- 1Faculty of Social Work, Central and Northern Alberta Region, University of Calgary, Edmonton, AB, Canada
- 2Edwin S.H. Leong Centre for Healthy Children, University of Toronto, Toronto, ON, Canada
- 3Department of Anesthesiology, Cumming School of Medicine, Perioperative and Pain Medicine, University of Calgary, Calgary, AB, Canada
- 4Child Health Evaluative Services, Hospital for Sick Children, Toronto, ON, Canada
- 5Children’s Healthcare Canada, Ottawa, ON, Canada
- 6Lawrence Bloomberg Faculty of Nursing, University of Toronto, Toronto, ON, Canada
Objective: Synchronous virtual care comprises real-time, online-mediated healthcare. This approach has increasingly been used in pediatrics, largely implemented in the COVID-19 pandemic. Evidence is limited on the impacts of this mode of care delivery on patient and family experience and care quality. To our knowledge, this is the first scoping review to amalgamate existing knowledge about the perceived impact of synchronous virtual care as it is experienced by children and their families across multiple disciplines.
Methods: Following guidance from the Joanna Briggs Institute, a search of the peer reviewed, published literature was conducted employing multiple databases: APA PsycInfo, CINAHL, EBSCO, Embase, and OVID. Reviewed articles were published in English from January 1, 2013 to December 31, 2023, and addressed virtual care for children and their families. The initial search generated 1,079 articles, which underwent abstract and then full-text screening. A total of 157 full text articles were screened, yielding 117 articles from which data was extracted.
Results: Virtual care interventions, generally appearing in the last decade (2013–2023), have been largely studied using quantitative approaches. They tend to be positively viewed by youth and parents as indicated by identified benefits and general satisfaction. However, articles report both facilitating and hindering elements of virtual care, and barriers are reported that reflect inequities associated with social determinants of health. Such barriers are shown to impede the use of virtual care among some marginalized communities. The review indicates that effective virtual care approaches require (a) program/organizational infrastructure support, (b) training for both service providers and users, and (c) tailoring to clinical needs.
Conclusion: Considering virtual care “fit” for target patients and families is important. Implications for clinical care as well as guidelines for future research are offered.
1 Introduction
Virtual care is an umbrella term for technology-based support in healthcare. Diverse terms to describe virtual care or telehealth have been used such as synchronous monitoring (1–3), telerehabilitation (4), eHealth (1, 5), mHealth (6), and web-based education (7). Pediatric virtual care has been applied in a range of clinical populations such as children and youth with autism (2), chronic illness (5), cancer (8), and acquired brain injury (9). At present, there is a growing body of reviews assessing the role of virtual care, however, these reviews have specific focus on (i) populations with specific conditions such as children with special health care needs (1), autism (2), asthma (3), chronic pulmonary disease (5), diabetes (10) and chronic illness (11), (ii) delivery within specific pediatric specialties such as rehabilitation (4) or surgery (6), (iii) certain online platforms such as mobile, eHealth or mHealth (6–9), (iv) geographical regions such as rural settings (12) and (v) research designs such as interventions that have been evaluated using random controlled trials (13).
Reviews have examined benefits and limitations of virtual care. Overall, general acceptance of virtual care in clinical practice and research has been reported by patients and family caregivers (3, 5–9, 12–16), physicians (17), and a range of health care professionals (18–23). Reviews conclude that virtual care can reduce costs related to travel (20, 24) for family caregivers and lower staff labor costs for organizations (18). However, patients and/or their caregivers have cited challenges with virtual care including limited personal interaction (24), technological challenges (24), and concerns with security of health information (6, 16) and privacy risks (14).
During the COVID-19 pandemic, there was widespread implementation of virtual care. While the literature has variably addressed the access, use, and impact of virtual care, there has been limited attention given to patient and family experiences of virtual care, thus raising questions about children/youth and caregiver preferences in using virtual care. To address this gap, a scoping review of the last decade of literature was undertaken to assess how virtual care intervention have been delivered and evaluated, and have impacted children and their families. An additional aim was to review how interventions incorporated equity considerations, particularly the social determinants of health (SDOH). We defined SDOH as “the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks” (25). SDOH also consider the broader forces and systems that shape daily life including economic and social policies, norms, political structures and systemic factors (e.g., racism, ableism, sexism) (25). To this end, this study addressed the following questions: (1) What virtual care approaches have been used in pediatric care relative to child and family experiences and benefits, (2) What are the aims and how are virtual care approaches implemented in clinical practice?, (3) What are families’ experiences and perceptions of virtual care?, (4) What study approaches have been used to evaluate children/youth and family experiences of virtual care?, and (5) How are SDOH considered in the design and/or implementation plans of virtual care?
2 Methods
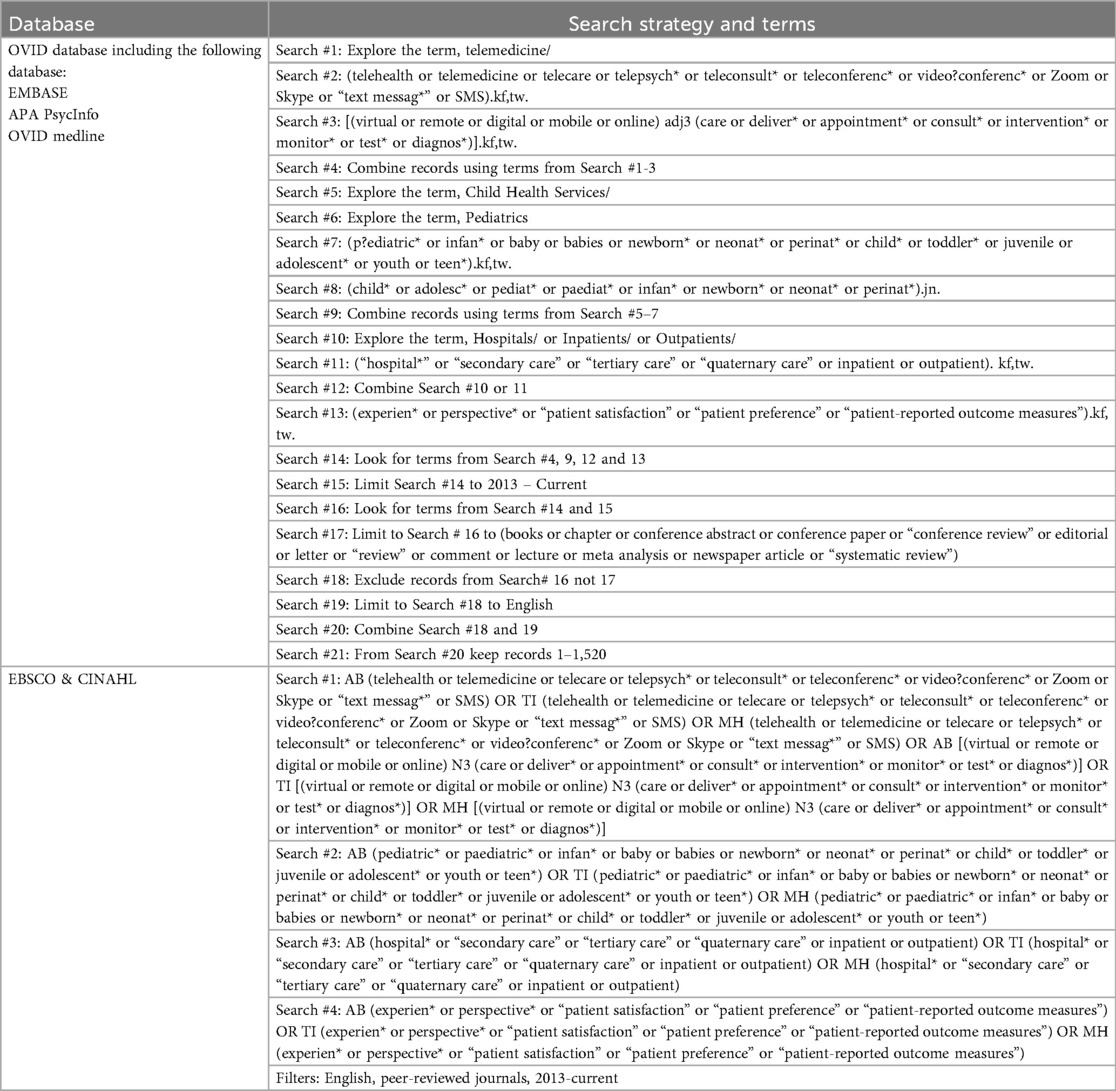
The scoping review was informed by guidelines outlined by the Joanna Briggs Institute (JBI) (26, 27). A search of the literature published between January 1, 2013, and December 31, 2023, was led by a research colleague with expertise in scoping reviews using APA PsycInfo, CINAHL, EBSCO, Embase, and MEDLINE electronic databases. Search terms were as follows: virtual (e.g., telemedicine, telehealth, telecare, teleconference, Zoom), pediatrics (e.g., infants, child, toddler, adolescent, youth), hospital (e.g., secondary care, tertiary care, inpatient, outpatient) and experience (e.g., perspectives, satisfaction, preferences) (search strategy in Table 1). Study inclusion criteria were: (1) peer-reviewed, (2) published in English, (3) focused on pediatric synchronous virtual care (e.g., online and/or phone) based on the following definition, “.real-time, virtual, direct-to-patient appointments. Synchronous telehealth happens in live, real-time settings, in which the patient interacts with a provider(s), usually via phone or video. Providers and patients communicate directly, often resulting in a diagnosis, treatment plan, and/or prescription” (28), (5) inclusive of pediatric patients (including birth to 18 years) and/or their family, (6) inclusive of primary data (e.g., surveys, interviews), and (7) inclusive of outcomes of family satisfaction, preferences and/or perspectives about the virtual care approaches. Exclusion criteria consisted of: (1) conference/meeting, proceedings, congress, guidelines, dissertation, or a review (e.g., literature review, systematic review, scoping review, meta-analysis), (2) sole focus on healthcare provider perspectives, (3) only administrative data provided, (4) development of a test or model of virtual care, and/or (5) focus on obstetrical care. At the last stage, when we extracted information from a full text review of each article, we examined how SDOH were addressed, including equity considerations (29, 30). Addressing these considerations emerged as critical in bringing an equity, diversity, inclusion, and accessibility (EDIA) lens to this work, in terms of interrogating study inclusion of diverse groups relative to the utility, impact and experience of virtual care. For reviews such as this current one, an EDIA lens can highlight how marginalized groups may experience unique challenges in accessing care.
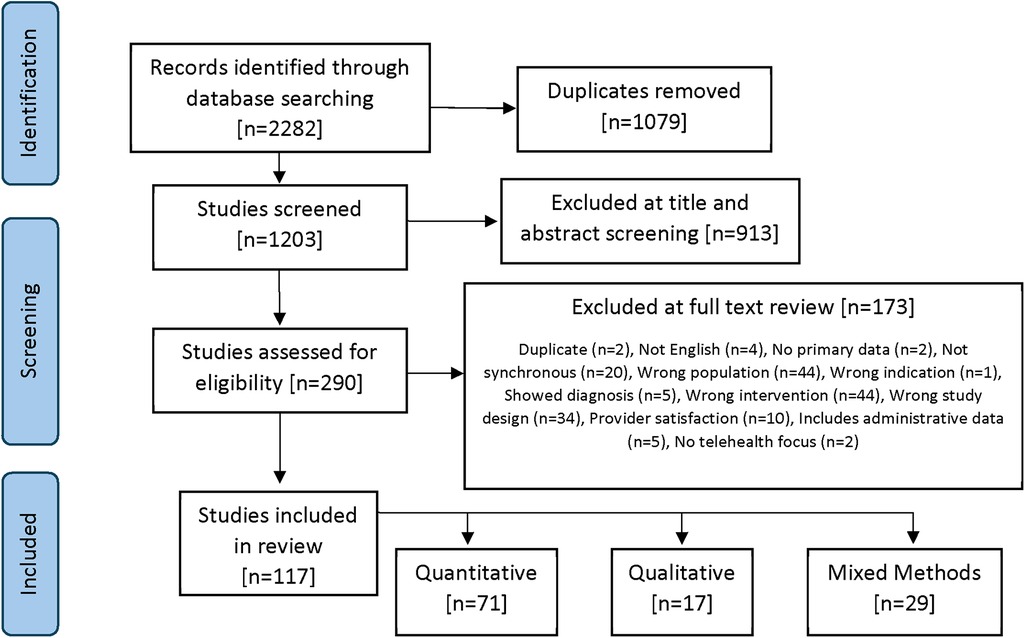
Using Covidence Systematic Review software, the search yielded 1,079 articles after removal of duplicates. Two rounds of screening were conducted, as follows. Two independent reviewers examined all titles and abstracts, and a third reviewer resolved disagreements as needed. Based on inclusion and exclusion criteria, the number of included articles was reduced to 157, which were subsequently advanced for full article review. This second review resulted in 117 articles (Figure 1). Article review was conducted by team leads (RTZ, SS), with supervision by team members who bring extensive experience in secondary review. As this was a scoping review, institutional ethics board approval was not required.
2.1 Data extraction
Following full-text review, a total of 117 articles, as noted above, were included in this review. Through an iterative process, we generated a table to document specific features of existing studies. These articles were independently coded for retrieval of the following information: study/article title, year of publication, author(s), country, study objectives, research questions/hypothesis, study design, data collection methodology, sample size, sample characteristics, purpose of study, definition of virtual care approach, subspecialty in which approach was studied, how approach was implemented, analysis methods, outcomes, key recommendations, and study strengths and limitations. Two reviewers (RTZ, SS) extracted and analyzed the data. Given that this initiative was a scoping review, we did not appraise study design methods.
3 Results
We addressed key questions to interrogate virtual care in reviewed articles, as follows: (1) how has virtual care been implemented?; (2) what are study objectives and aims of the virtual care application?, (3) by whom, when, where and how has virtual care been evaluated?, (4) how does virtual care address SDOH?, and (5) how do children, youth and families experience virtual care (e.g., benefits, satisfaction, challenges, and advice offered in improving care)? These questions are addressed below. Within the Supplementary Section, Supplementary Table 1 provides the full list of the 117 articles including details of each study aim and design, the virtual care intervention addressed and outcomes. Supplementary Table 2 summarizes findings reported in individual studies.
3.1 How has virtual care been implemented?
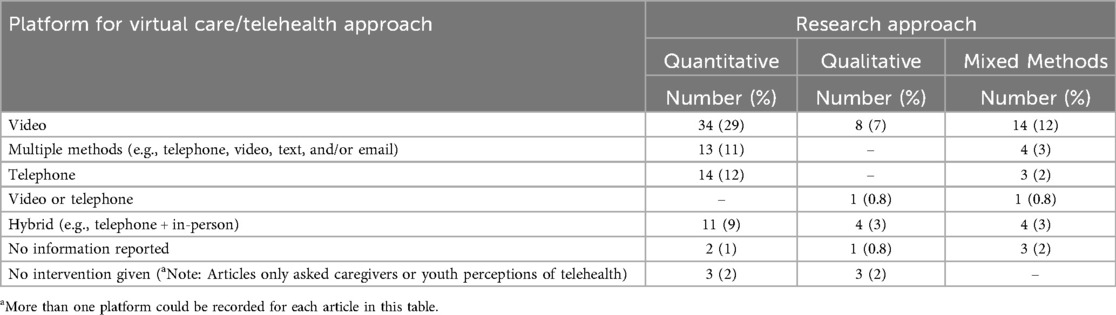
Virtual care approaches varied in terms of how they were described and the modalities, devices or software used to connect patients/families with their healthcare provider. Of the 117 articles analyzed, 56 (48%) used videoconferencing as their mode of communication; however, the approach description and its purpose varied, as outlined in Table 2.
Many articles (n = 14; 12%) used a range of approaches from which patients and families could choose (e.g., videoconferencing or telephone calls), based on what worked best for the child and family. In some articles (n = 17, 15%), parents/caregivers were required to gather and upload child/patient information to an online portal or send it via email pre/post appointment. For instance, a telemedicine cardiac program offered education and support through telephone mediation and required families to upload their child's health data via an app prior to a clinical visit (31). Some articles (n = 17, 15%) contrasted modalities (e.g., in-person vs. virtual) to determine if virtual care was a viable option based on satisfaction and/or care outcomes.
3.2 What are study objectives and the aims of the virtual care applications?
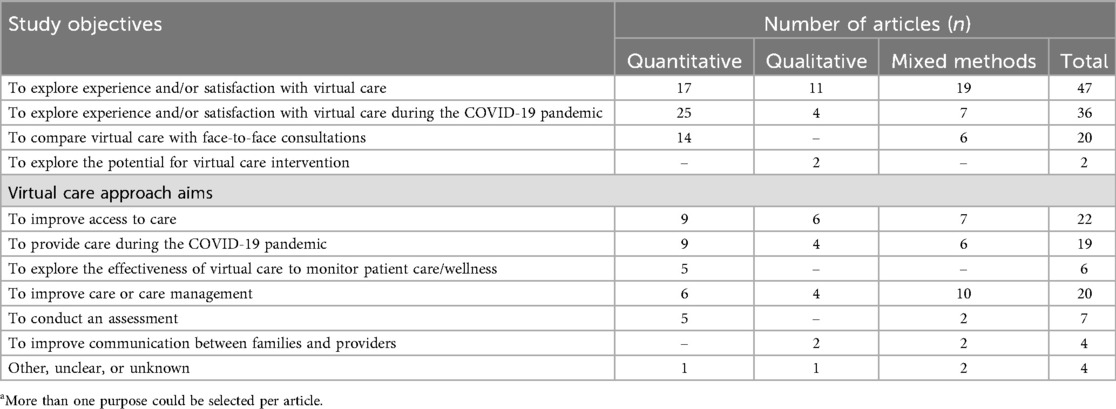
All reviewed articles focused on virtual care; however, specific aims varied. Most commonly, articles explored experiences of, or level of satisfaction with, virtual care (n = 47; 40%), followed by articles evaluating satisfaction with virtual care particularly during the COVID-19 pandemic (n = 36, 31%). Not surprisingly, there was a notable increase in papers focusing on virtual care during the height of the pandemic, i.e., the pandemic was determined to be between March 2020 and May 2023 (32).
A common aim across articles was to contrast virtual care with face-to-face care approaches (n = 20, 17%). In some articles (n = 19; 16%), virtual care was developed to seek continuity of care and/or offer care during the COVID-19 pandemic. Varied study objectives and virtual care approach aims are outlined in Table 3, with several articles having multiple aims.
3.3 By whom, when, where and how has virtual care been evaluated?
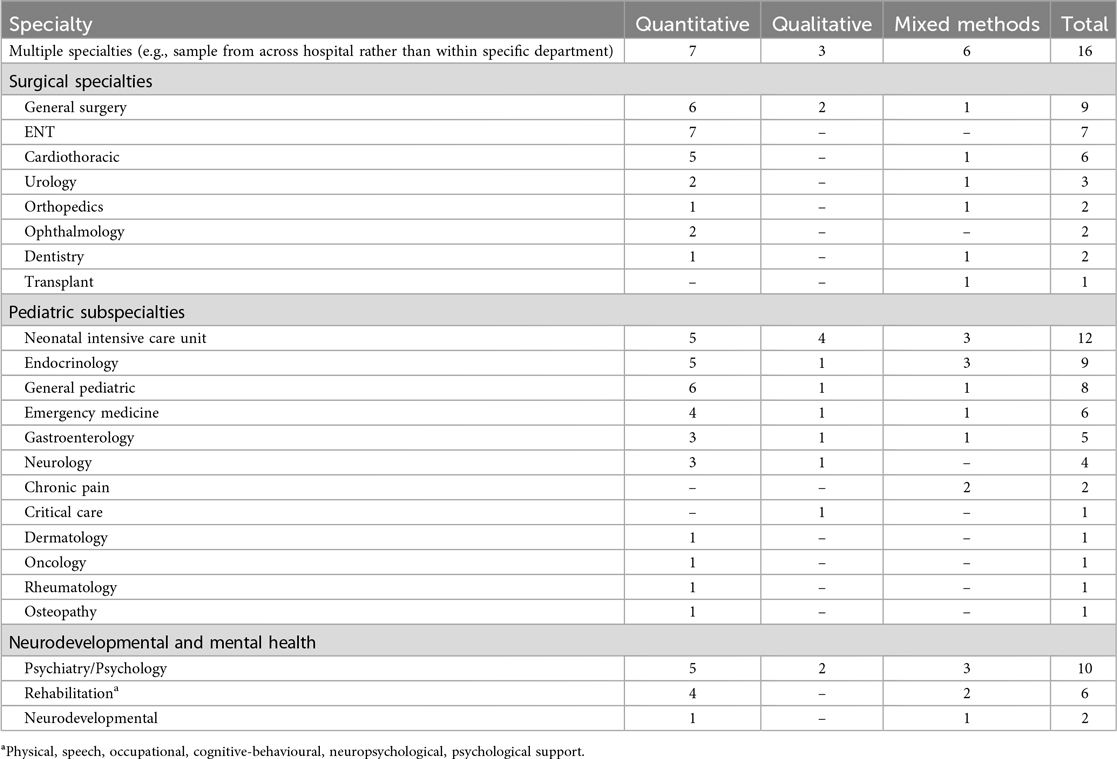
As shown in Table 4, articles were led by varying disciplines and specialty areas. Virtual care experiences were largely gathered from family caregivers solely (n = 47, 40%), from both family caregivers and children/youth (n = 57, 49%), and from children/youth solely (n = 15,13%). Most articles were published after 2019 (2 articles in 2013, 3 in 2015, 1 in 2016, 2 in 2017, 3 in 2018, 6 in 2019, 23 in 2020, 25 in 2021, 32 in 2022, and 20 in 2023). The number of articles remained relatively stable from 2013 to 2019, with an average of 3 per year. However, from 2020 to 2023 this number exponentially rose to a mean of just under 25 per year. This rapid rise likely reflects the limited in-person care available during the COVID-19 pandemic; hence, heightened attention devoted to virtual care as a common care offering and requisite. Notably, 63% of the total articles included quantitative approaches (33–75) that drew on data collected during the COVID-19 pandemic (based on pandemic dates of March 2020 to May 2023 (32), as noted above.
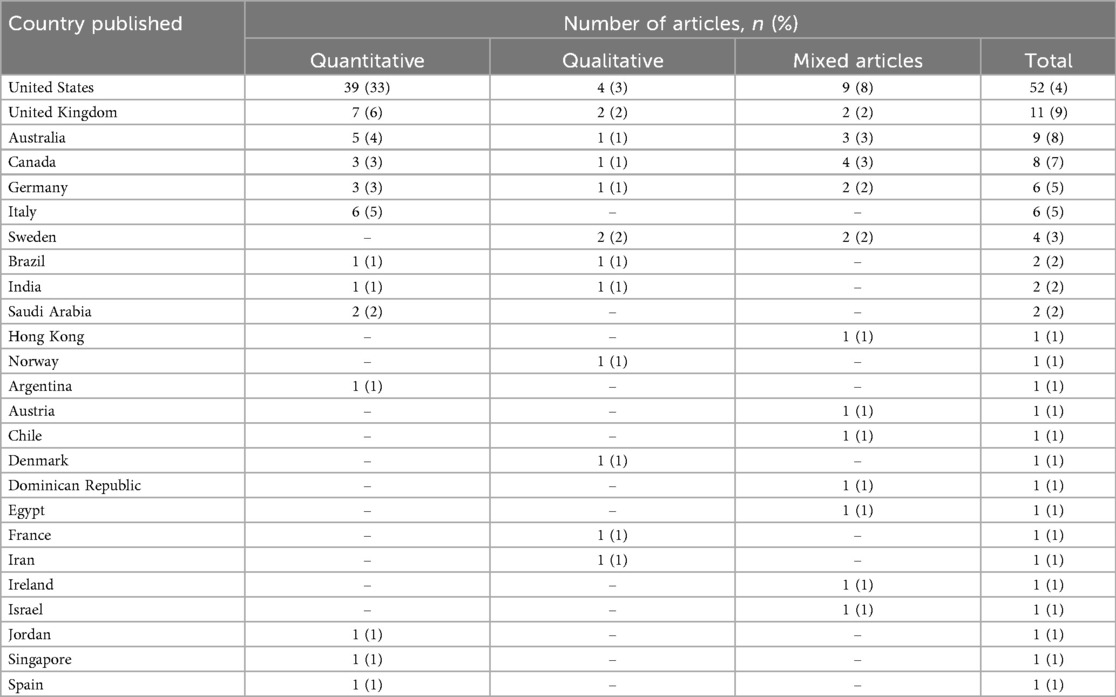
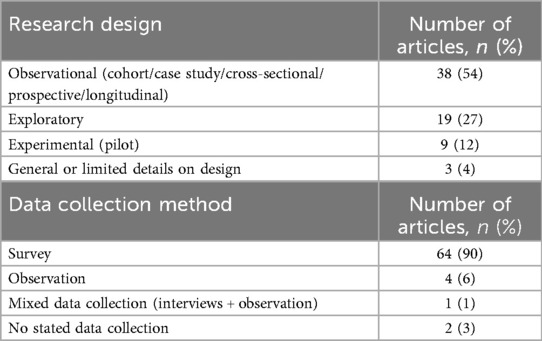
Articles were conducted in various world regions; however, almost half were based in the United States (n = 52, 44%; Table 5). Methodologies varied across articles. Quantitative articles tended to evaluate virtual care, using a range of approaches including observational design (cohort/case study/cross-sectional/prospective/longitudinal) (n = 38, 54%) (33–35, 38–41, 44, 47, 48, 53, 54, 56, 58–60, 62–66, 68, 70–72, 76–87), exploratory design (n = 19, 27%) (37, 42, 45, 49, 50, 55, 61, 69, 88–99), and experimental design (n = 11, 15%) (36, 49, 51, 87, 100–103) [Table 6]. Methods of data collection in articles almost exclusively used surveys (n = 64,90%) (33–44, 46–48, 51, 53–57, 59, 61–66, 68–70, 72–74, 77–79, 81–85, 88, 89, 91, 92, 95, 97, 98, 100–106), measured with Likert scales and/or dichotomous responses, although observation data (n = 4, 3%) (45, 60, 80, 87) were also collected (e.g., indication of improvement in health between admission and discharge via observation of cardiovascular endurance), along with mixed methods (e.g., survey and observation) (n = 1, 1%) (52).
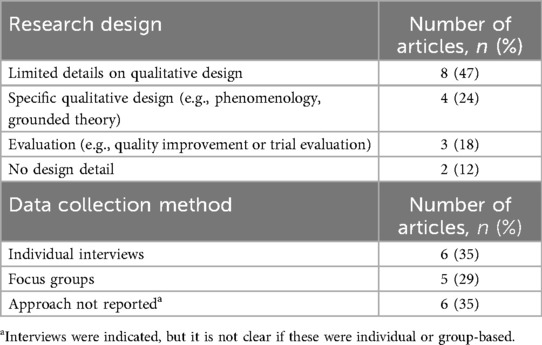
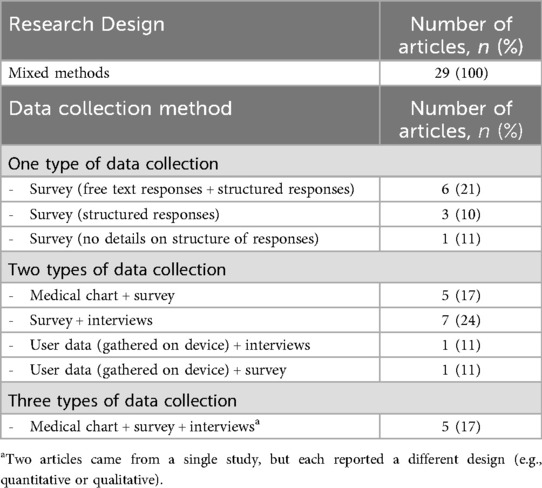
Qualitative articles elicited participant experiences and/or perspectives about virtual care [Table 7]. These articles utilized a range of qualitative approaches such as phenomenology (107, 108) and grounded theory (99). Two articles (109, 110) did not provide details about study design. Table 8 summarizes data collection methods in articles using mixed methods approaches.
3.4 How does virtual care address the social determinants of health?
We examined if, and if so how, articles addressed SDOH and equity considerations (Table 9). Addressing SDOH is important in considering care approach as it can be an indicator of resource/approach accessibility and affordability for families (e.g., buying a device for virtual care, affording a needed internet plan), reflecting salient requisites for virtual care such as access to the internet, level of technical proficiency, availability for care interactivity (e.g., during working hours), and barriers to accessing virtual care. In a recent review of the literature on the intersection of SDOH and telemedicine, Romain and colleagues (29) identified factors that hindered families’ access to telemedicine including not having broadband internet, inability to afford and/or maintain personal digital devices (e.g., desktop or laptop computer), poor digital literacy (e.g., not knowing how to find, process, discuss and share digital content), low English proficiency, and lack of or no internet infrastructure (e.g., poor broadband access, Internet “dead zones”) in specific regions.
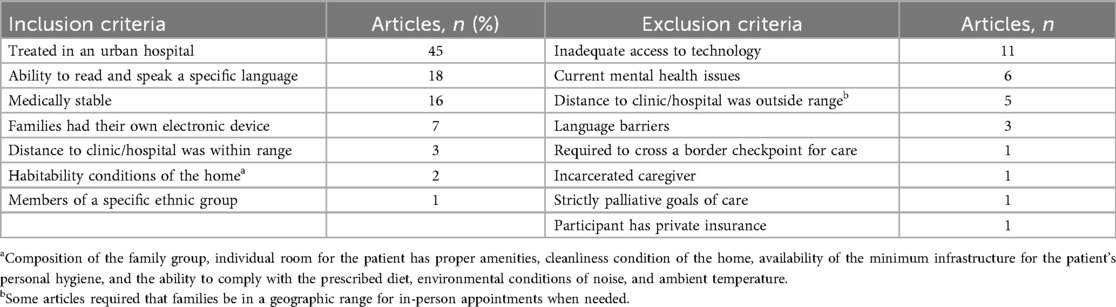
Table 9. Inclusion/exclusion criteria for all articles based on social determinants of health (n = 117).
Geographically, articles tended to reflect work in urban hospitals (n = 45, 38%), and often did not include participants living in rural or remote communities. Inclusion criteria varied regarding participants’ ability to read and speak a specific language (e.g., English or Spanish; n = 18, 15%). Study participants/families were variably required to have an electronic/technology device (n = 7, 6%), thus were rendered ineligible from study participation if lacking technology and/or technology access (n = 11, 9%). Such inclusion requirements systematically decrease representation of families with lower socioeconomic status and/or less access to the Internet.
3.5 How do families experience virtual care?
Articles reported a range of virtual care experiences and perceived outcomes. Generally, articles reported on benefits (n = 99, 85%) and challenges (n = 75, 64%), satisfaction (n = 62, 53%), utilization rates (n = 33, 28%), and approach preferences (n = 34, 29%). These findings are addressed below, as benefits, satisfaction, challenges, patterns of use, and recommendations.
3.5.1 Benefits of virtual care
Most articles (n = 99; 85%) identified one or more benefits of virtual care. Reported child benefits included (a) greater access to care and treatment options, (b) improved health, and/or decreased occurrence of acute episodes (e.g., seizure frequency) (31, 78, 111–113), and (c) heightened child/youth capacity to manage their care (114) and share their perspectives (115).
Parents/caregivers reported vicarious benefits of virtual care for themselves and/or their family. For instance, parents/caregivers reported increased ability to monitor their child's health (76, 107, 111, 116–119). Greater involvement in children's healthcare was reported to result in positive psychological impacts in the parent/caregiver-child relationship (77, 117, 120–122). One study reported that parental involvement in a virtual tele-rehabilitation intervention enabled parents/caregivers to spend more time with their child, including collaborating on treatment goals (121). Parents/caregivers also reported psychological benefits such as increased confidence (84, 94), a sense of self-efficacy (e.g., sense of control) (87, 116, 119, 122, 123), improved flexibility via engaging in appointments from home, decreased distress, and improved self-regulation (40, 48, 102, 124). In one study, fathers reported greater capacity for caregiving tasks (78).
Articles also reported improved relations between parents/caregivers and their children's healthcare providers (53, 94, 99, 107, 113, 117, 121, 125). In these articles, parents reported healthcare providers valuing or respecting their perspectives (36, 51, 113, 117, 126) and being more approachable (113). Moreover, parents reported feeling included in decisions related to their child's care (107, 126).
Virtual care enabled parents/caregivers to spend less time commuting to clinical appointments, thus reducing family expenses (107, 111, 114–116, 119, 121, 123, 126–128), and as a result, families were able to spend more time together (114, 127–129) and/or more time at work/school (107). In one study, cost savings associated with virtual care ($22.47 USD/session) were noted, with a reduction in distance traveled (132 miles or 212.4 kilometers) and time taken (210 min) through virtual care appointments (83). Virtual care further offered a sense of expedited care (41, 128) and continuity of care/access. This was particularly helpful during the COVID-19 pandemic (107, 110), with parents expressing gratitude that virtual care reduced risks of COVID-19 exposure and infection (110, 113, 115, 119, 126).
3.5.2 Satisfaction with virtual care
Over half of the articles (n = 62, 53%) focused on virtual care satisfaction, largely from parent/caregiver perspectives. Generally, satisfaction was reported in quantitative articles in that 82.1% of these studies indicated satisfaction with the care received, and 87.2% indicated satisfaction with the platform/approach used. Two articles reported unanimous family/caregivers and children/youth satisfaction with the virtual care provided (57, 63). A few quantitative articles (n = 35, 30%) reported increased satisfaction including improved access, experience or outcomes. For instance, one article (76) reported increased satisfaction over time, i.e., from 3 months (57%) to 12 months (84%). This change can be attributed to the initial hesitancy among families at the beginning of utilization, compared to more confidence and familiarity with the equipment supplied as well as, in this study, parents increasingly seeing wound healing/resolution.
Qualitative and mixed method articles reported satisfaction as contingent on specific aspects of the approach. For example, one article (117) reported that parents perceived video consultation to be safer, associated with a sense of closeness, and conducive to a more natural way of talking. Additionally, another (130) reported that telephone peer support supplemented in-person support in the hospital and was commonly rated by parents as helpful due to the expertise, care guidance, and emotional support received from peers.
3.5.3 Challenges with virtual care: families
Articles reported challenges (n = 75, 64%) that were largely attributed to difficulties with technology. Almost a quarter of quantitative articles reported some degree of technology barriers/issues (n = 27, 23%). Qualitative and/or mixed methods articles identified virtual care application issues including challenges with a) setting up or logging in (114, 120, 121, 126, 131), b) audio/visual problems (107, 114, 115, 119, 126, 127, 131–134), c) connectivity (107, 113, 115, 116, 120, 126, 127, 133, 134), d) inoperable technical equipment (31, 107, 119, 131, 135), e) prohibitive costs (e.g., not having a reliable battery, needing to purchase specific medical equipment) (119, 128, 131, 133), f) ability and comfort in using the technology to upload/gather information about the child's health (111, 128), and g) resources (e.g., not having Internet or a data plan) (112, 121, 125). Technology challenges resulted in difficulties in care (107, 119). For instance, in two articles, the quality of images using home-based equipment (e.g., a tablet) (107, 119) was poor and thus required in-person follow-up (119).
3.5.3.1 Challenges with virtual care: health care providers
Issues in implementing a virtual application emerged related to healthcare staff and organizational resources. For instance, parents/caregivers (a) experienced delayed responses from a healthcare provider (119, 131), (b) did not access the right health care provider (119), (c) lacked a contact for troubleshooting issues (74), (d) viewed healthcare consultations as overly time-consuming (119) or too complicated to understand (107), (e) reported difficulty retaining information (105), and/or (f) felt invalidated by their child's healthcare provider (120, 121).
Transitioning from in-person to virtual care required adaptation, and in some cases, resulted in relational and ethical challenges. Some parents/caregivers initially were unfamiliar with virtual platforms (97, 118, 126, 135), but as familiarity increased, they perceived virtual platforms to be comparable or better than in-person visits. However, relational challenges arose as families highlighted the loss of interactivity when using virtual care (e.g., not being able to view non-verbal cues, lack of eye contact) (108, 118, 126, 129, 133), with reported negative relational impacts (110). In some situations, care could not be delivered virtually. For instance, parents/caregivers were anxious because they could not obtain a much needed physical examination for their child due to prolonged restrictions during the pandemic (85). The lack of opportunity for physical examination was a major challenge when the attending healthcare provider needed to observe and assess the child in-person to determine next steps (39, 48, 55, 58, 62, 63, 65, 73, 75). In one study (40), parents/caregivers were asked to perform osteopathic interventions guided by a physician via video, but many reported difficulty and discomfort with this modality for such a task. This finding was echoed in another study in which parents/caregivers were provided with a pulse oximeter for home use, but they reported difficulty using this device (47). In reviewing this study, there were no details offered regarding whether the parents/caregivers received any instructional training on how to use the pulse oximeter.
Confidentiality and privacy issues also emerged in virtual care. Articles identified concerns articulating mental health symptoms via video (133), such as a lack of a visual roadmap for sharing private information with the healthcare provider (119), and the use of alternative spaces (e.g., sitting in a car) for therapy (108).
3.5.4 Patterns of using virtual care
Utilization-related considerations included (a) type of medical appointment (121, 127), (b) meeting/appointment duration (31, 62, 93, 125, 127), (c) type of virtual care platform used (94, 114, 136), (d) wait times (69, 88, 92), (e) amount of time spent using the virtual care platform (35, 77, 125, 126, 131), and (f) receiving education from a provider (59, 130).
Several articles identified contextual elements that were attributed to approach use. In three articles, “no-show” rates were due to technology issues (63, 74, 95). One such study suggested that optimizing applications via patient/family reminders, translator assistance, and briefer download speeds may decrease rates of no-shows (74).
3.5.6 What advice do families offer in delivering virtual care?
Several articles (n = 34, 29%) identified parent/caregiver and child preferences for virtual care design and implementation. Whether or not a virtual care application should be used was determined to be contingent on the platform (134), the type of care visit (e.g., follow-up) (110), the number of visits (110), familiarity with the technology (73, 119), and patient and family preference regarding how they could, and/or wished to, communicate with their healthcare provider. For instance, parents/caregivers without a strong understanding of English preferred face-to-face over virtual interactions (126).
Some articles recommended virtual care approach improvements (94, 114, 126, 131). As an example, families receiving hybrid care (in-person home care supplemented by virtual care) to support their infant at home wished for additional components to their virtual care such as a “better diagram function, direct contact with the nurse through, for example chat, compatibility with other web browsers, daily e-mail reminders to answer the questions, and more links to sites containing information about the growth and development of premature infants” (94) (p.7).
Articles reported facilitating vs. hindering factors related to virtual care. For instance, one study reported that adolescents and parents viewed the effectiveness of virtual care to be contingent on factors such as the severity of the child's condition and the nature of the child's relationship with the healthcare provider (134). In another study, virtual care was impeded as parents weren't given sufficient instructions regarding the virtual care process, and how to get in contact with their doctors (113). One study (110) noted gaps such as unreliable technology and internet connectivity; again, amplifying barriers related to SDOH and inequities in virtual care to marginalized communities.
4 Discussion
Virtual care approaches were conveyed as often implemented on a video-based platform, located largely within urban settings. Despite some variation of perceived impacts including reported barriers for marginalized communities, studies generally indicated benefits of implementing virtual care in pediatrics, as identified by families. Accordingly, virtual care generally was determined by children and their parents/caregivers as favorable. Findings also demonstrated that platforms and ways to implement virtual care approaches can vary relative to the needs of the child/youth and/or the parent/caregiver. These findings are complementary to results in other secondary reviews in this area which convey virtual care as acceptable, with emerging evidence of beneficial outcomes in care delivery. As an example, Shah & Badawy's (13) review of randomized controlled trials addressing telemedicine approaches demonstrated improved or comparable impacts of telemedicine compared to controls, based on outcomes of symptom management, satisfaction, quality of life, medication use adherence, visit completion, and disease progression.
This review adds to the overall literature by synthesizing primary studies specifically from the perspective of children and their families. In inclusively focusing on this literature across clinical areas and populations, this review importantly incorporates virtual care in a wide range of practice areas and methodological approaches. Other secondary reviews tend to address specific clinical areas or study designs. As an example, Mitra et al. (15) conducted a systematic review of telemedicine in pediatric emergency care, and Faical et al. (5) reviewed telehealth articles addressing youth with chronic pulmonary disease. Both reviews found overall benefits of virtual care including enhanced care, therapeutic decision-making, diagnostic accuracy in the pre-clinical setting, reduced costs, length of stay and patient satisfaction in emergency care (15), and improved treatment adherence, quality of life and physiological variables (5).
Cumulatively, articles invite greater precision in differentiating virtual care design relative to patient and family needs, and targeted benefits or preferences. This supports the careful consideration of virtual care design for specific purposes and populations. For instance, Siani et al. (7) note potential parental preference for “one type of communication technology over the other, for instance, videoconferencing vs. telephone discussion, due to accommodation of visual content, ability to record or repeat messages, and opportunities to ask questions, particularly when parents are not present for direct discussion following physician's daily evaluations” (7) (p.338).
This review, like others, raises questions about the design of virtual care, and the need for greater precision in complementing virtual or hybrid care relative to the specific care needs and ‘fit’ for a given child and family (121, 133). To facilitate this, shared decision-making between children/youth, their families and healthcare providers is necessary to address initial and emergent challenges throughout the design and implementation of virtual care. Study learnings demonstrate that a third of articles addressed design/implementation aspects that affected the accessibility of virtual care (e.g., need for digital equipment, need to speak in a specific language). Consulting with patients and their families (133), and managing families’ expectations of virtual care are highlighted as important in seeking optimal means of offering virtual care (126). This focus on the “fit” of virtual care approaches complements earlier reviews that amplify the need for greater applicability of research to the target population, clinical area and level of acuity (14, 15, 29). In addition, considerations related to “fit” are imperative as virtual care approaches may incorporate additional tasks (e.g., gathering and uploading children's information) that require guidance from the care team/technological staff and time for families to master.
Despite what generally emerged as benefits and preferences for the inclusion of virtual care in contemporary healthcare, caution and substantial research gaps remain. This review as well as other secondary reviews have found insufficient evidence of virtual care utility and outcomes for specific populations; hence, further evidence is needed in addressing outcomes and processes for targeted populations (2, 13, 14, 16),. Like in other reviews (2, 5, 7), heterogeneity and varying rigor were noted in articles. In moving forward, co-design of approaches may contribute to elements of salience for families.
Multiple articles, as reviewed, indicate concerns about SDOH-related inequities in virtual care. As an example, concern was raised about the need to better understand and accommodate logistical issues and reduce costs for patients and families (125, 128, 130) when designing and implementing virtual care, particularly for families in lower income strata (128). Several previous reviews also have identified inequities in virtual care access (14); however, it appears that advances have been made in this area. For instance, Obregon et al. (16) reviewed articles addressing telehealth among families with limited English proficiency. Their review demonstrates the acceptability and feasibility of telehealth in that population; however, health outcomes have not yet been extensively determined. Accordingly, targeted focus is needed with equity, inclusion, and accessibility lenses particularly for children and families from equity-deserving communities as emphasized by Birnie and colleagues (137). Priorities include widespread access to the internet, data plans, and wireless secure Internet hotspots for patients and their families (120, 121), equitable technology access (76), and reimbursement of costs related to virtual care (e.g., insurance payment to healthcare providers and families) (111).
Reviewed articles offer recommendations to improve access, experiences, and benefits of virtual care. In moving forward, robust organizational infrastructure and more support and training for both users and providers of virtual care are invited. This includes staff training, dedicated information technology (IT) support, improved IT applications, facilitators, and increased role clarity (120, 127, 128, 131, 133, 138). In alignment with EDIA, external staff resources such as interpreters and/or culture brokers are critical to help patients, families and/or healthcare providers overcome linguistic and/or cultural barriers that emerge in virtual care. Tailored approaches are required to meet the needs of all children and families (110, 119, 135, 139). Design considerations must accommodate children/families’ levels of comfort with the virtual care approach used, as well as ensuring its accessibility. Facilitating factors identified in this scoping review can be useful in tailoring virtual care approaches relative to needs. Doing so requires the development of a relationship with patients and their families as well as offering support and guidance to families as they transition from in-person to remote care.
Overall, articles included in this review convey over-arching benefits of virtual care, thereby supporting the use of virtual care. But similar to findings of Siani et al. (7), we suggest caution such that virtual care not be viewed as a replacement to face-to-face interaction. Other key takeaways include the urgent need to address SDOH barriers and offer virtual care applications tailored to patient and family needs as well as clinical context. To this end, we emphasize the incorporation of equity frameworks that can better support the design and implementation of virtual care for all.
While current guidelines of the JBI protocol do not incorporate scoping review consultation, scholars such as Arksey and O'Malley (140) and Oravec et al. (141) emphasize that seeking feedback from patients and caregivers for scoping reviews, increases the potential uptake of findings, increased satisfaction and the generalizability of results. We shared our learnings with a broad group of stakeholders, including caregivers, who expressed resonance with the review findings.
4.1 Review limitations
Limitations in this scoping review include the following. Search terms did not have variants associated with different online platforms that may have been used in virtual care. Only articles written in English were included, thus omitting potentially relevant information from non-English articles and populations. This gap also may have imposed bias reflective of study selection and language/ethnocultural population exclusion. Examination of sample diversity has not been a focus of this review, inviting future study with a focus on appraising considerations of accessibility in virtual care. In the Canadian context, as per the Truth and Reconciliation Commission of Canada, greater attention should focus on virtual care interventions for Indigenous children/youth and their families.
We acknowledge that this review elicited only articles on patient and family perspectives. We also limited our focus to notions of family satisfaction, preferences and experiences of virtual care. While benefits and challenges were illuminated, studies did not provide demonstrated impacts over time. Ascertaining outcomes (e.g., knowledge uptake, treatment adherence) of virtual and/or hybrid care, and examining the perspectives of healthcare providers and clinical decision makers, warrant further study. Also, the heterogeneity in research designs and methods of virtual care platforms impose complexity in assessing the quality of studies, which was not a focusing this review.
Lastly, the preponderance of articles on virtual care in the last decade is nuanced by the requisite of this shift in the COVID-19 pandemic. Also, the ten years reviewed (2013–2023) have reflected exponential shifts in technology and the accessibility of technology. It is recognized that until the pandemic, virtual care options lagged technology industry capacity. Technology advancement (including innovation in artificial intelligence) invites further investigation. Future study also is needed to advance precision in technology capacity and usefulness specific to population, clinical area, and level of acuity.
5 Conclusion
Included articles generally convey positive family perceptions about the use of virtual care in pediatrics. However, further research is needed to determine benefits of virtual care for particular populations and under what circumstances those benefits are incurred. Such work is anticipated to offer greater virtual care precision relative to patient and family need. Further refinement of approaches will inform care design; this invites engaging and empowering patients and families to co-design virtual care options. It appears that virtual care indeed is here to stay; thus, it is important to carefully determine care approaches for positive patient and family experience, equitable access and optimal outcomes.
Author contributions
RZ: Investigation, Writing – review & editing, Conceptualization, Writing – original draft. DN: Writing – review & editing, Investigation, Writing – original draft, Conceptualization. SS: Writing – review & editing, Writing – original draft, Conceptualization, Investigation. EC: Conceptualization, Investigation, Writing – review & editing, Writing – original draft. KB: Writing – review & editing, Writing – original draft, Conceptualization, Investigation. SA: Writing – review & editing. PR: Conceptualization, Writing – original draft, Investigation, Writing – review & editing. ES: Writing – review & editing. TK: Writing – review & editing, Investigation, Conceptualization, Writing – original draft. VM: Writing – review & editing. JS: Investigation, Writing – review & editing, Writing – original draft, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by Canadian Institutes for Health Research (Grant# PCS-183422).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issue please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2025.1610407/full#supplementary-material
References
1. Bird M, Li L, Ouellette C, Hopkins K, McGillion MH, Carter N. Use of synchronous digital health technologies for the care of children with special health care needs and their families: scoping review. JMIR Pediatr Parent. (2019) 2(2):1–18. doi: 10.2196/15106
2. Meimei L, Zenghui M. A systematic review of telehealth screening, assessment, and diagnosis of autism spectrum disorder. Child Adolesc Psychiatry Ment Health. (2022) 16(1):1–79. doi: 10.1186/s13034-022-00514-6
3. Van der Kamp MR, Hengeveld VS, Brusse-Keizer MGJ, Thio BJ, Tabak M. Ehealth technologies for monitoring pediatric asthma at home: scoping review. J Med Internet Res. (2023) 25:1–37. doi: 10.2196/45896
4. Dostie R, Gaboury I, Cinar E, Camden C. Acceptability of pediatric telerehabilitation interventions provided by physical therapists and occupational therapists. A scoping review. Phys Occup Ther Pediatr. (2022) 42(6):615–34. doi: 10.1080/01942638.2022.2064203
5. Faiçal AVB, Mota LR, d' Afonseca Correia D, Monteiro LP, de Souza EL, Terse-Ramos R. Telehealth for children and adolescents with chronic pulmonary disease: systematic review. Rev Paul Pediatr. (2023) 42:1–9. doi: 10.1590/1984-0462/2024/42/2022111
6. Nguyen N, Leveille E, Guadagno E, Kalisya LM, Poenaru D. Use of mobile health technologies for postoperative care in paediatric surgery: a systematic review. J Telemed Telecare. (2022) 28(5):331–41. doi: 10.1177/1357633X20934682
7. Siani SA, Dol J, Campbell-Yeo M. Impact of parent-targeted eHealth on parent and infant health outcomes: a scoping review. J Perinat Neonatal Nurs. (2017) 31(4):332–40. doi: 10.1097/JPN.000000000000265
8. Ramsey WA, Heidelberg RE, Gilbert AM, Heneghan MB, Badawy SM, Alberts NM. Ehealth and mHealth interventions in pediatric cancer: a systematic review of interventions across the cancer continuum. PsychoOncology. (2020) 29(1):17–37. doi: 10.1002/pon.5280
9. Corti C, Oldrati V, Oprandi MC, Ferrari E, Poggi G, Borgatti R, et al. Remote technology-based training programs for children with acquired brain injury: a systematic review and a meta-analytic exploration. Behav Neurol. (2019) 2019:1–31. doi: 10.1155/2019/1346987
10. Rajan R, Dovebenyuk R, Kshatriya M, Yanikomeroglu S, Banfield L, Athale U, et al. The impact of virtual care on health-related quality of life in pediatric diabetes mellitus: a systematic review. Adolesc Health Med Ther. (2025) 15:109–17. doi: 10.2147/AHMT.S482859
11. Pope N, Birnie KA, Noel M, Dol J, Li D, Macneil M, et al. Mapping the gaps: a scoping review of virtual care solutions for caregivers of children with chronic illnesses. Children. (2025) 12(1):1–19. doi: 10.3390/children12010077.s
12. Campbell J, Theodoros D, Hartley N, Russell T, Gillespie N. Implementation factors are neglected in research investigating telehealth delivery of allied health services to rural children: a scoping review. J Telemed Telecare. (2020) 26(10):590–606. doi: 10.1177/1357633X19856472
13. Shah AC, Badawy SM. Telemedicine in pediatrics: systematic review of randomized controlled trials. JMIR Pediatr. (2021) 4(1):1–20. doi: 10.2196/22696
14. Davidson SK, Sanci L, de Nicolás Izquierdo C, Watson CJ, Baltag V, Sawyer SM. Best practice during teleconsultations with adolescents: a scoping review. J Adolesc Health. (2022) 70(5):714–28. doi: 10.1016/j.jadohealth.2021.11.012
15. Mitra A, Veerakone R, Li K, Nix T, Hashikawa A, Mahajan P. Telemedicine in paediatric emergency care: a systematic review. J Telemed Telecare. (2023) 29(8):579–90. doi: 10.1177/1357633X211010106
16. Obregon E, Ortiz R, Wallis KE, Morgan S, Montoya-Williams D. Feasibility, acceptability, and health outcomes associated with telehealth for children in families with limited English proficiency: a systematic review. Acad Pediatr. (2024) 24(1):13–22. doi: 10.1016/j.acap.2023.06.025
17. Kermani F, Orooji A, Sheikhtaheri A. Teleoncology for children with cancer: a scoping review on applications and outcomes. Int J Med Inform. (2020) 139:1–9. doi: 10.1016/j.ijmedinf.2020.104118
18. Bradford N, Armfield NR, Young J, Smith AC. The case for home based telehealth in pediatric palliative care: a systematic review. BMC Palliat Care. (2013) 12(1):1–13. doi: 10.1186/1472-684X-12-4
19. Burshtein J, Buethe MG, Ghias MH, Stein AB, Glick S, Marmon S. Efficacy, perception, and utilization of pediatric teledermatology: a systematic review. JAAD International. (2023) 12:3–11. doi: 10.1016/j.jdin.2023.03.005
20. Jungbauer WN, Gudipudi R, Brennan E, Melvin CL, Pecha PP. The cost impact of telehealth interventions in pediatric surgical specialties: a systematic review. J Pediatr Surg. (2023) 58(8):1527–33. doi: 10.1016/j.jpedsurg.2022.10.008
21. Miller KA, Baird J, Lira J, Herrera Eguizabal J, Fei S, Kysh L, et al. The use of telemedicine for home-based palliative care for children with serious illness: a scoping review. J Pain Symp Manage. (2021) 62(3):619–36. doi: 10.1016/j.jpainsymman.2020.12.004
22. Southgate G, Yassaee AA, Harmer MJ, Livesey H, Pryde K, Roland D. Use of telemedicine in pediatric services for 4 representative clinical conditions: scoping review. J Med Internet Res. (2022) 24(10):1–10. doi: 10.2196/38267
23. Vinadé Chagas ME, Rodrigues Moleda Constant HM, Cristina Jacovas V, Castro da Rocha J, Galves Crivella Steimetz C, Cotta Matte MC, et al. The use of telemedicine in the PICU: a systematic review and meta-analysis. PLoS One. (2021) 16(5):1–12. doi: 10.1371/journal.pone.0252409
24. Kodjebacheva GD, Culinski T, Kawser B, Coffer K. Satisfaction with telehealth services compared with nontelehealth services among pediatric patients and their caregivers: systematic review of the literature. JMIR Pediatr Parent. (2023) 6:1–18. doi: 10.2196/41554
25. Office of Disease Prevention and Health Promotion. Social Determinants of Health - Healthy People 2030. Rockville, MD: Office of the Assistant Secretary for Health, Office of the Secretary, U.S. Department of Health and Human Services (2023). Available online at: https://health.gov/healthypeople/priority-areas/social-determinants-health#:∼:text=Social%20determinants%20of%20health%20(SDOH,of%2Dlife%20outcomes%20and%20risks (Accessed December 1, 2023).
26. Khalil H, Peters M, Godfrey CM, McInerney P, Soares CB, Parker D. An evidence-based approach to scoping reviews. Worldviews on Evid Based Nurs. (2016) 13(2):118–23. doi: 10.1111/wvn.12144
27. Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for conduct of scoping reviews. JBI Evid Synth. (2020) 18(10):2119–26. 10.11124.JBIES-20-0016733038124
28. Telehealth.HHS.Gov. Synchronous Direct-to-Consumer Telehealth. Telehealth.Hhs.Gov. North Bethseda, MD: Health Resources & Services Organization (2022). Available online at: https://telehealth.hhs.gov/providers/best-practice-guides/direct-to-consumer/synchronous-direct-to-consumer-telehealth (Accessed October 28, 2022).
29. Romain CV, Trinidad S, Kotagal M. The effect of social determinants of health on telemedicine access during the COVID-19 pandemic. Pediatr Ann. (2022) 51(8):e311–5. doi: 10.3928/19382359-20220606-04
30. Wang CP, Mkuu R, Andreadis K, Muellers KA, Ancker JS, Horowitz C, et al. Examining and addressing telemedicine disparities through the lens of the social determinants of health: a qualitative study of patient and provider during the COVID-19 pandemic. AMIA Annu Symp Proc. (2024) 2023:1287–96.38222380
31. Stagg A, Giglia TM, Gardner MM, Offit BF, Fuller KM, Natarajan SS, et al. Initial experience with telemedicine for interstage monitoring in infants with palliated congenital heart disease. Pediatr Cardiol. (2023) 44(1):196–203. doi: 10.1007/s00246-022-02993-y
32. Rigby J, Satija B. WHO declares end to COVID Global Health Emergency. London: Reuters (2023). Available online at: https://www.reuters.com/business/healthcare-pharmaceuticals/covid-is-no-longer-global-health-emergency-who-2023-05-05/
33. Assenza C, Catania H, Antenore C, Gobbetti T, Gentili P, Paolucci S, et al. Continuity of care during COVID-19 lockdown: a survey on stakeholders’ experience with telerehabilitation. Front Neurol. (2021) 11:1–10. doi: 10.3389/fneu.2020.617276
34. Bate NJ, Xu SC, Pacilli M, Roberts LJ, Kimber C, Nataraja RM. Effect of the COVID-19 induced phase of massive telehealth uptake on end-user satisfaction. Intern Med J. (2021) 51(2):206–14. doi: 10.1111/imj.15222
35. Cockrell H, Wayne D, Wandell G, Wang X, Greenberg SLM, Kieran K, et al. Understanding hispanic patient satisfaction with telehealth during COVID-19. J Pediatr Surg. (2022) 58(9):1783–8. doi: 10.1016/j.pedsurg.2022.12.006
36. Giuseppe DB, Giuseppina N, Desiree S, Angela S, Maurizio G, Perrone S. Improving care in neonatal intensive units during the COVID-19 pandemic: a survey on electronic health communication. J Intensive Care Med. (2022) 37(5):671–8. doi: 10.1177/08850666211055058
37. Guttmann-Bauman I, Kono J, Lin AL, Ramsey KL, Boston BA. Use of telehealth videoconferencing in pediatric type 1 diabetes in Oregon. Telemed J E Health. (2018) 24(1):86–8. doi: 10.1089/tmj.2017.0072
38. Holzman SA, Davis-Dao CA, Khoury AE, Fortier MA, Kain NZ. Telemedicine and patient satisfaction during the COVID-19 pandemic: a case-control study of outpatient pediatric urology patients. J Child Health Care. (2021) 27(3):351–9. doi: 10.1177/13674935211058272
39. Kilipiris EG, Horn F, Kolnikova M, Ochoa JV, Matuskova O, Jelovac D, et al. Parental satisfaction from telemedicine in the follow-up of children operated for craniosynostosis during COVID-19 pandemic. Cleft Palate J. (2023) 60(5):562–8. doi: 10.1177/10556656221074214
40. Kramer JL, De Asis K. Osteopathic interventions via telehealth in a pediatric population: a retrospective case series. J Osteopath Med. (2021) 121(11):857–61. doi: 10.151/jom-2021-0124
41. McCoy J, Shaffer J, Amber D, Dohar JE. Pediatric otolaryngology telemedicine amid a pandemic - and beyond. Int J Pediatr Otorhinolaryngol. (2022) 153:1–7. doi: 10.1049/j.ijporl.2021.111014
42. McNally Keehn R, Enneking B, James C, Tang Q, Rouse M, Hines E, et al. Telehealth evaluation of pediatric neurodevelopmental disabilities during the COVID-19 pandemic: clinician and caregiver perspectives. J Dev Behav Pediatr. (2022) 43(5):262–72. 10.1097.DBP.000000000000104334954761
43. Meininger L, Adam J, von Wirth E, Viefhaus P, Woitecki K, Walter D, et al. Cognitive-behavioral teletherapy for children and adolescents with mental disorders and their families during the COVID-19 pandemic: a survey on acceptance and satisfaction. Child Adolesc Psychiatry Ment Health. (2022) 16(1):1–11. doi: 10.1189/s13034-022-00494-7
44. Netson RA, Miller S, Incorvia J, Shah A, Estrada CR, Toomey SL, et al. Patient experience with virtual preoperative consultations in pediatric surgical specialties. J Pediatr Surg. (2023) 58(9):1776–82. doi: 10.1016/j.jpedsurg.2022.12.027
45. Onofri A, Pavone M, De Santis S, Verrillo E, Caggiano S, Ullmann N, et al. Telemedicine in children with medical complexity on home ventilation during the COVID-19 pandemic. Pediatr Pulmonol. (2021) 56(6):1395–400. doi: 10.1002/ppul.25289
46. Severini RDSG, Oliveira PCD, Couto TB, Simon Junior H, Andrade APMD, Nanbu DY, et al. Fast, cheap and feasible: implementation of pediatric telemedicine in a public hospital during the COVID-19 pandemic. J Pediatr (Rio J). (2022) 98(2):183–9. doi: 10.1016/j.jped.2021.05.007
47. Tan LO, Ganapathy S. A single centre study of the level of parents’ satisfaction with the COVID-19 telemedicine consultation. Eur J Pediatr. (2023) 188(1):213–8. doi: 10.1007/s00431-023-05276-7
48. von Sengbusch S, Schneidewind J, Bokelmann J, Scheffler N, Bertram B, Frielitz F, et al. Monthly video consultation for children and adolescents with type 1 diabetes mellitus during the COVID-10 pandemic. Diabetes Res Clin Pract. (2022) 193:1–6. doi: 10.1016/j.diabres.2022.110135
49. Weaver MS, Jurgens A, Neumann ML, Schalley SM, Kellas JK, Navaneethan H, et al. Actual solidarity through virtual support: a pilot descriptive study of an online support group for bereaved parents. J Palliat Med. (2021) 24(8):1161–5. doi: 10.1089/jpm.2020.0617
50. Weaver MS, Shostrom VK, Neumann ML, Robinson JE, Hinds PS. Homestead together: pediatric palliative care telehealth support for rural children with cancer during home-based end-of-life care. Pediatr Blood Cancer. (2021) 68(4):1–9. doi: 10.1002/pbc.28921
51. Zayde A, Kilbride A, Kucer A, Willis HA, Nikititiades A, Alpert J, et al. Connection during COVID-19: pilot study of a telehealth group parenting intervention. Am J Psychotherap. (2022) 75(2):67–74. doi: 10.1176/appi.psychotherapy.20210005
52. Hallford HG, Szyld E, McCoy M, Makkar A. A 360 evaluation of neonatal care quality at a level II neonatal intensive care unit when delivered using a hybrid telemedicine service. Am J Perinatol. (2022) 41:1–8. doi: 10.1055/a-1932-9921
53. Hendra K, Neemuchwala F, Chan M, Ly NP, Gibb ER. Patient and provider experience with cystic fibrosis telemedicine clinic. Front Pediatr. (2021) 9:1–7. doi: 10.3389/fped.2021.784692
54. Hiscock H, Pelly R, Hua X, West S, Tucker D, Raymundo CM, et al. Survey of paediatric telehealth benefits from the caregiver perspective. Aust Health Rev. (2022) 46(2):197–203. doi: 10.1071/AH21036
55. Love M, Hunter AK, Lam G, Muir LV, Lin HC. Patient satisfaction and perceived quality of care with telemedicine in a pediatric gastroenterology clinic. Pediatr Rep. (2022) 14(2):181–9. doi: 10.3390/pediatric14020025
56. Marques S, Cruz JAW, da Cunha MAVC, Tuon FF, de Moraes TP, Zdziarski AD, et al. Patient and family experience with telemedicine and in-person pediatric and obstetric ambulatory encounters throughout 2020, during the COVID-19 epidemic: the distance effect. BMC Health Serv Res. (2022) 22(1):1–8. doi: 10.1186/s12913-022-08037-8
57. Olateju A, Cervantes M, Dowshen N, Kuhns LM, Dhar CP. Acceptability of telemedicine among parents of adolescent patients in an adolescent clinic: cross-sectional survey study. JMIR Pediatr Parent. (2022) 5(4):1–7. doi: 10.2196/39704
58. Reid S, Bhatt M, Zemek R, Tse S. Virtual care in the pediatric emergency department: a new way of doing business? CJEM. (2021) 23(1):80–4. doi: 10.1007/s43678-020-00048-w
59. Sharma S, Daniel M. Telemedicine in paediatric otorhinolaryngology: lessons learnt from remote encounters during the Covid19 pandemic and implications for future practice. Int J Pediatr Otorhinolaryngol. (2020) 139:1–6. doi: 10.1016/j.ijporl.2020.110411
60. Shulman J, Conroy C, Bento S, Bryant G, Jervis K, Sethna NF. Pediatric pain rehabilitation during the COVID-19 pandemic: exploring the effectiveness of a hybrid intensive interdisciplinary pain treatment model. Disabil Rehabil. (2023) 45(19):3079–86. doi: 10.1080/09638288.2022.2125083
61. Lawrence J, Measey MA, Hoq M, Hiscock H, Rhodes A. Virtual health care for children: parental willingness to adopt virtual health-care technologies. J Paediatr Child Health. (2022) 58(8):1323–9. doi: 10.1111/jpc.15974
62. Singh N, Datta M. Single-centre telephone survey on patients’ perspectives regarding remote paediatric outpatient consultations in a district general hospital. BMJ Paediatr. (2020) 4(1):1–2. doi: 10.1136/bmjpo-2020-000885
63. Hoi KK, Brazina SA, Kolar-Anderson R, Zopf DA, Bohm LA. A longitudinal comparison of telemedicine versus in-person otolaryngology clinic efficiency and patient satisfaction during COVID-19. Ann Otol Rhinol Laryngol. (2022) 131(11):1177–84. doi: 10.1177/00034894211055349
64. Jones E, Kurman J, Delia E, Crockett J, Peterson R, Thames J, et al. Parent satisfaction with outpatient telemedicine services during the COVID-19 pandemic: a repeated cross-sectional study. Front Pediatr. (2022) 10:1–9. doi: 10.3389/fped.2022.908337
65. Lakshin G, Banek S, Keese D, Rolle U, Schmedding A. Telemedicine in the pediatric surgery in Germany during the COVID-19 pandemic. Pediatr Surg Int. (2021) 37(3):389–95. doi: 10.1007/s00383-020-04822-w
66. Lo WB, Herbert K, Rodrigues D. Clinical effectiveness of and family experience with telephone consultation in a regional pediatric neurosurgery center in the United Kingdom, journal of neurosurgery. Pediatr. (2021) 28(4):483–9. doi: 10.3171/2021.3.PEDS20862
67. Odeh R, Gharaibeh L, Daher A, Kussad S, Alassaf A. Caring for a child with type 1 diabetes during COVID-19 lockdown in a developing country: challenges and parents’ perspectives on the use of telemedicine. Diabetes Res Clin Pract. (2020) 168:1–7. doi: 10.1016/j.diabres.2020.108393
68. Sikka K. Parent’s perspective on teletherapy of pediatric population with speech and language disorder during COVID-19 lockdown in India. Indian J Otolaryngol Head Neck Surg. (2023) 75(1):14–20. doi: 10.1007/s12070-022-03310-y
69. Trivisano M, Specchio N, Pietrafusa N, Calabrese C, Ferretti A, Ricci R, et al. Impact of COVID-19 pandemic on pediatric patients with epilepsy – the caregiver perspective. Epilepsy Behav. (2020) 113:1–5. doi: 10.1016/j.yebeh.2020.107527
70. Alghamdi SA. Parent perceptions regarding virtual pediatric dental clinics during COVID-19 pandemic: a cross-sectional study. Peer J. (2023) 11:1–14. doi: 10.7717/peerj.15289
71. Alzahrani AM, Magliah SF, Turkistani HA, Abulaban BA, Sabban MF, Mashat MA, et al. Perception of primary caregiver toward virtual pediatric clinics for type 1 diabetes mellitus during COVID-19 pandemic in Jeddah, Saudi Arabia: a cross-sectional study. Ann Med Surg. (2022) 81:1–6. doi: 10.1016/j.amsu.2022.104550
72. Darr A, Senior A, Argyriou K, Limbrick J, Nie H, Kantczak A, et al. The impact of the coronavirus (COVID-19) pandemic on elective paediatric otolaryngology outpatient services – an analysis of virtual outpatient clinics in a tertiary referral centre using the modified paediatric otolaryngology telemedicine satisfaction survey (POTSS). Int J Pediatr Otorhinolaryngol. (2017) 138:1–8. doi: 10.1016/j.ijporl.2020.110383
73. Davis J, Gordon R, Hammond A, Perkins R, Flanagan F, Rabinowitz E, et al. Rapid implementation of telehealth services in a pediatric pulmonary clinic during COVID-19. Pediatr. (2021) 148(1):1–9. doi: 10.1542/peds.2020-030494
74. Kolb CM, Born K, Banker K, Barth PC, Aaronson NL. Improving attendance and patient experiences during the expansion of a telehealth-based pediatric otolaryngology practice. Otolaryngol Head Neck Surg. (2021) 164(5):952–8. doi: 10.1177/0194599820965917
75. Bales NJ, Perera DC, Foerster R, Poirier L, Ducis K. Analysis of a novel virtual pediatric concussion clinic in a rural setting. Childs Nerv Syst. (2023) 40:1–7. doi: 10.1007/s00381-023-06231-5
76. Bianciardi Valassina MF, Bella S, Murgia F, Carestia A, Prosseda E. Telemedicine in pediatric wound care. Clin Ter. (2016) 167(1 Supplement):21–3. doi: 10.7417/T.2016.1915
77. Finkelstein JB, Cahill D, Young K, Humphrey K, Campbell CS, Nelson CP, et al. Telemedicine for pediatric urological postoperative care is safe, convenient and economical. J Urol. (2020) 204(1):144–8. doi: 10.1097/JU.0000000000000750
78. Fortini S, Espeche A, Caraballo R. Telemedicine and epilepsy: a patient satisfaction survey of a pediatric remote care program. Epilepsy Res. (2020) 165:1–5. doi: 10.1016/j.eplepsyres.2020.106370
79. Jury SC, Walker AM, Kornberg AJ. The introduction of web-based video-consultation in a paediatric acute care setting. J Telemed Telecare. (2013) 19(7):383–7. doi: 10.1177/1357633X13506530
80. Khoury M, Phillips DB, Wood PW, Mott WR, Stickland MK, Boulanger P, et al. Cardiac rehabilitation in the paediatric fontan population: development of a home-based high-intensity interval training programme. Cardiol Young. (2020) 30:1409–16. doi: 10.1017/sS1047951120002097
81. Makkar A, McCoy M, Hallford G, Foulks A, Anderson M, Milam J, et al. Evaluation of neonatal services provided in a level II NICU utilizing hybrid telemedicine: a prospective study. Telemed J E Health. (2020) 26(2):176–83. doi: 10.1089/tmj.2018.0262
82. Qubty W, Patniyot I, Gelfand A. Telemedicine in a pediatric headache clinic. Neurology. (2018) 90(19):E1702–5. doi: 10.1212/WNL.0000000000005482
83. Frye WS, Gardner L, Mateus JS. Utilising telemental health in a paediatric outpatient psychology clinic: therapeutic alliance and outcomes. Couns Psychother Res. (2022) 22(2):322–30. doi: 10.1002/capr.12450
84. Walijee H, Sood S, Markey A, Krishnan M, Lee A, De S. Is nurse-led telephone follow-up for post-operative obstructive sleep apnoea patients effective? A prospective observational study at a paediatric tertiary centre. Int J Pediatr Otorhinolaryngol. (2020) 129:1–5. doi: 10.1016/j.ijporl.2019.109766
85. Bell S, Karamchandani U, Malcolmson K, Moosajee M. Acceptability of telegenetics for families with genetic eye diseases. Genes (Basel). (2021) 12(2):1–9. doi: 10.3390/genes12020276
86. Heath J, Dancel R, Stephens JR. Postdischarge phone calls after pediatric hospitalization: an observational study. Hosp Pediatr. (2015) 5(5):241–8. doi: 10.1542/hpeds.2014-0069
87. López Seguí F, Batlle Boada A, García García JJ, López Ulldemolins A, Achotegui Del Arco A, Adroher Mas C, et al. Families’ degree of satisfaction with pediatric telehomecare: interventional prospective pilot study in catalonia. JMIR Pediatr Parent. (2020) 3(1):1–8. doi: 10.2196/17517
88. Stewart C, Coffey-Standoval J, Souverein EA, Ho TC, Lee TC, Nallasamy S. Patient and provider experience in real-time telemedicine consultations for pediatric ophthalmology. Clin Ophthalmol. (2022) 16:2943–53. doi: 10.2147/OPTH.S374811
89. Taddei M, Bulgheroni S. Facing the real time challenges of the COVID-19 emergency for child neuropsychology service in Milan. Rs Dev Disabil. (2020) 107:1–6. doi: 10.1016/j.ridd.2020.103786
90. Wade SL, Cassedy AE, Sklut M, Taylor G, McNally KA, Kirkwood MW, et al. The relationship of adolescent and parent preferences for treatment modality with satisfaction, attrition, adherence, and efficacy: the coping with head injury through problem-solving (CHIPS) study. J Pediatr Psychol. (2019) 44(3):388–401. doi: 10.1093/jpepsy/jsy087
91. Weber JC, Sohn K, Sauers-Ford HS, Hanhauser A, Tancredi DJ, Marcin JP, et al. Impact of a parent video viewing program in the neonatal intensive care unit. Telemed J E Health. (2021) 27(6):679–85. doi: 10.1089/tmj.2020.0251
92. Young K, Gupta A, Palacios R. Impact of telemedicine in pediatric postoperative care. Telemed J E Health. (2019) 25(11):1083–9. doi: 10.1089/tmj.2018.0246
93. Akobeng AK, O’Leary N, Vail A, Brown N, Widiatmoko D, Fagbemi A, et al. Telephone consultation as a substitute for routine out-patient face-to-face consultation for children with inflammatory bowel disease: randomised controlled trial and economic evaluation. EbioMedicine. (2015) 2(9):1251–6. doi: 10.1016/j.ebiom.2015.08.011
94. Gund A, Sjöqvist BA, Wigert H, Hentz E. A randomized controlled study about the use of eHealth in the home health care of premature infants. BMC Med Inform Decis Mak. (2013) 13(1):1–11. doi: 10.1186/1472-6947-13-22
95. Brewster RCL, Zhang J, Stewart M, Kaur R, Arellano M, Bourgeois F. A prescription for internet: feasibility of a tablet loaner program to address digital health inequities. Appl Clin Inform. (2023) 14(2):273–8. doi: 10.1055/a-2016-7417
96. Sultan AA, Acuna AJ, Samuel LT, Rabin JM, Grits D, Gurd DP, et al. Utilization of telemedicine virtual visits in pediatric spinal deformity patients: a comparison of feasibility and patient satisfaction at a large academic center. J Pediatr Orthop. (2020) 40(8):e712–5. doi: 10.1097/BPO.0000000000001553
97. Bullock DR, Vehe RK, Zhang L, Correll CK. Telemedicine and other care models in pediatric rheumatology: an exploratory study of parents’ perceptions of barriers to care and care preferences. Pediatr Rheumatol. (2017) 15(1):1–8. doi: 10.1186/s12969-017-0184-y
98. Foster CC, Macy ML, Simon N, Stephen R, Lehnig K, Bohling K, et al. Emergency care connect: extending pediatric emergency care expertise to general emergency departments through telemedicine. Acad Pediatr. (2020) 20(5):577–84. doi: 10.1016/j.acap.2020.02.028
99. Moreno L, Peck JL. Nurse practitioner-led telehealth to improve outpatient pediatric tracheostomy management in south Texas. J Pediatr Health Care. (2020) 34(3):246–55. doi: 10.1016/j.pedhc.2019.11.008
100. Chalmers JA, Sansom-Daly UM, Patterson P, McCowage G, Anazodo A. Psychosocial assessment using telehealth in adolescents and young adults with cancer: a partially randomized patient preference pilot study. J Med Internet Res. (2018) 7(8):1–25. doi: 10.2196/resprot.8886
101. Elbin RJ, Stephenson K, Lipinski D, Maxey K, Womble MN, Reynolds E, et al. In-Person versus telehealth for concussion clinical care in adolescents: a pilot study of therapeutic alliance and patient satisfaction. J Head Trauma Rehab. (2022) 37(4):213–9. doi: 10.1097/HTR.0000000000000707
102. Rashid M, Haskett J, Parkinson McGraw L, Noble A, van Limbergen J, Otley A. Teaching families of children with celiac disease about gluten-free diet using distributed education: a pilot study. Can J Diet Pract Res. (2021) 82(1):38–40. doi: 10.3148/cjdpr-2020-021
103. Yen S, Ranney ML, Krek M, Peters JR, Mereish E, Tezanos KM, et al. Skills to enhance positivity in suicidal adolescents: results from a pilot randomized clinical trial. J Posit Psychol. (2020) 15(3):348–61. doi: 10.1080/17439760.2019.1615105
104. Nguyen HH, Van Hare GF, Rudokas M, Bowman T, Silva JNA. SPEAR trial: smartphone pediatric electrocardiogram trial. PLoS One. (2015) 10(8):1–9. doi: 10.1371/journal.pone.0136256
105. Charnell AM, Hannon E, Burke D, Iredale MR, Sutcliffe JR. Virtual consultations: delivering outpatient clinics in paediatric surgery during the COVID-19 pandemic. Ann Pediatr Surg. (2020) 16(1):1–5. doi: 10.1186/s43159-020-00060-w
106. Mollen CJ, Henien M, Jacobs LM, Myers S. Parent perceptions on transfers to pediatric emergency departments and the role of telemedicine. Pediatr Emerg Care. (2019) 35(3):180–4. doi: 10.1097/pec.000000000000957
107. Phillips D, Matheson L, Pain T, Kingston GA. Evaluation of an occupational therapy led paediatric burns telehealth review clinic: exploring the experience of family/carers and clinicians. Rural Remote Health. (2022) 22(1):1–8. doi: 10.22605/RRH6887
108. Carretier E, Bastide M, Lachal J, Moro MR. Evaluation of the rapid implementation of telehealth during the COVID-19 pandemic: a qualitative study among adolescents and their parents. Eur Child Adolesc Psychiatry. (2022) 32:963–73. doi: 10.1007/s00787-022-02108-1
109. Lanzarin CMV, von Wangenheim A, Rejane-Heim TC, Nascimento FS, Wagner HM, Abel HS, et al. Teleconsultations at a pediatrics outpatient service in COVID-19 pandemic: first results. Telemed J E Health. (2021) 27(11):1311–6. doi: 10.1089/tmj.2020.0471
110. Fletcher SE, Tsang VWL. The era of virtual care: perspectives of youth on virtual appointments in COVID-19 and beyond. Paediatr Child Health. (2021) 26(4):210–3. doi: 10.1093/pch/pxaa138
111. von Sengbusch S, Doerdelmann J, Lemke S, Lange K, Hiort O, Katalinic A, et al. Parental expectations before and after 12-month experience with video consultations combined with regular outpatient care for children with type 1 diabetes: a qualitative study. Diabet Med. (2021) 38(6):1–12. doi: 10.1111/dme.14410
112. Sprecher E, Conroy K, Krupa J, Shah S, Chi GW, Graham D, et al. A mixed-methods assessment of coronavirus disease of 2019-era telehealth acute care visits in the medical home. J Pediatr. (2023) 255:121–7. doi: 10.1016/j.jpeds.2022.10.036
113. Joseph HB, Kuppusamy S, Mahalik SK, Shetty AP, Das K. Telemedicine – a boon to parents of children with health care needs during COVID-19 pandemic: a qualitative study from India. Turk Arch Pediatr. (2022) 57(5):526–31. doi: 10.5152/TurkArchPediatr.2022.22046
114. Kelly SL, Steinberg EA, Suplee A, Upshaw NC, Campbell KR, Thomas JF, et al. Implementing a home-based telehealth group adherence intervention with adolescent transplant recipients. Telemed J E Health. (2019) 25(11):1040–8. doi: 10.1089/tmj.2018.0164
115. Trace SL, Collinson A, Searle AJ, Lithander FE. Using videoconsultations to deliver dietary advice to children with chronic kidney disease: a qualitative study of parent and child perspectives. J Hum Nutr Diet. (2020) 33(6):881–9. doi: 10.1111/jhn.12750
116. Doerdelman J, Frielitz FS, Lange K, Meinsen T, Reimers S, Ottersberg T, et al. Video consultation for parents with a child newly diagnosed with type 1 diabetes: a qualitative study. Exp Clin Endocrinol Diabetes. (2022) 130(8):519–24. doi: 10.1055/a-1655-5471
117. Garne Holm K, Brodsgaard A, Zachariassen G, Smith AC, Clemensen J. Parent perspectives of neonatal tele-homecare: a qualitative study. J Telemed Telecare. (2019) 25(4):221–9. doi: 10.1177/1357633X18765059
118. Tschamper MK Jakobsen R. Parents’ experiences of videoconference as a tool for multidisciplinary information exchange for children with epilepsy and disability. J Clin Nurs. (2019) 28:1506–16. doi: 10.1111/jocn.14755
119. Hylén M, Nilsson S, Kristensson-Hallstrὂm I, Kristjánsdóttir G, Stenstrὂm Vilhjálmsson R. Access to health care perceived by parents caring for their child at home supported by eHealth – a directed approach introducing aperture. BMC Health Serv Res. (2022) 22:1–11. doi: 10.1186/s12813-022-08398-0
120. Blagdon A, Smith D, Bramfield T, Soraisham A, Mehrem AA. Evaluation of family and staff experiences with virtual rounding and bedside presence in a tertiary neonatal intensive care unit during the COVID-19 pandemic. J Telemed Telecare. (2022) 30:1–15. doi: 10.1177/1357633X221081294
121. Gefen N, Steinhart S, Beeri M, Weiss PL. Lessons learned during a naturalistic study of online treatment for pediatric rehabilitation. Int J Environ Res Public Health. (2021) 18:1–17. doi: 10.3390/ijerph18126659
122. Hoyt-Austin AE, Miller IT, Kuhn-Riordon KM, Rosenthal JL, Chantry CJ, Marcin JP, et al. Bonding, relaxation, separation, and connection: expressing human milk while videoconferencing with the hospitalized premature infant. Breastfeed Med. (2022) 17(8):653–9. doi: 10.1089/bfm.2021.0214
123. Strand AS, Johnsson B, Hena M, Magnusson B, Hallstrom IK. Developing eHealth in neonatal care to enhance parents’ self-management. Scan J Caring Sci. (2022) 36(4):969–77. doi: 10.1111/scs.12994
124. Lee S, Dick BD, Jordan A, McMurty CM. A parent-targeted group intervention for pediatric pain delivered in-person or virtually: feasibility, acceptability, and effectiveness. Clin J Pain. (2023) 39(3):127–37. doi: 10.1097/AJP.0000000000001100
125. Mimila NA, Chung PJ, Elliott MN, Bethell CD, Chacon S, Biely C, et al. Well-child care redesign: a mixed methods analysis of parent experiences in the PARENT trial. Acad Pediatr. (2017) 17(7):747–54. doi: 10.1016/j.acap.2017.02.004
126. Chan EYH, Liu MS, Or PC, Ma ALT. Outcomes and perception of cloud-based remote patient monitoring in children receiving automated peritoneal dialysis: a prospective study. Pediatr Nephrol. (2022) 38:2171–8. doi: 10.1007/s00467-022-05828-3
127. Gan Z, Lee SY, Weiss DA, Van Batavia J, Siu S, Frazier J, et al. Single institution experience with telemedicine for pediatric urology outpatient visits: adapting to COVID-19 restrictions, patient satisfaction, and future utilization. J Pediatr Urol. (2021) 17(4):480.e1–e7. doi: 10.1016/j.jpurol.2021.05.012
128. Dempsey CM, Serino-Cipoletta JM, Marinaccio BD, O'Malley KA, Goldberg NE, Dolan CM, et al. Determining factors that influence parents’ perceptions of telehealth provided in a pediatric gastroenterological practice: a quality improvement project. J Pediatr Nurs. (2022) 62:36–42. doi: 10.1016/j.pedn.2021.11.023
129. Brothwood PL, Baudinet J, Stewart CS, Simic M. Moving online: young people and parents’ experiences of adolescent eating disorder day programme treatment during the COVID-19 pandemic. J Eat Disord. (2021) 9(1):1–10. doi: 10.1186/s40337-021-00418-4
130. McLardie-Hore FE, McLachlan HL, Shafiei T, Forster DA. Proactive telephone-based peer support for breastfeeding: a cross-sectional survey of women’s experiences of receiving support in the RUBY randomised controlled trial. BMJ Open. (2020) 10:1–11. doi: 10.1136/bmjopen-202-040412
131. Lindkvist RM, Sjostrom-Strand A, Landgren K, Johnsson BA, Stenstrom P, Hallstrom IK. “In a way we took the hospital home”-A descriptive mixed-methods study of Parents’ usage and experiences of eHealth for self-management after hospital discharge due to pediatric surgery or preterm birth. Int J Environ res Public Health. (2021) 18:1–13. doi: 10.3390/ijerph18126480
132. Huscsava MM, Scharinger C, Plener PL, Kothgassner OD. The world somehow stopped moving: impact of the COVID-19 pandemic on adolescent psychiatric outpatients and the implementation of teletherapy. Child and Adolesc Ment Health. (2022) 27(3):232–7. 10.1111.camh.12481
133. Ruskin D, Tremblay M, Szczech K, Rosenbloom BN, Mesaroli G, Sun N, et al. Virtual multidisciplinary pain treatment: experiences and feedback from children with chronic pain and their caregivers. Physiother Theory Pract. (2023) 40:1–22. doi: 10.1080/09593985.2023.2171750
134. Edwards LM, Parry M. Telephone consultations to manage paediatric outpatient clinics during the COVID-19 pandemic: a service evaluation. Ir J Med Sci. (2022) 191(3):977–83. doi: 10.1007/s11845-021-02672-6
135. Castro MJ, Rodriguez RJ, Hudson B, Weersing VR, Kipke M, Peterson BS, et al. Delivery of cognitive behavioral therapy with diverse, underresourced youth using telehealth: advancing equity through consumer perspectives. Evid Based Pract Child Adolesc Ment Health. (2022) 8(2):206–20. doi: 10.1080/23794925.2022.2062687
136. Tsai C, Savran A, Chau Y, Hurrell L, Forsyth C, Kumar H. Effectiveness of telehealth in providing preventive oral health care: a pilot evaluation of patient, carer, and clinician experience. J Public Health Dent. (2023) 83(4):331–9. doi: 10.1111/jphd.12580
137. Birnie KA, Killackey T, Backlin G, Gavin F, Harris C, Jordan I, et al. Ensuring equity and inclusion in virtual care best practices for diverse populations of youth with chronic pain. Healthc Q. (2022) 24:25–30. doi: 10.12927/hcq.2022.26778
138. Sinha N, Cornell M, Wheatley B, Munley N, Seeley M. Looking through a different Lens: patient satisfaction with telemedicine in delivering pediatric fracture care. J Am Acad Orthop Surg Glob Res Rev. (2019) 3(9):1–6. doi: 10.5435/JAAOSGlobal-D-19-00100
139. Hale AE, Bujoreanu S, LaVigne TW, Coakley R. Rapid mobilization of an evidence-based psychological intervention for pediatric pain during COVID-19: the development and deployment of the comfort ability program virtual intervention (CAP-V). Children. (2023) 10:1–14. doi: 10.3390/children10091523
140. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract. (2005) 8(1):19–32. doi: 10.1080/1364557032000119616
Keywords: virtual care, synchronous, telehealth, pediatrics, scoping review
Citation: Zulla RT, Nicholas DB, Sutherland S, Cohen E, Birnie K, Anthony S, Robeson P, Selkirk E, Killackey T, Mohabir V and Stinson J (2025) Synchronous virtual care in children’s health care: a scoping review. Front. Pediatr. 13:1610407. doi: 10.3389/fped.2025.1610407
Received: 11 April 2025; Accepted: 24 September 2025;
Published: 6 November 2025.
Edited by:
Toshiyo Tamura, Waseda University, JapanCopyright: © 2025 Zulla, Nicholas, Sutherland, Cohen, Birnie, Anthony, Robeson, Selkirk, Killackey, Mohabir and Stinson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: R. T. Zulla, cnp1bGxhQHVjYWxnYXJ5LmNh
 R. T. Zulla
R. T. Zulla D. B. Nicholas
D. B. Nicholas S. Sutherland1
S. Sutherland1 K. Birnie
K. Birnie S. Anthony
S. Anthony J. Stinson
J. Stinson