- 1Department of Pediatrics, Chinese People’s Liberation Army Eastern Theater Command General Hospital, Nanjing, China
- 2Nanjing Stomatological Hospital, Affiliated Hospital of Medical School, Institute of Stomatology, Nanjing University, Nanjing, China
Background: This study aimed to investigate the transition readiness of adolescent patients with kidney disease to understand their readiness status and ability to transition to adult healthcare and study the influencing factors, to provide a theoretical basis for improving the transition readiness of adolescent patients with kidney disease and developing intervention strategies.
Methods: The study sample was obtained from the follow-up data of the pediatric department at the General Hospital of the Eastern Theater of Operations from December 2024 to January 2025, and patients aged 13–18 years with renal disease were selected as the study subjects. The scores of the Chinese version of the Self-Management and Transitional Readiness Questionnaire were used to determine the readiness status of the study subjects, and binary logistic regression was used to analyze the influencing factors.
Results: A total of 242 questionnaires were distributed, and 12 invalid questionnaires were excluded, resulting in the inclusion of 230 samples for the analysis. Transitional readiness was at a low level in 123 cases (53.48%) and at a medium-high level in 107 cases (46.52%). The results of the binary logistic regression showed that the number of hospitalizations, treatment modalities, place of residence, caregiver's literacy, monthly income, and healthcare payment method were influencing factors for transition readiness in adolescent patients with kidney disease (P < 0.05).
Conclusion: The readiness of adolescent patients with kidney disease during their transition to adulthood is not ideal and is affected by a combination of factors related to themselves, their families, and their socioeconomic status. The relevant medical personnel should implement a multidimensional approach and carry out targeted interventions to improve these patients’ readiness for the transition.
Background
Chronic kidney disease (CKD) is a group of clinical syndromes characterized by structural damage and functional abnormalities of the kidneys, and its pathogenic mechanism involves multifactorial interactions (1). It is worth noting that epidemiological survey data show that the incidence of this disease in the pediatric population has shown a significant upward trend in recent years, and has become an important public health problem that threatens children's health (2). For adolescents with chronic kidney disease, the disease will accompany them throughout their growth, resulting in differences in their lives compared with the normal population. Clinical treatment of pediatric chronic kidney disease achieves partial remission, but there is a significant tendency toward relapse and risk of multisystem complications (3). Of particular concern is that long-term glucocorticoid regimens based on immunosuppression may trigger growth retardation, metabolic disorders, and other long-term endocrine system-related adverse effects, leading to an increasing tension between therapeutic benefits and developmental impairments (4). Studies of adolescents with chronic diseases have shown that the current healthcare system is characterized by intergenerational dependence, whereby patients rely primarily on their parents for disease monitoring and treatment decisions, and the lack of systematic transition preparedness education has resulted in patients failing to meet the desired standards of healthcare autonomy in the transition (5). This disruption in medical continuity significantly increases the risk of adverse clinical outcomes such as decreased treatment adherence, lack of self-management skills, and ultimately, accelerated disease progression and worsened long-term prognosis (6). One study showed that more than 50% of adolescents with chronic kidney disease were not prepared for transfer to adult care at the time of transfer (7). Currently, domestic research on the readiness of adolescents with kidney disease for the transition is still in its infancy, and there is a lack of research on the current readiness of the relevant population for the transition and the factors affecting it, with existing research only involving the exploration of the patient's inner feelings, behaviors, and perceptions (8). This study was a cross-sectional survey to understand the current readiness for transition among adolescents with kidney disease and the factors affecting it, with the aim of informing transitional care programs for adolescents with kidney disease.
Methods
Objectives of the study
Adolescent patients with nephropathy were selected for the study from the Department of Pediatrics, Eastern Theater General Hospital, from December 2024 to January 2025. The inclusion criteria were as follows: (1) meeting the diagnostic criteria for chronic kidney disease, (2) aged 13–18 years, and (3) informed parental consent to participate in this study. The exclusion criteria were as follows: (1) chronic kidney disease combined with severe cardiopulmonary and other organ failure, (2) chronic kidney disease combined with malignant tumors, (3) serious conditions that made it difficult to conduct investigations, and (4) hearing and speech communication disorders. All the patients’ disease information in this study was diagnosed and confirmed by physicians, and patient information was found in their medical records. The study was approved by the hospital’s ethics committee (2024DZKY-106-01).
Investigation content relevant to this study
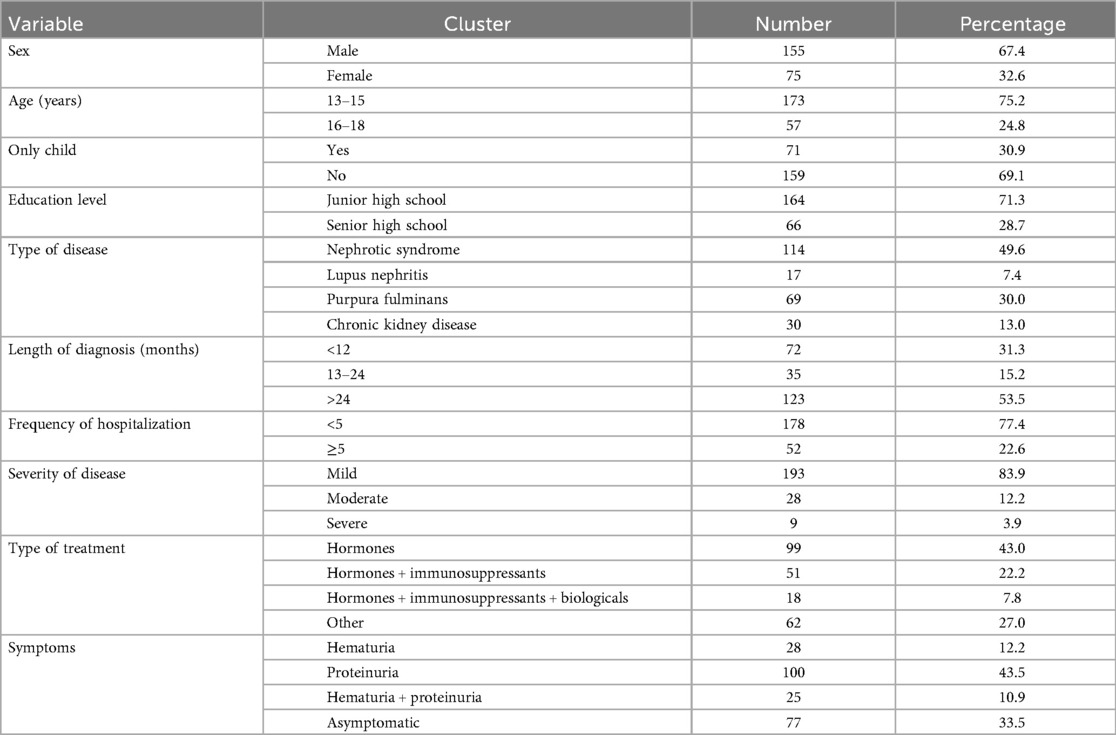
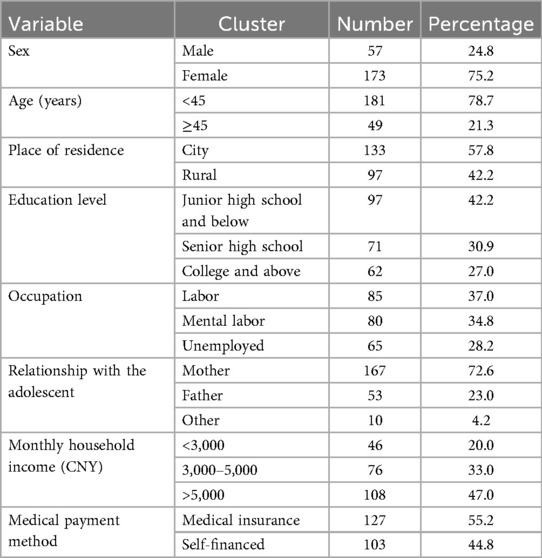
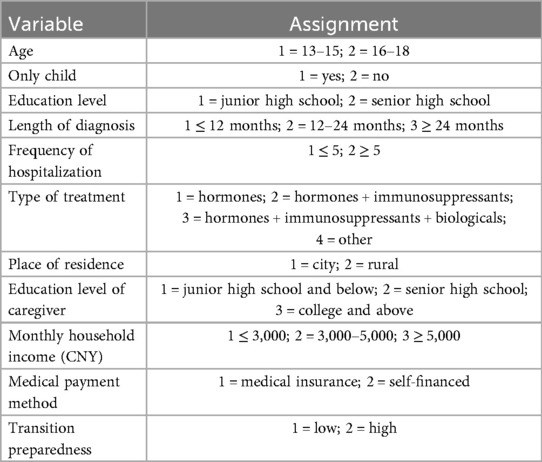
The Adolescent Kidney Disease Patient Profile Questionnaire provided data on the patients’ sex, age, education, type of disease, length of diagnosis, frequency of hospitalization, severity of disease, treatment, and symptoms, and whether they were an only child (Table 1). Furthermore, the Caregiver Profile Questionnaire for Adolescents with Kidney Disease provided data on the caregivers’ sex, age, place of residence, education level, occupation, relationship to the child, monthly family income, and mode of medical payment (Table 2).
The Chinese version of the Self-Management and Transition Readiness Questionnaire Self-Management and Over-Preparedness Questionnaire (STARx) was designed by Ferris et al. (9) for adolescents with chronic illnesses to identify the main factors related to transition readiness. The Chinese version of the Self-Management and Transition Readiness Questionnaire (SMARTQ) was used in this study as a Chinese version of the STARx questionnaire, with 18 unchanged entries, and the original six dimensions were modified and integrated into the following four dimensions: medication management, health participation, doctor–patient communication, and knowledge of disease. The Cronbach's coefficient for the modified scale was 0.83. The questions in the questionnaire were scored on a 5-point Likert scale, with higher total scores indicating better transition readiness, and scores of less than 60 being defined as a low level of transition readiness in this study (10).
Finally, the Adolescent Kidney Disease Patient Profile Questionnaire and the Chinese version of the STARx were applied to the adolescent patients, while the Caregiver Profile Questionnaire for Adolescents with Kidney Disease was applied to the patients’ caregivers.
Sample size estimation
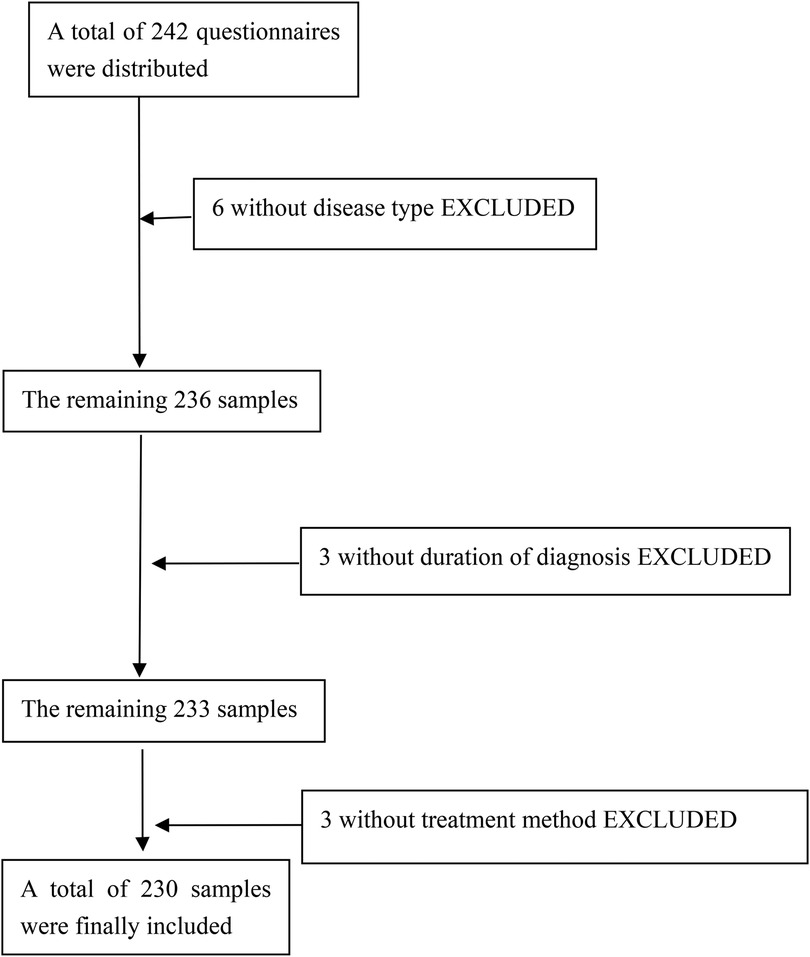
Based on the relevant reviewed literature (11), a sample size of 5–10 times the total number of variables was required for this study. Thus, with a total of 22 variables included in this study, and taking into account about 20% of invalid questionnaires, a total of 242 questionnaires were distributed. Among the 12 excluded samples, 6 were lacking data in “disease type,” 3 were lacking data in “duration of diagnosis,” and 3 were lacking data in “treatment method” (Figure 1).
Statistical methods
In this study, SPSS 27.0 software was used to statistically analyze the collected data. The count data were expressed as relative numbers and the χ2 test was used for the between-groups comparison. Measurement data with normal distribution were expressed as mean ± standard deviation and data with a non-normal distribution were expressed as M (P25, P75). Factors influencing transition readiness in adolescents with kidney disease were analyzed by binary logistic regression, and differences were considered statistically significant at P < 0.05.
Results
Univariate analysis of transition readiness in adolescents with kidney disease
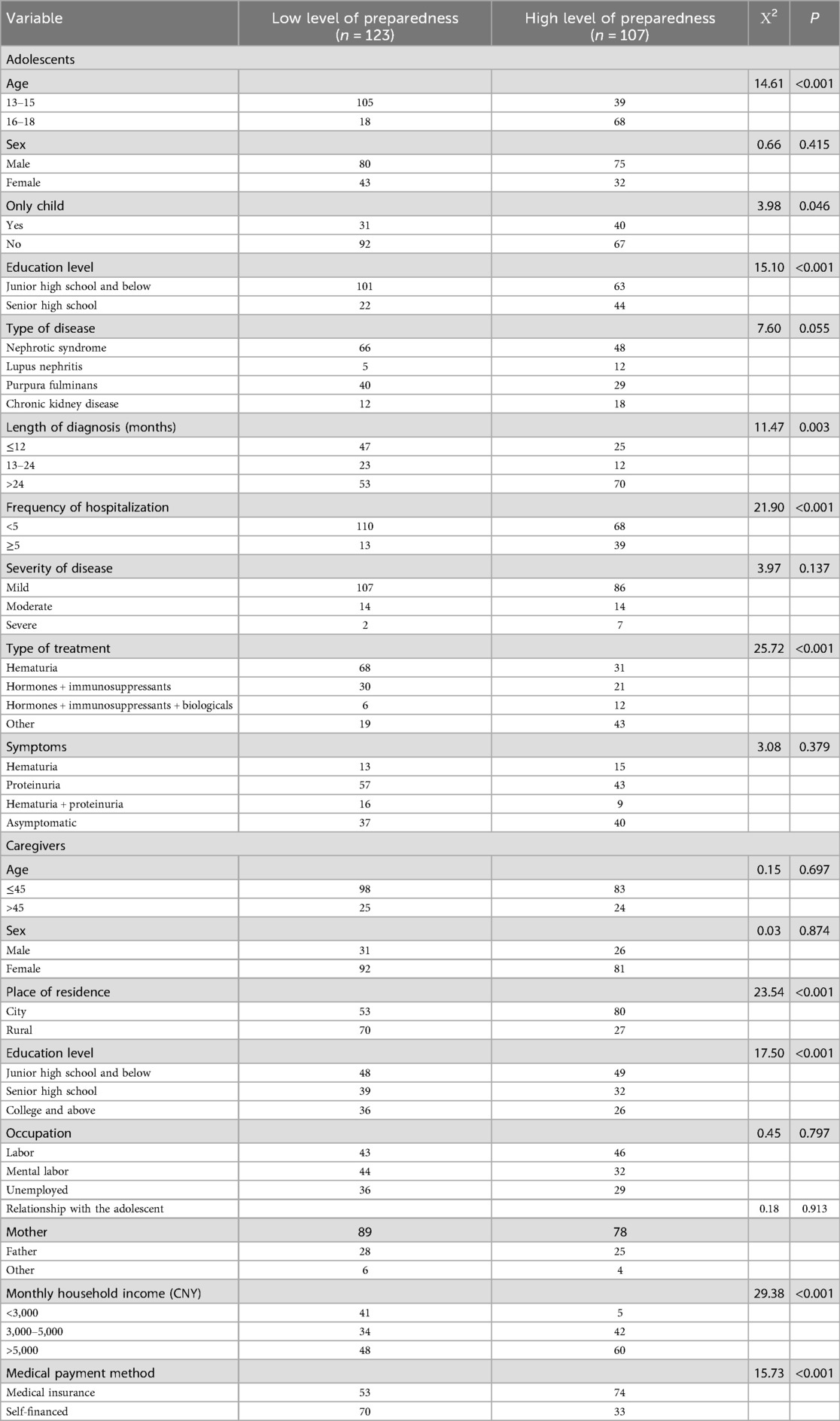
Of the 230 adolescent patients with kidney disease, 123 (53.48%) had a low level of transition readiness and 107 (46.52%) had a medium-high level. Of those with a low level of transition readiness, 105 (85.36%) were in the 13–15-year-old age group, and 18 (14.64%) were in the 16–18-year-old age group. In the univariate analysis, the differences between adolescent patients with low and high levels of transition readiness were statistically significant (P < 0.05) for age, whether they were an only child, education level, length of disease diagnosis, number of hospitalizations, and mode of treatment; Moreover, for the caregivers, there were statistically significant differences in place of residence, education level, monthly income, and mode of medical payment (Table 3).
Binary logistic regression analysis of transition readiness in adolescents with kidney disease
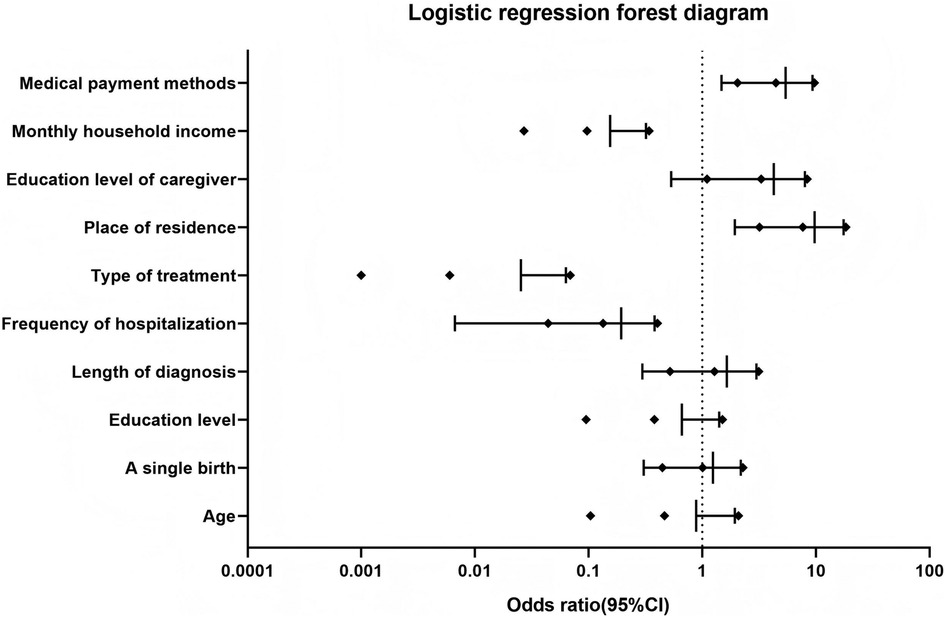
A binary logistic regression analysis was performed with the transition readiness of adolescent patients with kidney disease as the dependent variable and the statistically significant variables in the univariate analysis results as the independent variables (age, whether they were only child, education level, length of disease diagnosis, number of hospitalizations, and mode of treatment for the adolescent patients and place of residence, education level, monthly income, and mode of medical payment for the caregivers), which showed that the number of hospitalizations, treatment modalities, place of residence, caregiver's literacy, monthly income, and healthcare payment method were influencing factors for the transition readiness of adolescent patients with kidney disease (P < 0.05) (Tables 4, 5).
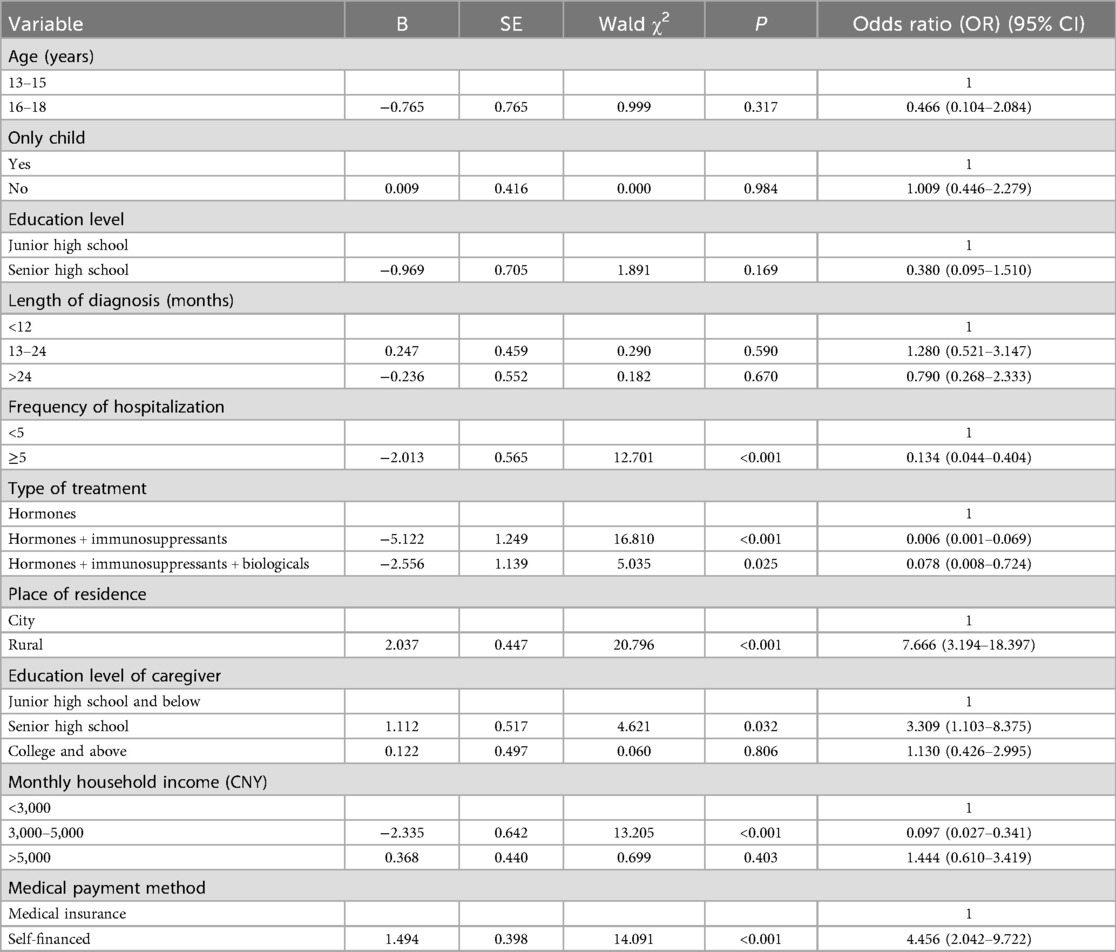
Table 5. Binary logistic regression analysis of transition readiness in adolescent patients with kidney disease.
We assessed multicollinearity by calculating the variance inflation factor (VIF) for all the variables included in the multivariate logistic regression model. The VIF values for both age and education level were below the commonly accepted threshold of 1.0, indicating no serious multicollinearity. Finally, we created a forest plot summarizing the main results from the multivariable logistic regression analysis (Figure 2).
Discussion
In this study, 53.48% of the adolescent patients with kidney disease had a low level of transition readiness, indicating that this problem has become a medical issue that cannot be ignored. This study adheres to the transitional guidelines of the European Society of Paediatric Nephrology (12).
In this study, adolescent kidney disease patients with ≥5 hospitalizations had lower transition readiness than those with <5 hospitalizations, a finding that differs from previous studies (13). Previous findings have suggested that patients with more hospitalizations have greater transition readiness because they have gradually adapted to their disease condition and have acquired some knowledge about their disease (14). The results of the present study are contrary to previous studies, and the reason for this phenomenon may be that frequent hospitalization of adolescent patients with kidney disease is caused by the complexity of the disease, poor control of the disease, or even deterioration of the disease, which results in adolescents having to rely on the decision-making of healthcare professionals for a long period of time, which weakens their own management (15). It may also be due to the fact that the medical care of the patient during hospitalization is led by healthcare professionals, and the patient is in the role of passive recipient of care for a long period of time, and lacks the opportunity to practice independent medication administration, symptom monitoring, etc., which leads to difficulties in adapting to being autonomous during the transition period (16). Therefore, healthcare professionals should pay attention to patients’ number of hospitalizations in daily patient management and develop their ability to participate in disease management from passive acceptance to active participation.
In this study, transition readiness was lower in adolescent patients with kidney disease treated with hormones + immunosuppressants or hormones + immunosuppressants + biologics compared to hormone therapy alone, which is consistent with previous findings (17). For patients, treatment complexity is positively correlated with cognitive load, and adolescent patients with kidney disease on multiple treatment modalities have to manage both hormonal treatment strategies and immunosuppressive blood level monitoring, with a management load that is significantly greater than that of patients on hormonal therapy alone (18). The risk of infection is greatly increased in patients treated with immunosuppressive drugs, and often the patient's daily social activities are compromised to avoid the risk of infection, leading to a decrease in social functioning and further dependence on parental decision-making (19). Co-medication can lead to an increase in the severity of a patient's disease, which can lead to negative self-perceptions and reduced motivation for self-health management in adolescent patients (20). This suggests that medical personnel involved in patient treatment and care should receive comprehensive education regarding the uses and precautions associated with medications. This will enable them to develop a thorough and clear understanding of their own medication regimens and disease conditions, thereby enhancing their confidence in treatment and helping to prevent negative or pessimistic attitudes.
In this study, the transition readiness of adolescent patients with kidney disease residing in rural areas was higher than that of patients in urban areas. It has been suggested that in rural areas, where there are more multigenerational families and a closer division of labor among relatives, patients may be involved in family affairs at an earlier age and develop independence and a sense of responsibility, which may enable them to take the initiative in disease management (21). Urban families may rely more on healthcare providers and have fewer opportunities for patient self-care, resulting in a lag in the development of self-management skills (22). Adolescent patients with kidney disease in rural areas are more adaptable to the independence requirements of the transition period because of the inconvenience of accessing medical care, which pushes them to learn medication management, disease monitoring, and some basic nursing care earlier; in urban areas, where healthcare resources are abundant, patients are accustomed to frequent visits and timely interventions, and there is a phenomenon of overprotection of children by their parents, which may neglect the development of long-term self-management skills (23). This leads to greater anxiety about independent living; therefore, transitional care should focus on fostering autonomy and designing differentiated support strategies for families from different backgrounds.
The results of this study showed that the transition readiness of adolescent patients with kidney disease with a monthly household income between $3,000 and $5,000 was lower than that of patients with a monthly household income of <$3,000, and that the transition readiness of patients who paid out-of-pocket was higher than that of patients who paid via medical insurance. Financial constraints force patients and families to acquire nursing skills at home earlier to reduce the financial burden of frequent visits to the doctor; thus, long-term financial pressure is an incentive for patients to take the initiative to learn disease management skills (24). Financially stressed patients and families may be forced to develop early recognition of symptoms and emergency management plans for their illnesses due to the inconvenience and cost of access, increasing their confidence to cope independently during the transition period (25). The experience of coping with resource scarcity over a long period of time leads to the development of problem-solving skills and resilience to stress, which are highly compatible with the psychological qualities needed for transition. Low-income patients, due to financial constraints, accept the reality of long-term coexistence with the disease earlier and incorporate self-management of the disease into their daily life planning (26). Higher-income families may become “service dependent” and rely more on paid services, resulting in less child autonomy and family engagement. Furthermore, higher-income families may be overprotective of their children, reducing their opportunities to face challenges and leading to weaker psychological adjustment. For patients covered by medical insurance, families may rely on insurance to a certain extent to cover costs, resulting in relatively low participation in the medical process. This may lead to patients lagging behind self-paying patients in terms of self-management skills and other areas, resulting in a slight lack of preparedness during the transition period. Self-pay means that families must bear the full cost of medical expenses, which makes them more attentive to the patient's condition and treatment process. Families may be more actively involved in treatment decisions, providing patients with greater support and guidance, thereby helping enhance patients’ understanding and management of their own conditions and prepare for the transition period. When managing adolescents during the transition period, healthcare professionals also need to be aware of the patient's family's financial situation and the child's caregiver's knowledge of the disease.
Conclusion
This study shows that the overall level of transition readiness in adolescents with kidney disease is at a low level and is influenced by a combination of factors related to one’s self, family, and socioeconomic status. The results of this study suggest that transition readiness is not determined solely by resource abundance but is the result of a combination of resource access, stress coping patterns, and goal integration capabilities. The healthcare team needs to look beyond the surface and identify the mechanisms of family functioning to develop effective individualized transition plans, and future interventions need to focus on improving patients’ practical skills, psychological resilience, and community support networks.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The data for this study were obtained from the Department of Pediatrics, Eastern Theater General Hospital, and all methods were performed in accordance with relevant guidelines and regulations. All adolescent patients participating in this study and their parents were informed and signed informed consent forms. The study was approved by the hospital’s ethics committee (2024DZKY-106-01).
Author contributions
SB: Writing – original draft. ML: Writing – original draft. JL: Data curation, Writing – review & editing. WL: Writing – review & editing. LJ: Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ferris ME, Cuttance JR, Javalkar K, Cohen SE, Phillips A, Bickford K, et al. Self-management and transition among adolescents/young adults with chronic or end-stage kidney disease. Blood Purif. (2015) 39(1–3):99–104. doi: 10.1159/000368978
2. Javalkar K, Fenton N, Cohen S, Ferris M. Socioecologic factors as predictors of readiness for self-management and transition, medication adherence, and health care utilization among adolescents and young adults with chronic kidney disease. Prev Chronic Dis. (2014) 11:E117. doi: 10.5888/pcd11.140072
3. Bertram JF, Goldstein SL, Pape L, Schaefer F, Shroff RC, Warady BA. Kidney disease in children: latest advances and remaining challenges. Nat Rev Nephrol. (2016) 12(3):182–91. doi: 10.1038/nrneph.2015.219
4. Caskey FJ, Morton RL. Optimising care for children with kidney disease. Lancet. (2017) 389(10084):2084–6. doi: 10.1016/S0140-6736(17)30267-2
5. Stern-Zimmer M, Calderon-Margalit R, Skorecki K, Vivante A. Childhood risk factors for adulthood chronic kidney disease. Pediatr Nephrol. (2021) 36(6):1387–96. doi: 10.1007/s00467-020-04611-6
6. Furth SL, Cole SR, Moxey-Mims M, Kaskel F, Mak R, Schwartz G, et al. Design and methods of the chronic kidney disease in children (CKiD) prospective cohort study. Clin J Am Soc Nephrol. (2006) 1(5):1006–15. doi: 10.2215/CJN.01941205
7. Crawford K, Wilson C, Low JK, Manias E, Williams A. Transitioning adolescents to adult nephrology care: a systematic review of the experiences of adolescents, parents, and health professionals. Pediatr Nephrol. (2020) 35(4):555–67. doi: 10.1007/s00467-019-04223-9
8. Qiaoyue Y, Yaqi Y, Genzhen Y, Ying L, Wanmei H, Wenshuai S, et al. A qualitative study on the preparation experience of adolescents during the transition period of chronic kidney disease. J Nurs. (2024) 39(09):116–20.
9. Ferris M, Cohen S, Haberman C, Javalkar K, Massengill S, Mahan JD, et al. Self-management and transition readiness assessment: development, reliability, and factor structure of the STARx questionnaire. J Pediatr Nurs. (2015) 30(5):691–9. doi: 10.1016/j.pedn.2015.05.009
10. Cohen SE, Hooper SR, Javalkar K, Haberman C, Fenton N, Lai H, et al. Self-management and transition readiness assessment: concurrent, predictive and discriminant validation of the STARx questionnaire. J Pediatr Nurs. (2015) 30(5):668–76. doi: 10.1016/j.pedn.2015.05.006
11. Mbalinda SN, Bakeera-Kitaka S, Lusota DA, Musoke P, Nyashanu M, Kaye DK. Transition to adult care: exploring factors associated with transition readiness among adolescents and young people in adolescent ART clinics in Uganda. PLoS One. (2021) 16(4):e0249971. doi: 10.1371/journal.pone.0249971
12. Forbes TA, Watson AR, Zurowska A, Shroff R, Bakkaloglu S, Vondrak K, et al. Adherence to transition guidelines in European paediatric nephrology units. Pediatr Nephrol. (2014) 29(9):1617–24. doi: 10.1007/s00467-014-2809-4
13. Brands MR, Janssen EAM, Cnossen MH, Smit C, van Vulpen LFD, van der Valk PR, et al. Transition readiness among adolescents and young adults with haemophilia in the Netherlands: nationwide questionnaire study. Haemophilia. (2023) 29(5):1191–201. doi: 10.1111/hae.14834
14. Allemang B, Samuel S, Greer K, Schofield K, Pintson K, Patton M, et al. Transition readiness of youth with co-occurring chronic health and mental health conditions: a mixed methods study. Health Expect. (2023) 26(6):2228–44. doi: 10.1111/hex.13821
15. Chisolm DJ, Keedy HE, Hart LC, Chavez LJ, Dolce M, Morack J, et al. Exploring health literacy, transition readiness, and healthcare utilization in Medicaid chronically ill youth. J Adolesc Health. (2021) 69(4):622–8. doi: 10.1016/j.jadohealth.2021.03.023
16. Cui C, Zhou H, Chen W, Li S, Zheng X. Behavioral dilemmas and support requirements of self-management for Chinese adolescents with epilepsy during transition readiness: a mixed-methods study. Patient Prefer Adherence. (2023) 17:2605–19. doi: 10.2147/PPA.S429890
17. Rhee H, Choi Y, Tumiel-Berhalter L. Transition readiness in middle and older adolescents with asthma and associated factors: a descriptive study. J Asthma. (2023) 60(5):991–9. doi: 10.1080/02770903.2022.2119864
18. Uzark K, Smith C, Donohue J, Yu S, Afton K, Norris M, et al. Assessment of transition readiness in adolescents and young adults with heart disease. J Pediatr. (2015) 167(6):1233–8. doi: 10.1016/j.jpeds.2015.07.043
19. Jensen PT, Paul GV, LaCount S, Peng J, Spencer CH, Higgins GC, et al. Assessment of transition readiness in adolescents and young adults with chronic health conditions. Pediatr Rheumatol Online J. (2017) 15(1):70. doi: 10.1186/s12969-017-0197-6
20. Mikola K, Rebane K, Kautiainen H, Aalto K. Transition readiness among Finnish adolescents with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. (2023) 21(1):149. doi: 10.1186/s12969-023-00938-0
21. Poamaneagra SC, Galos F, Tataranu E, Mihai C, Anton C, Andronic C-M, et al. Transition readiness in pediatric chronic digestive diseases: a regional perspective from north-eastern Romania. Medicina (Kaunas). (2024) 60(12):2104. doi: 10.3390/medicina60122104
22. Campbell F, Biggs K, Aldiss SK, O'Neill PM, Clowes M, McDonagh J, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev. (2016) 4(4):CD009794. doi: 10.1002/14651858.CD009794.pub2
23. Abdwani R, Al Sabri R, Al Hasni Z, Rizvi S, Al Wahshi H, Al Lawati B, et al. Transition readiness in adolescents and young adults with chronic rheumatic disease in Oman: today’s needs and future challenges. Pediatr Rheumatol Online J. (2022) 20(1):27. doi: 10.1186/s12969-022-00687-6
24. Varty M, Popejoy LL. A systematic review of transition readiness in youth with chronic disease. West J Nurs Res. (2020) 42(7):554–66. doi: 10.1177/0193945919875470
25. Seydel A. Transition of care in adolescents with chronic disease: a concept analysis. J Spec Pediatr Nurs. (2023) 28(3):e12414. doi: 10.1111/jspn.12414
26. Schwartz LA, Daniel LC, Brumley LD, Barakat LP, Wesley KM, Tuchman LK. Measures of readiness to transition to adult health care for youth with chronic physical health conditions: a systematic review and recommendations for measurement testing and development. J Pediatr Psychol. (2014) 39(6):588–601. doi: 10.1093/jpepsy/jsu028
Keywords: adolescents, kidney disease, transition readiness, current status, influencing factors
Citation: Bai S, Lv M, Liu J, Liu W and Jia L (2025) Analysis of the current transition readiness of adolescent patients with kidney disease and the factors influencing it. Front. Pediatr. 13:1613963. doi: 10.3389/fped.2025.1613963
Received: 18 April 2025; Accepted: 26 August 2025;
Published: 19 September 2025.
Edited by:
Constantinos J. Stefanidis, "Mitera" Children's Hospital, GreeceReviewed by:
Frederick Kaskel, Children's Hospital at Montefiore, United StatesAskiti Varvara, Panagiotis & Aglaia Kyriakou Children's Hospital, Greece
Copyright: © 2025 Bai, Lv, Liu, Liu and Jia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lili Jia, ZGluZ2t3bHdkQDE2My5jb20=
†These authors have contributed equally to this work
 Shuo Bai
Shuo Bai Maomao Lv1,†
Maomao Lv1,† Jinteng Liu
Jinteng Liu Lili Jia
Lili Jia