- Department of Rheumatology and Immunology, Children’s Hospital of Nanjing Medical University, Nanjing, China
Autosomal dominant gain-of-function (GOF) variants in the signal transducer and activator of transcription 3 (STAT3) result in an inborn error of immunity characterized by multi-organ autoimmunity and lymphoproliferation. In this study, we retrospectively analyzed a rare case of STAT3 GOF mutation with thrombocytopenia, immunoglobulin deficiency, and recurrent respiratory infections. Whole-exome sequencing revealed a heterozygous mutation (c. 2144C > T, p. P715l) in the STAT3 gene. The patient initially received only anti-infective and immunoglobulin-supportive therapies at an external hospital, which proved unsatisfactory. Over time, the patient developed severe interstitial lung disease (ILD) and arthritis, which were effectively managed with tocilizumab at our hospital. This case underscores the importance of early diagnosis and timely initiation of biological therapy for the management of ILD with STAT3 GOF mutations.
1 Introduction
Signal transducer and activator of transcription 3 (STAT3) belongs to the STAT protein family, which includes seven members and is widely expressed in various immune-related cells. STAT3 plays a central role in regulating cell survival, proliferation, differentiation, and effector functions (1). Human STAT3 is a 770-amino acid protein comprising six structural domains: the N-terminal domain, coiled-coil domain, DNA binding domain, linker domain, Src homology-2 domain, and transcriptional activation (TAD) domain in the C-terminal. Notably, the TAD domain plays a role in regulating phosphorylation (2). A gain-of-function (GOF) mutation in STAT3 results in an inborn error of immunity (IEI), characterized by multi-organ autoimmunity and lymphoproliferation (3). In this study, we describe a case of IEI with a predominant interstitial lung disease (ILD) phenotype and arthritis due to STAT3 GOF mutation. The manifestations of ILD and arthritis in the patient were effectively managed with tocilizumab.
2 Case description
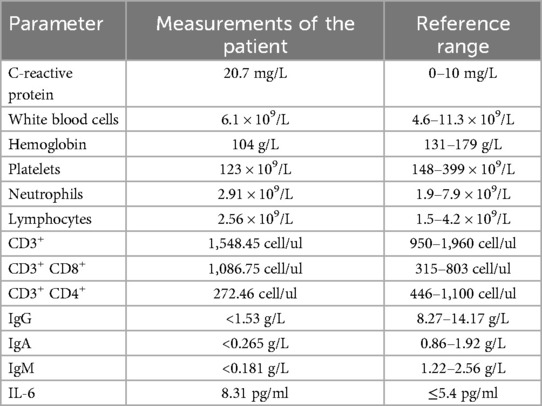
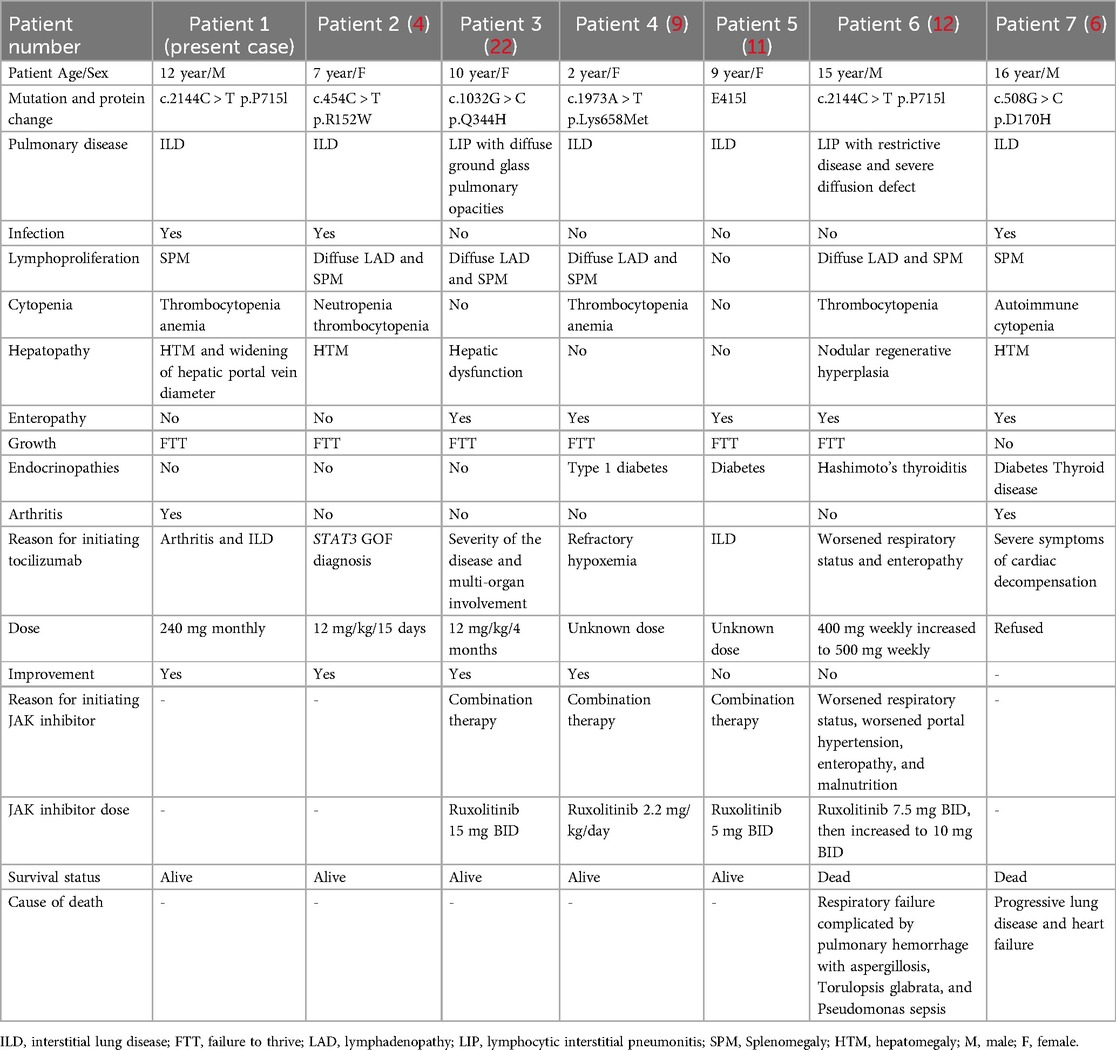
A 12-year-old boy with a 3-month history of pain in the left knee, left elbow, and right ankle presented to our clinic. In addition to arthralgia, the patient also experienced chronic cough for one month with viscous sputum and dyspnea particularly noticeable at night or after exercise. Digital clubbing was also observed. The patient presented with markedly elevated serum Krebs von den Lungen-6 (KL-6) levels (2,887 U/ml; normal <500 U/ml), a biomarker for disease severity assessment in ILD. High-resolution computed tomography (HRCT) revealed characteristic interstitial lung abnormalities including ground-glass opacities, reticulation, airspace consolidation, and traction bronchiectasis (Figure 1A). Pulmonary function testing demonstrated impaired gas exchange with diffusing capacity for carbon monoxide (DLCO) at 70% of predicted value. Functional capacity was compromised as evidenced by 6 min walk distance <80% predicted and oxygen desaturation during exertion (SpO₂ 95% at rest vs. 84% with exercise). Bronchoscopy with bronchoalveolar lavage (BAL) showed lymphocytic-predominant inflammation (lymphocytes 60%, neutrophils 15%, monocytes 25%), while metagenomic next-generation sequencing (mNGS) returned negative for pathogens. These collective findings confirmed associated interstitial lung disease. Other laboratory investigations after admission revealed anemia, thrombocytopenia, and hypogammaglobulinemia (Table 1). Magnetic resonance imaging of the left knee joint revealed periarticular inflammatory lesions accompanied by soft tissue swelling, consistent with the imaging characteristics of arthritis. Furthermore, abdominal ultrasonography demonstrated hepatosplenomegaly.
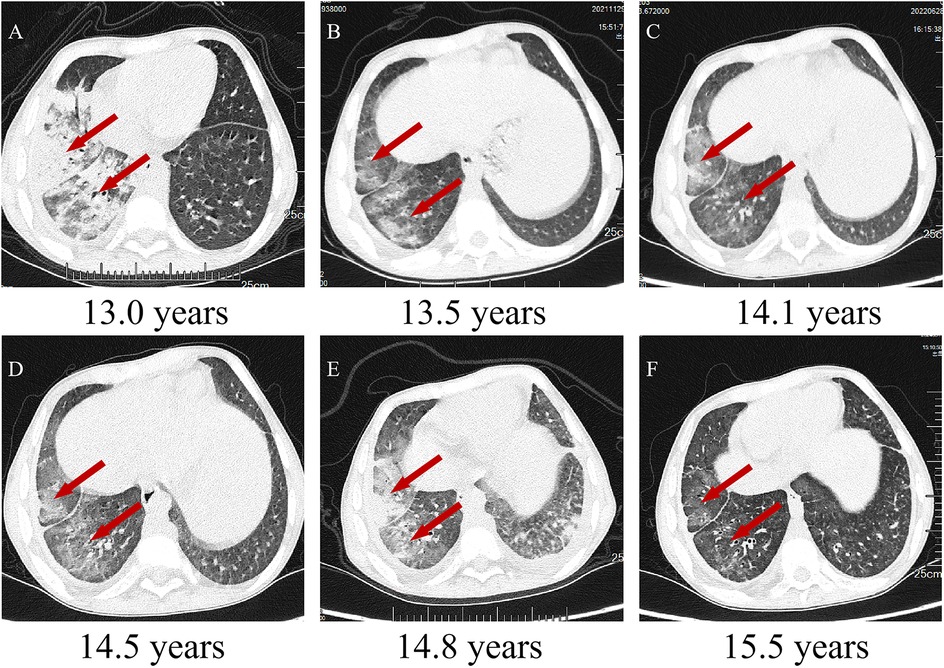
Figure 1. Chest CTs of the patient. (A–F) Chest CTs following regular routine treatment with tocilizumab. Inflammation of the middle and lower lobes of the right lung with ground-glass opacities, reticulation, airspace consolidation, and traction bronchiectasis (indicated by red arrows).
The medical history of the patient indicated recurrent respiratory infections starting at the age of 4 years, for which the patient received antibiotic therapy at external hospitals. At 8 years of age, thrombocytopenia and hypogammaglobulinemia were first documented, with persistently subnormal levels confirmed through repeated testing over the next 8 months. Consequently, regular intravenous immunoglobulin (IVIG) replacement therapy was initiated every 3 months (Supplementary Figure S1). The proband has a healthy younger sister. The parents were non-consanguineous and had no family history of inherited genetic disorders.
3 Diagnostic assessment
The patient underwent whole-exome sequencing (WES) at an external hospital to investigate the etiology of thrombocytopenia and hypogammaglobulinemia at the age of 8 years. His younger sister did not undergo WES due to parental refusal (Figure 2A). WES revealed a heterozygous mutation in exon 22 of the STAT3 gene, resulting in a missense mutation that substitutes proline with leucine at amino acid 715 of the encoded protein (c.2144C > T, p.P715l). Family segregation analysis revealed that neither parent harbored a mutation at this locus (Figure 2A). Conservative analysis revealed that the mutation site is highly conserved among species (Figure 2B). At the time, this variant was not documented in established databases or published literature, resulting in an indefinite diagnosis and the initiation of IVIG therapy at the external hospital. According to GenIA, the variant was initially reported in one boy and one woman from the Czech Republic. In 2020, Mauracher et al. (4) described a female patient carrying the same variant who presented with autoimmune hemolytic anemia and erythroid aplasia. in vitro functional charcterization conducted by the authors showed increased STAT3 phosphorylation by western blot and increased transactivation activity, using a luciferase reporter assay, in both resting and stimulated (Interleukin-6) conditions in HEK cells (4). These experimental findings collectively demonstrate the pathogenicity of this variant.
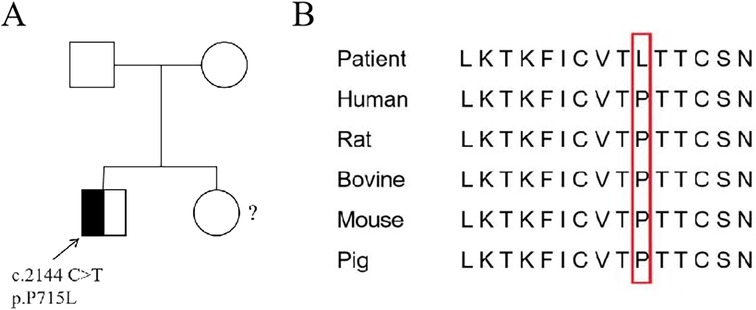
Figure 2. Sanger sequencing and conservative analysis of STAT3 in the patient. (A) The patient exhibited a heterozygous mutation c.2144C > T in exon 11 of the STAT3 gene (the arrow indicates the mutation location). The parents of the patient did not have this mutation and are wild type.?: The sister did not undergo WES. (B) Conservative comparison of STAT3 across five species showed that P 715 is highly conserved.
3.1 Therapeutic intervention
The patient was treated with monthly intravenous tocilizumab (8 mg/kg) along with quarterly IVIG administration for immunomodulatory support and infection prevention. Mild thrombocytopenia and anemia were managed conservatively with regular monitoring.
3.2 Follow-up and outcomes
The patient showed a marked improvement in arthritic symptoms following treatment with tocilizumab, and the ILD symptoms were also effectively managed. The patient maintained normal oxygen saturation levels, demonstrated gradual resolution of exertional dyspnea, and exhibited complete regression of digital clubbing. Following therapeutic intervention, significant improvement was observed: KL-6 decreased substantially to 390 U/ml. Follow-up HRCT demonstrated regression of ground-glass opacities, reticulation, and bronchial dilation (Figure 1B). DLCO increased to 85% predicted, 6-minute walk distance achieved 90% predicted and Oxygen saturation normalized (99% at rest, 93% on exertion). Following tocilizumab and IVIG therapy, the patient demonstrated partial recovery of immunoglobulin level (Figure 3), although they remained below the normal range (8.27–14.17 g/L). A marked reduction in infection frequency supported the continuation of the original IVIG dosing regimen for sustained supportive care. However, during longitudinal follow-up, the patient exhibited persistent failure to thrive (FTT), with anthropometric parameters revealing progressive deterioration. Specifically, at 14 years of age, height was 139 cm (z-score: −3.51) and weight was 27 kg (z-score: −2.67), and at 15 years of age, height was 140 cm (z-score: −4.07) and weight remained at 27 kg (z-score: −3.15). Parental heights were 174 cm (father) and 162 cm (mother), yielding a calculated mid-parental target height of 174.5 cm.
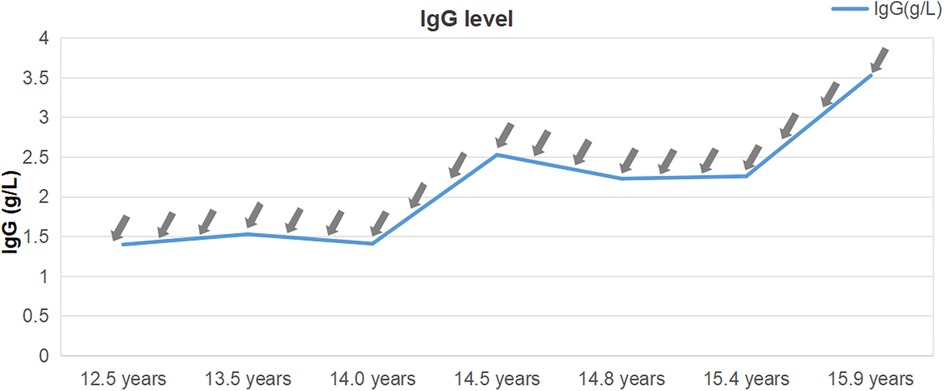
Figure 3. Immunoglobulin G levels from diagnosis to present. The immunoglobulin levels remained 1–4 g/L for a long period, notably below the reference range, despite receiving immunoglobulin G injections (0.5 mg/kg) every 2–3 months (indicated by grey arrows).
4 Literature review of patients with STAT3 GOF and ILD
Studies on STAT3 GOF mutation-associated ILD were comprehensively searched on PubMed up to December 31, 2024, using the search terms “STAT3,” “gain-of-function,” and “ILD.” We identified seven cases of STAT3 GOF-associated ILD treated using tocilizumab. Subsequently, we collected and analyzed the basic information, symptoms, treatments, and prognosis of these seven patients, including three males and four females, aged 2–16 years (Table 2). All patients exhibited three or more clinical phenotypes. Two of them were diagnosed with lymphocytic interstitial pneumonitis (LIP) on pathological examination (P3, P6). The earliest reported onset of ILD among them was at 3 months of age (5). This patient exhibited rapid ILD progression, culminating in acute respiratory distress syndrome by 12 months of age. Combination therapy with tocilizumab and ruxolitinib, augmented by extracorporeal membrane oxygenation support, significantly improved clinical and radiographic outcomes in ILD. One patient developed ILD at 15 years of age and declined targeted drug therapy (P7). Ultimately, the patient succumbed to progressive worsening of ILD and heart failure (6). The remaining six patients were treated with tocilizumab or a combination of JAK inhibitors. One patient was treated with a JAK inhibitor following the failure of tocilizumab but died of recurrent infections and pneumonia (P6). Among the remaining five patients, two were treated with tocilizumab alone, whereas the other three received combination therapy.
5 Discussion
IEIs are primarily caused by single gene mutations. The International Union of Immunological Societies Expert Committee has identified 583 distinct genetic mutation-induced immunodeficiency disorders, with the latest classification updated in 2024.
In an international cohort study, Leiding et al. (7) collected information of 191 patients (88 from Europe, 71 from the United States, and 32 from the rest of the world) with reported or new germline STAT3 GOF mutations. Patients with STAT3 GOF mutations predominantly presented with lymphoproliferation, characterized by elevated frequencies of double-negative (CD4− CD8−) T cells, autoimmune hematopenia, and hypogammaglobulinemia. Symptoms affecting the endocrine, digestive, and respiratory systems were common, whereas the involvement of the nervous and cardiovascular systems was generally less pronounced. Most patients presented with three or more disease phenotypes, and 43% of the patients had ILD, of which 26% also had bronchiectasis. Approximately 50% of the patients with ILD exhibited mutations in the DNA-binding domain at the genetic level. To date, no definitive evidence has been reported to supporting a genotype–phenotype correlation. However, in most cases, ILD progresses at a slow rate (8). Only a small number of patients experience infantile ILD, which is usually more aggressive (5, 9). STAT3 may be involved in pulmonary fibrosis through its role in fibroblast transformation, potentially contributing to the development of ILD in patients with STAT3 GOF (10). Various cytokines activate STAT3. Specifically, IL-6 binds to its corresponding receptors on the cell membrane, triggering downstream JAK phosphorylation, which in turn leads to STAT3 phosphorylation and homodimer formation (11, 12). The homodimeric STAT3 then enters the nucleus through the nuclear membrane and mediates RNA transcription (9, 13, 14). Abnormally activated STAT3 signaling promotes TGF-β-induced fibroblast activation and collagen release at the molecular level, potentially contributing to the persistence of ILD in patients (15). Notably, hyperactive STAT3 may disrupt growth hormone (GH) biosynthesis by forming heterodimers with STAT5, thereby interfering with STAT5-mediated GH synthesis pathways and ultimately leading to GH deficiency (16). Although the patient in our case exhibited normal height (50 cm) and weight (3.9 kg) at birth, the FTT observed during follow-up likely resulted from the synergistic effects of chronic malnutrition and underlying disease progression. Our patient also exhibited classic hematological abnormalities, including cytopenia and hypogammaglobulinemia, accompanied by arthritis and ILD. Although double-negative (CD4− CD8−) T cell quantification was not performed, the patient demonstrated disease-associated CD8+ T cell expansion alongside a reduction in CD4+ T cells, consistent with the typical immunophenotypic profile of this pathology (Table 1). The diagnostic delay prevented accurate assessment of the ILD onset timeline. Thoracic CT performed at our hospital demonstrated mediastinal displacement and bronchiectatic changes, highlighting the importance of early radiographic detection and prompt therapeutic initiation to mitigate disease progression.
Although clear and well-established treatment guidelines for this disease remain unavailable (17, 18), targeted therapies, such as tocilizumab and ruxolitinib, are preferred (19). JAK inhibitors or combination therapy could be more effective in controlling clinical symptoms (Table 2). However, one patient whose condition could not be controlled with tocilizumab alone died after switching to JAK inhibitors (Table 2). Owing to insufficient clinical data, the superiority of combination therapy remains unproven. JAK inhibitors are widely used to treat conditions associated with STAT3 GOF mutations. Our decision to administer tocilizumab was based on its proven effectiveness in controlling arthritis and ILD, which are common comorbidities in rheumatic and autoimmune disorders. In addition, JAK inhibitors are associated with severe adverse effects in the pediatric population. It may increase susceptibility to infections and potentiate adverse outcomes in the cardiovascular, gastrointestinal, and neurological systems. Notably, the patient exhibited significant improvements for both arthritis and ILD following tocilizumab treatment. Additionally, hematopoietic stem cell transplantation (HSCT) has emerged as a significant treatment option for cases progressing to severe conditions such as severe immunodeficiency, refractory cytopenia, and high malignancy risk (20). A previous international study reported a survival rate of 61% among 18 patients with STAT3 GOF mutations following HSCT, with infectious complications and graft-versus-host disease being the primary causes of mortality (21). The patient in our case remains clinically stable with tocilizumab therapy, and HSCT is not being considered at this time.
In conclusion, the clinical heterogeneity of the disease, coupled with limited current understanding, often results in misdiagnosis and underdiagnosis. When STAT3 GOF is suspected, early WES should be prioritized. The timely administration of tocilizumab and JAK inhibitors is essential for patients with ILD. When disease control is inadequate, combining tocilizumab with JAK inhibitors may be considered as a preferred strategy. A deeper understanding of this disease will improve the detection rate, and we look forward to future therapeutic advances and more detailed mechanistic insights into this condition.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Children's Hospital of Nanjing medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
PZ: Conceptualization, Data curation, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. MZ: Investigation, Writing – original draft. YP: Investigation, Writing – original draft. JJ: Investigation, Methodology, Writing – original draft. ZF: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. HY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the National Key R&D Program of China (grant number 2021YFC2702000) and the National Natural Science Foundation of China (grant number 82271838).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2025.1577746/full#supplementary-material
References
1. Vogel TP, Leiding JW, Cooper MA, Forbes Satter LR. STAT3 gain-of-function syndrome. Front Pediatr. (2022) 10:770077. doi: 10.3389/fped.2022.770077
2. Atschekzei F, Traidl S, Carlens J, Schütz K, von Hardenberg S, Elsayed A, et al. JAK inhibitors to treat STAT3 gain-of-function: a single-center report and literature review. Front Immunol. (2024) 15:1400348. doi: 10.3389/fimmu.2024.1400348
3. Zhou Q, Chen D, Yu J, Zheng B, Zhou W, Jia Z, et al. A novel gain-of-function STAT3 variant in infantile-onset diabetes associated with multiorgan autoimmunity. Mol Genet Genomic Med. (2024) 12(2):e2407. doi: 10.1002/mgg3.2407
4. Mauracher AA, Eekels JJM, Woytschak J, van Drogen A, Bosch A, Prader S, et al. Erythropoiesis defect observed in STAT3 GOF patients with severe anemia. J Allergy Clin Immunol. (2020) 145(4):1297–301. doi: 10.1016/j.jaci.2019.11.042
5. Deng M, Li Y, Li Y, Mao X, Ke H, Liang W, et al. A novel STAT3 gain-of-function mutation in fatal infancy-onset interstitial lung disease. Front Immunol. (2022) 13:866638. doi: 10.3389/fimmu.2022.866638
6. Erdős M, Tsumura M, Kállai J, Lányi Á, Nyul Z, Balázs G, et al. Novel STAT-3 gain-of-function variant with hypogammaglobulinemia and recurrent infection phenotype. Clin Exp Immunol. (2021) 205(3):354–62. doi: 10.1111/cei.13625
7. Leiding JW, Vogel TP, Santarlas VGJ, Mhaskar R, Smith MR, Carisey A, et al. Monogenic early-onset lymphoproliferation and autoimmunity: natural history of STAT3 gain-of-function syndrome. J Allergy Clin Immunol. (2023) 151(4):1081–95. doi: 10.1016/j.jaci.2022.09.002
8. Fabre A, Marchal S, Barlogis V, Mari B, Barbry P, Rohrlich P-S, et al. Clinical aspects of STAT3 gain-of-function germline mutations: a systematic review. J Allergy Clin Immunol Pract. (2019) 7(6):1958–1969.e9. doi: 10.1016/j.jaip.2019.02.018
9. Sarfati E, Hadjadj J, Fusaro M, Klifa R, Grimaud M, Berteloot L, et al. Life-saving, dose-adjusted, targeted therapy in a patient with a STAT3 gain-of-function mutation. J Clin Immunol. (2021) 41(4):807–10. doi: 10.1007/s10875-020-00914-3
10. Ray S, Ju X, Sun H, Finnerty CC, Herndon DN, Brasier AR. The IL-6 trans-signaling-STAT3 pathway mediates ECM and cellular proliferation in fibroblasts from hypertrophic scar. J Invest Dermatol. (2013) 133(5):1212–20. doi: 10.1038/jid.2012.499
11. Silva-Carmona M, Vogel TP, Marchal S, Guesmi M, Dubus J-C, Leroy S, et al. Successful treatment of interstitial lung disease in STAT3 gain-of-function using JAK inhibitors. Am J Respir Crit Care Med. (2020) 202(6):893–7. doi: 10.1164/rccm.201906-1204LE
12. Forbes LR, Vogel TP, Cooper MA, Castro-Wagner J, Schussler E, Weinacht KG, et al. Jakinibs for the treatment of immune dysregulation in patients with gain-of-function signal transducer and activator of transcription 1 (STAT1) or STAT3 mutations. J Allergy Clin Immunol. (2018) 142(5):1665–9. doi: 10.1016/j.jaci.2018.07.020
13. Milner JD, Vogel TP, Forbes L, Ma CA, Stray-Pedersen A, Niemela JE, et al. Early-onset lymphoproliferation and autoimmunity caused by germline STAT3 gain-of-function mutations. Blood. (2015) 125(4):591–9. doi: 10.1182/blood-2014-09-602763
14. Sediva H, Dusatkova P, Kanderova V, Obermannova B, Kayserova J, Sramkova L, et al. Short stature in a boy with multiple early-onset autoimmune conditions due to a STAT3 activating mutation: could intracellular growth hormone signalling be compromised? Horm Res Paediatr. (2017) 88(2):160–6. doi: 10.1159/000456544
15. Dees C, Pötter S, Zhang Y, Bergmann C, Zhou X, Luber M, et al. TGF-β–induced epigenetic deregulation of SOCS3 facilitates STAT3 signaling to promote fibrosis. J Clin Invest. (2020) 130(5):2347–63. doi: 10.1172/JCI122462
16. Gutiérrez M. Activating mutations of STAT3: impact on human growth. Mol Cell Endocrinol. (2020) 518:110979. doi: 10.1016/j.mce.2020.110979
17. Gadina M, Le MT, Schwartz DM, Silvennoinen O, Nakayamada S, Yamaoka K, et al. Janus kinases to jakinibs: from basic insights to clinical practice. Rheumatology. (2019) 58:i4–i16. doi: 10.1093/rheumatology/key432
18. Kang S, Tanaka T, Narazaki M, Kishimoto T. Targeting interleukin-6 signaling in clinic. Immunity. (2019) 50(4):1007–23. doi: 10.1016/j.immuni.2019.03.026
19. Faletti L, Ehl S, Heeg M. Germline STAT3 gain-of-function mutations in primary immunodeficiency: impact on the cellular and clinical phenotype. Biomed J. (2021) 44(4):412–21. doi: 10.1016/j.bj.2021.03.003
20. López-Nevado M, González-Granado LI, Ruiz-García R, Pleguezuelo D, Cabrera-Marante O, Salmón N, et al. Primary immune regulatory disorders with an autoimmune lymphoproliferative syndrome-like phenotype: immunologic evaluation, early diagnosis and management. Front Immunol. (2021) 12:671755. doi: 10.3389/fimmu.2021.671755
21. Bakhtiar S, Fekadu J, Seidel MG, Gambineri E on behalf of Inborn Errors Working Party Group of the EBMT. Allogeneic Hematopoietic Stem Cell Transplantation for Congenital Immune Dysregulatory Disorders [2296–2360 (Print)].
Keywords: STAT3, gain-of-function, inborn error of immunity, interstitial lung disease, tocilizumab
Citation: Zhou P, Zhu M, Pan Y, Jin J, Fan Z and Yu H (2025) Successful anti-IL-6 treatment for interstitial lung disease associated with STAT3 gain-of-function: a case report and literature review. Front. Pediatr. 13:1577746. doi: 10.3389/fped.2025.1577746
Received: 16 February 2025; Accepted: 23 June 2025;
Published: 9 July 2025.
Edited by:
Samuele Naviglio, Institute for Maternal and Child Health Burlo Garofolo (IRCCS), ItalyReviewed by:
Filippo Consonni, Azienda Ospedaliera Universitaria Meyer IRCCS—Firenze, ItalyAndrés Caballero-Oteyza, Hannover Medical School, Germany
Alessandro Amaddeo, Institute for Maternal and Child Health Burlo Garofolo (IRCCS), Italy
Copyright: © 2025 Zhou, Zhu, Pan, Jin, Fan and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhidan Fan, emhpZGFuZmFuQG5qbXUuZWR1LmNu; Haiguo Yu, aGFpZ3VvX3l1QG5qbXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship.
 Peng Zhou
Peng Zhou Meifang Zhu†
Meifang Zhu† Jing Jin
Jing Jin Haiguo Yu
Haiguo Yu