- Department of Children’s Medical Center, Hunan Provincial People’s Hospital, The First Affiliated Hospital of Hunan Normal University, Changsha, China
Background: A cavernous hemangioma in the small intestine is rare. Due to its hidden location and non-specific clinical symptoms, it is difficult to diagnose accurately. Here, we describe a 14-year-old boy with a cavernous hemangioma and bleeding at the junction of the jejunum and ileum.
Case summary: The patient presented with clinical manifestations including melena, dizziness, fatigue, pale complexion, and shock. Abdominal contrast-enhanced computed tomography identified a hyperdense lesion within the small bowel lumen. Digital subtraction angiography (DSA) revealed aneurysmal changes in the mid-to-lower abdominal branches of the ileojejunal artery, which were suggestive of a hemorrhage originating from a small intestinal hemangioma. However, subsequent DSA-guided interventional embolization failed to achieve hemostasis. Following a hospital-wide multidisciplinary consultation, a laparoscopic exploration was conducted. During the procedure, a 1.5 cm × 1.5 cm mass was detected at the ileojejunal junction and successfully resected. The postoperative pathological examination confirmed the lesion to be a cavernous hemangioma. One week after surgery, the patient's hemoglobin level increased to 86 g/L, with no recurrence of bloody stools. At the 1-month follow-up, no signs of disease recurrence were observed.
Conclusion: This case report presents significant clinical implications for the diagnosis and management of small intestinal cavernous hemangiomas in the pediatric population.
Introduction
A small intestinal hemangioma is a rare vascular malformation, accounting for 7%–10% of all benign small intestinal tumors. Approximately 60% of cases arise in the jejunum, whereas involvement of the ileum is less frequent (1, 2). Histopathologically, these lesions are congenital vascular malformations and are categorized into capillary, cavernous, or mixed subtypes, with the cavernous variant being the most prevalent (3).
Clinically, patients may present with symptoms such as abdominal pain, gastrointestinal bleeding, intestinal obstruction, intussusception, and intestinal perforation (3–6). Owing to their non-specific clinical manifestations and the absence of definitive ancillary test findings, a misdiagnosis or missed diagnosis is common. Although recent advancements in small bowel endoscopy have enhanced detection rates, the limited accessibility to this technology across hospitals remains a contributing factor to diagnostic delays—especially in the case of rare small intestinal cavernous hemangiomas.
Case description
A 14-year-old male patient presented with a 10-day history of melena (small in amount), accompanied by dizziness, fatigue, pallor, and low-grade fever (maximum temperature of 37.7°C). He denied a history of chills, abdominal pain, or perianal pain.
Prior to admission, he underwent a gastroscopy at another hospital, which revealed chronic non-atrophic gastritis with bile reflux and erosions; concurrent laboratory testing showed a hemoglobin level of 51 g/L. The initial diagnosis at the external hospital was “iron deficiency anemia or hemorrhagic anemia,” but treatment with a blood transfusion and iron supplementation failed to improve his symptoms or anemia indices.
One day before admission, the patient developed bright red hematochezia and was subsequently transferred to our hospital. He had an unremarkable medical history and no significant medication use.
Upon admission, the patient underwent a comprehensive workup, including coagulation function tests, anemia-related panels, liver and kidney function tests, cardiac enzymes, and electrolyte assessments; all the results were within the normal reference ranges.
Despite active interventions, including fasting, administration of hemostatic agents, blood transfusion, and supportive care to stabilize vital signs, the patient continued to have persistent melena, with a progressive downward trend in hemoglobin levels.
Abdominal contrast-enhanced CT revealed a hyperattenuating lesion in the small bowel of undetermined etiology (Figure 1C). Both a gastroscopy and a colonoscopy showed no abnormalities, indicating a small intestinal bleeding source. Scintigraphy for ectopic gastric mucosa was negative.
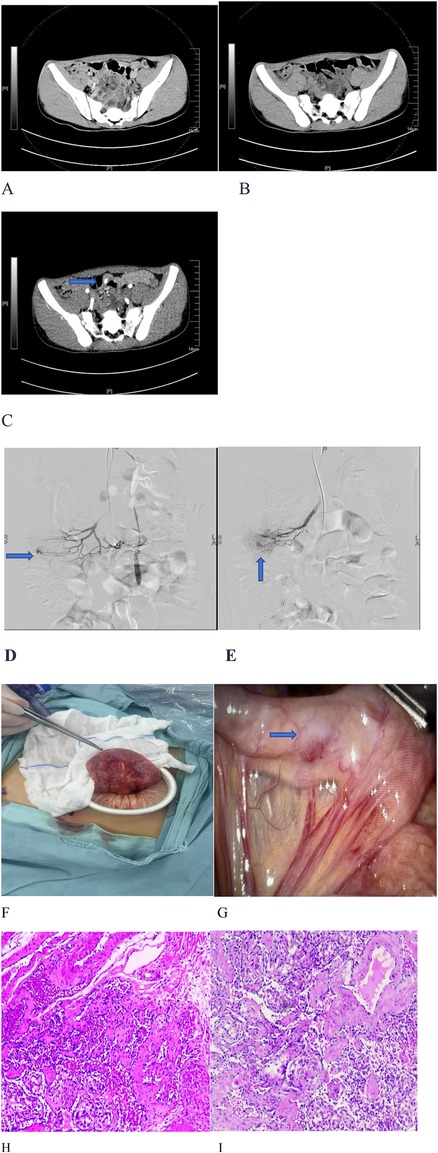
Figure 1. Imaging, angiography, surgery, and pathology of an ileal cavernous hemangioma. (A) No obvious lesion was identified on unenhanced phase imaging. (B) No abnormalities were observed in the portal venous phase. (C) A hyperattenuating lesion was detected during the arterial phase. (D,E) Superior mesenteric artery angiography revealed contrast extravasation from an ileojejunal artery branch, consistent with an active small bowel hemorrhage. (F,G) Laparoscopic exploration revealed a 1.5 cm × 1.5 cm mesenteric-based mass at the junction of the jejunum and ileum, which had a smooth and erythematous surface. (H,I) Hematoxylin-eosin staining demonstrated dilated congested sinusoidal spaces within the submucosa.
The Interventional Radiology Department recommended digital subtraction angiography (DSA) of the superior mesenteric artery. This examination showed contrast extravasation from the ileojejunal artery branches (Figures 1D,E), confirming an active small intestinal hemorrhage. A small intestinal hemangioma was initially suspected; however, after coil embolization of the ileojejunal artery branches, definitive hemostasis was not achieved.
Due to the child’s significant hemorrhage, the Pediatric Surgery Service recommended diagnostic and therapeutic laparoscopic exploration. Intraoperatively, a 1.5 cm × 1.5 cm mesenteric-based lesion with a smooth, erythematous surface was identified at the junction of jejunum and ileum (Figures 1F,G). The bleeding lesion was completely resected (Figures 1F,G). The final pathological examination confirmed it was a cavernous hemangioma (Figures 1H,I).
Physical examination
Upon admission, the patient’s heart rate was 128 beats/min with a blood pressure of 91/52 mmHg (converted from 12.1/6.9 kPa). Pallor was noted, and all other physical examination findings were unremarkable.
Laboratory examinations
Laboratory tests revealed severe normocytic anemia (hemoglobin: 5.0 g/dL) with a positive fecal occult blood test. No abnormalities were detected in liver and kidney function, coagulation profiles, or bone marrow aspiration smears.
Imaging examinations
Computed tomography (SOMATOM Definition Flash, Siemens, Germany) revealed an arterial-phase enhancing lesion in the small intestine (Figures 1A–C). No abnormalities were found in gastroscopy and colonoscopy. DSA (Figures 1D,E) was conducted under ultrasound guidance, with the modified Seldinger technique used to puncture the right femoral artery and insert a catheter sheath.
• Abdominal aortography revealed thickening and tortuosity of the intrahepatic arteries, with multiple clustered nodules throughout the liver suggestive of hemangiomas. No active extravasation was observed.
• Superior mesenteric angiography demonstrated patent main trunks but disorganized terminal branches without active bleeding.
• Microcatheters were sequentially superselected into jejunal and ileal artery branches, and angiography showed no bleeding.
After positioning the patient in a 30° right anterior oblique position (aligned with the prior CT scan for anatomical correlation), repeat angiography identified contrast extravasation from a jejunoileal artery branch in the mid-lower abdomen. Following superselection with a microguidewire-confirmed catheter, the branch was found to have aneurysmal changes with an active hemorrhage.
Coil embolization was performed; however, the therapeutic effect was suboptimal.
Treatment
Laparoscopic exploration was performed to expose the ileocecal region. The exploration progressed sequentially from the ileocecal region. At the ileojejunal junction, a 1.5 cm × 1.5 cm mass with a smooth, erythematous surface was identified. Its base was attached to the mesentery. The mesenteric plane surrounding the mass was dissected toward its base using a harmonic scalpel. Multiple mesenteric vessels were visualized at the base. Consequently, conversion to laparotomy was performed for small bowel resection of the mass, followed by intestinal anastomosis.
A microscopic examination revealed twisted and dilated thin-walled vascular channels within the submucosa at the hemorrhagic site. The definitive pathological diagnosis was a cavernous hemangioma at the ileojejunal junction.
Outcome and follow-up
The patient recovered quickly postoperatively with no further bleeding. At the 1-month follow-up, his hemoglobin levels had increased to 8.6 g/dL (normal range: 12–16 g/dL).
Discussion
In 1839, Philips first described gastrointestinal bleeding caused by vascular tumors. Since the 1950s, with the development of diagnostic techniques such as angiography, the number of reported cases of small intestinal hemangiomas has increased (7). The etiology of this disease is unknown, and it affects people of all age groups [no gender difference, with a high incidence in adolescents and adults around 30 years old (8)]. The lesions are usually located in the jejunum and ileum (can be single, multiple, or diffusely involved). The main symptoms are recurrent gastrointestinal bleeding and iron-deficiency anemia (accompanied by dizziness, fatigue, etc.). Early diagnosis is difficult due to atypical manifestations; complications include intussusception (9), and a definitive diagnosis relies on a pathological examination. For lower gastrointestinal bleeding in children, juvenile polyps and other conditions should be ruled out first, with colonoscopy the preferred examination.
Case examination and diagnosis
In this case, CT showed contrast extravasation in the arterial phase (suggesting active small intestinal bleeding), but no abnormalities were found in the venous and portal phases. Moreover, CT has low specificity in diagnosing vascular lesions (1). Common examinations for small intestinal bleeding include DSA and capsule endoscopy (CE) (10, 11). Since enteroscopy and CE were not available in our hospital, DSA was performed [the localization accuracy for bleeding ≥0.5 mL/min is 50%–72%, with simultaneous hemostasis possible; the diagnostic rate decreases to 25%–50% in a case with slow bleeding (12)]. DSA detected bleeding from the jejunoileal artery branch, and embolization failed. Different from the traditional diagnostic method relying on enteroscopy (1), DSA provides a new option for bleeding localization.
Endoscopic resection or embolization may be an option in some cases (13), but this pediatric patient required surgery due to acute massive bleeding leading to severe anemia and failed interventional therapy. CE is non-invasive but cannot be used for biopsy or localization (14, 15), while double-balloon enteroscopy (DBE) allows for biopsy and treatment but is invasive (16). Based on the CT, DSA (suspected vascular malformation), and high bleeding rate, laparoscopic exploration was selected in this case. A 1.5 cm × 1.5 cm mass was resected from the mid-jejunum, and postoperative pathology confirmed a small intestinal cavernous hemangioma (Fuhrman grade I–II).
The diagnosis of small intestinal cavernous hemangiomas is challenging because the lesions are usually located in the mid-jejunum and intestinal peristalsis interferes with localization. Selective mesenteric angiography is the first choice (it can detect bleeding ≥0.5 mL/min and simultaneous embolization can be performed, with the cessation of contrast extravasation the criterion for a successful embolization). If embolization fails (failure rate: 15%–30%), surgery is recommended; lesions >2 cm are easily identifiable during surgery. Segmental intestinal resection yields good results, with a 5-year recurrence rate of <5%.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
This study involving humans was approved by the Medical Ethics Committee of Hunan Provincial People's Hospital. The study was conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
TX: Writing – original draft. YL: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Natural Science Foundation of Hunan Province (Grant nos. 2023JJ60306 and 2025JJ90204).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hu PF, Chen H, Wang XH, Wang WJ, Su N, Shi B. Small intestinal hemangioma: endoscopic or surgical intervention? A case report and review of literature. World J Gastrointest Oncol. (2018) 10(12):516–21. doi: 10.4251/wjgo.v10.i12.516
2. Varma JD, Hill MC, Harvey LA. Hemangioma of the small intestine manifesting as gastrointestinal bleeding. Radiographics. (1998) 18(4):1029–33. doi: 10.1148/radiographics.18.4.9672985
3. Beraldo RF, Marcondes MB, da Silva DL, Grillo TG, Baima JP, de Barros JR, et al. Small intestinal hemangioma: a case report. Am J Case Rep. (2021) 22:e929618. doi: 10.12659/AJCR.929618
4. Hyun BH, Palumbo VN, Null RH. Hemangioma of the small intestine with gastrointestinal bleeding. JAMA. (1969) 208(10):1903–5. doi: 10.1001/jama.1969.03160100093021
5. Gordon FH, Watkinson A, Hodgson H. Vascular malformations of the gastrointestinal tract. Best Pract Res Clin Gastroenterol. (2001) 15(1):41–58. doi: 10.1053/bega.2000.0155
6. Rao AB, Pence J, Mirkin DL. Diffuse infantile hemangiomatosis of the ileum presenting with multiple perforations: a case report and review of the literature. J Pediatr Surg. (2010) 45(9):1890–2. doi: 10.1016/j.jpedsurg.2010.05.019
7. Nascimento CND, Albergaria D, Brito D, Canhoto M. Jejunum cavernous hemangioma: a rare cause of gastrointestinal bleeding. Rev Esp Enferm Dig. (2025) 117(5):279–80. doi: 10.17235/reed.2023.9812/2023
8. Zhang GY, Luo CJ, Zhao B, Zhan H, Long B, Guo LY, et al. Small intestinal cavernous hemangioma causing chronic hemorrhage: a case report. Nan Fang Yi Ke Da Xue Xue Bao. (2017) 37(7):866–8. doi: 10.3969/j.issn.1673-4254.2017.07.02
9. Kuo LW, Chuang HW, Chen YC. Small bowel cavernous hemangioma complicated with intussusception: report of an extremely rare case and review of literature. Indian J Surg. (2015) 77(Suppl 1):123–4. doi: 10.1007/s12262-014-1194-3
10. Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG clinical guideline: diagnosis and management of small bowel bleeding. Am J Gastroenterol. (2015) 110:1265–87; quiz 1288. doi: 10.1038/ajg.2015.246
11. Pennazio M, Rondonotti E, Despott EJ, Dray X, Keuchel M, Moreels T, et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) guideline—update 2022. Endoscopy. (2023) 55:58–95. doi: 10.1055/a-1973-3796
12. Kano T, Fukai S, Okamoto R, Motomura Y, Lefor AK, Mizokami K. An incidentally identified 15 cm cavernous hemangioma of the small intestine: case report and literature review. Int J Surg Case Rep. (2021) 84:106144. doi: 10.1016/j.ijscr.2021.106144
13. Soukoulis IW, Liang MG, Fox VL, Mulliken JB, Alomari AI, Fishman SJ. Gastrointestinal infantile he-mangioma: presentation and management. J Pediatr GastroenterolNutr. (2015) 61(4):415–20. doi: 10.1097/MPG.0000000000000812
14. Akahoshi K, Kubokawa M, Matsumoto M, Endo S, Motomura Y, Ouchi J, et al. Double-balloon endoscopy in the diagnosis and management of GI tract diseases: methodology, indications, safety, and clinical impact. World J Gastroenterol. (2006) 12(47):7654–9. doi: 10.3748/wjg.v12.i47.7654
15. Mensink PB, Haringsma J, Kucharzik T, Cellier C, Pérez-Cuadrado E, Mönkemüller K, et al. Complications of double balloon enteroscopy: a multicenter survey. Endoscopy. (2007) 39(7):613–5. doi: 10.1055/s-2007-966444
Keywords: cavernous hemangioma, hematochezia, children, anemia, multidisciplinary collaboration
Citation: Xie T and Long Y (2025) A cavernous hemangioma in the small intestine of a teenage boy: a case report and literature review. Front. Pediatr. 13:1654913. doi: 10.3389/fped.2025.1654913
Received: 27 June 2025; Accepted: 22 August 2025;
Published: 12 September 2025.
Edited by:
Luc Hervé Samison, Centre d'Infectiologie Charles Mérieux (CICM), MadagascarReviewed by:
Nilton Carlos Machado, Sao Paulo State University, BrazilLuca Giacomelli, Polistudium srl, Italy
Copyright: © 2025 Xie and Long. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Long, MTA4NDI3ODc2MkBxcS5jb20=
 Tian Xie
Tian Xie Yi Long
Yi Long