room was selected as the interview site. The audio recordings were converted into textual form within 24 h. Two researchers collected information, and used thematic analysis to refine themes.
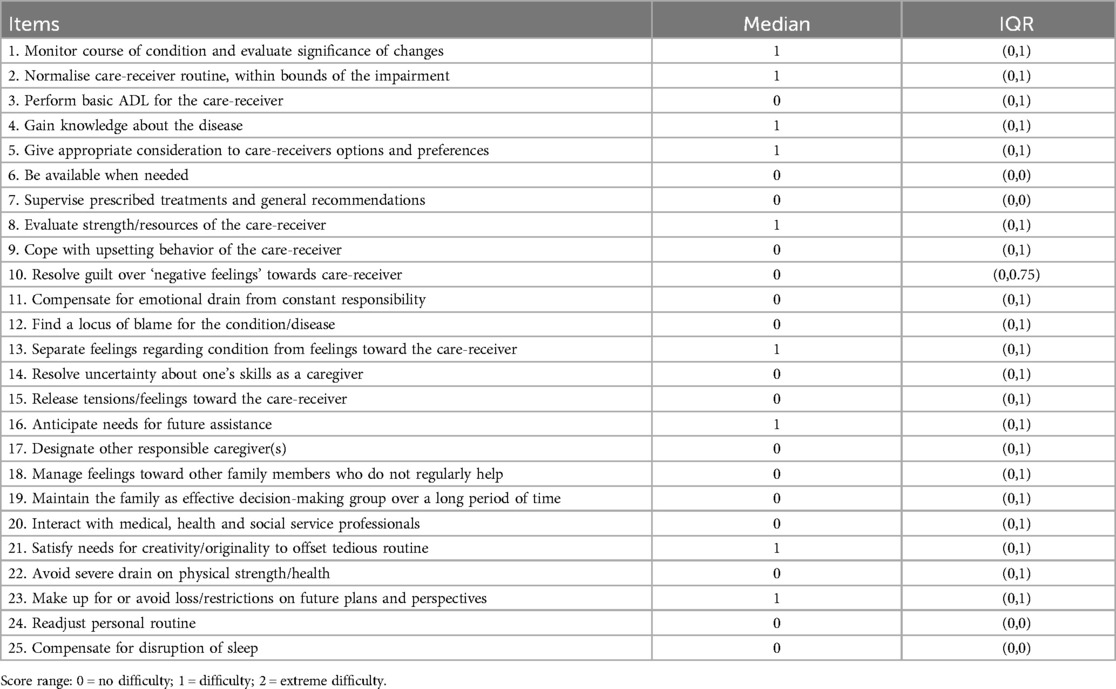
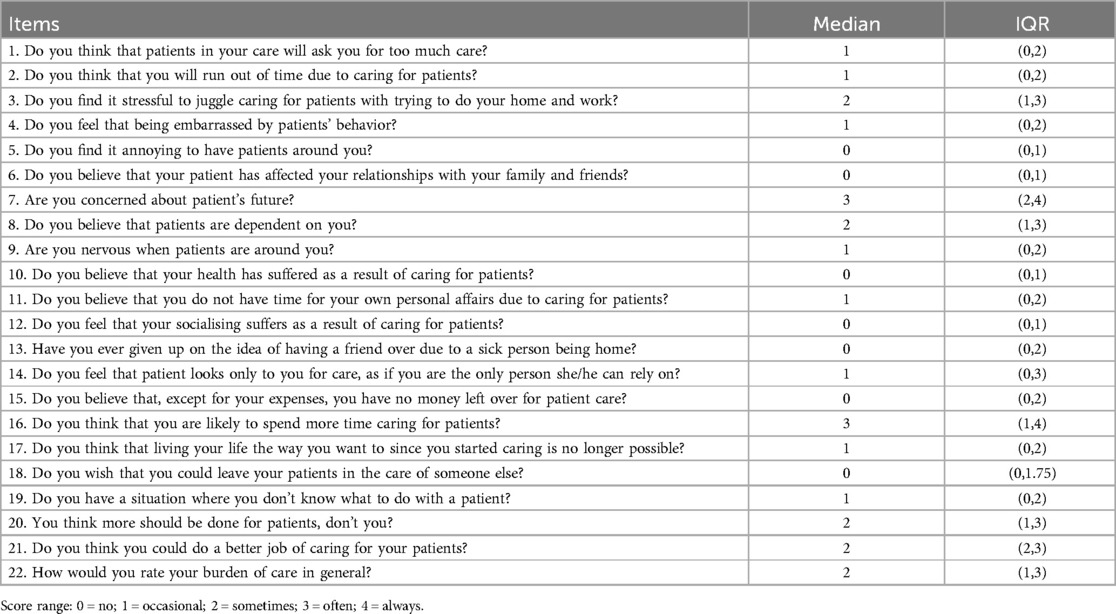
The Chinese version of Family Caregiver Task Inventory (FCTI), revised by Lee and Mok (24) of Hong Kong, was used in this study. It includes 25 items in 5 dimensions: (a) learning to cope with new role; (b) providing care according to care-receiver's needs; (c) managing own emotional needs; (d) appraising supportive resources; and (e) balancing caregiving needs and one's own needs. A 3-point Likert scale was used, with a score of 0 indicating no difficulty, 1 indicating difficulty, and 2 indicating extreme difficulty, for a total score of 0–50, with higher scores meaning poorer caregiving ability. Caregiving burden was measured using the Chinese version of the Zarit Caregiver Burden Interview (ZBI), which was localized by Wang Lie et al (25). It consisted of 22 entries in 2 dimensions: role burden and personal burden. A 5-point Likert scale was used (0 = no, 1 = occasional, 2 = sometimes, 3 = often, 4 = always) and a total score of 0–88, with higher scores indicating heavier caregiving burdens. Social Support Rate Scale (SSRS) was designed by Xiao in 1993 to reflect individual's level of social support (26). Questionnaire has 10 entries, including three dimensions: objective support, subjective support and utilization of social support. The total score ranges from 12 to 66, with higher scores indicating a better level of social support. Lower than 33 scores indicate a low level of social support, 33–45 scores show an average level, and higher than 45 scores indicate a good level of social support.
Qualitative data was collected using a semi-structured interview guide that included the following questions:
• How did you care for your child after she/he underwent surgery, including diet, skin, cast or brace, psychological, daily life, etc.?
• What difficulties or burdens have you faced in caring for your child after she/he received treatment?
• What were some of funny times you had while caring for your child after she/he received treatment?
• Please describe your caregiving abilities specifically.
Ethical considerations
The study was reviewed by the Ethics Committee of the Shanghai Children's Hospital under approval number 2023R066-E01. We assured that their treatment would not be affected if they refused to participate in this study. No identifying information was collected from the study subjects during research process and the privacy of their beliefs and opinions was ensured. In addition, we encrypted the data so that only researchers could access that.
Data analysis
SPSS 25.0 was used for statistical analysis. The Shapiro–Wilk test was used to assess the normality of the data, which showed an approximately normal distribution (P > 0.05). Total caregiving ability and caregiving burden scores were calculated by recording items under each scale and then summing scores. Qualitative data was analyzed using thematic analysis, including data familiarization and transcription, initial coding, thematic search, thematic review, thematic definition and naming, and thematic finalization (27). Finally, a joint presentation table was developed by integrating quantitative and qualitative information, identifying similar and dissimilar results. Data was combined by comparing the information to select confirming, disconfirming, or expanding results (23).
Rigor/validity and reliability
To ensure the reliability of interview outlines, detailed discussions were held between researchers and initial testing was conducted with two family caregivers. Interviews were transcribed by researchers and check against audio recordings. Codes and themes were developed separately by two researchers and then compared and modified. Themes and transcripts were reviewed and compared by another neutral person.
FCTI is a valid and reliable scale with a Cronbach's alpha of 0.844, which was developed by Clark and Rakowski. ZBI scale was developed by Zarit et al. with a Cronbach's alpha of 0.733. Both two scales have good structural, content and face validity.
Results
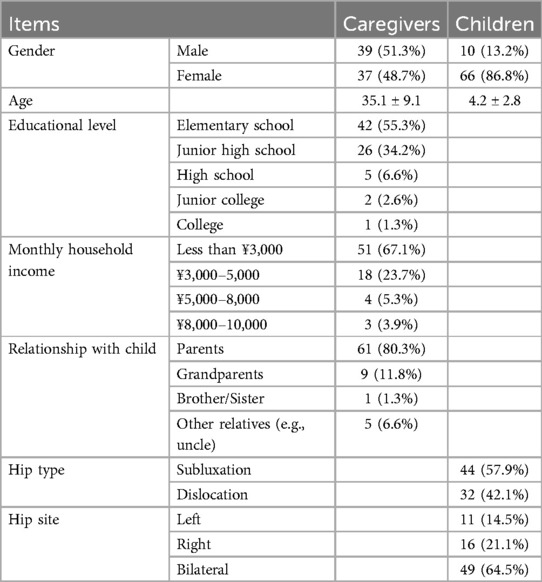
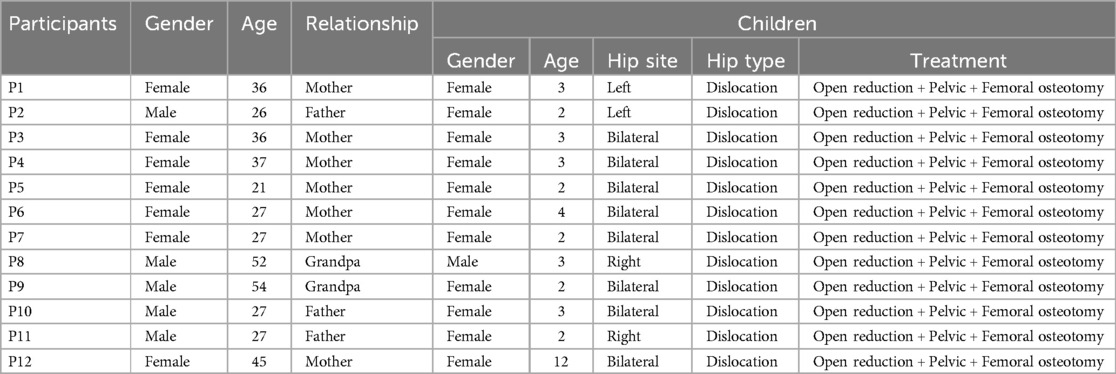
In the quantitative study, 76 family caregivers consisted 39 (51.3%) males and 37 (48.7%) females, with range of 21–60 years. 66 of children were female (86.8%) and 10 (13.2%) were male. Details can be seen in Table 1. In the qualitative interviews, 7 participants were females and 5 were males, aged between 21 and 54 years (Table 2).
Quantitative findings
Total score of FCTI and SSRS was (13.04 ± 7.16) and (45.13 ± 6.86), separately. Total score of ZBI was (29.87 ± 11.25), with role burden dimension score was (6.57 ± 3.30) and personal burden dimension score was (17.48 ± 5.88). When analyzing FCTI scores of each entry, we found that 55 (72.4%) chose “difficulty/extreme difficulty” for entry 5, “Give appropriate consideration to care-receiver's options and preferences”. Entry 7, “Supervise prescribed treatments and general recommendations” was selected as “no difficulty” by 61 person (80.3%). In analyzing scores for each entry of ZBI, it was found entry 7, “Are you worried about patient's future, in any way?” had the highest score, with majority of caregivers (81.6%) choosing “sometimes/often/always”. Entry 10, “Do you feel your health has suffered as a result of caring for the patient” was the lowest scoring, with 48 (63.1%) choosing “no” impact (Tables 3, 4).
Results of Pearson correlation analysis suggested that scores of FCTI were positively associated with scores of ZBI (r = 0.512, P < 0.01) and negatively correlated with scores of SSRS (r = −0.309, P < 0.01). However, higher scores of FCTI indicated poor caring capacity. This implied that the poorer caregiving ability of family caregivers, the more severe caregiving burden. Moreover, the higher level of social support, the poorer caregiving ability (Table 5).
Qualitative findings
Different emotions at different stages
Based on the analysis of qualitative data the following two themes emerged.
Initial worry
Many family members showed obvious anxiety and concern when they first learned of their child's illness, wondering if doctor had misdiagnosed. Others were puzzled and curious as to the cause of disease. For example, two family caregivers mentioned:
P4(female, age 37): I thought it was impossible when doctor told me that she had some problems with her hip joint, she’s been fine since birth. None of the other children in our family have had this situation, so I don’t understand. I was always anxious.
P9(male, age 54): My child had some problems with his walking posture, but I didn’t pay attention to it. The test result was hip dislocation, what was it? I’ve never heard of it before. What caused it? I was very worried!
Backend trust
Most of the interviewees were parents of children, who were receptive and their mood changed significantly after the diagnosis from initial worry and doubt to trust and support. For example, three family caregivers said:
P6(female, age 27): At first, our family members were very anxious when we knew she was sick. Then we heard from doctors in Shanghai that the treatment technology for this disease was very mature, so we trust them. Doctors in Shanghai are very good!
P10(male, age 27): This was the second time to Shanghai, the first time (surgery) we did the left side and this time we would do the right side. The doctor in Shanghai put me at ease (thumbs up).
P11(male, age 27): The medical conditions in our hometown were limited. Last year, Danzeng’s daughter also came to Shanghai for surgery. After surgery, her walking posture improved a lot, so I brought my daughter here this year…… No matter what kind of examination and treatment, I would cooperate, and I just hoped that my child could walk like a normal child in the future.
Caregiving process overwhelmed
Based on the analysis of qualitative data the following two themes emerged.
Role conflict
Interviewees in this study were adults, mostly parents of affected children, who, in addition to the responsibility of caring, also had social roles, such as those in workplace. For example, two family caregivers mentioned:
P2(male, age 26): I have already resigned from my job when I took my child to Shanghai for medical treatment. There were two elderly people in my family who were in poor health, and I was the only one who took care of them.
P5(female, age 21): I didn’t expect this to happen to my child. It’s a big expense, and my job wasn’t going well.
Lack of caregiving capacity
Developmental hip dislocation is a special disease, and caregiving involves plaster care, dietary guidance, rehabilitation exercises, life care, and other aspects. Caregivers need to have a wealth relevant knowledge and caregiving skills to cope with various emergencies that arise in children. The educational level of interviewees in this study was generally low, and 10(83.3%) of family members talked about how they felt overwhelmed by the caregiving process and lacked energy to take care of their children because of their own lack of ability. For example, two family caregivers said:
P1(female, age 26): The most troublesome part of caring for a child was changing her nappy. Because she was been wearing a cast since her surgery, my hands were full every time when I changed her nappy.
P8(male, age 52): I am his grandfather and had never attended to school. Nurse told me how to exercise his lower limbs, but I couldn’t understand. I dared not move his legs casually, so he had hardly exercised.
Insufficient information
Based on the analysis of qualitative data the following two themes emerged.
Disease-specific information
Caregivers had limited access to disease knowledge, there was a lack of evidence about the source and authenticity of information which they obtained from Internet. Moreover, the complexity of information on the Internet could easily mislead families, even delayed treatment of child. In addition, due to regional language differences, some family members need to go through an interpreter to communicate with healthcare workers, and there may be some communication errors. For example, two family caregivers said:
P3(female, age 36): A year ago, my child walked like a duckling, and the examination results indicated a hip joint issue. We learned from Baidu that this condition didn’t require surgery, so our family didn’t take it seriously. However, this year, when doctors in Shanghai re-examined, they informed us that surgery was necessary. Consequently, we traveled to Shanghai with the medical team.
P12(female, age 45): I can’t speak Mandarin, so I didn’t understand what doctors and nurses were saying. Although there was a translator, it was very inconvenient for us to communicate. It would be great if there were a specialized introduction in Tibetan about disease.
Actual care information
Many family caregivers mentioned that they had difficulties in caring for postoperative children and were eager to obtain more information about home care from medical staff, such as daily life care, plaster care, psychological care, and other aspects. For example, three family caregivers mentioned:
P6(female, age 27): At hospital, there were many nurses to assist us. But what should we do when we go home? Whenever I tried to turn her over, she cried out in pain, which made me hesitate to move her……The weather was hot now, and since she was wearing a cast, it was not easy for me to give her a bath. Today, she even wet the cast during urination. I am not sure if this will have any adverse effects. There were just so many issues.
P7(female, age 27): After the surgery, she kept crying. Today, she even got angry with me, complaining of leg pain and discomfort, and refused to eat. Oh, I was exhausted by her.
P11(male, age 27): This was the only child in our family, we were usually quite precious. It was very hard for me to see her in pain. I wanted to hold her but I was afraid to do that because of the cast, so we parents were at s loss as to what to do. I wish doctors and nurses could tell us what to do, but you were usually very busy and I was too embarrassed to ask some questions.
Social support
Economic status is an important influence on the burden of care for caregivers of children with DDH. However, Shanghai Children's Hospital and People's Hospital of Shigatse, Tibet, jointly launched a public assistance program, “Love of Gesang Flower”, in 2014 to support some of children with DDH for surgical treatment. The program alleviated economic pressure on some families and contributed to logistical support work for caregivers. Eight (66.7%) of caregivers interviewed expressed their recognition of the program. For example, two family caregivers mentioned:
P4(female, age 37): This program was fantastic! My family’s financial situation wasn’t good, and initially, I was deeply concerned about the high cost of surgery. Now, with the support of this project, I did not have to worry about money. I was deeply grateful to Shanghai Children’s Hospital.
P5(female, age 21): Shanghai boasted excellent policies, skilled doctors, and a good service attitude, making it an excellent place in every aspect.
Mixed methods findings
Themes derived from qualitative findings were compared and merged with quantitative findings, including level of caregiving competence of family caregivers, perceptions of caregiving process, and burdens incurred while caring. The findings were confirmed and extended by comparing and merging the data.
Five themes: initial worry, backend trust, role conflict, insufficient disease-specific information and social support confirmed the quantitative findings. The themes of lack of caregiving capacity and insufficient actual care information provided an expansion of the quantitative findings. In the survey, caregivers of children with DDH in Tibet showed a low level of caregiving capacity with scores of (13.04 ± 7.16) and moderate level of caregiving burden with scores of (29.87 ± 11.25). Due to long cycle of care for DDH, a greater burden of care was more likely to arise when there was insufficient capacity for caregivers. Additionally, in response to lack of information about actual care, caregivers indicated that casts were a major deterrent to their ability to perform a range of daily care tasks. But since casts needed to be worn for 2–3 months, this posed a great challenge in caring (Table 6).
Discussion
Shanghai Children's Hospital creates a comprehensive treatment and living environment for caregivers. Firstly, medical staff placed them in the same ward, making it easier for caregivers to communicate with each other about illness and points of caring. For caregivers who cannot communicate in Mandarin, this arrangement also facilitates centralized translation by interpreters and improves work efficiency. Secondly, hospital provides caregivers with basic hospitalization necessities such as beds, quilts, meals, and daily necessities, which greatly reduces burden of caregivers' life, so that they do not have to worry about basic life and can concentrate on receiving treatment. Thirdly, hospital also arranges special cars and nursing staff to pick up and drop off children and their caregivers at designated train station to ensure their safety as much as possible.
This mixed-method study utilized quantitative and qualitative methods to a comprehensive understanding of caring burden and experiences of family caregivers of children with DDH in Tibet, China. This provided greater insight than that gained by using either type of data in isolation, as quantitative method allowed for a greater degree of statistical generalization, while qualitative method provided deeper insight and a more nuanced view of phenomenon (23). Quantitative analysis of standardized questionnaires was used to determine status of caregiving burden and caregiving capacity of family caregivers of children with DDH, and qualitative analysis of semi-structured interviews was used to better understanding of caregiving experiences. Mixed-methods analyses were conducted to assess degree of agreement and disagreement between quantitative and qualitative results.
Caregiver capacity is ability of caregiver to effectively meet physical, emotional, and social needs of patients while maintaining their own health (28). This capacity includes knowledge, skills, resources and support systems available to caregivers. Findings from this study of FCTI showed that caregiving capacity was at a low level. Entries 1, 2, 5, 8 and 13 were the most difficult things for family caregivers to do with children. Of these, entries 1, 2, 5 belong to “Learning to cope with new role” dimension, entry 8 to “Providing care according to care-receiver's needs” dimension, and entry 13 to “Managing own emotional needs” dimension. These were in convergence with the findings of in-depth interviews. They reported not being able to adjust one's personal roles well enough to move from a work role to a caregiver role. In 1995, a scholar first introduced the concept of family caregiver role acquisition, which was a specific type of role transition occurring in families in response to changes in health (29). Some researchers showed family caregivers had low level of caregiving preparedness at discharge, which led to high caregiving burden in later weeks following discharge (30, 31). Adverse emotions such as distress and depression occurred during role transition (31). These results were congruent with some studies in the literature (20, 22, 32).
Caregiver burden is defined as the distressed results from providing care (33). Suffering from a reduction in free time and a lack of rest because of the influence of surgery tasks, caregivers are likely to feel burdened. Family caregivers’ burden was at a moderate level in this research. Entries 3, 7, 8, 16, 20, 21 were the ones that families found most burdensome to care for. Qualitative interview themes expanded on the findings of this part of the quantitative study, with caregivers indicating that burden was primarily caused by a lack of caregiving capacity. Due to lack of knowledge about disease, wearing a cast after surgery hindered all aspects of daily life care, including continence care, skin cleaning, and exercise. The average time for postoperative children to wear plaster is 8 weeks, during which lower limb functional exercise is required. However, due to distance and language issues, the effectiveness of functional exercise cannot be effectively evaluated. The uptake in caregiver burden in post-discharge has significant implications for patient's outcomes, such as symptom management, recovery, hospital re-admission, and caregivers’ health and well-being (30). It had been suggested that a structured education and training program for caregivers improved pre-discharge preparation, reduced caregiver's burden, and led to better outcomes for children (34). Extensive evidence suggested that caregiving burden was associated with mental and physical health problems (35–37). Strategies such as peer mentoring and peer support groups can also improve preparation, mental health and ability to handle stress of caregiving (38).
In addition, correlation analyses in quantitative study indicated that caregiving capacity was positively associated with caregiving burden and negatively correlated with social support. Some researchers suggested that social support mediated the relationship between caregiving capacity and caregiving burden (39). Previous researchers have demonstrated that social support is strongly associated with caregiver burden (40). Caregiving can be a lonely and demanding role, and social support is vital to mitigate the negative effects of caregiver burden (41). When caregivers felt socially supported-whether through family, friends, or community resources-they were more likely to develop resilience to cope with challenges of caregiving (42). Moreover, enhancing level of social support through some interventions (support groups or community resources) can significantly improve overall quality of life of caregivers. By meeting emotional and practical needs of caregivers, their burden can be reduced and their ability to care increased (43). Thus, it followed that role of strengthening the level of social support is crucial in development of family caregiving strategies. The children in this study benefited from the “Love of Gesang Flower” public welfare program, which paid for all costs of children's families, including surgical fees, transportation, and living expenses, which greatly reduced financial burden on their family. In addition, the program trained and taught community healthcare workers in Shigatse through courses on “Early screening, diagnosis and treatment of DDH”, teaching workshops, and on-site instruction in hip ultrasound and surgical skills. These initiatives help residents better understand the causes, clinical manifestations and treatment of DDH.
This study is part of the construction of a home care program for children with DDH in Tibet. Research was targeted and directed to caregivers of children with DDH in the highlands, and presented caregiving ability and burden levels using a convergent mixed-methods research, which enriched findings in the field of DDH nursing. Results were analyzed from caregivers’ perspective and study methodology was reproducible, which were useful and informative in other countries and regions. Comparing quantitative and qualitative data can improve our understanding of caring experiences of family caregivers in Tibet, China. Based on these findings, it is recommended that requirements for postoperative home care for children with DDH in Tibet deserves attention and measures should be taken to alleviate caregivers’ burden. Healthcare professionals should develop a targeted home care management program so that families can fully understand various care measures after discharge, including daily care, plaster care, skin care, continence care and so on. Internationally, more research is needed to identify strategies for reducing caring burden against family caregivers of children with DDH. With continuous development and improvement of AI technology, intelligent remote mutual medical model will be more conducive to the communication and exchange between healthcare professionals and children at a distance. Therefore, future research may need to be conducted in conjunction with AI to reflect the characteristics of the times.
Limitations
Purposive sampling was used for quantitative portion of this study, a method that may limit generalization to other similar populations. Insufficient sample size and single source of subjects affected credibility of study. In addition, as a non-intervention study, we were unable to recommend causality of the phenomenon from findings. Therefore, sample size should be increased and multicenter studies should be conducted in the future.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
YL: Writing – original draft, Writing – review & editing. JY: Formal analysis, Investigation, Supervision, Writing – review & editing. SWen: Data curation, Investigation, Methodology, Supervision, Writing – review & editing. SWei: Data curation, Methodology, Supervision, Writing – review & editing. XQ: Conceptualization, Data curation, Investigation, Writing – review & editing. FL: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Shanghai Jiao Tong University School of Medicine: Nursing Development Program (SJTUHLXK2023); Shanghai Jiao Tong University School of Medicine: Nursing Key Project (Jyhz2311); Shanghai Children’s Hospital hospital projects: Nursing Program (2023HLZX02); High-level local university construction project founded by Shanghai Municipal Education Commission (2023GJJD).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ömeroğlu H, Yüksel S, Demir P, Alexiev V, Alsiddiky A, Anticevic D, et al. An Eastern Europe and Middle East multinational expert delphi consensus study on the prevention, diagnosis, and treatment of developmental dysplasia of the hip before walking age. Int Orthop. (2024) 48(6):1373–80. doi: 10.1007/s00264-023-06077-1
2. Ding LJ, Liu YL, Ma G, Jia YQ, Wei YSH, Liu XM. Correlation of acetabular chondrocyte apoptosis with caspase-3 and bcl-2 expression in developmental dislocations of the hip. Genet Mol Res. (2016) 15(3). doi: 10.4238/gmr.15036809
3. Asturias A, Kiani S, Sadjadi R, Swarup I. The treatment of hip dysplasia in adolescent patients. Curr Rev Musculoskelet Med. (2025). doi: 10.1007/s12178-025-09953-y
4. Bracken J, Tran T, Ditchfield M. Developmental dysplasia of the hip: controversies and current concepts. J Paediatr Child Health. (2012) 48(11):963–72. 972–973. doi: 10.1111/j.1440-1754.2012.02601.x
5. Ulziibat M, Munkhuu B, Bataa AE, Schmid R, Baumann T, Essig S. Traditional Mongolian swaddling and developmental dysplasia of the hip: a randomized controlled trial. BMC Pediatr. (2021) 21(1):450. doi: 10.1186/s12887-021-02910-x
6. Skirving AP, Sims TJ, Bailey AJ. Congenital dislocation of the hip: a possible inborn error of collagen metabolism. J Inherit Metab Dis. (1984) 7(1):27–31. doi: 10.1007/BF01805617
7. Bradley C, Verma Y, Maddock CL, Wedge JH, Gargan MF, Kelley SP. A comprehensive nonoperative treatment protocol for developmental dysplasia of the hip in infants. Bone Joint J. (2023) 105-B(8):935–42. doi: 10.1302/0301-620X.105B8.BJJ-2023-0149.R1
8. Johnson MD, Kuschel C, Donnan L. Neonatal clinical examination and selective ultrasound screening are not reliable for the early diagnosis of hip dysplasia: a retrospective cohort study. J Paediatr Child Health. (2023) 59(10):1146–51. doi: 10.1111/jpc.16472
9. Osawa Y, Hasegawa Y, Seki T. Long-term outcomes of eccentric rotational acetabular osteotomy combined with femoral osteotomy for hip dysplasia. J Arthroplasty. (2020) 35(1):17–22. doi: 10.1016/j.arth.2019.07.041
10. Edelstein AI, Duncan ST, Akers S, Pashos G, Schoenecker PL, Clohisy JC. Complications associated with combined surgical hip dislocation and periacetabular osteotomy for complex hip deformities. J Hip Preserv Surg. (2019) 6(2):117–23. doi: 10.1093/jhps/hnz014
11. Schaeffer EK, Study GI, Mulpuri K. Developmental dysplasia of the hip: addressing evidence gaps with a multicentre prospective international study. Med J Aust. (2018) 208(8):359–64. doi: 10.5694/mja18.00154
12. Tanzhu L, Xiaodong Y, Xiang F, Xiaolian M. The clinical research of children’s prevalence of the developmental dysplasia of the hip in Xigaze of Tibetan. Orthop Biomech Mater Clin Study. (2016) 13(01):38–40. doi: 10.3969/j.issn.1672-5972.2016.01.012
13. Harris MD, Thapa S, Lieberman EG, Pascual-Garrido C, Abu-Amer W, Nepple JJ, et al. Identifying risk factors for disease progression in developmental dysplasia of the hip using a contralateral hip model. J Bone Joint Surg Am. (2024) 106(24):2322–9. doi: 10.2106/JBJS.24.00308
14. Ulziibat M, Munkhuu B, Schmid R, Baumann T, Essig S. Implementation of a nationwide universal ultrasound screening programme for developmental dysplasia of the neonatal hip in Mongolia. J Child Orthop. (2020) 14(4):273–80. doi: 10.1302/1863-2548.14.200029
15. Barrera CA, Cohen SA, Sankar WN, Ho-Fung VM, Sze RW, Nguyen JC. Imaging of developmental dysplasia of the hip: ultrasound, radiography and magnetic resonance imaging. Pediatr Radiol. (2019) 49(12):1652–68. doi: 10.1007/s00247-019-04504-3
16. Wen J, Ping H, Kong X, Chai W. Developmental dysplasia of the hip: a systematic review of susceptibility genes and epigenetics. Gene. (2023) 853:147067. doi: 10.1016/j.gene.2022.147067
17. Mahapatra SK, Hampannavar A, Choudhury S, Gourineni V, Sahu B, Rout J. Impact of avascular necrosis on outcomes in the management of developmental dysplasia of hip: a systematic review. Acta Orthop Belg. (2024) 90(3):535–42. doi: 10.52628/90.3.12274
18. Smart L, Cundy W, Williams N, Arnold A, Childs J, Pelentsov L, et al. Screening accuracy for developmental dysplasia of the hip by child health nurses. Children (Basel). (2024) 11(8):915. doi: 10.3390/children11080915
19. Yue Y, Guo J, Huang Y, Li W, Xue R, Li H, et al. Efficacy of post-surgery family-based participatory cluster pain care in children with developmental dislocation of hip. Technol Health Care. (2024) 32(5):2883–91. doi: 10.3233/THC-230879
20. Harry A, Johnston C, Twomey S, Wakely L. A survey of parents’ and carers’ perceptions of parenting a child with developmental dysplasia of the hip. Pediatr Phys Ther. (2022) 34(3):328–33. doi: 10.1097/PEP.0000000000000917
21. Grzybowski G, Bliven E, Wu L, Schaeffer EK, Gibbard M, Zomar BO, et al. Caregiver experiences using orthotic treatment options for developmental dysplasia of the hip in children. J Pediatr Orthop. (2023) 43(2):105–10. doi: 10.1097/BPO.0000000000002312
22. Gibbard M, Zivkovic I, Jivraj B, Schaeffer E, Robillard JM, Mulpuri K, et al. A global survey of patient and caregiver experiences throughout care for developmental dysplasia of the hip. J Pediatr Orthop. (2021) 41(6):e392–7. doi: 10.1097/BPO.0000000000001813
23. Robinson P. Designing and conducting mixed methods research. Aust N Z J Public Health. (2007) 31:388. doi: 10.1111/j.1753-6405.2007.00096.x
24. Lee RL, Mok ES. Evaluation of the psychometric properties of a modified Chinese version of the caregiver task inventory–refinement and psychometric testing of the Chinese caregiver task inventory: a confirmatory factor analysis. J Clin Nurs. (2011) 20(23–24):3452–62. doi: 10.1111/j.1365-2702.2011.03729.x
25. Lie W, Xiaoshi Y, Zhe H, Qiaolian F, Yinger WJ. Application and evaluation of Chinese version of zarit caregiver burden interview. Chin J Public Health. (2006) 08:970–2. doi: 10.11847/zgggws2006-22-08-47
26. Xiao S. Theoretical basis and research applications of social support rate scale. Lin Chuang Jing Shen Yi Xue Za Zhi. (1994) 02:98–100.
27. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
28. Frasco MA, Duffy EL, Trish E. Acceptability of hospital-at-home care and capacity for caregiver burden. JAMA. (2024) 332(5):422–4. doi: 10.1001/jama.2024.10035
29. Schumacher KL. Family caregiver role acquisition: role-making through situated interaction. Sch Inq Nurs Pract. (1995) 9(3):211–26. 227–229. doi: 10.1891/0889-7182.9.3.211
30. Roslin H, Muliira JK, Lazarus ER, Jacob D, Al-Habsi W, Al-Musallami F. Caregiving preparedness and caregiver burden in omani family caregivers for patients with acquired brain injury. Sultan Qaboos Univ Med J. (2023) 23(4):493–501. doi: 10.18295/squmj.6.2023.040
31. Dionne-Odom JN, Azuero A, Taylor RA, Wells RD, Hendricks BA, Bechthold AC, et al. Resilience, preparedness, and distress among family caregivers of patients with advanced cancer. Support Care Cancer. (2021) 29(11):6913–20. doi: 10.1007/s00520-021-06265-y
32. Wakely L, Easey P, Leys J, Johnston C. Exploring the lived experience of parenting a child with developmental dysplasia of the hip. Phys Occup Ther Pediatr. (2021) 41(5):503–14. doi: 10.1080/01942638.2020.1867694
33. Rha SY, Park Y, Song SK, Lee CE, Lee J. Caregiving burden and the quality of life of family caregivers of cancer patients: the relationship and correlates. Eur J Oncol Nurs. (2015) 19(4):376–82. doi: 10.1016/j.ejon.2015.01.004
34. Driscoll R, Fitzpatrick L, Karsten J, Scott S, Winters E. Care partner carryover day: a formalized training program to improve care partner preparedness for patients with acquired brain injury prior to discharge home. Arch Phys Med Rehabil. (2021) 102(10):e52. doi: 10.1016/j.apmr.2021.07.620
35. Grubic N, Amarasekera S, Mantella L, Stall NM. Heart of the matter: the physical and mental health burden of caregiving for cardiovascular patients. Can J Cardiol. (2024) 40(3):351–4. doi: 10.1016/j.cjca.2023.11.033
36. Hebdon MCT, Xu J, Reblin M, Clayton MF, Mooney K, Ellington L. Balancing work and hospice caregiving-a closer Look at burden, preparedness, and mental health. J Pain Symptom Manage. (2022) 63(2):283–92. doi: 10.1016/j.jpainsymman.2021.08.003
37. Nasreen HE, Tyrrell M, Vikström S, Craftman Å, Syed Ahmad SAB, Zin NM, et al. Caregiver burden, mental health, quality of life and self-efficacy of family caregivers of persons with dementia in Malaysia: baseline results of a psychoeducational intervention study. BMC Geriatr. (2024) 24(1):656. doi: 10.1186/s12877-024-05221-9
38. Jones M, Holley C, Jacobs M, Batchelor R, Mangin A. Effects of peer mentoring for caregivers of patients with acquired brain injury: a preliminary investigation of efficacy. Arch Rehabil Res Clin Transl. (2021) 3(3):100149. doi: 10.1016/j.arrct.2021.100149
39. Xu Q, Ma J, Zhang Y, Gan J. Family resilience and social support as mediators of caregiver burden and capacity in stroke caregivers: a cross-sectional study. Front Psychol. (2024) 15:1435867. doi: 10.3389/fpsyg.2024.1435867
40. Zhang Y, Ding Y, Liu C, Li J, Wang Q, Li Y, et al. Relationships among perceived social support, family resilience, and caregiver burden in lung cancer families: a mediating model. Semin Oncol Nurs. (2023) 39(3):151356. doi: 10.1016/j.soncn.2022.151356
41. Muñoz-Bermejo L, Adsuar JC, Postigo-Mota S, Casado-Verdejo I, de Melo-Tavares CM, Garcia-Gordillo MÁ, et al. Relationship of perceived social support with mental health in older caregivers. Int J Environ Res Public Health. (2020) 17(11):3886. doi: 10.3390/ijerph17113886
42. Balvert SCE, Milders MV, Bosmans JE, Heymans MW, van Bommel S, Dröes RM, et al. The MOMANT study, a caregiver support programme with activities at home for people with dementia: a study protocol of a randomised controlled trial. BMC Geriatr. (2022) 22(1):295. doi: 10.1186/s12877-022-02930-x
Keywords: developmental dislocation of the hip, care capacity, care burden, social support, convergent mixed-methods
Citation: Lei Y, Yan J, Wenjuan S, Weili S, Qianyi X and Lingyan F (2025) Caregivers’ care experiences of children with developmental dislocation of the hip in Tibet, China: a convergent mixed-methods study. Front. Pediatr. 13:1561246. doi: 10.3389/fped.2025.1561246
Received: 14 February 2025; Accepted: 24 April 2025;
Published: 9 May 2025.
Edited by:
Stefan Essig, University of Lucerne, SwitzerlandReviewed by:
Claudia Maizen, Barts Health NHS Trust, United KingdomThomas Baumann, Independent Researcher, Solothurn, Switzerland
Copyright: © 2025 Lei, Yan, Wenjuan, Weili, Qianyi and Lingyan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fan Lingyan, ZmFubHlAc2hjaGlsZHJlbi5jb20uY24=
 Yang Lei
Yang Lei Jiang Yan
Jiang Yan