- 1Paediatric Surgery, San Camillo-Forlanini Hospital, Rome, Italy
- 2Division of Paediatric Surgery, Department of Medical, Surgical and Neurological Sciences, University of Siena, Siena, Italy
Background: Acute gastric volvulus is a rare condition in children, and delayed diagnosis may lead to gastric ischemia, perforation, or even death. It is sometimes associated with a wandering spleen, a condition in which the spleen migrates from its normal anatomical position due to the absence of fixation ligaments. We report the first known case of a patient with Pitt–Hopkins syndrome (PTHS) presenting with simultaneous acute gastric volvulus and a wandering spleen.
Case report: A 6-year-old male with PTHS was urgently referred for acute abdominal pain and a 24 h history of non-bilious and non-bloody emesis. The x-ray showed a massive gastric dilatation, and an upper gastrointestinal series (UGI) revealed a gastric outlet obstruction. An emergency laparoscopy revealed a gastric mesoaxial volvulus with a hypotonic wall with no sign of ischemia or perforation associated with a wandering spleen. Gastropexy was performed by anchoring the gastric greater curvature to the anterior abdominal wall, covering the spleen in a good position in the left upper abdomen, completely covered by the gastric fundus. The patient made an uneventful recovery and was completely asymptomatic.
Conclusion: To our knowledge, this is the first reported case of simultaneous gastric volvulus and wandering spleen in a patient with PTHS. Laparoscopic gastropexy is a straightforward and effective procedure that combines the advantages of previously described surgical techniques.
Introduction
Gastric volvulus denotes the rotation of either the entirety or a segment of the stomach by at least 180° around an axis, leading to an obstruction within the foregut. This obstruction could manifest as acute, recurrent, intermittent, or chronic. There are three known types of gastric volvulus: organoaxial volvulus, mesenteroaxial volvulus, and combined volvulus (1). Wandering spleen is also a rare condition characterized by a migration of the spleen from its usual anatomical position, commonly to the lower abdomen or pelvis. Both defects are a result of the incomplete formation of the intraperitoneal suspensory ligaments and can sometimes be associated with surgical complications (2, 3). Their association is rare, but known in the literature, with several cases reported in the adult population (4–13) and also in the paediatric population (8, 14–20).
Pitt–Hopkins syndrome (PTHS) is a neurodevelopmental disorder with physical, cognitive, and behavioral characteristics, caused by deletions of or variants in the TCF4 gene located at 18q21.2, which encodes transcription factor 4 (21). Reliable prevalence figures have not been published, but based on the number of known affected individuals in the United Kingdom and the Netherlands, prevalence is estimated as one in 225,000–300,000 (22).
Patients with Pitt–Hopkins syndrome present with feeding difficulties, often constipation (80%–70%), and gastroesophageal reflux. Episodes of hyperventilation may cause aerophagia, resulting in excessive eructation and abdominal distension, which can be associated with discomfort or pain (23, 24).
In this paper, we report the first case report, to our knowledge, of simultaneous gastric volvulus and wandering spleen in a patient with Pitt–Hopkins syndrome.
Case description
A 6-year-old male with Pitt–Hopkins syndrome was urgently referred to our clinic for acute abdominal pain associated with a 24 h history of non-bilious and non-bloody emesis. The symptoms were also associated with lethargy and abdominal distension. He had no history of fever, diarrhea, toxic ingestion, or trauma.
On physical examination, he showed signs of dehydration, including dry mucous membranes and reduced skin turgor, as well as a firm, non-tender epigastric mass on abdominal palpation. A plain abdominal x-ray showed a massive gastric dilatation (Figure 1).
After intravenous resuscitation, a nasogastric tube was inserted, initially draining approximately 100–200 cc of gastric material, after which a second plain abdominal x-ray was performed and confirmed persistent gastric distension.
Since the stomach remained markedly dilated, a further aspiration was carried out, draining approximately an additional 1,000 cc of air and gastric content. At this stage, given the strong suspicion of gastric volvulus already raised by the radiographic findings and the significant decompression achieved, a CT scan was not performed. The patient remained hemodynamically stable, and as the radiologist felt confident in proceeding, an upper gastrointestinal (UGI) contrast study was performed to further clarify the diagnosis.
A barium study (Figure 2) demonstrated a partial rotation of the greater curvature toward the diaphragmatic side, raising suspicion of gastric volvulus, also supported by delayed gastric emptying. After intravenous resuscitation, the nasogastric tube was inserted, draining approximately 1,200 cc of gastric content with no evidence of bilious fluid. A repeat plain abdominal x-ray was performed, confirming the persistence of the volvulus.
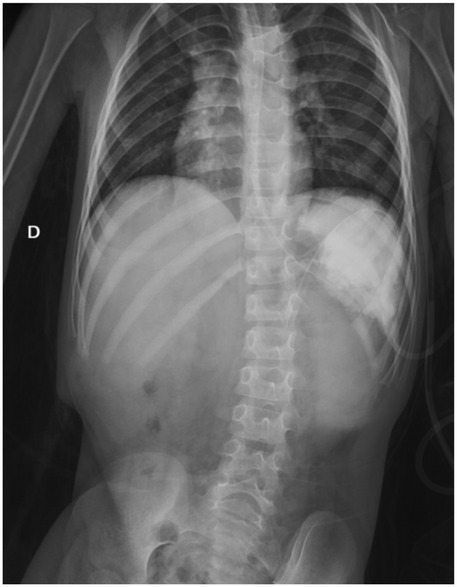
Figure 2. Plan abdominal x-ray after aspiration and UGI contrast showed partial rotation of the greater curvature toward the diaphragmatic side.
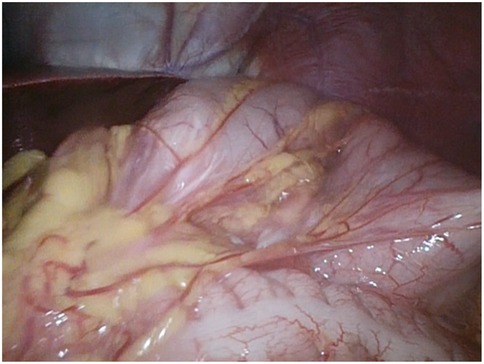
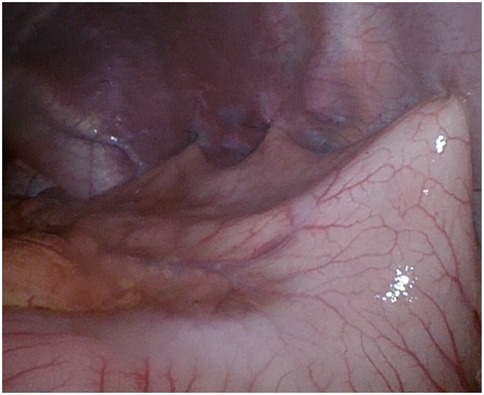
Due to the persistence of episodes of vomiting and the severe clinical condition, an urgent laparoscopic exploration was performed. A 10 mm trocar was inserted trans-umbilically, using the Hasson approach. A laparoscope (30°) was inserted through the umbilical port. Laparoscopic exploration revealed a gastric mesoaxial volvulus with a hypotonic wall with no sign of ischemia or perforation, associated with a wandering spleen, augmented in volume without normal supporting ligaments. The volvulus was promptly reduced (Figure 3), and the stomach began to regain its normal color almost immediately. The abdomen was copiously irrigated, and all other abdominal viscera were inspected and appeared normal. The diaphragm was examined on both sides and found to be normal. Faced with splenic viability, we decided to perform an isolated anterior gastropexy without splenectomy. Three additional working ports were inserted: left side and right side of the umbilicus and epigastrium. The spleen was then moved freely from its abnormal location (anterior abdominal wall) to its normal one (subdiaphragmatic). Gastropexy was performed by fixing the gastric greater curvature to the anterior abdominal wall, covering the spleen in a good position in the left upper abdomen, completely covered by the gastric fundus (Figure 4).
At the end of the procedure, we performed a gastroscopy with a flexible paediatric gastroscope to check the gastric mucosa. No tissue damage was found in the esophagus or inside the stomach (Figure 5). The duodenum showed no signs of tissue distress. Additionally, the orientation of the stomach was correct. This intraoperative gastroscopic evaluation also allowed direct assessment of gastric vitality, confirming the absence of ischemic or necrotic changes.
Postoperatively, the patient was transferred to the paediatric critical care unit for observation. Five days after surgery, the patient was discharged home without further complications. At the last follow-up 12 months after surgery, the patient was in good clinical condition, without further history of vomiting or any other symptoms.
At long-term follow-up, no impairment of gastric peristalsis was observed, and the patient maintained a normal feeding pattern, suggesting that the anterior gastropexy did not adversely affect gastric motility.
Discussion
Gastric volvulus is infrequent, with the incidence peaking after the fifth decade and adults comprising 80%–90% of the cases. It can be classified based on its etiology as primary or secondary. Primary (idiopathic) gastric volvulus is characterized by abnormalities of the gastric ligaments, such as agenesis, elongation, or disruption. Secondary gastric volvulus is observed in approximately two-thirds of patients with gastric volvulus and is attributed to various anatomical abnormalities, including paraesophageal hernia, diaphragmatic hernia or eventration, and phrenic nerve paralysis.
Additionally, anatomic abnormalities affecting other organs, especially the stomach or spleen, can also contribute to secondary gastric volvulus (25).
Wandering spleen is a rare condition characterized by a migration of the spleen from its usual anatomical position, commonly moving to the lower abdomen or pelvis. Its exact incidence is unknown and is likely underestimated. The peak incidence is reported between the ages of 20 and 40 but can also occur in the paediatric population. Similar to gastric volvulus, this condition is caused by defects in the abdominal ligaments that normally support the spleen (26, 27). Additionally, it has been reported to be associated with congenital defects (such as congenital diaphragmatic hernia or omphalocele) (28).
Rarely, an association between gastric volvulus and wandering spleen has been reported. Both conditions are associated with a failure of fusion of the mesogastrium with the posterior body wall, leading to incomplete formation of splenic supporting ligaments and facilitating gastric rotation (21).
The PTHS is characterized mainly by intellectual impairment, specific facial characteristics, and marked autonomic nervous system dysfunction, mainly involving respiration and intestinal mobility. Gastrointestinal manifestations are frequent and include constipation and gastroesophageal reflux disease. Moreover, hyper breathing due to disrupted regulation of respiration may lead to air swallowing with subsequent excessive burping and pain due to abdominal swelling. Conversely, structural visceral malformations are rarely observed in patients with PTHS (22).
We found no reported cases in the literature of gastric volvulus, with or without associated wandering spleen, in patients with Pitt–Hopkins syndrome. Nevertheless, we identified two cases of gastric volvulus associated with overeating and gastric distension: a 12-year-old girl (29) and a 28-year-old man (30).
Although this is the first reported case in the literature, we can speculate that gastric distension due to air ingestion typical of PTHS may have contributed to the onset of gastric volvulus in a patient with a predisposing anatomical configuration, notably of the abdominal ligaments. As shown in our case, gastric volvulus needs of a prompt diagnosis and treatment to reduce the mortality rate. When the stomach rotates more than 180°, indeed, it leads to complete obstruction of the gastric outlet, potentially resulting in ischemia, strangulation, necrosis, perforation, and abdominal sepsis. Cole and Dickinson (31) documented a mortality rate of 65% in case reports involving children with acute gastric volvulus prior to 1950.
Timely diagnosis is facilitated by recognizing common presentation patterns, such as the sudden onset of persistent, non-bilious vomiting, often accompanied by epigastric discomfort and bloating. Respiratory distress, cyanosis, or hematemesis may occur, albeit less frequently. Chest x-rays may reveal a prominently distended stomach situated at or above the diaphragm level, oriented either horizontally (organoaxial) or vertically (mesenteroaxial). In some cases, even more in patients with PTHS, who often present with gastric distension due to air ingestion in paraphysiologic conditions, further confirmation through advanced radiologic examinations may be necessary. In our case report, the diagnosis was supported by an UGI contrast study. Although a CT scan can also be useful, especially to assess associated anomalies, it is less commonly employed in paediatric patients. In emergency conditions such as gastric volvulus, however, prompt surgical exploration remains mandatory (32).
If gastric volvulus is confirmed and conservative treatment with a nasogastric tube fails, a surgical intervention is needed. Although it can be performed using either open or laparoscopic techniques. The last one has the undeniable advantage of allowing exploration of the abdominal cavity for associated malformations.
The choice of the surgical procedure, however, may vary based on associated pathological findings. In fact, although classically, the treatment of wandering spleen involved splenectomy, conservative treatment with splenopexy is now preferred. In 2010, Fiquet-Francois et al. (33) hypothesized that splenopexy might be associated with secondary splenic ischemia, whereas gastropexy alone might have the advantage of not manipulating the spleen.
However, a standardized surgical approach for gastric volvulus associated with a wandering spleen has not yet been established (34).
In our case report, given the spleen's good condition at the time of inspection, we decided to preserve it by repositioning it to its anatomical location in the left hypochondrium. We secured it in place with an anterior gastropexy, which also served to prevent recurrence of the gastric volvulus.
Conclusion
Gastric volvulus associated with wandering spleen is a rarely described condition in the paediatric age group, being potentially life-threatening if not immediately managed. The classical Borchardt triad is observed in approximately 50% of cases. Plain and contrast radiographs are helpful in the preoperative diagnosis. Laparoscopic exploration in this case has a dual relevance: diagnosis and therapy. Laparoscopic gastropexy for gastric volvulus associated with a wandering spleen is an easy procedure and combines the advantages of all surgical techniques adopted in previous eras. Clinicians caring for patients with Pitt–Hopkins syndrome, given their tendency toward aerophagia, over-breathing, and gastric distension, should consider the possibility of a gastric volvulus in the presence of compatible symptomatology. To our knowledge, this is the first case of gastric volvulus with wandering spleen in a patient affected by Pitt–Hopkins syndrome.
Ethics statement
Written informed consent was obtained from the minor(s)’ legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
GV: Conceptualization, Data curation, Resources, Writing – original draft. RA: Supervision, Validation, Writing – review & editing. GC: Writing – review & editing. MP: Supervision, Writing – review & editing. FM: Supervision, Writing – review & editing. LT: Writing – review & editing. CP: Supervision, Validation, Writing – review & editing. VB: Conceptualization, Investigation, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence, and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cribbs RK, Gow KW, Wulkan ML. Gastric volvulus in infants and children. Pediatrics. (2008) 122(3):e752–62. doi: 10.1542/peds.2007-3111
2. Dalgaard JB. Volvulus of the stomach: case report and survey. Acta Chir Scand. (1952) 103(2):131–53.14943396
3. Eek S, Hagelsteen H. Torsion of the stomach as a cause of vomiting in infancy. Lancet. (1958) 1(7010):26–8. doi: 10.1016/S0140-6736(58)92518-2
4. Hanifa H, Al-Shami K, Al-Shaher T, Ataya J, Al-Abrass M, Moezzen H, et al. Gastric volvulus with necrosis and gangrene associated with wandering spleen: a rare case report from Syria. SAGE Open Med Case Rep. (2024) 12. doi: 10.1177/2050313X241262141
5. Belayneh ES, Belete AW, Mitku A, Ahmed HM, Yirdaw H, Ketema T. Gastric volvulus and splenopancreatic torsion with wandering spleen: a case report. Int J Surg Case Rep. (2024) 116:109338. doi: 10.1016/j.ijscr.2024.109338
6. Chopko TC, Schassberger M, Bingener J. Mesenteroaxial volvulus due to wandering spleen: a unique repair via mesenteric splenopexy and gastropexy. BMJ Case Rep. (2023) 16:e258235.38011954
7. Basu S, Pratap A, Bhartiya SK, Shukla VK. Wandering spleen and acute gastric volvulus in an elderly woman with acute abdomen: a case report. Clin Exp Gastroenterol. (2023) 16:181–5. doi: 10.2147/CEG.S428679
8. Bhambu SK, Awasthi PK, Mangal R, Mehta R, Shreyas N. Acute gastric volvulus with wandering spleen in a two-year-old child: a rare association. Cureus. (2023) 15(5):e38386. doi: 10.7759/cureus.38386
9. Shen MR, Barrett M, Waits S, Williams AM. Wandering spleen leading to splenic torsion with gastric and pancreatic volvulus. BMJ Case Rep. (2021) 14:e235918. doi: 10.1136/bcr-2020-235918
10. Karaisli S, Acar T, Acar N, Kamer E, Hacıyanlı M. Torsion of wandering spleen nine years after gastric volvulus: effect of multiparity? Ulus Travma Acil Cerrahi Derg. (2020) 26(3):489–92. doi: 10.14744/tjtes.2019.91606
11. Mocanu SN, Cáceres Díez M, Garay Solà M. Atypical mesenteroaxial gastric volvulus with wandering spleen as a late complication of vagotomy and pyloromyotomy for peptic duodenal ulcer. ANZ J Surg. (2020) 90(12):E186–7. doi: 10.1111/ans.15966
12. Gandhi C, Fowler RL, Hersey S, Heffernan DS, Stafford T. Wandering spleen in a geriatric patient—a rare presentation of gastric volvulus. JRSM Open. (2019) 10(6). doi: 10.1177/2054270419851325
13. Asafu Adjaye Frimpong G, Aboagye E, Ayisi-Boateng NK, Antwi K, Bawuah KA, Coleman NE, et al. Concurrent occurrence of a wandering spleen, organoaxial gastric volvulus, pancreatic volvulus, and cholestasis—a rare cause of an acute abdomen. Radiol Case Rep. (2019) 14(8):946–51. doi: 10.1016/j.radcr.2019.05.018
14. Garcia JA, Garcia-Fernandez M, Romance A, Sanchez JC. Wandering spleen and gastric volvulus. Pediatr Radiol. (1994) 24:535–6. doi: 10.1007/BF02015024
15. Uc A, Kao SC, Sanders KD, Lawrence J. Gastric volvulus and wandering spleen. Am J Gastroenterol. (1998) 93(7):1146–8. doi: 10.1111/j.1572-0241.1998.00349.x
16. François-Fiquet C, Belouadah M, Chauvet P, Lefebvre F, Lefort G, Poli-Merol ML. Laparoscopic gastropexy for the treatment of gastric volvulus associated with wandering spleen. J Laparoendosc Adv Surg Tech A. (2009) 19(Suppl 1):S137–9. doi: 10.1089/lap.2008.0091.supp
17. Oyachi N, Numano F, Fukatsu T, Nemoto A, Naito A. Volvulus of the stomach and wandering spleen after repair of congenital diaphragmatic hernia: unexpected manifestations in a neonate. Surg Case Rep. (2022) 8(1):178. doi: 10.1186/s40792-022-01537-z
18. Kataria R, Sundaram J, Agarwal P, Lal T. Laparoscopic management of gastric volvulus, diaphragmatic eventration and wandering spleen in a child. BMJ Case Rep. (2021) 14:e242441.34162614
19. Umeda S, Kimura K, Takama Y, Yamauchi K, Yonekura T. Laparoscopic retroperitoneal splenopexy for wandering spleen: a novel technique using a three-incision retroperitoneal pouch. Asian J Endosc Surg. (2021) 14(3):644–7. doi: 10.1111/ases.12894
20. Okazaki T, Ohata R, Miyano G, Lane GJ, Takahashi T, Yamataka A. Laparoscopic splenopexy and gastropexy for wandering spleen associated with gastric volvulus. Pediatr Surg Int. (2010) 26:1053–5. doi: 10.1007/s00383-010-2657-7
21. Pitt D, Hopkins I. A syndrome of mental retardation, wide mouth and intermittent overbreathing. Aust Paediatr J. (1978) 14(3):182–4. doi: 10.1111/jpc.1978.14.3.182
22. Zollino M, Zweier C, Van Balkom ID, Sweetser DA, Alaimo J, Bijlsma EK, et al. Diagnosis and management in Pitt-Hopkins syndrome: first international consensus statement. Clin Genet. (2019) 95(4):462–78. doi: 10.1111/cge.13506
23. de Winter CF, Baas M, Bijlsma EK, van Heukelingen J, Routledge S, Hennekam RC. Phenotype and natural history in 101 individuals with Pitt-Hopkins syndrome through an internet questionnaire system. Orphanet J Rare Dis. (2016) 11:37. doi: 10.1186/s13023-016-0422-2
24. Grubišić V, Kennedy AJ, Sweatt JD, Parpura V. Pitt-Hopkins mouse model has altered particular gastrointestinal transits in vivo. Autism Res. (2015) 8(5):629–33. doi: 10.1002/aur.1467
25. Wasselle JA, Norman J. Acute gastric volvulus: pathogenesis, diagnosis, and treatment. Am J Gastroenterol. (1993) 88(10):1780–4.8213725
26. Rashid F, Thangarajah T, Mulvey D, Larvin M, Iftikhar SY. A review article on gastric volvulus: a challenge to diagnosis and management. Int J Surg. (2010) 8(1):18–24. doi: 10.1016/j.ijsu.2009.11.002
27. Wu MH, Chang YC, Wu CH, Kang SC, Kuan JT. Acute gastric volvulus: a rare but real surgical emergency. Am J Emerg Med. (2010) 28(1):118.e5–7. doi: 10.1016/j.ajem.2009.04.031
28. Cantone N, Gulia C, Miele V, Trinci M, Briganti V. Wandering spleen and organoaxial gastric volvulus after Morgagni hernia repair: a case report and review of the literature. Case Rep Surg. (2016) 2016:6450765. doi: 10.1155/2016/6450765
29. Chung YS. Acute primary gastric volvulus occurring after overeating in a 12-year-old girl. Pediatr Emerg Med J. (2021) 8(2):104–7. doi: 10.22470/pemj.2021.00388
30. De’Ath HD, Kelly JJ. Overeating and a wandering spleen: what is the link? Gastroenterology. (2019) 157(6):e11–2. doi: 10.1053/j.gastro.2019.07.022
31. Cole BC, Dickinson SJ. Acute volvulus of the stomach in infants and children. Surgery. (1971) 70(5):707–17.5120891
32. Stephenson RH, Hopkins WA. Volvulus of the stomach complicating eventration of the diaphragm: report of a case. Am J Gastroenterol. (1964) 41:225–34.14134419
33. Fiquet-Francois C, Belouadah M, Ludot H, Defauw B, Mcheik JN, Bonnet JP, et al. Wandering spleen in children: multicenter retrospective study. J Pediatr Surg. (2010) 45(7):1519–24. doi: 10.1016/j.jpedsurg.2010.03.003
Keywords: gastric volvulus, wandering spleen, Pitt–Hopkins syndrome, laparoscopic gastropexy, paediatric surgery case report
Citation: Vasta G, Angotti R, Contini G, Perrotta ML, Molinaro F, Tarallo L, Plessi C and Briganti V (2025) Gastric volvulus and wandering spleen in Pitt–Hopkins syndrome: first paediatric case report. Front. Pediatr. 13:1705547. doi: 10.3389/fped.2025.1705547
Received: 15 September 2025; Accepted: 5 November 2025;
Published: 25 November 2025.
Edited by:
Hiroo Uchida, Nagoya University Graduate School of Medicine, JapanReviewed by:
Satoshi Obata, Fukuoka University School of Medicine and Hospital, JapanAttila Vastyan, University of Pécs, Hungary
Copyright: © 2025 Vasta, Angotti, Contini, Perrotta, Molinaro, Tarallo, Plessi and Briganti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriele Vasta, Z2FicmllbGUudmFzdGFAaG90bWFpbC5pdA==
 Gabriele Vasta
Gabriele Vasta R. Angotti
R. Angotti G. Contini
G. Contini M. L. Perrotta1
M. L. Perrotta1 F. Molinaro
F. Molinaro C. Plessi
C. Plessi