- 1Department of Anesthesiology, Shunde Heping Surgery Hospital, Foshan, China
- 2Department of Anesthesiology, The Affiliated Shunde Hospital of Jinan University, Foshan, China
Background: Effective perioperative analgesia is critical for pediatric patients undergoing concealed penis correction surgery. Despite the utility of regional techniques like caudal block (CB) and dorsal penile nerve block (DPNB), evidence comparing their efficacy in this population remains limited. This study aimed to compare ultrasound-guided CB and DPNB for perioperative analgesia in pediatric concealed penis surgery.
Methods: In this prospective, double-blind, randomized controlled trial, 86 children (aged 5–12 years, ASA I–II) were allocated to CB (n = 44) or DPNB (n = 42) groups. All the children were induced with general anesthesia using propofol and sevoflurane, followed by laryngeal mask placement. Anesthesia was maintained with sevoflurane inhalation (spontaneous respiration preserved) under depth-of-anesthesia monitoring. The CB group received ultrasound-guided CB, while the DPNB group underwent bilateral dorsal penile nerve block, both using 0.2% ropivacaine. Primary outcomes included postoperative analgesic requirements within 24 h. Secondary outcomes encompassed pain scores, hemodynamic parameters, adverse events, and satisfaction.
Results: The CB group demonstrated significantly lower analgesic requirements (38.6% vs. 71.4%, p = 0.005) within 24 h and reduced early postoperative pain scores (at 2,4,6 h, p < 0.05). Intraoperatively, CB required fewer anesthesia deepening (20.5% vs. 52.4%, p = 0.004) and shorter surgical duration (71.1 ± 13.7 vs. 79.7 ± 9.9 min, p = 0.001). Adverse events, including tachycardia (2.3% vs. 26.2%, p = 0.004) and body movements (6.8% vs. 42.9%, p < 0.001), were less frequent with CB. Parental and surgeon satisfaction were higher in the CB group (p = 0.049 and p < 0.001).
Conclusions: Ultrasound-guided CB provides superior perioperative analgesia, fewer complications, and higher satisfaction compared to DPNB in pediatric concealed penis surgery, supporting its preference for this specific procedure in clinical practice.
Clinical Trial Registration: https://www.chictr.org.cn/showproj.html?proj=178288, identifier ChiCTR2200065359.
1 Introduction
Effective perioperative pain management is crucial for pediatric patients undergoing surgery, as inadequate analgesia may prolong recovery, increase postoperative complications, parental anxiety and medical costs (1–3). The ideal anesthetic technique should provide optimal analgesia while minimizing risks. Although general endotracheal anesthesia effectively resolved intraoperative pain management, it inadequately meets postoperative analgesic demands. Thereby, many surgical procedures have gradually adopted regional anesthesia to improve postoperative pain management and patient recovery (4). Regional anesthesia techniques offer both intraoperative and postoperative analgesia, and their combination with general anesthesia intubation is particularly valuable (5). Despite significant advances in pediatric anesthesia, the selection of the most effective and safest regional anesthesia technique for these procedures remains controversial.
Caudal block (CB) and dorsal penile nerve block (DPNB) are two commonly used regional anesthetic techniques in pediatric urological surgery, each with distinct advantages and limitations (6, 7). CB provides extensive neural blockade covering the sacral dermatomes (S2–S4), which innervate the penis, perineum, and relevant visceral structures involved in penile surgery (8–10). This extensive coverage targets both somatic and visceral nociceptive pathways. Conversely, DPNB provides localized analgesia but often require bilateral blockade in pediatric patients with variable success rates (11, 12). The application of ultrasound-guided technology has improved the accuracy of these two anesthesia procedures, yet evidence comparing their intraoperative and postoperative analgesic efficacy in concealed penis correction surgery remains insufficient. Elucidating the analgesic effectiveness and safety of CB vs. DPNB could significantly improve pain management strategies for this vulnerable patient population.
This randomized controlled trial was designed to compare the perioperative analgesic efficacy between ultrasound-guided CB and DPNB in pediatric concealed penis surgery. This study evaluates perioperative safety, analgesic consumption, pain scores, and adverse event incidence to optimize pain management protocols for this common pediatric urological procedure, ultimately aiming to enhance clinical outcomes and patient satisfaction.
2 Methods
2.1 Study design
A prospective, randomized, double-blind study was conducted from January 2022 to September 2024. The study received approval from the Ethics Committee of the Shunde Heping Surgical Hospital (Approval No. HPYY-LL-2022001) and was registered with the Chinese Clinical Trial Registry (Registration No. ChiCTR2200065359). Informed consent was obtained from the family members of the children for this study.
2.2 The inclusion and exclusion criteria
Children scheduled to undergo pediatric concealed penis correction surgery.
The inclusion criteria: Age between 5 and 12 years old; confirmed diagnosis of concealed penis through clinical physical examination and imaging examinations such as ultrasound. American Society of Anesthesiologists (ASA) physical status classification of grade I–II.
Exclusion criteria: Those with severe cardiac, hepatic, or renal diseases; neurological disorders; a known allergy to anesthetic agents; mental health conditions or impaired cognitive function; a history of hemorrhagic disorders; or recent use of analgesics or sedatives within the past three months; fail to complete the required study observations, have incomplete records, or exhibit extremely poor compliance.
2.3 Grouping and blinding method
Children were randomized using a computer-generated random number table. Each patient was assigned a unique identification number and allocated to one of two groups based on the parity of the random number: patients with odd numbers were assigned to the CB group, while those with even numbers were assigned to the DPNB group. A double-blind design was used, with patients, parents, and the research team (surgeons and data collectors) unaware of group assignments. During the procedure, an independent anesthesia team performed the regional block, while the surgical team and the intraoperative/postoperative assessment team remained unaware of the group allocations. After the anesthesia procedure was completed, a separate intraoperative assessment team collected relevant data. Postoperative pain assessments were conducted by an independent nursing team, who were also blinded to the group assignments.
2.4 Anesthesia procedure
Upon entering the operating room, children underwent intravenous injection of propofol at a dose of 2 mg/kg and inhalational induction with sevoflurane, followed by laryngeal mask insertion. Anesthesia was maintained with sevoflurane inhalation while preserving spontaneous respiration. Standard monitoring was applied to all patients, including mean arterial pressure (MAP), heart rate (HR), oxygen saturation (SpO2), depth of anesthesia, body temperature, respiratory rate (RR), end-tidal carbon dioxide concentration (ETCO2), and end-tidal concentration of inhaled anesthetics.
For the CB group, patients were placed in the left lateral decubitus position with their legs flexed toward the abdomen to fully expose the sacral region. The skin around the sacral hiatus was routinely disinfected. Using an ultrasound machine equipped with a high-frequency linear array probe, the probe was placed along the midline of the dorsal sacrum to obtain a transverse view of the sacral hiatus. After identifying the sacral cornu and sacrococcygeal ligament, the probe was rotated 90° to obtain a longitudinal view. A 22G needle was inserted using an in-plane technique under direct ultrasound visualization. The needle tip position within the sacral canal was confirmed by both a distinct loss of resistance as it penetrated the sacrococcygeal ligament and real-time ultrasound imaging showing its path and final location. After negative aspiration for blood or cerebrospinal fluid, 0.2 ml/kg of 0.2% ropivacaine was injected. Ultrasound imaging confirmed cephalad spread of local anesthetic within the epidural space, targeting blockade of the S2–S4 nerve roots which innervate the penis and perineum. Patients were then placed supine.
For the DPNB group, patients were placed in the supine position with their legs abducted and slightly flexed to fully expose the penile region. The skin around the root of penis was routinely disinfected. Using an ultrasound machine equipped with a high-frequency linear array probe, the probe was placed transversely at the root of penis to obtain a clear transverse view of the urethral sponge, bulbospongiosus, dorsal artery and vein of penis, Buck's fascia, and tunica albuginea. The dorsal nerve of penis, located between Buck's fascia and the tunica albuginea and accompanying the dorsal artery of penis, appeared as a hypoechoic cord-like structure on the ultrasound image. A 22G block needle was inserted using an in-plane technique under ultrasound guidance, advancing from the lateral side of the root of penis toward the dorsal side. The needle was advanced through the hyperechoic superficial fascia, and a loss of resistance indicated that the needle tip had passed through the superficial fascia. The needle tip was then positioned between Buck's fascia and the tunica albuginea, adjacent to the dorsal artery of penis. After confirming the absence of blood upon aspiration, 0.2% ropivacaine was injected at a dose of 0.1 ml/kg. The same procedure was repeated on the contralateral side using an identical concentration and volume of local anesthetic.
Surgery began 20 min after block completion in both groups. Rescue anesthesia (propofol 1 mg/kg and fentanyl 1 μg/kg IV) was administered if body movement or a HR increase ≥20% from baseline occurred during skin incision, with repeat doses as needed.
2.5 Outcomes
1. The primary outcome was the proportion of patients requiring analgesics within 24 h postoperatively. Rescue analgesia (diclofenac sodium 25 or 50 mg rectally or intravenous ketorolac tromethamine 15 or 30 mg based on body weight) was administered if the resting pain score > 3 during this period.
2. Secondary outcome
(1) Pain assessment: VAS scores (0 = no pain, 10 = severe pain) were recorded at 2, 4, 6, 12, 24, and 48 h postoperatively. For verbal children, self-reported pain levels were obtained. For non-verbal children, pain intensity was assessed using the FLACC (Face, Legs, Activity, Cry, Consolability) behavioral scale (13).
(2) Surgical and anesthetic parameters: Surgery duration (duration from skin incision to wound closure), anesthesia time (duration from induction to the last administration of anesthetic agents), recovery time (duration from surgery completion to full awakening), anesthetic drug consumption (sevoflurane and propofol administered during the procedure). The number of cases in which the anesthesia needed to be deepened, as well as the MAP, HR, SpO2, RR were recorded before anesthesia (T1) and at the time of skin incision (T2).
(3) Adverse events: Intraoperative and postoperative adverse events were documented, including tachycardia (HR increase >20% from baseline), intraoperative body movement (the child's body showed obvious involuntary movements, which affected the surgical operation), emergence agitation (restlessness, disorientation, or thrashing during recovery), postoperative nausea and vomiting (PONV), lower limb weakness, urinary retention, and wound complications (e.g., bleeding, edema, infection, and itching).
(4) Satisfaction evaluation: Parents’ satisfaction was assessed 24 h postoperatively via a questionnaire administered by an independent anesthesia nurse. The questionnaire evaluated pain relief, recovery quality, and adverse events. Surgeons’ satisfaction was evaluated immediately post-surgery using a questionnaire focusing on patient cooperation and analgesic efficacy during the procedure. Both evaluations categorized satisfaction as “satisfied,” “partially satisfied,” or “unsatisfied” based on predefined criteria.
2.6 Statistical analysis
Sample size calculation: The primary observation indicator of this study was the proportion of children using analgesics within 24 h after surgery. The results of the preliminary trial showed that the proportion of children using analgesics within 24 h after surgery was 30% in the CB group and 60% in the DPNB group. After setting a significance level of 5% and a power of 80%, and fully taking into account a 5% dropout rate, the required sample size for each group was determined to be 44 cases.
The statistical analysis was performed using IBM SPSS Statistics (version 27.0). Continuous variables were expressed as mean ± standard deviation (SD) if normally distributed, or median (interquartile range [IQR]) if non-normally distributed. Normality of data distribution was assessed using the Shapiro–Wilk test. Categorical variables were described as frequency (percentage). Intergroup comparisons were conducted in the following ways: for continuous variables, independent t-tests were utilized for data with a normal distribution, while the Mann - Whitney U test was applied to non-parametric data. As for categorical variables, either the Chi-square test or Fisher's exact test was used, depending on the expected cell frequencies. p < 0.05 was considered statistically significant.
3 Results
3.1 Study flowchart and basic information of children
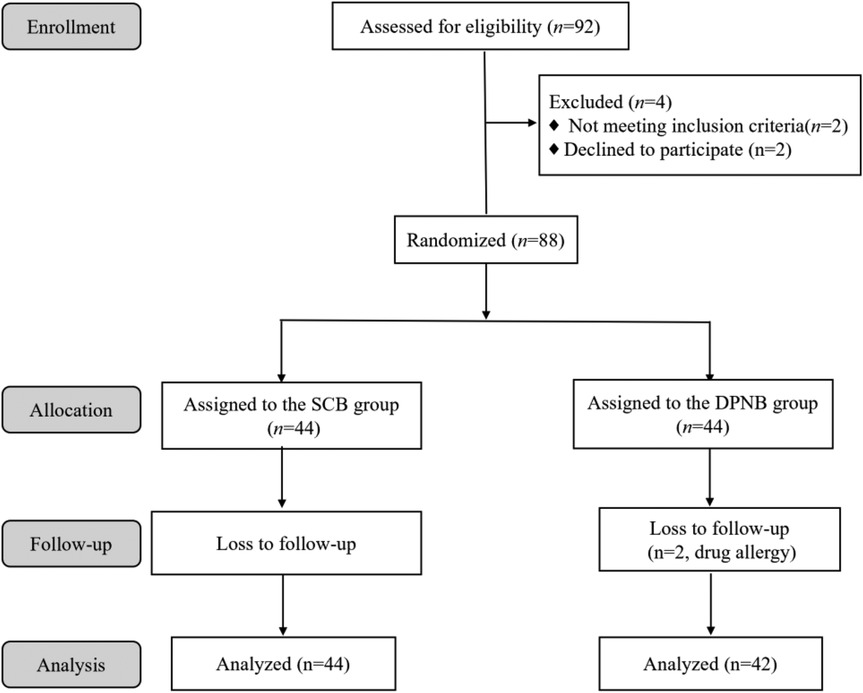
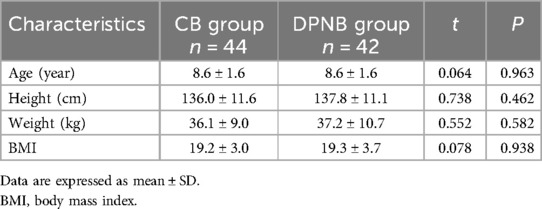
A total of 92 pediatric patients were initially assessed for eligibility, of whom 4 were excluded. Consequently, 88 patients were randomly assigned to either the CB or DPNB group, with 44 patients in each group. Two patients from the DPNB group were lost to follow-up due to drug allergies, resulting in a final sample size of 86 patients who completed the study. This included 44 patients in the CB group and 42 patients in the DPNB group, as shown in Figure 1. No significant differences in age, height, weight, or body mass index (BMI) between groups (all p > 0.05), as shown in Table 1.
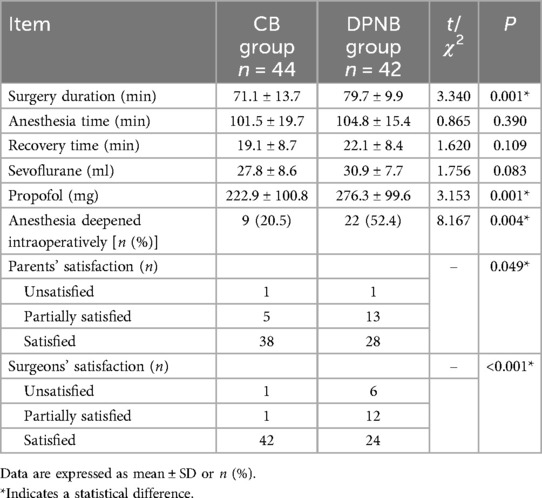
3.2 Perioperative related indicators and satisfaction
CB group demonstrated a shorter surgery duration (P = 0.001), lower propofol consumption (P = 0.001), and fewer children of intraoperative anesthesia deepening (P = 0.004). Both parents and surgeons demonstrated significantly higher satisfaction with outcomes in CB group compared to DPNB group (p = 0.049 and p < 0.001, respectively). Other measures like anesthesia time, recovery time, and drug usage (sevoflurane) showed no significant differences, as shown in Table 2.
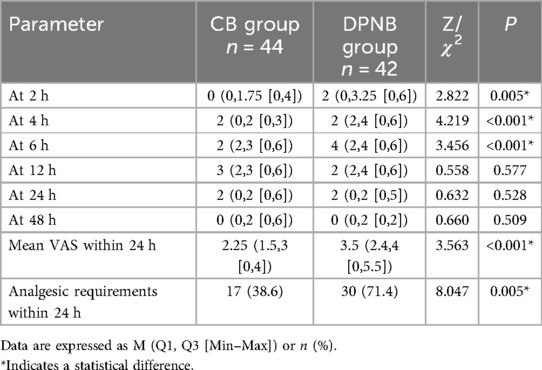
3.3 Postoperative pain scores and analgesic requirements
Significantly lower pain scores were observed in CB group compared to DPNB group at 2 h, 4 h, 6 h (P < 0.05). No significant differences were noted at 12, 24, or 48 h (P > 0.05). The mean VAS within 24 h was significantly lower in the CB group (P < 0.001). Additionally, the CB group demonstrated a reduced proportion of analgesic requirements within 24 h (38.6% vs. 71.4%, p = 0.005), as shown in Table 3.
3.4 The proportion of children with pain scores > 3 of postoperative
The proportion of children with clinically significant pain scores >3 demonstrated distinct patterns between the two groups across postoperative time points (Figure 2). Statistically significant intergroup differences were observed at 2 h (2.3% vs. 23.8%., p = 0.005), 4 h (0 vs. 32.9%, p < 0.001), and 6 h (18.2% vs. 54.1%, p = 0.001). The proportion of children with pain scores >3 reached a peak at 6 h. Subsequently, it gradually decreased over time. Moreover, at 48 h, the pain of the children in both groups was basically and completely relieved.
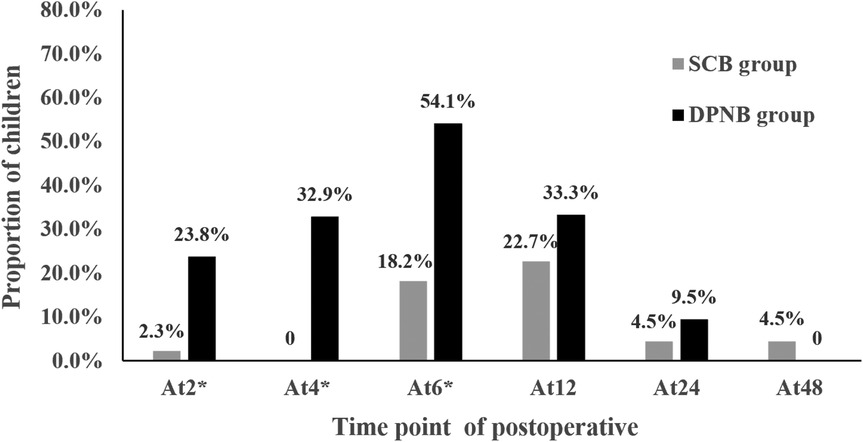
Figure 2. Proportion of children with pain scores > 3 at different time points of postoperative. *Indicates a statistical difference.
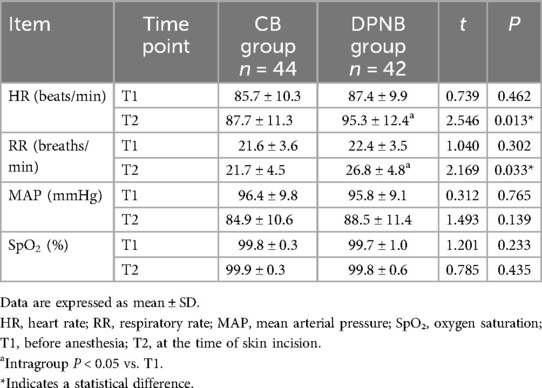
3.5 Hemodynamic changes during skin incision
The DPNB group exhibited significantly higher HR and RR during skin incision compared to CB group (p = 0.013 and p = 0.033, respectively). Intragroup analysis revealed a significant increase in HR and RR from T1 to T2 in the DPNB group (p < 0.05), while no significant change occurred in the CB group. MAP and SpO₂ levels showed no significant differences between groups, as shown in Table 4.
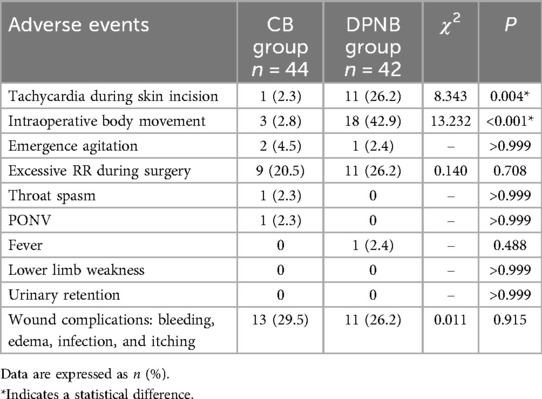
3.6 Adverse events
More rate in the DPNB group (26.2%) than in the CB group (2.3%, p = 0.004) in tachycardia during skin incision. Higher in the DPNB group (42.9%) compared to the CB group (6.8%, p < 0.001) in intraoperative body movement. Other adverse reactions showed no significant differences between groups, as shown in Table 5.
4 Discussion
This study demonstrates that ultrasound-guided CB provides superior perioperative analgesia compared to DPNB in pediatric concealed penis correction surgery. These conclusions are supported by the following findings: the CB group required fewer intraoperative anesthesia deepening interventions, exhibited significantly reduced postoperative analgesic requirements within 24 h, lower pain scores during early recovery, fewer complications, and higher satisfaction rates.
The superior efficacy of CB is anatomically grounded. It reliably blocks the sacral nerve roots (S2–S4), which carry both somatic sensory fibers (via the pudendal nerve) innervating the penile shaft and glans, and autonomic fibers (via the pelvic plexus) innervating deeper penile structures, the urethra, and bladder neck (8, 14–16). This dual blockade effectively addresses the somatic and visceral nociceptive input generated during concealed penis surgery (16, 17). In contrast, DPNB primarily targets the terminal somatic branches (dorsal nerves of the penis) and lacks significant visceral coverage (18–20). Our results confirm this broader blockade: CB significantly reduced intraoperative hemodynamic fluctuations (tachycardia, elevated HR/RR during incision) and body movements, indicating better suppression of the surgical stress response mediated via unblocked visceral pathways during DPNB. The lower proportion of patients requiring rescue analgesics within 24 h (38.6% vs. 71.4%) and significantly reduced early pain scores (2 h, 4 h, 6 h) in the CB group further reflect its more comprehensive and prolonged analgesic effect, likely encompassing both somatic incision pain and visceral discomfort from tissue manipulation and bladder/urethral traction.
Ultrasound guidance enhanced the precision and safety of both techniques in this study. For CB, real-time visualization allowed confirmation of needle placement within the sacral canal and monitoring of local anesthetic spread (21, 22), mitigating challenges posed by anatomical variations in the sacral hiatus (9, 15). Our technique utilized longitudinal and transverse views to confirm needle tip position post-loss-of-resistance, ensuring accurate drug delivery targeting the S2–S4 roots. The use of low-concentration ropivacaine (0.2%, 0.2 ml/kg) minimized motor block risks; no urinary retention or lower limb weakness occurred, consistent with sparing of higher sacral/lumbar roots responsible for leg movement and bladder voiding (23). Conversely, the higher incidence of tachycardia, movement, and subsequent propofol/fentanyl requirements in the DPNB group likely stem from incomplete blockade of deeper nociceptive pathways despite technically adequate bilateral somatic blocks under ultrasound (11, 24).
Postoperative wound complications (bleeding, edema, infection, itching) occurred in >26% of patients in both groups. It is essential to clarify that these complications are primarily determined by surgical technique and postoperative wound care, not by the choice of regional anesthetic technique (CB or DPNB). Other adverse events showed no significant differences. Higher parental satisfaction with CB (p = 0.049) reflects effective analgesia reducing caregiver anxiety (25, 26). Greater surgeon satisfaction (p < 0.001) is attributable to fewer intraoperative disruptions and smoother procedural flow with CB.
Limitations of this study warrant consideration. First, the single-center design and moderate sample size (n = 86) may limit generalizability. Second, while using validated FLACC and VAS scales, pain assessment remains inherently subjective, especially in preverbal children. Third, anatomical variations in the sacral canal (present in up to 20% of children) can challenge CB placement even with ultrasound, potentially impacting success rates (9, 15). Fourth, our findings are specific to concealed penis correction surgery; extrapolation to other pediatric urological procedures requires caution. Future research should include: (1) multicenter randomized trials with larger samples; (2) longer-term outcome assessment; (3) investigation of adjuvants (e.g., dexmedetomidine) to prolong CB duration; and (4) comparison with other advanced regional techniques like pudendal nerve block.
In conclusion, ultrasound-guided CB offers superior perioperative analgesia, fewer complications, and higher satisfaction compared to DPNB in pediatric concealed penis surgery. The extensive blockade of S2–S4 dermatomes effectively addresses both somatic and visceral pain components of this procedure. These findings support CB as the preferred regional anesthetic technique for this specific surgery, although broader recommendations await validation through multicenter studies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the study received approval from the Ethics Committee of the Shunde Heping Surgical Hospital (Approval No. HPYY-LL-2022001). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
ZL: Writing – review & editing, Software, Writing – original draft. YS: Data curation, Writing – review & editing. HL: Methodology, Writing – review & editing. ZC: Writing – review & editing, Data curation, Methodology. YL: Data curation, Writing – review & editing. SW: Data curation, Writing – review & editing, Investigation. NL: Writing – review & editing, Data curation. ZZ: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Foshan Self-funded Science and Technology Innovation Project, Number: 2220001005144 and 2018AB000363; Key medical talents training project of Shunde District. Beijing Medical Award Foundation, Number: YXJL-2021-0307-0584. Medical Association Foundation of Jinan University (YXJC2022003).
Acknowledgments
We express our gratitude to all the staff involved in this research, as well as to the gynecological abortion clinic for providing the venue.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. He HG, Zhu L, Chan SW, Klainin-Yobas P, Wang W. The effectiveness of therapeutic play intervention in reducing perioperative anxiety, negative behaviors, and postoperative pain in children undergoing elective surgery: a systematic review. Pain Manag Nurs. (2015) 16(3):425–39. doi: 10.1016/j.pmn.2014.08.011
2. Fan YL, Qian JL, Ma EL, Stricker PA, Zuo YX. Incidence and risk factors of postoperative severe discomfort after elective surgery under general anesthesia: a prospective observational study. J Perianesth Nurs. (2021) 36(3):253–61. doi: 10.1016/j.jopan.2020.10.006
3. van Boekel RLM, Warlé MC, Nielen RGC, Vissers KCP, van der Sande R, Bronkhorst EM, et al. Relationship between postoperative pain and overall 30-day complications in a broad surgical population: an observational study. Ann Surg. (2019) 269(5):856–65. doi: 10.1097/sla.0000000000002583
4. Fanelli A, Balzani E, Memtsoudis S, Abdallah FW, Mariano ER. Regional anesthesia techniques and postoperative delirium: systematic review and meta-analysis. Minerva Anestesiol. (2022) 88(6):499–507. doi: 10.23736/s0375-9393.22.16076-1
5. Relland LM, Neel ML, Gehred A, Maitre NL. Regional anesthesia in neonates and infants outside the immediate perioperative period: a systematic review of studies with efficacy and safety considerations. Paediatr Anaesth. (2021) 31(2):132–44. doi: 10.1111/pan.14042
6. Naja ZM, Ziade FM, Kamel R, El-Kayali S, Daoud N, El-Rajab MA. The effectiveness of pudendal nerve block versus caudal block anesthesia for hypospadias in children. Anesth Analg. (2013) 117(6):1401–7. doi: 10.1213/ANE.0b013e3182a8ee52
7. Choudhry DK, Heredia L, Brenn BR, Brown M, Carvalho NF, Whaley MC, et al. Nerve stimulation guided bilateral pudendal nerve block versus landmark-based caudal block for hypospadias repair in young children: a prospective, randomized, pragmatic trial. Reg Anesth Pain Med. (2022) 47(12):744–8. doi: 10.1136/rapm-2022-103680
8. Karagözlü Akgül A, Canmemiş A, Eyvazov A, Hürel H, Kiyan G, Umuroğlu T, et al. Effects of caudal and penile blocks on the complication rates of hypospadias repair. Balkan Med J. (2022) 39(4):239–45. doi: 10.4274/balkanmedj.galenos.2022.2022-1-62
9. Nastoulis E, Tsiptsios D, Chloropoulou P, Karapepera V, Thomaidis V, Pavlidis P, et al. Morphological and morphometric features of sacral hiatus and its clinical significance in caudal epidural anaesthesia. Folia Morphol (Warsz). (2023) 82(3):603–14. doi: 10.5603/FM.a2022.0078
10. Kao SC, Lin CS. Caudal epidural block: an updated review of anatomy and techniques. Biomed Res Int. (2017) 2017:9217145. doi: 10.1155/2017/9217145
11. Ozen V, Yigit D. Caudal epidural block versus ultrasound-guided dorsal penile nerve block for pediatric distal hypospadias surgery: a prospective, observational study. J Pediatr Urol. (2020) 16(4):438.e1–e8. doi: 10.1016/j.jpurol.2020.05.009
12. Ozen V, Ozen N. Ultrasound-guided pudendal nerve block versus ultrasound-guided dorsal penile nerve block for pediatric distal hypospadias surgery. Urol Int. (2023) 107(4):370–6. doi: 10.1159/000521718
13. Nilsson S, Finnström B, Kokinsky E. The FLACC behavioral scale for procedural pain assessment in children aged 5-16 years. Paediatr Anaesth. (2008) 18(8):767–74. doi: 10.1111/j.1460-9592.2008.02655.x
14. Yan T-T, Yang X-L, Wang S, Chen J-Q, Hu J-C, Zhou L, et al. Application of continuous sacral block guided by ultrasound after comprehensive sacral canal scanning in children undergoing laparoscopic surgery: a prospective, randomized, double-blind study. J Pain Res. (2023) 16:83–92. doi: 10.2147/JPR.S391501
15. Bagheri H, Govsa F. Anatomy of the sacral hiatus and its clinical relevance in caudal epidural block. Surg Radiol Anat. (2017) 39(9):943–51. doi: 10.1007/s00276-017-1823-1
16. Pastelín CF, Pacheco P, Camacho M, Cruz Y. Another component of the pelvic plexus that innervates the penis in the rat. Urology. (2011) 78(1):232.e7–e13. doi: 10.1016/j.urology.2011.03.020
17. Lee SH, Koh KS, Song WC. Macro/microscopic distribution of the dorsal nerve of penis in human glans penis. J Anat. (2020) 237(5):849–53. doi: 10.1111/joa.13263
18. Ozen V, Yigit D. A comparison of the postoperative analgesic effectiveness of ultrasound-guided dorsal penile nerve block and ultrasound-guided pudendal nerve block in circumcision. Urol Int. (2020) 104(11-12):871–7. doi: 10.1159/000509173
19. Yiğit D, Özen V, Kandirici A, Dokucu A. Ultrasound-guided dorsal penile nerve block is a safe block in hypospadias surgery: a retrospective clinical study. Medicine (Baltimore). (2022) 101(26):e29700. doi: 10.1097/md.0000000000029700
20. Aggarwal A, Aggarwal A, Harjeet Sahni D. Morphometry of sacral hiatus and its clinical relevance in caudal epidural block. Surg Radiol Anat. (2009) 31(10):793–800. doi: 10.1007/s00276-009-0529-4
21. Ahiskalioglu A, Yayik AM, Ahiskalioglu EO, Ekinci M, Gölboyu BE, Celik EC, et al. Ultrasound-guided versus conventional injection for caudal block in children: a prospective randomized clinical study. J Clin Anesth. (2018) 44:91–6. doi: 10.1016/j.jclinane.2017.11.011
22. Karaca O, Pinar HU, Gokmen Z, Dogan R. Ultrasound-guided versus conventional caudal block in children: a prospective randomized study. Eur J Pediatr Surg. (2019) 29(6):533–8. doi: 10.1055/s-0038-1676980
23. Heine C, Rovner M, Irick W, Wolf B, McCoy N, Massman K, et al. Effect of clonidine on duration of high-volume, low-concentration caudal epidurals. Cureus. (2024) 16(12):e75151. doi: 10.7759/cureus.75151
24. Toprak H, Kandemir E. Comparison of the effects of ring block and dorsal penile nerve block on parental satisfaction for circumcision operation in children: randomized controlled trial. Pediatr Surg Int. (2024) 40(1):101. doi: 10.1007/s00383-024-05681-5
25. Lim PS, Fortier MA, Kaplan SH, Masague SG, Kain ZN. Predictors of pain concordance among caregiver-child dyads undergoing elective surgery. Paediatr Anaesth. (2025) 35(5):359–66. doi: 10.1111/pan.15082
Keywords: caudal block, dorsal penile nerve block, pediatric analgesia, regional anesthesia, concealed penis surgery
Citation: Lin Z, Shao Y, Li H, Chen Z, Li Y, Wu S, Liu N and Zhang Z (2025) Comparing the analgesic effects of ultrasound-guided caudal block and dorsal penile nerve block in pediatric concealed penis correction surgery: a randomized controlled trial. Front. Pediatr. 13:1607309. doi: 10.3389/fped.2025.1607309
Received: 7 April 2025; Accepted: 8 July 2025;
Published: 24 July 2025.
Edited by:
Walid Farhat, University of Wisconsin-Madison, United StatesReviewed by:
Shin-Hyo Lee, Wonkwang University, Republic of KoreaSalah Nagla, Tanta University, Egypt
Karim Awad, Bristol Royal Hospital for Children, United Kingdom
Copyright: © 2025 Lin, Shao, Li, Chen, Li, Wu, Liu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhongqi Zhang, anh6enExMUAxNjMuY29t
†These authors have contributed equally to this work
 Zhuopeng Lin1
Zhuopeng Lin1 Zhongqi Zhang
Zhongqi Zhang