- Centro de Investigación Traslacional, Instituto Nacional de Pediatría, Mexico City, Mexico
Background: Appendicitis is the most common abdominal emergency in pediatrics and is suggested as a quality indicator for timely access to care in time-sensitive conditions. Despite advances in diagnostics, the incidence of complicated appendicitis (CA) remains high due to delays in pediatric surgical care, which can increase disease severity. Social vulnerability has been associated with surgical access, particularly in low- and middle-income populations. This study examines the relationship between surgical delay and social determinants of complicated appendicitis in children without social security in the Metropolitan Zone of México.
Methods: This retrospective cohort study was conducted in a pediatric public hospital. Consecutive cases from 2018 to 2021 with confirmed appendicitis diagnoses were included. The primary outcome variable was the type of appendicitis (acute/complicated), while two independent variables were the time of evolution (patient and hospital timing) and socioeconomic factors associated with social vulnerability. A logistic regression analysis assessed the relationship between appendicitis type and covariates.
Results: A total of 943 pediatric cases of appendicitis were included. Out of these, 62.67% presented CA, with a mean age 10 ± 4 years. 60.9% were well-nourished, and 16% had at least one comorbidity. Most subjects (76%) met at least two criteria for social vulnerability, and 74.7% of families held unskilled jobs. The median symptom-to-admission time was 2 days, with a median hospital-to-surgery time of 19.5 h (p25–p75). Prehospital delays affected 57.8% of cases (n = 545), and 39% (n = 365) experienced intrahospital delays. In the multivariable logistic regression, prehospital delay ≥48 h (OR 3.27, 95% CI 2.43–4.39) and children under 5 years (OR 1.76, 95% CI 1.09–2.84) were associated with higher odds of CA.
Conclusion: The high frequency of CA in uninsured children at a public hospital is due to surgical delays of two or more days. Social vulnerabilities, as observed globally, hinder access to quality care. Thus, appendicitis should be recognized as both a medical and social issue, requiring a comprehensive approach that addresses social vulnerability.
1 Introduction
Appendicitis is the most common abdominal emergency in pediatrics (1, 2), where age and delays in accessing healthcare are the most consistent clinical risk factors influencing the disease's natural progression (3). Consequently, some authors have proposed it as a key quality indicator for access to emergency care for time-dependent conditions (4, 5).
Despite technological advances and substantial progress in the diagnostic evaluation of children with suspected appendicitis, the incidence of complicated appendicitis (CA) has not declined over time (6, 7). Access to pediatric surgical care is often associated with delays in diagnosis and treatment, which can lead to increased disease severity (8, 9). Among these factors, surgical delay is identified as the primary risk factor for complicated cases (10).
The disparity in access to surgical care is linked to outcomes in pediatric appendicitis. Barriers related to this disparity in healthcare systems are evaluated through social vulnerability, a set of standardized indexes based on social and individual risk indicators tailored to each population (11). Over the years, these indexes have been strongly associated with access to surgical care (10). According to the International Labor Organization, there is a global crisis due to the lack of social protection (12), which disproportionately impacts low- and middle-income countries (13). This situation creates barriers to accessing healthcare, such as out-of-pocket expenses, longer distances to medical facilities, limitations in the range of available services, low quality, poor acceptability of services, and long waiting times (14).
In Mexico, access to social protection is intricately linked to employment status, determining the public or private healthcare options available to individuals. Unfortunately, public healthcare services often fail to meet the needs of many users (15). Previous reports estimated that 40%–60% of the Mexican population lacks access to these services (15, 16), which are provided through the public healthcare system for the uninsured. Despite government efforts to reform this fragmented system, there has been no substantial documentation of changes in access to health services (17). In this context, it is important to investigate the frequency of complications in this surgical abdominal emergency among children of uninsured households. To address this, we analyzed the relationship between surgical delays and the social vulnerability of families, focusing on children diagnosed with CA who visited the emergency department of a hospital with a high volume of pediatric surgeries between 2018 and 2021.
2 Methods
2.1 Study design
This retrospective cohort study was conducted in a high-volume pediatric public hospital in Mexico City that primarily serves a population without social security. The primary sources of information were institutional databases and electronic records. The health research committees approved the protocol, registration number 069/2022. The report followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (18).
2.2 Data source
Five institutional databases were utilized: the “Hospital Administration System” under the “Surgery Control” section, “Electronic Medical Record”, “Emergency Admission Register”, “Death Control”, and “Socioeconomic Study” from January 1, 2018, to December 31, 2021. The databases were linked, and the records were anonymized for data curation and analysis.
2.3 Study population
This study included subjects aged 1–18 years who met the following criteria: postoperative diagnosis of appendectomy and histopathological reports that included samples of the cecal appendix. Cases with a clinical diagnosis of appendicitis were confirmed through histopathological examination. Exclusion criteria included subjects with a diagnosis of a normal cecal appendix, interval appendectomy, or incomplete information. All patients diagnosed with appendicitis were taken to the operating room directly from the emergency department, and according to hospital protocols, all patients received at least one dose of antimicrobial treatment before surgery.
2.4 Outcomes
The primary outcome was the classification of appendicitis as either acute appendicitis (AA) or complicated appendicitis (CA). This classification was determined based on the intraoperative clinical diagnosis recorded in the postoperative notes of each record, following the criteria defined by Cameron (19) and validated by McKie (20). The histological report was used to confirm the diagnosis of a normal appendix.
Independent variables included the time of evolution and socioeconomic factors associated with social vulnerability. The evaluation of the time of evolution included patient time, defined as the days from initial presentation to admission to the emergency department as reported by the primary caregiver, and hospital time, defined as the hours from admission to the emergency department until admission to the operating room (1). Prehospital delay was considered when subjects had two or more days of symptoms (1, 8), while intrahospital delay was defined as taking 24 or more hours to arrive at the operating room (1, 21).
Socioeconomic factors associated with social vulnerability were assessed and evaluated, including: (1) location of residence; (2) employment status, categorized as unemployed, unskilled, and skilled workers (22). Two indicators of social deprivation proposed by “Consejo Nacional de Evaluación la Política de Desarrollo Social” CONEVAL (16): Inadequate housing quality and overcrowding, which occur if the home exhibits at least one of the following characteristics: (a) floors made of mud; (b) roofs constructed from cardboard sheeting or waste materials; (c) walls made of mud, reed, bamboo, palm, cardboard sheeting, metal, or other waste materials; (d) overcrowding, defined as more than two persons per room (16); and lack of basic housing services, defined as having at least one of the following characteristics: (a) water obtained from a well, river, lake, stream, or pipe; or piped water acquired by carrying it from another home or from a public tap or hydrant; (b) lack of sewage service or drainage connected to a pipe leading to a river, lake, sea, ravine, or crevice; (c) lack of electricity; (d) use of firewood or charcoal for cooking or heating food (16).
2.5 Study covariates
Other data included: admission date (year/month), sex (male/female), age group (young children under 5 years, school-age 6–11 years, and adolescents 12–18 years), shift of admission to the emergency department (morning/afternoon/night), nutritional status (underweight/normal/overweight/obesity according to BMI percentiles in growth charts proposed by the Centers for Disease Control and Prevention) (23), comorbidity (presence of any coexisting disease before the diagnosis of appendicitis, as reported in your medical record), and antimicrobial treatment prior to admission to the emergency department (yes/no, type, dose, and duration).
2.6 Statistical analysis
For the descriptive analysis of time variables, medians and ranges were calculated. Clinical and socioeconomic variables were described using frequencies and proportions. The comparison between clinical and socioeconomic variables and the type of appendicitis was made using the Chi-square test. We compared clinical characteristics, socioeconomic factors, and time delays between types of appendicitis using univariable logistic regression with CA as the dependent variable. Finally, a binary logistic regression analysis was performed to assess the association between the time of evolution, socioeconomic factors, and clinical characteristics and the likelihood of classifying appendicitis. Variables included in the model were selected based on biological plausibility, potential confounders, and a p-value of less than 0.20 in bivariate analysis. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated.
3 Results
3.1 Study cohort and case selection
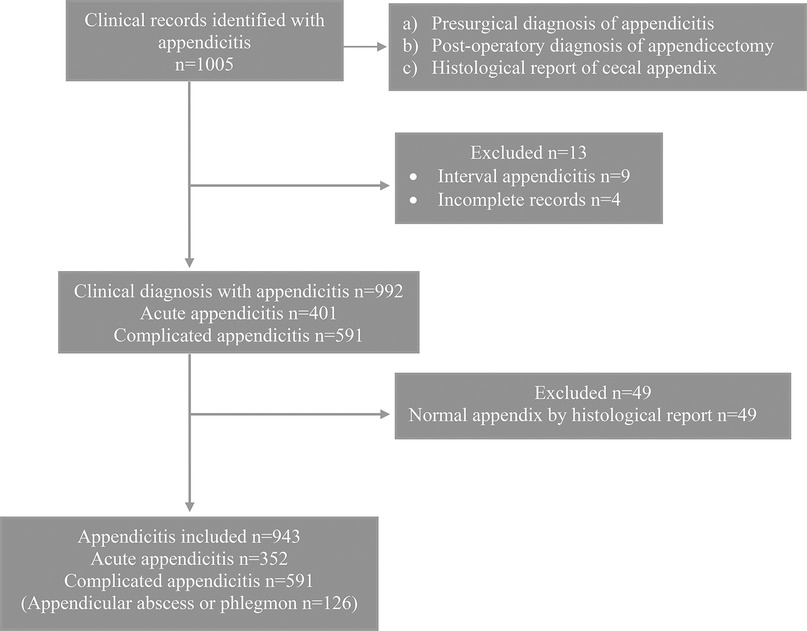
A total of 1,005 cases of appendicitis were identified between January 2018 and December 2021. An average of 21 appendectomies per month (±7.4) were performed, with a minimum of 16 (±8.3) in February 2020 and a maximum of 25.6 (±7.8) in June 2019. A total of 992 records of patients with appendicitis were included in the study, of which 401 were identified as having a diagnosis of AA. However, 49 were histologically identified as a normal appendix. Ultimately, 943 subjects were included in this study (Figure 1).
3.2 Population clinical characteristics
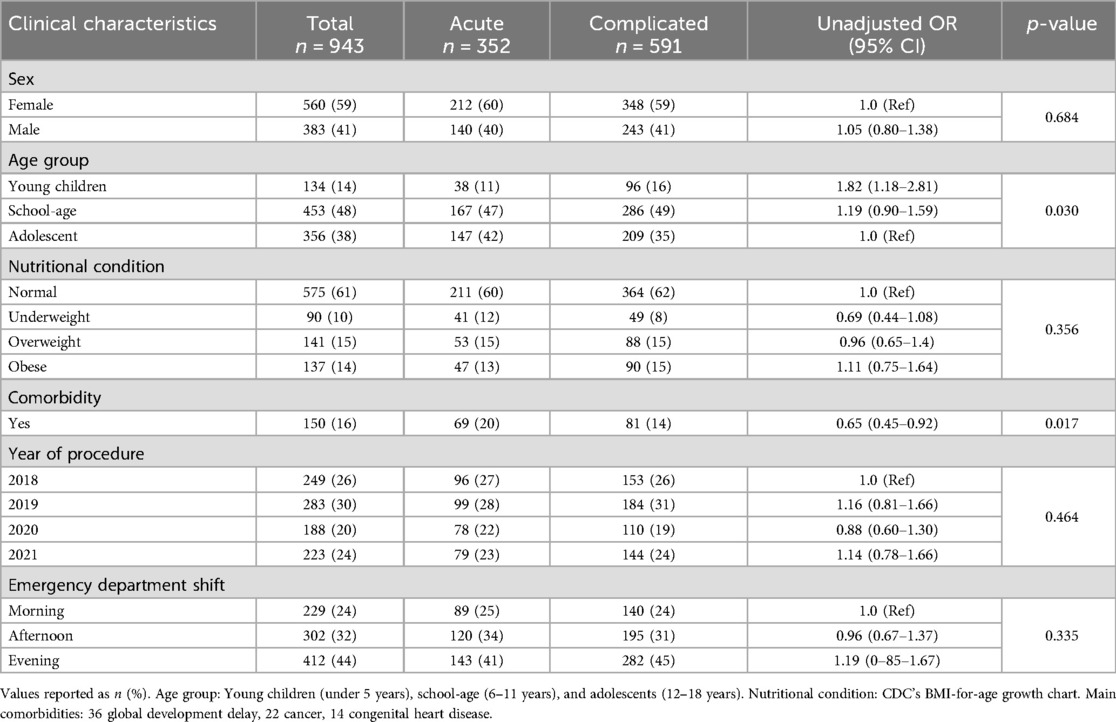
Of the 943 subjects included, 59.3% (560 subjects) were female, with a mean age of 10 years (±4). At the time of admission, 575 subjects (60.9%) exhibited a normal nutritional status. Comorbidities were identified in 150 subjects (16%), with the most common being global developmental delay 36 cases (3.8%), complete congenital heart defects 14 cases (1.5%), acute lymphoblastic leukemia in treatment 13 cases (1.4%), moderate persistent asthma 13 cases (1.4%), metabolic syndrome and obesity 8 cases (0.8%), systemic lupus erythematosus 5 cases (0.5%), Down syndrome 5 cases (0.5), autism spectrum disorder 4 cases (0.4%), central nervous system tumors 3 cases (0.3%), autoimmune diseases congenital 2 cases (1.3%) and various other morbidities (47 cases). Being in preschool or school was associated with a higher probability of CA, while the probability of having comorbidities was lower in patients with CA (OR 0.65, 95% CI 0.45–0.92) (Table 1).
3.3 Sociodemographic characteristics and social vulnerability
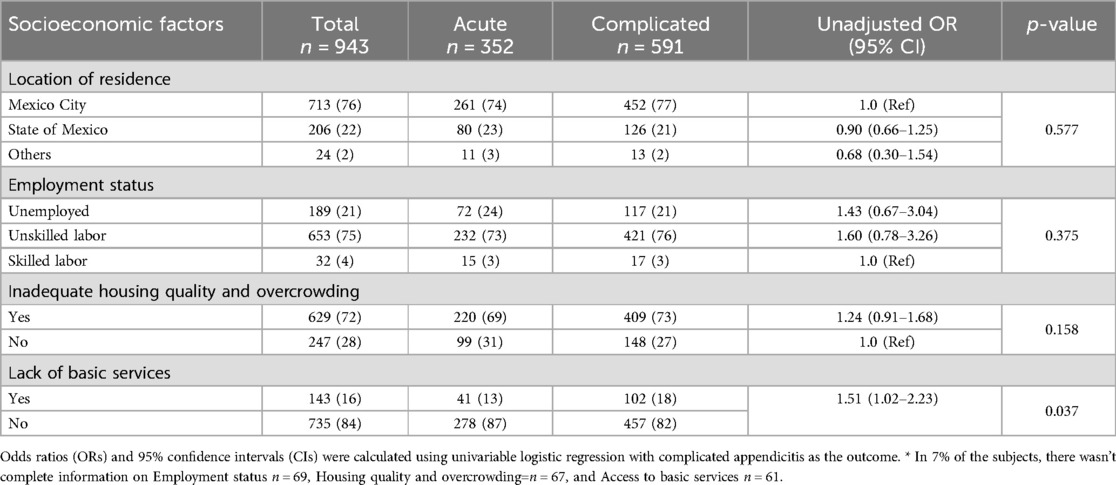
We identified 919 families (97.5%) living in the Metropolitan Zone of Mexico City, a geographic area comprising Mexico City and neighboring municipalities in the states of Mexico and Hidalgo (an area of 7,180 km2 inhabited by 20 million people). 453 families (48%) resided in the five most densely populated municipalities with the highest poverty levels in Mexico City. Due to the primary caregiver's status of employment, the households were uninsured. At the time of hospital admission, we identified that in 189 families (21.6%), the primary caregiver was unemployed, and in 653 families (74.7%), caregivers were engaged in unskilled jobs (Table 2). Finally, 719 households (76%) met at least one criterion of social vulnerability (16).
3.4 Role of delay among complicated appendicitis
Regarding the time of evolution of the population, the overall median time from the onset of symptoms to hospital admission (patient time) was 2 days (min 0–max 30). For patients with AA, the median was 1 day (min 0–max 8), while for CA, it was 2 days (min 0–max 30). The median time from hospital admission to the operating room (hospital time) was 19.5 h (min 1.1–max 137.2). For subjects with AA, it was 20.7 h (min 2.1–max 127.4), and for CA, it was 18.6 h (min 1.1–max 137.2). The prehospital delay was observed in 545 subjects, of whom 401 (67.8%) presented with CA. The intrahospital delay was observed in 365 patients (39%), with similar percentages in subjects with AA vs. CA (39.8% vs. 38%). The univariable logistic regression model for the likelihood of CA is presented in Table 3. Finally, the multivariate logistic regression model indicated that only young children and prehospital delay were associated with CA (Figure 2).
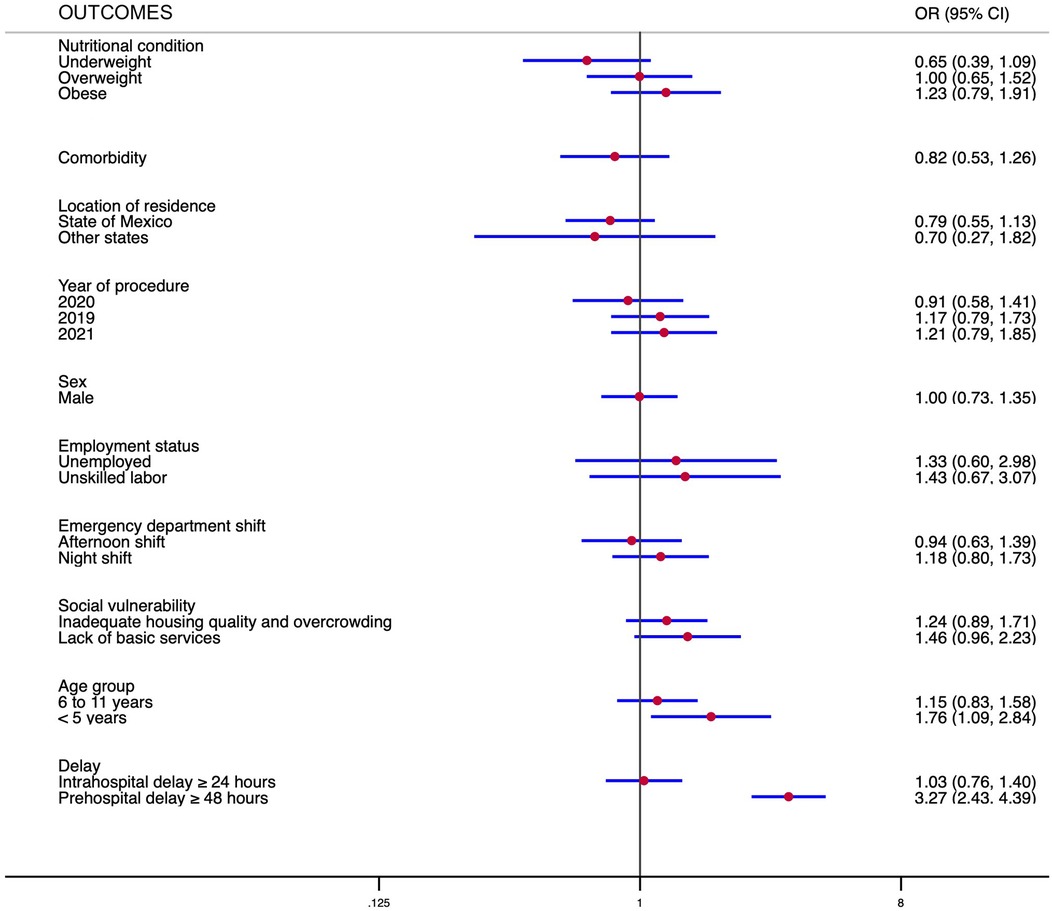
Figure 2. Multiple regression model examining the association between independent variables and covariates with complicated appendicitis. Foot note: Logistic regression, Log likelihood = −528.826, ch2(20) = 89.44, p < 0.000. Revealed significant findings: an increased risk for children under five years of age [odds ratio (OR) 1.76, 95% IC 1.09–2.84] and a prehospital delay of 48 h or more (OR 3.27, 95% CI 2.43–4.39).
4 Discussion
This study was conducted in a high-volume pediatric hospital that provides surgical care for children without social security in Mexico. It identified a high prevalence of CA that has not changed significantly, even during the COVID-19 pandemic. The proportion was higher than that reported in similar studies worldwide and in a series from Mexico City with comparable characteristics (24). The discrepancy in this outcome could be attributed to the population's social characteristics associated with delays in the diagnosis of appendicitis (25). In 1982, Luckmann R et al. proposed that AA and CA are distinct entities (26); since then, the proportion of CA as a hospital quality indicator for surgical care has been controversial (27). The geographic variability in the incidence rates of AA and CA (3, 28), favorable outcomes to medical treatment (29, 30), and differing gene expression profiles in children CA (31) support the hypothesis that using the proportion of CA as an indicator of institutional quality may not be appropriate.
A key finding in this study was the time elapsed from the onset of symptoms to hospital admission, which is the main risk factor associated with CA. This aligns with the first systematic review by Li et al. (9), which demonstrated that the incidence of CA is related to the total time from symptom onset to either admission or surgery. An updated systematic review by Calpin et al. (1). reported similar results, emphasizing (1) that the risk of complications decreases if patients undergo surgery within the first 24 h after hospital admission. This contrasts with our findings, as hospital delays did not increase the risk of CA This may be attributed to the fact that many patients already had CA due to delays in admission to the emergency department.
According to Bergmark RW (32), two understudied aspects when evaluating access to quality surgical care are when the patient recognizes the need to access the healthcare system and the process of contacting the surgeon who will address their condition. If the main identified risk was prehospital delay, there is sufficient evidence of the association between appendiceal perforation and factors attributable to the patient or those occurring before hospital admission.
Consistent with previous reports, the only risk factor for CA attributable to the patient was being under five years old, which remained significant in the adjusted risk analysis. Some authors associate age with the risk of delayed diagnosis, but the analysis of this population supports the hypothesis of independent risks. In clinical practice, we observe the need for a higher degree of suspicion (25), the difficulty in communicating symptoms, and the variability in the clinical presentation of appendicitis at this age (33). The findings of Dhillon BK regarding a dysregulated immune response in children with CA (31) could support our results.
A relevant limitation of this analysis was the exclusion of antibiotic use before the diagnosis of appendicitis from the risk model. Although we attempted to include this variable, the retrospective design introduced several biases in its measurement, so we decided to exclude it. Antibiotic stewardship is imperative in pediatric perforated appendicitis, although its impact has not yet been well studied (34). In cities such as ours, where we have documented excessive or inappropriate use of antibiotics (35), this factor could modify the evolution of children with appendicitis before they reach specialized care centers.
In children from high-income countries, the association between appendiceal perforation and social vulnerability, as well as barriers to accessing quality surgical care, is strong and consistent (36, 37). In Mexico, we lack comprehensive information on this association, primarily due to fragmented health coverage in both public and private systems and the absence of population data that could help us draw meaningful conclusions. Currently, it is recognized that 96.1% of the Mexican population has access to a hospital with the capacity to perform surgical procedures, based solely on their geographical location (38). However, the reality differs depending on the type of access to healthcare systems and socioeconomic factors associated with social vulnerability. In children from uninsured households, we observed a high frequency of CA, which was related to prehospital delay; consequently, when families contact the surgeon, the children often develop CA.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Health research committees approved the protocol, registration number 069/2022 at the National Pediatrics Hospital (Mexico City, Mexico). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
V-AE: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Funding acquisition. M-MK: Conceptualization, Data curation, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. A-GC: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing, Resources, Validation. G-OA: Conceptualization, Validation, Writing – original draft, Writing – review & editing, Formal analysis, Methodology, Software. G-ZJ: Conceptualization, Formal analysis, Methodology, Software, Validation, Writing – original draft, Writing – review & editing, Data curation, Investigation, Project administration, Resources, Supervision, Visualization, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was financed with Fiscal Resources of the Federal Budget for Research under Modes A and B, assigned to the National Institute of Pediatrics, Mexico, 2022–2023.
Acknowledgments
We would like to sincerely thank our colleagues Beatriz Eugenia Perez-Guille, Rosa Eugenia Soriano-Rosales, Leonardo Baruch Rios-Garcia, Mariana Santos-Cortes and Silvio Carmona-Librado for their insightful feedback during the research process.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. We use AI to translate and correct style.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AA, acute appendicitis; CA, complicated appendicitis; STROBE, the strengthening the reporting of observational studies in epidemiology; CONEVAL, consejo nacional de evaluación de la política de desarrollo social; OR, odds ratios; CI, confidence interval; CDC, Centers for Disease Control and Prevention.
References
1. Calpin GG, Hembrecht S, Giblin K, Hehir C, Dowling GP, Hill ADK. The impact of timing on outcomes in appendicectomy: a systematic review and network meta-analysis. World J Emerg Surg. (2024) 19(1):24. doi: 10.1186/s13017-024-00549-4
2. Jablonski KA, Guagliardo MF. Pediatric appendicitis rupture rate: a national indicator of disparities in healthcare access. Popul Health Metr. (2005) 3(1):4. doi: 10.1186/1478-7954-3-4
3. Golz RA, Flum DR, Sanchez SE, Liu X, Donovan C, Drake FT. Geographic association between incidence of acute appendicitis and socioeconomic status. JAMA Surg. (2020) 155(4):330. doi: 10.1001/jamasurg.2019.6030
4. Gadomski A, Jenkins P. Ruptured appendicitis among children as an indicator of access to care. Health Serv Res. (2001) 36(1 Pt 1):129–42.11324740
5. Narsule CK, Kahle EJ, Kim DS, Anderson AC, Luks FI. Effect of delay in presentation on rate of perforation in children with appendicitis. Am J Emerg Med. (2011) 29(8):890–3. doi: 10.1016/j.ajem.2010.04.005
6. Serres SK, Cameron DB, Glass CC, Graham DA, Zurakowski D, Karki M, et al. Time to appendectomy and risk of complicated appendicitis and adverse outcomes in children. JAMA Pediatr. (2017) 171(8):740. doi: 10.1001/jamapediatrics.2017.0885
7. Rice-Townsend S, Barnes JN, Hall M, Baxter JL, Rangel SJ. Variation in practice and resource utilization associated with the diagnosis and management of appendicitis at freestanding children’s hospitals: implications for value-based comparative analysis. Ann Surg. (2014) 259(6):1228–34. doi: 10.1097/SLA.0000000000000246
8. Bouchard ME, Kan K, Tian Y, Casale M, Smith T, De Boer C, et al. Association between neighborhood-level social determinants of health and access to pediatric appendicitis care. JAMA Netw Open. (2022) 5(2):e2148865. doi: 10.1001/jamanetworkopen.2021.48865
9. Li J, Xu R, Hu DM, Zhang Y, Gong TP, Wu XL. Effect of delay to operation on outcomes in patients with acute appendicitis: a systematic review and meta-analysis. J Gastrointest Surg. (2019) 23(1):210–23. doi: 10.1007/s11605-018-3866-y
10. Estrella JB, Carmichael H, Myers QWO, Lee S, Velopulos CG. Making it complicated: does disparity in access to care lead to more perforated appendicitis? J Surg Res. (2021) 266:405–12. doi: 10.1016/j.jss.2021.04.031
11. Mah JC, Penwarden JL, Pott H, Theou O, Andrew MK. Social vulnerability indices: a scoping review. BMC Public Health. (2023) 23(1):1253. doi: 10.1186/s12889-023-16097-6
12. Mah JC. Social Protection at the Crossroads—in Pursuit of a Better Future. Geneva: International Labour Office (2021). p. 315. (World social protection report).
13. Platt E, Doe M, Kim NE, Chirengendure B, Musonda P, Kaja S, et al. Economic impact of surgery on households and individuals in low income countries: a systematic review. Int J Surg. (2021) 90:105956. doi: 10.1016/j.ijsu.2021.105956
14. Michelson KA, Bachur RG, Rangel SJ, Finkelstein JA, Monuteaux MC, Goyal MK. Disparities in diagnostic timeliness and outcomes of pediatric appendicitis. JAMA Netw Open. (2024) 7(1):e2353667. doi: 10.1001/jamanetworkopen.2023.53667
15. Garcia-Diaz R. Effective access to health care in Mexico. BMC Health Serv Res. (2022) 22(1):1027. doi: 10.1186/s12913-022-08417-0
16. Consejo Nacional de Evaluación de la Política de Desarrollo Social. Informe de Evaluación de la Política de Desarrollo Social 2022. Ciudad de México: CONEVAL (2022).
17. Colchero MA, Gómez R, Bautista-Arredondo S. A systematic review of the literature on the impact of the seguro popular. Health Res Policy Syst. (2022) 20(1):42. doi: 10.1186/s12961-022-00839-w
18. Vandenbroucke JP, Von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology. (2007) 18(6):805–35. doi: 10.1097/EDE.0b013e3181577511
19. Cameron DB, Anandalwar SP, Graham DA, Melvin P, Serres SK, Dunlap JL, et al. Development and implications of an evidence-based and public health-relevant definition of complicated appendicitis in children. Ann Surg. (2020) 271(5):962–8. doi: 10.1097/SLA.0000000000003059
20. McKie KA, Graham DA, Cramm SL, Saito JM, Rangel SJ. Population-based intraoperative disease severity criteria for pediatric appendicitis. JAMA Surg. (2024) 159(9):1041. doi: 10.1001/jamasurg.2024.1759
21. Van Dijk ST, Van Dijk AH, Dijkgraaf MG, Boermeester MA. Meta-analysis of in-hospital delay before surgery as a risk factor for complications in patients with acute appendicitis. Br J Surg. (2018) 105(8):933–45. doi: 10.1002/bjs.10873
22. Acuerdo por el que se emiten los criterios generales y la metodología a los que deberán sujetarse los procesos de clasificación socioeconómica de pacientes en los establecimientos que presten servicios de atención médica de la Secretaría de Salud y de las entidades coordinadas por dicha Secretaría. Diario Oficial de la Federación [Internet]. Available at: https://www.dof.gob.mx/nota_detalle.php?codigo=5300256&fecha=27/05/2013#gsc.tab=0 (Accessed January 02, 2025).
23. Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am J Clin Nutr. (2002) 75(6):978–85. doi: 10.1093/ajcn/75.6.978
24. Chang YJ, Chen LJ, Chang YJ. Did the severity of appendicitis increase during the COVID-19 pandemic? PLoS One. (2022) 17(2):e0263814. doi: 10.1371/journal.pone.0263814
25. Trinidad S, Parrado R, Gavulic A, Hoang M, Duan Q, Overmann KM, et al. Characterizing inequities in pediatric appendicitis delayed diagnosis and perforation. J Pediatr Clin Pract. (2024) 11:200108. doi: 10.1016/j.jpedcp.2024.200108
26. Luckmann R. Incidence and case fatality rates for acute appendicitis in California. Am J Epidemiol. (1989) 129(5):905–18. doi: 10.1093/oxfordjournals.aje.a115224
27. Andersson RE. Proportion of cases of perforated appendicitis: a bad measure of quality of care. Arch Surg. (2011) 146(7):885. doi: 10.1001/archsurg.2011.168
28. Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. (2007) 245(6):886–92. doi: 10.1097/01.sla.0000256391.05233.aa
29. Sippola S, Haijanen J, Grönroos J, Rautio T, Nordström P, Rantanen T, et al. Effect of oral moxifloxacin vs intravenous ertapenem plus oral levofloxacin for treatment of uncomplicated acute appendicitis: the APPAC II randomized clinical trial. JAMA. (2021) 325(4):353. doi: 10.1001/jama.2020.23525
30. Salminen P, Sippola S, Haijanen J, Nordström P, Rantanen T, Rautio T, et al. Antibiotics versus placebo in adults with CT-confirmed uncomplicated acute appendicitis (APPAC III): randomized double-blind superiority trial. Br J Surg. (2022) 109(6):503–9. doi: 10.1093/bjs/znac086
31. Dhillon BK, Kortbeek S, Baghela A, Brindle M, Martin DA, Jenne CN, et al. Gene expression profiling in pediatric appendicitis. JAMA Pediatr. (2024) 178(4):391. doi: 10.1001/jamapediatrics.2023.6721
32. Bergmark RW, Burks CA, Schnipper JL, Weissman JS. Understanding and investigating access to surgical care. Ann Surg. (2022) 275(3):492–5. doi: 10.1097/SLA.0000000000005212
33. Horwitz JR, Gursoy M, Jaksic T, Lally KP. Importance of diarrhea as a presenting symptom of appendicitis in very young children. Am J Surg. (1997) 173(2):80–2. doi: 10.1016/S0002-9610(96)00417-5
34. Snyder KB, Hunter CJ, Buonpane CL. Perforated appendicitis in children: management. microbiology, and antibiotic stewardship. Pediatr Drugs. (2024) 26(3):277–86. doi: 10.1007/s40272-024-00630-0
35. Sánchez-Huesca R, Lerma A, Guzmán-Saldaña RME, Lerma C. Prevalence of antibiotics prescription and assessment of prescribed daily dose in outpatients from Mexico City. Antibiotics. (2020) 9(1):38. doi: 10.3390/antibiotics9010038
36. Elliott BM, Bissett IP, Harmston C, STRATA Collaborative. The impact of delay and prehospital factors on acute appendicitis severity in New Zealand children: a national prospective cohort study. ANZ J Surg. (2023) 93(7–8):1978–86. doi: 10.1111/ans.18615
37. Georgeades C, Bodnar C, Bergner C, Van Arendonk KJ. Association of complicated appendicitis with geographic and socioeconomic measures in children. Surgery. (2024) 176(5):1475–84. doi: 10.1016/j.surg.2024.07.044
38. Pérez-Soto RH, Trolle-Silva AM, Valdés GABR, Sánchez-Morales GE, Velázquez-Fernández D, Medina ARDL, et al. Timely access to essential surgery, surgical workforce, and surgical volume: global surgery indicators in Mexico. Glob Health Sci Pract. (2023) 11(1):e2100745. doi: 10.9745/GHSP-D-21-00745
Keywords: complicated appendicitis, prehospital delay, access to surgical care, social vulnerability, health inequities, Hispanic pediatric, Mexican population
Citation: Estefany V-A, Karen M-M, Citlali A-G, Ailema G-O and Jose Francisco G-Z (2025) Surgical delay in appendicitis among children: the role of social vulnerability. Front. Pediatr. 13:1591200. doi: 10.3389/fped.2025.1591200
Received: 10 March 2025; Accepted: 16 June 2025;
Published: 2 July 2025.
Edited by:
Rose Saint Fleur-Calixte, Downstate Health Sciences University, United StatesReviewed by:
Bruno Martinez-Leo, MD, Momentum Foundation for Congenital Colorectal Diseases, AC, MexicoShahidul Islam, Northwell Health, United States
Copyright: © 2025 Estefany, Karen, Citlali, Ailema and Jose Francisco. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gonzalez-Zamora Jose Francisco, amYuZ29uemFsZXp6YW1vcmFAZ21haWwuY29t
†ORCID:
Marín-Morales Karen
orcid.org/0009-0003-7095-8337
 Villa-Aguilar Estefany
Villa-Aguilar Estefany Marín-Morales Karen
Marín-Morales Karen Ayala-Galvan Citlali
Ayala-Galvan Citlali Gonzalez-Ortiz Ailema
Gonzalez-Ortiz Ailema Gonzalez-Zamora Jose Francisco
Gonzalez-Zamora Jose Francisco