- Pediatric Orthopedics Department, Northwest Women’s and Children’s Hospital, Xian, China
Objective: To investigate and analyze the application value of elbow arthrography in the treatment of chronic radial head dislocation in children.
Methods: From January 2014 to January 2017, 15 children with chronic anterior radial head dislocation were treated (11 boys, 4 girls; average age 9 years, range 3–11 years). Intraoperative elbow arthrography was performed to assess the position of the radial head relative to the joint capsule. The nature of the dislocation was confirmed by opening the joint capsule to directly observe the relationship between the radial head and capitellum, as well as the morphology of the radial head. Reduction of the radial head was achieved via proximal ulnar osteotomy, and fixation was performed using a plate and screws with or without Kirschner wires (K-wires).
Results: Elbow arthrography showed the radial head was located within the joint capsule in 12 cases and outside the capsule in 3 cases. Among the cases: All 8 congenital dislocations had the radial head within the joint capsule. Of the 7 traumatic dislocations, 4 had the radial head within the capsule and 3 outside. Direct inspection after capsulotomy confirmed the arthrography findings and revealed characteristic morphological differences. In congenital dislocations, there was no scar tissue between the radial head and capitellum, and the radial head fovea was shallow and flat. In traumatic dislocations, obvious scar tissue was present between the radial head and capitellum, and the radial head fovea was distinct. Three patients with traumatic dislocations (all with the radial head outside the capsule on arthrogram) required supplemental trans-articular K-wire fixation due to instability after reduction. Follow-up ranged from 9 months to 4 years (average 2 years 5 months). Postoperative radiographs showed no cases of radial head re-dislocation or subluxation. Postoperative elbow range of motion improved in all patients, with no reports of pain or functional instability.
Conclusion: Elbow arthrography serves as a valuable adjunct for differentiating between congenital and traumatic radial head dislocations, thereby informing both surgical strategy and the decision for supplemental fixation. When stable bony alignment is achieved, proximal ulnar osteotomy without annular ligament reconstruction represents an effective management strategy for chronic radial head dislocation in children.
Introduction
Chronic radial head dislocation in children arises either as a sequela of missed Monteggia fracture (1–3) or as a congenital condition (4). This pathology can lead to progressive valgus deformity of the affected elbow and impair its function. Over time, longitudinal growth discrepancy may develop, resulting in relative overgrowth of the radius compared to the ulna. Consequently, the ulna on the affected side becomes shorter than that on the contralateral, unaffected side (5). Treatment of chronic radial head dislocation is challenging (6–9). Among the clinical approaches available, proximal ulnar osteotomy, with or without gradual lengthening, is the most frequently recommended procedure. However, numerous postoperative complications can occur throughout the treatment course (10). Achieving satisfactory outcomes remains a significant challenge for pediatric surgeons.
Due to the unclear history in children, distinguishing between traumatic and congenital etiologies can be challenging. This study utilized intraoperative elbow arthrography to indirectly assess the relationship between the radial head and the joint capsule as an indicator of etiology (traumatic vs. congenital), which was subsequently verified by direct observation upon opening the capsule. Treatment involved proximal ulnar osteotomy for radial head reduction, followed by plate and screw fixation with or without Kirschner wires (K-wires). Satisfactory short-term outcomes were achieved, as reported below.
Materials and methods
Fifteen children with anterior radial head dislocation were treated between January 2014 and January 2017 (11 boys, 4 girls; average age 9 years, range 3–11 years). Dislocation involved the left side in 3 cases and the right side in 12 cases. All dislocations were anterior.
Preoperative imaging included anteroposterior (AP) and lateral views of the affected elbow. Intraoperatively, the child was placed supine. After anesthesia induction and standard sterile preparation and draping, posterior or lateral elbow arthrography was performed. A 5 ml syringe needle was used for puncture. After confirming intra-articular placement, approximately 1 ml of iohexol (Omnipaque) contrast agent was injected. Fluoroscopy was used to visualize the position of the radial head. A posterior elbow approach was used: an incision was made along the lateral border of the ulna, dissecting through skin and subcutaneous tissue to reach the proximal ulna. The incision was extended laterally, the joint capsule was opened, and the radial head was exposed. An oscillating saw was used to perform an osteotomy from posterior to anterior at the proximal ulna, near the level of the coronoid process. The proximal ulnar segment was flipped. Any scar tissue between the radial head and capitellum was thoroughly debrided. The proximal ulna was then rotated or angulated posteriorly to reduce the radial head. With the radial head satisfactorily reduced, the osteotomy site was fixed using a plate and screws with or without K-wires. Forearm pronation and supination were tested to assess radial head stability. For cases unstable in pronation, a percutaneous Kirschner wire was inserted through the capitellum to fix the radial head with the elbow flexed at 90°, in a supinated position. No annular ligament reconstructions were performed in this series.
Results
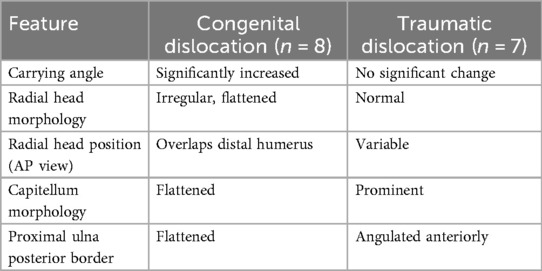
Preoperative radiographic assessment revealed differences between the two etiologies, summarized in Table 1. Congenital dislocations typically presented with an increased carrying angle, an irregular and flattened radial head, overlap of the radial head and distal humerus on AP view, and a flattened capitellum. Traumatic dislocations generally had a normal carrying angle, a relatively normal radial head shape, and a prominent capitellum.
Elbow arthrography showed the radial head within the joint capsule in 12 cases and outside the capsule in 3 cases. Regarding capsule position: All 8 congenital cases had the radial head within the capsule. Among the 7 traumatic cases, 4 had the radial head within the capsule and 3 outside. Direct inspection after capsulotomy confirmed these relationships and revealed characteristic findings: In the 8 congenital dislocation cases, there was no scar tissue between the radial head and capitellum, and the radial head fovea was shallow and flat. In the 7 traumatic dislocation cases, significant scar tissue was present between the radial head and capitellum, and the radial head fovea was distinct.
Arthrography was helpful for the surgical decision. When the dislocation was confirmed congenital, the proximal ulnar rotation osteotomy was performed. When the dislocation was detected traumatic, the posterior bending correction osteotomy of proximal ulna was performed. However, in 3 of the 7 traumatic cases (all of which had the radial head outside the capsule on arthrogram), intraoperative testing revealed persistent instability after reduction, necessitating supplemental trans-articular K-wire fixation. Supplemental trans-articular K-wire fixation was used in 2 of the 8 congenital cases because of instability during forearm pronation.
The K-wire stabilizing the radial head was typically removed 4 weeks postoperatively. Removal of the plate and screws was determined based on radiographic evidence of osteotomy union. All osteotomies healed primarily. Follow-up ranged from 9 months to 4 years (average 2 years 5 months). Follow-up radiographs showed no instances of radial head re-dislocation or subluxation. No intraoperative or postoperative complications, such as nerve injury, infection, or nonunion, were observed. While formal functional scores were not used, clinical assessment at final follow-up indicated improved elbow range of motion in all patients, with no reports of pain or functional instability.
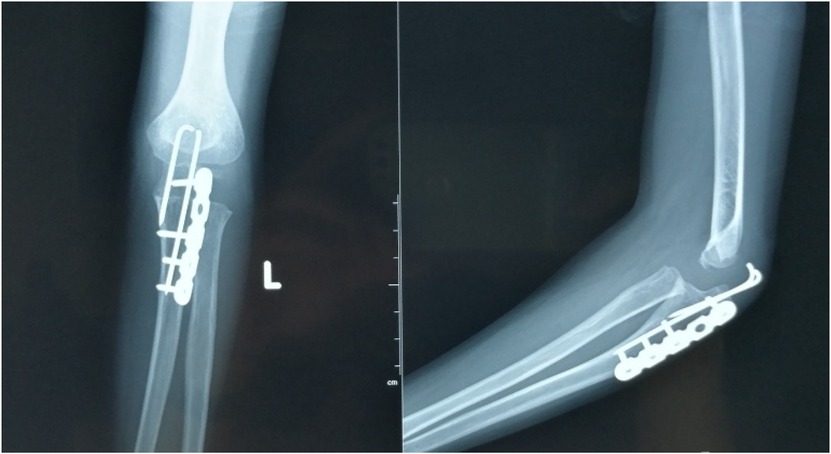
There were two typical patients. An 11-year-old boy presented with a 5-year interval between elbow trauma and surgical intervention. Intraoperative elbow arthrography confirmed the radial head remained within the joint capsule. Upon capsulotomy, scar tissue was observed around the radial head, though the depression of the radial head maintained a normal morphology (Figures 1–3).
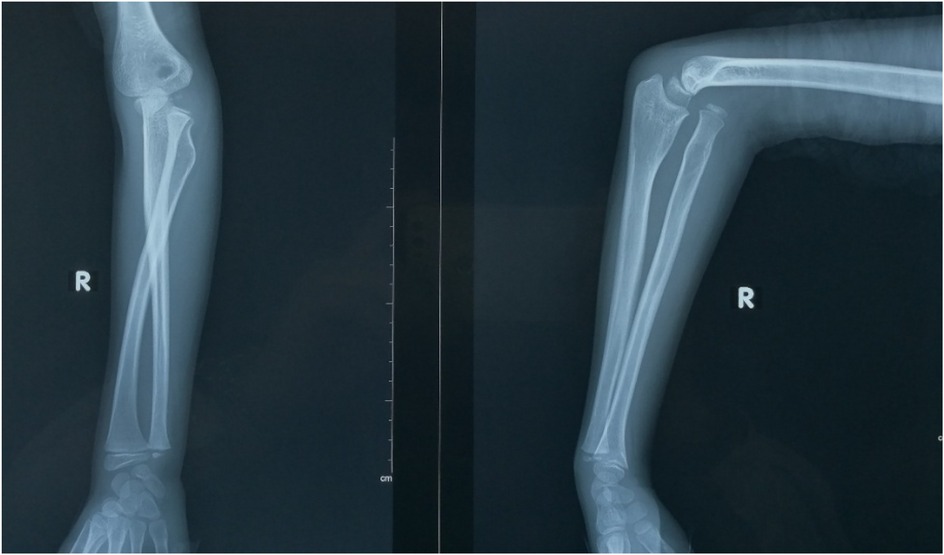
Figure 1. This was an anterior dislocation of the radial head. There was a “ulnar bow sign” in the affected ulna.
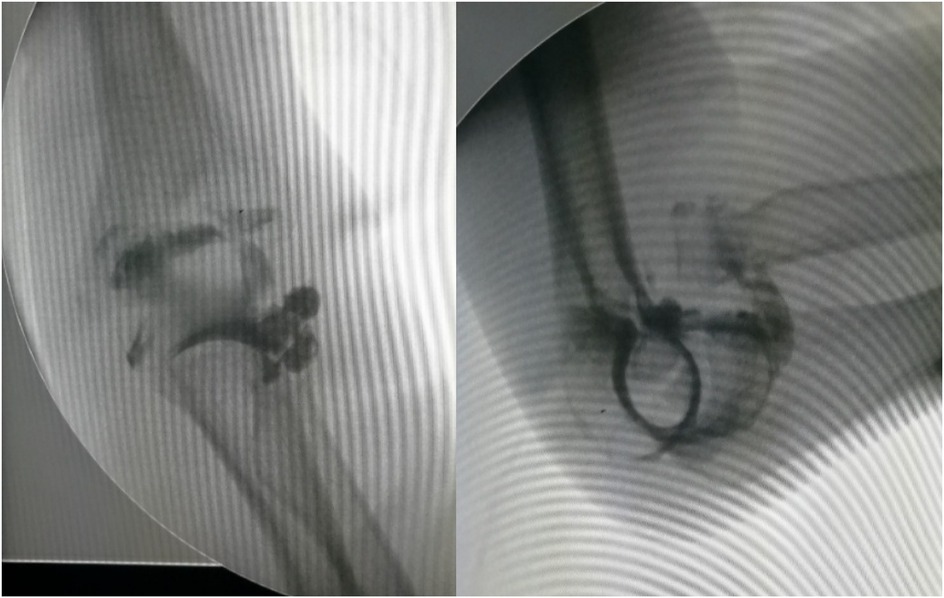
Figure 2. Intraoperative elbow arthrography confirmed the radial head remained within the joint capsule.

Figure 3. Upon capsulotomy, scar tissue was observed around the radial head, though the depression of the radial head maintained a normal morphology.
A 5-year-old boy had no history of left elbow trauma. Intraoperative arthrography also showed the radial head within the capsule. Capsulotomy revealed no scar tissue between the radial and humeral heads, but the radial head depression was shallow and flattened (Figures 4–6). Proximal ulnar osteotomy was performed with plate and K-wires internal fixation (Figure 7), with bony union achieved at 6 months postoperatively (Figure 8). Four-year follow-up demonstrated optimal realignment of the radial head within the elbow joint (Figure 9).

Figure 6. Capsulotomy revealed no scar tissue between the radial and humeral heads, but the radial head depression was shallow and flattened.
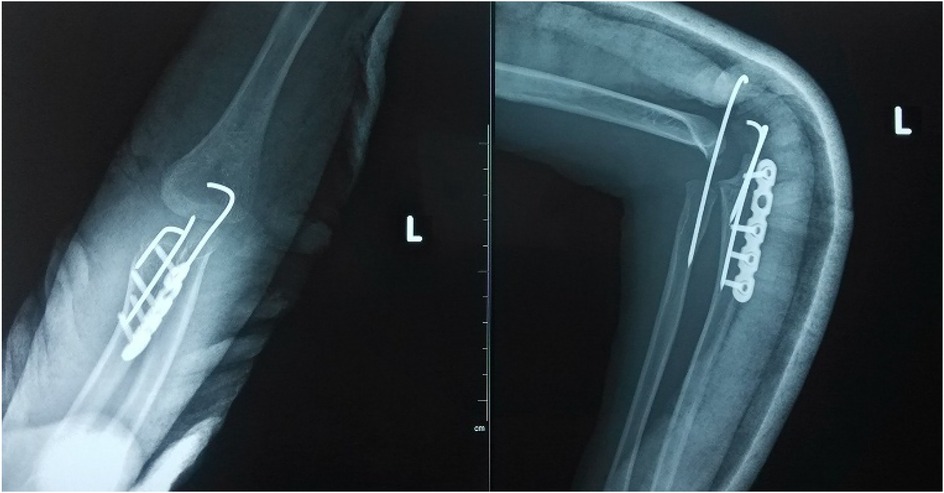
Figure 7. Proximal ulnar osteotomy was performed with plate and K-wires internal fixation. Supplemental trans-articular K-wire fixation was performed because of the instability in the forearm pronation movement.
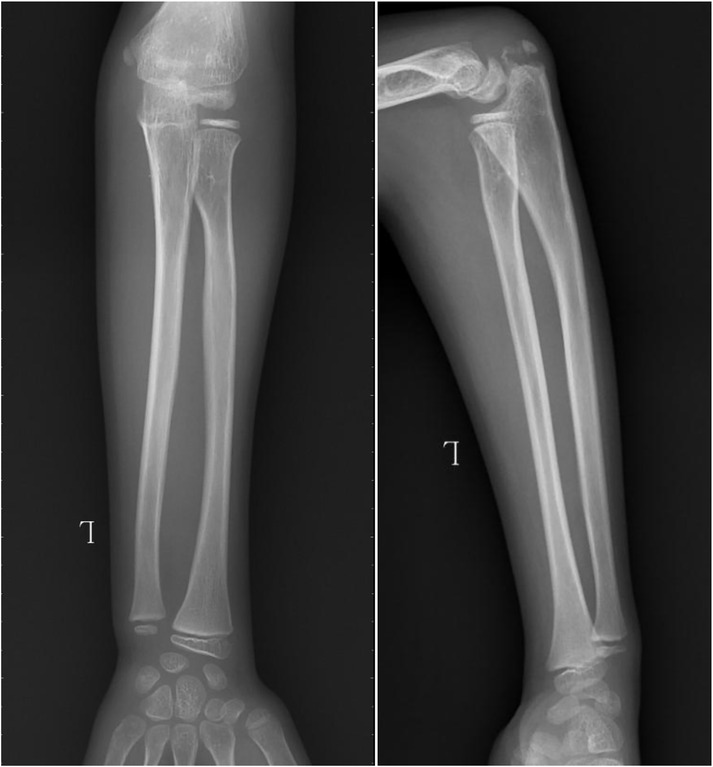
Figure 9. Four-year follow-up demonstrated optimal realignment of the radial head within the elbow joint.
Discussion
Monteggia fracture in children involves a fracture of the ulna combined with radial head dislocation. It is frequently missed initially, leading to chronic radial head dislocation. Anterior dislocation is more common clinically than lateral or posterior dislocation. The dislocated radial head, lacking the constraints of the capitellum and proximal ulna, develops abnormally, often becoming deformed. Long-standing post-traumatic radial head dislocation can present similarly to congenital dislocation. Without a clear history, differentiation is difficult.
In our series, 4 of the 7 traumatic cases had a definite history of trauma, while the other 3 had unclear histories. All 7 traumatic dislocations had been present for over 1 month (longest duration 5 years). None of the 8 congenital cases had a definite trauma history. Specific post-injury symptoms could not be reliably assessed due to the chronic nature in all cases. No associated deformities were found in any of the 15 patients. Preoperative closed reduction attempts were unsuccessful in all 15 cases.
Elbow arthrography is commonly used to diagnose elbow fractures in children with unossified epiphyses, aiding differentiation between distal humeral epiphyseal separation, lateral condylar fractures, and elbow dislocations (11–14). Its use specifically for assessing radial head dislocation in children is less frequently reported domestically or internationally (15, 16). In this study, intraoperative arthrography revealed that in congenital dislocations, the radial head and capitellum resided within the same joint capsule, surrounded by contrast. Traumatic dislocations presented two scenarios. In acute dislocations with significant ulnar angulation, arthrography showed the radial head outside the joint capsule relative to the capitellum, without surrounding contrast. In contrast, in gradual dislocations due to minimal ulnar angulation or greenstick fracture, arthrography showed the radial head within the joint capsule. Therefore, elbow arthrography provides auxiliary value in differentiating the nature of radial head dislocation. The findings of this study indicate that intraoperative elbow arthrography constitutes a valuable adjunct in the surgical management of pediatric chronic radial head dislocation. Its principal utility lies in enabling real-time, indirect assessment of the spatial relationship between the radial head and the joint capsule, thereby providing insight into the etiology. This imaging modality was especially diagnostic in scenarios where the patient history was ambiguous. Meanwhile, as noted in the results, arthrography guided the choice of osteotomy technique.
The traditional treatment for congenital radial head dislocation in children is radial head excision in adulthood, which may alleviate pain but does not significantly improve elbow flexion/extension or forearm rotation (17). Recent literature increasingly advocates for early surgical intervention in children (18, 19). Early reduction allows the radial head to remodel and develop (20), improving congruence with the capitellum and proximal ulna, potentially leading to a more functional elbow joint. Outcomes are generally superior to delayed excision. Techniques reported include proximal ulnar osteotomy, with or without annular ligament reconstruction, and radial shortening (20, 21). We achieved satisfactory results using isolated proximal ulnar osteotomy for reduction, without annular ligament reconstruction. We believe that precise correction of the bony deformity is paramount for maintaining radial head reduction.
We intentionally did not perform annular ligament reconstruction as part of our surgical approach. Our core principle was that a stable, anatomical reduction of the radial head via precise ulnar osteotomy was the foundation of treatment. In our cohort, this method-using temporary K-wire fixation only if instability was detected after the bony correction-produced excellent radiographic outcomes with no re-dislocations. This success indicates that ligament reconstruction is likely unnecessary when stable bony alignment is achieved, which simplifies the surgery and can reduce morbidity. Our results align with a growing body of literature that supports the efficacy of isolated bony procedures (18, 20).
Operative findings corroborated the value of arthrography by revealing a clear pathological profile. Congenital cases were uniformly characterized by a lack of scar tissue and a shallow, flat radial head fovea. In contrast, traumatic cases invariably featured scar tissue and a distinct fovea. This morphological distinction, supported by preoperative radiographic differences (Table 1), was dynamically confirmed by arthrography during surgery. Furthermore, we noted that an extracapsular position of the radial head, identified intraoperatively in three traumatic cases, was correlated with more severe instability-all three required trans-articular K-wire fixation. Consequently, the arthrography finding of an extracapsular radial head appears to be a valuable indicator of the potential need for additional stabilization.
This study has several limitations. Its retrospective, single-center design and small sample size limit the generalizability of the findings. The gender distribution is imbalanced. The lack of a control group managed without arthrography prevents a direct measurement of its added value. Furthermore, the assessment of functional outcomes was not standardized with validated scores, relying instead on clinical observation and absence of complications. Future prospective, multi-center studies with larger cohorts, long-term follow-up, and detailed functional assessments are warranted to further validate these findings.
Conclusion
Elbow arthrography serves as a valuable adjunct for differentiating between congenital and traumatic radial head dislocations, thereby informing both surgical strategy and the decision for supplemental fixation. When stable bony alignment is achieved, proximal ulnar osteotomy without annular ligament reconstruction represents an effective management strategy for chronic radial head dislocation in children.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Northwest women's and Children's Hospital Committee Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
HJ: Data curation, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. TL: Conceptualization, Formal analysis, Supervision, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gryson T, Van Tongel A, Plasschaert F. The management of chronic paediatric Monteggia fracture-dislocation. J Orthop. (2021) 24:65–76. doi: 10.1016/j.jor.2021.02.009
2. Tan SHS, Low JY, Chen H, Tan JYH, Lim AKS, Hui JH. Surgical management of missed pediatric Monteggia fractures: a systematic review and meta-analysis. J Orthop Trauma. (2022) 36(2):65–73. doi: 10.1097/BOT.0000000000002219
3. Ko KR, Shim JS, Park J, Won J. Predictors of ideal outcomes after reconstructive surgery for chronic Monteggia fracture in children. J Orthop Sci. (2022) 27(5):1025–31. doi: 10.1016/j.jos.2021.06.009
4. Al-Qattan MM, Abou Al-Shaar H, Alkattan WM. The pathogenesis of congenital radial head dislocation/subluxation. Gene. (2016) 586(1):69–76. doi: 10.1016/j.gene.2016.04.002
5. Oka K, Tanaka H, Shigi A, Abe S, Miyamura S, Shiode R, et al. Quantitative analysis for the change in lengths of the radius and Ulna in missed bado type I Monteggia fracture. J Pediatr Orthop. (2020) 40(10):e922–26. doi: 10.1097/BPO.0000000000001648
6. Loose O, Morrison SG, Langendoerfer M, Eberhardt O, Wirth T, Fernandez FF. Radial head distalisation with an external ring fixator as a therapy option in children with chronic posttraumatic radiocapitellar dislocations. Eur J Trauma Emerg Surg. (2023) 49(4):1803–10. doi: 10.1007/s00068-022-02173-w
7. Zivanovic D, Marjanovic Z, Bojovic N, Djordjevic I, Zecevic M, Budic I. Neglected Monteggia fractures in children-A retrospective study. Children (Basel). (2022) 9(8):1100. doi: 10.3390/children9081100
8. Eamsobhana P, Chalayon O, Kaewpornsawan K, Ariyawatkul T. Missed Monteggia fracture dislocations treated by open reduction of the radial head. Bone Joint J. (2018) 100-B(8):1117–24. doi: 10.1302/0301-620X.100B8.BJJ-2017-0866.R3
9. Xu P, Zhang Z, Ning B, Wang D. Outcomes and experience after open reduction for chronic Monteggia fracture in children. Transl Pediatr. (2022) 11(7):1122–9. doi: 10.21037/tp-21-614
10. Soni JF, Valenza WR, Pavelec AC. Chronic Monteggia. Curr Opin Pediatr. (2019) 31(1):54–60. doi: 10.1097/MOP.0000000000000710
11. Rehm A, Ngu A, Thahir A. Does an elbow arthrogram change management after closed reduction of mildly displaced lateral condyle fractures in children? J Pediatr Orthop B. (2022) 31(3):310–2. doi: 10.1097/BPB.0000000000000928
12. Chou ACC, Wong HYK, Kumar S, Mahadev A. Using the medial and lateral humeral lines as an adjunct to intraoperative elbow arthrography to guide intraoperative reduction and fixation of distal humerus physeal separations reduces the incidence of postoperative cubitus varus. J Pediatr Orthop. (2018) 38(5):e262–6. doi: 10.1097/BPO.0000000000001156
13. Cha SM, Shin HD, Choi ES. Long-term outcomes of distal humeral epiphyseal separations treated via closed reduction and pinning under arthrogram. Injury. (2020) 51(2):207–11. doi: 10.1016/j.injury.2019.11.038
14. Tomori Y, Nanno M, Takai S. Posteromedial elbow dislocation with lateral humeral condylar fracture in children: three case reports and a literature review. Medicine (Baltimore). (2018) 97(36):e12182. doi: 10.1097/MD.0000000000012182
15. Yamazaki H, Kato H. Open reduction of the radial head with ulnar osteotomy and annular ligament reconstruction for bilateral congenital radial head dislocation: a case with long-term follow-up. J Hand Surg Eur Vol. (2007) 32(1):93–7. doi: 10.1016/j.jhsb.2006.09.003
16. Kosay C, Akcali O, Manisali M, Ozaksoy D, Ozcan C. Congenital anterior dislocation of the radial head: a case with radiographic findings identical to traumatic dislocation. Eur J Radiol. (2002) 43(1):57–60. doi: 10.1016/s0720-048x(01)00424-7
17. Bengard MJ, Calfee RP, Steffen JA, Goldfarb CA. Intermediate-term to long-term outcome of surgically and nonsurgically treated congenital, isolated radial head dislocation. J Hand Surg Am. (2012) 37(12):2495–501. doi: 10.1016/j.jhsa.2012.08.032
18. Gao J, Tang J, Li M, Li H, Peng Y, Wang C, et al. Bilateral anterior congenital radial head dislocation in adults: a case report and literature review. Front Surg. (2023) 10:1155461. doi: 10.3389/fsurg.2023.1155461
19. Liu R, Miao W, Mu M, Wu G, Qu J, Wu Y. Ulnar rotation osteotomy for congenital radial head dislocation. J Hand Surg Am. (2015) 40(9):1769–75. doi: 10.1016/j.jhsa.2015.06.005
20. Karuppal R, Marthya A, Raman RV, Somasundaran S. Case report: congenital dislocation of the radial head -a two-in-one approach. F1000Res. (2014) 3:22. doi: 10.12688/f1000research.3-22.v1
Keywords: elbow arthrography, children, radial head, dislocation, diagnosis
Citation: Jiang H and Li T (2025) Application value of elbow arthrography in the treatment of chronic radial head dislocation in children. Front. Pediatr. 13:1645613. doi: 10.3389/fped.2025.1645613
Received: 12 June 2025; Accepted: 30 October 2025;
Published: 14 November 2025.
Edited by:
Xin Tang, Zhejiang University, ChinaReviewed by:
Adrian Surd, University of Medicine & PHarmacy "Iuliu Hațieganu", RomaniaMarwa Raafat Kamal Ibrahim, Alexandria University, Egypt
Copyright: © 2025 Jiang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Li, MTU3NzcxMDlAcXEuY29t
 Hai Jiang
Hai Jiang Tao Li*
Tao Li*