- 1Division of Neonatology, Department of Pediatrics, University of Illinois College of Medicine Peoria, Peoria, Illinois
- 2OSF Children's Hospital of Illinois, Peoria, Illinois
- 3Department of Pediatrics, University of Illinois College of Medicine Peoria, Peoria, Illinois
- 4University of Illinois College of Medicine Peoria, Peoria, Illinois
Background: Advancements in prenatal diagnosis and obstetric care have changed the epidemiology of neonatal birth trauma in developed countries. Improving women's access to health care is key to preventing, detecting, and treating conditions that increase pregnancy complications and adverse neonatal outcomes.
Objective: To identify new risk factors—focusing on social determinants of health—and short-term outcomes associated with neonatal birth trauma.
Study design: Term neonates with unexpected complications born between January 1, 2019, and March 31, 2023, at 10 diverse hospitals in our health system were identified using Perinatal Care-06 coding. Maternal and neonatal charts were reviewed and recorded in REDCap. Neonates with and without birth trauma were assigned to case and control groups, respectively. Risk factors were identified using Pearson chi-square tests and multivariable logistic regression.
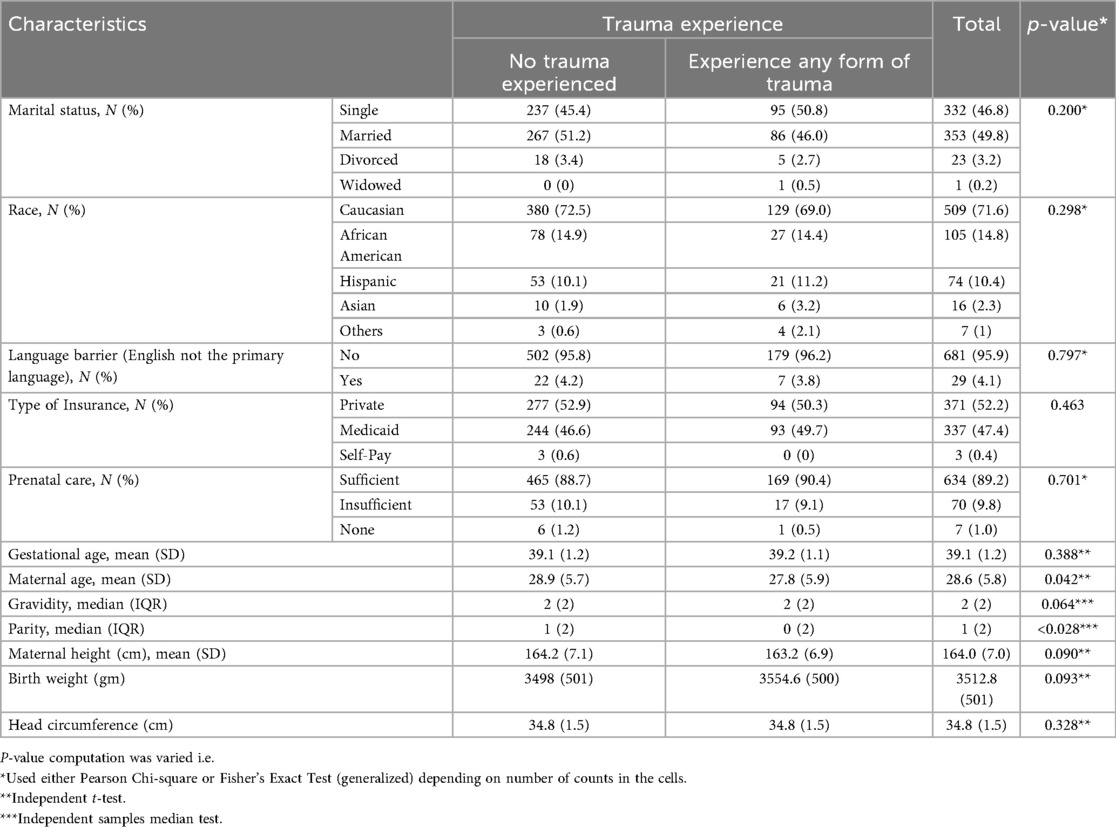
Results: Of 711 neonates, 187 (26.3%) experienced birth trauma, primarily scalp injuries (Caput Succedaneum 42%, Ecchymosis/Bruising 27%). There were no significant differences in race, language barriers, insurance type, marital status, prenatal care access, mean household income (zip code), gestational age, maternal height, birth weight, or head circumference (all p > 0.05). Significant differences were observed in maternal age (p = 0.042), gravidity (p = 0.04), and parity (p = 0.002), with affected mothers being younger, with fewer pregnancies and lower parity. Mothers with chronic or gestational hypertension, with or without preeclampsia, had higher odds of neonatal birth trauma (OR = 1.582, 95% CI: 1.081–2.316, p = 0.018). Emergent deliveries nearly tripled the odds (OR = 2.8, 95% CI: 1.934–4.054, p < 0.001). Neonates exposed to maternal epidural anesthesia were more likely to suffer from birth trauma (77.5 vs. 51.7%, p < 0.001).
Conclusion: Social determinants and prenatal care access did not significantly impact birth trauma. However, hypertension, exposure to epidural anesthesia and emergent delivery were associated with an increased risk.
Introduction
Birth trauma, often interchanged with birth injury, is defined as any trauma occurring during the process of labor, delivery or neonatal resuscitation leading to structural and/or functional damage of the neonate's body (1–4). These events range from minor injuries such as skin lacerations to major life-threatening injuries such as subgaleal hemorrhage, leading to significant morbidity and mortality (2). Up to 37 birth traumas per 1,000 births have been reported in a few population-based studies conducted (4). The quality of obstetric care is often measured by the rate of birth trauma. Parents frequently believe that birth traumas can be avoided, and when they occur, it can result in feelings of anger, frustration, and, in some cases, legal action (5).
Risk factors identified for neonatal birth traumas can be categorized into maternal factors, fetal factors and the application of instrumentation during delivery (6). Maternal factors that may contribute to neonatal birth trauma include young and old maternal age, parity, poor maternal health, and abnormalities in the shape or size of pelvis. Fetal factors that may contribute to birth trauma include macrosomia, fetal weight and height, prematurity and postdates. Labor and delivery related factors include prolonged labor, fetal malpresentation and malposition, cesarean, and instrumental deliveries (7).
The epidemiology of risk factors has changed over the last two decades as the number of instrumental deliveries has decreased (8). Cesarean deliveries, a protective factor for birth trauma (9), have increased owing to increasing incidence of large for gestational age (LGA) neonates secondary to maternal obesity and gestational diabetes (10). Along with obesity, diabetes, and hypertension before and during pregnancy, the rise in cesarean deliveries has also been associated with increasing maternal morbidity (11). Cesarean deliveries have been associated with increased neonatal intensive care unit admissions (12) along with lower rates and early cessation of breast feeding secondary to delayed milk production (13) and postoperative pain (14).
Improving a woman's access to health care during her reproductive years is essential for the prevention, early detection, and treatment of conditions that could otherwise lead to pregnancy-related complications and increased infant mortality (15). Maternal morbidity rates remain disproportionately higher among Black and Hispanic women compared to their Caucasian counterparts. Similarly, women who are uninsured or enrolled in Medicaid exhibit higher morbidity rates than those with private insurance coverage (16). These disparities underscore the significant impact of social determinants of health (SDOH)—factors that influence how individuals grow, live, work, and perceive control over their environment (17). Addressing these determinants is crucial in reducing health inequities and improving maternal and neonatal outcomes across diverse populations.
Advancements in prenatal diagnosis and improvements in obstetric care have made it possible to identify risk factors for most birth traumas in neonates. However, it becomes difficult to predict and prevent birth traumas without identifiable risk factors (5). Therefore, knowledge of the pattern of birth traumas and the related risk factors can benefit both obstetricians and the pediatrician/neonatologist in case management and prognostication. Our study aims to identify new risk factors focusing on SDOH and outcomes associated with neonatal birth trauma.
Materials and methods
Study design and period
This retrospective cohort study investigated term neonates born at ≥37 + 0/7 weeks gestational age with unexpected complications at birth between January 1, 2019, and March 31, 2023. Data was collected from 10 diverse OSF hospitals across the states of Illinois and Michigan. Nine of the hospitals were in the state of Illinois that included St. Francis Medical Center in Peoria, St. Joseph Medical Center in Bloomington, Sacred Heart Medical Center in Danville, St. Mary Medical Center in Galesburg, Heart of Mary Medical Center in Urbana, St. James Medical Center in Pontiac, St. Elizabeth Medical Center in Ottawa, St. Anthony Medical Center in Rockford, Little Company of Mary in Chicago. The final hospital was St. Francis Hospital in Escanaba, Michigan. Maternal and neonatal medical records were thoroughly reviewed to gather comprehensive demographic, clinical, and outcome data.
Data management
Data was securely captured in REDCap, a web-based platform managed by the University of Illinois at Chicago's Center for Clinical and Translational Science. After abstraction for 711 patients, the dataset was downloaded into Excel and subsequently exported to IBM SPSS for data cleaning and analysis. The study included all neonatal births at the participating hospitals during the study period, and no data points were excluded.
Inclusion criteria
Term neonates born at ≥37 + 0/7 weeks gestational age at the 10 OSF hospitals. These hospitals ranged from having a Level 1 Newborn Nursery to a Level 4 neonatal intensive care unit.
Exclusion criteria
Preterm neonates born ≤36 + 6/7 weeks gestational age. Also, those born at home or with pre-existing conditions or congenital malformations were excluded.
Source and study population
Source population
Term neonates with no preexisting conditions who experienced unexpected complications were identified using the Perinatal Care-06 coding.
Study population
Term neonates with no preexisting conditions who experienced birth trauma.
Outcome Variable
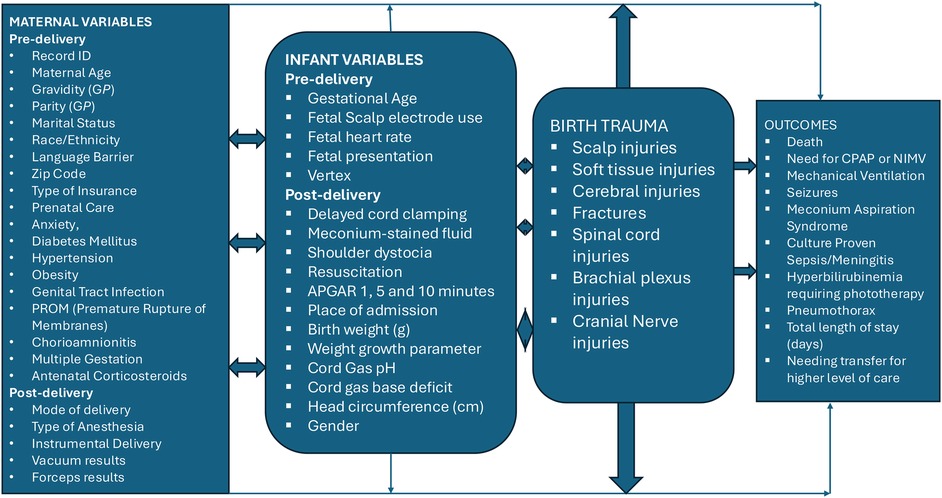
The primary outcome of the study was birth trauma, defined as the presence of one or more injuries sustained during delivery. These injuries were categorized (1) as follows:
Scalp injuries
Included cephalohematoma, caput succedaneum, subgaleal hemorrhage, and other scalp lesions.
Soft tissue injuries
Included erythema, abrasions, petechiae, ecchymoses (bruising), subcutaneous fat necrosis and lacerations.
Cerebral injuries
Included subdural, subarachnoid, tentorial, intraventricular, and intracranial hemorrhages.
Fractures
Included skull, clavicle and long bone fractures.
Spinal cord injuries
Brachial plexus injuries
caused by stretching of the cervical nerve roots from traction on the neck during delivery. These include upper arm palsy (Erb-Duchenne), lower arm palsy (Klumpke) and Horner's syndrome.
Cranial nerve injuries
Other neonatal outcomes of interest included neonatal death, need for respiratory support including continuous positive airway pressure (CPAP) or non-invasive mechanical ventilation (NIMV) or invasive mechanical ventilation, seizures, hypoxic-ischemic encephalopathy (HIE), meconium aspiration syndrome (MAS), culture-proven sepsis/meningitis, hyperbilirubinemia requiring phototherapy, pneumothorax, total length of stay, and transfer to higher-level care.
Data collection
This retrospective study utilized patient medical records to obtain detailed maternal, labor and delivery, and neonatal variables. All data collection procedures adhered to Institutional Review Board (IRB) protocols. Data were entered into REDCap, a secure, web-based platform administered by the University of Illinois College of Medicine, and underwent rigorous cleaning to ensure completeness, accuracy, and standardized coding before statistical analysis.
See details on variables in Figure 1 below.
Data analysis
Descriptive statistics were used to summarize study variables. For continuous variables, means and standard deviations were calculated, while counts and percentages were used for categorical data. Categorical data analysis included Pearson's chi-square test assessed associations between neonatal birth trauma and categorical predictors and independent unpaired t-tests (with unequal variance) compared continuous variables. A multivariable logistic regression was performed using a conditional forward approach to identify predictors of birth trauma. Key confounders, including maternal age, gestational age, and prenatal care status, were adjusted in the final models. A contingency table (2 × 2) was constructed to compare the exposure and outcome variables of interest. The odds ratio (OR) and corresponding 95% confidence interval (CI) were calculated to quantify the strength and direction of the association between exposure and outcome. Given the small cell counts in the table, the exact method was applied to obtain both the OR and its CI, ensuring accurate estimation without reliance on large-sample assumptions. Fisher's exact test was used to assess statistical significance. A p-value <0.05 was considered statistically significant. All statistical analyses were conducted using IBM SPSS Statistics version 20.
Results
Of the 711 records, we found 187 (26.3%) records with birth trauma. Neonates with and without birth trauma were assigned to the case and control group respectively. There were no significant differences between the groups in terms of race, language barrier, type of insurance, marital status, prenatal care, maternal height, birth weight and head circumference (all p-values >0.05). The independent median test was applied to compare the central tendency of gravidity and parity between participants with and without a history of trauma. This nonparametric test was chosen because these variables were expressed as medians with interquartile ranges (IQR), indicating non-normal distributions. Gravidity did not differ significantly between groups [median (IQR): 2 (2) in both; p = 0.064]. In contrast, parity showed a statistically significant difference, with lower median parity among those who had experienced trauma [median (IQR): 0 (2)] compared to those without trauma [median (IQR): 1 (2); p = 0.028] (Table 1).
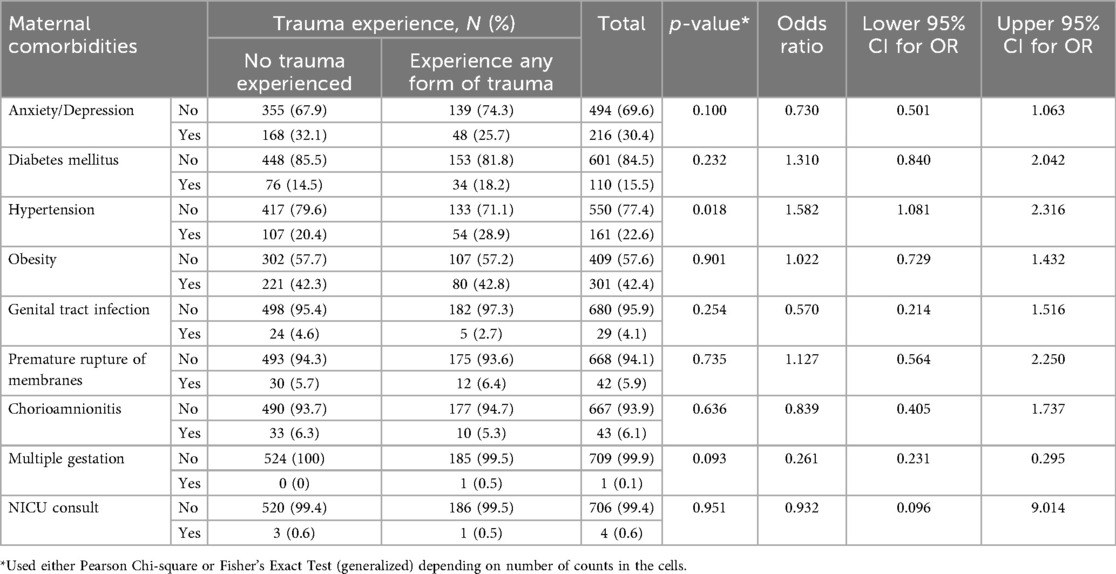
Maternal comorbidities and labor/delivery variables
There were no significant differences between the groups in terms of mothers with anxiety or depression, diabetes, obesity, genital tract infection, premature rupture of membranes, chorioamnionitis, multiple gestation, needing antenatal corticosteroids or neonatology consult (all p-values >0.05). However, chronic or gestational hypertension with or without pre-eclampsia was more prevalent in mothers that delivered neonates with birth trauma compared to those without birth trauma (28.9% vs. 20.4%, p = 0.018). The odds for mothers to be hypertensive were 1.582 times higher (95% CI: 1.081–2.316), indicating a potential association between hypertension and neonatal birth trauma (Table 2).
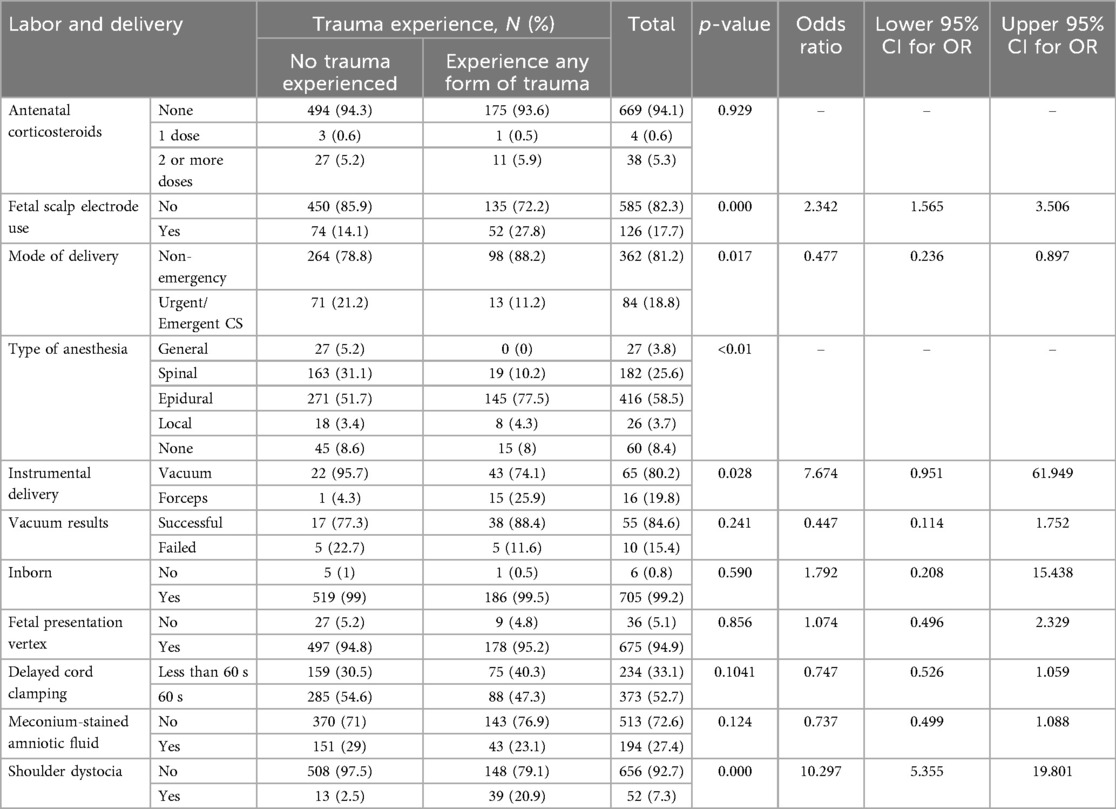
Mothers with history of FSE electrode use had significantly higher odds of having neonates with birth trauma (OR = 2.342, 95% CI: 1.565–3.506, p < 0.001). There was a statistically significant association between the type of anesthesia used during delivery and the experience of birth trauma (p < 0.001). Notably, 77.5% of neonates who experienced any form of trauma were born to mothers who received epidural anesthesia, compared to 51.7% in the non-trauma group. None of the mothers who received general anesthesia had neonates with birth trauma, despite representing 5.2% of the non-trauma group. Smaller proportions of trauma cases were also observed among those who received spinal (10.2%), local (4.3%), or no anesthesia (8%). Neonates born via operative vaginal delivery (vacuum or forceps-assisted delivery) had significantly higher odds of having birth trauma (OR = 7.674, 95% CI: 0.951–61.949, p = 0.028). Emergent deliveries nearly tripled the odds of having neonates with birth trauma (OR = 2.8, 95% CI: 1.934–4.054, p < 0.001). Neonates with shoulder dystocia had significantly higher odds of having birth trauma (OR = 10.297, 95% CI: 5.355–19.801, p < 0.001). There were no significant differences between the groups in terms of fetal presentation, meconium-stained amniotic fluid and delayed cord clamping (p-values >0.05). Given the distribution of ACS use across trauma groups—None: 94.3%, 1 dose: 0.6%, 2+ doses: 5.2% in the no-trauma group vs. None: 93.6%, 1 dose: 0.5%, 2+ doses: 5.9% in the trauma group—and a non-significant p-value of 0.929, ACS use does not appear to be associated with neonatal trauma in this dataset. Among the 711 neonates, resuscitation patterns differed slightly between those who experienced birth trauma and those who did not. The most common intervention was CPAP plus drying and stimulation, used in 70% of all cases (71% no trauma vs. 67% trauma). Basic resuscitation with just drying and stimulation was more common in the trauma group (56%) than in the non-trauma group (51%). More intensive interventions, such as intubation and chest compressions, were slightly more frequent among those with trauma (e.g., 30% vs. 27% for intubation; 3% vs. 3% for chest compressions). Although higher levels of resuscitation were used in both groups, there was no major difference, suggesting a modest association between trauma experience and the intensity of neonatal resuscitation (Table 3).
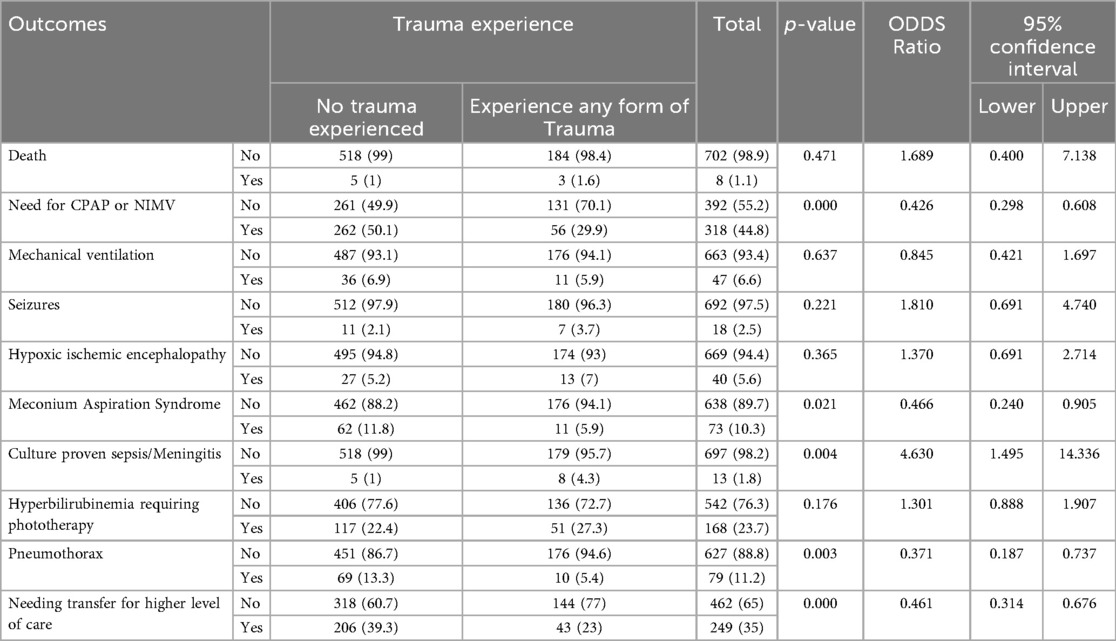
Neonatal outcomes
Of the 711 neonates, 187 (26.3%) experienced birth trauma, primarily scalp injuries (Caput Succedaneum 42%, Ecchymosis and Bruising 27%). These were primarily scalp injuries followed by soft tissue injuries, brachial plexus injury, clavicular fracture, others, cerebral injuries, fracture of long bones, cranial nerve injury, and skull fracture (Figure 2). There were no significant differences between the groups in terms of death, mechanical ventilation, hyperbilirubinemia needing phototherapy, seizures and HIE. Neonates with birth trauma were less likely to require respiratory support in the form of continuous positive airway pressure or non-invasive mechanical ventilation (29.9% vs. 50.1%, p < 0.001). Meconium Aspiration Syndrome was significantly less common among neonates who experienced any form of trauma compared to those who did not (5.9% vs. 11.8%, p = 0.021). The odds of experiencing trauma were reduced by more than half in the presence of MAS, with an odds ratio of 0.466. Neonates who experienced trauma were significantly less likely to develop pneumothorax compared with those without trauma (5.4% vs. 13.3%, p = 0.003). The odds of pneumothorax were 63% lower in this group (OR = 0.37). In contrast, neonates with birth trauma were over four times more likely to develop culture-proven sepsis or meningitis (4.3% vs. 1.0%, p = 0.004). We acknowledge that the higher-than-expected pneumothorax rate in our cohort may reflect contributing factors such as ventilation practices, underlying lung pathology, or selection bias. The observed association between lower pneumothorax rates and trauma cases may also be related to the involvement of more experienced providers, though this remains speculative. Those with birth trauma were less likely to require transfer to a higher-level of care facility (23% vs. 39.3%, p < 0.001) (Table 4).
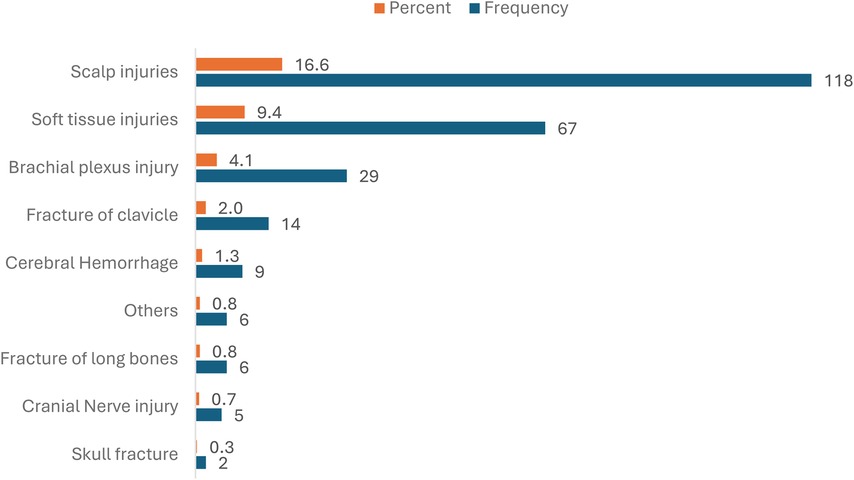
Figure 2. Types of birth trauma. **There were 256 birth injuries noted with 187 neonates having at least 1 birth injury. See Supplementary Table S1.
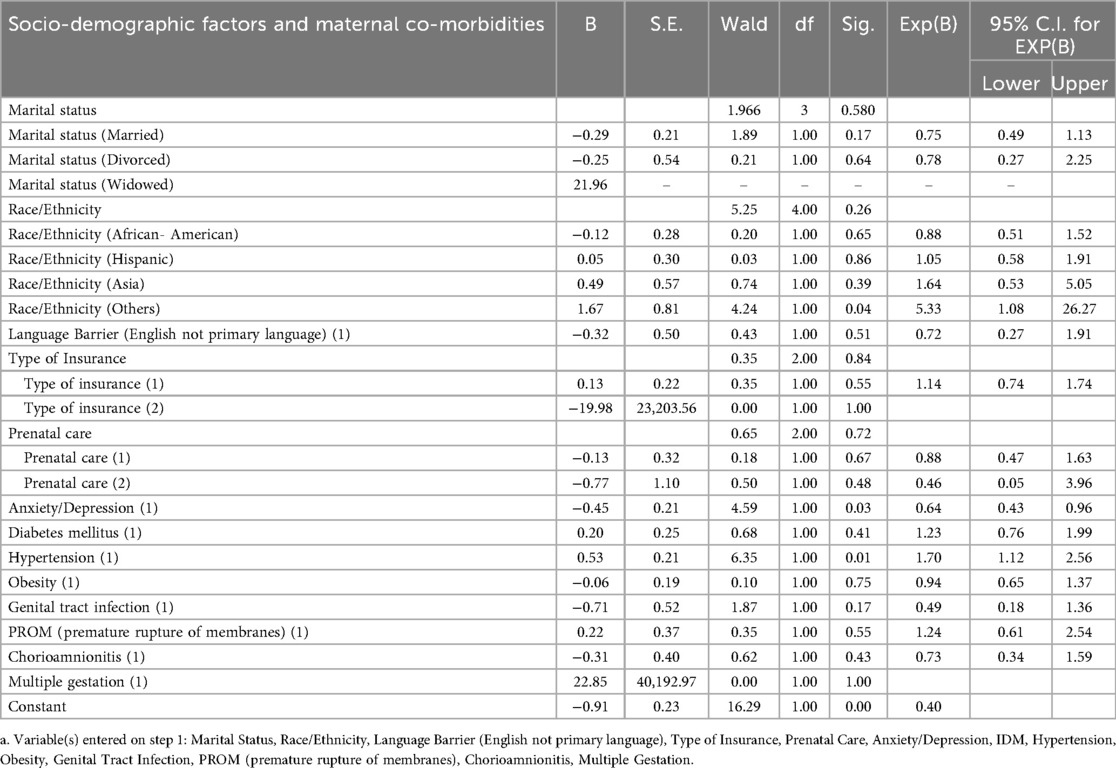
Logistic regression
The logistic regression analysis (Table 5) examining factors associated with birth trauma, compared to no trauma, included maternal sociodemographic, obstetric, and medical variables. After adjusting for all predictors, significant associations were observed for race/ethnicity, anxiety/depression, and hypertensive disorders. Mothers identifying as Race/Ethnicity group 4 had over five times the odds of experiencing birth trauma compared to the reference group (OR = 5.33, 95% CI: 1.08–26.27, p = 0.04). A history of anxiety or depression was associated with a 36% reduction in the odds of birth trauma (OR = 0.64, 95% CI: 0.43–0.96, p = 0.03). Conversely, chronic hypertension, gestational hypertension, or preeclampsia increased the odds of birth trauma by 70% (OR = 1.70, 95% CI: 1.12–2.56, p = 0.01). All other variables, including marital status, language barrier, type of insurance, prenatal care, obesity, genital tract infection, PROM, chorioamnionitis, and multiple gestation, were not statistically significant predictors in the model.
Discussion
The incidence of major birth trauma, such as non-scalp injuries, has decreased over the years (2, 18). This study showed that scalp injuries were the most common form of neonatal birth trauma. Although previously considered benign, scalp injuries have been associated with increased morbidity, including longer hospital stays and, consequently, higher hospital charges (2). In our study, neonates who experienced birth trauma were less likely to require transfer to a higher-level care facility (23% vs. 39.3%, p < 0.001). Scalp injuries, being the most common in our study and generally benign in nature, may explain this finding.
Our study found that mothers who delivered neonates with birth trauma were younger, had fewer pregnancies, and had lower parity. Younger maternal age has been associated with skeletal immaturity and tighter pelvic musculature, which may contribute to birth trauma in some populations (7, 19, 20). However, in our cohort, the mean age (28.9 vs. 27.8 years, p = 0.042) and height (164.2 vs. 163.2 cm, p = 0.09) differences between groups fall within the range of full skeletal maturity and above thresholds typically linked to cephalopelvic disproportion. Thus, while the proposed mechanism is biologically plausible, these findings suggest it may not be clinically relevant in this sample and could represent a chance association.
Our initial hypothesis was that women with limited access to resources or care—such as those of lower socioeconomic status, those facing language barriers, or those without adequate prenatal care—would be at higher risk of delivering infants with birth trauma. We analyzed variables including race, presence of language barriers, type of insurance, marital status, access to prenatal care, and mean household income based on zip code. However, no statistically significant differences were observed between the groups. The six SDOH factors we selected may not fully capture the complexity of healthcare disparities, which could explain the lack of observed differences. A prospective study would allow for more comprehensive data collection, including variables not typically documented in medical records. Incorporating tools such as the Social Vulnerability Index, as used in a Canadian study (21), may provide deeper insight into the relationship between social factors and birth trauma. The hospital network involved in this study comprises nine locations in Central Illinois and one in Michigan, encompassing rural, suburban, and urban centers. Of these, eight facilities are equipped to provide Level II newborn nursery care, one offers only Level I care, and the primary hospital within the network can provide Level IV NICU services. For ease of data collection, our study included only neonates with unexpected complications. Expanding future research to include healthy neonates—thereby increasing the sample size—may offer a completer and more representative picture of potential disparities. Since the time of data collection, several smaller facilities in the region have closed, resulting in the emergence of obstetric care deserts. We emphasize the critical importance of maintaining access to local obstetric services to ensure optimal outcomes for both mothers and their infants.
In the U.S., up to 10% of pregnancies are affected by maternal hypertension (22, 23). These women are at increased risk for obstetric interventions such as earlier induction of labor or undergoing cesarean section. Since the neonates are physiologically less ready for birth, they have a higher risk of morbidities such as preterm birth, low birth weight, respiratory distress syndrome, and sepsis, leading to an increased need for NICU admission (24). Our study found that chronic or gestational hypertension, with or without pre-eclampsia, was more prevalent among mothers who delivered neonates with birth trauma compared to those without. To our knowledge, no previous studies have demonstrated an association between maternal hypertension and neonatal birth trauma.
About 20% of deliveries in the U.S. involve the use of FSE. It is an important tool for intrapartum fetal surveillance, particularly in cases of non-reassuring fetal heart rate tracings or when external monitoring is difficult due to maternal body habits or excessive fetal movement (25). However, FSE use increases the risk of scalp injury, cephalohematoma, and neonatal sepsis, regardless of the mode of delivery (1, 25). Our study also found that mothers with a history of FSE use had twice the odds of delivering neonates with birth trauma.
Shoulder dystocia, an obstetric emergency, occurs in up to 1% of spontaneous vaginal deliveries and 9% of operative vaginal deliveries (26, 27). It has been associated with brachial plexus injuries, fractures, and adverse neonatal outcomes such as HIE and death (1, 28). Our study similarly found that neonates who experienced shoulder dystocia had ten times higher odds of sustaining birth trauma.
The association between epidural analgesia and birth trauma observed in our study warrants further exploration. Among neonates who experienced birth trauma, 77.5% were born to mothers who received epidural anesthesia, compared to 51.7% in the non-trauma group. This disparity may be attributed to factors such as prolonged second stage of labor, abnormal fetal head position, and increased frequency of operative vaginal deliveries or cesarean sections (29–31). Although our dataset did not include detailed labor duration metrics, existing literature suggests that epidural analgesia is associated with longer second stage labor and a higher incidence of instrumental delivery—both of which are established risk factors for neonatal trauma.
Despite these associations, the overall risk to neonates exposed to maternal epidural anesthesia remains low. However, short-term effects such as lower Apgar scores at 1 and 5 min, increased need for resuscitation, higher NICU admission rates, and delayed initiation of breastfeeding have been reported (29–32). These results underscore the importance of careful intrapartum management and informed decision-making regarding analgesia use during labor.
Operative vaginal deliveries, such as those involving forceps or vacuum extraction, have been major risk factors for birth trauma. Common injuries—including scalp edema, bruising, cephalohematoma, subgaleal hemorrhage, and intracranial hemorrhage—are more prevalent with unsuccessful extractions (33, 34). Our study found that neonates born via operative vaginal delivery or emergent cesarean section had significantly higher odds of experiencing birth trauma. However, when vacuum and forceps deliveries were analyzed separately, we did not find a significant association between failed extraction and birth trauma.
Non-scalp injuries have been associated with higher odds of transient tachypnea of the newborn, meconium aspiration, respiratory distress syndrome, the need for CPAP or mechanical ventilation, HIE, seizures, and sepsis. Scalp injuries have additionally been shown to increase the odds of hyperbilirubinemia (2, 35). Our study found that neonates with birth trauma were less likely to require respiratory support, such as continuous positive airway pressure or non-invasive mechanical ventilation. Scalp injuries, which were the most common type of birth trauma in our study group, may explain the lower likelihood of requiring respiratory support. In contrast, the control group included neonates with unexpected complications, which may account for the observed association. Also, those with birth trauma were over four times more likely to have culture-proven sepsis or meningitis compared to those who did not experience trauma.
Meconium-stained amniotic fluid is a condition that requires notification and the presence of a Neonatal Advanced Life Support (NALS)-credentialed provider at delivery (36). In our study, the odds of experiencing birth trauma were reduced by more than half in the presence of MAS compared to those without MAS (5.9% vs. 11.8%, p = 0.021). This may be attributed to the advanced resuscitation skills of the provider attending. Additionally, neonates with birth trauma were significantly less likely to develop a pneumothorax compared to those without trauma (5.4% vs. 13.3%, p = 0.003). We hypothesize that this, too, may be due to the involvement of highly skilled providers, who are more likely to be present at high-risk deliveries such as cesarean sections and operative vaginal deliveries among others.
Strength and limitations of this study
This study was conducted across 10 locations representing a mix of rural, suburban, and urban centers. These sites served populations with diverse socioeconomic backgrounds and offered varying levels of neonatal care. A key strength of the study lies in the diversity of settings and patient populations, which enhances the generalizability of the findings within the region.
However, several limitations should be acknowledged. First, the study was limited to the Midwest region, which may affect the applicability of the results to other geographic areas. As a retrospective study, data collection relied on the accuracy and completeness of existing medical records, which introduces potential variability. Additionally, the providers attending deliveries varied across sites and included general pediatricians, neonatal nurse practitioners, and neonatal fellows. In some locations, initial resuscitation efforts were initiated by obstetric staff before more advanced neonatal providers arrived, potentially contributing to inconsistencies in care across the network.
Selection bias is another important limitation. Rather than include all neonates born during the study period, we focused only on those with unexpected complications requiring admission to the Special Care Nursery or NICU. This enriched our study population with higher-risk neonates, which may make the observed rate of birth trauma appear higher than in a general newborn population. Moreover, this approach may have affected the distribution of social determinants of health (SDOH), as differences between complicated neonates with and without trauma are likely smaller than those between healthy neonates and those who experience trauma. While this decision was made in part to reduce the chart review burden, it introduces a potential source of selection bias that should be considered when interpreting the results.
Conclusion
This study highlights important associations between maternal and labor/delivery factors and neonatal birth trauma. Factors such as young maternal age, low gravidity and parity, use of FSE, shoulder dystocia, and operative vaginal deliveries have been documented in the literature. However, SDOH did not appear to influence the incidence of neonatal birth trauma. The associations with maternal hypertension and epidural anesthesia warrant further investigation.
These findings can benefit both obstetricians and pediatricians/neonatologists in case management and prognostication, allowing for more informed decision-making and tailored care strategies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was approved by the Institutional Review Board of the University of Illinois College of Medicine at Peoria (UICOM Peoria). A waiver of informed consent was granted, as the study was observational in nature and involved the collection of only limited patient identifiable data.
Author contributions
NP: Data curation, Writing – original draft, Writing – review & editing, Formal analysis, Funding acquisition. CO: Formal analysis, Methodology, Writing – review & editing. HM: Formal analysis, Data curation, Writing – original draft. GB: Data curation, Formal analysis, Writing – original draft. AC: Writing – review & editing, Formal analysis, Methodology, Supervision. GK: Conceptualization, Funding acquisition, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This project was internally funded through the Community Health Advocacy (CHA) award, a collaborative grant mechanism between OSF HealthCare and the University of Illinois Chicago.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2025.1648252/full#supplementary-material
Abbreviations
LGA, large for gestational age; SDOH, social determinants of health; CPAP, continuous positive airway pressure; NIMV, non-invasive mechanical ventilation; HIE, hypoxic-ischemic encephalopathy; MAS, meconium aspiration syndrome; FSE, fetal scalp electrode; NICU, neonatal intensive care unit; OR, odds ratio; CI, confidence interval; NALS, neonatal advanced life support.
References
1. Akangire G, Carter B. Birth injuries in neonates. Pediatr Rev. (2016) 37(11):451–62. doi: 10.1542/pir.2015-0125
2. Gupta R, Cabacungan ET. Neonatal birth trauma: analysis of yearly trends, risk factors, and outcomes. J Pediatr. (2021) 238:174–80.e3. doi: 10.1016/j.jpeds.2021.06.080
3. Woldegeorgis BZ, Gebrekidan AY, Kassie GA, Azeze GA, Asgedom YS, Alemu HB, et al. Neonatal birth trauma and associated factors in low and middle-income countries: a systematic review and meta-analysis. PLoS One. (2024) 19(3):e0298519. doi: 10.1371/journal.pone.0298519
4. Sauber-Schatz EK, Markovic N, Weiss HB, Bodnar LM, Wilson JW, Pearlman MD. Descriptive epidemiology of birth trauma in the United States in 2003. Paediatr Perinat Epidemiol. (2010) 24(2):116–24. doi: 10.1111/j.1365-3016.2009.01077.x
5. Kumar P, Papile LA, Watterberg K. Are current measures of neonatal birth trauma valid indicators of quality of care? J Perinatol. (2015) 35(11):903–6. doi: 10.1038/jp.2015.71
6. McKee-Garrett T. Delivery room emergencies due to birth injuries. Semin Fetal Neonatal Med. (2019) 24(6):101047. doi: 10.1016/j.siny.2019.101047
7. Belay AS, Negese K, Manaye GA, Debebe S. Prevalence and associated factors of birth injury among neonates admitted at neonatal intensive care unit (NICU) in governmental hospitals of southwest Ethiopian people regional state, Ethiopia: a multicenteric cross-sectional study. Front Pediatr. (2022) 10:1052396. doi: 10.3389/fped.2022.1052396
8. Mazza F, Kitchens J, Akin M, Elliot B, Fowler D, Henry E, et al. The road to zero preventable birth injuries. Jt Comm J Qual Patient Saf. (2008) 34(4):201–5. doi: 10.1016/s1553-7250(08)34025-2
9. Linder N, Linder I, Fridman E, Kouadio F, Lubin D, Merlob P, et al. Birth trauma–risk factors and short-term neonatal outcome. J Matern Fetal Neonatal Med. (2013) 26(15):1491–5. doi: 10.3109/14767058.2013.789850
10. Lavery JA, Friedman AM, Keyes KM, Wright JD, Ananth CV. Gestational diabetes in the United States: temporal changes in prevalence rates between 1979 and 2010. BJOG. (2017) 124(5):804–13. doi: 10.1111/1471-0528.14236
11. Gunja MZ, Tikkanen R, Seervai S, Collins SR. What is the Status of Women’s Health and Health Care in the United States Compared to Ten Other Countries? Commonwealth Fund (2018). doi: 10.26099/wy8a-7w13
12. Goer H, Romano A, Sakala C. Vaginal or Cesarean Birth: What is at Stake for Women and Babies? New York: Childbirth Connections (2012).
13. Hobbs AJ, Mannion CA, McDonald SW, Brockway M, Tough SC. The impact of Caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth. (2016) 16:90. doi: 10.1186/s12884-016-0876-1
14. Karlström A, Engström-Olofsson R, Norbergh KG, Sjöling M, Hildingsson I. Postoperative pain after cesarean birth affects breastfeeding and infant care. J Obstet Gynecol Neonatal Nurs. (2007) 36(5):430–40. doi: 10.1111/j.1552-6909.2007.00160.x
15. Ely DM, Driscoll AK. Infant mortality in the United States, 2017: data from the period linked birth/infant death file. Natl Vital Stat Rep. (2019) 68(10):1–20. PMID: 32501205
16. Fingar KR, Hambrick MM, Heslin KC, Moore JE. Trends and disparities in delivery hospitalizations involving severe maternal morbidity, 2006–2015. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US) (2018). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK532465/
17. World Health Organization. Social Determinants of Health: Key Concepts. United Nations. Geneva (2015). Available online at: https://www.who.int/news-room/questions-and-answers/item/social-determinants-of-health-key-concepts
18. Wen Q, Muraca GM, Ting J, Coad S, Lim KI, Lisonkova S. Temporal trends in severe maternal and neonatal trauma during childbirth: a population-based observational study. BMJ Open. (2018) 8(3):e020578. doi: 10.1136/bmjopen-2017-020578
19. Völgyi E, Tylavsky FA, Xu L, Lu J, Wang Q, Alén M, et al. Bone and body segment lengthening and widening: a 7-year follow-up study in pubertal girls. Bone. (2010) 47(4):773–82. doi: 10.1016/j.bone.2010.07.007
20. Emeka CK, Uchenna E, Tochukwu EJ, Chukwuebuka NO, Chikaodili ET, Chigozie IC. Profile of birth injuries in a tertiary hospital in Enugu, Nigeria. Am J Biomed Life Sci. (2019) 7(5):99–103. doi: 10.11648/j.ajbls.20190705.11
21. Mah JC, Theou O, Perez-Zepeda MU, Penwarden JL, Godin J, Rockwood K, et al. A standard procedure for constructing a multi-level social vulnerability index using CLSA and SOS data as working examples. PLoS One. (2024) 19(12):e0315474. doi: 10.1371/journal.pone.0315474
22. DeFreitas MJ, Griffin R, Sanderson K, Nada A, Charlton JR, Jetton JG, et al. Maternal hypertension disorders and neonatal acute kidney injury: results from the AWAKEN study. Am J Perinatol. (2024) 41(5):649–59. doi: 10.1055/a-1780-22499
23. Booker WA. Hypertensive disorders of pregnancy. Clin Perinatol. (2020) 47(4):817–33. doi: 10.1016/j.clp.2020.08.011
24. Bromfield SG, Ma Q, DeVries A, Inglis T, Gordon AS. The association between hypertensive disorders during pregnancy and maternal and neonatal outcomes: a retrospective claims analysis. BMC Pregnancy Childbirth. (2023) 23:514. doi: 10.1186/s12884-023-05818-9
25. Kawakita T, Reddy UM, Landy HJ, Iqbal SN, Huang CC, Grantz KL. Neonatal complications associated with use of fetal scalp electrode: a retrospective study. BJOG. (2016) 123(11):1797–803. doi: 10.1111/1471-0528.13817
26. Deneux-Tharaux C, Delorme P. Epidemiology of shoulder dystocia. J Gynecol Obstet Biol Reprod (Paris). (2015) 44(10):1234–47. doi: 10.1016/j.jgyn.2015.09.036
27. Nesbitt TS, Gilbert WM, Herrchen B. Shoulder dystocia and associated risk factors with macrosomic neonates born in California. Am J Obstet Gynecol. (1998) 179(2):476–80. doi: 10.1016/S0002-9378(98)70382-5
28. Mendez-Figueroa H, Hoffman MK, Grantz KL, Blackwell SC, Reddy UM, Chauhan SP. Shoulder dystocia and composite adverse outcomes for the maternal-neonatal dyad. Am J Obstet Gynecol MFM. (2021) 3(4):100359. doi: 10.1016/j.ajogmf.2021.100359
29. American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin No. 209: obstetric analgesia and anesthesia. Obstet Gynecol. (2019) 133(3):e208–25. doi: 10.1097/AOG.0000000000003132
30. Herrera-Gómez A, García-Martínez O, Ramos-Torrecillas J, De Luna-Bertos E, Ruiz C, Ocaña-Peinado FM. Retrospective study of the association between epidural analgesia during labour and complications for the newborn. Midwifery. (2015) 31(6):613–6. doi: 10.1016/j.midw.2015.02.013
31. Grobman WA, Bailit J, Lai Y, Reddy UM, Wapner RJ, Varner MW, et al. Association of the duration of active pushing with obstetric outcomes. Obstet Gynecol. (2016) 127(4):667–73. doi: 10.1097/AOG.0000000000001354
32. Penuela I, Isasi-Nebreda P, Almeida H, López M, Gomez-Sanchez E, Tamayo E. Epidural analgesia and its implications in the maternal health in a low parity comunity. BMC Pregnancy Childbirth. (2019) 19(1):52. doi: 10.1186/s12884-019-2191-0
33. Auger N, Wei SQ, Ayoub A, Luu TM. Severe neonatal birth injury: observational study of associations with operative, cesarean, and spontaneous vaginal delivery. J Obstet Gynaecol Res. (2023) 49(12):2817–24. doi: 10.1111/jog.15801
34. Ahlberg M, Norman M, Hjelmstedt A, Ekéus C. Risk factors for failed vacuum extraction and associated complications in term newborn neonates: a population-based cohort study. J Matern Fetal Neonatal Med. (2016) 29(10):1646–51. doi: 10.3109/14767058.2015.1057812
35. Chang HY, Cheng KS, Liu YP, Hung HF, Fu HW. Neonatal infected subgaleal hematoma: an unusual complication of early-onset E. coli sepsis. Pediatr Neonatol. (2015) 56(2):126–8. doi: 10.1016/j.pedneo.2013.03.003
Keywords: neonates, birth trauma, social determinants of health, risk factors, outcomes
Citation: Parikh NS, Odhiambo C, McMasters H, Borkowski GK, Cross A and Kopec G (2025) Neonatal birth trauma: identifying new risk factors and short-term outcomes. Front. Pediatr. 13:1648252. doi: 10.3389/fped.2025.1648252
Received: 16 June 2025; Accepted: 11 September 2025;
Published: 7 October 2025.
Edited by:
Licia Lugli, University Hospital of Modena, ItalyReviewed by:
Laxman Shrestha, Institute of Medicine, NepalJose Francisco Gonzalez-Zamora, National Institute of Pediatrics, Mexico
Copyright: © 2025 Parikh, Odhiambo, McMasters, Borkowski, Cross and Kopec. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nirzar Samir Parikh, cGFyaWtobmlyemFyQGdtYWlsLmNvbQ==
 Nirzar Samir Parikh
Nirzar Samir Parikh Collins Odhiambo
Collins Odhiambo Holleigh McMasters2,3
Holleigh McMasters2,3 Gretchen Kopec
Gretchen Kopec