- 1Department of Pharmacy, Children's Hospital of Nanjing Medical University, Nanjing, China
- 2Department of Emergency, Children's Hospital of Nanjing Medical University, Nanjing, China
Next-generation sequencing (NGS), known as massively parallel sequencing, is transitioning from research tools to a clinical diagnostic methods. Whole-exome sequencing (WES), a specific applications of NGS, has emerged as a valuablefirst-line diagnostic tool for patients with rare diseases and shows promise as aas a comprehensive approach for assessing the prevalence of hereditary pancreatitis. Herein, we present a pediatric case that highlights the pitfalls of false-positive missense variants calls in the PRSS1 gene when using NGS. The patient was ultimately diagnosed with valproic acid-induced acute pancreatitis. Our findings emphasize that relying solely on WES data in epidemiological studies of hereditary pancreatitis might introduce bias, given the difficulties in accurately detecting variants within highly homologous genomic regions.
Introduction
Variants in the PRSS1 gene, which encodes human cationic trypsinogen have been conclusively associated with autosomal dominant hereditary pancreatitis (1). The p.A16V and p.N29I mutations, both high-penetrance PRSS1 pathogenic variants, may contribute to the multigenic inheritance of a predisposition to pancreatitis. Next-generation sequencing (NGS) enables high-throughput, massively parallel sequencing of thousands to billions of DNA fragments independently and simultaneously. A previous study reported a validation rate of 99.965% for NGS-detected variants, suggesting that routine Sanger sequencing confirmation may not always be necessary (2). Whole-exome sequencing (WES), a prominent application of NGS, is valuable for molecular diagnosis and family genetic counseling (3). It is emerging as a first-line diagnostic tool for patients with rare diseases (4) and holds promise as a comprehensive genetic approach for estimating the prevalence of hereditary pancreatitis (5). We report a case involving false-positive variant calls in PRSS1 identified by NGS in a pediatric patient with pancreatitis. This case underscores the potential for false positives when relying solely on WES for PRSS1 mutation screening.
Case description
A 6-year-old boy weighing 31 kg was admitted to our Emergency Care Unit after experiencing persistent acute abdominal pain for 23 h. Notably, he had a medical history of viral encephalitis complicated by secondary epilepsy. One day before admission, he underwent a routine follow-up examination at a local hospital and subsequently developed severe abdominal later that evening. An abdominal computed tomography(CT) was performed at the local facility revealed significant enlargement pancreatic enlargement with blurred peripancreatic fat, findings suggestive of acute pancreatitis. As his abdominal pain progressively worsened, he was transferred to our institution for further management. He had no prior history of pancreatitis.
Five months before admission, valproic acid (VPA) was initiated for epilepsy control, with the dosage gradually increased from 300 mg/day–1,000 mg/day. A serum drug concentration measured two months earlier was 75.1 mg/L, which is within the therapeutic range. Concomitant medications included oxcarbazepine and topiramate (both started five months earlier), clonazepam (started two months earlier), lacosamide (started one month earlier), and a low dose of prednisone (1.25 mg/kg/day) for steroid tapering.
On arrival, the patient was afebrile with with stable vital signs, including a heart rate of 112 beats/min and a blood pressure of 135/79 mmHg. Physical examination showed peritoneal irritation, absent bowel sounds, and no skin lesions or palpable abdominal masses. Initial laboratory tests showed leukocytosis (22.31 × 109/L) with neutrophilia (18.45 × 109/L), hyperlactatemia (5.2 mmol/L), and markedly elevated amylase (773 U/L). C-reaction protein (CRP < 8 mg/L), procalcitonin (0.084 ng/ml), lipid profile, liver and kidney function, electrolytes, and coagulation parameters were all within normal limits. Urine analysis revealed a significantly elevated urinary amylase level (9,710 U/L).
Following initial fluid resuscitation, the boy was transferred to Pediatric Intensive Care Unit (PICU) for supportive care and management, where he received supportive care including fasting, total parenteral nutrition, empiric antibiotic therapy (ceftriaxone, 50 mg/kg intravenously), analgesia (remifentanil infusion), acid suppression therapy (omeprazole, 40 mg/day intravenously), and anti-pancreatic enzyme therapy (octreotide, 300 μg/day intravenously). On the second hospital day, the patient developed a fever. Concurrently, accompanied by elevated amylase (1,177 U/L) and CRP(143 mg/L). Comprehensive investigations excluded common causes of acute pancreatitis, including biliary obstruction or gallstones (no history or imaging evidence), trauma (denied by the patient and family), infection (initial inflammatory markers were within normal limits, making infectious pancreatitis unlikely), hyperlipidemia, and hypercalcemia (both serum lipid and calcium levels were normal). Liver and kidney function, electrolytes, and coagulation profiles remained unremarkable, effectively excluding systemic diseases as contributing factors. In the absence of other common causes and in light of the recent initiation and dose escalation of VPA, drug-induced pancreatitis was suspected, prompting the discontinuation of VPA therapy. Following its withdrawal, the patient's clinical symptoms and biochemical parameters gradually improved; CRP decreased to 20 mg/L and amylase to 92 U/L within one week. After two weeks, the patient was transferred back to the neurology department without reinitiating VPA treatment.
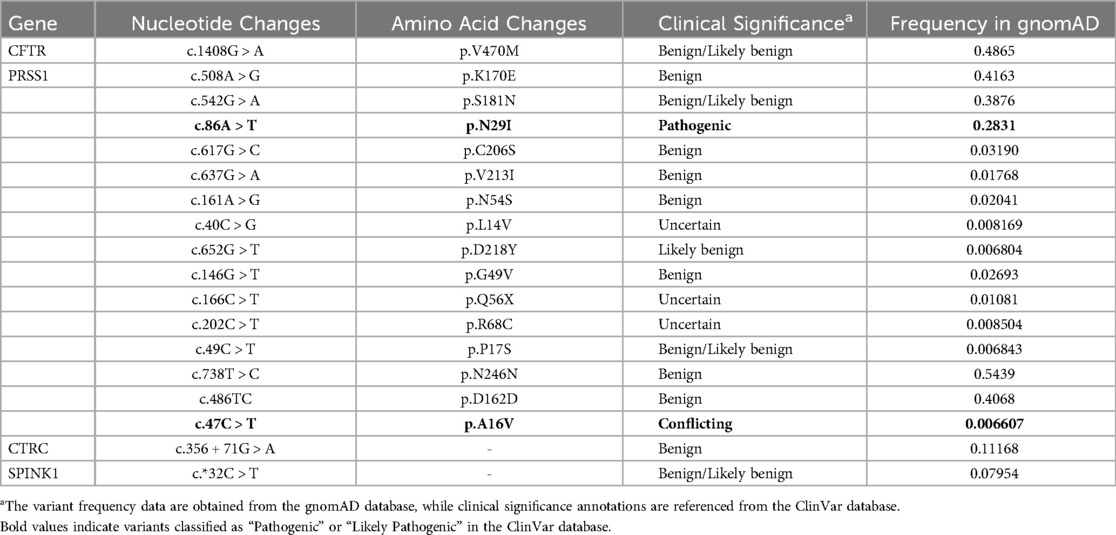
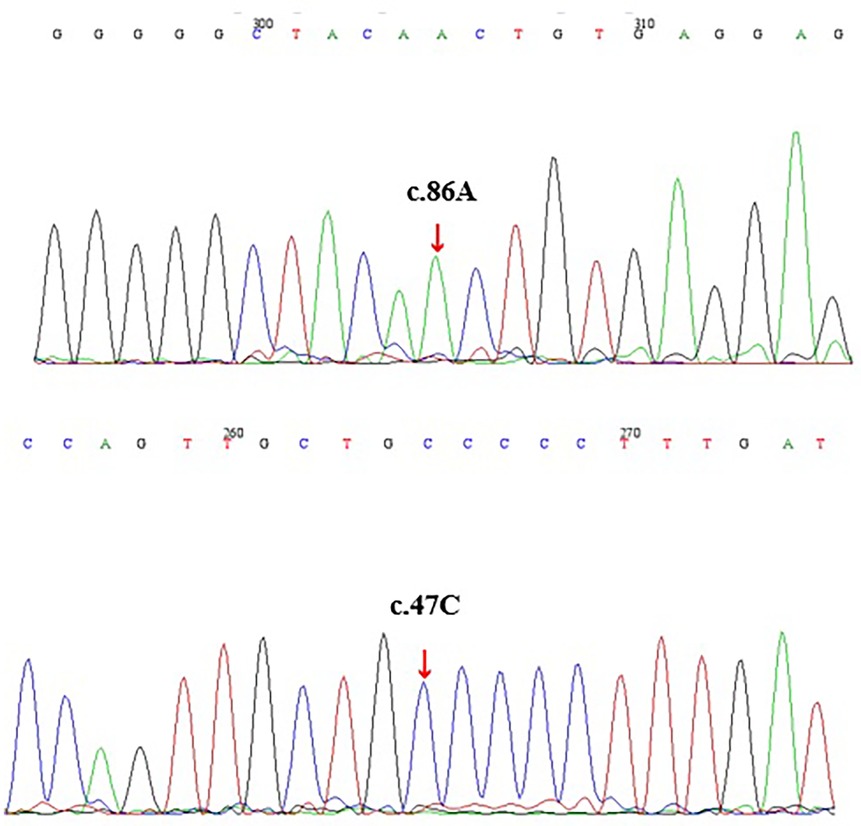
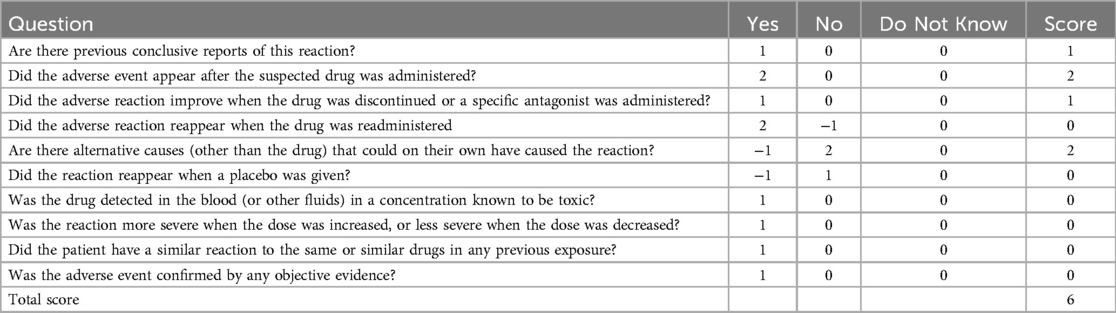
Given the patient's family history of pancreatitis (Supplementary Figure S1), hereditary pancreatitis was investigated using WES following informed parental consent and approval from the Ethics Committee of the Children's Hospital of Nanjing Medical University. WES initially identified two heterozygous variants in exon 2 of the PRSS1 gene: c.47C > T (p.A16V) and c.86A > T (p.N29I) (Table 1). However, subsequent validation by Sanger sequencing of all five PRSS1 exons failed to confirm these variants in either the patient or his parents (Figure 1, Supplementary Figures S2, S3). Based on the Naranjo Adverse Drug Reaction Probability Scale (score = 6; Table 2), VPA was determined to be the likely causative agent, leading to a final diagnosis of drug-induced acute pancreatitis. Druing 21 months of follow-up, the child exhibited normal growth and development without recurrence of abdominal pain or other symptoms of pancreatitis.
Discussion
The global incidence of acute pancreatitis in the pediatric population is increasing, with an estimated estimated annual incidence of approximately 1 in 10,000 from all causes (6). The etiologies of acute pancreatitis in children are diverse and include infectious diseases, metabolic causes, drugs, and toxins, genetic disorders, obstructive causes, and trauma (6). Among these, genetic factors have received growing attention. Since the PRSS1 gene, which encodes human cationic trypsinogen, was first linked to autosomal dominant hereditary pancreatitis, more than 50 PRSS1 variants have been reported (7). The p.N29I, the second most common PRSS1 mutation, first described in 1997, accounts for nearly 25% of hereditary pancreatitis cases (8). p.A16V, the third most common PRSS1 mutation (9), is primarily associated with idiopathic pancreatitis and shows variable clinical penetrance (10).
The present study revealed a high rate of false-positive missense variants at the PRSS1 gene when using NGS. These false positives are likely caused by the strong sequence homology among PRSS1, PRSS2, and the pseudogenes PRSS3P3, a known challenge reported in previous studies (11). In particular, the c.86A > T (p.N29I) and c.47C > T (p.A16V) variants are located within regions of about 80 bases pairs that shares very high sequence similarity, making it difficult to accurately align the short reads generated by NGS (Figure 2). This issue leads to the misalignment of sequencing fragments, causing erroneous variant calls (12). Moreover, inherent limitations of NGS technology, such as short read lengths, reliance on reference-based alignment, and intrinsic limitations of variant calling algorithms, further complicate accurate variant detection in these highly homologous regions, frequently resulting in false-positive calls within PRSS1 (13, 14).
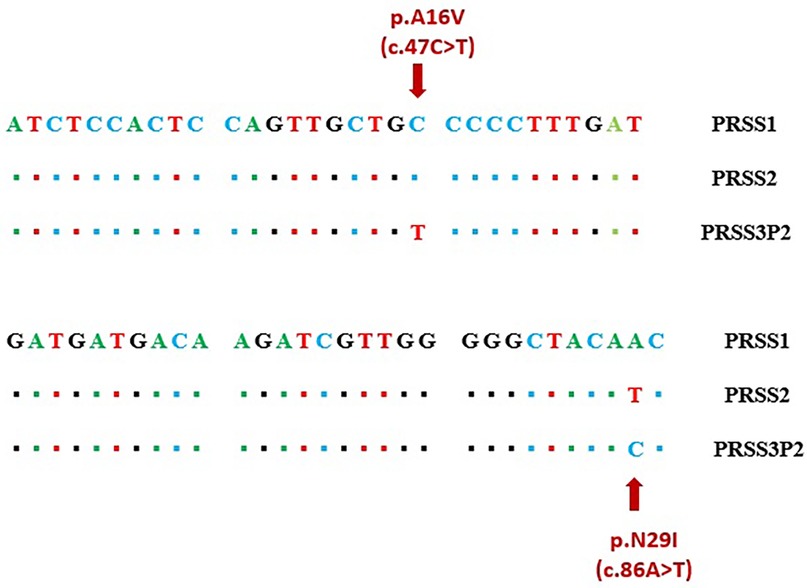
Figure 2. Region of high homology in exon 2 including sequence variants c.47C > T (A16V) and c.86A > T (N29I).
To validate the NGS findings, we performed Sanger sequencing of all five PRSS1 exons in the proband and identified only two synonymous variants (c.486T > C/p.D162 = and c.738T > C/p.N246=), while none of the missense variants reported by NGS were detected (Supplementary Figures S2, S3). This clearly demonstrates the false-positive issue associated with NGS in detecting PRSS1 variants and highlights the need for cautious interpretation of NGS results in highly homologous gene regions, supported by confirmatory methods such as Sanger sequencing. Furthermore, we observed that the relatively high allele frequency of p.A16V variant (0.66%) in the gnomAD v2.1.1 database may be influenced by these false-positive calls, potentially explaining the conflicting interpretations of its pathogenicity in the ClinVar database (13).
Drugs account a notable proportion of pediatric acute pancreatitis cases, representing approximately 0.1%–2% (15). In our case, the patient exhibited with severe abdominal pain, markedly elevated serum and urinary amylase levels, and abnormal pancreatic findings on abdominal CT. Based on the Atlanta classification for acute pancreatitis (16), the boy was diagnosed with acute pancreatitis. Comprehensive lipid profile, abdominal CT, and biochemistry excluded other common causes, and long-term use of VPA was identified as the likely etiology. After discontinuing VPA, the patient's symptoms rapidly resolved, and he remained symptom-free over a 21-month follow-up period while continuing treatment with oxcarbazepine, topiramate, clonazepam, and lacosamide, further supporting the diagnosis of drug-induced pancreatitis.
Nonetheless, this study did not assess mutations in the CFTR gene, limiting the ability to exclude other potential genetic factors. Future research should include a comprehensive screening of additional genetic susceptibility genes associated with pancreatitis to better define the genetic background and underlying disease mechanisms.
Conclusions
The present case highlights the challenges of using NGS to diagnose hereditary pancreatitis. The high sequence homology among genomic regionsposes significant difficulties for accurate genome assembly and variant calling. WES using NGS alone has limitations in reliably detecting mutations in PRSS1. Therefore, confirmation of NGS findings by Sanger sequencing should remain the gold standard for diagnosing hereditary pancreatitis. Furthermore, the use of WES in epidemiological studies of hereditary pancreatitis may introduce data bias, emphasizing the need for cautious interpretation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Children's Hospital of Nanjing Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YL: Writing – original draft, Conceptualization, Data curation, Funding acquisition. HM: Data curation, Writing – review & editing. QZ: Writing – review & editing, Data curation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Heng-rui Hospital Medical Project of the Jiangsu Pharmaceutical Association (H202338).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2025.1572366/full#supplementary-material
References
1. Németh BC, Sahin-Tóth M. Human cationic trypsinogen (PRSS1) variants and chronic pancreatitis. Am J Physiol. (2014) 306:G466–73. doi: 10.1152/ajpgi.00419.2013
2. Beck TF, Mullikin JC, Biesecker LG. Systematic evaluation of sanger validation of next-generation sequencing variants. Clin Chem. (2016) 62:647–54. doi: 10.1373/clinchem.2015.249623
3. Sánchez-Luquez KY, Carpena MX, Karam SM, Tovo-Rodrigues L. The contribution of whole-exome sequencing to intellectual disability diagnosis and knowledge of underlying molecular mechanisms: a systematic review and meta-analysis. Mutat Res. (2022) 790:108428. doi: 10.1016/j.mrrev.2022.108428
4. Ibañez K, Polke J, Hagelstrom RT, Dolzhenko E, Pasko D, Thomas ERA, et al. Whole genome sequencing for the diagnosis of neurological repeat expansion disorders in the UK: a retrospective diagnostic accuracy and prospective clinical validation study. The Lancet Neurol.. (2022) 21:234–45. doi: 10.1016/S1474-4422(21)00462-2
5. Wu D, Bampton TJ, Scott HS, Brown A, Kassahn K, Drogemuller C, et al. The clinical and genetic features of hereditary pancreatitis in South Australia. Med J Aust. (2022) 216:578–82. doi: 10.5694/mja2.51517
6. Uc A, Husain SZ. Pancreatitis in children. Gastroenterology. (2019) 156:1969–78. doi: 10.1053/j.gastro.2018.12.043
7. Girodon E, Rebours V, Chen JM, Pagin A, Levy P, Ferec C, et al. Clinical interpretation of PRSS1 variants in patients with pancreatitis. Clin Res Hepatol Gastroenterol. (2021) 45:101497. doi: 10.1016/j.clinre.2020.07.004
8. Gorry MC, Gabbaizedeh D, Furey W, Gates LK Jr., Preston RA, Aston CE, et al. Mutations in the cationic trypsinogen gene are associated with recurrent acute and chronic pancreatitis. Gastroenterology. (1997) 113:1063–8. doi: 10.1053/gast.1997.v113.pm9322498
9. Grocock CJ, Rebours V, Delhaye MN, Andrén-Sandberg A, Weiss FU, Mountford R, et al. The variable phenotype of the p.A16V mutation of cationic trypsinogen (PRSS1) in pancreatitis families. Gut. (2010) 59:357–63. doi: 10.1136/gut.2009.186817
10. Witt H, Luck W, Becker M. A signal peptide cleavage site mutation in the cationic trypsinogen gene is strongly associated with chronic pancreatitis. Gastroenterology. (1999) 117:7–10. doi: 10.1016/S0016-5085(99)70543-3
11. Lou H, Xie B, Wang Y, Gao Y, Xu S. Improved NGS variant calling tool for the PRSS1-PRSS2 locus. Gut. (2023) 72(1):210–2. doi: 10.1136/gutjnl-2022-327203
12. Weiss FU, Laemmerhirt F, Lerch MM. Next generation sequencing pitfalls in diagnosing trypsinogen (PRSS1) mutations in chronic pancreatitis. Gut. (2020):gutjnl-2020-322864. doi: 10.1136/gutjnl-2020-322864
13. Génin E, Cooper DN, Masson E, Férec C, Chen JM. NGS Mismapping confounds the clinical interpretation of the PRSS1 p.Ala16Val (c.47C > T) variant in chronic pancreatitis. Gut. (2022) 71:841–2. doi: 10.1136/gutjnl-2021-324943
14. Lou H, Xie B, Wang Y, Gao Y, Xu S. Improved NGS variant calling tool for the PRSS1-PRSS2 locus. Gut. (2023) 72:210–2. doi: 10.1136/gutjnl-2022-327203
15. Chadalavada P, Simons-Linares CR, Chahal P. Drug-induced acute pancreatitis: prevalence, causative agents, and outcomes. Pancreatology. (2020) 20:1281–6. doi: 10.1016/j.pan.2020.07.401
Keywords: PRSS1, pediatric, acute pancreatitis, NGS - next generation sequencing, pitfall
Citation: Liu Y, Miao H and Zhang Q (2025) Next generation sequencing misguided the clinical interpretation of the PRSS1 variant in pediatric pancreatitis: a case report. Front. Pediatr. 13:1572366. doi: 10.3389/fped.2025.1572366
Received: 7 February 2025; Accepted: 29 July 2025;
Published: 11 August 2025.
Edited by:
Joanna Zawitkowska, Medical University of Lublin, PolandReviewed by:
Balázs Németh, University of Szeged, HungaryMaja Krajinovic, Montreal University, Canada
Copyright: © 2025 Liu, Miao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yao Liu, bGl1eWFvX25jaEAxNjMuY29t; Qin Zhang, emhhbmdxaW4yNDFAYWxpeXVuLmNvbQ==
 Yao Liu
Yao Liu Hongjun Miao
Hongjun Miao Qin Zhang
Qin Zhang