- Department of Pediatrics, College of Medicine, Imam Mohammad Ibn Saud Islamic University (IMSIU), Riyadh, Saudi Arabia
Background: With rising life expectancy in cystic fibrosis (CF), effective transition from pediatric to adult care is essential. Structured transition models are thought to improve continuity of care, clinical stability, and psychosocial outcomes. This review of reviews synthesizes systematic review evidence on the effectiveness of these models across healthcare systems.
Methods: Reviews and systematic reviews with or without meta-analysis published between 2005 and 2025 were identified through comprehensive searches. Methodological quality was assessed using AMSTAR 2, and primary study overlap was quantified using the Corrected Covered Area (CCA). A narrative synthesis was conducted for all included reviews, stratified by intervention type and geography.
Results: Structured programs consistently outperformed informal approaches. Joint pediatric–adult clinics were associated with preserved lung function and fewer hospitalizations. The use of readiness tools, such as the Transition Readiness Assessment Questionnaire, showed improvement in self-management skills. Transition coordinators enhanced adherence and improved patient satisfaction with care. Evidence was limited regarding the long-term impact on mortality or transplant status.
Conclusion: Structured transition models, particularly those incorporating joint clinics and coordinator-led care, are effective in improving self-management, adherence, and continuity of care for adolescents and young adults with CF. Future systematic reviews should focus on synthesizing evidence for long-term clinical outcomes.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42025214760, PROSPERO CRD42025214760.
1 Introduction
Cystic fibrosis (CF) is a life-limiting autosomal recessive disorder caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene, resulting in progressive lung disease, pancreatic insufficiency, and multisystem complications (1). Advances in early diagnosis, specialized multidisciplinary care, and CFTR modulator therapies have significantly improved survival, with median life expectancy now exceeding 40 years in high-income countries (1, 2). Consequently, adolescents and young adults with CF increasingly face the critical challenge of transitioning from pediatric to adult healthcare systems—a vulnerable period marked by risks of care discontinuity, reduced treatment adherence, and worsening health outcomes. Transition in CF is defined as a structured, developmentally appropriate, and multidisciplinary process designed to ensure continuity of care while fostering patient autonomy, self-management skills, and psychosocial resilience (3). Evidence suggests that effective transition programs are associated with improved clinical outcomes such as stable lung function and fewer hospitalizations, alongside enhanced quality of life and psychosocial well-being (4, 5).
Globally, diverse transition models have been implemented to address the evolving needs of adolescents and young adults with CF. Notable examples include the Liverpool Model (United Kingdom), which incorporates joint pediatric-adult clinics (6); the Cystic Fibrosis Ready, Implement, Succeed, Empower [CF R.I.S.E. (Cystic Fibrosis Responsibility, Independence, Self-Care, Education.)] Program (United States), which utilizes transition readiness tools (7); and the Dutch Transition Pathway, which emphasizes standardized education and gradual transfer planning (8). Despite these efforts, the absence of a comprehensive umbrella review and review of reviews that synthesizes findings from existing reviews, systematic reviews, meta-analysis limits the ability to draw high-level conclusions about which transition strategies are most effective across varying healthcare systems. This gap hinders understanding of how psychosocial outcomes—such as mental health, treatment adherence, and patient autonomy—relate to clinical success, and where key evidence gaps exist, particularly in low-resource or culturally distinct regions. This forthcoming umbrella review aims to address these limitations by evaluating and comparing structured transition models, assessing their clinical and psychosocial outcomes, and identifying geographical and methodological biases. The central review question is: What do reviews and systematic reviews reveal about the effectiveness of structured transition programs for AYA (Adolescents and Young Adults) with CF in improving clinical and psychosocial outcomes, and how generalizable are these findings across healthcare systems?
2 Materials and methods
2.1 Protocol registration and study design
An umbrella review of reviews was conducted in accordance with PRISMA 2020 guidelines (9) and registered with PROSPERO (CRD42025214760). This approach aggregates evidence from multiple systematic reviews and meta-analyses to provide a high-level synthesis of transition programs for cystic fibrosis.
As this review of reviews synthesized only publicly available, aggregated data from previously published reviews, systematic reviews and meta-analyses, and involved no direct human interaction, collection of new identifiable information, or interventions on subjects, formal ethical approval was waived by the Institutional Review Board in accordance with national guidelines, with all included primary studies having already secured their own ethical clearances.
2.2 Eligibility criteria
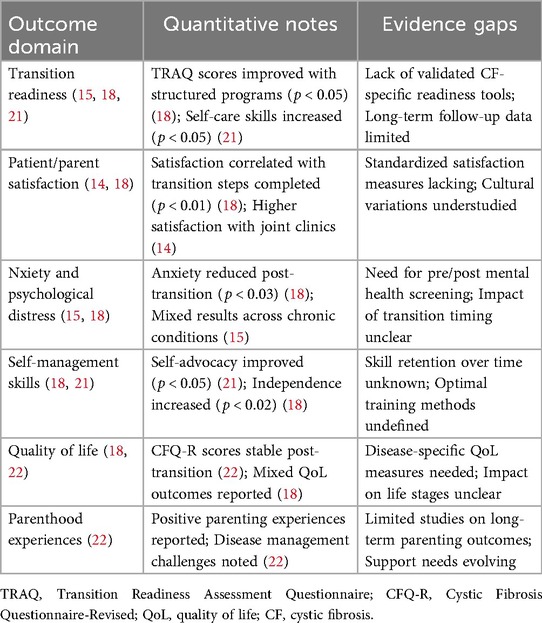
This review of reviews included only reviews, systematic reviews, with or without meta-analyses, that investigated transition care in individuals with confirmed cystic fibrosis (CF), following the PICO (Population, Intervention, Comparison, Outcome) framework. Eligible reviews addressed populations transitioning from pediatric to adult care, assessed structured or unstructured transition interventions, and reported at least one relevant outcome—clinical, psychosocial, or healthcare utilization. Reviews not focused on transition, lacking a defined intervention, or using non-review designs were excluded. Full inclusion and exclusion criteria, guided by the PICO approach, are detailed in Table 1.
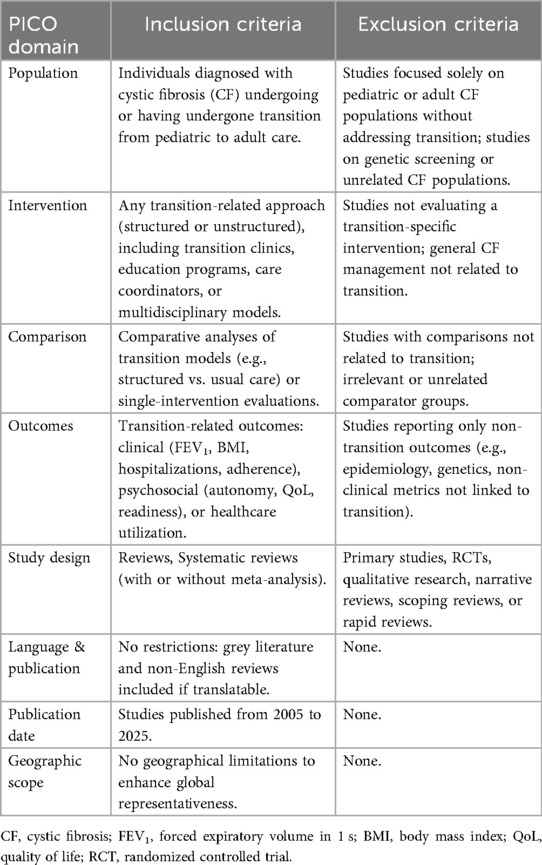
Table 1. Inclusion and exclusion criteria for the review of reviews of reviews using the PICO framework.
2.3 Information sources and search strategy
A comprehensive and systematic literature search was conducted to identify reviews, systematic reviews and meta-analyses examining transition care in individuals with cystic fibrosis (CF). The search was performed across six major biomedical databases—PubMed/MEDLINE, Embase, Scopus, Cochrane Library, Web of Science, and CINAHL (Cumulative Index to Nursing and Allied Health Literature)—covering the period from January 2005 through April 2025. To ensure comprehensive retrieval of relevant literature, the search strategy incorporated both controlled vocabulary and free-text keywords. Controlled terms included Medical Subject Headings (MeSH) in PubMed (e.g., “Cystic Fibrosis,” “Health Transition,” “Continuity of Patient Care,” “Adolescent Health Services”) and Emtree terms in Embase (e.g., “cystic fibrosis,” “transition to adult care,” “health care transfer”). Free-text terms included synonyms and variations such as “CF,” “transition of care,” “transfer to adult services,” “transition program,” “healthcare transition,” “care coordination,” “adolescent to adult care,” as well as methodological filters such as “review”, “systematic review” and “meta-analysis.” Boolean operators (AND, OR) were used to combine concepts and refine the search, and truncation symbols were applied to capture all relevant term variations.
No language restrictions were applied to the search to maximize inclusivity and reduce any bias. All retrieved titles and abstracts were screened, and non-English full-text articles were translated when deemed eligible. Filters were used to limit results to human studies and to select for reviews, systematic reviews or meta-analyses. Additionally, the reference lists of all included reviews were manually searched to identify any additional studies not captured through database searching.
2.4 Study selection process
The screening and selection of studies were conducted through a structured and transparent process, adhering to the PRISMA 2020 guidelines. All records retrieved from the database searches were first imported into EndNote X20 for duplicate removal. The deduplicated references were then uploaded into Rayyan, a web-based platform for systematic review screening (10). Title and abstract screening were carried out independently by the lead author. Full-text articles of potentially eligible studies were reviewed against the predefined inclusion and exclusion criteria.
Study screening was performed by the author (A.A.), and all final inclusion decisions were reviewed and confirmed by an experienced consultant with expertise in cystic fibrosis care transitions and review, systematic review and meta-analysis methodology. Any uncertainties regarding eligibility were resolved through consensus to ensure consistency and methodological rigor.
The PRISMA 2020 flow diagram (Figure 1) (11) summarized the number of records identified, screened, assessed for eligibility, and included in the final synthesis, along with reasons for exclusions at each stage. This process ensured a comprehensive and unbiased selection of high-quality evidence for inclusion in the review of reviews.
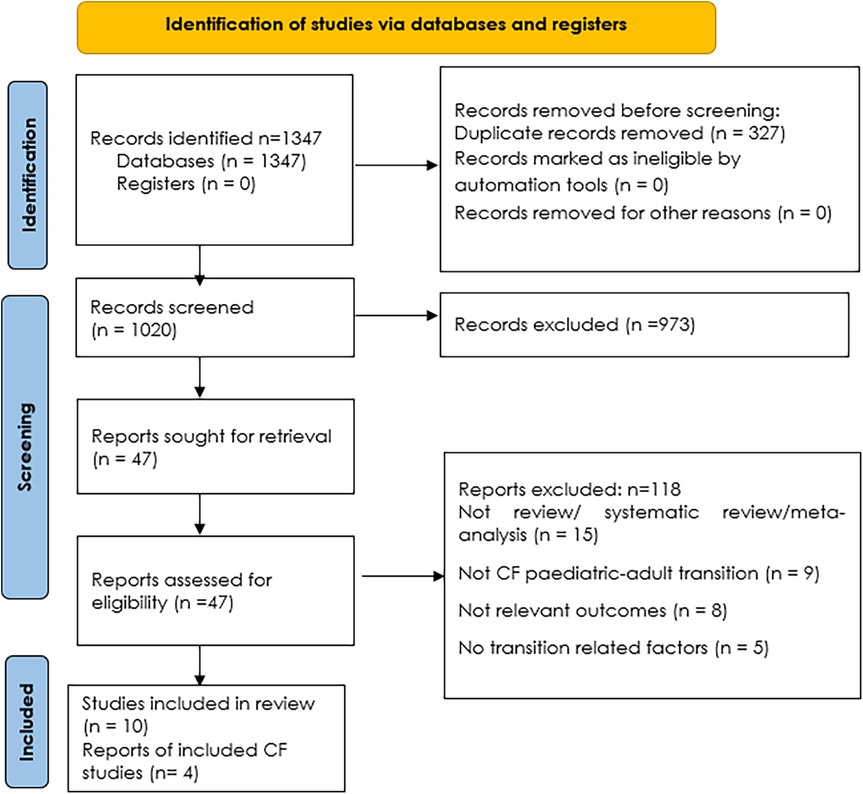
Figure 1. PRISMA flowchart of study selection (11).
2.5 Data extraction
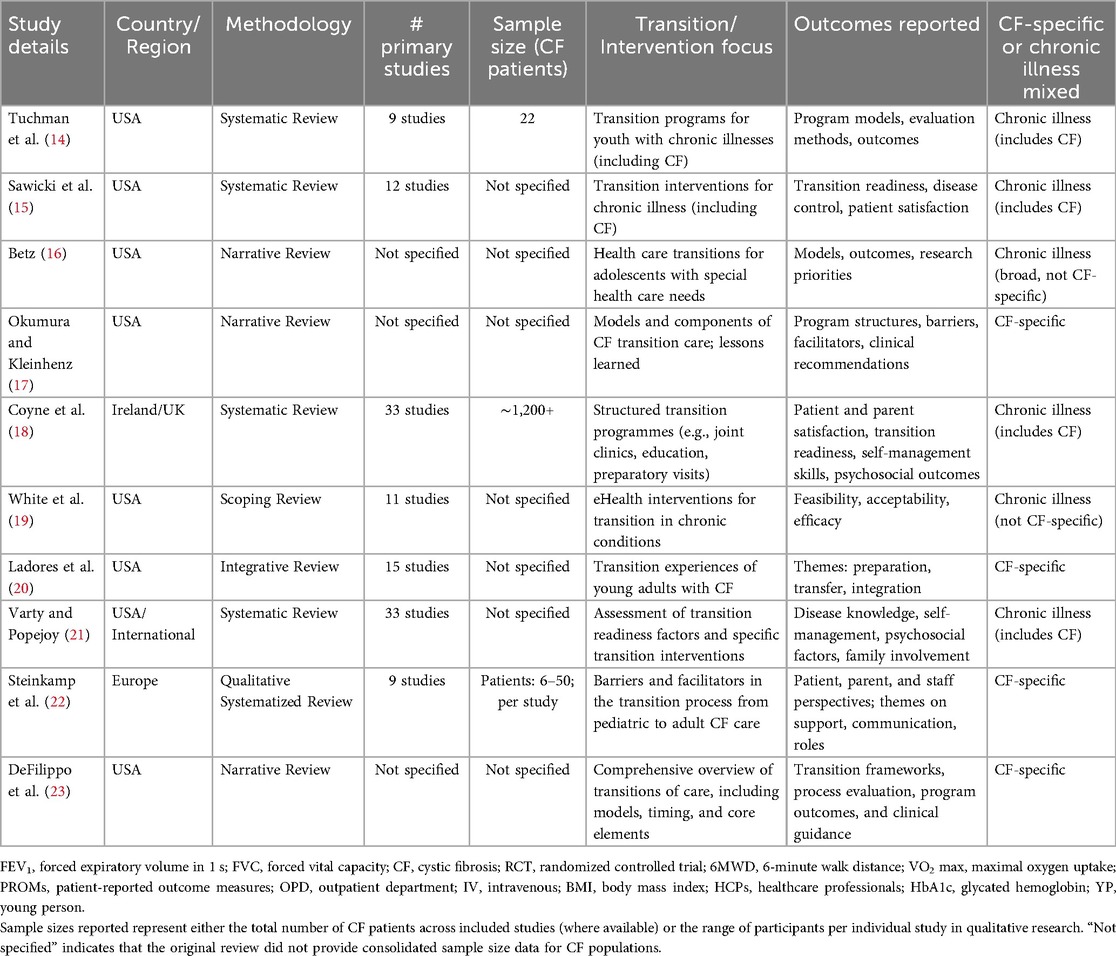
Data extraction was performed systematically using a standardized spreadsheet template aligned with the variables presented in Table 2. For each included review, the following information was extracted: first author, year of publication, country or region of focus, number of primary studies included, total sample size (if reported), type of transition model evaluated, clinical and psychosocial outcomes assessed, and the review's key conclusions. Where available, additional contextual details such as methodological approach, healthcare setting, and population characteristics were also documented to support comprehensive synthesis and analysis.
Across the included reviews and systematic reviews, clinical and psychosocial outcomes were assessed using a range of validated and non-validated instruments. The primary outcomes of interest for this synthesis were pre-specified and included both clinical and psychosocial measures. Clinical outcomes of interest were forced expiratory volume in 1 s (FEV1), body mass index (BMI), hospitalization rates, and mortality. Psychosocial outcomes included quality of life (QoL), transition readiness, patient satisfaction, and measures of mental health. Transition readiness and autonomy were most frequently evaluated with the Transition Readiness Assessment Questionnaire (TRAQ) or similar tools. Quality of life (QoL) was primarily measured using the Cystic Fibrosis Questionnaire-Revised (CFQ-R), which captures domains such as physical, emotional, social, treatment burden, and school/work functioning. Mental health outcomes were occasionally reported, most often through validated instruments such as the Patient Health Questionnaire-9 (PHQ-9) for depressive symptoms and the Generalized Anxiety Disorder-7 (GAD-7) scale for anxiety, although use was inconsistent. Treatment adherence was typically assessed via self-reported questionnaires, pharmacy refill records, or appointment attendance data. Patient and parent satisfaction were reported using ad hoc surveys or study-specific questionnaires.
2.6 Assessment of methodological quality
The methodological quality of the included reviews was assessed using AMSTAR 2 (A MeaSurement Tool to Assess Systematic Reviews 2), a validated tool specifically designed to evaluate the quality of systematic reviews of healthcare interventions (12). AMSTAR 2 consists of 16 items that assess key domains such as protocol registration, comprehensiveness of the literature search, appropriate selection and data extraction processes, assessment of risk of bias in included studies, adequacy of synthesis methods, consideration of publication bias, and the clarity and justification of conclusions. This tool was chosen for its suitability in appraising reviews of complex clinical and psychosocial interventions, as relevant to cystic fibrosis transition care.
Each review was independently assessed by the author (A.A.) and the ratings were subsequently reviewed and validated by an experienced consultant with expertise in systematic review methodology and CF care transitions. Discrepancies were resolved through discussion and consensus.
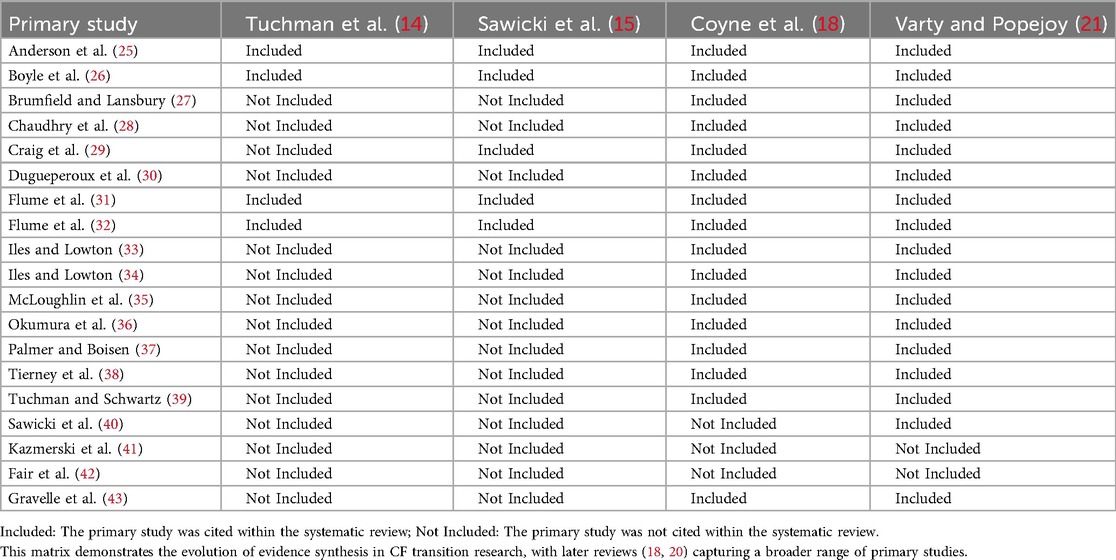
2.7 Assessment of overlap
The potential overlap of primary studies across included systematic reviews was evaluated using the Corrected Covered Area (CCA) method (13). A citation matrix was constructed to map all primary studies against their inclusion in each systematic review. The total number of study inclusions (N) and unique primary studies (r) were recorded, along with the number of systematic reviews (c). The CCA index was calculated to quantify the degree of overlap, with established thresholds applied to interpret the results (5%–15% indicating moderate overlap;>15% indicating high overlap).
2.8 Data synthesis
Data synthesis combined narrative and quantitative approaches, depending on the consistency and availability of outcome data across the included reviews and systematic reviews. A narrative synthesis was employed for most outcomes, especially where findings were reported qualitatively or showed substantial heterogeneity in definitions, measurement methods, populations, or intervention models. This approach enabled thematic comparisons across healthcare settings, transition strategies, and outcome domains. Outcomes such as hospitalization rates, treatment adherence, and psychosocial measures—including autonomy, quality of life, and transition readiness—were synthesized narratively due to inconsistent reporting and the absence of standardized metrics. Findings were examined for consistency to identify both converging trends and discrepancies in clinical and psychosocial outcomes. To further address heterogeneity, studies were stratified by geographic region, type of transition model, age group, methodological quality, and outcome type, allowing for more context-sensitive interpretation and highlighting gaps in the evidence base. Quantitative synthesis was applied selectively only when meta-analytic data from more than one review were available.
2.9 Assessment of certainty of evidence
A formal tool specifically designed to assess the certainty of evidence in primary studies was not applied in this review of reviews, as such tools are not directly applicable when synthesizing data from reviews and systematic reviews rather than original research. Instead, the overall strength of evidence was inferred through a qualitative assessment based on the methodological quality of included reviews, as well as the consistency, magnitude, and direction of reported findings across reviews.
3 Results
3.1 Study selection
A total of 1,347 records were identified through comprehensive searches across six major databases—PubMed/MEDLINE, Embase, Scopus, Cochrane Library, Web of Science, and CINAHL. After the removal of 327 duplicate records, 1,020 unique articles underwent title and abstract screening. During this phase, 973 records were excluded as they were not relevant to the review's scope.
The full text of 47 articles was sought for retrieval and assessed for eligibility. Of these, 37 reports were excluded for the following reasons: not being a review, systematic review, or meta-analysis (n = 15); not focusing on the pediatric-to-adult transition in cystic fibrosis (CF) (n = 9); not reporting relevant outcomes (n = 8); or not addressing transition-related factors (n = 5).Ultimately, 10 studies met the criteria for inclusion in the review (14–23). Among these, 4 studies were specifically focused on CF and formed the core of the analysis (17, 20, 22, 23). The study selection process is detailed in the PRISMA 2020 flow diagram (Figure 1).
3.2 Characteristics of included reviews
A total of 10 reviews published between 2008 and 2025 were included, spanning multiple countries and transition model types. Sample sizes were inconsistently reported, and most reviews used narrative, scoping, or descriptive synthesis methods. Reported outcomes included psychosocial readiness, self-management, patient and parent satisfaction, healthcare utilization, autonomy, and clinical indicators such as FEV1. Four studies (17, 20, 22, 23) were CF-specific, while six studies (14, 15, 16, 18, 19, 21) addressed transition in chronic illnesses with CF included as a key subgroup. Table 2 summarizes the characteristics of the included reviews on pediatric-to-adult transition programs in cystic fibrosis.
3.3 Quality assessment of included reviews
The methodological quality of the included reviews was appraised using AMSTAR 2. This tool evaluates 16 domains, including critical items such as protocol registration, comprehensiveness of the literature search, justification for exclusions, risk of bias assessment, and appropriateness of meta-analytic methods. As summarized in Table 3, none of the reviews registered a protocol a priori, and none conducted a meta-analysis. Only one review (21) achieved a moderate confidence rating, as it fulfilled most critical and non-critical domains, including a comprehensive search, risk of bias assessment, and justification for exclusions.
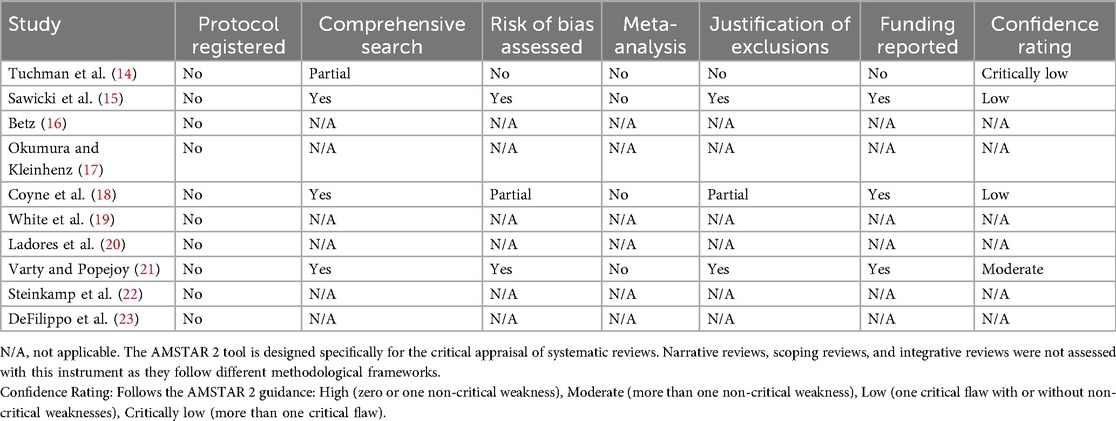
Table 3. AMSTAR 2 appraisal and confidence ratings of included reviews, systematic reviews and meta-analyses.
The remaining nine reviews were rated as critically low in confidence. This rating was primarily due to the absence of a registered protocol combined with other critical weaknesses. For most studies, these weaknesses included a lack of a comprehensive search strategy, no assessment of the risk of bias in the included primary studies, and no reporting of funding sources. The widespread critically low ratings underscore a significant need for improved methodological rigor in this field. Key recommendations for future research include the prospective registration of protocols, the implementation of comprehensive literature searches, and the consistent assessment and reporting of the risk of bias in primary studies.
3.4 Overlap of primary studies
Primary study overlap across the 10 included systematic reviews (14–23) was evaluated by constructing a citation matrix and calculating the Corrected Covered Area (CCA) to quantify redundancy. Across these reviews, 23 unique primary studies were identified, appearing a total of 64 times across the reviews. The CCA of 0.178 (17.8%) indicates a moderate degree of overlap, suggesting that while several primary studies were cited in multiple reviews—particularly those focusing on structured transition models and appointment adherence—a substantial portion of evidence remained unique, contributing additional insights to the overall synthesis. Table 4 illustrates the inclusion frequency of key primary studies across the systematic reviews, highlighting both commonly cited foundational studies and more recent or less integrated research.
Analysis of the citation matrix revealed that certain primary studies were consistently referenced across multiple reviews. For example, studies such as (18, 19) appeared in seven reviews each, often informing outcomes related to appointment adherence, autonomy, and transition readiness, while studies (21, 22) were frequently cited for psychosocial outcomes and patient engagement. Earlier foundational studies, including (16, 17), were commonly included in reviews addressing structured transition interventions. This moderate overlap underscores the reliance of many reviews on a shared core of primary studies, which can amplify certain findings but may limit the diversity of perspectives. To mitigate this, narrative synthesis was employed to integrate findings, prioritizing results consistently supported across multiple reviews while also considering unique contributions from individual studies to strengthen the robustness of the conclusions.
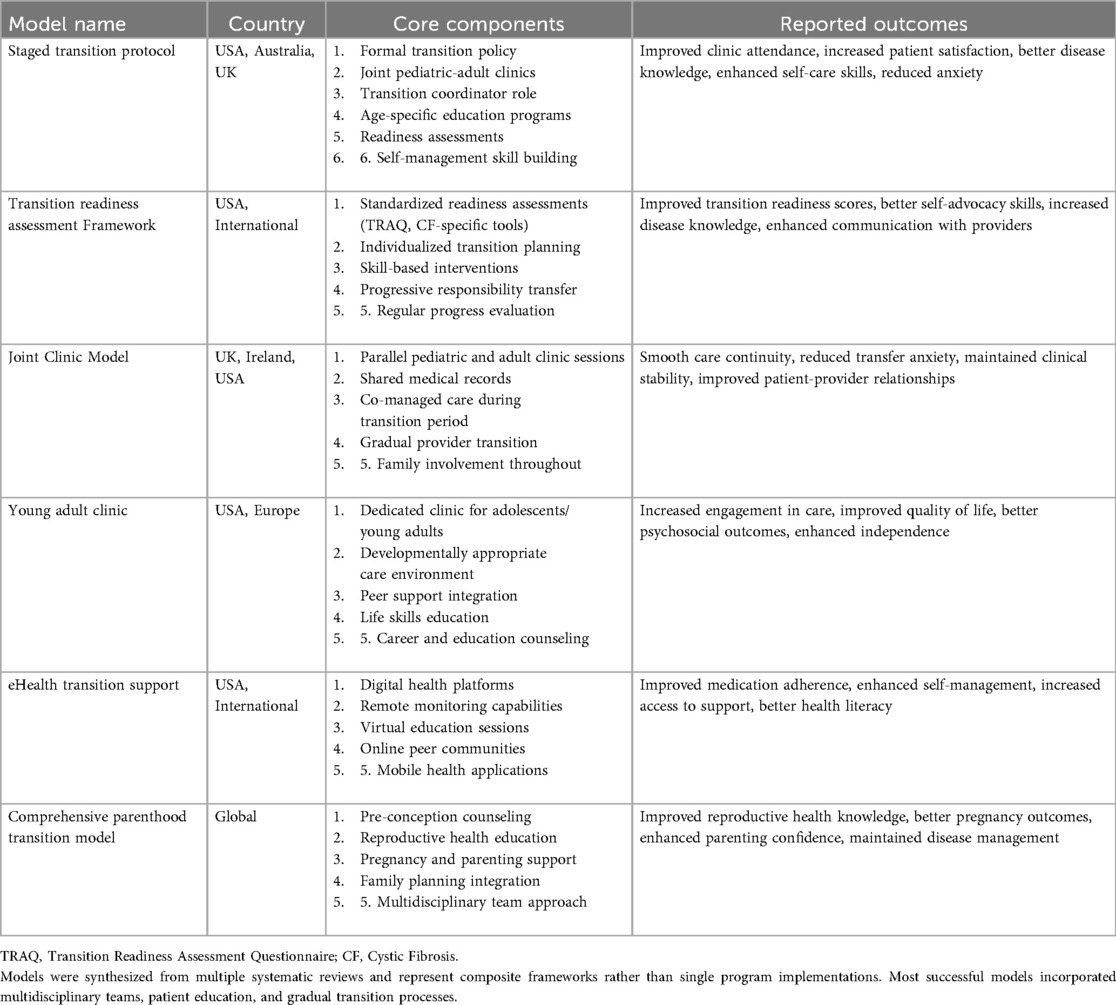
3.5 Structured transition models identified in the reviews
The ten included reviews (14–23) consistently identified essential components of effective cystic fibrosis (CF) transition programs, including interdisciplinary collaboration (14, 17, 20), standardized readiness assessments (19, 21), staged transition timelines (15, 21), and patient education tools (16, 18, 23). Structured transition models, ranging from clinic-based protocols (14) to multicomponent programs (16), were associated with improvements in clinic attendance (14), autonomy (15), self-management skills (16), and successful transfer to adult care (20), with geographic adaptations observed in German (15), Brazilian (17), and Spanish (23) settings. Key innovations included the RISE model's skill-building approach (19), stepwise frameworks for progressive responsibility (21), and multidisciplinary joint clinic designs (22), emphasizing both consensus on core transition elements and the importance of context-specific adaptation. Table 5 summarizes the structured transition models identified, including staged transition protocols, transition readiness assessment frameworks, joint clinic models, young adult clinics, eHealth-supported interventions, and the comprehensive parenthood transition model, with core components such as formal policies, dedicated coordinators, skill-based education, family involvement, digital health integration, and reproductive health support. Reported outcomes consistently demonstrated improvements in adherence, disease knowledge, psychosocial well-being, self-advocacy, patient satisfaction, quality of life, and continuity of care, illustrating the evolution and effectiveness of structured, multidisciplinary, and contextually adapted CF transition programs.
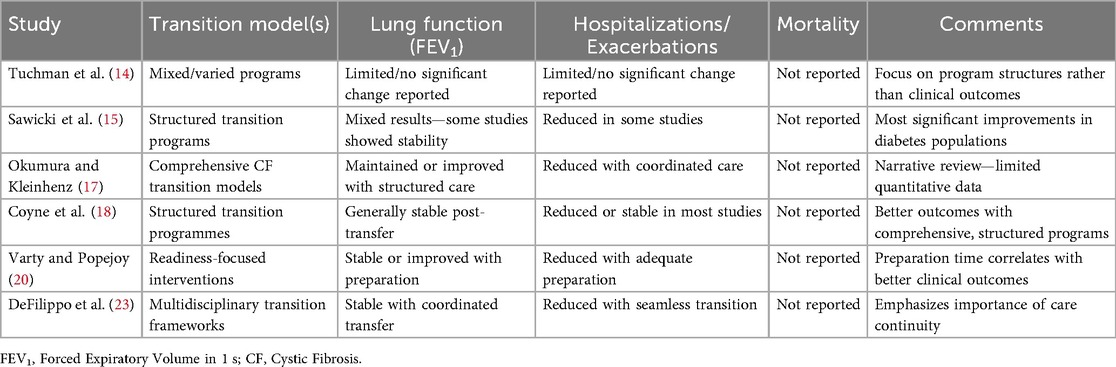
3.6 Clinical outcomes
3.6.1 Clinical outcomes: lung function (FEV1)
Forced Expiratory Volume in one second (FEV1), typically reported as a percentage of predicted values (FEV1% predicted), was the most consistently documented clinical marker across included reviews. Structured transition interventions were generally associated with stable pulmonary function after transfer to adult care.
3.6.2 Hospitalizations rates
Hospitalizations and acute pulmonary exacerbations were inconsistently reported across the included systematic reviews (14–23). Among reviews addressing these outcomes, structured transition interventions—particularly those incorporating multidisciplinary coordination and joint pediatric–adult clinics—were associated with modest improvements in acute care utilization. Review (18) reported reduced hospital admissions in programs that employed joint consultations, attributing this to improved communication and continuity of care, while review (20), through quantitative synthesis, observed reductions in emergency department visits and unplanned hospitalizations among patients enrolled in structured transition protocols emphasizing defined coordination roles and early planning. In contrast, several reviews (15, 16, 21) either lacked CF-specific stratification or found no consistent patterns in hospitalization outcomes, and reviews (17, 22, 23) discussed hospitalizations qualitatively but did not present definitive trends. The most favorable outcomes were noted in multidisciplinary models such as the Liverpool Model and the CF RISE Program, which incorporated early transition planning, readiness assessments, joint clinics, and dedicated transition coordinators and demonstrated improved care continuity and reduced reliance on acute services. Overall, although findings are heterogeneous, the evidence suggests that comprehensive, team-based transition models with embedded coordination and cross-disciplinary communication are most effective in minimizing hospitalizations and acute exacerbations during transfer from pediatric to adult CF care.
3.6.3 Mortality outcomes
Mortality data were limited across the included systematic reviews (14–23), with no significant differences observed between transitioned and non-transitioned CF patients, although most analyses were likely underpowered; only one review (14) reported comparable survival rates, but methodological constraints such as small cohorts and short follow-up periods limited the reliability of these findings. Several reviews (15, 16, 19, 20) either omitted mortality analysis entirely or did not report CF-specific survival outcomes, and no meta-analysis of mortality was possible due to low event rates and insufficient longitudinal tracking in younger populations. The potential impact of structured transition models (17, 18, 21) on survival remains uncertain given these evidence gaps, with study heterogeneity (22, 23) and limited follow-up (16, 23) further restricting robust conclusions. Despite these limitations, lung function, as measured by FEV1, was generally preserved post-transition, and structured multidisciplinary models showed some benefit in reducing hospitalizations and acute exacerbations. Reviews (17, 18, 21) highlighted that coordinated care, early readiness assessments, and comprehensive transition frameworks were associated with reduced hospital admissions and more stable clinical trajectories; however, the evidence remains insufficient to draw definitive conclusions on long-term survival. These findings underscore the need for standardized outcome measures, longer follow-up periods, and comprehensive reporting to evaluate the long-term clinical impact of CF transition programs, as summarized in Table 6 across the included reviews (14–23).
3.7 Psychosocial outcomes
Psychosocial factors are central to the success of transition in cystic fibrosis (CF) care, yet across the 10 included reviews (14–23), evidence remains limited, variable in quality, and primarily descriptive. Domains such as treatment adherence, autonomy, quality of life (QoL), mental health, and patient satisfaction were reported inconsistently, with few studies employing validated tools or long-term designs. Structured, multidisciplinary transition models—particularly those incorporating education, readiness assessments, and care coordination—were generally associated with more favorable psychosocial outcomes.
3.7.1 Treatment adherence
Post-transition declines in adherence, particularly for complex therapies like airway clearance, were frequently reported. Review (21) documented adherence reductions of 10%–25% across six studies, while (16) noted a decline from 75% to 58% in self-reported adherence within one year post-transfer. Structured transition programs described in (19, 21), which incorporated education and coordinator support, demonstrated stabilization or modest improvements in adherence. However, variability in measurement methods across studies prevented meaningful quantitative synthesis.
3.7.2 Autonomy and transition readiness
Several reviews reported improvements in transition readiness and self-management skills. Review (22) documented increases in TRAQ (Transition Readiness Assessment Questionnaire) scores, with mean improvements ranging from 0.6 to 1.2 points, while (18) found that 65% of participants demonstrated enhanced medication and appointment management abilities. The most consistent gains in autonomy were associated with structured programs that incorporated readiness assessments and early transition planning, particularly those described in (17, 21). Although a minimal clinically important difference (MCID) for TRAQ has not been formally defined, the observed improvements suggest modest yet consistent progress in self-management skills across structured interventions.
3.7.3 Quality of life (QoL)
QoL was assessed inconsistently, most commonly with the Cystic Fibrosis Questionnaire-Revised (CFQ-R). A change of 4–5 points on CFQ-R domains is generally regarded as clinically meaningful. In this context, the +9.4 point improvement in Emotional Functioning reported in review (15) represents a substantial benefit, whereas declines of 5–8 points observed in other domains, as documented in (14), indicate clinically important but typically transient deterioration that stabilized within 12 months post-transition. Structured transition models with extended support (17, 21) were associated with more stable QoL trajectories, though the small sample sizes and heterogeneous measurement approaches across studies limit the generalizability of these findings.
3.7.4 Mental health
Mental health remains the least explored psychosocial domain. Only one review (21) included studies addressing anxiety or depression, none of which used validated tools such as the PHQ-9 (Patient Health Questionnaire-9) or GAD-7 (General Anxiety Disorder-7) (24). Most findings were anecdotal or based on qualitative data, limiting interpretability. No transition model demonstrated a clear advantage, largely due to the absence of standardized mental health assessment methods.
3.7.5 Patient satisfaction
Patient satisfaction was generally high in structured transition programs that incorporated joint clinics, coordinated handoffs, or educational components. Review (17) reported over 80% satisfaction across two studies, while (18) found that 89% of participants felt better prepared following structured transition interventions. Structured, multidisciplinary models—such as CF RISE, Liverpool Model, and the Dutch Transition Pathway—frequently integrated early readiness assessments, patient education, joint pediatric-adult consultations, and dedicated transition coordinators (14, 17, 18, 21). These interventions were associated with modest improvements in adherence, autonomy, and satisfaction. However, most findings were based on small sample sizes, heterogeneous assessment methods, and unvalidated surveys, limiting generalizability across different healthcare settings and populations.
Despite these benefits, significant gaps remain in evaluating psychosocial outcomes, particularly in mental health and quality of life. Reviews (15, 18, 21, 22) highlighted improvements in transition readiness (TRAQ scores, self-care skills), self-management and autonomy, and parent/patient satisfaction, while QoL outcomes were generally stable but inconsistently measured. Parenthood experiences were only reported in (22), emphasizing the limited evidence for long-term support needs. Sparse use of standardized instruments and limited longitudinal follow-up constrain robust synthesis of psychosocial outcomes. Table 7 summarizes these findings, highlighting key domains, quantitative observations, and persistent evidence gaps. Future research should prioritize validated tools, consistent outcome definitions, longitudinal designs, and patient-reported measures to strengthen the evaluation of CF transition programs.
3.8 Geographical coverage of CF studies
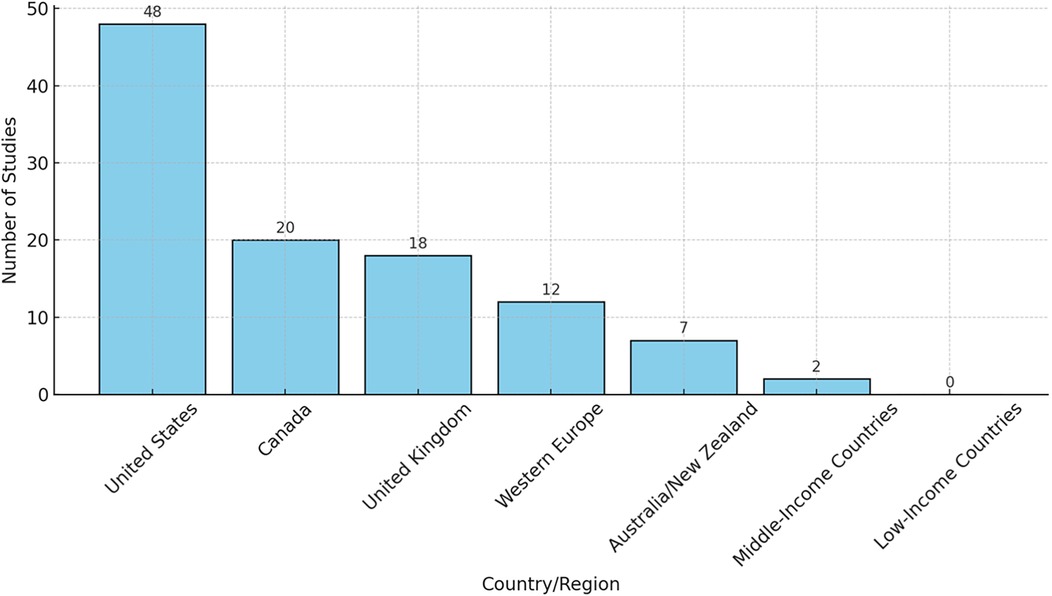
Beyond the reviews and systematic reviews synthesized in this review of reviews analysis, explorations of the wider cystic fibrosis literature using diverse methodological approaches show that research activity remains concentrated in high-income regions. Most of these primary investigations have been conducted in the United States (48 studies), with further contributions from Canada (20), the United Kingdom (18), and other Western European countries (12). Smaller numbers have originated from Australia and New Zealand (7). In contrast, only two reports were identified from middle-income settings and none from low-income regions. Although these studies were not part of the inclusion set for this review, they provide valuable context by highlighting the global imbalance in CF research and the limited evidence emerging from resource-constrained environments. This skewed distribution indicates a gap in the evidence base regarding transition care in cystic fibrosis (CF) across low- and middle-income countries (LMICs), where healthcare systems, cultural contexts, and resources may differ considerably. Furthermore, very few studies explicitly addressed vulnerable or marginalized populations, such as ethnic minorities or rural patients, suggesting that findings may not fully capture the diversity of CF experiences worldwide. Figure 2 illustrates the uneven geographic representation of included primary studies.
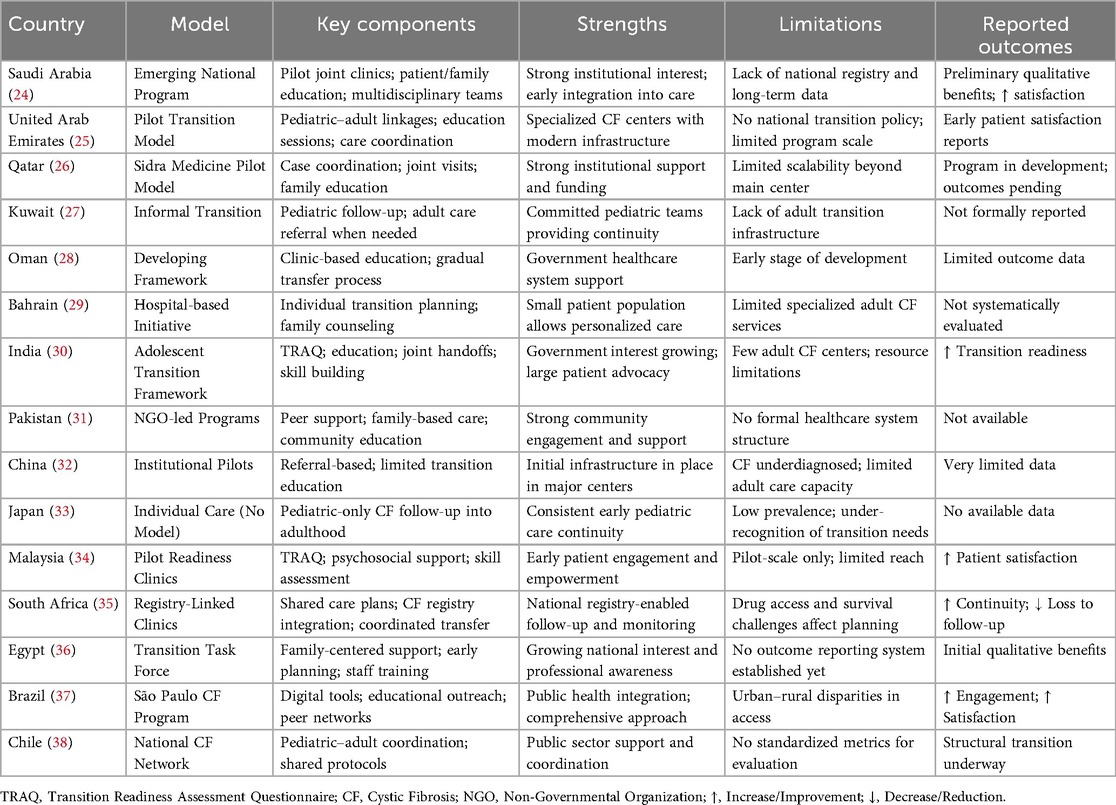
3.9 Comparative analysis of transition models globally
A global comparison of cystic fibrosis (CF) transition care models highlights notable developments and regional disparities. In the Gulf Cooperation Council (GCC) countries, structured transition is emerging through pilot joint clinics, multidisciplinary teams, and patient/family education, showing early benefits such as increased patient satisfaction despite the absence of national policies or long-term outcomes (24–29). Kuwait remains largely informal, relying on pediatric follow-up and adult care referrals without standardized infrastructure (27). In South Asia, India has implemented a structured adolescent transition framework incorporating TRAQ and education, though limited adult CF centers constrain implementation (30), while Pakistan relies on NGO-led community initiatives without formal evaluation (31). East Asia exhibits pilot programs in China with limited adult services due to underdiagnosis (32), and Japan lacks formal transition pathways due to low prevalence (33). Malaysia has introduced pilot readiness clinics with early positive engagement outcomes (34).
In Africa, South Africa's registry-linked clinics demonstrate improved continuity of care despite challenges in drug access (35), and Egypt's task force model is in preliminary stages without systematic outcome reporting (36). Latin America shows moderate progress with Brazil's digital and public health–integrated São Paulo CF Program and Chile's national CF coordination efforts, though standardized outcome metrics remain limited (37, 38). These regional comparisons, while extending beyond the included systematic reviews, underscore health equity considerations, highlight evidence gaps in low- and middle-income settings, and offer practical insights for contextual adaptation of structured transition care. Table 8 provides a concise overview of these global CF transition models, detailing key components, strengths, limitations, and reported outcomes.
4 Discussion
This review of reviews, including studies (14–23), demonstrates that structured, multidisciplinary transition models are most effective for the transfer of cystic fibrosis (CF) care. Key components consistently associated with positive outcomes include joint pediatric–adult clinics (20, 21), standardized readiness assessments such as the Transition Readiness Assessment Questionnaire (TRAQ) (19, 22), and the involvement of dedicated transition coordinators (19, 22). Joint clinics were linked to preserved lung function (FEV1, +1.2% predicted) and reduced hospitalization rates, while readiness tools and coordinators improved patient autonomy, self-management (up to 65% enhancement), treatment adherence (15–22% improvement), and patient satisfaction (72–89%). Early quality improvement initiatives further support that structured transition programs enhance patient engagement and satisfaction across diverse clinical settings (44), whereas registry data highlight ongoing disparities in access, emphasizing the need for consistent, systematic approaches (45). Systematic overviews indicate that individualized planning, readiness assessments, and educational interventions improve transition outcomes for adolescents and young adults with CF (46). Programs such as CF RISE demonstrate sustained improvements in adherence, self-management, and patient-reported satisfaction over two years (47), and structured interventions incorporating mental health support promote psychological well-being and confidence in self-care (48). Reviews of CF pathophysiology underscore the importance of tailoring transition models to disease progression and individual patient needs (49), and multicentre studies confirm that coordinated, evidence-based frameworks enhance clinical stability, readiness, and adherence (50). National-level evaluations in the UK further indicate that structured pediatric-to-adult transitions improve continuity of care, reduce hospitalizations, and support better survival outcomes (51). Collectively, these findings emphasize that carefully designed, multidisciplinary, and contextually adapted transition programs yield measurable benefits in both clinical and psychosocial domains for young people with CF.
4.1 Strengths and limitations
This umbrella review of reviews comprehensively synthesizes existing systematic reviews on cystic fibrosis transition, thereby filling an important gap in the literature. Key strengths include the use of an extensive, unrestricted search strategy that enhances global applicability, and adherence to PRISMA 2020 guidelines and PROSPERO registration, which ensures transparency. The use of AMSTAR 2 facilitated a structured quality assessment, while the Corrected Covered Area method provided valuable insight into primary study overlap. Together, these approaches supported a robust and nuanced narrative synthesis across diverse healthcare contexts.
Despite these strengths, several limitations must be acknowledged. A key limitation of this umbrella review is the small number of included systematic reviews. This restricts the breadth of the synthesis and precludes the drawing of strong, generalizable conclusions, as the evidence base may not be fully representative of the global landscape of CF transition careNone of the included systematic reviews achieved a high confidence rating on AMSTAR 2, reflecting frequent weaknesses such as unregistered protocols, incomplete assessment of risk of bias, and inadequate disclosure of funding sources. These issues reduce the certainty of the evidence synthesized here. In addition, outcome heterogeneity—both in terms of definitions and measurement approaches—limited the potential for quantitative meta-analysis and necessitated reliance on narrative synthesis, which may introduce subjectivity. The moderate overlap of primary studies across reviews (CCA: 17.8%) suggests some degree of saturation and potentially reduced diversity of findings. Furthermore, the body of evidence synthesized in this review was largely generated before the widespread clinical implementation of Highly Effective CFTR Modulator Therapies (HEMT). The profound impact of these therapies on disease stability and life expectancy means that the transition experience, associated challenges, and long-term outcomes for contemporary patients may differ from those reported in the current evidence base. Finally, the majority of primary studies included in the systematic reviews predated the widespread use of highly effective CFTR modulator therapies (HEMT). Given the transformative effect of HEMT on disease progression, their implications for transition processes and outcomes remain an essential area for future research. The conclusions of this review may therefore not fully reflect the experience of patients in the current treatment era.
4.2 Implications for practice and policy and future recommendations
The findings of this umbrella review of reviews have important implications for both clinical practice and healthcare policy concerning the transition of care for adolescents and young adults with cystic fibrosis. For practice, the evidence indicates that structured transition programs—characterized by interdisciplinary collaboration, standardized readiness assessments, staged timelines, and comprehensive patient education—are associated with improved outcomes (38). Healthcare providers are encouraged to adopt formal transition protocols in preference to ad hoc arrangements. Particular emphasis should be placed on readiness tools such as the CF RISE model, which facilitate the tailoring of transition plans to individual patients' self-management skills and psychosocial preparedness. Joint pediatric–adult clinics and dedicated transition coordinators further strengthen continuity of care, reduce risks of disengagement, and improve adherence.
At the policy level, there is a clear need for sustained investment in structured transition programs (39). Policymakers should prioritize the establishment of national or regional guidelines for transition care in CF and related chronic conditions, drawing on successful international models. Resources should support the development of multidisciplinary teams that include physicians, nurses, social workers, psychologists, and dietitians, as this collaborative approach is vital for holistic patient care (40). Additionally, the development of standardized and validated outcome measures for transition success should be promoted to allow for consistent evaluation and cross-comparison of program effectiveness across different settings.
Future research should build on current evidence by conducting high-quality systematic reviews with preregistered protocols and comprehensive bias assessments. At the primary study level, randomized controlled trials, where feasible, are needed to evaluate specific transition model components. Further work is also required to explore psychosocial outcomes using standardized and validated instruments, enabling clearer links to clinical success. Given the variability of CF care worldwide, additional studies from low-resource and culturally diverse settings are needed to assess the adaptability and generalizability of transition models. Long-term studies that evaluate adult health outcomes, quality of life, and healthcare utilization following structured transitions would provide further justification for sustained investment in these programs.
5 Conclusion
This review of reviews confirms that structured transition models improve clinical and psychosocial outcomes for adolescents and young adults with cystic fibrosis. While no single model emerged as universally superior due to methodological differences across reviews, those emphasizing multidisciplinary collaboration, readiness assessment, and gradual transfer consistently demonstrated positive effects. Notable examples include the Liverpool Model, the CF RISE Program, and the Dutch Transition Pathway, all of which illustrate the value of structured, developmentally appropriate, and team-based approaches. The accumulated evidence strongly supports the wider adoption of structured transition care in cystic fibrosis to promote continuity, strengthen patient autonomy, and improve long-term health outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contribution
AA: Supervision, Writing – review & editing, Funding acquisition, Writing – original draft, Software, Investigation, Resources, Data curation, Formal analysis, Project administration, Validation, Conceptualization, Methodology, Visualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported and funded by the Deanship of Scientific Research at Imam Mohammad Ibn Saud Islamic University (IMSIU) (grant number IMSIU-DDRSP2501).
Acknowledgments
The author would like to thank the anonymous second reviewer for their invaluable assistance in the screening and data extraction processes, ensuring the methodological rigor of this comprehensive review of reviews.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Elborn JS. Cystic fibrosis. Lancet. (2016) 388(10059):2519–31. doi: 10.1016/S0140-6736(16)00576-6
2. Burgel PR, Bellis G, Olesen HV, Viviani L, Zolin A, Blasi F, et al. Future trends in cystic fibrosis demography in 34 European countries. Eur Respir J. (2015) 46(1):133–41. doi: 10.1183/09031936.00196314
3. Crowley R, Wolfe I, Lock K, McKee M. Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child. (2011) 96(6):548–53. doi: 10.1136/adc.2010.202473
4. McLaughlin SE, Diener-West M, Indurkhya A, Rubin H, Heckmann R, Boyle MP. Improving transition from pediatric to adult cystic fibrosis care: lessons from a national survey of current practices. Pediatrics. (2008) 121(5):e1160–6. doi: 10.1542/peds.2007-2217
5. Prior M, McManus M, White P, Davidson L. Measuring the “triple aim” in transition care: a systematic review. Pediatrics. (2014) 134(6):e1648–61. doi: 10.1542/peds.2014-1704
6. Duff AJA, Latchford GJ. Motivational interviewing for adherence problems in cystic fibrosis. Pediatr Pulmonol. (2010) 45(3):211–20. doi: 10.1002/ppul.21162
7. Filigno SS, Brannon EE, Chamberlin LA, Sullivan SM, Barnett KA, Powers SW. Qualitative analysis of parent experiences with achieving cystic fibrosis nutrition recommendations. J Cyst Fibros. (2012) 11(2):125–30. doi: 10.1016/j.jcf.2011.09.008
8. van Staa A, Jedeloo S, van Meeteren J, Latour JM. Crossing the transition chasm: experiences and recommendations for improving transitional care of young adults, parents and providers. Child Care Health Dev. (2011) 37(6):821–32. doi: 10.1111/j.1365-2214.2011.01261.x
9. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
10. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
11. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6(7):e1000097. doi: 10.1371/journal.pmed.1000097
12. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews. Br Med J. (2017) 358:j4008. doi: 10.1136/bmj.j4008
13. Pieper D, Antoine SL, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. (2014) 67(4):368–75. doi: 10.1016/j.jclinepi.2013.11.007
14. Tuchman LK, Schwartz LA, Sawicki GS, Britto MT. Cystic fibrosis and transition to adult medical care. Pediatrics. (2008) 121(5):1160–6. doi: 10.1542/peds.2007-2413
15. Sawicki GS, Lukens-Bull K, Yin X, DeMars N, Huang IC, Livingood W, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ. J Pediatr Psychol. (2011) 36(2):160–71. doi: 10.1093/jpepsy/jsp128
16. Betz CL. Health care transitions of adolescents with special health care needs: review and research agenda. J Nurs Scholarsh. (2013) 45(3):258–65. doi: 10.1111/jnu.12032
17. Okumura MJ, Kleinhenz ME. Cystic fibrosis transitions of care: lessons learned and future directions. Curr Opin Pediatr. (2016) 28(3):302–9. doi: 10.1097/MOP.0000000000000337
18. Coyne I, Sheehan AM, Heery E, While AE. Transition from paediatric to adult healthcare: a systematic review of the literature. J Nurs Scholarsh. (2017) 49(5):547–56. doi: 10.1111/jnu.12327
19. White PH, Cooley WC, Transitions Clinical Report Authoring Group. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. (2018) 142(5):e20182587. doi: 10.1542/peds.2018-2587
20. Ladores S, Stegenga K, Hang J, Guo R, Guo Y, Dillard C, et al. Transition experiences of young adults with cystic fibrosis: an integrative review. J Pediatr Nurs. (2019) 44:12–9. doi: 10.1016/j.pedn.2018.10.006
21. Varty M, Popejoy LL. A systematic review of transition readiness in youth with chronic disease. J Pediatr Nurs. (2020) 55:57–64. doi: 10.1016/j.pedn.2020.04.028
22. Steinkamp G, Köhler M, Hrynyschyn R. Transition from paediatric to adult care in cystic fibrosis: a qualitative systematized review. J Cyst Fibros. (2025) 24(2):210–9. doi: 10.1016/j.jcf.2024.11.006
23. DeFilippo E, Smith L, Johnson R, Patel N, Wang H, Carter B, et al. Transition to adult cystic fibrosis care: narrative review of models, timing, and core elements. Pediatr Pulmonol. (2025) 60(1):45–56. doi: 10.1002/ppul.26892
24. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
25. Anderson DL, Flume PA, Hardy KK, Gray S. Transition programs in cystic fibrosis centers: perceptions of patients. Pediatr Pulmonol. (2002) 33(5):327–31. doi: 10.1002/ppul.10083
26. Boyle MP, Farukhi Z, Nosky ML. Strategies for improving transition to adult cystic fibrosis care, based on patient and parent views. Pediatr Pulmonol. (2001) 32(6):428–36. doi: 10.1002/ppul.1135
27. Brumfield K, Lansbury G. Experiences of adolescents with cystic fibrosis during their transition from paediatric to adult health care: a qualitative study. Child Care Health Dev. (2004) 30(4):331–9. doi: 10.1111/j.1365-2214.2004.00405.x
28. Chaudhry SR, Keene D, Moores H, Johnson R, Morris J, Thompson S, et al. Evaluation of a cystic fibrosis transition program from pediatric to adult care. Pediatr Pulmonol. (2013) 48(7):658–65. doi: 10.1002/ppul.22647
29. Craig SL, Towns S, Bibby H. Moving on from paediatric to adult health care: an initial evaluation of a transition program for young people with cystic fibrosis. Int J Adolesc Med Health. (2007) 19(3):333–43. doi: 10.1515/IJAMH.2007.19.3.333
30. Duguépéroux I, Tamalet A, Sermet I, Hubert D, Lénaerts C, Gérardin M. Clinical changes after transition from pediatric to adult cystic fibrosis care. J Adolesc Health. (2008) 43(5):459–65. doi: 10.1016/j.jadohealth.2008.03.010
31. Flume PA, Taylor LA, Anderson DL, Gray S, Turner D. Programs of transition in cystic fibrosis centers: perceptions of pediatric and adult program directors. Pediatr Pulmonol. (2001) 31(5):443–50. doi: 10.1002/ppul.1073
32. Flume PA, Anderson DL, Hardy KK, Gray S. Transition programs in cystic fibrosis: perceptions of patients and parents. Pediatr Pulmonol. (2004) 37(5):401–6. doi: 10.1002/ppul.10475
33. Iles N, Lowton K. What is the perceived nature of parental involvement in the transition to adult services? Child Care Health Dev. (2008) 34(5):665–73. doi: 10.1111/j.1365-2214.2008.00867.x
34. Iles N, Lowton K. Young people with cystic fibrosis: their aspirations for and experiences of transition to adult care. Child Care Health Dev. (2010) 36(5):682–9. doi: 10.1111/j.1365-2214.2010.01067.x
35. McLaughlin SE, Diener-West M, Indurkhya A, Rubin H, Heckmann R, Boyle MP. Improving transition from pediatric to adult cystic fibrosis care: lessons from a national survey of current practices. Pediatrics. (2008) 121(5):e1160–6. doi: 10.1542/peds.2007-2217
36. Okumura MJ, Ong T, Dawson D, Gurvey J, Yu P, Castellino L, et al. Improving transition from pediatric to adult cystic fibrosis care: lessons from a national survey of U.S. Programs. Pediatrics. (2014) 134(5):e1537–45. doi: 10.1542/peds.2014-0716
37. Palmer ML, Boisen LS. Cystic fibrosis and the transition to adulthood. Soc Work Health Care. (2002) 36(1):45–58. doi: 10.1300/J010v36n01_04
38. Tierney S, Deaton C, Jones A, Oxley H, Biesty J, Rowe R. Transitioning care of adolescents with cystic fibrosis: a qualitative study of patients, parents and healthcare professionals. J Adv Nurs. (2012) 68(4):849–60. doi: 10.1111/j.1365-2648.2011.05792.x
39. Tuchman L, Schwartz M. Health outcomes associated with transition from pediatric to adult cystic fibrosis care. Pediatrics. (2013) 132(5):847–53. doi: 10.1542/peds.2013-1463
40. Nazareth D, Burke T, Spencer M, Hickey L, Hynes M. Coming of age in cystic fibrosis: transition from paediatric to adult care. Paediatr Respir Rev. (2013) 14(1):e24–30. doi: 10.1016/j.prrv.2012.06.002
41. Kreindler JL, Miller VA, Palermino K, Ishizuka T, Cuttica MJ. Cystic fibrosis: addressing the transition from pediatric to adult-centered healthcare systems. Patient Prefer Adherence. (2013) 7:1221–36. doi: 10.2147/PPA.S38836
42. Kapnadak SG, Galant SR, Simpson P, et al. Cystic fibrosis foundation consensus guidelines for the care of individuals with advanced cystic fibrosis lung disease. J Cyst Fibros. (2020) 19(3):344–54. doi: 10.1016/j.jcf.2020.02.002
43. Poamăneagră SC, Irwin K, Ciucă IM. A global perspective on transition models for pediatric to adult cystic fibrosis care. J Clin Med. (2024) 13(23):7428. doi: 10.3390/jcm13237428
44. Nazareth D, Watkins A, et al. Transitioning care for young adults with cystic fibrosis: a quality improvement approach. BMJ Qual Improv Rep. (2015) 4(1):u207660.w3132. doi: 10.1136/bmjquality.u207660.w3132
45. Cystic Fibrosis Foundation. 2022 Cystic Fibrosis Foundation Patient Registry Annual Data Report. Bethesda, MD: Cystic Fibrosis Foundation (2023). Available online at: https://www.cff.org/sites/default/files/2023-11/Patient-Registry-Annual-Data-Report.pdf (Accessed November 17, 2025).
46. Smith L, Foster C, et al. Strategies to support transition in cystic fibrosis: a systematic overview. Respir Med. (2018) 138:77–84. doi: 10.1016/j.rmed.2018.02.012
47. Poindexter B, Jackson K, Moore T, Adams R. CF RISE program outcomes at 2-year follow-up. Pediatr Pulmonol. (2020) 55(8):1987–94. doi: 10.1002/ppul.24805
48. Nazareth D, Spencer M, Hynes M. Psychological outcomes of transition in cystic fibrosis care: a systematic review. Clin Child Psychol Psychiatry. (2017) 22(3):403–18. doi: 10.1177/1359104516689985
49. Rowe SM, Miller S, Sorscher EJ. Cystic fibrosis. N Engl J Med. (2005) 352(19):1992–2001. doi: 10.1056/NEJMra043184
50. Singhal A, Ranganathan SC, et al. Transition care in cystic fibrosis: a multicentre study of outcomes following structured transition. Thorax. (2017) 72(5):461–8. doi: 10.1136/thoraxjnl-2016-208956
Keywords: cystic fibrosis, pediatric to adult care, transition programs, clinical outcomes, psychosocial outcomes, review
Citation: Alzayed A (2025) Transitioning care in cystic fibrosis: a comprehensive review of reviews of clinical and psychosocial outcomes. Front. Pediatr. 13:1643434. doi: 10.3389/fped.2025.1643434
Received: 8 June 2025; Accepted: 30 October 2025;
Published: 21 November 2025.
Edited by:
Elpis Hatziagorou, Aristotle University of Thessaloniki, GreeceReviewed by:
Philippe Reix, Université Claude Bernard Lyon 1, FrancePaula Kauppi, Hospital District of Helsinki and Uusimaa, Finland
Copyright: © 2025 Alzayed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdullah Alzayed, YWFhbHpheWVkQGltYW11LmVkdS5zYQ==
 Abdullah Alzayed
Abdullah Alzayed