- Department of Obstetrics and Gynecology, Second Hospital of Shanxi Medical University, Taiyuan, Shanxi, China
Background: Dynamic changes in maternal blood pressure influence neonatal birth weight however, studies investigating the association between blood pressure trajectories during pregnancy and low birth weight (LBW) remain limited. This study aims to identify maternal blood pressure trajectories based on three time points using group-based trajectory modeling (GBTM) and explore their association with LBW.
Methods: This study was based on the NHANES 2005–2006 database and included 330 pregnant women meeting the eligibility criteria (41 cases in the LBW group and 289 in the control group). GBTM was applied to model three blood pressure measurements [systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse pressure (PP)] taken during pregnancy. Multilevel logistic regression was used to assess the relationship between blood pressure trajectories and LBW. Additionally, stratified analyses were conducted to evaluate the modifying effects of age, body mass index (BMI), and education level, and directed acyclic graph (DAG) were employed for covariate selection.
Results: Three distinct blood pressure trajectory patterns were identified. Logistic regression revealed that, compared with the low blood pressure trajectory, mothers with a high-medium SBP trajectory had a significantly increased risk of delivering an LBW infant [odds ratio [OR] = 4.479, 95% confidence interval [CI]: 2.541–7.895, P < 0.001]. Stratified analyses indicated that this association was more pronounced in mothers who were older than 40 years, had a BMI >28, had lower income, did not consume alcohol, and had abnormal cholesterol levels. The DAG analysis further supported the independent effect of blood pressure trajectories on LBW.
Conclusions: Maternal blood pressure trajectories based on three prenatal measurements are closely associated with LBW, particularly among mothers with a high-medium SBP trajectory. This study underscores the importance of monitoring blood pressure fluctuations during pregnancy and suggests that early intervention may help reduce the risk of LBW.
Introduction
Low birth weight (LBW) refers to a newborn's birth weight of less than 2,500 g (1). It is not only a significant factor influencing neonatal mortality and morbidity, but is also associated with an increased risk of long-term metabolic diseases, cardiovascular diseases, and neurodevelopmental disorders (2–4). Maternal blood pressure changes during pregnancy may affect placental perfusion and fetal growth, thereby having a significant impact on neonatal birth weight (5, 6). Previous studies have shown that hypertensive disorders of pregnancy (HDP) significantly increase the risk of LBW (7). However, even in pregnant women without HDP, the dynamic changes in blood pressure (trajectories) may still have a potential impact on LBW (8, 9). For example, Teng et al. (10) examined the association between systolic blood pressure (SBP) trajectories and a range of pregnancy outcomes, including low birth weight (LBW), and found that variations in SBP patterns were significantly associated with LBW risk. Building upon this line of research, our study focuses specifically on the relationship between SBP trajectories and LBW by applying a data-driven clustering approach to classify SBP change patterns over time, aiming to better capture dynamic maternal blood pressure profiles during pregnancy. Currently, research on the relationship between blood pressure trajectories during pregnancy and LBW is still limited, especially regarding long-term blood pressure patterns in non-HDP populations and their impact on LBW. Therefore, exploring maternal blood pressure trajectories during pregnancy and evaluating their potential effects on LBW is of significant clinical importance. The methodological innovation of this study lies in the first-time application of Group-based trajectory modeling (GBTM) and Directed Acyclic Graphs (DAG) to study maternal blood pressure trajectories during pregnancy and their association with LBW.
GBTM has been widely applied in epidemiology and public health to analyze health parameter patterns over time, allowing researchers to identify different blood pressure trajectory groups and revealing long-term trends in maternal blood pressure (11–13). Although Linear Mixed Effects (LME) models could also analyze longitudinal data, GBT was chosen because it better captures the heterogeneous, non-linear changes in blood pressure over time, whereas LME assumes a single, linear trajectory for the entire population. This method offers a novel perspective for early prediction and intervention to prevent LBW (14). Moreover, this study is the first to use DAG methodology for covariate selection in this context, with the goal of reducing, confounding, optimizing model specification, and informing suggestive of causality in the analysis of pregnancy blood pressure and LBW (15).
Previous studies have mainly focused on the association between a single blood pressure measurement during pregnancy and LBW, while neglecting the dynamic changes in blood pressure patterns. Some studies suggest that stable blood pressure trajectories may have a protective effect on fetal growth, whereas persistently elevated or highly fluctuating blood pressure trajectories may increase the risk of adverse pregnancy outcomes (16, 17). However, how different blood pressure trajectory patterns affect the risk of LBW remains to be further investigated.
In addition, the relationship between maternal blood pressure trajectories and LBW may be influenced by various factors, including maternal age, BMI, education level, economic status, smoking, and alcohol consumption behaviors (18, 19). For instance, older pregnant women (>40 years) and those with a BMI > 28 may be more likely to exhibit abnormal blood pressure trajectories, thereby increasing the risk of LBW (8, 20). To more accurately assess the independent effect of blood pressure trajectories on LBW, this study employed DAG methodology for covariate selection, aiming to reduce the influence of potential confounding factors. The DAG method is widely used in causal inference studies, helping researchers identify and adjust for potential confounders, thereby optimizing statistical models and enhancing the robustness of causal inference (15).
Building on this background, this study utilized the NHANES 2005–2006 database and applied GBTM to identify maternal blood pressure trajectories during pregnancy and assess their relationship with LBW. Additionally, the study explored potential moderating effects of various population characteristics (such as age, BMI, and education level) on this relationship through stratified analyses, and employed DAG for suggestive of causality. The results of this study may provide new epidemiological evidence for managing maternal blood pressure during pregnancy and offer potential intervention strategies for preventing LBW.
Methods
Data sources and study population
This study utilized the NHANES 2005–2006 dataset, organized by the National Center for Health Statistics (NCHS) and the Centers for Disease Control and Prevention (CDC). The dataset employs a multi-stage, stratified, probability sampling method to collect health data from a nationally representative sample of the U.S. population (21). The data includes various health indicators, including health behaviors, physical examinations, and laboratory tests, providing key health metrics such as maternal blood pressure measurements and neonatal birth weight. The study population consisted of pregnant women who participated in the NHANES 2005–2006 survey, with the following inclusion criteria: complete data for three pregnancy-related blood pressure measurements (systolic blood pressure, SBP; diastolic blood pressure, diastolic blood pressure, DBP); pulse pressure, PP) and complete neonatal birth weight records. Exclusion criteria included participants with missing data, those with pregnancy complications (such as gestational hypertension or diabetes), and pregnant women with chronic diseases (such as chronic hypertension or cardiovascular diseases). All participants provided written informed consent prior to data collection. Due to the use of de-identified publicly available data, and the absence of personal identifiers, this study did not require approval from an institutional review board. All results were reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines to ensure transparency and reliability.
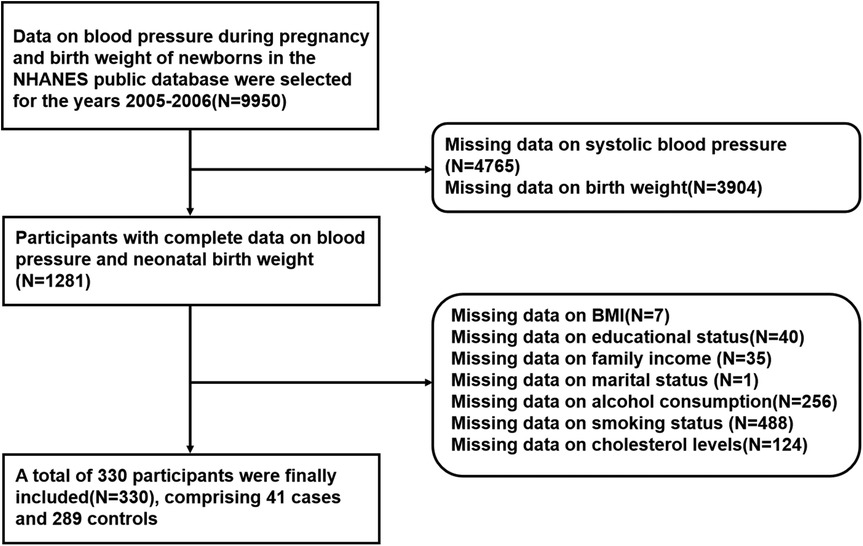
Data selection
To ensure data integrity and enhance the comparability of the results, the following data selection process was applied in this study (Figure 1). First, data on maternal blood pressure and neonatal birth weight from the NHANES 2005–2006 dataset were selected, with an initial sample size of 9950 participants. Next, participants with complete data on blood pressure and neonatal birth weight were selected, resulting in a total of 1,281 participants. Additionally, missing data were identified in variables such as BMI, education level, family income, marital status, alcohol consumption, smoking, and cholesterol levels, and participants with missing data in these variables were excluded. After the data cleaning process, a final sample of 330 participants with complete data was included, comprising 41 cases in the LBW group (birth weight <2,500 g) and 289 controls in the non-LBW group (birth weight ≥2,500 g).
Study design
This study employed GBTM to analyze the trends in maternal blood pressure during pregnancy and to explore the association between different blood pressure trajectories and neonatal LBW. GBTM uses a finite mixture model to analyze longitudinal data and selects the optimal trajectory classification scheme based on the Bayesian Information Criterion (BIC) and the Likelihood Ratio Test (LRT). In this study, maternal blood pressure trajectories during pregnancy were categorized into high-medium, high-low, and medium-low patterns to reflect different trends in blood pressure changes over pregnancy.
The exposure variable in this study was maternal blood pressure trajectory, based on three measurements of SBP, DBP, and PP, taken at the 10th, 20th, and 30th weeks of pregnancy. The outcome variable was neonatal LBW, defined as birth weight <2,500 g. Additionally, demographic factors (age, race, education level, income, marital status), health behaviors (alcohol consumption, smoking during pregnancy), and biological factors (BMI, cholesterol levels) were included as covariates to control for potential confounding factors. To improve the scientific rigor of covariate selection, DAG analysis was used to screen variables, ensuring the rationality of model construction and minimizing confounding bias. The final selected covariates were used for subsequent statistical analyses.
Statistical analysis
This study used GBT to analyze the relationship between maternal blood pressure trajectories and neonatal LBW, adjusting for covariates stepwise. The modeling was performed using R with the “traj” package. The Bayesian Information Criterion (BIC) was used to select the optimal number of trajectory groups. In this study, the number of groups was determined by minimizing the BIC, and the optimal solution was three trajectory groups based on maternal blood pressure measurements (systolic blood pressure, diastolic blood pressure, and pulse pressure). Three distinct blood pressure trajectory groups were initially identified during pregnancy using group-based trajectory modeling. In the multilevel model, individual-level random effects were included to account for the repeated blood pressure measurements within each participant. Specifically, the random effect in the multilevel model was applied to the participant level to account for the correlation between multiple blood pressure measurements collected from the same individual. Exposures were categorized into three types based on maternal blood pressure trajectories (systolic blood pressure, diastolic blood pressure, and pulse pressure). Inverse probability weighting (IPW) was calculated based on propensity scores derived from the covariates. The weights were stabilized to improve the precision of the potential causal relationship. Stabilized weights were used to reduce the potential bias in the estimation caused by extreme weights. Standardized mean differences were computed to compare the balance of measured variables between groups before and after applying IPW. In model 1, only blood pressure trajectories were adjusted to assess their primary impact on LBW. Model 2 incorporated maternal age to explore the moderating effect of age on the relationship between blood pressure trajectories and LBW. In model 3, additional covariates such as BMI, race, education level, income, marital status, alcohol consumption, smoking, and cholesterol levels were included to control for potential confounding factors. Finally, in model 4 (the final model), inverse probability weighting (IPW)-logistic regression was used based on model 3 to perform causal inference, reducing the impact of confounding factors and improving the precision of potential causal relationship.
To further investigate the relationship between blood pressure trajectories and LBW, this study performed stratified analyses to evaluate the impact of blood pressure trajectories on LBW across different subgroups. The stratification criteria included: age (≤40 years vs. >40 years), BMI (≤28 vs. >28), education level (high school or below vs. college and above), income (≤75,000 vs. >75,000), and lifestyle (alcohol consumption vs. no alcohol, smoking vs. no smoking). Stratified analyses help to examine whether different population characteristics influence the relationship between blood pressure trajectories and LBW. Additionally, IPW-Logistic regression was employed for potential causal relationship to simulate a randomized controlled trial (RCT) scenario, minimizing the impact of covariate imbalance. By calculating propensity scores based on covariates, weights were assigned to each individual, and samples were weighted to balance the covariate distribution across different blood pressure trajectory groups, thereby enhancing the accuracy of potential causal relationship. All statistical analyses were performed using R and the “traj” package for the group-based trajectory modeling. The Bayesian Information Criterion (BIC) was used to select the optimal number of trajectory groups.
Results
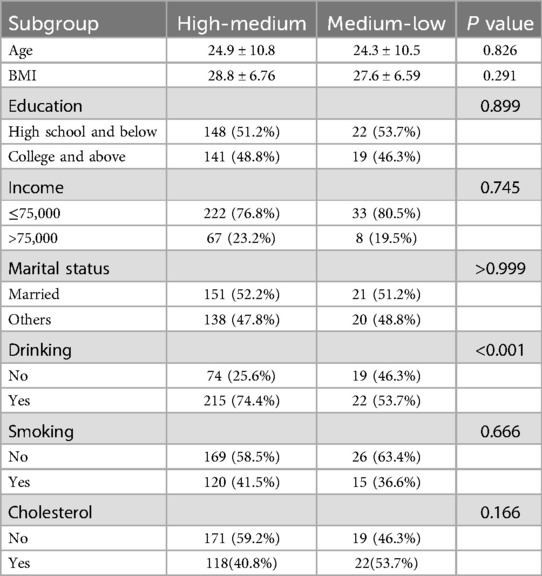
Comparison of demographic data between high-medium and medium-low groups
Table 1 summarizes the baseline demographic and clinical characteristics of participants in the high-medium and medium-low systolic pressure groups. No significant differences were observed between the two groups in terms of age (24.9 ± 10.8 vs. 24.3 ± 10.5 years, P = 0.826), BMI (28.8 ± 6.76 vs. 27.6 ± 6.59, P = 0.291), education level, income, marital status, smoking, or cholesterol status (P > 0.05 for all). However, a significant difference was observed in drinking behavior: 74.4% of participants in the high-medium group reported alcohol consumption, compared to 53.7% in the medium-low group (P < 0.001).
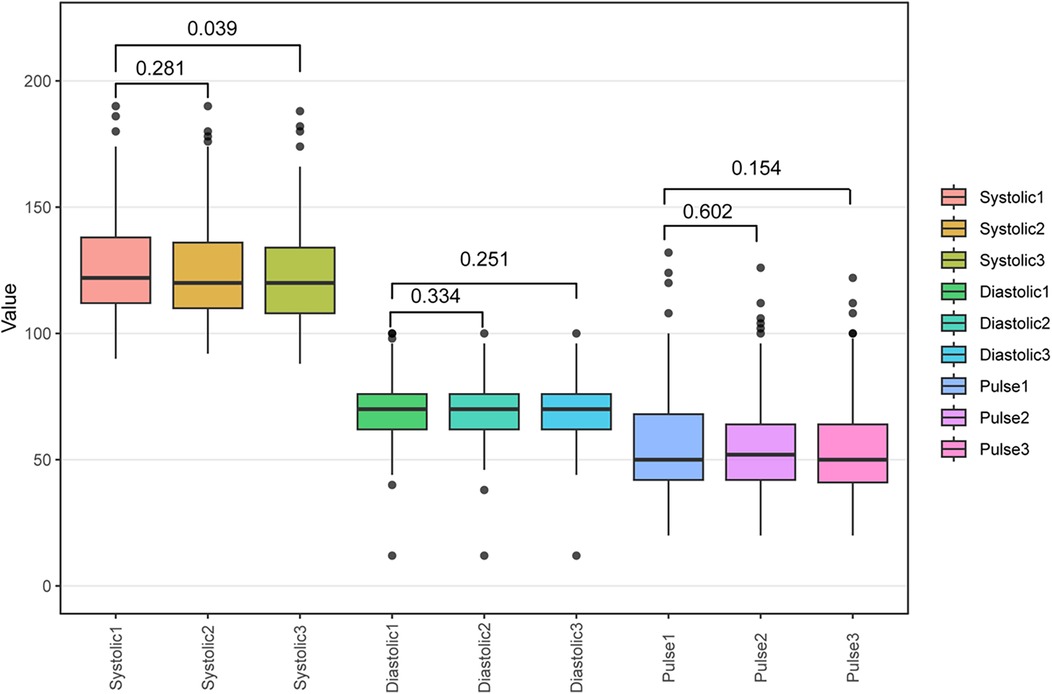
Consistency and stability analysis: reproducibility assessment of blood pressure measurements during pregnancy
To assess the stability of blood pressure measurements during pregnancy, this study compared three repeated measurements of SBP, DBP, and PP taken at the 10th, 20th, and 30th weeks of pregnancy. These measurements were collected using standardized automatic blood pressure measurement devices and visualized their variations using box plots (Figure 2). The results indicate that a significant difference was observed only between the first (Systolic1) and third (Systolic3) SBP measurements (P = 0.039), whereas no significant differences were found in other blood pressure measurements, including DBP and PP (P > 0.05). These findings suggest that SBP may fluctuate over time, particularly between early and later measurements, highlighting the need for careful monitoring of its dynamic changes during pregnancy. In contrast, DBP and PP remained stable across the three measurements, indicating good reproducibility and reliability as blood pressure assessment indicators during pregnancy.
Maternal blood pressure trajectories and dynamic changes during pregnancy
GBTM identified three distinct maternal blood pressure patterns for each indicator throughout pregnancy (Figure 3). For systolic blood pressure (SBP), the high–medium group maintained the highest levels with a slight decline over time, the high–low group showed a moderate initial level with a gradual decrease, while the medium–low group presented the lowest SBP levels and a steady downward trend. DBP trajectories demonstrated relative stability in the high–medium group, a modest decline in late pregnancy in the high–low group, and a shallow U-shaped pattern in the medium–low group, characterized by a slight mid-pregnancy dip followed by a late rebound. In terms of PP, the high–medium group exhibited the highest values with a slight decrease, the high–low group remained intermediate and stable, and the medium–low group maintained the lowest PP with minimal fluctuation. These trajectory characteristics suggest that persistently elevated SBP and PP, especially in the high–medium group, may reflect increased vascular stiffness or subclinical hypertensive changes during pregnancy, which are known to impair placental perfusion and elevate the risk of adverse outcomes such as low birth weight (10, 14). In contrast, the declining SBP and stable, low DBP and PP observed in the medium–low group may indicate favorable cardiovascular adaptation. The mild rebound of DBP in late gestation seen in this group could represent a physiological response to increasing circulatory demands. Collectively, these findings suggeated that both the level and pattern of maternal blood pressure changes during pregnancy are critical for predicting perinatal outcomes.
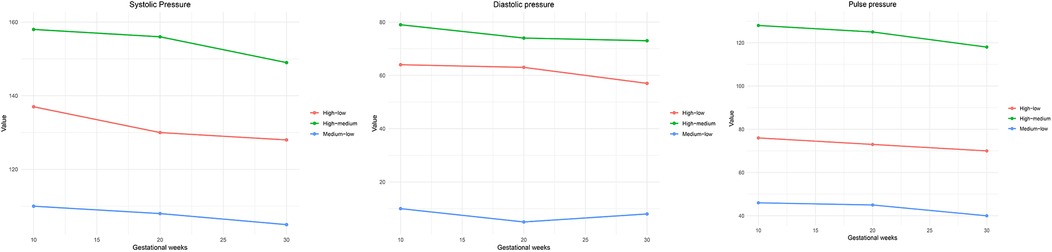
Figure 3. Maternal blood pressure trajectory model (GBTM) analysis results. This figure displays three distinct trajectory groups for (A) systolic blood pressure, (B) diastolic blood pressure, and (C) pulse pressure across gestational weeks 10, 20, and 30. The identified trajectories are labeled as high–low, high–medium, and medium–low, reflecting different trends in blood pressure changes over time. Pulse pressure was calculated as the difference between systolic and diastolic blood pressure.
Impact of blood pressure trajectories on LBW
As shown in Table 2, this study analyzed the relationship between maternal blood pressure trajectories and LBW using multilevel logistic regression models. The analysis was conducted on 330 pregnant women from the NHANES 2005–2006 database. Model 1 adjusted for blood pressure trajectories only. The results indicated that the high-medium systolic pressure trajectory had an odds ratio (OR) of 3.520 [95% confidence interval (CI): 1.422–8.713], suggesting a significant association between maternal systolic pressure trajectories and LBW. Additionally, the high-medium diastolic pressure trajectory had an OR of 0.935 (95% CI: 0.486–1.792), showing some degree of association. However, the high-medium pulse pressure trajectory had an OR of 1.658 (95% CI: 0.086–10.396), indicating a weaker relationship.
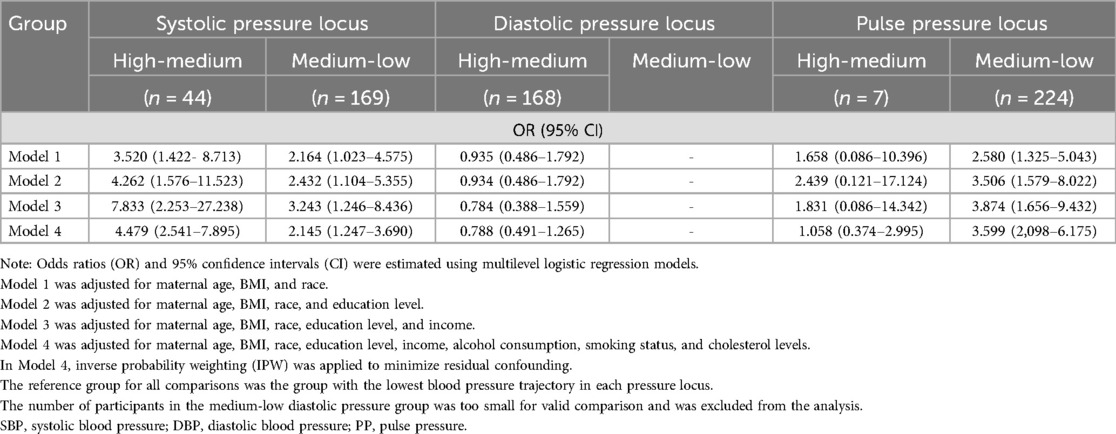
Table 2. Association between maternal blood pressure trajectories and LBW across different pressure loci.
In model 2, maternal age was added as a covariate to examine its moderating effect on the relationship between blood pressure trajectories and LBW. The results showed that maternal age played a moderating role. The OR for the high-medium systolic pressure trajectory increased to 4.262 (95% CI: 1.576–11.523), suggesting that age strengthens the relationship between systolic blood pressure trajectories and LBW. Other blood pressure trajectory groups showed similar trends, indicating that age plays a moderating role in the relationship between blood pressure trajectories and LBW.
In model 3, the relevant covariates are further added. The results showed that the OR for the high-medium systolic pressure trajectory was 7.833 (95% CI: 2.253–27.238), significantly increasing the risk of LBW. Moreover, OR values for other blood pressure trajectory groups also changed substantially, indicating that these covariates played a moderating role in the relationship between blood pressure trajectories and LBW.
Finally, in model 4, based on model 3, IPW logistic regression was used for potential causal relationship, further controlling for confounding factors. The results showed that the OR for the high-medium systolic pressure trajectory was 4.479 (95% CI: 2.541–7.895), further supporting the potential causal relationship between blood pressure trajectories and LBW. The analysis of other blood pressure trajectory groups also showed that the IPW method effectively reduced the impact of confounding factors, enhancing the reliability of association.
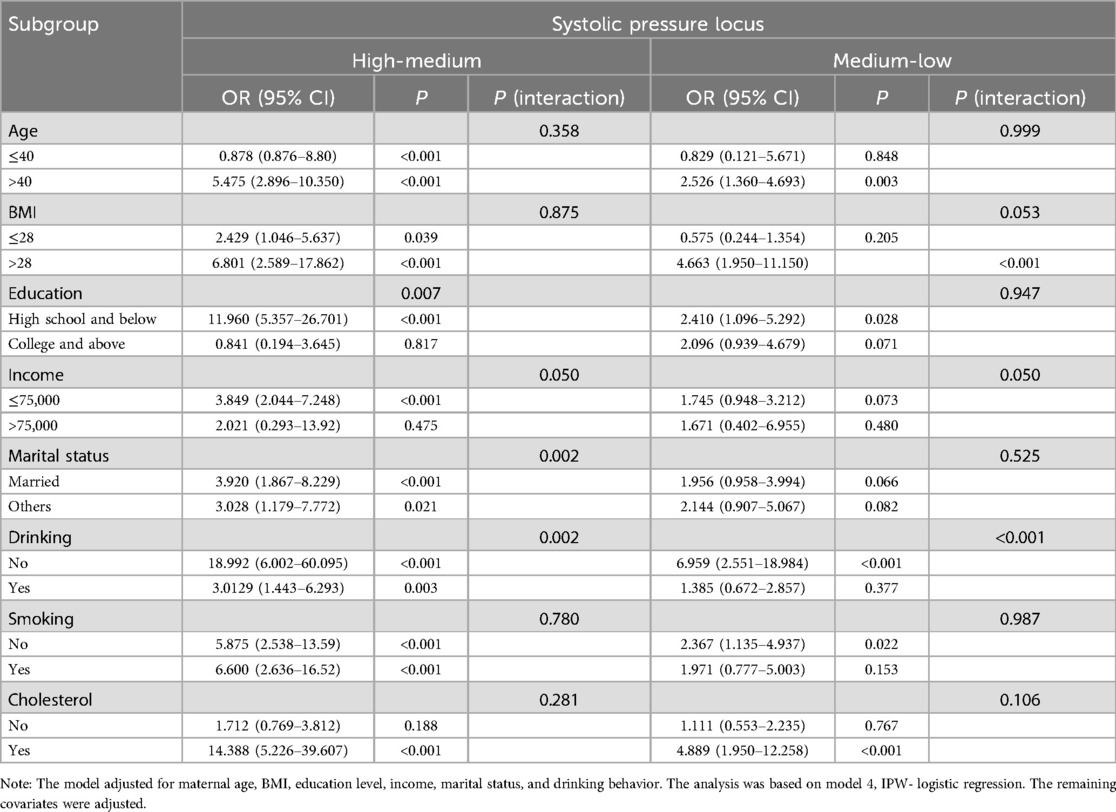
Stratified analysis of systolic pressure locus and LBW
Due to the limited sample size for DBP and PP trajectories, stratified analysis was only conducted to examine the relationship between systolic pressure locus and LBW in 330 pregnant women from the NHANES 2005–2006 database, as shown in Table 3. The results indicate that maternal age, BMI, education level, income, marital status, alcohol consumption, and cholesterol levels may be important modifiers of this association.
In the age-stratified analysis, the association between high-medium SPL and LBW was more pronounced in mothers aged > 40 years (OR = 5.475, P < 0.001) compared to those aged ≤40 years (OR = 0.878, P < 0.001). The BMI-stratified analysis showed that the association was stronger in the BMI > 28 group (OR = 6.801, P < 0.001) than in the BMI ≤ 28 group (OR = 2.429, P = 0.039). Mothers with lower education levels (high school or below) exhibited the highest LBW risk in the high-medium SPL group (OR = 11.960, P < 0.001), whereas the association was not significant in those with higher education (P = 0.817). In the low-income group (≤75,000 USD), the association was stronger (OR = 3.849, P < 0.001), while no significant relationship was observed in the high-income group (P = 0.475). Regarding marital status, married women in the high-medium SPL group had a higher LBW risk (OR = 3.920, P < 0.001). For lifestyle factors, the association between SPL and LBW was more pronounced in non-drinkers (OR = 18.992, P < 0.001), whereas smoking status had a minimal effect on this relationship (P for interaction = 0.780). Additionally, in the abnormal cholesterol group, the association between high-medium SPL and LBW was stronger (OR = 14.388, P < 0.001), while no significant relationship was found in those with normal cholesterol levels (P = 0.188).
In summary, advanced maternal age (>40 years), higher BMI (>28), lower education levels, lower income, non-drinking status, and abnormal cholesterol levels may enhance the association between SPL and LBW. These findings highlight the importance of maternal demographic and lifestyle factors in pregnancy management.
Association and covariate selection: DAG analysis
To explore the potential association between blood pressure trajectories (exposure) and LBW (outcome), this study utilized DAG approach for covariate selection and identification of potential confounders among 330 pregnant women from the NHANES 2005–2006 database, as shown in Figure 4). The analysis involved adjusting for all confounders identified by the DAG to improve the robustness of the association estimation between blood pressure trajectories and LBW. The results showed that, after adjustment, blood pressure trajectories remained significantly associated with LBW, suggesting a potential independent effect and a possible causal relationship. Additionally, the DAG results indicated that, although variables such as age, BMI, education level, income, marital status, alcohol consumption, smoking, and cholesterol levels had some influence on LBW, they did not fully explain the effect of blood pressure trajectories.
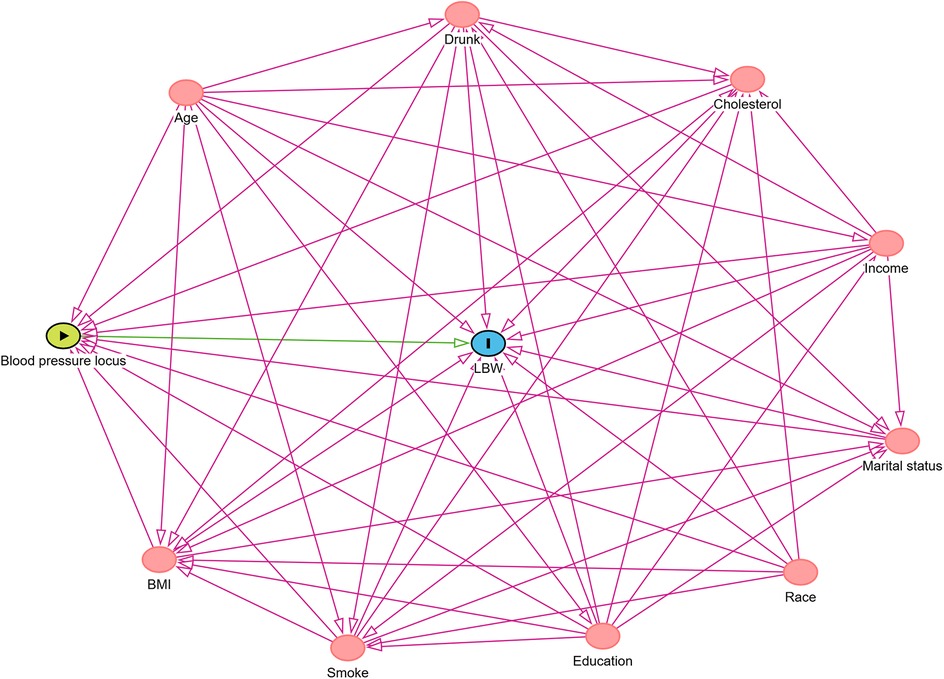
Figure 4. DAG analysis for covariate selection. The green node represents the exposure variable (blood pressure trajectory), the blue node represents the outcome variable (LBW), and the pink nodes represent potential confounders, including age, BMI, race, education level, income, marital status, alcohol consumption, smoking, and cholesterol levels.
Discussion
This study, based on the NHANES 2005–2006 database, utilized GBTM to identify maternal blood pressure trajectories during pregnancy and examine their relationship with LBW. The results showed that maternal blood pressure trajectories during pregnancy exhibited distinct grouping characteristics. Mothers with a high-medium systolic pressure trajectory had a significantly increased risk of LBW in their newborns (OR = 4.479, 95% CI: 2.541–7.895, P < 0.001). Further stratified analyses revealed that this association was more pronounced among mothers aged >40 years, with a BMI > 28, low income, non-drinkers, and those with abnormal cholesterol levels. Additionally, DAG analysis further supported the independent effect of maternal blood pressure trajectories on LBW.
Maternal blood pressure trajectories may influence fetal growth and birth weight through various physiological mechanisms. Although women with diagnosed chronic hypertension and gestational diabetes were excluded from this study, it is possible that some participants—particularly those in the high-medium blood pressure trajectory group—may have exhibited subclinical vascular dysfunction or pre-hypertensive states. These latent abnormalities, although not clinically apparent, could still impair placental perfusion and fetal nutrient exchange, thereby contributing to the observed associations (22, 23). Prior studies have shown that hypertensive conditions are associated with inadequate placental blood flow, reduced oxygen and nutrient delivery to the fetus, and an increased risk of intrauterine growth restriction (IUGR) and LBW (24–26). Moreover, dynamic fluctuations in blood pressure may reflect maternal vascular maladaptation, such as decreased arterial compliance or increased vascular contractility, which could further compromise uteroplacental circulation (22, 27). This study found that even in the absence of a diagnosis of HDP, pregnant women with a high-medium systolic pressure trajectory still faced a higher risk of LBW, suggesting that it is not only the absolute blood pressure values but also the patterns of its changes over time that may have significant effects on fetal growth.
Stratified analysis results showed that the relationship between maternal blood pressure trajectories and low birth weight (LBW) was more pronounced in older mothers (>40 years) and those with a BMI > 28. Older pregnant women may exhibit early vascular aging or subclinical arterial stiffness, which—although not clinically diagnosed as hypertension—can impair vascular adaptability during pregnancy and potentially reduce placental perfusion (23, 28). Similarly, pregnant women with elevated BMI may present with insulin resistance and low-grade systemic inflammation, which are not limited to overt gestational diabetes but may reflect underlying metabolic disturbances associated with vascular dysfunction (29, 30). These early or subclinical changes may act synergistically to exacerbate the adverse effects of abnormal blood pressure trajectories on fetal development, particularly in older or high-BMI pregnant women. Furthermore, this study found that the relationship between blood pressure trajectories and LBW was more significant in pregnant women with low income and abnormal cholesterol levels. The impact of socioeconomic status on maternal health has been well-documented in numerous studies (31). Low-income pregnant women may face higher risks of malnutrition, increased pregnancy stress, and limited access to medical resources, all of which can further exacerbate the adverse effects of blood pressure on fetal growth by affecting placental function (32). On the other hand, abnormal cholesterol levels may be associated with vascular dysfunction and metabolic abnormalities, which could influence blood pressure regulation during pregnancy and increase the risk of LBW (33). DAG analysis results showed that even after adjusting for potential confounders such as age, BMI, education level, income, marital status, alcohol consumption, smoking, and cholesterol levels, blood pressure trajectories still had a significant impact on LBW. These findings suggest that maternal blood pressure trajectories may be an independent predictor of LBW, rather than merely an indirect reflection of other confounding factors.
The covariate selection based on DAG further support for a potential causal association between blood pressure trajectories and LBW, highlighting the clinical importance of monitoring blood pressure patterns throughout pregnancy.
This study has several limitations. First, the NHANES database includes only three blood pressure measurements during pregnancy, which may not fully reflect the long-term trends in maternal blood pressure changes over the course of pregnancy. Future studies could integrate higher-frequency blood pressure monitoring data to derive refined blood pressure trajectory patterns. Second, this study did not include maternal lifestyle factors (such as diet and physical activity), which may influence maternal blood pressure trajectories and their impact on LBW (34, 35), we further acknowledge that additional important confounding variables—including maternal dietary intake, physical activity levels, medication use (especially antihypertensive drugs), and pregnancy-related complications (e.g., gestational diabetes, preeclampsia)—were not systematically available or complete in the selected sample of pregnant women from NHANES. Therefore, these variables could not be included in the current analysis, which may result in residual confounding and bias the reported associations. Future research should incorporate such covariates to better isolate the independent effect of blood pressure trajectories on LBW. Furthermore, since the NHANES data are observational, although a potential causal relationship was explored using DAG in this study, RCTs are needed to further validate the suggestive causal link between blood pressure trajectories and LBW. Despite statistical adjustments using DAG and IPW, the potential for residual confounding in observational studies remains. Therefore, these findings should be interpreted as suggestive of causality rather than definitive evidence. Additionally, it is important to note that the data used in this study were derived from the American population, which may limit the generalizability of the findings to other populations. Lastly, due to the sampling methodology used in NHANES, the sample size in this study was relatively small. Future studies should validate these findings using larger datasets to enhance the robustness and generalizability of the conclusions.
Conclusion
This study found that mothers with a high-medium systolic blood pressure trajectory during pregnancy had a significantly increased risk of LBW in their newborns, with this association being more pronounced in older mothers, those with a BMI >28, low income, and those with abnormal cholesterol levels. DAG analysis further suggested a potential causal association between maternal blood pressure trajectories based on three time points and LBW. This study emphasizes the importance of monitoring blood pressure trajectories during pregnancy and suggests that early identification of high-risk pregnant women and personalized interventions may help reduce the risk of LBW.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
HL: Conceptualization, Methodology, Writing – review & editing. YW: Formal analysis, Writing – original draft. WZ: Formal analysis, Writing – original draft. FM: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. ND: Writing – review & editing. XL: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Natural Science Foundation of Shanxi Province (202203021221277).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Juárez S, Ploubidis GB, Clarke L. Revisiting the ‘low BirthWeight paradox’ using a model-based definition. Gac Sanit. (2014) 28:160–2. doi: 10.1016/j.gaceta.2013.08.001
2. Chawla D. Survival of extremely-low-birth-weight neonates in India. Indian J Pediatr. (2023) 90:217–8. doi: 10.1007/s12098-023-04479-y
3. Andreoli L, Andersen J, Avcin T, Chambers CD, Fazzi EM, Marlow N, et al. The outcomes of children born to mothers with autoimmune rheumatic diseases. Lancet Rheumatol. (2024) 6:e573–86. doi: 10.1016/S2665-9913(24)00096-1
4. Alonso-lopez P, Arroyas M, Beato M, Ruiz-gonzalez S, Olabarrieta I, Garcia-Garcia ML. Respiratory, cardio-metabolic and neurodevelopmental long-term outcomes of moderate to late preterm birth: not just a near term-population. A follow-up study. Front Med (Lausanne). (2024) 11:1381118. doi: 10.3389/fmed.2024.1381118
5. Milazzo R, Garbin M, Consonni D, Casati D, Faiola S, Laoreti A, et al. Maternal hemodynamic evaluation in monochorionic twin pregnancy complicated by twin-to-twin transfusion syndrome treated with fetoscopic laser surgery. Am J Obstet Gynecol MFM. (2024) 6:101270. doi: 10.1016/j.ajogmf.2023.101270
6. Chang CL, Cai Z, Hsu SYT. Stable adrenomedullin analog mitigates placental ischemia-induced hypertension and fetal growth restriction in rats. J Hypertens. (2023) 41:1127–41. doi: 10.1097/HJH.0000000000003440
7. Luo Y, Mo Y, Xiong Y, Huang S. The association between serum uric acid and low birth weight in advance maternal age women with hypertension: an observational study. Medicine (Baltimore). (2024) 103:e38486. doi: 10.1097/MD.0000000000038486
8. Oh JH, Hong YM. Blood pressure trajectories from childhood to adolescence in pediatric hypertension. Korean Circ J. (2019) 49:223–37. doi: 10.4070/kcj.2018.0448
9. Jańczewska I, Wierzba J, Jańczewska A, Szczurek-Gierczak M, Domżalska-Popadiuk I. Prematurity and low birth weight and their impact on childhood growth patterns and the risk of long-term cardiovascular sequelae. Children (Basel). (2023) 10:1599. doi: 10.3390/children10101599
10. Teng H, Wang Y, Han B, Liu J, Cao Y, Wang J, et al. Gestational systolic blood pressure trajectories and risk of adverse maternal and perinatal outcomes in Chinese women. BMC Pregnancy Childbirth. (2021) 21:155. doi: 10.1186/s12884-021-03599-7
11. Xu L, Abudunaibi B, Zeng Z, Zhao Y, Wang Y, Guo X, et al. Relationship of various COVID-19 antibody titer with individual characteristics and prediction of future epidemic trend in Xiamen city, China. J Thorac Dis. (2024) 16:2404–20. doi: 10.21037/jtd-23-1516
12. Huang J, Xu T, Dai Y, Li Y, Tu R. Age-related differences in the number of chronic diseases in association with trajectories of depressive symptoms: a population-based cohort study. BMC Public Health. (2024a) 24:2496. doi: 10.1186/s12889-024-19975-9
13. Huang J, Chen L, Chen H, Liu Q, Tu C, Dai Y, et al. Abnormal blood biomarkers and trajectories of depressive symptoms among Chinese middle-aged and older adults. J Psychosom Res. (2025) 191:112052. doi: 10.1016/j.jpsychores.2025.112052
14. Malaba TR, Cois A, Madlala HP, Matjila M, Myer L, Newell ML, et al. Blood pressure trajectories during pregnancy and associations with adverse birth outcomes among HIV-infected and HIV-uninfected women in South Africa: a group-based trajectory modelling approach. BMC Pregnancy Childbirth. (2020) 20:742. doi: 10.1186/s12884-020-03411-y
15. Tennant PWG, Murray EJ, Arnold KF, Berrie L, Fox MP, Gadd SC, et al. Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations. Int J Epidemiol. (2021) 50:620–32. doi: 10.1093/ije/dyaa213
16. Zhu Z, Xie H, Liu S, Yang R, Yu J, Yan Y, et al. Effects of physical exercise on blood pressure during pregnancy. BMC Public Health. (2022) 22:1733. doi: 10.1186/s12889-022-14074-z
17. Broseus L, Vaiman D, Tost J, Martin CRS, Jacobi M, Schwartz JD, et al. Maternal blood pressure associates with placental DNA methylation both directly and through alterations in cell-type composition. BMC Med. (2022) 20:397. doi: 10.1186/s12916-022-02610-y
18. Herath MP, Hills AP, Beckett JM, Jayasinghe S, Byrne NM, Ahuja KDK. Trends and associations between maternal characteristics and infant birthweight among indigenous and non-indigenous people in Tasmania, Australia: a population-based study. Public Health. (2023) 221:10–6. doi: 10.1016/j.puhe.2023.05.016
19. Matsas A, Panopoulou P, Antoniou N, Bargiota A, Gryparis A, Vrachnis N, et al. Chronic stress in pregnancy is associated with low birth weight: a meta-analysis. J Clin Med. (2023) 12:7686. doi: 10.3390/jcm12247686
20. Sato N, Fudono A, Imai C, Takimoto H, Tarui I, Aoyama T, et al. Placenta mediates the effect of maternal hypertension polygenic score on offspring birth weight: a study of birth cohort with fetal growth velocity data. BMC Med. (2021) 19:260. doi: 10.1186/s12916-021-02131-0
21. Huang X, Petito LC, Shah NS, Lloyd-Jones DM, Khan SS, Cameron NA. Cholesterol, triglyceride, and glucose levels across birth cohorts in the US. JAMA Netw Open. (2024b) 7:e2449481. doi: 10.1001/jamanetworkopen.2024.49481
22. Gyselaers W. Maternal venous hemodynamic dysfunction in proteinuric gestational hypertension: evidence and implications. J Clin Med. (2019) 8:335. doi: 10.3390/jcm8030335
23. Wooldridge AL, Pasha M, Chitrakar P, Kirschenman R, Quon A, Spaans F, et al. Advanced maternal age impairs uterine artery adaptations to pregnancy in rats. Int J Mol Sci. (2022) 23:9191. doi: 10.3390/ijms23169191
24. Ortega MA, Fraile-Martínez O, García-Montero C, Sáez MA, Álvarez-Mon MA, Torres-Carranza D, et al. The pivotal role of the placenta in normal and pathological pregnancies: a focus on preeclampsia, fetal growth restriction, and maternal chronic venous disease. Cells. (2022) 11:568. doi: 10.3390/cells11030568
25. Alexander BT. Placental insufficiency leads to development of hypertension in growth-restricted offspring. Hypertension. (2003) 41:457–62. doi: 10.1161/01.HYP.0000053448.95913.3D
26. Turpin CA, Sakyi SA, Owiredu WK, Ephraim RK, Anto EO. Association between adverse pregnancy outcome and imbalance in angiogenic regulators and oxidative stress biomarkers in gestational hypertension and preeclampsia. BMC Pregnancy Childbirth. (2015) 15:189. doi: 10.1186/s12884-015-0624-y
27. Tauber Z, Burianova A, Koubova K, Mrstik M, Jirkovska M, Cizkova K. The interplay of inflammation and placenta in maternal diabetes: insights into Hofbauer cell expression patterns. Front Immunol. (2024) 15:1386528. doi: 10.3389/fimmu.2024.1386528
28. Cooke CM, Davidge ST. Advanced maternal age and the impact on maternal and offspring cardiovascular health. Am J Physiol Heart Circ Physiol. (2019) 317:H387–94. doi: 10.1152/ajpheart.00045.2019
29. Lewandowska M. Maternal obesity and risk of low birth weight, fetal growth restriction, and macrosomia: multiple analyses. Nutrients. (2021) 13:1213. doi: 10.3390/nu13041213
30. Cuevas S, Do Carmo JM, Marañón RO. Editorial: hypertension in obese women: gender-specific challenges and solutions. Front Endocrinol (Lausanne). (2025) 16:1558754. doi: 10.3389/fendo.2025.1558754
31. Terefe B, Jembere MM, Abrha NN, Asgedom DK, Assefa SK, Assimamaw NT. Pooled prevalence and multilevel determinants of stillbirths in sub-Saharan African countries: implications for achieving sustainable development goal. Glob Health Res Policy. (2025) 10:11. doi: 10.1186/s41256-024-00395-6
32. González-Fernández D, Muralidharan O, Neves PA, Bhutta ZA. Associations of maternal nutritional status and supplementation with fetal, newborn, and infant outcomes in low-income and middle-income settings: an overview of reviews. Nutrients. (2024) 16:3725. doi: 10.3390/nu16213725
33. Adachi H. Relation between low birth weight or maternal obesity during pregnancy and cardiovascular risk factors. Hypertens Res. (2024) 47:3077–8. doi: 10.1038/s41440-024-01901-6
34. Grieger JA, Clifton VL. A review of the impact of dietary intakes in human pregnancy on infant birthweight. Nutrients. (2014) 7:153–78. doi: 10.3390/nu7010153
Keywords: pregnancy blood pressure trajectories, low birth weight (LBW), group-based trajectory modeling (GBTM), directed acyclic graph (DAG), systolic blood pressure (SBP), maternal risk factors
Citation: Liu H, Wei Y, Zhang W, Meng F, Ding N and Liu X (2025) Association between three-timepoint maternal blood pressure trajectories during pregnancy and low birth weight: a longitudinal study based on NHANES 2005–2006. Front. Pediatr. 13:1604845. doi: 10.3389/fped.2025.1604845
Received: 2 April 2025; Accepted: 4 June 2025;
Published: 19 June 2025.
Edited by:
Xin Li, Sichuan University, ChinaCopyright: © 2025 Liu, Wei, Zhang, Meng, Ding and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huiqiang Liu, c3h0eWN5akAxNjMuY29t
 Huiqiang Liu
Huiqiang Liu Yanping Wei
Yanping Wei