- 1Research Institute, Imperial College London Diabetes Centre, Abu Dhabi, United Arab Emirates
- 2Department of Psychology, Georgetown University, Washington, DC, United States
- 3Department of Nutritional Sciences, The Pennsylvania State University, University Park, PA, United States
Aims: Paediatric obesity is associated with both physical and psychosocial health. Whether those associations, which are most widely reported in Western samples, are also observed in other sociocultural settings is not well known. This study aimed to characterise lifestyle, physical, and psychological characteristics associated with excess weight in Emirati youth, a population that has not been widely studied.
Materials and methods: Height and weight were measured for 107 youth (46 male; 7–17 years) from Abu Dhabi. A detailed medical history was obtained from the Imperial College London Diabetes Centre. Parents reported relevant family history and demographics, sleep using the Children's Sleep Habits Questionnaire, and mental health problems using the Strengths and Difficulties Questionnaire.
Results: Older youth and those with a family history were more likely to have obesity; however, weight status did not differ by sex, income, or parental education. Anaemia was more prevalent in youth with a healthy weight, while hyperlipidemia was more prevalent in youth with overweight or obesity. Obesity was associated with disordered breathing during sleep but not with sleep times or duration. Overall, weight status did not relate to mental health problems; however, obesity was associated with a greater risk for peer problems in females but not males.
Conclusions: These results highlight factors that may play a role in culturally specific drivers of paediatric obesity in the Middle East and will help to natively tailor prevention and intervention efforts.
1 Introduction
The growing burden of obesity in children and adolescents is a significant public health concern worldwide (1). The prevalence of overweight and obesity among 5–19-year-olds has risen from 4% in 1975 to over 18% in 2016 (2). Similarly, rates of paediatric obesity are increasing in Gulf Cooperation Council (GCC) countries, including the United Arab Emirates (UAE), Saudi Arabia, Bahrain, Qatar, Oman, and Kuwait (3), with the UAE Ministry of Health and Prevention reporting 17.4% of 5–17-year-old children and adolescents had obesity in 2019 (4). However, the lack of uniformity in reference standards and reporting systems renders comparisons difficult (3). Children with obesity face a lifelong burden of deleterious comorbidities, with obesity contributing to over one-third of adult non-communicable disease incidence, including cardiovascular diseases, cancers, chronic respiratory disorders, type 2 diabetes mellitus, and mental health disorders (5). The economic burden of obesity, with the annual global cost of childhood obesity projected to increase from $13.62 billion to $49 billion by 2050 (6). Therefore, early prevention and intervention are necessary, which requires a better understanding of the factors that contribute to the development and maintenance of excess weight in childhood.
The aetiology of childhood obesity is multifactorial, including behavioural, sociocultural, environmental, and genetic contributions, which complicate strategies for its prevention and management (7–9). Additionally, the current understanding of the factors associated with paediatric obesity largely stems from Western studies, where socioeconomic disparities remain a key determinant of obesity risk across countries. For example, lower socioeconomic status and paediatric obesity are both independently associated with cognitive, sleep, and mental health problems (9–12). Examination of these associations in countries with different socioeconomic and sociocultural structures is needed to understand the contributing factors and inform the management of excess adiposity and its consequences (13). Recent reviews and meta-analyses of risk factors for childhood obesity in GCC found that the risk for obesity was greater in older children, in children whose parents and/or siblings had elevated body mass index (BMI), in children with lower physical activity, and in children who ate out at restaurants more than twice a week and consumed more fast food (3, 14). However, the review noted inconsistencies across studies and countries. To better understand the factors that contribute to paediatric obesity in the UAE, more comprehensive studies are needed that assess familial, lifestyle, and medical histories.
There have been calls for more research on the biological, environmental, and cultural drivers of obesity in the Gulf region (15). Therefore, this study examined the associations of weight status with demographic characteristics, sleep and physical health, and mental health in Emirati children and adolescents living in Abu Dhabi.
2 Materials and methods
2.1 Participants
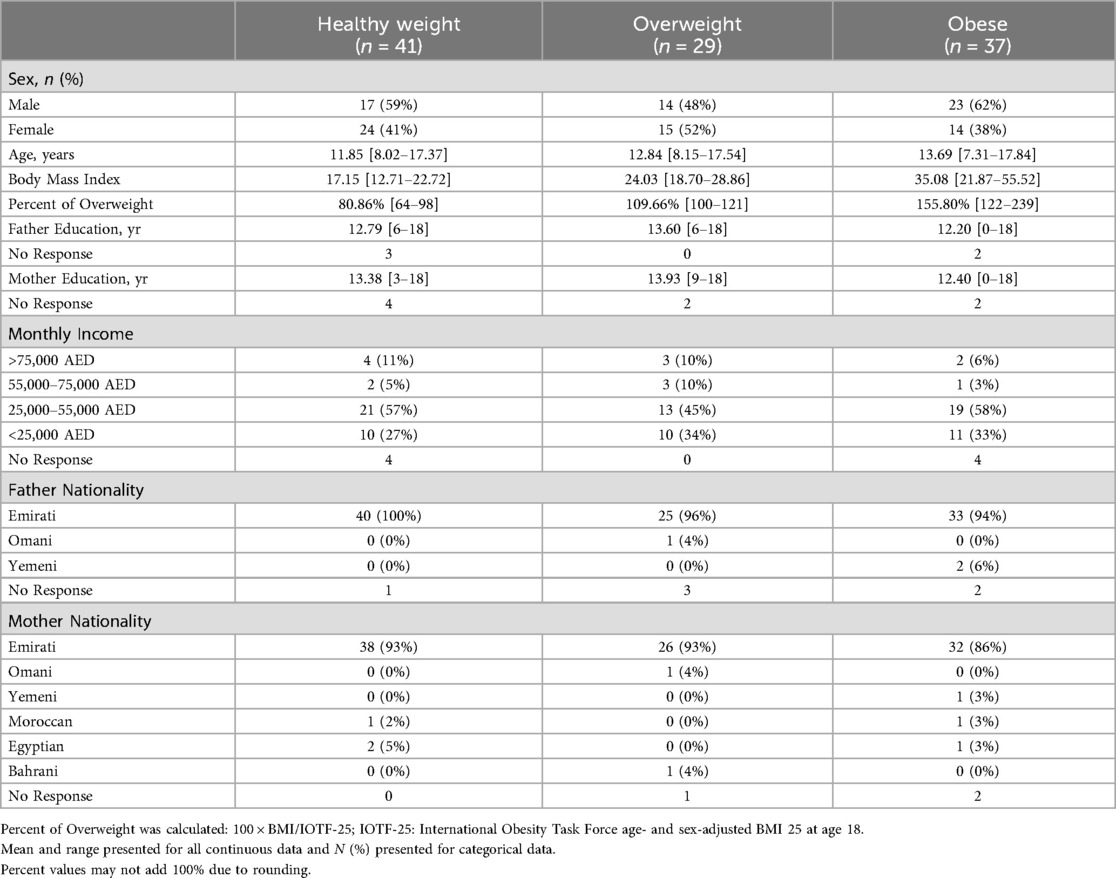
A sample of 107 children and adolescents (61 female, 46 male) aged 7–17 years old were recruited from the Imperial College London Diabetes Centre (ICLDC) in Abu Dhabi, UAE, from 2019 to 2020. Clinic patients were invited to participate if they were not currently diagnosed with type 2 diabetes. Using the International Obesity Task Force (IOTF) criteria (16), 41 (38%) had a healthy weight, 29 (27%) had overweight, and 37 (35%) had obesity (see Table 1 for participant characteristics). Participants were excluded if they were diagnosed with a neuropsychiatric disorder, were currently taking any psychotropic medications, had a learning disability or difficulty that would make completing the study protocol difficult, or had a history of or current seizure disorder or use of neuroleptic medications. According to the Institutional Review Board at ICLDC, informed consent and assent were obtained before participation.
2.1.1 Power analysis
Based on findings from a US sample of a similar age range (7–18 years old), the anticipated effect size for the association between weight status and sleep health and mental health is medium-large (r = 0.48) (17) and small-medium (r = 0.22), respectively. The present study was powered to detect associations between %IOTF-25 and sleep health (0.90 power) and to detect main effects and interactions between %IOTF-25 and sex for mental health (0.73 power).
2.2 Protocol
Participants completed the study on the same day of their visit to ICLDC. Parents completed questionnaires pertaining to their family demographics, history of obesity and eating disorders, and their child's sleep and mental health. Youth height and weight were measured, and children and adolescents also completed a series of cognitive assessments (reported in Pearce et al.). Participants' medical histories at the ICLDC were reviewed to identify medical conditions (medical record data collected at the time of participant from 2019 to 2020). A trained researcher administered all surveys in Arabic to the parents.
2.2.1 Anthropometrics
Height and weight were recorded twice on the same day, once by a qualified nurse and once by trained researchers at the researcher using a standard scale (Tanita Japan) and stadiometer (Seca). Weight status was classified using the IOTF age- and sex-adjusted cut-offs (16). Percent of overweight was calculated by dividing BMI by the age- and sex-adjusted overweight cut-off . Therefore, values less than 100% indicate a healthy weight, a value of 100% indicates the participant is overweight and his/her BMI is right at the overweight cut-off, and values over 100% indicate overweight or obesity (see Figure 1). Percent of overweight has shown to have a more appropriate distribution (18) and better correspondence with measured body circumferences and fat mass than BMI-z/BMI-SDS or BMI-percentile in samples with moderate (19) and severe obesity (19, 20).
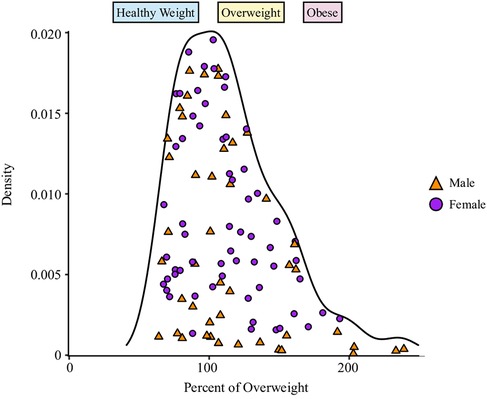
Figure 1. Density distribution of percent of overweight. The shaded regions indicate weight status: healthy weight = blue, overweight yellow, obese = red. Sex is indicated by shape and colour: male = orange triangle, female = purple circle.
2.2.2 Demographics and family history
Parents completed a demographic questionnaire asking them to report their ethnicity, years of education, and monthly household income. In addition to demographic information, parents also reported whether any members of the family had a history of or currently have obesity or eating disorders (e.g., anorexia, binge eating) and to mark which categories of family relationships (e.g., mother, brother, uncle) had a history or currently have the respective condition. This provides an index of the extent to which a family has been impacted by obesity and/or eating disorders.
2.2.3 Sleep behaviours
The Children's Sleep Habits Questionnaire (CSHQ) is a validated screening instrument used to identify behavioural sleep problems in children (21). As part of the CSHQ, parents also reported their child's typical bedtime and waketime, which was used to compute duration in bed for each participant. Additionally, participants were categorised according to whether their reported bedtime and total sleep duration met current international sleep recommendations for school-aged children and adolescents (22, 23).
2.2.4 Mental health
The Strengths and Difficulties Questionnaire (SDQ) is a widely validated instrument for assessing emotional and behavioural difficulties in children across diverse cultures (24, 25). Parents completed the Arabic version of the SDQ, validated for Arabic-speaking populations, which measures emotional, conduct, hyperactivity, and peer problems, as well as prosocial behaviours (26). To examine risk for mental health-related issues, the four-band categorisation was reduced to two categories: typical (i.e., “Close to Average”) and at-risk behaviour (i.e., “Slightly Raised/Lowered” to “Very High/Low”) (27).
2.3 Analyses
2.3.1 Analytic approach
All analyses were conducted in R (28) with data and code available at https://osf.io/4w725/.
For demographic characteristics and sleep behaviour, associations with %IOTF-25 were tested using Pearson's correlation for continuous outcomes (e.g., years of maternal education, age). To test mean differences in %IOTF-25 between groups, t-tests or one-way analyses of variance (ANOVA) were used (e.g., sex, income category). We used Fisher's exact p-value to test the prevalence of different medical comorbidities across weight status categories. For medical comorbidities observed in more than 20 participants, t-tests were used to test for mean differences in %IOTF-25 between those with and without the comorbidity. For count data (e.g., number of family members), associations with %IOTF-25 were assessed using Poisson regressions. Given well-established global differences in the prevalence of mental disorders between males and females (29), logistic regressions were used to examine potential sex × %IOTF-25 interactions in the odds of experiencing behavioural problems or low prosociality (see 2.2.3 Mental Health). Due to the inclusion of an interaction, %IOTF-25 was centered at 100% for these models.
Sensitivity analyses were conducted for all significant associations with %IOTF-25 to test the stability of the effect after accounting for individual differences in sex, age, and socio-economic status, which was indexed by monthly income and maternal education. Additional sensitivity analyses were conducted for family history, sleep, and mental health models after removing youth with Growth/Stature co-morbidities (n = 10; Table 2). Removal of these youth did not change the patterns of results for any models.
3 Results
3.1 Participant characteristics
This sample ranged in BMI from 11.85 to 55.52 kg/m2 with all weight categories fairly evenly represented (using IOTF criteria) (16): healthy weight: 38%, n = 41; overweight: 27%, n = 29; obese: 35%, n = 37. Of those with obesity, 62% (n = 23) had morbid obesity, which was defined as a BMI greater or equal to the IOTF age- and sex-adjusted BMI of 35 at 18 years (BMI-35) (16). %IOTF-25 had a well-balanced, continuous distribution (Figure 1), which ranged from 63.95% to 239.00% (Figure 1 and Table 1).
IOTF-25 did not differ by sex [t(79) = −072, p = 0.471] or monthly income [F(3, 95) = 0.24, p = 0.867] and was not associated with maternal (r = −0.15, p = 0.131) or paternal (r = −0.07, p = 0.491) education. There was, however, a significant association between %IOTF-25 and age (r = 0.26, p = 0.006), indicating older participants tended to have higher %IOTF-25. The follow-up sensitivity test (see 2.3.1) showed that after adjusting for covariates, age was positively associated with %IOTF-25 such that for each year older, a youth's percent of overweight is expected to be 4.24 percentage points higher [β(se) = 4.24 (1.46), p = 0.005]. This indicates the degree of excess weight was greater in older than younger participants in this sample.
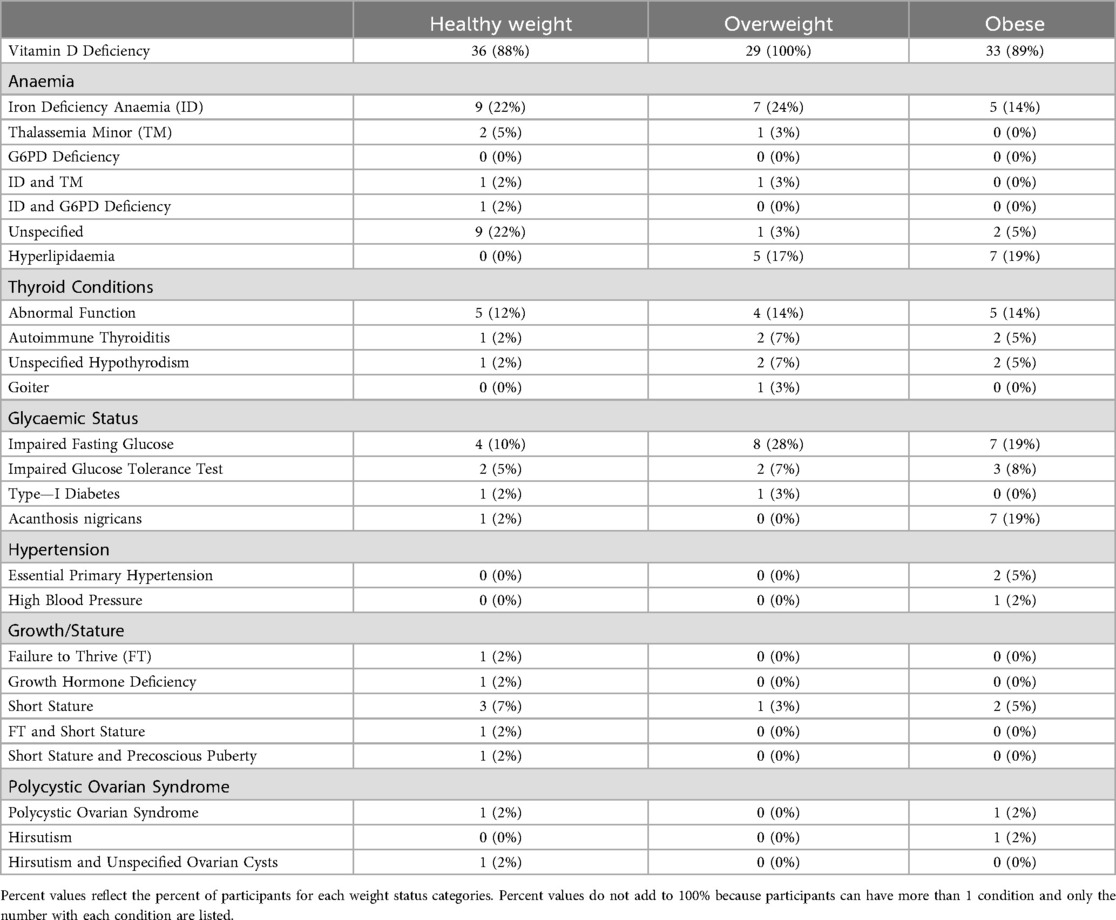
3.2 Medical comorbidities
Overall, the number of medical comorbidities ranged from zero to four with an average of two comorbidities per participant (mean = 2.15, SD = 1.04), not including overweight/obesity. The number of comorbidities was not associated with %IOTF-25 [β(se) = 0.001 (0.002), p = 0.598] and did not differ by sex [t(101) = 1.13, p = 0.263] (Table 2).
3.3 Family history of obesity and eating disorders
Overall, 70% (n = 70 of 101) of parents reported at least one family member with a history of or present obesity. %IOTF-25 was greater if the family reported a history of obesity (mean = 125.09%, SD = 38.38%) than if they did not [mean = 94.77%, SD = 23.87%; t(87.9) = 4.83, p < 0.001]. The number of different family relationship categories selected as having a history of obesity was positively associated with %IOTF-25 [β(se) = 0.009 (0.002), p < 0.001] such that a youth with 110% of overweight would have 9% greater odds of having an additional family relationship category with a history of obesity compared to a youth at 100% of overweight . A sensitivity test showed %IOTF-25 remained significant after adjusting for covariates [β(se) = 0.008 (0.002), p < 0.001].
In contrast, fewer families reported a history of eating disorders (11%, n = 11 of 96). Due to the limited number of participants with a family history, differences in %IOTF-25 could not be tested. However, the prevalence of a family history did not differ across weight statuses (Fisher's p = 0.263). When asked to indicate which family relationship categories had or currently have an eating disorder, the number of categories selected ranged from one to seven across the 11 participants who reported a family history (overall sample mean = 0.21, SD = 1.75). For those that reported a history (n = 11), the child's aunt was selected 64% of the time (n = 7), grandmother was selected 36% of the time (n = 4), uncle was selected 27% of the time (n = 3), brother, father, sister, and grandfather were each selected 18% of the time (n = 2) and mother was selected 9% of the time (n = 1).
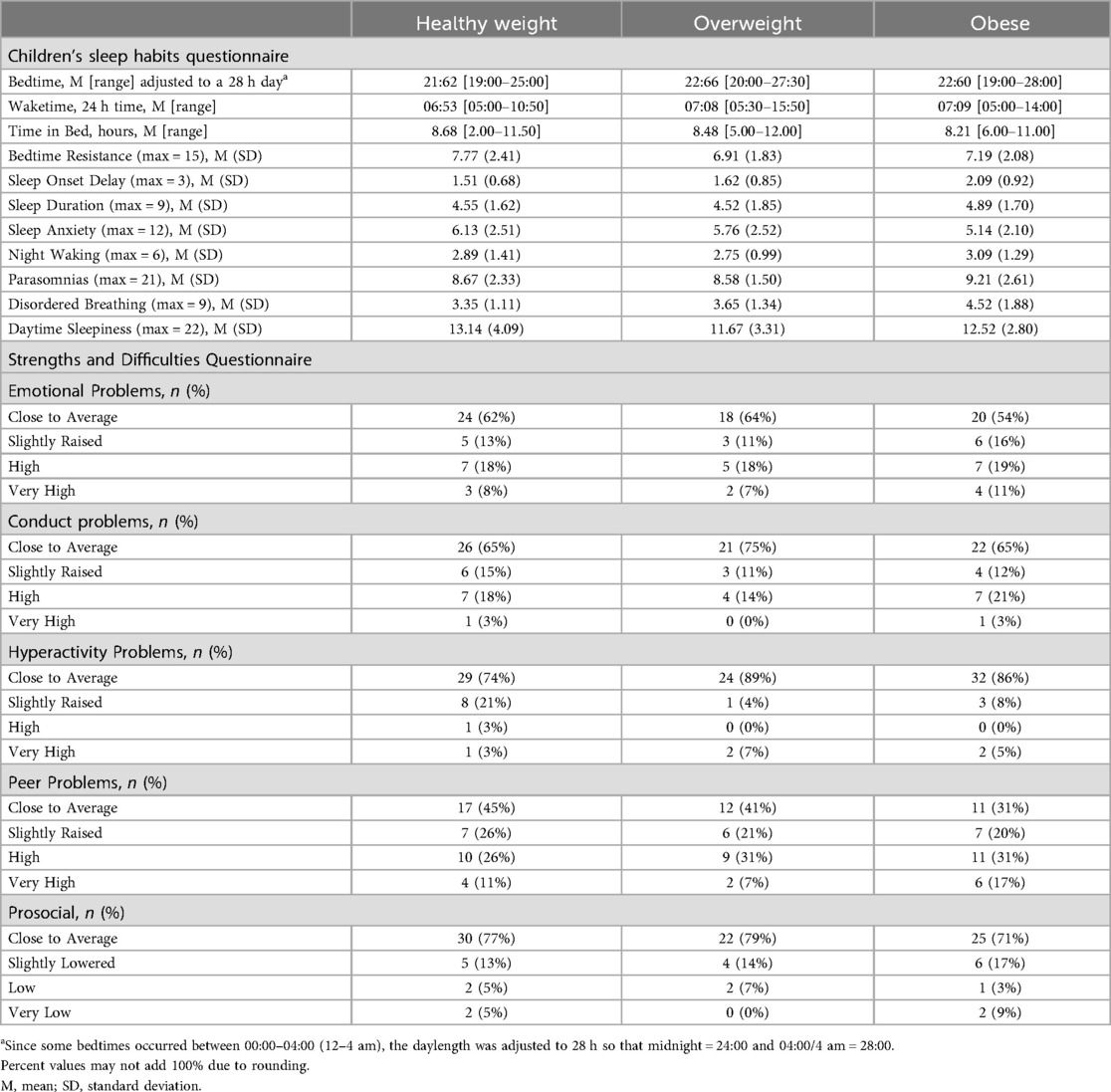
3.4 Sleep behaviour
The average bedtime reported was 22:14 (SD = 1.86 h). Reported waketimes ranged from 05:00 (5 am) to 15:30 (3:30 pm) with an average waketime of 06:52 (SD = 1.79 h). Time spent in bed ranged from 2 to 12 h with an average of 8.46 h (SD = 1.65 h). Overall, 53% (n = 52 of 47) of participants met the recommendation to have a bedtime within the 21:00/9 pm hour (22), and 44% (n = 43 of 97) met the recommendations for total sleep time (9–11 h for 7–12-year-olds and 8–10 h for 13–17-year-olds) (23). %IOTF-25 was not associated with bedtime (r = 0.13, p = 0.192), time in bed (r = −0.09, p = 0.392), or waketime (r = 0.06, p = 0.584) and did not differ if sleep duration [t(96) = 0.50, p = 0.615] or bedtime [t(85) = 1.68, p = 0.098] recommendations were met (Table 3).
Although %IOTF-25 was not associated with sleep duration or typical sleep patterns, it was associated with CSHQ subscales Sleep Onset Delay (r = 0.31, p = 0.002) and Sleep Disordered Breathing (r = 0.37, p < 0.001). No other CSHQ subscales were associated with %IOTF-25 (r's = −0.18–0.10, p's = 0.070–0.692). Sensitivity test adjusting for covariates (see 2.3.1) showed %IOTF-25 was positively associated with both Sleep Onset Delay [β(se) = 0.006 (0.003), p = 0.037] and Sleep Disordered Breathing [β(se) = 0.016 (0.005), p = 0.002]. After accounting for covariates, a youth with 110% of overweight, relative to 100% overweight, would be expected to have a 0.06-point higher Sleep Onset Delay score (range 0–3) and 0.12-point higher Sleep Disordered Breathing score (range 3–9). Together, this suggests that while overall sleep patterns do not differ by percent of overweight, youth with higher weight status are more likely to take longer to fall asleep and have more sleep-related disordered breathing (e.g., snoring, snorts/gasps) (21).
3.5 Mental health
There was no evidence for elevated mental health problems in this sample, with the majority of participants experiencing typical or “Close to Average” behavioural profiles for the primary mental health dimensions (emotional: 60%, n = 62; conduct: 68%, n = 69; hyperactivity: 83%, n = 85) and prosociality (75%, n = 77). After adjusting for all covariates, logistic regressions showed no significant associations with %IOTF-25 or sex-by-%IOTF-25 interactions for the likelihood of experiencing at-risk levels for emotional, conduct, hyperactivity, or prosocial problems (p's > 0.055). Relative to the other SDQ subscales, the proportion of participants with typical or “Close to Average” peer problems was lower (39%, n = 40). Sensitivity tests (see 2.3.1) showed a significant sex × %IOTF-25 interaction for peer problems [β(se) = −0.030 (0.014), p = 0.036; Figure 2]. post-hoc tests showed males had no association between %IOTF-25 and odds of being at-risk for peer problems [β(se) = −0.006 (0.009), 95% CI: −0.02–0.01] while females had a significant positive association [β(se) = 0.024 (0.012), 95% CI: 0.001–0.046]. Thus, while males did not show increased risk for peer problems with greater weight status, a female youth with 110% overweight had 27% greater odds of having peer problems than a female youth with 100% of overweight (Table 3).
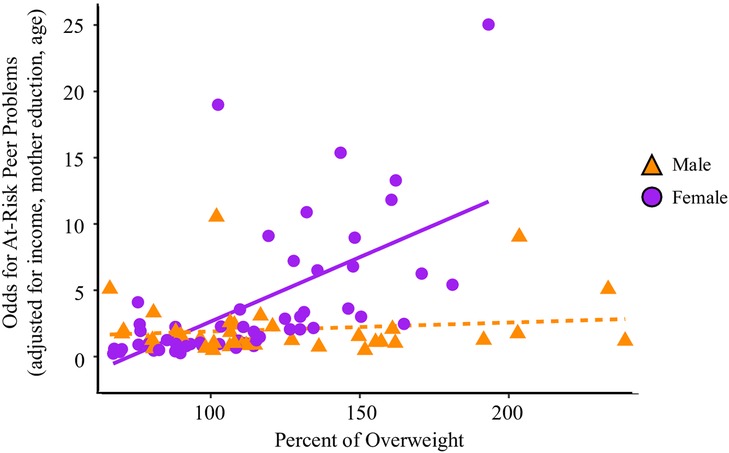
Figure 2. Peer problems sex × percent of overweight. This figure shows the predicted odds of experiencing At-Risk peer problems by sex and percent of overweight after adjusting for monthly income, maternal education, and age. The shaded regions indicate the standard error region around each slope. Sex is indicated by shape and colour: male = orange triangle, female = purple circle.
4 Discussion
This is a preliminary, comprehensive examination of the association between physical, behavioural, and psychosocial characteristics and the weight status of Emirati youth in the UAE. Prevalence of obesity was higher in older youth and in those having more family members with obesity; however, obesity was not associated with sex, parental education or family income. Among the many physical health conditions observed, only two were associated with weight status: anaemia was more prevalent in youth with a healthy weight, while hyperlipidemia was more prevalent in youth with overweight or obesity. Among sleep characteristics, only delayed sleep onset and disordered breathing were associated with obesity. Lastly, there was no evidence of elevated behavioural problems regarding attention/hyperactivity, conduct, emotional, and social behaviour in youth with obesity. However, girls with obesity experienced more problems with peer relations than their male counterparts. Overall, this study identified preliminary health and behavioural risk factors in Emirati youth with obesity. These findings provide a foundation to generate hypotheses that can be tested in larger samples of Emirati youth. Overall, these results highlight the need for directing culturally tailored prevention and intervention efforts.
To better understand the physical complications associated with obesity in Emirati youth, medical records were reviewed. Not considering the medical conditions of overweight or obesity, participants had an average of two medical conditions. Vitamin D deficiency was most prevalent and did not differ by weight status. A high prevalence of Vitamin D deficiency has been noted in the UAE (30, 31) and other Gulf region countries (32) and clinical practice guidelines have been proposed to address this for the UAE (33). However, prevalence of anaemia was greater in youth with healthy weight while prevalence of hyperlipidaemia was greater in those with overweight and obesity. This replicates previous findings from the UAE showing dyslipidaemia in youth with excess weight (34, 35). Together, the reported patterns of medical complications align with previously observed patterns in the UAE indicating good generalizability with other studies of youth in the UAE.
The current study showed both similarities and differences from studies in Western samples. In the current study, there was no association between weight status and family income or parental education level. This is in contrast to patterns seen in Western populations, where youth with lower socioeconomic status experience increased risk for obesity, which suggests that risk for obesity may not be reliably associated with socioeconomic status across different sociocultural settings. Similar to findings in Western samples (36), the prevalence of obesity was associated with current and/or past family history of obesity. Seventy percent of participants had at least one member in their family who currently has obesity or has had obesity in the past and youth with a greater number of relatives with a history of obesity also had higher weight status. Consistent associations between youth obesity and a family history of obesity across studies suggest efforts should be made to identify both heritable and cultural risk factors for obesity.
Although there have been suggestions that obesity is related to sleep disturbances in youth, the lack of well-designed prospective investigations has made it difficult to arrive at firm conclusions for the UAE. While about half the youth met the recommended bedtime, only 44% met the recommendations for total sleep. Sleep recommendations norms are based on studies of Western samples and thus, the observed low rates suggest notable cultural differences in sleep habits. Overall, there was no association between weight status and bedtime, time in bed, or wake time. However, higher weight status was associated with delayed onset of sleep and more sleep-disordered breathing incidents, such as snoring and snorts or gasps, commonly associated with obstructive sleep apnea. This replicates findings from the UAE (37) and Western (17) studies showing worse sleep health and sleep disordered breathing in children and adolescents with obesity. Pediatric obesity has been associated with increased risk for obstructive sleep apnea in both Western (38) and Eastern (39) samples; therefore, it is important to continue efforts to understand better the role of paediatric obesity in sleep health in the Gulf region.
As in adults, obesity in children and adolescents is associated with physical complications, as well as psychosocial issues. The latter manifests in different ways in children and has been investigated to a lesser extent in the Middle Eastern population. While Western samples show an association between paediatric obesity and internalising (e.g., depression) and externalising (e.g., hyperactivity) disorders (17, 40), there was no evidence for an association between weight status and mental health problems in the current sample of UAE youth. However, there was an interaction between risk for experiencing peer problems and sex. For girls, risk for peer problems was elevated for those with higher weight status. This same pattern was observed in the first wave of the US-based Adolescent Brain and Cognitive Development (ABCD) study (40). One explanation may be that girls whose body types diverge from sociocultural norms are more likely to experience weight-related stigma and social exclusion (41). Indeed, a recent qualitative study in the UAE, parents of children with obesity reported concerns related to bullying and social isolation (42). Therefore, it is important to consider the role of social stigma in long-term psychosocial health (43), with particular attention to girls. In the UAE, recent studies show that dietary preferences and eating behaviours are closely linked to body weight, particularly among young women, with higher intake of fast foods and sweetened drinks associated with overweight and obesity (44). A national nutrition review further highlights the ongoing shift toward Westernised diets and lifestyle patterns in the UAE (45). These sociocultural factors may help explain the body-image pressures and peer challenges observed among girls with obesity in this study.
These preliminary findings can have significant implications locally and regionally, as paediatric obesity is increasingly prevalent and relevant in the Middle East. However, the study has a few limitations that must be considered. First, this was a cross-sectional study design with non-random sampling, and therefore may not be representative of all youth in the general population. While recruiting participants exclusively from the ICLDC enabled characterisation of medical records, it might limit the generalizability of the findings to younger individuals who do not seek treatment for a chronic condition. Future studies that incorporate random or school-based sampling across multiple regions of the UAE would yield more representative prevalence estimates.
Additionally, while %IOTF-25 is more closely associated with adiposity than BMI (19), particularly in youth with morbid obesity (18), it is an indirect measure of adiposity and faces similar limitations to other BMI-based metrics (46). While the questionnaires have well-established reliability, sleep and mental health were based on parent report. Parent-reported SDQ scores may under-detect internalising symptoms such as anxiety or depression, particularly among adolescents, who may not express such concerns to parents. Future research should integrate adolescent self-reports to provide a more comprehensive assessment of psychosocial functioning. To draw more definitive conclusions and gain a deeper understanding, larger studies including a broader range of participants are needed. Small subgroup sizes may have limited power to detect modest effects, and the lack of correction for multiple comparisons increases the risk of Type I error. However, the consistency of associations across sensitivity models provides some confidence in the robustness of findings. Therefore, more research is necessary to inform better healthcare plans and interventions that are tailored to the unique needs of different regions and populations.
While there is a need for better powered studies of paediatric obesity in the Gulf region, this preliminary study highlights the importance of considering culturally specific factors. While paediatric obesity is associated with lower socioeconomic status and emotional and behavioural problems in Western samples, these patterns were not observed in Emirati youth.
5 Conclusion
This study highlights the need for continued examination of paediatric obesity to support the development of proactive, natively tailored healthcare plans based on a deep understanding of the causal factors in different regions. The recent rise in prevalence in the Gulf region highlights the importance of focusing on specific studies, particularly from the Middle East. Recognition and response to the specific health and social consequences of obesity should be a goal of paediatric obesity interventions and policies in the UAE.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statement
The studies involving humans were approved by Institutional Ethics Committee: ICLDC Research Ethics Committee, REC ref # IREC035. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
TA: Data curation, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft, Writing – review & editing. AP: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft, Writing – review & editing. RH: Investigation, Project administration, Supervision, Writing – review & editing. SS: Data curation, Investigation, Project administration, Writing – review & editing. CV: Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Validation, Visualization, Writing – review & editing. NL: Methodology, Project administration, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. AP was supported by NIDDK F32 DK122669-01, NCATS TR002015, UL1 TR002014, and research was supported by Georgetown University Institutional funds.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Okati-Aliabad H, Ansari-Moghaddam A, Kargar S, Jabbari N. Prevalence of obesity and overweight among adults in the Middle East countries from 2000 to 2020: a systematic review and meta-analysis. Velotti N, editor. J Obes. (2022) 2022:1–18. doi: 10.1155/2022/8074837
2. World Health Organization. Obesity and Overweight. World Health Organization (2021). Available online at: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (Accessed February 3, 2023).
3. Al Yazeedi B, Berry DC. Childhood overweight and obesity is increasing in gulf cooperation council countries: a review of the literature. J Transcult Nurs. (2019) 30(6):603–15. doi: 10.1177/1043659619829528
4. AlBlooshi A, Shaban S, AlTunaiji M, Fares N, AlShehhi L, AlShehhi H, et al. Increasing obesity rates in school children in United Arab Emirates. Obes Sci Pract. (2016) 2(2):196–202. doi: 10.1002/osp4.37
5. Obita G, Alkhatib A. Disparities in the prevalence of childhood obesity-related comorbidities: a systematic review. Front Public Health. (2022) 10:923744. doi: 10.3389/fpubh.2022.923744
6. Ling J, Chen S, Zahry NR, Kao TA. Economic burden of childhood overweight and obesity: a systematic review and meta-analysis. Obes Rev. (2023) 24(2):e13535. doi: 10.1111/obr.13535
7. Yanovski JA. Pediatric obesity. An introduction. Appetite. (2015) 93:3–12. doi: 10.1016/j.appet.2015.03.028
8. Ang YN, Wee BS, Poh BK, Ismail MN. Multifactorial influences of childhood obesity. Curr Obes Rep. (2013) 2(1):10–22. doi: 10.1007/s13679-012-0042-7
9. Kansra AR, Lakkunarajah S, Jay MS. Childhood and adolescent obesity: a review. Front Pediatr. (2021) 8:581461. doi: 10.3389/fped.2020.581461
10. Dennis E, Manza P, Volkow ND. Socioeconomic status, BMI, and brain development in children. Transl Psychiatry. (2022) 12(1):33. doi: 10.1038/s41398-022-01779-3
11. Morrissey B, Taveras E, Allender S, Strugnell C. Sleep and obesity among children: a systematic review of multiple sleep dimensions. Pediatr Obes. (2020) 15(4):e12619. doi: 10.1111/ijpo.12619
12. Tomfohr-Madsen L, Cameron EE, Dhillon A, MacKinnon A, Hernandez L, Madigan S, et al. Neighborhood socioeconomic status and child sleep duration: a systematic review and meta-analysis. Sleep Health. (2020) 6(5):550–62. doi: 10.1016/j.sleh.2020.02.012
13. Aceves-Martins M, López-Cruz L, García-Botello M, Godina-Flores NL, Gutierrez-Gómez YY, Moreno-García CF. Cultural factors related to childhood and adolescent obesity in Mexico: a systematic review of qualitative studies. Obes Rev. (2022) 23(9):e13461. doi: 10.1111/obr.13461
14. Farrag NS, Cheskin LJ, Farag MK. A systematic review of childhood obesity in the Middle East and North Africa (MENA) region: prevalence and risk factors meta-analysis. Adv Pediatr Res. (2017) 4:3.4.8. doi: 10.12715/apr.2017.4.8
15. Khalil AB, Beshyah SA, Abdella N, Afandi B, Al-Arouj MM, Al-Awadi F, et al. Diabesity in the Arabian gulf: challenges and opportunities. Oman Med J. (2018) 33(4):273–82. doi: 10.5001/omj.2018.53
16. Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. (2012) 7(4):284–94. doi: 10.1111/j.2047-6310.2012.00064.x
17. Pearce AL, Mackey E, Nadler EP, Vaidya CJ. Sleep health and psychopathology mediate executive deficits in pediatric obesity. Child Obes. (2018) 14(3):189–96. doi: 10.1089/chi.2017.0281
18. Freedman DS, Berenson GS. Tracking of BMI z scores for severe obesity. Pediatrics. (2017) 140(3):e20171072. doi: 10.1542/peds.2017-1072
19. Freedman DS, Butte NF, Taveras EM, Lundeen EA, Blanck HM, Goodman AB, et al. BMI z-scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999–2000 to 2013–2014. Obesity. (2017) 25(4):739–46. doi: 10.1002/oby.21782
20. Løkling HL, Roelants M, Kommedal KG, Skjåkødegård H, Apalset EM, Benestad B, et al. Monitoring children and adolescents with severe obesity: body mass index (BMI), BMI z-score or percentage above the international obesity task force overweight cut-off? Acta Paediatr. (2019) 108(12):2261–6. doi: 10.1111/apa.14898
21. Owens JA, Spirito A, McGuinn M. The children's sleep habits questionnaire (CSHQ): psychometric properties of A survey instrument for school-aged children. Sleep. (2000) 23(8):1043–52. doi: 10.1093/sleep/23.8.1d
22. Beattie L, Kyle SD, Espie CA, Biello SM. Social interactions, emotion and sleep: a systematic review and research agenda. Sleep Med Rev. (2015) 24:83–100. doi: 10.1016/j.smrv.2014.12.005
23. Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. (2015) 1(1):40–3. doi: 10.1016/j.sleh.2014.12.010
24. Goodman R. Psychometric properties of the Strengths and Difficulties Questionnaire (SDQ). J Am Acad Child Adolesc Psychiatry. (2001) 40(11):1337–45. doi: 10.1097/00004583-200111000-00015
25. Ortuño-Sierra J, Fonseca-Pedrero E, Paino M, Aritio-Solana R. The SDQ across cultures: updated psychometric validation. Front Psychol. (2021) 12:687543. doi: 10.3389/fpsyg.2021.687543
26. Stone LL, Otten R, Engels RC, Vermulst AA, Janssens JM. Psychometric properties of the parent and teacher SDQ in Dutch populations. BMC Psychiatry. (2010) 10:81. doi: 10.1007/s10567-010-0071-2
27. Scoring the Strengths & Difficulties Questionnaire for age 4–17 or 18+. YouthInMind (2016). Available online at: https://www.sdqinfo.org/py/sdqinfo/c0.py (Accessed October 6, 2021).
28. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing (2020). Available online at: https://www.R-project.org/
29. Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, et al. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry. (2009) 66(7):785–95. doi: 10.1001/archgenpsychiatry.2009.36
30. Beshyah S, Hafidh K, Abdelmannan D, Jabbar A, Wafa W, Khalil A. Paradoxical vitamin D deficiency in a sunny country: a narrative review of the literature from the United Arab Emirates (1992–2018). Ibnosina J Med Biomed Sci. (2019) 11(03):97–108. doi: 10.4103/ijmbs.ijmbs_50_19
31. Alawadhi F, Yavuz L. Signs and symptoms of vitamin D deficiency in children: a cross-sectional study in a tertiary pediatric hospital in the United Arab Emirates. Cureus. (2021) 13:e18998. doi: 10.7759/cureus.18998
32. Al Saleh Y, Beshyah SA, Hussein W, Almadani A, Hassoun A, Al Mamari A, et al. Diagnosis and management of vitamin D deficiency in the Gulf Cooperative Council (GCC) countries: an expert consensus summary statement from the GCC vitamin D advisory board. Arch Osteoporos. (2020) 15(1):35. doi: 10.1007/s11657-020-0709-8
33. Haq A, Wimalawansa SJ, Pludowski P, Anouti FA. Clinical practice guidelines for vitamin D in the United Arab Emirates. J Steroid Biochem Mol Biol. (2018) 175:4–11. doi: 10.1016/j.jsbmb.2016.09.021
34. Aburawi EH, Al Hamad S, Yasin J, Almekhaini LA, Souid AK. Dyslipidemia, subclinical inflammation, hepatic cholestasis and endothelial dysfunction in schoolchildren with excess fat: a study from the United Arab Emirates. Bhatnagar A, editor. PLoS One. (2019) 14(1):e0210316. doi: 10.1371/journal.pone.0210316
35. Deeb A, Attia S, Mahmoud S, Elhaj G, Elfatih A. Dyslipidemia and fatty liver disease in overweight and obese children. J Obes. (2018) 2018:1–6. doi: 10.1155/2018/8626818
36. Wang Y, Min J, Khuri J, Li M. A systematic examination of the association between parental and child obesity across countries. Adv Nutr. (2017) 8(3):436–48. doi: 10.3945/an.116.013235
37. Abdalla M, Halabi M, Kowash M, Hussein I, Khamis A, Salami A. Sleep-disordered breathing in children and adolescents seeking paediatric dental care in Dubai, UAE. Eur Arch Paediatr Dent. (2022) 23(3):485–94. doi: 10.1007/s40368-022-00697-8
38. Bachrach K, Danis DO, Cohen MB, Levi JR. The relationship between obstructive sleep apnea and pediatric obesity: a nationwide analysis. Ann Otol Rhinol Laryngol. (2022) 131(5):520–6. doi: 10.1177/00034894211028489
39. Dong Z, Xu X, Wang C, Cartledge S, Maddison R, Shariful Islam SM. Association of overweight and obesity with obstructive sleep apnoea: a systematic review and meta-analysis. Obes Med. (2020) 17:100185. doi: 10.1016/j.obmed.2020.100185
40. Gray JC, Schvey NA, Tanofsky-Kraff M. Demographic, psychological, behavioral, and cognitive correlates of BMI in youth: findings from the Adolescent Brain Cognitive Development (ABCD) study. Psychol Med. (2020) 50(9):1539–47. doi: 10.1017/S0033291719001545
41. Puhl RM, Lessard LM. Weight stigma and youth mental health: emerging evidence and policy implications. Lancet Child Adolesc Health. (2020) 4(8):697–708. doi: 10.1007/s13679-020-00408-8
42. Zuarub S, Stojanovska L, Ali HI. Barriers and facilitators of weight management among school children with obesity: a qualitative investigation of parents’ perceptions. Nutrients. (2022) 14(23):5117. doi: 10.3390/nu14235117
43. van Vuuren CL, Wachter GG, Veenstra R, Rijnhart JJM, van der Wal MF, Chinapaw MJM, et al. Associations between overweight and mental health problems among adolescents, and the mediating role of victimization. BMC Public Health. (2019) 19(1):612. doi: 10.1186/s12889-019-6832-z
44. Haleama AS, Abir A, Cheikh IL, Ayesha AD, Sharifa A, Siham A, et al. The association between food preferences, eating behavior, and body weight among female university students in the United Arab Emirates. Public Health. (2024) 12:Article 2024. doi: 10.3389/fpubh.2024.1395338
45. Al Sabbah H, Assaf EA, Al-Jawaldeh A, AlSammach AS, Madi H, Al Ali NK, et al. Nutrition situation analysis in the UAE: a review study. Nutrients. (2023) 15(2):363. doi: 10.3390/nu15020363
Keywords: paediatric obesity, sleep, psychosocial health, socio-economic status, obesity
Citation: Ashraf T, Pearce AL, Helal R, Saidi S, Vaidya CJ and Lessan N (2025) Physical, behavioural, and psychosocial factors associated with childhood and adolescent obesity: a study from the United Arab Emirates. Front. Pediatr. 13:1701873. doi: 10.3389/fped.2025.1701873
Received: 9 September 2025; Accepted: 24 October 2025;
Published: 14 November 2025.
Edited by:
Andrew M. H. Siu, Brunel University London, United KingdomReviewed by:
Risza Choirunissa, Diponegoro University, IndonesiaNihad Abdallah Selman, University of Babylon, Iraq
Copyright: © 2025 Ashraf, Pearce, Helal, Saidi, Vaidya and Lessan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tanveer Ashraf, dGFzaHJhZkBpY2xkYy5hZQ==
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
 Tanveer Ashraf
Tanveer Ashraf Alaina L. Pearce
Alaina L. Pearce Radwa Helal
Radwa Helal Sarah Saidi1
Sarah Saidi1 Chandan J. Vaidya
Chandan J. Vaidya Nader Lessan
Nader Lessan