- 1College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, China
- 2Department of Pediatric Surgery, Fujian Children’s Hospital (Fujian Branch of Shanghai Children’s Medical Center), College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, China
- 3Fujian Maternity and Child Health Hospital College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, China
Purpose: The aim of this study was to explore the relationship between excessive sugar intake and symptoms of paediatric overactive bladder (OAB).
Methods: Clinical data was collected from 97 patients diagnosed with OAB at our hospital between July 2024 and January 2025. The relationships between sugar intake and OAB symptom scores were analysed.
Results: A total of 97 children diagnosed with OAB were included in this study, with 78 (80.41%) exhibiting excessive sugar intake and 19 (19.59%) exhibiting non-excessive sugar intake. Patients in the excessive sugar intake group had a significantly longer duration of OAB symptoms compared to those in the non-excessive sugar intake group (P < 0.05). A comparison of OAB symptoms between the two groups revealed that patients in the excessive sugar intake group had significantly higher total scores on the overactive bladder symptom score (OABSS) and higher scores for daytime urinary frequency, urgency frequency, and urgency urinary incontinence compared to those in the non-excessive sugar intake group (P < 0.05). Correlation analysis between sugar intake and OAB symptoms revealed significant positive correlations between average daily total sugar intake and the symptom duration of OAB, OABSS total score, daytime urination frequency score, urgency frequency score, and urgency urinary incontinence score (P < 0.05). The duration of excessive sugar intake was significantly positively correlated with the symptom duration of OAB, OABSS total score, and urgency urinary incontinence score (P < 0.05). The average daily sugar intake from fruits was also significantly positively correlated with the symptom duration of OAB, OABSS total score, daytime urination frequency score, urgency frequency score, and urgency urinary incontinence score (P < 0.05).
Conclusion: Excessive sugar intake was closely associated with the severity of OAB symptoms in children. Both the quantity of sugar intake and the duration of excessive sugar intake were positively correlated with the severity of OAB symptoms. Among all types of sugary foods consumed, the average daily intake of fructose was positively correlated with the severity of OAB symptoms.
Introduction
Overactive bladder (OAB) is an extremely common functional bladder disorder during childhood. According to the definition of the International Children's Continence Society, OAB is characterized by urgency, increased urinary frequency, and nocturnal enuresis, and it may or may not be associated with daytime incontinence in the absence of urinary tract infection or other identifiable neurogenic pathology (1). The persistent and recurrent nature of this condition, coupled with the distressing experience of uncontrollable urgency and wetting accidents, significantly impairs the quality of life of affected children (2). In recent years, the prevalence of OAB in children has been increasing, with reported rates ranging from 5% to 12% (3, 4).
The pathogenesis of paediatric OAB remains unclear. The latest expert consensus on paediatric OAB suggests that the condition may be associated with various factors, including: improper toileting habits, obesity, and hormonal metabolic imbalances (5, 6). Additionally, recent studies have indicated that changes in lifestyle and dietary habits, particularly the increased consumption of sugary beverages, are significant contributors to the development of OAB in adults (7). However, research examining the correlation between excessive sugar intake and OAB in children remains limited both domestically and internationally. Our team has proposed the scientific hypothesis that excessive sugar intake is closely associated with symptoms of paediatric OAB. The aim of this study was to explore the relationship between excessive sugar intake and symptoms of paediatric OAB by analysing the associations between sugar intake and objective measures of OAB symptom scores.
Methods
Clinical data were collected from 97 patients diagnosed with OAB at our hospital between July 2024 and January 2025. The data included age, sex, body mass index (BMI), duration of OAB symptoms, age at which diapers were discontinued, sugar intake (including total sugar intake, duration of excessive sugar intake, and daily sugar intake from various sugary foods), OAB symptom scores, maximum urinary flow rate, and average urinary flow rate. The non-invasive urine flow rate was measured via urodynamic detection equipment (Laborie, China), and the maximum and average urine flow rates were recorded. During testing, bladder volume was required to reach at least 50% of the child's expected bladder capacity.
The inclusion criteria were as follows: (1) children diagnosed with OAB and (2) aged between 4 and 18 years. The exclusion criteria were as follows: (1) inability to cooperate with the study, (2) current urinary tract infection, (3) neurogenic bladder, (4) history of urethral injury or surgery, (5) lower urinary tract malformation, and (6) refusal to participate in the study.
The diagnostic criteria for OAB include the following: (1) daytime frequency of urination exceeding 12 times per day, (2) presence of symptoms, including urgent urinary incontinence and nocturnal enuresis, (3) postvoid residual examination showing less than 20 ml of residual urine in the bladder, and (4) absence of other neurological bladder diseases and no evidence of urinary tract infection (8).
The overactive bladder symptom score (OABSS) was used to collectively express OAB symptoms (9). The score consists of 4 questions: (1) “How many times do you typically urinate from waking in the morning until sleeping at night?” (2) “How many times do you typically wake up to urinate from sleeping at night until waking in the morning?” (3) “How often do you have a sudden desire to urinate, which is difficult to defer?” (4) “How often do you leak urine because you cannot defer the sudden desire to urinate?” A higher score corresponds to a greater severity of symptoms. OABSS ≤5 was classified as mild, 6≤ OABSS ≤11 was classified as moderate, and OABSS ≥12 was classified as severe.
The criterion for excessive sugar intake was based on the recommendations of the Dietary Guidelines for Chinese Residents (10). Excessive sugar intake in children was defined as an average daily sugar intake of ≥50 g. To categorize the types of sugar intake, we recorded the most frequently consumed sugary foods in the week preceding the clinic visit. These were classified into the following categories: carbonated beverages, fruit juices (including apple, orange, grape, and watermelon juices), fruits (including apples, grapes, oranges, and watermelons), other sugary drinks (e.g., yogurt-based drinks), sugary tea beverages, chocolate, and ice cream. To accurately calculate the average daily sugar intake of the children, we adopted the methodology of Maserejian et al. (11) and utilized the food composition table from the open-source database of the Zhejiang University AI and Nutritional Big Data Research Center (https://nutrition.zju.edu.cn).
Statistical analysis
Statistical analysis was performed using SPSS version 25.0. Continuous data are presented as medians and quartiles. Comparisons between groups of continuous variables with a normal distribution were performed with the t-test. Continuous variables without a normal distribution were compared using the Mann‒Whitney U-test. A paired t-test was used to compare the effects before and after treatment. Comparisons between groups of categorical variables were performed via the chi-square test. Correlation analysis was used to analyse the relationships between sugar intake (including average daily total sugar intake, duration of excessive sugar intake, and average daily sugar intake from the main types of sugary foods) and OAB symptoms (including symptom scores and symptom duration). A p-value of <0.05 was considered indicative of statistical significance.
Results
A total of 97 children diagnosed with OAB were included in this study, with 78 (80.41%) exhibiting excessive sugar intake and 19 (19.59%) exhibiting non-excessive sugar intake. The children were divided into two groups based on their sugar consumption (excessive or non-excessive). Comparisons of clinical data between the excessive sugar intake group and the non-excessive sugar intake group revealed no significant differences in sex, age, BMI, age at which daytime diapers were discontinued, age at which nighttime diapers were discontinued, average urinary flow rate, or maximum urinary flow rate. However, patients in the excessive sugar intake group had a significantly longer duration of OAB symptoms compared to those in the non-excessive sugar intake group (P < 0.05) (Table 1).
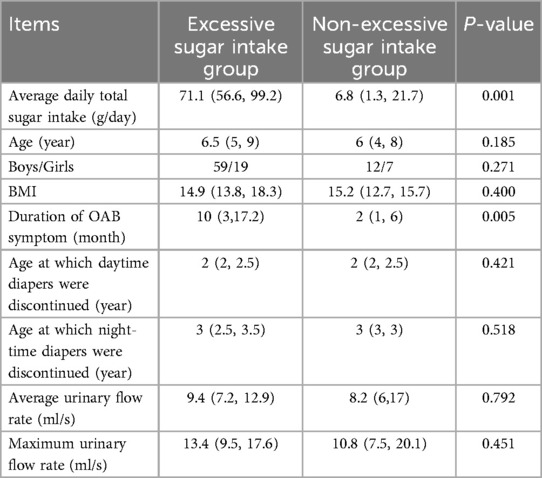
Table 1. Comparison of clinical data of patients with OAB in the excessive sugar intake group and non-excessive sugar intake group.
A comparison of OAB symptoms between the two groups revealed that patients in the excessive sugar intake group had significantly higher total scores on the OABSS, as well as higher scores for daytime urination frequency, urgency frequency, and urgency urinary incontinence compared to those in the non-excessive sugar intake group (P < 0.05). A comparison of the severity grading of OAB symptoms also revealed that patients in the excessive sugar intake group had more severe OAB symptoms than those in the non-excessive sugar intake group (P < 0.05). No significant difference was observed in the number of nocturnal urinations between the two groups (Table 2).
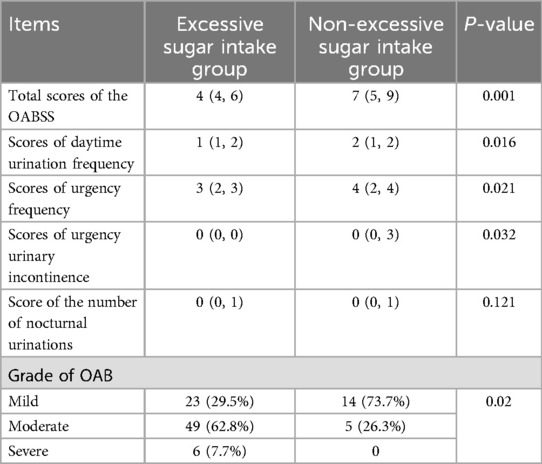
Table 2. Comparison of OABss scale score of patients with OAB in the excessive sugar intake group and non-excessive sugar intake group.
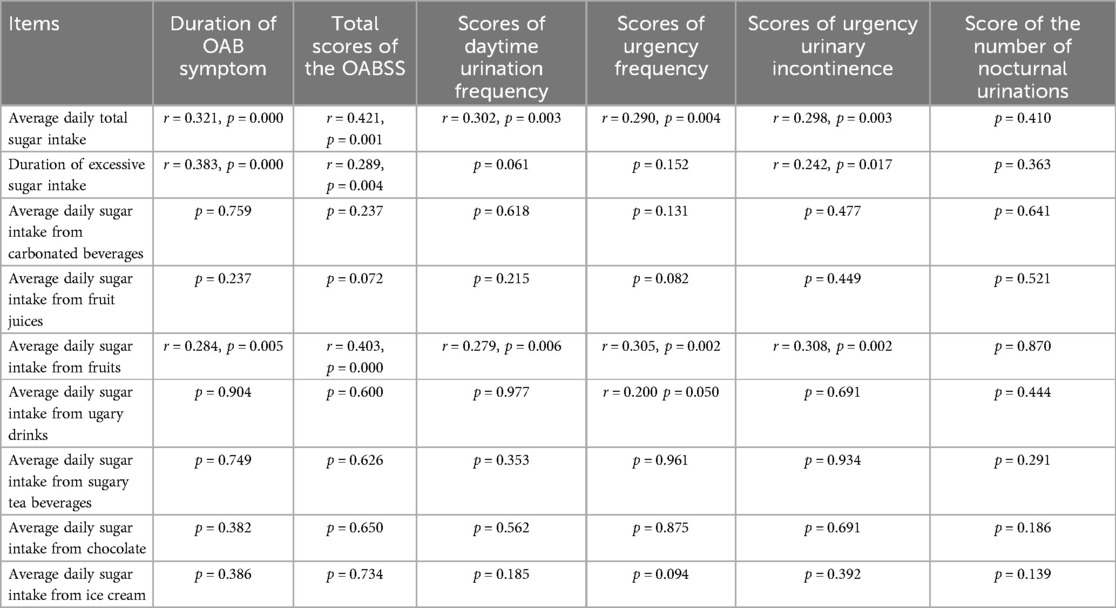
Correlation analysis between sugar intake and OAB symptoms revealed significant positive correlations between average daily total sugar intake and the symptom duration of OAB, OABSS total score, daytime urination frequency score, urgency frequency score, and urgency urinary incontinence score (P < 0.05). The duration of excessive sugar intake was significantly positively correlated with the symptom duration of OAB, OABSS total score, and urgency urinary incontinence score (P < 0.05). The average daily sugar intake from fruits was also significantly positively correlated with the symptom duration of OAB, OABSS total score, daytime urination frequency score, urgency frequency score, and urgency urinary incontinence score (P < 0.05). In contrast, no significant correlations were observed between OAB symptoms and average daily sugar intake from other sources, including carbonated beverages, fruit juices, sugary drinks, sugary tea beverages, chocolate, and ice cream (P > 0.05) (Table 3).
Discussion
OAB is a common functional bladder disorder in children, with an incidence rate as high as 9.01% among Chinese children. Recent studies reported that obesity, primary nocturnal enuresis, constipation, excessive diaper dependence, bladder–bowel dysfunction, hormonal metabolic disorders, and psychological factors may be associated with the development of OAB (12–14). However, the exact aetiology of OAB remains unclear.
Flores MV et al. (15) reported that insulin resistance and excessive succinate intake are associated with OAB in women with metabolic syndrome. A short-term randomized cohort study by Firouzmand S et al. (16) revealed a direct link between urinary ATP and NO levels and the severity of urinary frequency and urgency symptoms in adult OAB patients. Peyronnet et al. (17) further reported that OAB induced by metabolic syndrome is refractory to traditional anticholinergic therapy and sacral neuromodulation. These studies collectively suggested that high sugar intake leading to metabolic syndrome and insulin resistance can induce OAB in adults and rats. However, these studies have focused primarily on adults, and there is currently a lack of both clinical and basic research data on OAB induced by excessive sugar intake in children. We performed this study to explore the relationship between excessive sugar intake and the occurrence of OAB symptoms in children. Our results revealed that patients in the excessive sugar intake group had significantly higher total OABSS scores, as well as higher scores for daytime urination frequency, urgency frequency, and urgency urinary incontinence compared to those in the non-excessive sugar intake group (P < 0.05). Correlation analysis between sugar intake and OAB symptoms revealed significant positive correlations between average daily total sugar intake and symptom duration of OAB, OABSS total score, daytime urination frequency score, urgency frequency score, and urgency urinary incontinence score (P < 0.05). The duration of excessive sugar intake was significantly positively correlated with the symptom duration of OAB, OABSS total score, and urgency urinary incontinence score (P < 0.05). These findings suggest that, similar to the results of previous studies in adults, excessive sugar intake may also be an important factor contributing to OAB in children.
To further investigate the impact of daily sugar intake from different food sources on OAB symptoms, we found that the average daily sugar intake from fruits was significantly positively correlated with the symptom duration of OAB, OABSS total score, daytime urination frequency score, urgency frequency score, and urgency urinary incontinence score in children with OAB (P < 0.05). This association may be related to the effects of fructose (the primary sugar component in fruits) on bladder contractility and stability. In recent years, basic research on the effects of fructose on smooth muscle function has increased. Aimaretti et al. (18) reported that different muscle tissues adapt differently to high-fructose diets and speculated that bladder dysfunction might be associated with mitochondrial dysfunction caused by oxidative stress. Lee et al. (19) recently demonstrated that a high-fructose diet during the postpartum period could induce metabolic syndrome and OAB symptoms in adult mice, with the effects being positively correlated with fructose intake and mediated through specific signalling pathways that affect the relaxation function of the bladder detrusor muscle.
Our study has several limitations. First, this was a single-centre study with a limited number of OAB patients, and the effects of daily sugar intake from some food sources on clinical symptoms may not have reached statistical significance. In particular, the small number of patients with non-excessive sugar intake may introduce bias into the results. Second, the range of food types considered in this study was limited, and potential confounding factors, such as the consumption of small amounts of caffeine in carbonated beverages, may have influenced the results. Third, all participants in this study were patients diagnosed with OAB, and there was no control group of children without OAB. Therefore, while this study can assess the relationship between excessive sugar intake and the severity of OAB symptoms, it cannot be used to determine whether this relationship is related to the occurrence of OAB. In the next phase of the research, we will include a control group to further evaluate the correlation between excessive sugar intake and the development of OAB. Fourth, although children with OAB have lower water intake compared to healthy children, hydration status can influence bladder symptoms. This study did not record the water intake of each child, which may have affected our results. To increase the accuracy and objectivity of future findings, we will include water intake data in future studies.
Conclusion
Excessive sugar intake was closely associated with the severity of OAB symptoms in children. Both the quantity of sugar intake and the duration of excessive sugar intake were positively correlated with the severity of OAB symptoms. Among all types of sugary foods consumed, the average daily intake of fructose was positively correlated with the severity of OAB symptoms. This study provides a scientific basis for the use of sugar-restricted diets in children with OAB and offers novel insights for the treatment of paediatric OAB.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author. Requests to access these datasets should be directed to Xu CuiMTY4MDI5MzdAcXEuY29t.
Ethics statement
The studies involving humans were approved by Fujian Children's Hospital (Fujian Branch of Shanghai Children's Medical Center). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
XC: Conceptualization, Data curation, Funding acquisition, Methodology, Writing – original draft. B-CW: Data curation, Methodology, Project administration, Software, Writing – original draft. Z-QC: Data curation, Methodology, Software, Writing – original draft. L-YX: Investigation, Methodology, Validation, Writing – original draft. B-QY: Investigation, Software, Writing – original draft. C-MZ: Conceptualization, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the General Project of Fujian Natural Science Foundation (No. 2024J011124), Health Science and Technology Program of Fujian Province (2024QNB005), and Sponsored by Fujian Medical University (2023QH1239).
Acknowledgments
We thank all doctors in our center and Liang Zheng from Shanghai Children's Medical Center for their fruitful advice and discussions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
OAB, overactive bladder; OABSS, overactive bladder symptom score; BMI, body mass index.
References
1. Franco I. Overactive bladder in children. Nat Rev Urol. (2016) 13(9):520–32. doi: 10.1038/nrurol.2016.152
2. Savaser S, Kizilkaya Beji N, Aslan E, Gozen D. The prevalence of diurnal urinary incontinence and enuresis and quality of life: sample of school. Urol J. (2018) 15(4):173–9. doi: 10.22037/uj.v0i0.3982
3. Linde JM, Nijman RJM, Trzpis M, Broens PMA. Prevalence of urinary incontinence and other lower urinary tract symptoms in children in The Netherlands. J Pediatr Urol. (2019) 15(2):164.e1–7. doi: 10.1016/j.jpurol.2018.10.027
4. Shrestha N, Sahukhala S, Diva KC, Sandalcidi D, Adhikari SP. Prevalence of urinary incontinence in school going children: a cross-sectional study. J Nepal Health Res Counc. (2021) 18(4):676–80. doi: 10.33314/jnhrc.v18i4.2506
5. Chinese Society of Pediatric Urodynamics and Pelvic Floor. China Expert consensus of diagnosis and treatment of urinary incontinence in children (2024 edition). J Clin Pediatr Surg. (2024) 23(3):201–9.
6. Chinese Society of Pediatric Urodynamics and Pelvic FloorChinese Society of Pediatric Surgery, Chinese Medical Association. Chinese Expert consensus on diagnosis and treatment of overactive bladder in children. Chin J Med. (2021) 101(40):3278–86.
7. Turmel N, Hentzen C, Chesnel C, Charlannes A, Le Breton F, Amarenco G. Alimentation, régimes et diététique dans le syndrome clinique d’hyperactivité vésicale: revue de la littérature [food, diet and dietetic in treatment of urinary tract dysfunctions. A review]. Prog Urol. (2017) 27(7):395–401. doi: 10.1016/j.purol.2017.05.001
8. Tekgul S, Stein R, Bogaert G, Undre S, Nijman RJM, Quaedackers J, et al. EAU-ESPU guidelines recommendations for daytime lower urinary tract conditions in children. Eur J Pediatr. (2020) 179(7):1069–77. doi: 10.1007/s00431-020-03681-w
9. Homma Y, Yoshida M, Seki N, Yokoyama O, Kakizaki H, Gotoh M, et al. Symptom assessment tool for overactive bladder syndrome–overactive bladder symptom score. Urology. (2006) 68(2):318–23. doi: 10.1016/j.urology.2006.02.042
10. Chinese Journal of Nutrition. The Chinese dietary guidelines for residents (2022) was released in Beijing. Chin J Health Sci. (2022) 44(6):521–2.
11. Maserejian NN, Wager CG, Giovannucci EL, Curto TM, McVary KT, McKinlay JB. Intake of caffeinated, carbonated, or citrus beverage types and development of lower urinary tract symptoms in men and women. Am J Epidemiol. (2013) 177(12):1399–410. doi: 10.1093/aje/kws411
12. Xing D, Wang YH, Wen YB, Li Q, Feng JJ, Wu JW, et al. Prevalence and risk factors of overactive bladder in Chinese children: a population-based study. Neurourol Urodyn. (2020) 39(2):688–94. doi: 10.1002/nau.24251
13. Liang X, Hu HJ, Zhang ZW, Dou QF, Song CP, Lu CB, et al. Prevalence of overactive bladder in female university freshmen and its psychological impact. Chin J Urol. (2020) 41(12):931–5.
14. Xu PC, Wen YB, Shang XP, Wang XZ, Wang YH, Zhou W, et al. Effect of using diapers on the incidence of bladder and rectal dysfunction in children. Chin J Pediatr Surg. (2019) 40(8):723–7.
15. Velasquez Flores M, Mossa AH, Cammisotto P, Campeau L. Succinate decreases bladder function in a rat model associated with metabolic syndrome. Neurourol Urodyn. (2018) 37(5):1549–58. doi: 10.1002/nau.23488
16. Firouzmand S, Young JS. A pilot study to investigate the associations of urinary concentrations of NO, ATP and derivatives with overactive bladder symptom severity. Exp Physiol. (2020) 105(6):932–9. doi: 10.1113/EP088450
17. Peyronnet B, Mironska E, Chapple C, Cardozo L, Oelke M, Dmochowski R, et al. A comprehensive review of overactive bladder pathophysiology: on the way to tailored treatment. Eur Urol. (2019) 75(6):988–1000. doi: 10.1016/j.eururo.2019.02.038
18. Aimaretti E, Chimienti G, Rubeo C, Di Lorenzo R, Trisolini L, Dal Bello F, et al. Different effects of high-fat/high-sucrose and high-fructose diets on advanced glycation End-product accumulation and on mitochondrial involvement in heart and skeletal muscle in mice. Nutrients. (2023) 15(23):4874. doi: 10.3390/nu15234874
Keywords: overactive bladder, child, OABSS, sugar intake, types of sugary foods
Citation: Cui X, Wei B-C, Chen Z-Q, Xu L-Y, Yin B-Q and Zhou C-M (2025) Correlation between excessive sugar intake and overactive bladder in children. Front. Pediatr. 13:1581852. doi: 10.3389/fped.2025.1581852
Received: 23 February 2025; Accepted: 24 April 2025;
Published: 8 May 2025.
Edited by:
Alberto Parente, Reina Sofia University Hospital, SpainReviewed by:
Sibel Tiryaki, Ege University, TürkiyeShuai Yang, First Affiliated Hospital of Zhengzhou University, China
Copyright: © 2025 Cui, Wei, Chen, Xu, Yin and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chao-Ming Zhou, ZmpzZXR5eXpjbUAxNjMuY29t
 Xu Cui1,2,3
Xu Cui1,2,3 Long-Yao Xu
Long-Yao Xu Chao-Ming Zhou
Chao-Ming Zhou