- 1Department of Surgical Specialties, Faculty of Medicine and Pharmacy, University of Oradea, Oradea, Romania
- 2Department of Physical Education, Sport and Physiotherapy, Human Performance Research Center, University of Oradea, Oradea, Romania
- 3Help&Care Association, Oradea, Romania
- 4Orthopedics and Traumatology Department, Avram Iancu Military Hospital, Oradea, Romania
- 5Doctoral School of Biomedical Sciences, Faculty of Medicine and Pharmacy, University of Oradea, Oradea, Romania
Background: Correct posture during preadolescence is crucial for harmonious physical development and long-term musculoskeletal health. The examination of spinal and lower limb deficiencies in this age group represents a highly relevant and underexplored topic.
Objective: To determine the prevalence of postural deficiencies among Romanian preadolescents and to assess their correlations with body composition, coordination, and foot morphology.
Methods: A total of 983 children aged 8–12 years (507 boys, 51.6%; 476 girls, 48.4%) were recruited from six middle schools in Oradea, Bihor County, Romania. Postural assessment followed Kendall et al.'s protocol using a plumb line and grid chart. Plantar pressure and center of gravity displacement were evaluated through baropodometry, while general coordination was assessed using the Matorin test.
Results: Forward head posture was the most prevalent deficiency (641/983, 65.2%). Boys exhibited a higher prevalence of kyphosis (n = 448, 52.3%) compared with girls (n = 368,40.4%), while scoliosis occurred more frequent in girls (n = 306, 33.6%) vs. (n = 257, 26.1%). Significant correlations were observed between ankle valgus and scoliosis [x2(1) = 7.87, p = .005], flatfoot and scoliosis [x2(1) = 7.87, p = .005], and flatfoot and coordination deficits [x2(3) = 22.96, p = .005].
Conclusions: Forward head posture emerged as the most common spinal deficiency. Notable associations were identified between body composition and kyphosis, hyperlordosis, and ankle valgus, as well as between flatfoot, scoliosis, and impaired coordination. These findings underscore the importance of early detection and the implementation of targeted prevention programs to address postural deficiencies during childhood.
Introduction
Correct posture during preadolescence is fundamental for balanced physical development and long-term health. Regular physical activity appropriate ergonomics, and healthy lifestyle habits play essential roles in maintaining postural alignment. Children should be encouraged to monitor their posture and to take frequent breaks during sedentary activities in order to prevent muscle stiffness (1). Proper posture reflects musculoskeletal balance which protects anatomical structures from injury or deformity, whereas poor posture, characterised by improper alignment, increases tension in supporting structures and negatively affects balance. Posture is influenced by multiple factors, including age, gender, somatic structure, psychological state, lifestyle, and level of physical activity (2).
Postural deviations are increasingly recognised as a significant public health concern among school-aged children. Epidemiological studies from Romania reporting a high prevalence of spinal misalignments, including scoliosis, kyphosis, and lordosis, frequently identified through school-based screenings using visual methods such as the plumb line (3, 4). Similar findings have been documented in other European countries, where between one-third and more than half of children and adolescents exhibit some form of postural deficiency, underscoring the widespread nature of the problem (5, 6). Beyond their clinical relevance, these deviations carry important social implications: they may affect physical performance, self-image, and quality of life during a sensitive developmental stage, while also predisposing individuals to musculoskeletal pain and dysfunction in adulthood. Consequently, the early identification and monitoring of postural deviations represent not only a medical but also a social priority, highlighting the need for reliable assessment methods and preventive interventions within the school environment. Throughout life, and particularly during prepubertal and pubertal phases, body posture undergoes significant changes as a result of multiple factors. Environmental influences, sedentary behaviour, reduced physical activity, and inadequate diet exert increasingly negative effects on posture (2). Among these influences, childhood obesity has emerged as a major concern, profoundly affecting postural indices. Contributing elements include reduced physical activity and prolonged screen time, trends that have been further intensified by the recent pandemic. Increased body mass index (BMI) has been associated with decreased stability, alterations of the pelvic axis, exaggerated lumbar lordosis, abdominal prominence, internal hip rotation, valgus knees, and flat feet (7).
Research has demonstrated correlations between body composition and postural or foot abnormalities in both children and adults (8–10). Elevated fat mass is associated with deviations from normal posture, whereas a higher percentage of skeletal muscle mass and fat-free mass correlates with fewer postural anomalies (8). Greater total fat mass and fat percentage are also linked to a more pronated foot posture (9). Jorgić et al. also highlighted the consistent influence of body composition parameters—such as fat mass and skeletal muscle percentage—on posture among children from different environments (10).
The relationship between posture and balance in children has been extensively studied. Ludwig et al. reported weak but significant correlation between age, BMI, and sway path length, but no significant association between posture parameters and sway path length (11). In a subsequent study, Ludwig also examined the influence of age on posture and balance control in a healthy pediatric population, finding subtle age-related changes (12).
Foot deformities and their relationship to balance reactions have also received attention. Wilczyński and Paprocki found significant correlations between foot abnormalities and balance deficits in school-aged children (13). Wilczyński et al. subsequently confirmed the association between postural variables and postural stability, observing that poorer balance is correlated with more pronounced postural defects (14).
Research into the interplay between posture and balance has expanded considerably. Azevedo et al. analysed the relationship between sagittal spinal angles and static equilibrium among 1,154 subjects, concluding that spinal postural angles are poor predictors of stabilometric outcomes (15). Nevertheless, posture remains fundamental for maintaining proprioception and coordinating movement, with posture and balance control systems operating in concert during locomotion and object manipulation (16).
Postural control relies on sensory input from visual, vestibular, and somatosensory systems, which integrate environmental information during motor planning and provide continuous feedback for movement adjustment (17). While previous research focused primarily on balance and posture separately, recent studies are beginning to explore potential links between poor posture, foot deformities, and coordination. For instance, variability in lower limb inter-joint coordination has been observed during gait in children with flexible flat feet (18). Moreover, Azevedo et al. emphasized the critical role of the foot in postural stability, through mechanical support, muscle coactivation, and sensory feedback from plantar mechanoreceptors (15).
Given the importance of early detection, somatoscopic assessment has become a widely used methods for identifying postural deficiencies, particularly spinal deformities (19). The existing literature underscores the complex interrelationship between posture and balance, yet important gaps remain in in understanding the specific correlations between common spinal deficiencies and foot deformities in preadolescents.
Current studies have mainly balance and its association with general posture parameters.
The aim of this study is therefore to estimate the prevalence of spinal and foot postural deficiencies among preadolescents and to determine whether correlations exist between bad posture, body composition and coordination as well as between foot conditions and spinal postural deficiencies.
Methods
Study area
Data collection was conducted in Oradea, Bihor County, Romania, an important economic and cultural center located in the northwestern part of Romania, Crisana region, with a population of approximately 245,537 inhabitants.
The district covers an area of 115,6 km2 with an estimated population of 245,537 inhabitants according to the 2021 census, resulting in a population density of approximately 1,585 inhabitants/km, which places Oradea as the 9th most populous city in Romania.
According to the information available for the 2023–2024 school year, Oradea's educational network includes17 middle schools (14 public and 3 private), with an average number of 850 children/units, providing a representative sample for assessing postural health in this age group.
Study design and period
This descriptive observational study was conducted in a cross-sectional manner, without intervention, between February to June 2024. The objective was to assess the prevalence of spine and feet postural deficiencies among preadolescents. The evaluation was performed by an experienced team of two physical therapists from Help&Care Association, Oradea, Romania.
Study population
The study population comprised preadolescent children enrolled in the middle school network of Oradea, Bihor County, Romania.
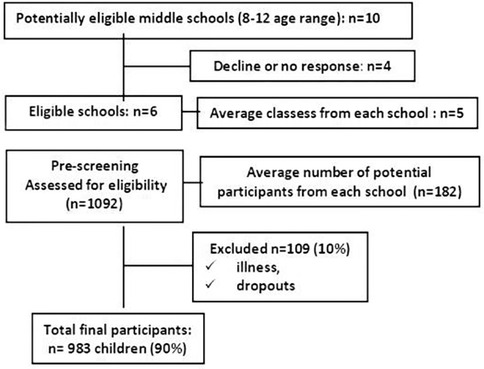
Sample size
To establish the sample size, the total number of children in all 17 middle schools of Oradea (approximately 14,450, with an average of 850 pupils per school) was used as the reference population. The calculation assumed a 95% confidence level, a 5% margin of error, and a population proportion of 0.5. Using an online sample size calculator (https://www.calculator.net/sample-size-calculator), the minimum recommended sample size was determined to be 357. Ultimately, 983 participants were included in this study, exceeding the minimum requirement.
Sampling procedures
A simple random sampling method was used for the recruitment process. The study protocol was submitted to the Institutional Review Board (IRB) for ethical approval prior to recruitment. The County School Inspectorate authorised the project, approved its implementation within educational institutions, and sent an invitation to ten local middle schools in Oradea. Enrollment followed a “first come, first served” principle. Six schools agreed to participate; four either declined or did not respond. No schools withdrew after enrollment.
The principals of participating schools distributed invitation to homeroom teachers of classes with pupils aged 8–12 years. The materials described the study's aims, procedures, evaluation process, and potential risks and benefits, and were forwarded to parents or legal guardians. They were asked to review the informations and provide written consent for their child's participation within one week.
On average, five classes per school (n = 182 children) agreed to participate. Based on parental consent, homeroom teacher compiled lists of students who wished to participate and submitted them to the project coordinator.
In total, 1,092 potential participants were screened for eligibility, with inclusion criteria requiring age 8–12 years and the absence of disability, congenital locomotor defects, genetic, hormonal, or neuromuscular diseases, and absence of minor musculoskeletal issues. On average, 10% of students per school were excluded owing to dropout or illness.
Ultimately, 983 children (average 164 per school; 90% of the initial sample) completed the one-time postural screening session (Figure 1).
Data analysis and communication of results
Trained professionals analysed the data. Parents received results along with tailored recommendations for exercises or interventions. Certificates of participation were distributed at the end of the study to encourage voluntary involvement and minimize selection bias.
Data protection and GDPR compliance
Participant identities and data were anonymized and securely stored, with access restricted to the research team. All procedures adhered to the General Data Protection Regulation (GDPR).
Blinding procedure
To reduce bias and enhance reliability, partial blinding was applied. Participants were not informed of the specific hypotheses to limit response bias. Data analysts worked with de-identified datasets to prevent unconscious bias. These measures strengthened objectivity, validity, and reproducibility.
Participants
The final cohort comprised 983 children aged 8–12 years, mean 10.03 (SD 1.41). Height ranged from 116 to 179 cm, mean 145.15 (SD 11.76), weight from 18.4 to 118.3 kg, mean 41.36 (SD 13.47) and body mass index (BMI) from 11 to 168, mean 19.41 (SD 6.44). All were recruited from middle schools in Oradea, western Romania.
The inclusion criteria were: age 8–12 years, no certificate of physical or intellectual disability, no diagnosed syndromes or congenital defects of the locomotor system that might impair psychomotor development, no genetic syndromes, hormonal disorders, neuromuscular diseases, no congenital motor system defects. The exclusion criteria were: the presence of syndromes and congenital musculoskeletal system defects, certificate of physical or intellectual disability, disorders likely to cause pathological posture (e.g., genetic syndromes, hormonal disorders, neuromuscular diseases, congenital defects of the locomotor system, slight musculoskeletal problems), age below 8 and above 12, no written consent for testing.
Ethical considerations
The study was conducted at the Research Center of Human Performance, Oradea University, in collaboration with Help&Care Association. Approval was obtained from the University Ethics Committee (No. 570/25.04). The study adhered to the Declaration of Helsinki to protect participants’ rights and well-being. Participants were fully informed, and minors provided consent via legal representatives. Confidentiality was ensured by assigning unique codes, with all data stored securely on encrypted servers. No compensation was provided.
Procedure
Body fat was assessed using the Jackson and Pollock method (20). Three skinfold sites were measured with a skinfold caliper: in girls—triceps, abdomen, thigh; in boys—chest, abdomen, thigh. Body fat percentage was calculated using the Jackson and Pollock 3-site equation. The GIMA brand adipocentimeter was used, which allows a correct assessment of the nutritional status and the sectoral distribution of adipose tissue, dimensions: 16.5 cm × 10 cm × 0.5 cm, weight 22 g.
Posture was examined following Kendall et al.'s protocol, employing a plumb line and a grid chart (5 × 5 cm vertical and horizontal lines) to identify imbalances of the head, trunk and lower limbs (21). Posture was assessed in the sagittal and frontal planes. Children were evaluated individually, standing and wearing appropriate clothing. Each child was instructed to assume a natural, relaxed standing position. The presence or absence of postural deviations was recorded as a dichotomous variable (Yes/No), with deviations defined as protracted or retracted shoulders, forward or backward head position, and inward or outward alignment of the knees or ankles. In view of the presence of gibbosity, a scoliometer was employed to measures the asymmetry of the trunk in scoliosis or the rotation angle of the trunk (22). It is a non-invasive device that is placed on the spine while a person is in a “lean forward” position. A GIMA brand scoliometer was used to confirm the presence of scoliosis. For the purposes of this study, posture analysis results were expressed as the total number of cases for each type of postural deviation.
Intra-rater reliability was assessed by a single evaluator re-analysing the same children, while inter-rater reliability was tested by a second evaluator. Agreement was quantified using Cohen's kappa (k).
Plantar analysis was performed using baropodometry (23). Baropodometry involves the assessment of static and dynamic plantar pressure using a foot pressure plate. When the foot encounters the sensors, a pressure map is generated instantaneously. The signal produced by the sensor activation are recorded and processed to create an image in which pressures magnitudes are represented by different shades of color. For this study, a flexible resistive baropodometric platform (Wiva® Smart FLex Plate-Letsense) was used. The system connects via WI-FI through the BIOMECH ® application (compatible with IOS and Android tablets) or via USB cable to a computer, enabling rapid acquisition of both static and the dynamic measurements (24). The analysis documented the presence or absence of plantar arch flattening and yielded the distribution of anterior, posterior, and lateral load. The following variables were recorded: anterior displacement of the center of gravity (COGA), posterior displacement of the center of gravity (COGP), right displacement of the center of gravity (COGR), left displacement of the center of gravity (COGL). Flattening of the plantar arch has been shown to correlate with pressure ratios across plantar regions (25, 26) and with displacement of the center of gravity (27).
General coordination was evaluated using the Matorin test (28). To perform the test, a circle must be drawn on the ground on which the degrees (0°, 45°, 90°, 135°, 180°, 225°, 270°, 315°, 360°) are noted. The subject places himself in the center of the circle and performed rotational jumps around the longitudinal axis, to the right or to the left. The subject is asked to land in the same place and position as when starting. The degrees of rotation achieved were recorded, with three attempts per child; the best performance was considered.
Statistical analysis
Quantitative and qualitative variables
Data analysis was performed using SPSS Evaluation version 15.0.0 (IBM, Oradea, Romania). Means and standard deviations were calculated for quantitative variables, while categorical variables were expressed as percentages. Extreme values were excluded to minimise bias. The normality of quantitative data distribution was tested using the Kolmogorov–Smirnov test. For qualitative variables, the Chi-square test for homogeneity was applied to evaluate whether frequency counts differed significantly between groups according to age and gender.
Statistical methods
Descriptive statistics were used to characterise the parameters of interest: mean ± standard deviation for ordinal data and percentages for categorical data. To determine whether significant gender-related differences existed in spinal postural deficiencies and foot conditions (flatfoot and ankle valgus), the Pearson Chi-square test was applied. Adjusted Standardised Residuals were computed to identify the specific groups contributing to significant differences.
The Phi coefficient was employed to assess correlations between foot conditions and spinal postural misalignment, with 95% confidence intervals (CIs) reported where appropriate. Point-biserial correlation was used to examine associations between BMI or BFI and the presence of spinal or foot deficiencies. As the analysis involved testing correlations between a dichotomous and a continuous variable, the point-biserial correlation was considered more appropriate than Spearman's correlation. A binomial logistic regression was conducted to examine the effects of age, gender, and BMI on the likelihood of presenting with flatfoot, ankle valgus, forward head posture, kyphosis, hyperlordosis, and scoliosis.
Finally, independent-samples t-tests were performed to compare coordination outcomes and center of gravity (COG) displacements between boys and girls.
Results
Table 1 presents the characteristics of the study population in terms of age, height, weight, body mass index, body fat index and activity level, both for the entire group and stratified by gender. The preadolescents group comprised 507 boys (51.6%) and 476 girls (48.4%). No significant gender-differences were observed in age, height, weight, BMI, or BFI. With respect to activity level, 476 participants (48.4%) reported regular engagement in sport. Of these, 261 boys (54.8%) and 215 girls (42.3%) engaged in regular sport activity.
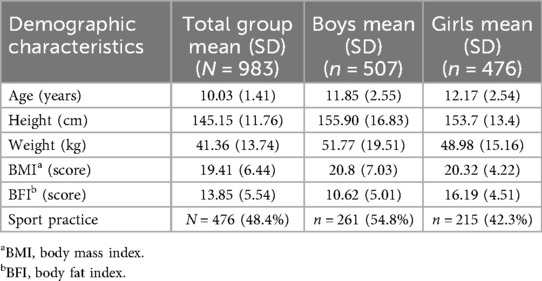
Table 1. Demographic characteristics for total preadolescents group and according to gender in Bihor County, Romania, 2024.
Table 2 presents the incidence of spinal and foot postural deficiencies in entire cohort, as well as gender-specific comparisons. Within the entire group, forward head posture was the most prevalent spinal deficiency (641/983, 65.2%). According to gender, forward head posture was the most common deficiency in both boys (545/983, 63.6%) and girls (572/ 983, 62.9%), while ankle valgus represented the most common foot deficiency in boys (387/983, 45.2%) and in girls (388/983, 42.6%).
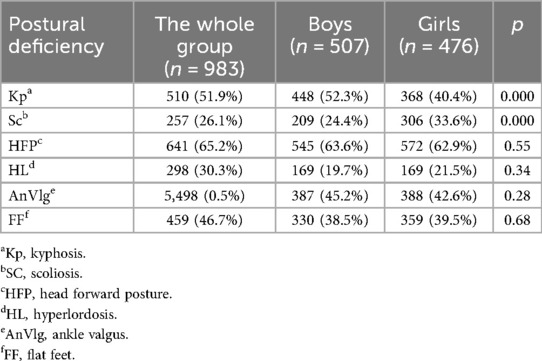
Table 2. The prevalence of spine and feet preadolescents postural deficiency for total group and according to gender in Bihor County, Romania, 2024.
In the preadolescent boys, the most prevalent postural deficiencies are head forward posture (545/983, 63.6%), followed by kyphosis (448/983, 52.3%), and ankle valgus (330/983, 38.5%). In the preadolescent girls, also the most prevalent postural deficiencies are head forward posture (572/983, 62.9%), followed by ankle valgus (388/983, 42.6%) and kyphosis (368/893, 40.4%).
The comparison analysis between preadolescent boys and girls showed that there is a significand difference in the prevalence of kyphosis in boys n = 448 (52.3%) comparing to girls n = 368 (40.4%) [x2(1) = 24.87, p˂0.001], and in the prevalence of scoliosis in girls n = 306 (33.6%) comparing to boys n = 257 (26.1%), [x2(1) = 18.24, p˂0.001]. There is no significant difference between groups regarding the head forward posture [x2 (2) = 1.187, p = 0.55]. Hyperlordosis [x2(1) = 0.891, p = 0.34], calcaneus valgus [x2(1) = 0.113, p = 0.28] and flat feet [x2(1) = 0.165, p = 0.68].
Intra-rater reliability of all spine and feet postural deficiency (kyphosis, scoliosis, head forward posture, hyperlordosis, ankle valgus and flat feet) showed moderate results, with Cohen's kappa (k) values for inter-rater reliability of all spinal postural deficiencies ranged from 0.356 to 0.579, showing no statistical difference in measurements between different raters.
In the total cohort, point-biserial correlation analysis indicated a weak positive association between BMI and scoliosis (r = .123, n = 983, p < 0.001), calcaneus valgus (r = .163, n = 983, p < 0.001) and flatfoot (r = .054, n = 983, p = 0.007). This means that there is a weak inverse association between elevated BMI and the presence of scoliosis and calcaneus valgus. A weak negative correlation was found between BMI and kyphosis (r = −.072, n = 983, p < 0.001) while hyperlordosis showed an even weaker positive correlation (r = .020, n = 983, p = 0.009) meaning that a high BMI is poor associated with kyphosis and hyperlordosis (Figure 2). No significant correlation was observed between BMI and forward head posture (r = −.050, n = 983, p = 0.11).
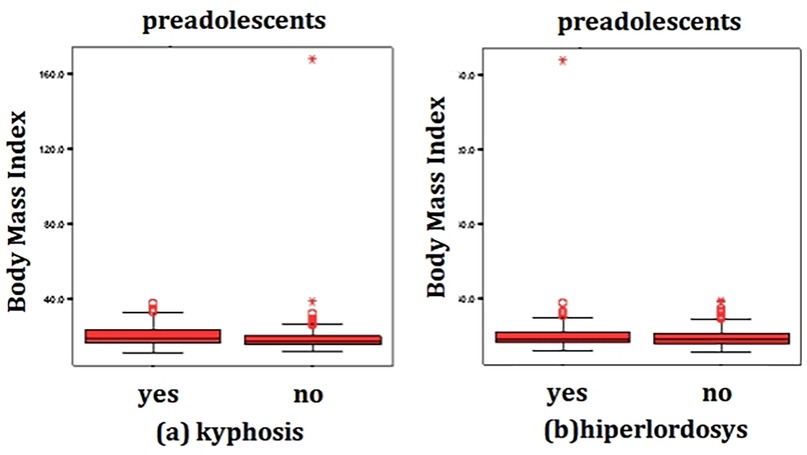
Figure 2. Correlation between BMI and the presence of kyphosis (a) and hyperlordosis (b) in preadolescents (n = 983), in Bihor County, Romania, 2024.
Point biserial correlation analysis of BFI demonstrated a weak positive correlation with ankle valgus (r = .073, n = 983, p < 0.001) and weak negative correlation with the presence of kyphosis (r = −.095, n = 983, p = 0.003) and hyperlordosis (r = −.162, n = 983, p < 0.001) (Figure 3). No significant correlations were identified between BFI and scoliosis (r = .014, n = 983, p = 0.66), forward head posture (r = −.023, n = 983, p = 0.46), or flatfoot (r = −.023, n = 983, p = 0.47). These results indicate that higher BFI showed a weak inverse association with ankle valgus and a weak positive association with kyphosis.
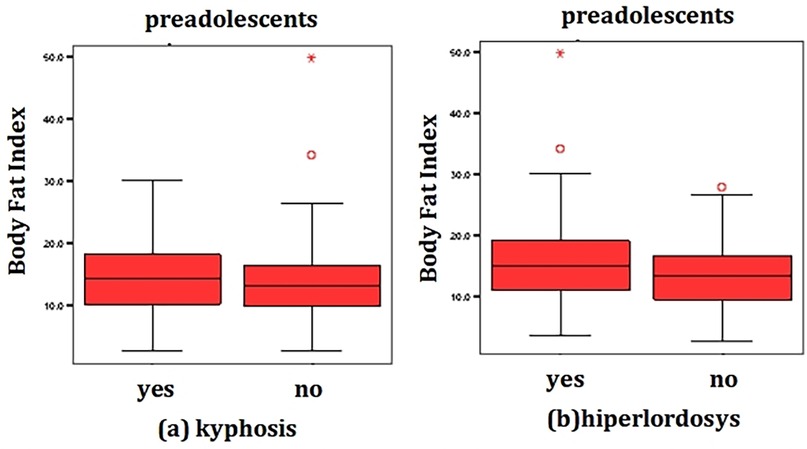
Figure 3. Correlation between BFI and the presence of kyphosis (a) and hyperlordosis (b) in preadolescents (n = 983), in Bihor County, Romania, 2024.
Analyses revealed a significant correlation between ankle valgus and scoliosis [x2(1) = 7.87, p = 0.005]. No significant associations were found coordination level [x2(3) = 3.69, p = 0.15], forward head posture [x2(1) = 1.20, p = 0.77], kyphosis [x2(2) = .306, p = 0.23], or hyperlordosis [x2(1) = 0.108, p = 0.15]. Flatfoot was significantly associated with both coordination [x2(3) = 22.96, p = 0.005] and scoliosis [x2(1) = 12.18, p < 0.001], but not with kyphosis [x2(1) = 2.70, p = 0.23], forward head posture [x2(2) = 6.38, p = 0.38], or hyperlordosis [x2(1) = 2.71, p = 0,27].
Table 3 presents the comparison of coordination and center of gravity (COG) displacement between boys and girls. Significant gender difference were observed for anterior displacement (COGA) [t(981)=−2.65, p = 0.005] and posterior displacement (COGP) [t(981) 753.24 = 2.309, p = 0.02]. No significant difference were found for rightward Matorin turns (RMT) [t(782)=−0.82, p = 0.056], leftward Matorin turns (LMT) [t(782)=−0.40, p = 0.13], rightward COG displacement (COGR) [t(981) = 0.89, p = 0.314], or leftward COG displacement (COGL) [t(981) = 0.60, p = 0.560].
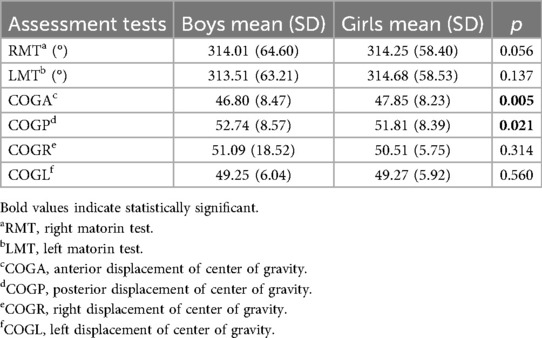
Table 3. Comparison between boys (n = 507) and girls (n = 476) regarding the results of coordination and center of gravity displacement, in Bihor County, Romania, 2024.
The logistic regression model was statistically significant for kyphosis [χ2(3) = 58.299, p < .0005], hyperlordosis [χ2(3) = 42.37, p < .0005], scoliosis [χ2(3) = 60.445, p < .0005], and calcaneus valgus [χ2(3) = 11.410, p < .0005].
For kyphosis, the Hosmer-Lemershow test indicated a good model fit [x2(8) = 14.86, p = .062]. The model explained of the variance 70.0% (Nagelkerke R2) and correctly classified 62.4% of cases with sensitivity of 65.8%, specificity of 58.8%, positive predictive value of 63.20% and negative predictive value of 61.5%. All three predictor—age, gender, and BMI—were statistically significant. Boys had 5.19 times lower odds of exhibiting kyphosis compared with girls (B = −.655, Wald = 24.76, p = .000; Exp(B) = .519, 95% CI [.401,.672]. Increasing age [B = −.125, Wald = 6.83, p = .009; Exp(B) = 1.134, 95% CI [1.032, 1.245]] and BMI [B = −.085, Wald = 26.71, p = .000. Exp(B) = .919, 95% CI [.889, .949]] were also associated with an increased likelihood of kyphosis.
For hyperlordosis, the Hosmer-Lemershow test also suggest a good fit [x2(8) = 10.67, p = .221]. The model explained 60.0% of the variance (Nagelkerke R2) and correctly classified 69.7% of cases, with sensitivity of 5.7%, specificity of 99.7%, positive predictive value of 98.47% and negative predictive value of 29.17%. Age and BMI were statistically significant predictors. Increasing age [B = .304, Wald = 32.44, p = .000; Exp(B) = 1.355, 95% CI [1.221, 1.504]] and BMI [B = −.057, Wald = 12.23, p = .000; Exp(B) = .944, 95% CI [.915,.975]] were associated with a higher likelihood of hyperlordosis.
For scoliosis, the Hosmer-Lemershow test indicated adequate model fit [x2(8) = 8.634, p = .374]. The model explained 87.3% of the variance (Nagelkerke R2) and correctly classified 73.9% of cases, with sensitivity of 8%, specificity of 99.3%, positive predictive value of 15.7% and negative predictive value of 26.05%. BMI (B = −.108, Wald = 26.60, p = .000. Exp(B) = 1.114, 95% CI [1.069, 1.161] and gender [B = .802, Wald = 17.88, p = .000; Exp(B) = 2.230, 95% CI [1.656, 3.004]] emerged as significant predictors. Boys had 2.23 times higher odds of scoliosis compared with girls, and higher BMI was associated with greater likelihood of scoliosis.
For calcaneus valgus the Hosmer-Lemershow test also showed good model fit [x2(8) = 11.148, p = .193]. The model explained 20% of the variance (Nagelkerke R2) and correctly classified 64.4% of cases. Sensitivity was 0%, while specificity was 100%. BMI [B = −.057, Wald = 9.661, p = .002. Exp(B) = 1.056, 95% CI [1.021, 1.089]], indicating that children with higher MBI demonstrated 1.05 times greater of presenting calcaneus valgus.
Discussion
This study aimed to estimate the prevalence of spinal and foot postural deficiencies among preadolescents and to explore correlations between posture, body composition, coordination, and foot conditions in relation to spinal deviations.
The most prevalent spinal deficiency identified was forward head posture, observed across the entire cohort. Considering that the head constitutes approximately 8% of total body weight, proper alignment is critical for musculoskeletal health (29). Misalignment may lead to dysfunction in the head, neck, trunk, and upper limbs (29). Reported prevalence rates of forward head posture vary by age: Szczygieł et al. found that only 7.6% maintained correct head posture (29, 30), whereas Ruivo et al. documented a prevalence of 68% among adolescents aged 15–17 years (31). Such discrepancies likely reflect age-related differences in postural adaptation.
With respect to kyphotic posture, an overall prevalence of 51.9% was recorded, with boys (52.3%) more affected than girls (40.4%). This finding is consistent with previous studies reporting a higher prevalence of kyphotic posture among boys (32–35). However, other research has identified no significant gender differences (36), or has reported a higher prevalence of other spinal deformities among girls (37, 38).
Ankle valgus emerged as the most common lower limb postural deficiency, followed by flatfoot, with both conditions affecting boys and girls at similar rates. If uncorrected, ankle valgus may progress to secondary deformities such as hallux valgus, metatarsalgia, and osteoarthritis (39, 40), and it is often associated with flatfoot during growth phases (40, 41). Findings regarding flatfoot prevalence remain inconsistent: Xu et al. reported higher incidence in boys (42), whereas Sadeghi-Demneh observed no gender difference but documented a decline with age (43). Given these inconsistencies, the results suggest that the particularities related to sex between boys and girls during the early school years exert minimal influence on the development of postural and foot abnormalities. Supporting this, no major anthropometric or strength differences exist between prepubescent boys and girls (44).
A significant but weak correlation was observed between BMI, BFI, and the presence of kyphosis and hyperlordosis. This finding is consistent with prior research by Miranda et al. (45) and others, which identified associations between increased BMI and both thoracic kyphosis and lumbar lordosis (46–51). However, the correlations in the present study were weaker, possibly due to the younger age of participants compared to earlier studies that examined older adolescents.
Another important observation was the association between ankle valgus, flatfoot, and scoliosis. Prior research has also demonstrated relationship between calcaneal valgus angle and scoliosis (52), as well as between flatfoot and spinal deformities (53). These association are thought to result from kinetic chain disruptions caused by excessive foot pronation, which alters musculoskeletal alignment (54). Children with flatfoot frequently exhibit altered center of gravity shifts, potentially contributing to spinal asymmetries (55).
Flatfoot is further recognised as negatively affecting daily activities and quality of life in children (56). Sung et al. affecting that individuals with symptomatic flatfoot develop compensatory movement patterns that impair postural stability (57). Although balance was not directly assessed in the present study, a significant link between flatfoot and body coordination was observed. Similar findings were reported by Takabayashi et al., who noted impaired coordination during running in children with flatfoot (58).
Limitations
This study has several limitations. First, postural deviations were assessed through visual inspection using a plumb line. Although this method is widely applied in clinical and field settings owing to its simplicity and low cost, it is inherently subjective and may be influenced by the examiner's experience and judgment, thereby affecting the reliability and accuracy of the findings. The absence of precise quantitative measurements also limits the detection of subtle deviations and reduces comparability with studies of greater accuracy. Moreover, the correlation analysis was based on the number of children presenting deficiencies rather than the degree of postural deviation relative to BMI, which may have influenced the strength of the associations. To address this limitation, future research should consider incorporating more objective assessment tools, such as computerized postural analysis systems that capture images and allow for angular measurements of postural deviations, thereby ensuring greater reliability and reproducibility.
Nonetheless, visual observation remains a rapid, cost-effective, and non-invasive method suitable for large-scale screening. A further limitation is the exclusion of potentially relevant factors such as genetics, hormonal status, and nutrition, which may also influence posture. Finally, children's emotional discomfort during assessment—being outside their familiar environment and during assessment—being outside their familiar environment and evaluated in partial undress—may have affected posture evaluation.
Conclusions
This study identified forward head posture as the most prevalent postural deficiency among preadolescents, followed by kyphotic posture and ankle valgus. Body composition was significantly associated with the presence of kyphosis, hyperlordosis, ankle valgus, and flatfoot, with flatfoot also linked to scoliosis and impaired general coordination. These findings underscore the importance of early detection of postural deficiencies and the implementation of targeted preventive and corrective programmes for school-aged children. Such initiatives are essential to reduce the risk of subsequent musculoskeletal disorders in the adult population and to promote healthier physical development trajectories into adulthood.
Data availability statement
The raw/processed data required to reproduce the above findings cannot be shared at this time as the data also forms part of an ongoing study. Requests to access the datasets should be directed toZGNpb2JhbnVAdW9yYWRlYS5ybw==.
Ethics statement
The studies involving humans were approved by Help&Care Association Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
SV: Conceptualization, Project administration, Resources, Supervision, Validation, Writing – original draft. DC: Investigation, Methodology, Software, Writing – original draft. JF: Data curation, Investigation, Project administration, Writing – original draft. NM: Data curation, Investigation, Writing – original draft. DC: Data curation, Formal analysis, Software, Visualization, Writing – original draft. MS-A: Formal analysis, Investigation, Writing – original draft. FB: Validation, Visualization, Writing – review & editing. DI: Resources, Supervision, Validation, Visualization, Writing – review & editing. AI: Conceptualization, Investigation, Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The publishing costs were supported by the University of Oradea.
Acknowledgments
The authors thank all the subjects who were involved in the research and their parents.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issue please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
IRB, institutional review board; GDPR, general data protection regulation; BMI, body mass index; BFI, body fat index.
References
1. Rhodes RE, Guerrero MD, Vanderloo LM, Barbeau K, Birken CS, Chaput JP, et al. Development of a consensus statement on the role of the family in the physical activity, sedentary, and sleep behaviours of children and youth. Int J Behav Nutr Phys Act. (2020) 17:74. doi: 10.1186/s12966-020-00973-0
2. Latalski M, Bylina J, Fatyga M, Repko M, Filipovic M, Jarosz MJ, et al. Risk factors of postural defects in children at school age. Ann Agric Environ Med. (2013) 20(3):583–7.24069870
3. Dop D, Pădureanu V, Pădureanu R, Niculescu S-A, Drăgoescu AN, Moroșanu A, et al. Risk factors involved in postural disorders in children and adolescents. Life. (2024) 14(11):1463. doi: 10.3390/Life14111463
4. Serbescu C, Ianc D, Straciuc O, Carp G, Courteix D. Epidemiological study of scoliosis and postural faults of Romanian schoolchildren. In: Jurimae T, Armstrong N, Jurimae J, editors. Children and Exercise XXIV: The Proceedings of the 24th Pediatric Work Physiology Meeting. London: Routledge (2008). p. 141–4. doi: 10.4324/9780203890851
5. Puszczałowska-Lizis E, Szwed K, Mikuláková W, Dul M. Prevalence of postural abnormalities among primary school children in podkarpackie voivodeship. Fizjoterapia Polska. (2025) 25(2):68–77. doi: 10.5604/01.3001.0017.7847
6. Rusnák R, Kolarová M, Aštaryová I, Kutiš P. Screening and early identification of spinal deformities and posture in 311 children: results from 16 districts in Slovakia. Rehabil Res Pract. (2019) 2019:4758386. doi: 10.1155/2019/4758386
7. Wyszyńska J, Podgórska-Bednarz J, Drzał-Grabiec J, Rachwa M, Baran J, Czenczek-Lewandowska E, et al. Analysis of relationship between the body mass composition and physical activity with body posture in children. BioMed Res Int. (2016) 2016:1851670. doi: 10.1155/2016/1851670
8. Wilczyński J, Cieślik M, Maszczyk A, Zwierzchowska A. The importance of posture and body composition for the stability and selected motor abilities of professional handball players. J Hum Kinet. (2022) 82:264–73. doi: 10.2478/hukin-2022-0025
9. Yam TTT, Fong SSM, Tsang WWN. Foot posture index and body composition measures in children with and without developmental coordination disorder. PLoS One. (2022) 17(3):e0265280. doi: 10.1371/journal.pone.0265280
10. Jorgić BM, Đorđević SN, Hadžović MM, Milenković S, Stojiljković NĐ, Olanescu M, et al. The influence of body composition on sagittal plane posture among elementary school-aged children. Children (Basel). (2023) 11(1):36. doi: 10.3390/children11010036
11. Ludwig O. Interrelationship between postural balance and body posture in children and adolescents. J Phys Ther Sci. (2017) 29(7):1154–8. doi: 10.1589/jpts.29.1154
12. Ludwig O, Kelm J, Hammes A, Schmitt E, Fröhlich M. Neuromuscular performance of balance and posture control in childhood and adolescence. Heliyon. (2020) 6(7):e04541. doi: 10.1016/j.heliyon.2020.e04541
13. Wilczyński J, Paprocki M. Correlations between foot defects and balance reactions among young school-children. Med Stud. (2020) 36(4):265–72. doi: 10.5114/ms.2020.102320
14. Wilczyński J, Bieniek K, Margiel K, Sobolewski PK, Wilczyński I, Zieliński R. Correlations between variables of posture and postural stability in children. Med Stud. (2022) 38(1):6–13. doi: 10.5114/ms.2022.115142
15. Azevedo N, Ribeiro JC, Machado L. Balance and posture in children and adolescents: a cross-sectional study. Sensors. (2022) 22:4973. doi: 10.3390/s22134973
16. Takakusaki K. Functional neuroanatomy for posture and gait control. J Mov Disord. (2017) 10(1):1–17. doi: 10.14802/jmd.16062
17. Virmani T, Bazanova OM, Larson-Prior LJ. Editorial: neuroscience of posture and gait control: mechanisms, influencing factors and cognitive-motor retraining. Front Hum Neurosci. (2023) 17:1197022. doi: 10.3389/fnhum.2023.1197022
18. Jafarnezhadgero A, Mousavi SH, Madadi-Shad M, Hijmans JM. Quantifying lower limb inter-joint coordination and coordination variability after four-month wearing arch support foot orthoses in children with flexible flat feet. Hum Mov Sci. (2020) 70:102593. doi: 10.1016/j.humov.2020.102593. Erratum in: Hum Mov Sci. (2020) 71:102613. doi: 10.1016/j.humov.2020.10261332217211
19. Constantinescu M, Onu I, Trofin D, Talaghir LG, Coja DM, Iordan DA, et al. Scoliotic postural alignment in prepubertal children: somatoscopic analysis of anatomical landmarks and development of a working model to limit spinal changes. Balneo PRM Res J. (2024) 15(1):655. doi: 10.12680/balneo.2024.655
20. Jackson AS, Pollock ML. Practical assessment of body composition. Phys Sportsmed. (1985) 13(5):76–90. doi: 10.1080/00913847.1985.11708790
21. Kendall EP, McCreary EK, Provance PG, Rodgers M, Romani WA. Muscles Testing & Function with Posture and Pain. 5th ed. Baltimore, MD: Lippincott Williams & Wilkins (2005).
22. Hresko MT, Talwalkar VR, Schwend RM. Position Statement - Screening for the Early Detection for Idiopathic Scoliosis in Adolescents. Milwaukee, WI: Scoliosis Research Society. AAOS, SRS, POSNA, and AAP (2015). Available online at: www.aaos.org
23. Rosário JL. A review of the utilization of baropodometry in postural assessment. J Bodyw Mov Ther. (2014) 18(2):215–9. doi: 10.1016/j.jbmt.2013.05.016
24. Zammit GV, Menz HB, Munteanu SE. Reliability of the TekScan MatScan®system for the measurement of plantar forces and pressures during barefoot level walking in healthy adults. J Foot Ankle Res. (2010) 3(1):11. doi: 10.1186/1757-1146-3-11
25. Zhao Y, Zhou J, Qiu F, Liao X, Jiang J, Chen H, et al. A deep learning method for foot-type classification using plantar pressure images. Front Bioeng Biotechnol. (2023) 11:1239246. doi: 10.3389/fbioe.2023.1239246
26. Panaet A, Zwierzchowska A, Peyré-Tartaruga L, Alexe D, Rosołek B, Alexe C. Distribution of plantar pressures under static conditions, in various areas of the pediatric flatfoot in sensitive period of development – pilot study. Balneo PRM Res J. (2023) 14(4):607. doi: 10.12680/balneo.2023.607
27. Paolucci T, Pezzi L, Mannocci A, La Torre G, Bellomo RG, Saggini R. Flat foot and postural harmony in 6-year-old caucasians: what is their relationship? Ann Rehabil Med. (2020) 44(4):320–6. doi: 10.5535/arm.19091
28. Szabo DA, Neagu N, Ardelean M, Sopa IS. Psychomotor evaluation of athlete and non-athlete children. Phys Educ Sport Kinetotherapy J. (2020) 59(1):56–69. doi: 10.35189/dpeskj.2020.59.1.6
29. Szczygieł E, Fudacz N, Golec J, Golec E. The impact of the position of the head on the functioning of the human body: a systematic review. Int J Occup Med Environ Health. (2020) 33(5):559–68. doi: 10.13075/ijomeh.1896.01585
30. Szczygieł E, Waśniowski D, Chmiel J, Golec J. Is the forward head posture a health problem affecting children and adolescents? J Kinesiol Exerc Sci. (2022) 32(98):37–44. doi: 10.5604/01.3001.0015.8788
31. Ruivo RM, Pezarat-Correia P, Carita AI. Cervical and shoulder assessment of adolescent between 15 and 17 years old and association with upper quadrant pain. Braz J Phys Ther. (2014) 18(4):364–71. doi: 10.1590/bjpt-rbf.2014.0027
32. Grabara M, Bieniec A, Nawrocka A. Spinal curvatures of children and adolescents – a cross-sectional study. Biomed Hum Kinet. (2017) 9(1):69–74. doi: 10.1515/bhk-2017-0011
33. Drzał-Grabiec J, Snela S, Truszczyńska A. The development of anterior-posterior spinal curvature in children aged 7–12 years. Biomed Hum Kinet. (2016) 8(1):72–82. doi: 10.1515/BHK-2016-0011
34. Szczepanowska-Wołowiec B, Drzał Grabiec J, Sztandera P, Dudek J, Kotela I. Bad posture in the sagittal plane of children aged 10–12 from the świętokrzyskie voivodeship. Med Stud. (2012) 27:31–5.
35. Gouveia JP, Forte P, Coelho E. Study of postural misalignments between sex, school cycle and physical activity. J Hum Sport Exerc. (2022) 17(2):424–34. doi: 10.14198/jhse.2022.172.17
36. Minghelli B. School screening: the importance of early detection of scoliotic postures in adolescents from silves schools, algarve. Revista Portuguesa de Saúde Pública. (2008) 26(2):61–8.
37. Braz H, Borges M. The relevance of postural assessment in schools. Coleção Pesquisa em Educação Física. (2007) 6(2):25–32.
38. Kussuki M, João S, Cunha A. Postural characterization of the spine of obese children aged 7 to 10 years. Fisioterapia em Movimenot. (2017) 20(1):77–84.
39. Smith SD, Millar EA. Arthrorisis by means of a subtalar polyethylene peg implant for correction of hindfoot pronation in children. Clin Orthop Relat Res. (1983) 181:15–23. doi: 10.1097/00003086-198312000-00004
40. Faldini C, Nanni M, Traina F, Fabbri D, Borghi R, Giannini S. Surgical treatment of hallux valgus associated with flexible flatfoot during growing age. Int Orthop. (2016) 40(4):737–43. doi: 10.1007/s00264-015-3019-9
41. Panaet A, Alexe C, Stangaciu O, Hazar F, Rata G, Alexe D, et al. The effects of pediatric flat foot on the frontal alignment of proximal segment. Balneo PRM Res J. (2022) 13(2):499. doi: 10.12680/balneo.(2022).499
42. Xu L, Gu H, Zhang Y, Sun T, Yu J. Risk factors of flatfoot in children: a systematic review and meta-analysis. Int J Environ Res Public Health. (2022) 19(14):8247. doi: 10.3390/ijerph19148247
43. Sadeghi-Demneh E, Jafarian F, Melvin JM, Azadinia F, Shamsi F, Jafarpishe M. Flatfoot in school-age children: prevalence and associated factors. Foot Ankle Spec. (2015) 8(3):186–93. doi: 10.1177/1938640015578520
45. Miranda APOC, Penha PJ, Pereira LG, Pessoa WC, João SMA. Influence of sex and body mass Index on the thoracic kyphosis and lumbar lordosis. J Manipulative Physiol Ther. (2022) 45(7):508–14. doi: 10.1016/j.jmpt.2022.12.001
46. Golalizadeh D, Toopchizadeh V, Farshbaf-khalili A, Salekzamani Y, Dolatkhah N, Pirani A. Faulty posture: prevalence and its relationship with body mass Index and physical activity among female adolescents. Biomed Hum Kinet. (2020) 12:25–33. doi: 10.2478/bhk-2020-0004
47. Valdovino AG, Bastrom TP, Reighard FG, Cross M, Bartley CE, Shah SA, et al. Obesity is associated with increased thoracic kyphosis in adolescent idiopathic scoliosis patients and nonscoliotic adolescents. Spine Deform. (2019) 7(6):865–9. doi: 10.1016/j.jspd.2019.03.010
48. Gouveia JP, Coelho E, Forte P. Postural misalignments in school students: comparisons between gender, school cycles and body composition. Research Square [Preprint] (Version 1). (2024). doi: 10.21203/rs.3.rs-4253334/v1
49. Wati KAP, Adhitya IPGS, Kinandana GP. Relationship between body mass indexand lumbar lordosis curve. Kinesiol Physiother Comprehen. (2024) 3(1):1–5. doi: 10.62004/kpc.v3i1.33
50. Jankowicz-Szymańska A, Bibro M, Wodka K, Smola E. Does excessive body weight change the shape of the spine in children? Child Obes. (2019) 15(5):346–52. doi: 10.1089/chi.2018.0361
51. Grabara M, Witkowska A. Sagittal spinal curvatures of young adults in the context of their self-reported physical activity and somatic parameters. Sci Rep. (2024) 14:12221. doi: 10.1038/s41598-024-62929-9
52. Park J, Lee SG, Bae J, Lee JC. The correlation between calcaneal valgus angle and asymmetrical thoracic-lumbar rotation angles in patients with adolescent scoliosis. J Phys Ther Sci. (2015) 27(12):3895–9. doi: 10.1589/jpts.27.3895
53. Romanova E, Kolokoltsev M, Vorozheikin A, Baatar B, Khusman O, Purevdorj D, et al. Comprehensive program for flat foot and posture disorders prevention by means of physical education in 6-year-old children. J Phys Educ Sport. (2022) 22(11):2655–62.
54. Dodelin D, Tourny C, L’Hermette M. The biomechanical effects of pronated foot function on gait. An experimental study. Scand J Med Sci Sports. (2020) 30(11):2167–77. doi: 10.1111/sms.13785
55. Kim JA, Lim OB, Yi CH. Difference in static and dynamic stability between flexible flatfeet and neutral feet. Gait Posture. (2015) 41(2):546–50. doi: 10.1016/j.gaitpost.2014.12.012
56. Kothari A, Stebbins J, Zavatsky AB, Theologis T. Health-related quality of life in children with flexible flatfeet: a cross-sectional study. J Child Orthop. (2014) 8(6):489–96. doi: 10.1007/s11832-014-0621-0
57. Sung PS, Zipple JT, Andraka JM, Danial P. The kinetic and kinematic stability measures in healthy adult subjects with and without flat foot. Foot (Edinb). (2017) 30:21–6. doi: 10.1016/j.foot.2017.01.010
Keywords: posture, spine, valgus ankle, baropodometry, preadolescents
Citation: Vlad S, Ciobanu DI, Fulop J, Matei N, Cristea DI, Szabo-Alexi M, Blaga FN, Ianc D and Ilies AB (2025) Postural deficiencies prevalence and correlation with foot conditions, body composition, and coordination, in Romanian preadolescents children: descriptive observational study. Front. Pediatr. 13:1621792. doi: 10.3389/fped.2025.1621792
Received: 1 May 2025; Accepted: 22 September 2025;
Published: 14 October 2025.
Edited by:
Rafael Lomas-Vega, University of Jaén, SpainReviewed by:
Cihad Dundar, Ondokuz Mayıs University, TürkiyeAgnieszka Wasiluk, Józef Piłsudski University of Physical Education in Warsaw, Poland
Copyright: © 2025 Vlad, Ciobanu, Fulop, Matei, Cristea, Szabo-Alexi, Blaga, Ianc and Ilies. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Doriana I. Ciobanu, ZGNpb2JhbnVAdW9yYWRlYS5ybw==; Dorina Ianc, ZGlhbmNAdW9yYWRlYS5ybw==
 Silviu Vlad1
Silviu Vlad1 Doriana I. Ciobanu
Doriana I. Ciobanu Dorina Ianc
Dorina Ianc