- 1Department of Cardiology, The First Affiliated Hospital With Nanjing Medical University, Nanjing, China
- 2Department of Cardiology, Northern Jiangsu Province Hospital and Clinical Medical College, Yangzhou University, Yangzhou, China
- 3Department of Cardiology, The First Affiliated Hospital of Soochow University, Suzhou, China
- 4Department of Pathogenic Microorganism, Nanjing Medical University, Nanjing, China
- 5Key Laboratory of Antibody Technique of National Health Commission of China, Department of Pathogen Biology, Nanjing Medical University, Nanjing, China
- 6Department of Cardiology, Xuyi People’s Hospital, Huai’an, China
- 7Department of Laboratory Medicine, The Affiliated Wuxi No.2 People’s Hospital of Nanjing Medical University, Wuxi, China
Purpose: To determine the incidence and risk factors of bleeding events as well as assess the performance of the PRECISE-DAPT score in elderly patients (≥75 years) who underwent percutaneous coronary intervention (PCI) and one-year dual antiplatelet therapy (DAPT).
Methods: A total of 940 patients (≥75 years) who received PCI and one-year DAPT were retrospectively enrolled into the study. The multivariable logistic regression analysis was conducted to identify risk factors of antiplatelet-related bleeding complications. The receiver operating characteristic (ROC) curve analysis and the Delong test were performed to obtain the optimized PRECISE-DAPT score.
Results: It was observed that 89 (9.47%) patients suffered bleeding complications, while 37 (3.94%) of them had the Bleeding Academic Research Consortium (BARC, type ≥2) bleeding events. We stratified the PRECISE-DAPT score in tertiles (T1: ≤23; T2:24 to 32; T3: ≥33) and found that BARC ≥ 2 type bleeding occurred more frequently in T3 than in T1 and T2 (8.25 vs. 1.46% vs. 2.40%, p <0.05). The ROC curve analysis revealed that the PRECISE-DAPT score cutoff for BARC ≥2 type bleeding prediction was 33. In comparison with the current recommended cutoff score of 25 (AUC: 0.608, based on ROC analysis), the Delong test indicated significantly improved ability for predicting BARC ≥ 2 type bleeding events using the proposed cutoff value of 33, AUC of 0.676 (p = 0.03), and Brier Score of 0.04. The multivariable logistic regression analysis demonstrated that the PRECISE-DAPT score ≥ 33 [OR: 3.772; 95% CI (1.229, 11.578); p = 0.02] was associated with BARC ≥ 2 type bleeding event, along with a history of hemorrhagic stroke [OR: 6.806; 95% CI (1.465, 31.613); p = 0.014], peptic ulcer [OR: 3.871; 95% CI (1.378, 10.871); p = 0.01], and/or myocardial infarction [MI, OR: 3.081; 95% CI (1.140, 8.326); p = 0.027].
Conclusion: A higher PRECISE-DAPT score of 33 might be a more reasonable cutoff value for predicting BARC ≥2 type bleeding risk in CAD patients (≥75 years). In addition, the history of hemorrhagic stroke, peptic ulcer, and myocardial infarction were identified as the risk factors of BARC ≥2 type bleeding events.
Introduction
Age is a risk factor for coronary artery diseases (CADs) (Shanmugam et al., 2015). Thus, an increasing number of the elderly population (aged ≥75 years) usually develop CAD, wherein percutaneous coronary intervention (PCI) is considered as the definitive treatment option. Dual antiplatelet therapy (DAPT), consisting of aspirin with a P2Y12 receptor inhibitor (mainly clopidogrel and ticagrelor in participating centers), is an essential treatment regimen in patients undergoing PCI with decreased risks of ischemic complications but increased risks of bleeding, wherein the condition can sometimes be fatal and culminate in adverse clinical events (Wang et al., 2011; Levine et al., 2016; Tammam et al., 2017; Palmerini et al., 2017a; Xu et al., 2018). Elderly patients are a special group in CAD studies since they present with extensive atherosclerosis, complex lesions, comorbidities, and increased incidences of both thrombosis and bleeding (Wang et al., 2011; Shanmugam et al., 2015; Arahata and Asakura, 2018). Nevertheless, an existing evidence showed that the elderly remained as an underrepresented group in clinical trials (Dodd et al., 2011). Bleeding risk is regarded as an important limiting factor that affects patient’s decision for the antithrombotic strategies (Almendro-Delia et al., 2017), and thus, existing guidelines recommend careful consideration for complications of bleeding risk during DAPT (Valgimigli et al., 2017; Kedhi et al., 2018; Mazlan-Kepli et al., 2019). Besides, a careful assessment of bleeding risk may change the prognosis of the patients. Several bleeding risk scores, namely, CRUSADE, ACUITY, and PRECISE-DAPT scores, have been proposed albeit having a lower representation of the elderly patients. Notwithstanding, the PRECISE-DAPT score is recommended (by the European Society of Cardiology guidelines) as a guide for the length of DAPT (Subherwal et al., 2009; Mehran et al., 2010; Ariza-Solé et al., 2014; Faustino et al., 2014; Valgimigli et al., 2017; Choi et al., 2018). The PRECISE-DAPT score is a simple tool that was developed with five items (age, creatinine clearance, hemoglobin, white blood cell count, and previous spontaneous bleeding). Importantly, it can be applied in daily clinical practice to assess bleeding risks during the initiation of treatment (Costa et al., 2017). Current guidelines suggest a relative conservative antiplatelet approach in patients with the PRECISE-DAPT score above the recommended 25 cutoff value (Valgimigli et al., 2017). However, only few studies have assessed the predictive ability of the PRECISE-DAPT score in CAD patients (≥75 years). In this study, we investigated the clinical factors of the Bleeding Academic Research Consortium (BARC, type ≥2) bleeding events in elderly patients (≥75 years) who received coronary stenting and one-year DAPT. Also, the performance of the PRECISE-DAPT score to predict bleeding complications in patients (≥75 years) was evaluated.
Of note, this article has been presented in accordance with the STROBE reporting checklist.
Methods
This was a multicenter, retrospective study conducted among CAD patients (≥75 years) who received DAPT after PCI, with implantation of drug-eluting stents (DESs) from three hospitals (viz., the first affiliated hospital with Nanjing Medical University, the first affiliated hospital of Soochow University, and affiliated hospital of Yangzhou University), regardless of being presented with acute coronary syndromes or chronic coronary syndromes (from September 2016 to June 2018). All the CAD patients who met the inclusion criteria were retrospectively selected from the medical electronic database at the three centers. The criteria were as follows: 1) age equal to or older than 75 years, 2) patients who received PCI treatment between September 2016 and June 2018, and 3) all the patients received one-year DAPT therapy, except for some of them changed to single antiplatelet therapy (SAPT) treatment due to bleeding complications. In addition, patients were excluded due to the following reasons: 1) contraindications to DAPT, namely, active bleeding, peptic ulcer, or allergic to one or more antiplatelet drugs; 2) bleeding complications that were not caused by antiplatelet therapy, such as trauma; 3) hematological disorders; 4) complications of serious diseases like malignant tumor with less than 1-year life expectancy; and 5) incomplete follow-up data due to loss of contact. Furthermore, patients with a history of PCI intervention or coronary artery bypass surgery within 1 year before enrollment were also excluded in order to rule out a possible increased bleeding risk associated with prolonged DAPT. The study protocol was conducted in accordance with the Declaration of Helsinki and was approved by the institutional ethics committee of each participating center (No. 2020-SR-472). Informed consent of the participants was waived in the study and approved by our ethical committee.
The clinical and laboratory variables at the time of index PCI for the analysis were collected retrospectively from the hospital medical electronic database. The clinical parameters included demographics, risk factors and previous histories, clinical presentations, laboratory examinations, angiographic and procedural characteristics, PRECISE-DAPT score, and discharge medication information. All patients who met the inclusion criteria were called (at least 1 year) after admission for the PCI in order to obtain the end point information. End point events referred to those bleeding complications that happened at any time between the starting of the DAPT regimen and the end of the 1-year follow-up time. Furthermore, the bleeding outcomes were further confirmed in some of the patients by checking their outpatient visit record or reviewing their related medical electronic record. The creatinine clearance rate (cCr) was calculated using Cockcroft–Gault equation. The PRECISE-DAPT score was calculated for all the patients through the web calculator (http://www.precisedaptscore.com/predapt/).
The clinical bleeding outcomes included complications caused by DAPT within 1 year after PCI in accordance with the BARC criteria (Supplementary Table S1) (Mehran et al., 2011). Bleeding events were subgrouped by BARC ≥2 type bleeding events (excluding BARC four type) and BARC <2 type bleeding events.
Continuous variables were presented as mean ± SD for normally distributed variables or median with IQR (interquartile range) (Q1–Q3) for non-normally distributed variables, while categorical variables were expressed as frequencies (percentages). Continuous variables were compared using the one-way ANOVA or Kruskal–Wallis H test, while the Pearson χ2 or Fisher exact test was used to compare categorical parameters. The incidence of bleeding events was calculated by dividing the number of patients who had bleeding events with the total number of patients in the subgroup. Since advanced age may push the PRECISE-DAPT score toward right, we stratified the PRECISE-DAPT score into tertiles to see if a higher score may relate to a higher incidence of bleeding events because the current recommended cutoff value of 25 might be too low for elderly patients in clinical practice. Furthermore, the optimal cutoff value of the PRECISE-DAPT score for the elderly patients was obtained through the receiver operating characteristic (ROC) curve analysis. In order to compare the predictive ability of bleeding events between the newly proposed PRECISE-DAPT cutoff score of 33 and the current recommended score of 25 in elderly patients, two cutoff values were, respectively, calculated for ROC curves and Brier scores. Meanwhile, the Delong test was used to determine the difference between two areas under the curves (AUCs) of ROC curves. Variables that were statistically significant in the univariate analysis were further analyzed in the multivariate logistic regression analysis. The univariate and multivariable binomial logistic regression analyses were performed to determine the clinical risk factors of bleeding events, and the results were expressed as the odds ratios (ORs) with corresponding 95% confidence intervals (CIs). All statistical analyses were performed using SPSS23.0 software or R language software, where appropriate. A two-sided p‐value of <0.05 was considered statistically significant.
Results
Baseline Characteristics
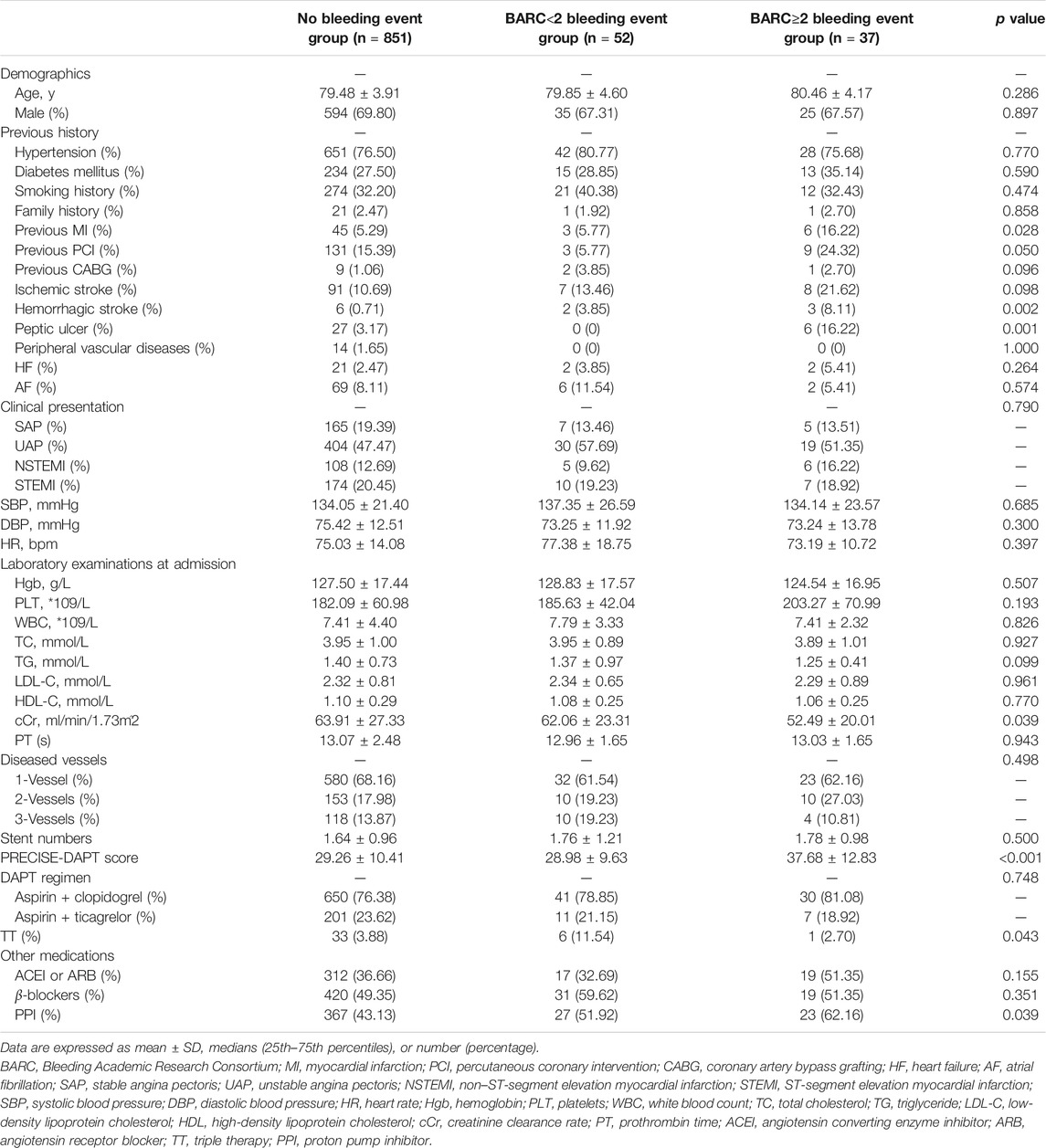
A total of 940 CAD patients (aged ≥75 years) who received PCI treatment were enrolled in this study. Their mean age was 79.54 ± 3.96 years, with 69.57% of the patients being male. Among them, 12.13% of the patients were 85 years or older. Meanwhile, 177 patients (18.83%) were diagnosed with stable angina (SA), 453 patients (48.19%) with unstable angina (UA), 119 patients (12.66%) with non–ST-segment elevation myocardial infarction (NSTEMI), and 191 patients (20.32%) with ST-segment elevation myocardial infarction (STEMI). In terms of the DAPT regimen, 721 patients (76.70%) used aspirin with clopidogrel, while 219 patients (23.30%) used aspirin with ticagrelor after discharge. Within 1 year after PCI, 89 patients (9.47%) suffered from bleeding complications, namely, 37 (3.94%) with BARC ≥2 (excluding BARC 4) bleeding events and 52 (5.53%) with BARC <2. Notably, 46 patients switched to SAPT due to bleeding events, while five permanently stopped antiplatelet treatment owing to recurrent bleeding complications. The most common locations where bleeding occurred were digestive, intracranial, nasal and oral, or urological. Characteristics of the patients are shown in Table 1. Compared with the no bleeding group, patients with BARC (type ≥2) bleeding events had a significantly lower cCr (52.49 ± 20.01 vs. 63.91 ± 27.33 ml/min, p = 0.031) and a higher PRECISE-DAPT score (37.68 ± 12.83 vs. 29.26 ± 10.41, p < 0.001). More patients with BARC ≥2 type bleeding events showed a history of myocardial infarction (MI) (16.22 vs. 5.29%, p = 0.011), hemorrhagic stroke (8.11 vs. 0.71%, p = 0.005), and peptic ulcer (16.22 vs. 3.17%, p = 0.002) than the patients without bleeding events. In comparison with the BARC <2 type bleeding event group, patients in the BARC ≥2 type bleeding event group had a higher PRECISE-DAPT score (37.68 ± 12.83 vs. 28.98 ± 9.63, p < 0.001), while more patients exhibited a history of PCI (24.32 vs. 5.77%, p < 0.05) and peptic ulcer (16.22 vs. 0%, p = 0.004).
Performance of the PRECISE-DAPT Score in Predicting the Bleeding Events in Elderly Patients
Patients were divided into low score (<25) and high score groups (≥25) according to the recommended PRECISE-DAPT score cutoff value of 25 (Figure 1). In the high-score group, the incidence of BARC ≥2 type bleeding events was significantly higher (5.05 vs. 1.84%, p = 0.016) than that in the low-score group. However, no significant difference was observed in BARC <2 type bleeding events between the two groups (5.32 vs. 6.56%, p = 0.442). We further stratified the PRECISE-DAPT score into low [<the 33rd percentile (
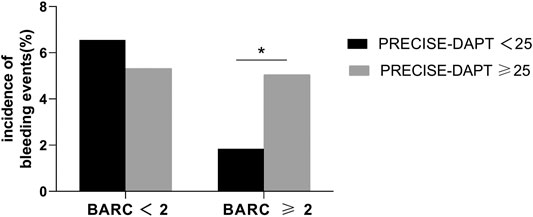
FIGURE 1. Incidence of bleeding events in patients with the PRECISE-DAPT score <25 or ≥25. The incidence of BARC ≥2 type bleeding events was higher in patients with the PRECISE-DAPT score ≥25 (5.05%) than in those with the PRECISE-DAPT score <25 (1.84%). * indicates p < 0.05. No significant difference was observed in BARC <2 bleeding events.
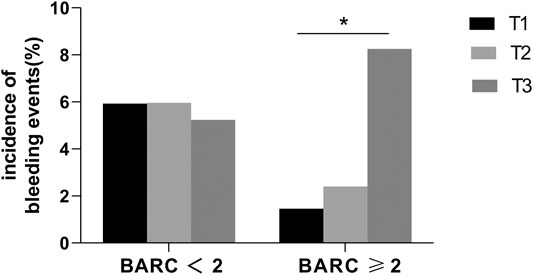
FIGURE 2. Incidence of bleeding events in low (T1), medium (T2), and high (T3) PRECISE-DAPT score groups. Low PRECISE-DAPT score: <the 33rd percentile (≤23), medium PRECISE-DAPT score: from the 33rd percentile to the 67th percentile (24–32), and high PRECISE-DAPT score: >the 67th percentile (≥33). The incidence of BARC ≥2 type bleeding events was significantly higher in the high PRECISE-DAPT score group (8.25%) than in the low (1.46%) and middle (2.40%) groups. * indicates p < 0.05. No significant difference was observed in BARC <2 bleeding events.
The ROC curve of the PRECISE-DAPT score for BARC ≥2 type bleeding prediction is shown in Figure 3A, with an area under the curve (AUC) of 0.697 [95% CI (0.609, 0.784); p < 0.001]. The cutoff value obtained for the PRECISE-DAPT score via the ROC curve was 33, which was similar to the 67th percentile of the same score. When compared to the ROC of the current recommended cutoff value of 25 (AUC: 0.608), the cutoff value of 33 revealed an AUC of 0.676 (p = 0.03 with Delong test) (Figure 3B) and a Brier score of 0.04, indicating a significant improvement in the ability of newly proposed 33 (cutoff value) to predict BARC ≥2 type bleeding events in elderly patients.
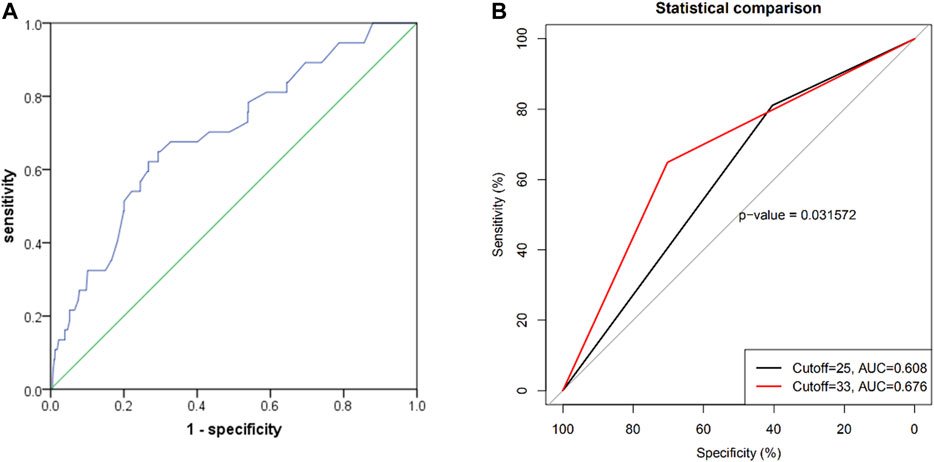
FIGURE 3. (A) Receiver operating characteristic curve for the prediction of BARC ≥2 type bleeding events by PRECISE-DAPT risk score systems in elderly patients with 1-year DAPT after PCI [AUC: 0.697; 95% CI (0.609, 0.784); p < 0.001]; (B) the comparison between the ROC curves of the PRECISE-DAPT score of 25 and the newly proposed cutoff score of 33 for prediction on the 1-year BARC ≥2 type bleeding events (p = 0.03).
Risk Factors of BARC ≥2 Type Bleeding Events in Elderly Patients With One-Year DAPT After PCI
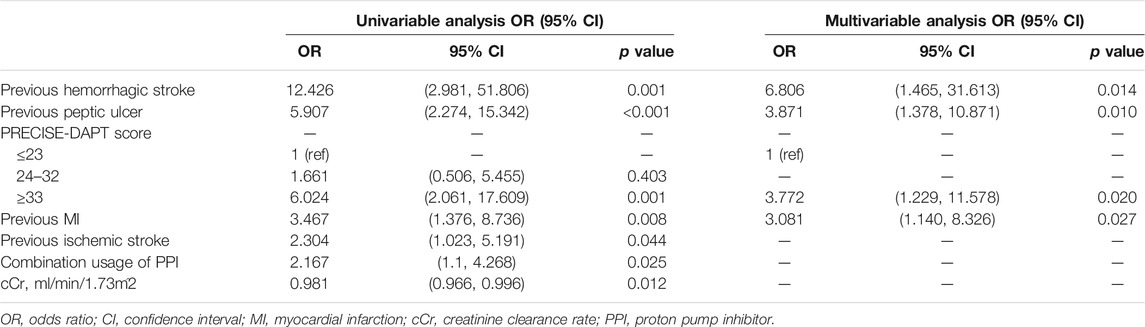
The univariate logistic regression analysis showed that the PRECISE-DAPT score ≥33, history of MI, ischemic stroke, hemorrhagic stroke and peptic ulcer, combined usage of PPI, and cCr were independent risk factors for BARC ≥2 type bleeding events. Multivariable logistic regression analysis further demonstrated that the PRECISE-DAPT score ≥33 [OR: 3.772; 95% CI (1.229, 11.578); p = 0.02] remained a significant risk factor for BARC ≥2 type bleeding events, together with the history of hemorrhagic stroke [OR: 6.806; 95% CI (1.465, 31.613); p = 0.014], peptic ulcer [OR: 3.871; 95% CI (1.378, 10.871); p = 0.01], or previous MI [OR: 3.081; 95% CI (1.140, 8.326); p = 0.027] (Table 2).
Discussion
In this retrospective study of patients (aged ≥75 years) who were treated with DAPT following PCI, two main findings were revealed (Shanmugam et al., 2015): the PRECISE-DAPT is an effective score system which can predict one-year bleeding events in elderly patients over 75 years. However, a higher score of 33, rather than the recommended 25, might be a more reasonable cutoff value for the PRECSE-DAPT score to diagnose BARC ≥2 type bleeding complications in elderly patients (Wang et al., 2011). The history of hemorrhagic stroke, peptic ulcer, and MI were the predominant risk factors associated with BARC ≥2 type bleeding complications in CAD patients (aged ≥75 years) who received PCI and one-year DAPT.
DAPT-related bleeding which led to higher mortality, lower life quality, and higher medical service charges has been identified as a common complication after PCI (Khandelwal et al., 2012; Amin et al., 2013). A higher incidence of bleeding complications has been found to be common in acute coronary syndrome patients (over 75 years) than in their younger counterparts (Alonso Salinas et al., 2018). Thus, antiplatelet therapy–associated bleeding risk increases with age (Li et al., 2017). To buttress this point, Oxford Vascular Study Group recently analyzed 3,166 patients who received secondary prevention (mostly with aspirin). The authors observed that the general bleeding risk in patients (≥75 years) increased by a 3.1 fold with the risk of fatal bleeding also increasing by 5.5 fold (Arahata and Asakura, 2018). Recently, an increased bleeding risk in older adults has been ascribed to more cardiovascular risk factors, complex anatomical structures, additional comorbidities, functional decline of important organs (including kidney, liver, and brain), platelet hyperreactivity, hemodynamic instability, combinatory usage of multiple medications, and frailty (Ariza-Solé et al., 2014; Shanmugam et al., 2015; Schoenenberger et al., 2016; Arahata and Asakura, 2018; Martí et al., 2020). Herein, the incidence of BARC ≥2 type (excluding BARC four type) bleeding events in elderly patients was 3.94%, while the BleeMACS sub-study involving 3,376 ACS patients (aged ≥75 years) reported the incidence of severe bleeding after discharge to be 5.6% (Garay et al., 2018). Several other studies have shown a higher incidence of major bleeding events than that in our study (Sharma et al., 2017; Chen et al., 2019; Shimizu et al., 2019; Martí et al., 2020), which may be due to the inclusion of more lower bleeding risk subjects, such as stable CAD patients in our study.
Several bleeding risk scores have been proposed to predict the occurrence of bleeding complications (Costa et al., 2017; Pavasini et al., 2019). Previous research studies suggested that the CRUSADE score might be the most appropriate tool to predict major bleeding events. However, the score was proven to be suitable for predicting in-hospital bleeding, wherein Faustino A et al., reported less ability of the score to discriminate major bleeding events in NSTE-ACS octogenarians, thus indicating its limited application in elderly population (Subherwal et al., 2009; Faustino et al., 2014; Choi et al., 2018). The PRECISE-DAPT score is a simple tool with only five items from eight multicenter randomized clinical trials for weighing the risk of post-discharge bleeding to provide an effective tool for guiding the duration of DAPT (Choi et al., 2018; Costa et al., 2019a). PRECISE-DAPT series had a fewer involvement of older patients with their mean age ranging 60–65 years, while patients (≥75 years) accounted for only ∼25% (Choi et al., 2018; Guerrero et al., 2018). Since advanced age may push the PRECISE-DAPT score toward right, it is necessary to investigate whether the PRECISE-DAPT scoring system is still suitable for assessing the bleeding risk in elderly CAD patients, amidst the criteria for determining an optimal cutoff value for this score remain unanswered. There are limited studies on the performance of the PRECISE-DAPT score in older patients. Our results demonstrated that the PRECISE-DAPT score has the potential to predict BARC ≥2 type bleeding events in elderly CAD patients who received DAPT following PCI, despite its limited predictive ability upon applying the recommended cutoff value of 25. Previous study further suggested that a cutoff value of the PRECISE-DAPT score of ≥25 might be too low for elderly patients to be used in clinical practice (Costa et al., 2019b). In this regard, we stratified the PRECISE-DAPT score into tertiles (T1:≤23; T2:24 to 32; T3:≥33) and found that BARC ≥2 type bleeding events occurred more frequently in T3 versus T1 [odds ratio: 3.772; 95% confidence interval (1.229, 11.578); p = 0.02]. Interestingly, the comparison between the AUCs under the ROC curves of the current recommended cutoff value of 25 and the newly proposed 33 via the Delong test further indicated significant improvement in the ability of latter to predict the one-year BARC ≥2 type bleeding events compared to the former. The IFFANIAM study confirmed that the quartiles of PRECISE-DAPT values, rather than the recommended 25 value, showed good performance in assessing bleeding risk in elderly STEMI patients (Guerrero et al., 2018). Therefore, further studies should be conducted on the performance of the PRECISE-DAPT score to evaluate the bleeding complications in the elderly patients.
Severe bleeding complications may result in an increased mortality, cessation of antiplatelet drugs, and potential ischemic events, especially in the elderly patients (Lopes et al., 2012; Ndrepepa et al., 2014; Palmerini et al., 2017b). Numerous data have indicated that Asians displayed a higher bleeding risk than the western natives (Levine et al., 2014). Therefore, it is important for us to identify risk factors of bleeding and perform accurate risk stratification. Our regression analysis confirmed that the PRECISE-DAPT score system was efficient for predicting BARC ≥2 type bleeding events in elderly patients with an optimized cutoff score. In addition, it was further observed in this study that the history of hemorrhagic stroke, peptic ulcer, and MI were the main risk factors to predict BARC ≥2 type bleeding complications in CAD patients (≥75 years) and those undergoing one-year DAPT following PCI. As elderly patients with a history of bleeding or MI had a higher risk of BARC ≥2 type bleeding, it is therefore important to tailor the DAPT regimen for patients (≥75 years) undergoing PCI. The usage of PPI was supposed to have a protective role to reduce the gastrointestinal bleeding risk in CAD patients who received antiplatelet treatment (Khan et al., 2019); however, no association was found between the use of PPI and the reduction of BARC ≥2 type bleeding events in elderly patients in our study. The reasons may be due to the irregular usage of PPIs in the clinics and the limited number of patients enrolled in our study. Therefore, more studies are needed to investigate the correlation between PPI use and the reduction of bleeding risk so as to guide the rational for using PPI in clinical practice.
Several limitations in our study should be considered. First, this is a retrospective study with a relatively small sample size and a lower incidence of bleeding complications in comparison with other studies. Second, bleeding events were reported by patients, which may lead to some inaccuracy and bias. Third, although we analyzed a number of possible risk factors, some other predisposing factors such as frailty, malignant tumor, and revascularization procedure were not assessed in our study.
In conclusion, our study revealed that the current recommended PRECISE-DAPT score cutoff value of 25 might be useful in predicting BARC ≥2 type bleeding events. However, a higher cutoff value of 33 was more suitable in predicting BARC ≥2 type bleeding complications among elderly patients (≥75 years) who received DAPT following PCI. In addition, a history of hemorrhagic stroke, peptic ulcer, and MI provided additional information for the prediction of BARC ≥2 type bleeding events in elderly patients who underwent PCI and one-year DAPT.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University. The ethics committee waived the requirement of written informed consent for participation.
Author Contributions
Conception and design: JW and ZH; administrative support: XL, SB, ZH, and JW; provision of study materials or patients: BX, XQ, XL, and JW; collection and assembly of data: YQ, LC, and YC; data analysis and interpretation: YQ, BX, XQ, LC, and YC; manuscript writing: all authors; final approval of manuscript: all authors.
Funding
This work was supported by the National Natural Science Foundation of China (NSFC 81570328, JW), the Jiangsu Province “333” project (BRA2018389, JW) and the Jiangsu Province’s Key Provincial Talents Program (ZDRCB2016005, JW), the Jiangsu health and family planning commission project (No. Z2019042, SB), and Key Talents of Science, Education, and Health in Yangzhou during the 13th Five-Year Plan (ZDRC20188, BX).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Yuxiang Wang (George) from the Departments of cardiovascular medicine, Mayo Clinic Arizona, for his critical revision of the English language and grammar of the manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2021.661619/full#supplementary-material
References
Almendro-Delia, M., García-Alcántara, Á., de la Torre-Prados, M. V., Reina-Toral, A., Arboleda-Sánchez, J. A., Butrón-Calderón, M., et al. (2017). Safety and Efficacy of Prasugrel and Ticagrelor in Acute Coronary Syndrome. Results of a "Real World" Multicenter Registry. Rev. Port. Cardiol. (English Edition) 70 (11), 952–959. doi:10.1016/j.rec.2017.05.003
Alonso Salinas, G. L., Sanmartin, M., Pascual Izco, M., Rincon, L. M., Martin-Acuna, A., Pastor Pueyo, P., et al. (2018). The Role of Frailty in Acute Coronary Syndromes in the Elderly. Gerontology 64 (5), 422–429. doi:10.1159/000488390
Amin, A. P., Bachuwar, A., Reid, K. J., Chhatriwalla, A. K., Salisbury, A. C., Yeh, R. W., et al. (2013). Nuisance Bleeding with Prolonged Dual Antiplatelet Therapy after Acute Myocardial Infarction and its Impact on Health Status. J. Am. Coll. Cardiol. 61 (21), 2130–2138. doi:10.1016/j.jacc.2013.02.044
Arahata, M., and Asakura, H. (2018). Antithrombotic Therapies for Elderly Patients: Handling Problems Originating from Their Comorbidities. Cia 13, 1675–1690. doi:10.2147/cia.s174896
Ariza-Solé, A., Formiga, F., Lorente, V., Sánchez-Salado, J. C., Sánchez-Elvira, G., Roura, G., et al. (2014). Efficacy of Bleeding Risk Scores in Elderly Patients with Acute Coronary Syndromes. Rev. Port. Cardiol. (English Edition) 67 (6), 463–470. doi:10.1016/j.rec.2013.10.008
Chen, Y., Yin, T., Xi, S., Zhang, S., Yan, H., Tang, Y., et al. (2019). A Risk Score to Predict Postdischarge Bleeding Among Acute Coronary Syndrome Patients Undergoing Percutaneous Coronary Intervention: BRIC-ACS Study. Catheter Cardiovasc. Interv. 93 (7), 1194–1204. doi:10.1002/ccd.28325
Choi, S. Y., Kim, M. H., Cho, Y. R., Sung Park, J., Min Lee, K., Park, T. H., et al. (2018). Performance of PRECISE-DAPT Score for Predicting Bleeding Complication during Dual Antiplatelet Therapy. Circ. Cardiovasc. interventions 11 (12), e006837. doi:10.1161/circinterventions.118.006837
Costa, F., Van Klaveren, D., Feres, F., James, S., Räber, L., Pilgrim, T., et al. (2019). Dual Antiplatelet Therapy Duration Based on Ischemic and Bleeding Risks after Coronary Stenting. J. Am. Coll. Cardiol. 73 (7), 741–754. doi:10.1016/j.jacc.2018.11.048
Costa, F., van Klaveren, D., James, S., Heg, D., Räber, L., Feres, F., et al. (2017). Derivation and Validation of the Predicting Bleeding Complications in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) Score: a Pooled Analysis of Individual-Patient Datasets from Clinical Trials. The Lancet 389 (10073), 1025–1034. doi:10.1016/s0140-6736(17)30397-5
Costa, F., van Klaveren, D., Steyerberg, E., and Valgimigli, M. (2019). Reply: Use of Clinical Risk Score in an Elderly Population: Need for Ad Hoc Validation and Calibration. J. Am. Coll. Cardiol. 74 (1), 162–163. doi:10.1016/j.jacc.2019.05.005
Dodd, K. S., Saczynski, J. S., Zhao, Y., Goldberg, R. J., and Gurwitz, J. H. (2011). Exclusion of Older Adults and Women from Recent Trials of Acute Coronary Syndromes. J. Am. Geriatr. Soc. 59 (3), 506–511. doi:10.1111/j.1532-5415.2010.03305.x
Faustino, A., Mota, P., and Silva, J. (2014). Non-ST-elevation Acute Coronary Syndromes in Octogenarians: Applicability of the GRACE and CRUSADE Scores. Rev. Port. Cardiol. (English Edition) 33 (10), 617–627. doi:10.1016/j.repce.2014.01.022
Garay, A., Formiga, F., Raposeiras-Roubín, S., Abu-Assi, E., Sánchez-Salado, J., Lorente, V., et al. (2018). Prediction of Post-Discharge Bleeding in Elderly Patients with Acute Coronary Syndromes: Insights from the BleeMACS Registry. Thromb. Haemost. 118 (5), 929–938. doi:10.1055/s-0038-1635259
Guerrero, C., Ariza-Solé, A., Formiga, F., Martínez-Sellés, M., Vidán, M. T., and Aboal, J. (2018). Applicability of the PRECISE-DAPT Score in Elderly Patients with Myocardial Infarction. J. Geriatr. Cardiol. 15 (12), 713–717. doi:10.11909/j.issn.1671-5411.2018.12.003
Kedhi, E., Fabris, E., van der Ent, M., Buszman, P., von Birgelen, C., Roolvink, V., et al. (2018). Six Months versus 12 Months Dual Antiplatelet Therapy after Drug-Eluting Stent Implantation in ST-Elevation Myocardial Infarction (DAPT-STEMI): Randomised, Multicentre, Non-inferiority Trial. Bmj 363, k3793. doi:10.1136/bmj.k3793
Khan, S. U., Lone, A. N., Asad, Z. U. A., Rahman, H., Khan, M. S., Saleem, M. A., et al. (2019). Meta-Analysis of Efficacy and Safety of Proton Pump Inhibitors with Dual Antiplatelet Therapy for Coronary Artery Disease. Cardiovasc. Revascularization Med. 20 (12), 1125–1133. doi:10.1016/j.carrev.2019.02.002
Khandelwal, D., Goel, A., Kumar, U., Gulati, V., Narang, R., and Dey, A. B. (2012). Frailty Is Associated with Longer Hospital Stay and Increased Mortality in Hospitalized Older Patients. J. Nutr. Health Aging 16 (8), 732–735. doi:10.1007/s12603-012-0369-5
Levine, G. N., Bates, E. R., Bittl, J. A., Brindis, R. G., Fihn, S. D., Fleisher, L. A., et al. (2016). 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients with Coronary Artery Disease. J. Am. Coll. Cardiol. 68 (10), 1082–1115. doi:10.1016/j.jacc.2016.03.513
Levine, G. N., Jeong, Y.-H., Goto, S., Anderson, J. L., Huo, Y., Mega, J. L., et al. (2014). World Heart Federation Expert Consensus Statement on Antiplatelet Therapy in East Asian Patients with ACS or Undergoing PCI. Nat. Rev. Cardiol. 11 (10), 597–606. doi:10.1038/nrcardio.2014.104
Li, L., Geraghty, O. C., Mehta, Z., and Rothwell, P. M. (2017). Age-specific Risks, Severity, Time Course, and Outcome of Bleeding on Long-Term Antiplatelet Treatment after Vascular Events: a Population-Based Cohort Study. The Lancet 390 (10093), 490–499. doi:10.1016/s0140-6736(17)30770-5
Lopes, R. D., Subherwal, S., Holmes, D. N., Thomas, L., Wang, T. Y., Rao, S. V., et al. (2012). The Association of In-Hospital Major Bleeding with Short-, Intermediate-, and Long-Term Mortality Among Older Patients with Non-ST-segment Elevation Myocardial Infarction. Eur. Heart J. 33 (16), 2044–2053. doi:10.1093/eurheartj/ehs012
Martí, D., Carballeira, D., Morales, M. J., Concepción, R., Del Castillo, H., Marschall, A., et al. (2020). Impact of Anemia on the Risk of Bleeding Following Percutaneous Coronary Interventions in Patients ≥75 Years of Age. Am. J. Cardiol. 125 (8), 1142–1147. doi:10.1016/j.amjcard.2020.01.010
Mazlan-Kepli, W., Dawson, J., Berry, C., and Walters, M. (2019). Cessation of Dual Antiplatelet Therapy and Cardiovascular Events Following Acute Coronary Syndrome. Heart 105 (1), 67–74. doi:10.1136/heartjnl-2018-313148
Mehran, R., Pocock, S. J., Nikolsky, E., Clayton, T., Dangas, G. D., Kirtane, A. J., et al. (2010). A Risk Score to Predict Bleeding in Patients with Acute Coronary Syndromes. J. Am. Coll. Cardiol. 55 (23), 2556–2566. doi:10.1016/j.jacc.2009.09.076
Mehran, R., Rao, S. V., Bhatt, D. L., Gibson, C. M., Caixeta, A., Eikelboom, J., et al. (2011). Standardized Bleeding Definitions for Cardiovascular Clinical Trials. Circulation 123 (23), 2736–2747. doi:10.1161/circulationaha.110.009449
Ndrepepa, G., Neumann, F.-J., Schulz, S., Fusaro, M., Cassese, S., Byrne, R. A., et al. (2014). Incidence and Prognostic Value of Bleeding after Percutaneous Coronary Intervention in Patients Older Than 75 Years of Age. Cathet. Cardiovasc. Intervent. 83 (2), 182–189. doi:10.1002/ccd.25189
Palmerini, T., Della Riva, D., Benedetto, U., Bacchi Reggiani, L., Feres, F., Abizaid, A., et al. (2017). Three, Six, or Twelve Months of Dual Antiplatelet Therapy after DES Implantation in Patients with or without Acute Coronary Syndromes: an Individual Patient Data Pairwise and Network Meta-Analysis of Six Randomized Trials and 11 473 Patients. Eur. Heart J. 38 (14), 1034–1043. doi:10.1093/eurheartj/ehw627
Palmerini, T., Bacchi Reggiani, L., Della Riva, D., Romanello, M., Feres, F., Abizaid, A., et al. (2017). Bleeding-Related Deaths in Relation to the Duration of Dual-Antiplatelet Therapy after Coronary Stenting. J. Am. Coll. Cardiol. 69 (16), 2011–2022. doi:10.1016/j.jacc.2017.02.029
Pavasini, R., Maietti, E., Tonet, E., Bugani, G., Tebaldi, M., Biscaglia, S., et al. (2019). Bleeding Risk Scores and Scales of Frailty for the Prediction of Haemorrhagic Events in Older Adults with Acute Coronary Syndrome: Insights from the FRASER Study. Cardiovasc. Drugs Ther. 33 (5), 523–532. doi:10.1007/s10557-019-06911-y
Schoenenberger, A. W., Radovanovic, D., Windecker, S., Iglesias, J. F., Pedrazzini, G., Stuck, A. E., et al. (2016). Temporal Trends in the Treatment and Outcomes of Elderly Patients with Acute Coronary Syndrome. Eur. Heart J. 37 (16), 1304–1311. doi:10.1093/eurheartj/ehv698
Shanmugam, V. B., Harper, R., Meredith, I., Malaiapan, Y., and Psaltis, P. J. (2015). An Overview of PCI in the Very Elderly. J. Geriatr. Cardiol. 12 (2), 174–184. doi:10.11909/j.issn.1671-5411.2015.02.012
Sharma, P. K., Chhatriwalla, A. K., Cohen, D. J., Jang, J.-S., Baweja, P., Gosch, K., et al. (2017). Predicting Long-Term Bleeding after Percutaneous Coronary Intervention. Cathet. Cardiovasc. Intervent. 89 (2), 199–206. doi:10.1002/ccd.26529
Shimizu, A., Sonoda, S., Muraoka, Y., Setoyama, K., Inoue, K., Miura, T., et al. (2019). Bleeding and Ischemic Events during Dual Antiplatelet Therapy after Second-Generation Drug-Eluting Stent Implantation in Hemodialysis Patients. J. Cardiol. 73 (6), 470–478. doi:10.1016/j.jjcc.2018.12.009
Subherwal, S., Bach, R. G., Chen, A. Y., Gage, B. F., Rao, S. V., Newby, L. K., et al. (2009). Baseline Risk of Major Bleeding in Non-ST-segment-elevation Myocardial Infarction. Circulation 119 (14), 1873–1882. doi:10.1161/circulationaha.108.828541
Tammam, K., Ikari, Y., Yoshimachi, F., Saito, F., and Hassan, W. (2017). Impact of Transradial Coronary Intervention on Bleeding Complications in Octogenarians. Cardiovasc. Interv. Ther. 32 (1), 18–23. doi:10.1007/s12928-016-0383-3
Valgimigli, M., Bueno, H., Byrne, R. A., Collet, J. P., Costa, F., Jeppsson, A., et al. (2017). 2017 ESC Focused Update on Dual Antiplatelet Therapy in Coronary Artery Disease Developed in Collaboration with EACTS: The Task Force for Dual Antiplatelet Therapy in Coronary Artery Disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J.2018 39 (3), 213–260. doi:10.1093/eurheartj/ehx419
Wang, T. Y., Gutierrez, A., and Peterson, E. D. (2011). Percutaneous Coronary Intervention in the Elderly. Nat. Rev. Cardiol. 8 (2), 79–90. doi:10.1038/nrcardio.2010.184
Keywords: bleeding risk, dual antiplatelet therapy, elderly patients, PRECISE-DAPT score, risk factors
Citation: Qian Y, Xu B, Qian X, Cao L, Cheng Y, Liu X, Bai S, Han Z and Wang J (2021) Incidence and Risk Factors for Antiplatelet Therapy–Related Bleeding Complications Among Elderly Patients After Coronary Stenting: A Multicenter Retrospective Observation. Front. Pharmacol. 12:661619. doi: 10.3389/fphar.2021.661619
Received: 09 February 2021; Accepted: 30 June 2021;
Published: 30 July 2021.
Edited by:
Brian Godman, University of Strathclyde, United KingdomReviewed by:
Muhammad Usman, University of Veterinary and Animal Sciences, PakistanTanja Mueller, University of Strathclyde, United Kingdom
Copyright © 2021 Qian, Xu, Qian, Cao, Cheng, Liu, Bai, Han and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junhong Wang, d2FuZ2p1bmhvbmdAanNwaC5vcmcuY24=; Zhijun Han, empoYW4xMTI1QDE2My5jb20=
†These authors have contributed equally to this work
 Yanxia Qian
Yanxia Qian Bing Xu
Bing Xu Xiaodong Qian
Xiaodong Qian Lu Cao
Lu Cao Yujia Cheng
Yujia Cheng Xinjian Liu
Xinjian Liu Song Bai
Song Bai Zhijun Han
Zhijun Han Junhong Wang
Junhong Wang