- 1Neonatal Intensive Care Unit, Institute of Child and Maternal Health, IRCSS Burlo Garofolo, Trieste, Italy
- 2Public Health Research Unit, Institute for Maternal and Child Health—IRCCS “Burlo Garofolo”, Trieste, Italy
- 3Community Medicine, University Hospital Giuliano Isontino, Gorizia, Italy
Objectives: the study aims to determine whether real-time ultrasound-guided umbilical venous catheter (UVC) insertion could enhance the accuracy of the procedure and reduce the number of x-ray, thereby minimizing radiation exposure of the newborn.
Methods: A pre-post study was conducted, comparing outcomes before and after the introduction of ultrasound during catheter placement. All included newborns required placement of the UVC. In the study population (interventional group) the catheter tip was visualized using both ultrasound and radiography, whereas in the in historical cohort (control group) the catheter tip was visualized solely through radiography. Exclusion criteria included hemodynamic instability, known vascular malformations and major congenital malformations.
Results: During the study period, 33 eligible neonates underwent tip navigation and were enrolled, all of whom had a centrally-placed UVC. Additionally, 36 newborns were retrospectively identified as control group. The median gestational ages were 34 weeks and 33 weeks respectively for the interventional and control group (p 0.74). The median birth weights were 2,087 (1,400–3,220) g and 1,966 (1,489–2,695) g respectively for the interventional and control group (p 0.67). The catheter was correctly positioned at first attempt in 29/33 (87%) patients with US guidance and 17/36 (47%) in the control group (p < 0.001). The mean numbers of x-rays taken were 1.1 and 1.8 respectively for the interventional and control group (p < 0.001). In the control group, the mean number of antero-posterior thoracoabdominal radiograph (TAR) ranged from 1 to 3 for each patient.
Conclusion: In conclusion, ultrasound could be the standard of care for umbilical catheter placement, ensuring accurate vessel assessment and real-time visualization. Despite our limited sample, our findings highlight its superior precision and safety, reducing complications and the need for radiography. Integrating ultrasound into daily neonatal practice can improve catheter placement and patient outcomes.
Introduction
The umbilical venous catheter (UVC) is the most commonly used venous access in Neonatal Intensive Care Unit (NICU) and can be placed in premature infants or full-term infants. It is crucial in managing both critical and non-critical patients for the administration of parenteral nutrition, hypertonic solutions, medications, transfusions, and for providing emergency venous access. The placement of a UVC is a procedure performed by adequately trained personnel, and it is essential to confirm its correct placement to avoid serious complications and administer infusions with higher osmolarity. Common complications include cardiac arrhythmias, thrombosis, myocardial perforation, pericardial effusion, or tamponade if the tip is intracardiac. Alternatively, the presence of the UVC in the portal vein can cause thrombosis, portal hypertension, or hepatic necrosis (1).
Typically, the UVC is inserted to a predetermined length from the umbilicus and tip position is then assessed by antero-posterior thoracoabdominal radiograph (TAR). If the catheter is not correctly placed, it must be repositioned and checked again with x-rays involving additional handling of the central line and of the neonate, radiation exposure, and treatment delays. Various methods to calculate the UVC insertion length have been studied, including Dunn's shoulder umbilical length graph (2) and Shukla's formula based on birth weight (3). However, Lean et al. (4) demonstrated that, even when the best formula is used, almost half of umbilical venous catheters inserted may require manipulation to achieve a safe position.
The ideal UVC tip position to minimize complications is outside the heart, at the junction of inferior vena cava (IVC) and right atrium (RA). However, this is not easily translated into a well defined radiological landmark. Traditionally, UVC tip position is evaluated in relation to vertebral bodies, cardiac silhouette and diaphragm. The catheter should be at the diaphragm level or slightly above or between the vertebral bodies T8 and T9 (5) or at the cavo-atrial junction obtained by extrapolating the curve of the RA medial border up to its intersection with the IVC or with the right border of the vertebral bodies (6).
Furthermore, radiography exposes the patient to radiation, even multiple times in case of repositioning, and requires the use of multiple resources (radiology technician, radiologist) that are not always readily available. Conversely, echocardiography allows direct visualization of the cavo-atrial junction, making this technique superior to chest radiography in determining the position of the UVC tip. Moreover, real-time ultrasound use during umbilical vein catheterization is a promising technique for rapid and precise catheter placement (7–10). Compared to traditional methods, ultrasound significantly reduces malpositioning, complications, and the need for repositioning attempts. Additionally, it enhances the effectiveness of facilitation maneuvers ensuring optimal placement (11). Ultrasound for tip navigation, therefore, due to its rapid execution, non-invasiveness, and accuracy, is a technique rapidly spreading within our Neonatal Intensive Care Units (12). There is increasing literature highlighting the qualities of this method, which, among other things, requires operators with simple basic training.
Our study aims to verify if real-time ultrasound-guided UVC insertion could increase the accuracy of the procedure itself and limit the number of x-rays, thus reducing the radiation exposure of the newborn.
Methods
This is a pre-post study conducted in IRCCS Burlo Garofolo, Italy, before and after the introduction of ultrasound during catheter placement. The study protocol was approved by the Bioethical Committee.
The study population (interventional group) included infants born between October 2019 and September 2020 who required placement of the umbilical venous catheter for therapeutic reasons. In the Interventional group, the catheter tip was visualized both with ultrasound and radiography.
Our historical cohort (control group) included all neonates born at our tertiary-level hospital, Institute for Maternal and Child Health IRCCS Burlo Garofolo of Trieste, Italy, between February 2018 and March 2019 who required placement of the umbilical venous catheter for therapeutic reasons. In the control group, the catheter tip was visualized only with radiography.
All the newborns admitted to our NICU were enrolled after obtaining informed written consent from parents. Exclusion criteria included hemodynamic instability, known vascular malformations and major congenital malformations.
Umbilical catheters were inserted under sterile conditions by the clinical team (neonatologists and neonatal fellows), with their length predetermined using Shukla's formula or Dunn's graph based on shoulder-umbilicus length, while the gauge was selected according to the patient's weight. In critically ill neonates requiring multiple incompatible therapies, a double-lumen catheter was chosen; otherwise, a single-lumen catheter was placed.
Ultrasound scans were performed by trained neonatologists using a Logiq E9 Ultrasound Unit (GE Healthcare) equipped with S4–10 microconvex. The US operator stayed by the bedside and put the probe under the sterile field either immediately after initial catheter insertion or later, when the predefined depth was almost reached without feeling any resistance, indicating a good chance of having bypassed the ductus venosus. In order to visualize the pathway of the catheter and especially the junction between IVC and RA, scans were performed through a subcostal view. When necessary, a small volume of saline was injected so that turbulence could better identify the catheter tip. The neonatologists who performed the ultrasound scans underwent training in pediatric cardiology to learn the correct ultrasound window for visualizing the atriocaval junction. Subsequently, in the NICU, they performed over 15 scans on different patients with an umbilical venous catheter to assess the correct positioning of the tip. Throughout the study, the trained neonatologists were supervised by an experienced neonatologist in echocardiography, who confirmed the correct catheter placement.
Iconographic documentation (photography or video) was recorded for each patient.
Once the position was considered optimal, the catheter was secured and TAR taken.
The primary outcome was the difference in the rate of success of correct UVC placement at first attempt (defined as correct placement after the first x-ray, with no need of repositioning) between the two groups. Newborn with low-lying UVC were excluded from the analysis.
The secondary outcome was the difference in the number of radiographs obtained in the two groups.
Categorical variables are presented as numbers and percentages, and continuous variables as medians and interquartile ranges (IQR), given the non-normal distribution of data. Differences between groups were evaluated with the Chi-square test (or Fisher's exact test when appropriate) for categorical variables and with the Mann–Whitney test for continuous variables since a non-normal distribution of data was found both visually and with the Kolmogorov–Smirnov test. Differences with p-value <0.05 were considered statistically significant. The sample size was predetermined. Preliminary data showed in the control population a first-attempt success rate (primary outcome of the study) of 30%. Assuming in the intervention group a first-attempt success rate of 70%, it was estimated the enrollment of 30 subjects per group to conduct the study (60 in all), setting alpha at 0.05% and beta at 0.20.
Results
During the study period, among the neonates who underwent tip navigation 33 were enrolled and all of them had a centrally-placed UVC. 36 newborns were retrospectively identified as Control group.
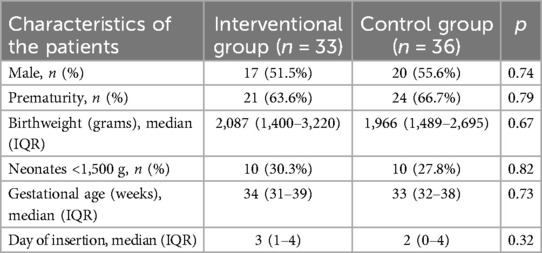
The median gestational ages were 34 weeks and 33 weeks respectively for the interventional and control group (p 0.74). The median birth weights were 2,087 (1,400–3,220) g and 1,966 (1,489–2,695) g respectively for the interventional and control group (p 0.67). Table 1 shows the baseline characteristics of the patients in the 2 groups (Table 1).
The catheter was correctly positioned at first attempt in 29/33 (87%) patients with US guidance and 17/36 (47%) in the control group (p < 0.001). Figure 1 shows a representative ultrasound image of a correctly placed catheter. In the US group, in the 4 neonates where the CVO was not visualized, the ultrasound window was not adequate due to pulmonary barrier or excessive gastric bubble. The mean numbers of x-rays taken were 1.1 and 1.8 respectively for the interventional and control group (p < 0.001). In the control group, the mean number of TAR ranged from 1 to 3 for each patient.
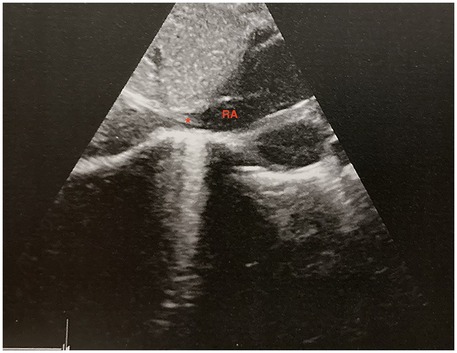
Figure 1. Ultrasound image of the correct placement of the umbilical venous catheter during a saline solution flush. RA, right atrium. * Catheter's tip.
Discussion
US-guided UVC placement improves the success rate of the procedure, defined as correct catheter tip placement, reduces the number of catheter manipulations, and decreases the number of radiographs required.
Proper catheter placement is crucial in an emergency setting such as in a NICU because it ensures safe vascular access during emergencies and allows the administration of life-saving therapies. If the catheter is properly positioned, it prevents the onset of complications such as cardiac arrhythmias, thrombosis, myocardial perforation, pericardial effusion, and tamponade (1). Several studies demonstrated that ultrasound enables faster and more accurate catheter placement (1, 13, 14) than radiography. Fleming et al. highlighted that using US-guided UVC placement saves of over an hour of time for the procedure. This result is extremely important when considering NICU patients who are at risk of severe hypoglycaemia and early sepsis. Having rapid and secure vascular access allows for the prompt administration of parenteral nutrition and antibiotics.
The speed of the sonographic technique is attributed to the reduced involvement of resources (radiology technicians, radiologists, computer systems, machinery). For the same reason, this technique also proves to be less costly (15).
Another benefit of US-guided UVC placement is the reduction in catheter manipulations, as confirmed by Fleming. Each catheter manipulation increases the risk of trauma, infection, and thrombosis (13, 11). Reducing manipulations also decreases the need for repeat radiographs and, consequently, radiation exposure. In our study, ultrasound reduced the use of radiographs by 40% (p < 0.001), despite our protocol stipulating that radiographs be performed in all patients in the interventional group. Other studies with smaller sample sizes than ours have also confirmed this result (1, 13, 14).
The limitations of our study are the study design and the sample size. We opted for a pre-post study design because, when the ultrasound machine was introduced in the department, it was preferred to also maintain radiographic control, as the staff was more confident with radiographic interpretation. The sample size was limited but it was calculated before conducting the study to ensure statistically significant; moreover, in the literature, studies rarely present numbers larger than ours.
In conclusion, ultrasound guidance enables accurate vessel assessment and real-time catheter visualization (16). Its routine application improves precision, decreases complications, and reduces reliance on radiography, which should be reserved for cases where ultrasound alone proves insufficient. Although our study was conducted on a limited sample, with a low representation of extremely low birth weight preterm neonates, our findings highlight the superior sensitivity, effectiveness, and safety of ultrasound in the general neonatal population. Further studies specifically targeting ELBW infants are needed to confirm the safety and feasibility of ultrasound-guided UVC placement in this particularly fragile group. Integrating ultrasound into daily neonatal practice can significantly improve catheter placement and overall patient outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institute for Maternal and Child Health—IRCCS "Burlo Garofolo". The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
FC: Conceptualization, Data curation, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. FG: Data curation, Writing – review & editing. LR: Formal analysis, Writing – review & editing. LT: Conceptualization, Supervision, Validation, Writing – review & editing. CB: Conceptualization, Data curation, Writing – original draft. AT: Conceptualization, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Italian Ministry of Health, through the contribution given to the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste—Italy.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rubortone SA, Costa S, Perri A, D’Andrea V, Vento G, Barone G. Real-time ultrasound for tip location of umbilical venous catheter in neonates: a pre/post intervention study. Ital J Pediatr. (2021) 47(1):68. doi: 10.1186/s13052-021-01014-7
2. Dunn PM. Localization of the umbilical catheter by post-mortem measurement. Arch Dis Child. (1966) 41(215):69–75. doi: 10.1136/adc.41.215.69
3. Shukla H. Rapid estimation of insertional length of umbilical catheters in newborns. Arch Pediatr Adolesc Med. (1986) 140(8):786. doi: 10.1001/archpedi.1986.02140220068034
4. Lean WL, Dawson JA, Davis PG, Theda C, Thio M. Accuracy of five formulae to determine the insertion length of umbilical venous catheters. Arch Dis Child Fetal Neonatal Ed. (2019) 104(2):F165–9. doi: 10.1136/archdischild-2017-314280
5. Greenberg M, Movahed H, Peterson B, Bejar R. Placement of umbilical venous catheters with use of bedside real-time ultrasonography. J Pediatr. (1995) 126(4):633–5. doi: 10.1016/S0022-3476(95)70366-7
6. Hoellering AB, Koorts PJ, Cartwright DW, Davies MW. Determination of umbilical venous catheter tip position with radiograph. Pediatr Crit Care Med. (2014) 15(1):56–61. doi: 10.1097/PCC.0b013e31829f5efa
7. Barone G, Pittiruti M, Biasucci DG, Elisei D, Iacobone E, La Greca A, et al. Neo-ECHOTIP: a structured protocol for ultrasound-based tip navigation and tip location during placement of central venous access devices in neonates. J Vasc Access. (2022) 23(5):679–88. doi: 10.1177/11297298211007703
8. Seigel A, Evans N, Lutz T. Use of clinician-performed ultrasound in the assessment of safe umbilical venous catheter tip placement. J Paediatr Child Health. (2020) 56(3):439–43. doi: 10.1111/jpc.14658
9. Kozyak BW, Fraga MV, Juliano CE, Bhombal S, Munson DA, Brandsma E, et al. Real-time ultrasound guidance for umbilical venous cannulation in neonates with congenital heart disease. Pediatr Crit Care Med. (2022) 23(5):e257–66. doi: 10.1097/PCC.0000000000002919
10. Meinen RD, Bauer AS, Devous K, Cowan E. Point-of-care ultrasound use in umbilical line placement: a review. J Perinatol. (2020) 40(4):560–6. doi: 10.1038/s41372-019-0558-8
11. Kishigami M, Shimokaze T, Enomoto M, Shibasaki J, Toyoshima K. Ultrasound-guided umbilical venous catheter insertion with alignment of the umbilical vein and ductus venosus. J Ultrasound Med. (2020) 39(2):379–83. doi: 10.1002/jum.15106
12. D'Andrea V, Prontera G, Cota F, Perri A, Russo R, Barone G, et al. Real-time ultrasound tip location reduces malposition and radiation exposure during umbilical venous catheter placement in neonates: a retrospective, observational study. Neonatology. (2025) 122(1):32–7. doi: 10.1159/000538905
13. Fleming SE, Kim JH. Ultrasound-guided umbilical catheter insertion in neonates. J Perinatol. (2011) 31(5):344–9. doi: 10.1038/jp.2010.128
14. Manerkar S, Mondkar J, Kaur A. Ultrasound-guided umbilical venous catheter insertion to reduce rate of catheter tip malposition in neonates: a randomized, controlled trial: authors’ reply. Indian J Pediatr. (2022) 89(11):1164–1164. doi: 10.1007/s12098-022-04370-2
15. Rossi S, Jogeesvaran KH, Matu E, Khan H, Grande E, Meau-Petit V. Point-of-care ultrasound for neonatal central catheter positioning: impact on x-rays and line tip position accuracy. Eur J Pediatr. (2022) 181(5):2097–108. doi: 10.1007/s00431-022-04412-z
Keywords: umbilical catheters, ultrasound, position, catheter tip, radiography
Citation: Cossovel F, Galdo F, Ronfani L, Travan L, Bibalo C and Trappan A (2025) Real-time ultrasound enhances umbilical venous catheters placement in preterm newborns. Front. Pediatr. 13:1567586. doi: 10.3389/fped.2025.1567586
Received: 27 January 2025; Accepted: 29 April 2025;
Published: 13 May 2025.
Edited by:
Simone Pratesi, Careggi University Hospital, ItalyReviewed by:
Vito D'Andrea, Department of Women's Health, Children's Health and Public Health, Agostino Gemelli University Polyclinic (IRCCS), ItalyRose M. Viscardi, University of Maryland, United States
Copyright: © 2025 Cossovel, Galdo, Ronfani, Travan, Bibalo and Trappan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Francesca Cossovel, ZnJhbmNlc2NhLmNvc3NvdmVsQGJ1cmxvLnRyaWVzdGUuaXQ=
 Francesca Cossovel
Francesca Cossovel Francesca Galdo1
Francesca Galdo1 Luca Ronfani
Luca Ronfani