- 1Department of Pediatrics, Division of Critical Care Medicine, Baylor College of Medicine, Houston, TX, United States
- 2Department of Pediatrics, Division of Critical Care Medicine, Vanderbilt University Medical Center, Nashville, TN, United States
- 3Institute for Clinical & Translational Research, Baylor College of Medicine, Houston, TX, United States
- 4Department of Pediatrics, Division of Cardiology, Baylor College of Medicine, Houston, TX, United States
Importance: Disparities in congenital heart disease, pediatric intensive care unit (ICU) outcomes, and acute pain control are common. The impact of patient race, ethnicity, and language on postoperative sedation and analgesia for pediatric patients undergoing cardiac surgery is unknown.
Objective: This study aims to investigate whether there are differences in sedation and analgesia in patients undergoing cardiac surgery according to patient race, ethnicity, and language in a study site that uses protocolized postoperative sedation and analgesia. We hypothesized that non-white and patients who prefer a language other than English would have differences in total doses of sedation compared with their white and English-speaking counterparts.
Design: This is a single-center, retrospective, observational cohort of pediatric patients admitted postoperatively to the cardiac ICU.
Setting: The study took place in an urban, quaternary, academic pediatric referral center.
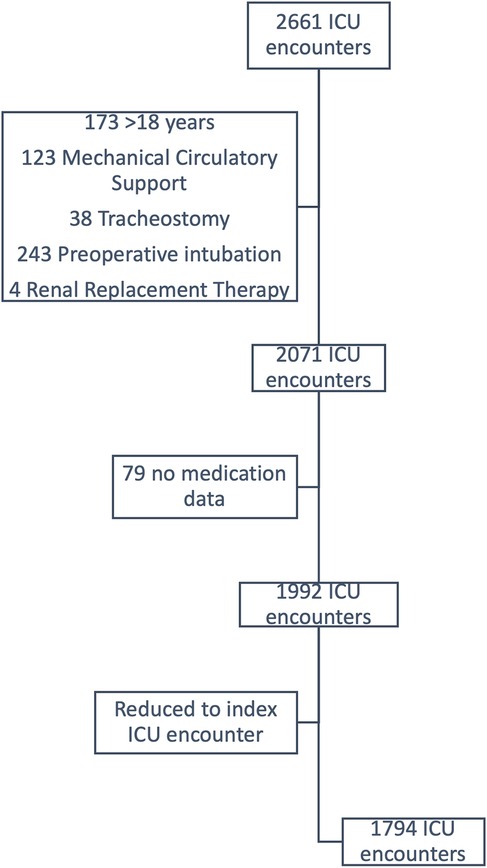
Participants: All pediatric patients, age 0–18 years, admitted to the cardiac ICU following their index cardiac surgery from 7/1/2018 to 6/30/2022 were included. Patients requiring renal replacement therapy, non-cardiac surgery during the same admission, tracheostomy, preoperative mechanical ventilation, or mechanical circulatory support prior to or following cardiac surgery were excluded.
Exposures: Exposure variables included patient race and ethnicity, preferred language, age, gender, Society of Thoracic Surgeons-European Association for Cardiothoracic Surgery category, use of cardiopulmonary bypass, duration of postoperative mechanical ventilation, and delayed sternal closure (DSC).
Main outcome and measure: The primary outcome was weight-adjusted doses of opioids in morphine equivalents, benzodiazepines in midazolam equivalents, and dexmedetomidine received in the first 72 h postoperatively.
Results: There were 1,794 postoperative admissions. 100% of patients received opioids, 42.5% received benzodiazepines, and 85% received dexmedetomidine. There were no differences in opioid, benzodiazepine, or dexmedetomidine doses according to patient race and ethnicity or preferred language. Patient race, ethnicity, and language were not associated with opioid or benzodiazepine dose in multivariable quantile regression. Multivariable regression for dexmedetomidine demonstrated similar results with age also being inversely correlated.
Conclusions: and Relevance: Doses of postoperative sedation and analgesia are not correlated with patient race, ethnicity, and language. Factors that were associated with differences in medication doses are reflective of postoperative acuity and are expected. Protocolized sedation and analgesia may be responsible for the lack of differences seen in this study when compared with other studies in similar settings. Future studies should compare protocolized and non-protocolized sedation and analgesia to further evaluate the protective effects of protocols against bias in clinical settings.
Introduction
Social determinants of health are known to effect health outcomes for pediatric patients and are often the root cause of health inequities among racially, ethnically, and linguistically diverse groups. These effects have been specifically identified in outcomes for patients in pediatric intensive care units (ICU), with congenital heart disease (CHD), and with acute pain complaints (1–5). For pediatric patients admitted to the ICU, differences include higher rates of admission and longer lengths of stay for patients with higher rates of poverty (1). Higher rates of mortality have been reported for Hispanic patients, patients from lower socioeconomic backgrounds, and patients without insurance (6–8). Black patients are also overrepresented in those admitted to the PICU relative to the general population, even when controlling for insurance status and initial illness severity (1). Additionally, patients who prefer a language other than English encounter elevated hospitalization costs, increased incidence of serious adverse events, and more frequent transfers to the ICU, all while expressing diminished satisfaction with communication from medical teams during their hospitalization (2, 4, 9–11).
Similar disparities are seen in pediatric patients with CHD. Though there have been marked advancements in surgical outcomes, non-Hispanic white children have experienced greater reductions in mortality rate than their Black counterparts (3). Similarly, Black children also exhibit higher rates of postoperative complications after cardiac surgery (12, 13).
Regarding acute pain management, non-white children with long bone fractures or abdominal pain in emergency departments are less likely to achieve optimal pain reduction during their visits (14, 15). Results from the perioperative period are mixed with some studies finding differences in post- or intraoperative opioid administration or receipt of regional anesthesia, but equivocal results are reported (16–18).
Several studies have evaluated the use of sedation protocols that are driven by nursing assessments of level of sedation and pain with medication doses adjusted accordingly (19–22). Overall, these studies suggest that sedation targets using validated scores can safely reduce doses of benzodiazepines while not effecting duration of mechanical ventilation, PICU LOS, pain scores, or rates of unplanned extubations. While these studies have demonstrated the safety of protocolized sedation, they have not evaluated these protocols through the lens of health equity. A secondary analysis of the RESTORE trial, one of the largest randomized studies that has evaluated protocolized sedation in pediatrics, found no differences in doses of sedation and analgesia according to race and ethnicity in both the control and intervention arms (Nathaly 2021). Importantly, this study did not evaluate the contribution of language and was limited to the original study cohort of pediatric patients intubated for respiratory failure.
Despite knowledge of disparities in pediatric ICUs, CHD, and acute pain management, there is a paucity of knowledge on the impact of race, ethnicity, and language on sedation and analgesia for postoperative cardiac patients in the immediate postoperative period.
Given what is known about disparities in PICU outcomes and sedation and analgesia, we hypothesize that following cardiac surgery, differences will exist in the cumulative doses of medications received for sedation and analgesia among non-white and non-English speaking patients compared to their white and English-speaking counterparts. The primary aim of this study is to compare the weight-adjusted dose of medications received for sedation and analgesia following cardiac surgery based on patient race, ethnicity, and language in a study site that uses protocolized post-operative sedation and analgesia. The secondary aim is to evaluate patient outcomes such as ventilator days, rate of unplanned extubations, cardiac arrest, and mortality.
Methods
This study is a single-center, retrospective observational cohort of pediatric patients (age 0–18 years) who were admitted to the cardiac ICU following cardiac surgery from July 1, 2018, to June 30, 2022. Patients were excluded if they required renal replacement therapy, had non-cardiac surgery during the same admission, pre-existing tracheostomy, preoperative mechanical ventilation, or required mechanical circulatory support prior to or following the cardiac surgery. Patients who had pain managed with exclusively patient-controlled analgesia (PCA) were also excluded due to incomplete data collection. The study site is a large, urban, academic pediatric hospital system in the United States. A standardized sedation and pain management protocol was implemented in the cardiac ICU in 2017 and was adopted prior to the study. The pathways give providers starting medications and doses and include the use of documented State Behavior Scale (SBS) for sedation as well as validated scores for pain based on age to allow nurses and practitioners to titrate sedative and pain medications to desired effect.
Data for doses of sedation and analgesia, race, ethnicity, and language were obtained from the electronic medical record and all other information from the local Pediatric Cardiac Critical Care Consortium (PC4) registry database. Both databases were used equally for all patients. The study was approved by the Baylor College of Medicine Institutional Review Board and informed consent for this historical study was waived.
Exposure variables included combined patient race and ethnicity, patient preferred language, age, gender, Society of Thoracic Surgeons-European Association for Cardio-Thoracic Surgery (STAT) category, use of cardiopulmonary bypass (CPB), duration of postoperative mechanical ventilation, and delayed sternal closure (DSC). Race, ethnicity, and preferred language are either self-reported by parents or documented by staff upon admission to the hospital or an inpatient setting. Patients with missing race and ethnicity, or language data were excluded from analysis (n = 10).
The primary outcome was weight-adjusted doses of opioids, benzodiazepines, and dexmedetomidine received in the first 72 h postoperatively. By using the first 72 postoperative hours, the focus remains on treatment of acute, perioperative pain and avoiding variations that occur due to length of stay, comorbidities, or other complications. Opioids were converted to morphine milligram equivalents and benzodiazepines were converted to midazolam milligram equivalents for the purpose of comparison. The secondary outcomes were duration of mechanical ventilation, unplanned extubations, cardiac arrest, and mortality as collected in PC4.
Patient characteristics and non-parametric outcomes are described using mean with standard deviation (SD), median with interquartile range (IQR), and frequency with percentage. Wilcoxon rank sum test, Chi square test, and Fisher's exact test were used to compare categorical characteristics. Unadjusted and multivariable quantile regression were performed to assess the association between characteristics and medication doses. A p-value of <0.05 was considered statistically significant for all comparisons and all analyses were performed using Stata v18 (College Station, TX).
Results
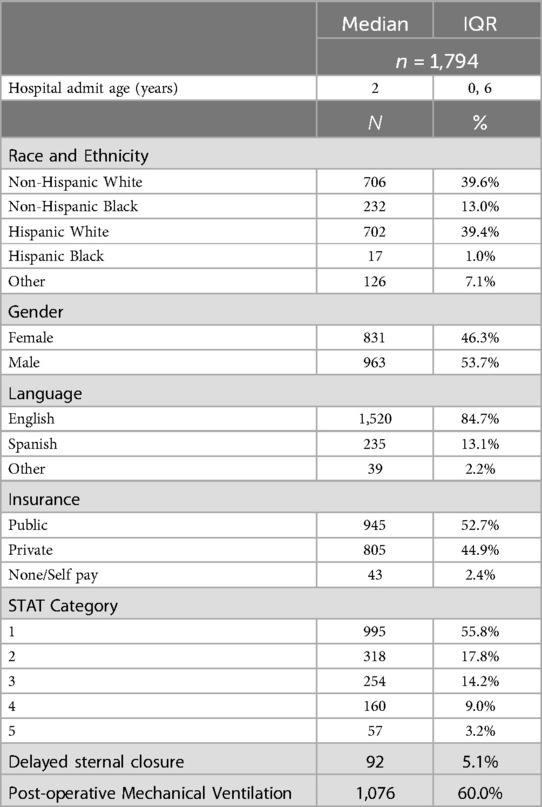
The cohort included 2,661 postoperative CICU encounters. After applying exclusion criteria, there were 1,794 remaining encounters (Figure 1). Demographics of the cohort are found in Table 1. Notably, the median age of the cohort upon admission was 2 years (IQR 0–6 years) and the majority were male (n = 963, 53.7%). Despite 702 (39.4%) of patients identifying as Hispanic white, only 235 (13.1%) preferred Spanish as a primary language. Most surgeries were classified as STAT 1 (n = 995, 55.8%) and only 57 (3.2%) as STAT 5. Comparisons in DSC, STAT category distribution, operation requiring CPB, or rates of postoperative mechanical ventilation according to patient race and ethnicity or language revealed no differences (Table 2).
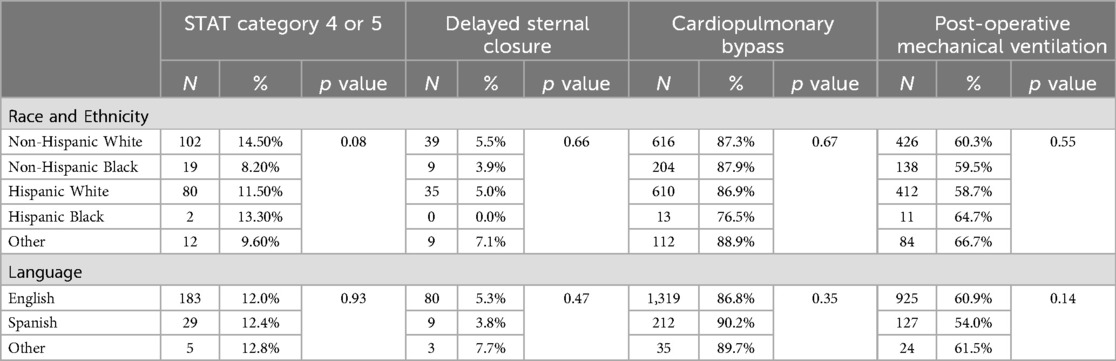
Table 2. Comparison of STAT category, DSC, CPB, and post-operative mechanical ventilation according to patient race, ethnicity, and language.
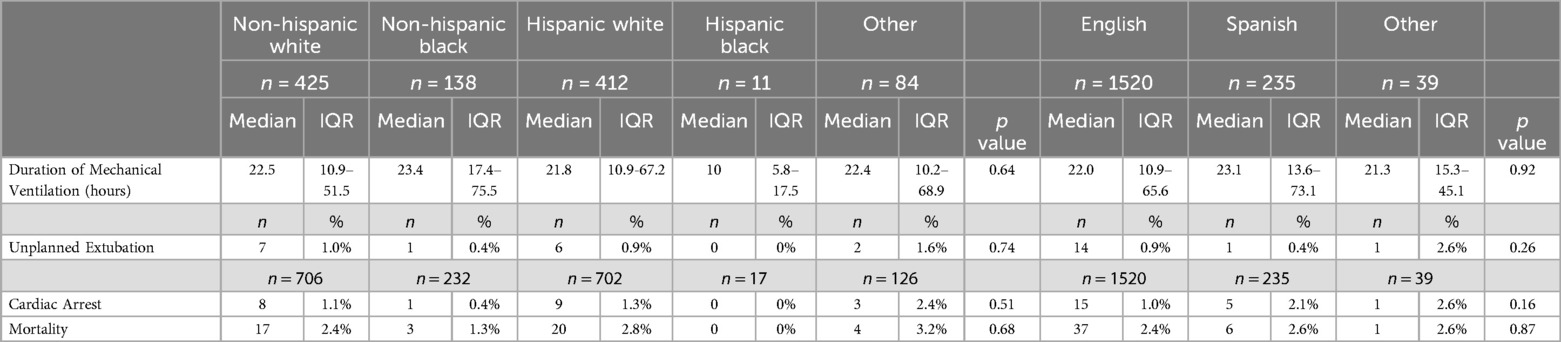
All patients included in the cohort received postoperative opioids, 763 (42.5%) received benzodiazepines, and 1,525 (85%) received dexmedetomidine. There were no differences in total doses of opioids, benzodiazepines, or dexmedetomidine according to patient race and ethnicity or patient preferred language (Table 3). These results are consistent with other studies of the interaction between race and ethnicity and doses of sedation during mechanical ventilation (Nathaly 2021), but no other study has evaluated the intersection of protocolized sedation and language or focused specifically on postoperative cardiac patients. There were also no differences in duration of mechanical ventilation, or rates of unplanned extubations, cardiac arrest or mortality according to patient race and ethnicity or language (Table 4).
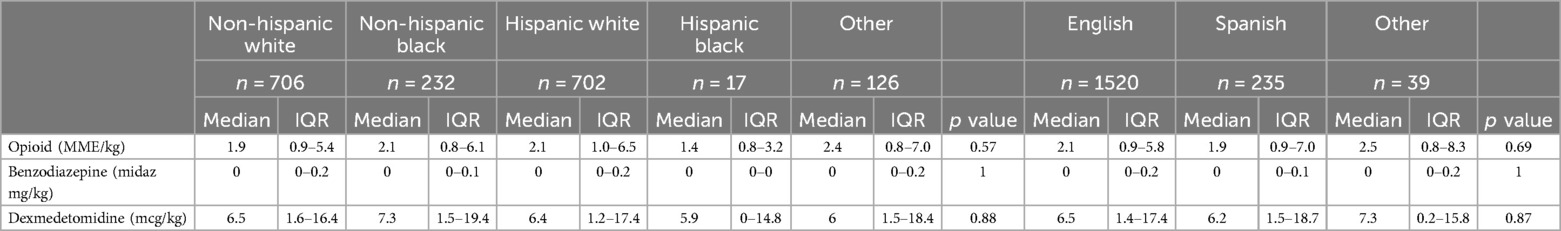
Table 3. Doses of opioids, benzodiazepines, and dexmedetomidine in the first 72 h post-operatively according to patient race and ethnicity.
Race and ethnicity, language, and insurance were not associated with total doses of opioids, benzodiazepines, or dexmedetomidine in unadjusted or multivariable quantile regression. There were several significant associations in unadjusted regression that would be clinically expected including higher doses of opioids and benzodiazepines for patients who were mechanically ventilated (coefficient 2.21, p < 0.05), had longer hospital length of stay (coefficient 0.03, p < 0.05), and underwent DSC (coefficient 7.19, p < 0.05). Dexmedetomidine demonstrated similar findings with lower doses for older age (coefficient −0.26, p < 0.05) and higher doses for patients who were mechanically ventilated (coefficient 5.95, p < 0.05), had longer hospital length of stay (coefficient 0.06, p < 0.05), and underwent DSC (coefficient 10.55, p < 0.05). Multivariable regression with age, STAT category, and post-operative cardiac arrest yielded similar results.
Discussion
Our study found no association between race, ethnicity, or language, and the total dose of opioids, benzodiazepines, and dexmedetomidine received in pediatric patients in the first 72 h following cardiac surgery. This study contributes uniquely to existing literature by focusing specifically on postoperative pediatric cardiac patients and consideration of patient-preferred language in comparisons. The observed variances in medication amounts align with clinical expectations based on illness severity and the typical postoperative trajectory involving mechanical ventilation, DSC, and longer LOS.
While numerous studies have highlighted disparities in analgesia administration based on race, ethnicity, and language, our study did not replicate these findings. This discrepancy is likely attributed to stringent adherence to standard sedation and analgesic protocols based on validated tools, which may have minimized implicit biases. Implicit biases in assessment of pain or sedation needs may still be influenced by the presence of family at the bedside, family health literacy, patient and provider racial or language concordance, and pre-operative illness severity despite the use of protocolized sedation and analgesia.
Despite the widespread adoption of sedation protocols in many adult and pediatric ICUs, research has failed to demonstrate a consistent effect of their impact on total medication dosages, duration of mechanical ventilation, ICU and hospital length of stay, or mortality rates as noted in a Cochrane review (23). Future investigations should extend beyond the acute postoperative period and focus on patients with prolonged hospitalizations in multicenter studies. Furthermore, it will be important to evaluate the efficacy of protocols in managing patients undergoing advanced treatment modalities such as renal replacement therapy and mechanical circulatory support. Centers currently not employing standardized management could benefit from comprehensive analyses comparing pre- and post-implementation outcomes.
Our study found no differences in duration of mechanical ventilation, rates of unplanned extubations, cardiac arrest, or mortality. These findings were unexpected and are in contrast to much of the published data regarding disparities in ICU outcomes according to race, ethnicity, and language. This may be due to the narrow scope of the study population, the variation in patient reported demographics from the study site population, adherence to strict postoperative care standards, and the study site being a large, high volume center for cardiac surgery. Further investigation in this realm is warranted to determine if there are factors that could be replicated in other settings to eliminate common disparities.
Limitations inherent in retrospective EMR data should be acknowledged, along with the absence of real-time decision-making details. Additionally, despite the large study sample size, the racial, ethnic, and language subgroups varied significantly in size and are not representative of the general population of the study site. This could result in selection bias or be reflective of the inadequacy of the current methods for reporting self-identified race and ethnicity and preferred language. While insurance is often used as a proxy for patient socioeconomic status, it lacks nuance and specificity that other markers of socioeconomic status may provide. Notably, this study period coincided with the global COVID pandemic, during which visitation restrictions were in place, yet medication dosages remained consistent, underscoring the robustness of the sedation practices. Nevertheless, it is essential to recognize the limitations of historical data, particularly regarding self-reported or assigned language and ethnicity, which may not fully capture the diversity within these categories or truly reflect patients' racial identities. Additionally, acknowledging race as a social construct underscores the need to consider the multifaceted social and environmental factors influencing health outcomes. Our study may also lack generalizability given it was a single center study with robust sedation and analgesia protocols, a racially, ethnically, and linguistically diverse patient and provider cohort, in a diverse U.S. city.
Overall, our study suggests that protocolized sedation should be further studied as a potential strategy to mitigate racial and language biases among postoperative pediatric cardiac patients admitted to the ICU. Further study is needed to better understand the interplay between sedation protocols and race and ethnicity biases longitudinally and at a multicenter level.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Baylor College of Medicine IRB. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because Minimal risk to participants given retrospective nature of study.
Author contributions
NL: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. BA: Investigation, Methodology, Writing – review & editing. AA: Data curation, Methodology, Supervision, Writing – review & editing. DG: Data curation, Formal analysis, Methodology, Writing – review & editing. KL: Methodology, Supervision, Writing – review & editing. NA: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Andrist E, Riley CL, Brokamp C, Taylor S, Beck AF. Neighborhood poverty and pediatric intensive care use. Pediatrics. (2019) 144(6):e20190748. doi: 10.1542/peds.2019-0748
2. Khan BA, Perkins A, Hui SL, Gao S, Campbell NL, Farber MO, et al. Relationship between African-American race and delirium in the ICU. Crit Care Med. (2016) 44(9):1727. doi: 10.1097/ccm.0000000000001813
3. Lopez KN, Morris SA, Sexson Tejtel SK, Espaillat A, Salemi JL. US Mortality attributable to congenital heart disease across the lifespan from 1999 through 2017 exposes persistent racial/ethnic disparities. Circulation. (2023) 142(12):1132. doi: 10.1161/circulationaha.120.046822
4. Cohen AL, Rivara F, Marcuse EK, Mcphillips H, Davis R. Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics. (2005) 116(3):575. doi: 10.1542/peds.2005-0521
5. Khan A, Yin HS, Brach C, Graham DA, Ramotar MW, Williams DN, et al. Association between parent comfort with English and adverse events among hospitalized children. JAMA Pediatr. (2020) 174(12):e203215. doi: 10.1001/jamapediatrics.2020.3215
6. Anand KJS, Sepanski RJ, Giles K, Shah SH, Juarez PD. Pediatric intensive care unit mortality among latino children before and after a multilevel health care delivery intervention. JAMA Pediatr. (2015) 169(4):383–90. doi: 10.1001/jamapediatrics.2014.3789
7. Colvin JD, Zaniletti I, Fieldston ES, Gottlieb LM, Raphael JL, Hall M, et al. Socioeconomic status and in-hospital pediatric mortality. Pediatrics. (2013) 131(1):e182. doi: 10.1542/peds.2012-1215
8. Turner D, Simpson P, Li S, Scanlon M, Quasney MW. Racial disparities in pediatric intensive care unit admissions. South Med J. (2011) 104(9):640. doi: 10.1097/smj.0b013e3182296e52
9. Zurca AD, Fisher KR, Flor RJ, Gonzalez-Marques CD, Wang J, Cheng YI, et al. Communication with limited English-proficient families in the PICU. Hosp Pediatr. (2017) 7(1):9. doi: 10.1542/hpeds.2016-0071
10. Mcdade JE, Olszewski AE, Qu P, Ramos J, Bell S, Adiele A, et al. Association between language use and ICU transfer and serious adverse events in hospitalized pediatric patients who experience rapid response activation. Front Pediatr. (2022) 10::872060. doi: 10.3389/fped.2022.872060
11. Lion KC, Wright DR, Desai AD, Mangione-Smith R. Costs of care for hospitalized children associated with preferred language and insurance type. Hosp Pediatr. (2017) 7(2):70. doi: 10.1542/hpeds.2016-0051
12. Gallegos FN, Woo JL, Anderson BR, Lopez KN. Disparities in surgical outcomes of neonates with congenital heart disease across regions, centers, and populations. Semin Perinatol. (2022) 46(4):151581. doi: 10.1016/j.semperi.2022.151581
13. Chan T, Pinto NM, Bratton SL. Racial and insurance disparities in hospital mortality for children undergoing congenital heart surgery. Pediatr Cardiol. (2012) 33(7):1026. doi: 10.1007/s00246-012-0221-z
14. Goyal MK, Johnson TJ, Chamberlain JM, Cook L, Webb M, Drendel AL, et al. Racial and ethnic differences in emergency department pain management of children with fractures. Pediatrics. (2020) 145(5):e20193370. doi: 10.1542/peds.2019-3370
15. Johnson TJ, Weaver MD, Borrero S, Davis EM, Myaskovsky L, Zuckerbraun NS, et al. Association of race and ethnicity with management of abdominal pain in the emergency department. Pediatrics. (2013) 132(4):e851. doi: 10.1542/peds.2012-3127
16. King MR, De Souza E, Rosenbloom JM, Wang E, Anderson TA. Association between race and ethnicity in the delivery of regional anesthesia for pediatric patients: a single-center study of 3189 regional anesthetics in 25,664 surgeries. Anesth Analg. (2021) 131(1):255. doi: 10.1213/ane.0000000000004456
17. Jette CG, Rosenbloom JM, Wang E, Souza ED, Anderson TA. Association between race and ethnicity with intraoperative analgesic administration and initial recovery room pain scores in pediatric patients: a single-center study of 21,229 surgeries. J Racial Ethn Health Disparities. (2022) 8(3):547. doi: 10.1007/s40615-020-00811-w
18. Nafiu OO, Chimbira WT, Stewart M, Gibbons K, Porter LK, Reynolds PI. Racial differences in the pain management of children recovering from anesthesia. Pediatr Anesth. (2018) 27(7):760. doi: 10.1111/pan.13163
19. Curley MA, Wypij D, Watson RS, Grant MJC, Asaro LA, Cheifetz IM, et al. Protocolized sedation vs usual care in pediatric patients mechanically ventilated for acute respiratory failure: a randomized clinical trial. JAMA. (2015) 313(4):379–89. doi: 10.1001/jama.2014.18399
20. Deeter KH, King MA, Ridling D, Irby GL, Lynn AM, Zimmerman JJ. Successful implementation of a pediatric sedation protocol for mechanically ventilated patients. Crit Care Med. (2011) 39(4):683–8. doi: 10.1097/CCM.0b013e318206cebf
21. Larson GE, McKeever S. Nurse titrated analgesia and sedation in intensive care increases the frequency of comfort assessment and reduces midazolam use in paediatric patients following cardiac surgery. Aust Crit Care. (2018) 31(1):31–6. doi: 10.1016/j.aucc.2017.02.001
22. Natale JE, Asaro LA, Joseph JG, Ulysse C, Ascenzi J, Bowens C, et al. Association of race and ethnicity with sedation management in pediatric intensive care. Ann Am Thorac Soc. (2021) 18(1):93–102. doi: 10.1513/AnnalsATS.201912-872OC
Keywords: disparities health, sedation, analgesia & critical care, critical care, cardiac surgery
Citation: Lawson NR, Achuff BJ, Ankola A, Guffey D, Lopez K and Afonso N (2025) Sedation and analgesia doses do not differ across demographic factors in pediatric cardiac surgery patients. Front. Pediatr. 13:1577461. doi: 10.3389/fped.2025.1577461
Received: 15 February 2025; Accepted: 27 June 2025;
Published: 16 July 2025.
Edited by:
Avihu Z. Gazit, University of Pittsburgh, United StatesReviewed by:
Catherine M. T. Sherwin, University of Western Australia, AustraliaPaolo Biban, Integrated University Hospital Verona, Italy
Copyright: © 2025 Lawson, Achuff, Ankola, Guffey, Lopez and Afonso. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nikki R. Lawson, bmxhd3NvbkBiY20uZWR1
 Nikki R. Lawson
Nikki R. Lawson Barbara Jo Achuff2
Barbara Jo Achuff2 Danielle Guffey
Danielle Guffey Natasha Afonso
Natasha Afonso