- 1Department of Anatomical Science, School of Medicine, Kerman University of Medical Sciences, Kerman, Iran
- 2Key Laboratory of Anti-Inflammatory and Immune Medicine, Anhui Collaborative Innovation Center of Anti-Inflammatory and Immune Medicine, Institute of Clinical Pharmacology, Anhui Medical University, Ministry of Education, Hefei, China
Crocin, the main biologically active carotenoid of saffron, generally is derived from the dried trifid stigma of Crocus sativus L. Many studies have demonstrated that crocin has several therapeutic effects on biological systems through its anti-oxidant and anti-inflammatory properties. The wide range of crocin activities is believed to be because of its ability to anchor to many proteins, triggering some cellular pathways responsible for cell proliferation and differentiation. It also has therapeutic potentials in arthritis, osteoarthritis, rheumatoid arthritis, and articular pain probably due to its anti-inflammatory properties. Anti-apoptotic effects, as well as osteoclast inhibition effects of crocin, have suggested it as a natural substance to treat osteoporosis and degenerative disease of bone and cartilage. Different mechanisms underlying crocin effects on bone and cartilage repair have been investigated, but remain to be fully elucidated. The present review aims to undertake current knowledge on the effects of crocin on bone and cartilage degenerative diseases with an emphasis on its proliferative and differentiative properties in mesenchymal stem cells.
Introduction
Crocus sativus L. (C. sativus L.) is one of about 88 species from the Crocus genus, which is part of the Iridaceae family. It is well known in herbal medicine and has attracted the attention of researchers because of its properties, especially its anti-inflammatory and proliferative capacities in bone and cartilage destructive diseases (Ríos et al., 1996; Mollazadeh et al., 2015). This plant is mainly cultivated in Iran, China, India, Azerbaijan, Turkey, Morocco, Greece, Spain, Italy, Mexico, and other places (Xue, 1982; Alavizadeh and Hosseinzadeh, 2014). It is a perennial herb that grows up to about 20 cm and usually produces 2-3 blue-purple flowers (Melnyk et al., 2010). The dried stigma, called saffron, is the most widely used part (Gismondi et al., 2012; Winterhalter and Straubinger, 2000). Because of the distinguished color, odor, and flavor, it is used as a food coloring and flavoring substances (Winterhalter and Straubinger, 2000; Caballero-Ortega et al., 2007; Mollazadeh et al., 2015). Carotenoids, the main metabolites of saffron, are responsible for the red color, smell, and bitterness (Srivastava et al., 2010; Gismondi et al., 2012). Water-soluble carotenoids can affect certain cellular pathways and molecules because of their ability to bind to a wide range of proteins, including membrane proteins, transcription factors, mitochondrial proteins, structural proteins, and enzymes (Hosseinzadeh et al., 2014; Li S et al., 2017). Among these biologically active components, there are four well-established ingredients that are likely responsible for the therapeutic potential of saffron, including crocin, crocetin, safranal, and picrocrocin (Pfander and Schurtenberger, 1982; Tsimidou and Tsatsaroni, 1993; Liakopoulou-Kyriakides and Kyriakides, 2002; Srivastava et al., 2010; Gohari et al., 2013; Hosseinzadeh and Nassiri-Asl, 2013). Crocin has five proper subsets; the principal one in saffron is α-crocin (Alonso et al., 2001; Ordoudi et al., 2015). Chemical studies have shown that crocin is a diester composed of the disaccharide gentiobiose and the dicarboxylic acid crocetin (Figure 1) (Alavizadeh and Hosseinzadeh, 2014). In the past, saffron was used as a sexual stimulant, and as a treatment for infertility and impotence (Asadi et al., 2014). Recent studies have revealed other therapeutic and pharmacological activities of saffron, such as neuroprotective (Baghishani et al., 2018; Haeri et al., 2019), neurogenetic (Ebrahimi et al., 2021), antidepressant (Shafiee et al., 2018), anti-apoptotic (Vafaei et al., 2020), antioxidant (Altinoz et al., 2016; Hatziagapiou et al., 2019), and anti-inflammatory (Nam et al., 2010; Lv et al., 2016) effects. Crocin is one of essential ingredients that responsible for the therapeutic effects of saffron. Specifically, the antioxidative properties of crocin involve several signaling pathways and molecules. For example, it modulates GPx, GST, CAT, and SOD (Korani et al., 2019), inhibits reactive oxygen species (ROS) and interacts with peroxidase (Mostafavinia et al., 2016). Overall, it inhibits free radicals (Ebadi, 2006) and affects certain pathways, such as CREB signaling (Zheng et al., 2007). Crocin also has anti-inflammatory properties via the downregulation of inflammatory marker levels such as interleukin (IL)-1ß, IL-6, tumor necrosis factor (TNF)-α, and insulin-like growth factor (IGF)-1, or through modulation of signaling pathways such as PI3K/Akt and Nuclear factor-kappa B (NF-κB) (Deng et al., 2018; Xie et al., 2019). It has been shown that crocin can polarize macrophages to the M2 (anti-inflammatory) phenotype by suppressing the p38 and JNK pathways. Therefore, its anti-inflammatory effects are associated with this pathway, in addition to other pathways (Zhu et al., 2019). Furthermore, crocin is metabolized in the liver and exerts protective effects on liver toxicity induced by morphine (Salahshoor et al., 2016) and nicotine (Jalili et al., 2015).
Methods
Crocin exerts its effects under various conditions, and its antioxidant and anti-inflammatory properties contribute to the treatment of various diseases, including bone and cartilage inflammation. In this review, we summarized studies published through 2021 on the effect of crocin on bone and cartilage diseases. We chose crocin, bone, cartilage, and inflammation as keywords. The related articles were collected from online literature resources such as Web of Knowledge, PubMed, Scopus, and Google Scholar.
Role of Crocin in Bone and Cartilage Diseases
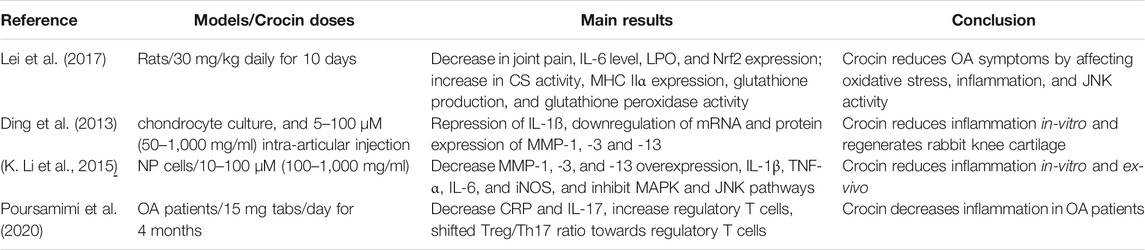
Crocin and Osteoarthritis
One of the most common joint diseases worldwide is osteoarthritis (OA), which is considered the main cause of disability in elderly people and often presents with pain and limited movement (Krasnokutsky et al., 2007; Silverwood et al., 2015; Dubin, 2016). OA severity varies from localized to chronic inflammation (Feldmann, 2001) and leads to joint cartilage degeneration, synovitis, and even bone remodeling (Benazzo et al., 2016). OA is reinforced by several factors such as obesity, age, trauma, mechanical stress, oxidative stress, and inflammation (Chen D. et al., 2017; Lim et al., 2017; Min et al., 2018; Yoo et al., 2018). In mild and severe OA, symptoms of inflammation are pronounced (Sinkov and Cymet, 2003), and inflammatory cytokines, including IL-2, interferon (IFN)-γ, TNF-α, and IL-1ß, are thought to be involved in the pathology (Goldring, 2000; Linton and Fazio, 2003; Chen D. et al., 2017). Overall, inflammatory cytokines lead to NF-κB signaling pathway activation, which can induce expression of matrix-degrading enzymes, such as matrix metalloproteinase (MMP) and C-reactive protein (CRP) 5, and increase erythrocyte sedimentation rate (ESR), which are involved in cartilage degeneration and osteoarthritis (Pennock et al., 2007; Sakkas and Platsoucas, 2007; Mohamadpour et al., 2013; Chen D. et al., 2017). MMPs, especially MMP1 and MMP3, destroy the extracellular matrix, thereby disrupting normal joint performance and leading to OA progression (Largo et al., 2003; Tardif et al., 2004; Burrage et al., 2006; Takaishi et al., 2008). Researchers have shown that the anti-inflammatory properties of crocin have a therapeutic effect on OA. In the study by Lei et al., OA rats were administered 30 mg/kg crocin daily for 10 days. After treatment, joint pain, IL-6 level, muscular lipid peroxidation (LPO), and Nrf2 levels were decreased, while citrate synthase (CS) activity, myosin heavy chain (MHC) IIα expression, glutathione production, and glutathione peroxidase activity were increased. They concluded that crocin could reduce OA symptoms by alleviating oxidative stress and inflammation and inhibiting JNK activity, which is an interesting property for OA treatment (Lei et al., 2017). A study by Ding et al. demonstrated the chondrogenic effects of crocin. In their study, crocin repressed IL-1ß expression and reduced the synthesis of MMP-1, -3, and -13 in chondrocytes, probably by blocking the NF-κB pathway. In the in vivo phase of their study, intra-articular injections of crocin were performed, and the results showed that crocin can reduce cartilage degeneration in OA-induced rabbit knees (Ding et al., 2013). In a study conducted by Li et al. on the anti-inflammatory effects of crocin on rat intervertebral discs, nucleus pulposus cells were isolated from rats and treated with different doses of crocin. Crocin reduced MMP-1, -3, and -13 overexpression, pro-inflammatory factors including IL-1β, TNF-α, IL-6, and inducible nitric oxide synthase (iNOS), and inhibited mitogen-activated protein kinase (MAPK) and JNK pathways (K. Li et al., 2015). In a clinical trial conducted by Poursamim et al., 40 patients with OA received Krocina (crocin tablets, 15 mg/daily) or placebo for 4 months. The results demonstrated that crocin reduced serum CRP and IL-17 levels. In addition, the number of regulatory T cells increased while the number of T helper and CD8+ cells decreased in crocin-and placebo-treated individuals, respectively. Finally, in the crocin group, the Treg/Th17 ratio shifted towards regulatory T cells (Poursamimi et al., 2020). The aforementioned reports demonstrate the possible curative potential of crocin on OA, which makes this herbal plant an appropriate candidate for OA treatment. In Table 1, a summary of studies on crocin and OA is presented.
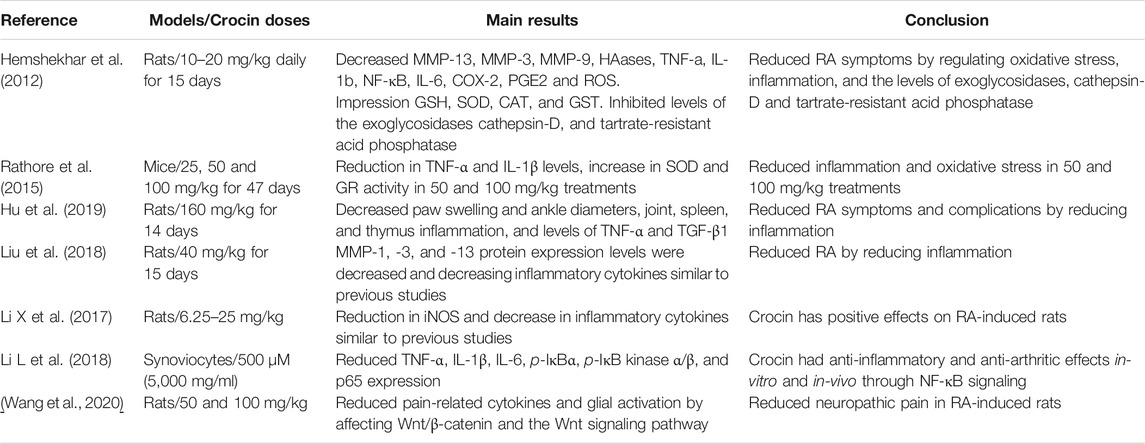
Crocin and Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic autoimmune disease characterized by synovitis and degeneration of the cartilage and underlying bone, which can lead to lasting joint disorders (Turco, 1963; Nakken et al., 2017; Dreher et al., 2019). In this comprehensive disease, joint symptoms are most prevalent, which develop and progress through inflammation (Hamerman, 1966; CADTH Common Drug Reviews, 2015; Borthwick, 2016; Szekanecz et al., 2016). Studies have demonstrated a pivotal role for inflammatory cytokines, including TNF-α, IL-1β, and IL-6, in RA initiation and progression (Benucci et al., 2012; do Prado et al., 2016; Duesterdieck-Zellmer et al., 2012; Furman et al., 2014; Giacomelli et al., 2016; Hreggvidsdottir et al., 2014; G.; Li et al., 2016). Similar to the above studies, there are some reports demonstrating the probable roles of oxidative stress in RA development (Kacsur et al., 2002; Meki et al., 2009; Filaire and Toumi, 2012; Radhakrishnan et al., 2014). Studies have also shown that some signaling pathways can affect the progression and prognosis of RA, including Wnt/β-catenin signaling pathways. The Wnt/β-catenin pathway can regulate inflammatory cytokine secretion, which can affect fibroblast-like synoviocyte (FLS) proliferation and give rise to bone metabolism/destruction (Brunt et al., 2018; Liang et al., 2019; Macedo et al., 2019; Wang et al., 2020; Miao et al., 2021). When the Wnt signaling pathway is activated, pro-inflammatory cytokines, including TNF-α and IL-1β, are produced (Wu et al., 2017; Brunt and Scholpp, 2018; Yuan et al., 2018). NF-κB, which acts as an RA initiator, is another important molecule involved in RA pathogenesis (Gilston et al., 1997; Makarov, 2001). It has been suggested that NF-κB activation occurs prior to type II collagen-induced arthritis (CIA), which is associated with autoimmunity to type II collagen, B cells, and T cells, especially Th17, macrophages, and cytokines (Mulherin et al., 1996; Ehinger et al., 2001; Murphy et al., 2003; Roman-Blas and Jimenez, 2006; Zhu et al., 2010; Hu et al., 2013; Al-Zifzaf et al., 2015). Given the inflammatory nature of RA initiation, and the anti-inflammatory effects of crocin, studies have been designed to understand the possible effects of crocin on RA inhibition and treatment. In a study by Hemshekhar et al., in 2012, 10–20 mg/kg crocin was administered for 15 consecutive days in a rat model of arthritis. They demonstrated that crocin modulates the serum levels of enzymatic and non-enzymatic inflammatory cytokines, including MMP-13, MMP-3, MMP-9, HAases, TNF-α, IL-1β, NF-κB, IL-6, COX-2, and PGE2, as well as ROS mediators, which were increased in the RA-induced rats. Furthermore, crocin also increased the levels of GSH, SOD, CAT, and GST. In addition, inhibiting the exoglycosidases cathepsin-D and tartrate-resistant acid phosphatase in the bones adjacent to the joints by crocin protected bone resorption (Hemshekhar et al., 2012). Rathore et al. administered three doses of crocin (25, 50, and 100 mg/kg) for 47 days in a mouse model of RA. They observed a reduction in TNF-α and IL-1β levels and an increase in SOD and GR activity when higher doses were administered (Rathore et al., 2015). Hu et al. injected 160 mg/kg crocin for 14 days into RA-induced rats. Paw swelling and ankle diameters in crocin-treated rats were significantly decreased as compared to controls. Histological analysis also showed that inflammation was reduced in the joints and other organs, such as the spleen. In addition, TNF-α and TGF-β1 levels decreased in synovial tissues (Hu et al., 2019). In a similar study, Liu et al. showed that the anti-inflammatory and anti-arthritic effects of 40 mg/kg crocin lasted for 15 days. Their study showed that MMP-1, -3, and -13 protein expression levels were decreased in RA-induced rats (Liu et al., 2018). At the same time, Li et al. showed similar results, in addition to a reduction in iNOS production. This study, along with others, showed that crocin has positive effects on RA-induced rats (Li X et al., 2017). In an in vitro study, Li et al. demonstrated that 500 µM (5,000 mg/ml) of crocin reduced the levels of TNF-α, IL-1β, and IL-6 in human FLS. In addition, crocin caused lower levels of p-IκBα, p-IκB kinase α/β, and p65 expression, demonstrating its effect on the NF-κB pathway. The in vivo phase of their study showed that crocin can decrease TNF-α, IL-1β, and IL-6 serum levels, and that NF-κB signaling could suppress inflammation in FLS in RA-induced mice (Li L et al., 2018). Wang et al. showed that crocin inhibits Wnt/β-catenin and the Wnt signaling pathway to reduce pain-related cytokines, and glial activation may reduce neuropathic pain in RA-induced rats (J. F. Wang et al., 2020). Collectively, crocin may be an efficient treatment for RA and is effective for its associated secondary complications. Table 2 summarizes these studies.
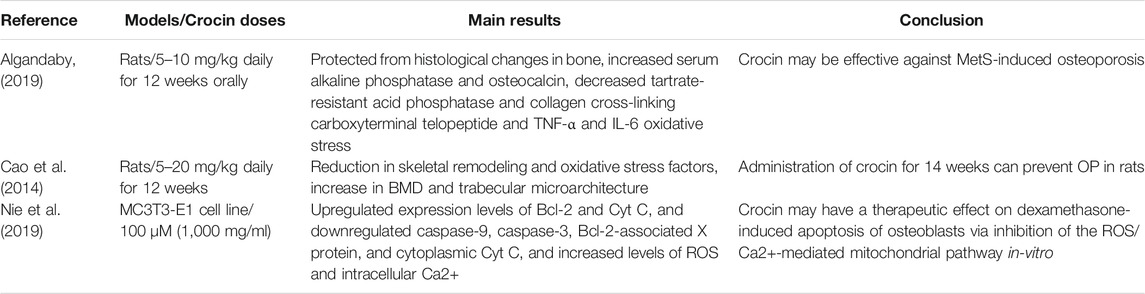
Crocin and Osteoporosis
Osteoporosis (OP) is a progressive systemic skeletal disorder characterized by a reduction in bone mass and deterioration of bone tissue, which occurs following an imbalance of bone formation/absorption, leading to bone fragility. The risk of bone fractures, morbidity, and mortality increases in OP, which increases treatment expenses as well (NHI, 2001; Todd and Robinson, 2003; Bliuc et al., 2009; Bawa, 2010). There are numerous factors that contribute to OP pathogenesis, including metabolic syndrome (MetS), which involves abnormal glucose metabolism, dyslipidemia, hypertension, and abdominal obesity (Zhou et al., 2013). In MetS, fat tissue secretes inflammatory factors and hyperglycemia results in an increase in glycation end products, which leads to a reduction in bone mineral density (BMD) (Yamaguchi, 2014). Due to the positive effects of crocin on hypertension, body fat balance, and MetS, along with its anti-inflammatory properties, crocin as a potential treatment for osteoporosis should receive more attention (Sheng et al., 2006; Imenshahidi et al., 2015; Shafiee et al., 2017). In a study by Algandaby, 5 and 10 mg/kg crocin was administered to a rat model of metabolic syndrome-induced osteoporosis. In the crocin treatment group, bone tissue was histologically protected against OP effects, bone formation markers including serum alkaline phosphatase and osteocalcin increased, and bone resorption markers, including tartrate-resistant acid phosphatase and collagen cross-linking carboxyterminal telopeptide, were inhibited. In addition, crocin reduced TNF-α and IL-6 serum levels and oxidative stress in the epiphyseal tissue of rats. These results demonstrated that crocin may protect against MetS-induced osteoporosis (Algandaby, 2019). Another cause of OP is hormone (including estrogen, testosterone, and parathyroid hormone) deficiency, which usually effects cancerous bone and can cause a reduction in BMD. OP is more common in women than in men, and women over 50 years of age are more vulnerable to causes of OP, likely because of estrogen deficiency in the postmenopausal period (Hunter and Sambrook, 2000; Marcus, 2002; Johnell and Kanis, 2006; Sugerman, 2014; Noh et al., 2020). Cao et al. studied the effects of 5–20 mg/kg/day of crocin for 12 weeks in ovariectomized rats. They demonstrated that crocin protected rats from reduced BMD in L4 vertebrae and femurs, and prevented deterioration of the trabecular microarchitecture in rats caused by ovariectomy. A significant reduction in skeletal remodeling, as evidenced by lower levels of bone turnover markers, was also observed. Oxidative stress factors in the serum or bone tissue returned to near-normal conditions. Collectively, these results demonstrated that crocin administration can prevent OP in rats (Cao et al., 2014). In an in vitro study by Nie et al., crocin was used to protect against glucocorticoid-induced osteoporosis and osteonecrosis by inhibiting the ROS/Ca2+-mediated mitochondrial pathway. They showed that crocin decreases mitochondrial transmembrane potential and increases ROS and intracellular Ca2+ levels following induction of OP by dexamethasone in osteoblasts. In addition, the expression levels of B-cell lymphoma-2(Bcl-2) and mitochondrial cytochrome c (Cyt-C) were upregulated, and cleaved caspase-9, cleaved caspase-3, Bcl-2-associated X protein, and cytoplasmic Cyt C were downregulated by crocin (Nie et al., 2019). Taken together, these studies demonstrated that crocin is a potential medicine for OP treatment. Table 3 shows the relationship between crocin and OP.
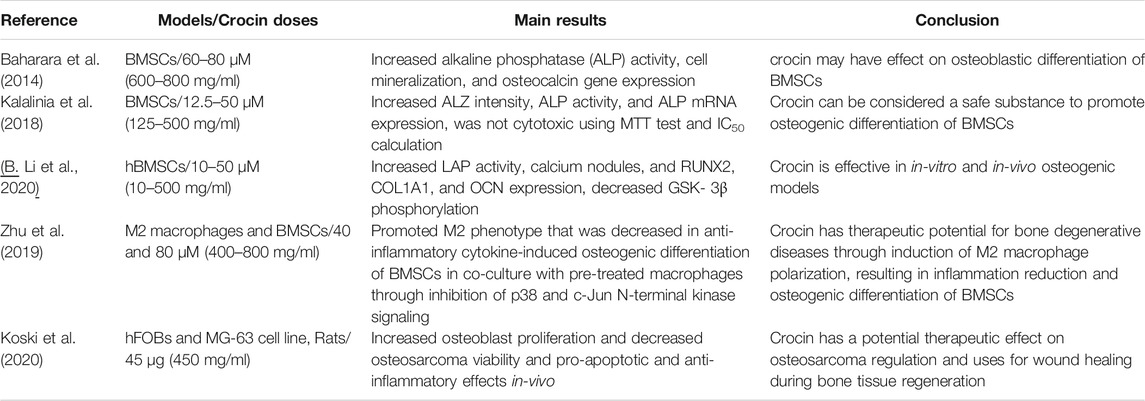
Effects of Crocin on Cell Differentiation
Bone regeneration is a complex procedure that occurs in abnormal conditions, such as bone degenerative diseases and fractures, but is insufficient and inefficient in some circumstances (Marzona and Pavolini, 2009; Dimitriou et al., 2011). Following the inflammatory phase of bone defects, there is a proliferative phase called the mesenchymal activation phase. During this phase, mesenchymal stem cells (MSCs) differentiate into chondrocytes and osteoblasts, which facilitate bone regeneration, either through endochondral ossification or intramembranous ossification (Knight and Hankenson, 2013). Bony tissue cells include osteoclasts, osteoblasts, and osteocytes, which are involved in bone regeneration and remodeling. These cells are derived from MSCs depending on the environmental stimulants that coordinate bone formation and bone absorption (Boyle et al., 2003; Zaminy et al., 2008; Knight and Hankenson, 2013; Noh et al., 2020). For example, studies have demonstrated that bone marrow MSCs (BMSCs) as multipotent stem cells can differentiate into bone and cartilage cells. This occurs through the expression of different growth factors, including platelet-derived growth factor (PDGF), bone morphogenetic proteins (BMPs), and transforming growth factor-β(TGF-β), and likely via the ERK and JNK MAPK signaling pathways. However, these growth factors are highly limited in these cells owing to rapid degradation and high cytotoxicity, as well as the high financial cost of these factors; thus, it is desirable to investigate novel osteoblastic inducers, especially natural products (Friedman et al., 2006; Fan et al., 2011; Mostafa et al., 2012; Yu et al., 2012; Udalamaththa et al., 2016; Li C et al., 2017). Baharara et al. (2014) reported successful differentiation of BMSCs into osteoblasts following treatment with crocin, which was confirmed by an increase in alkaline phosphatase (ALP) activity, cell mineralization, and osteocalcin gene expression (Baharara et al., 2014). Kalalinia et al. (2018) demonstrated that 12.5–50 µM (125–500 mg/ml) crocin is not cytotoxic based on the MTT assay and IC50 calculation. Moreover, at these concentrations, it may enhance osteogenesis in BMSCs, as measured by ALZ intensity, ALP activity, and ALP mRNA expression. Thus, crocin can be considered a safe substance to promote the osteogenic differentiation of BMSCs (Kalalinia et al., 2018). Li et al. (2017) also studied the osteogenic effect of crocin both in vitro and in vivo. For the in vitro study, they treated human BMSCs with crocin and demonstrated an increase in ALP activity and calcium nodule formation (assayed by alizarin red S staining). In addition, they treated male rats with femoral head osteonecrosis with crocin and showed considerable histopathological changes in the femoral head tissues with H&E staining. Western blotting and q-PCR assays showed an increase in the expression levels of RUNX2, COL1A1, and OCN, and a decrease in GSK-3β phosphorylation in both bone tissue and BMSCs after treatment with crocin, in a dose-dependent manner. These researchers suggested that crocin has potential for use in the treatment of osteogenic diseases in the future (B. Li et al., 2020). Koski et al. administered crocin over 7 weeks to human fetal osteoblasts and observed an increase in cell proliferation. In addition, crocin decreased human osteosarcoma (MG-63) cells viability in vitro. In contrast, the in vivo application of crocin showed pro-apoptotic and anti-inflammatory effects in a rat model of femoral inflammation. These results suggest that crocin may have a therapeutic effect on osteosarcoma regulation and potential for use in wound healing during bone tissue regeneration (Koski et al., 2020). Studies have shown that in some diseases involving bone degeneration and dysregulation of bone homeostasis besides osteogenesis, the influence of osteoclast formation and osteo-immunomodulation is important (Chen et al., 2017b; Chen et al., 2017c). On the other hand, M2 macrophages (anti-inflammatory macrophages) secrete cytokines such as BMP-2 that contribute to osteogenesis (Yuan et al., 2017). Note that crocin may be effective in macrophage polarization and promotion of the M2 phenotype (Li J et al., 2018). Zhu et al. showed that crocin promoted macrophage polarization toward the M2 phenotype and reduced the expression of anti-inflammatory cytokines in vitro and in vivo. In addition, pre-treatment of macrophages with crocin induced the osteogenic differentiation of BMSCs in co-culture media. This is probably due to the inhibition of p38 and c-Jun N-terminal kinase signaling. This study indicated that crocin has therapeutic potential for bone degenerative disease by inducing M2 macrophage polarization, which results in inflammation reduction and osteogenic differentiation of BMSCs (Zhu et al., 2019). The above-mentioned studies have emphasized that crocin may have a positive effect on osteogenesis by promoting osteoblastic differentiation. A summary of these studies is provided in Table 4.
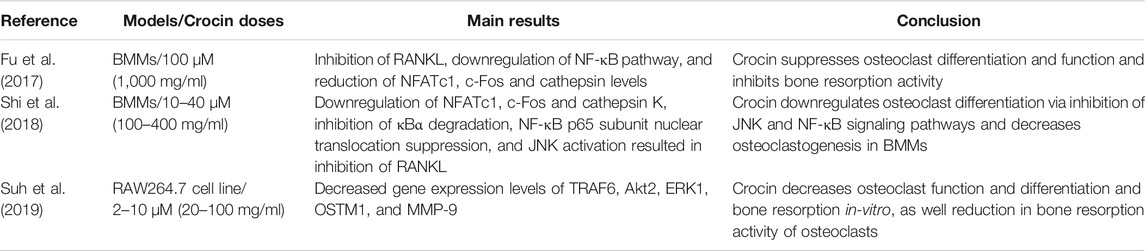
In some pathological conditions related to bone loss-associated diseases (osteoporosis, arthritis, osteomyelitis, etc.), osteoclast cells are activated, leading to bone resorption. Under similar conditions, an imbalance occurs between osteoblast activities (leading to bone formation) and osteoclast activities (leading to bone resorption) (Boyle et al., 2003; Walsh and Gravallese, 2010; Redlich and Smolen, 2012). Stimulation of hematopoietic stem cells (HSCs) by inflammatory cytokines, such as IL-1, IL-6, and TNF-α (which are inhibited by crocin, as mentioned above) or other factors such as monocyte/macrophage colony-stimulating factor (M-CSF) and activation of receptor activator of nuclear factor kappaB (RANK) with its ligand (RANKL) can lead to osteoclast differentiation (Udagawa et al., 1999; Azuma et al., 2000; Teitelbaum, 2000; Ross, 2006; Walsh and Gravallese, 2010; Redlich and Smolen, 2012; Yamashita et al., 2012; Xu and Teitelbaum, 2013; Yokota et al., 2014). Studies have indicated that RANKL, a membrane protein of the TNF family, plays a role in osteoclast differentiation (Yasuda et al., 1998; Takayanagi et al., 2000; Roodman, 2006). RANKL is expressed on osteoblast cell membranes in response to stimulatory factors and then engages RANK on osteoclast cell membranes, along with activation of the NF-κB and MAPK signaling pathways. The final product of these cascades is the expression of tartrate-resistant acid phosphatase (TRAP) and other enzymes, which are involved in osteoclast-mediated bone resorption (Asagiri and Takayanagi, 2007). Fu et al. demonstrated that crocin suppresses osteoclast differentiation and function by directly inhibiting RANKL in bone marrow-derived macrophages (BMM). Downregulation of the NF-κB pathway and reduction in osteoclast-specific gene expression, including NFATc1, c-Fos, and cathepsin, are involved, leading to inhibition of bone resorption activity (Fu et al., 2017). A similar study by Shi et al. demonstrated that crocin downregulates osteoclast differentiation via inhibition of JNK and NF-κB signaling pathways in BMM cells in vitro. In the crocin-treated group, osteoclast markers including NFATc1, c-Fos, and cathepsin K, were downregulated. An inhibitor of κBα degradation and NF-κB p65 subunit nuclear translocation was suppressed, while c-Jun N-terminal kinase (JNK) was activated, resulting in the inhibition of RANKL in BMM. These results demonstrated that crocin decreased osteoclastogenesis in BMM (Shi et al., 2018). Suh et al. showed that crocin treatment decreased gene expression of TRAF6, Akt2, ERK1, OSTM1, and MMP-9, which are related to osteoclast differentiation and function and bone resorption in vitro, as well as a reduction in bone resorption activity of osteoclasts (Suh et al., 2019). These studies demonstrate the potential therapeutic effect of crocin on osteoclast and bone resorption dysfunction, as well as bone loss-associated diseases. A summary of these studies is provided in Table 5.
Conclusion
Studies have shown that crocin, the main biologically active component of saffron, has anti-inflammatory and antioxidant effects. In addition, crocin has potential therapeutic effects on bone and cartilage diseases that involve inflammation and accumulation of free radicals, including OA, RA, and osteoporosis. Crocin can reduce oxidative stress and inflammatory cytokines via inhibiting molecular pathways include Wnt, MAPK and JNK signaling pathway. It modulates PI3K/Akt and NF-κB signaling pathways and polarizes macrophages to the M2 (anti-inflammatory) phenotype by suppressing the p38 and JNK pathways. Crocin also has proliferative and anti-apoptotic effects, especially on osteoblasts, and positive effects on osteoblastic differentiation of MSCs, while it also inhibits osteoclast activity. These data suggest promising potential therapeutic use of crocin in bone degenerative and bone-loss diseases, which require more precise laboratories and clinical trials. For example, crocin in high doses exhibited a cytotoxic effect and acts as an apoptotic promotor (Li et al., 2013), so it seems that further researches are needed to the determination of proper crocin dosage for both in-vitro and in-vivo studies. Also, the molecular mechanisms of various crocin effects are not recognized very well yet, so future studies may need to clarify the molecular mechanisms that they are involved. Overall regarding the beneficial effects of crocin in bone and cartilage diseases and due to lack of human studies in crocin effects in this field, the need for human trials is felt and future studies can be done in this research area.
Author Contributions
JT and SN-M conceived this manuscript. SV drafted this manuscript. XW revised this manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (31900616) and the Project of Improvement of Scientific Ability of Anhui Medical University (2020xkjT009).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Al-Zifzaf, D. S., El Bakry, S. A., Shawarby, L. A., Ghaffar, A. Y. A., Amer, H. A., et al. (2015). FoxP3+T Regulatory Cells in Rheumatoid Arthritis and the Imbalance of the Treg/TH17 Cytokine axis. The Egypt. Rheumatologist 37 (1), 7–15. doi:10.1016/j.ejr.2014.06.004
Alavizadeh, S. H., and Hosseinzadeh, H. (2014). Bioactivity Assessment and Toxicity of Crocin: a Comprehensive Review. Food Chem. Toxicol. 64, 65–80. doi:10.1016/j.fct.2013.11.016
Algandaby, M. M. (2019). Crocin Attenuates Metabolic Syndrome-Induced Osteoporosis in Rats. J. Food Biochem. 43 (7), e12895. doi:10.1111/jfbc.12895
Alonso, G. L., Salinas, M. R., Garijo, J., and Sánchez-fernández, M. A. (2001). Composition of Crocins and Picrocrocin from Spanish Saffron (Crocus Sativus L.). J. Food Qual. 24 (3), 219–233. doi:10.1111/j.1745-4557.2001.tb00604.x
Altinoz, E., Ozmen, T., Oner, Z., Elbe, H., Erdemli, M. E., and Bag, H. G. (2016). Effect of Crocin on Oxidative Stress in Recovery from Single Bout of Swimming Exercise in Rats. Gen. Physiol. Biophys. 35 (1), 87–94. doi:10.4149/gpb_2015018
Asadi, M. H., Zafari, F., Sarveazad, A., Abbasi, M., Safa, M., Koruji, M., et al. (2014). Saffron Improves Epididymal Sperm Parameters in Rats Exposed to Cadmium. Nephrourol Mon 6 (1), e12125. doi:10.5812/numonthly.12125
Asagiri, M., and Takayanagi, H. (2007). The Molecular Understanding of Osteoclast Differentiation. Bone 40 (2), 251–264. doi:10.1016/j.bone.2006.09.023
Azuma, Y., Kaji, K., Katogi, R., Takeshita, S., and Kudo, A. (2000). Tumor Necrosis Factor-Alpha Induces Differentiation of and Bone Resorption by Osteoclasts. J. Biol. Chem. 275 (7), 4858–4864. doi:10.1074/jbc.275.7.4858
Baghishani, F., Mohammadipour, A., Hosseinzadeh, H., Hosseini, M., and Ebrahimzadeh-Bideskan, A. (2018). The Effects of Tramadol Administration on Hippocampal Cell Apoptosis, Learning and Memory in Adult Rats and Neuroprotective Effects of Crocin. Metab. Brain Dis. 33 (3), 907–916. doi:10.1007/s11011-018-0194-6
Bawa, S. (2010). The Significance of Soy Protein and Soy Bioactive Compounds in the Prophylaxis and Treatment of Osteoporosis. J. Osteoporos. 2010, 891058. doi:10.4061/2010/891058
Benazzo, F., Perticarini, L., Padolino, A., Castelli, A., Gifuni, P., Lovato, M., et al. (2016). A multi-centre, Open Label, Long-Term Follow-Up Study to Evaluate the Benefits of a New Viscoelastic Hydrogel (Hymovis®) in the Treatment of Knee Osteoarthritis. Eur. Rev. Med. Pharmacol. Sci. 20 (5), 959–968.
Benucci, M., Saviola, G., Baiardi, P., Manfredi, M., Sarzi Puttini, P., and Atzeni, F. (2012). Determinants of Risk Infection during Therapy with Anti TNF-Alpha Blocking Agents in Rheumatoid Arthritis. Open Rheumatol. J. 6, 33–37. doi:10.2174/1874312901206010033
Bliuc, D., Nguyen, N. D., Milch, V. E., Nguyen, T. V., Eisman, J. A., and Center, J. R. (2009). Mortality Risk Associated with Low-Trauma Osteoporotic Fracture and Subsequent Fracture in Men and Women. Jama 301 (5), 513–521. doi:10.1001/jama.2009.50
Borthwick, L. A. (2016). The IL-1 Cytokine Family and its Role in Inflammation and Fibrosis in the Lung. Semin. Immunopathol 38 (4), 517–534. doi:10.1007/s00281-016-0559-z
Boyle, W. J., Simonet, W. S., and Lacey, D. L. (2003). Osteoclast Differentiation and Activation. Nature 423 (6937), 337–342. doi:10.1038/nature01658
Brunt, L., and Scholpp, S. (2018). The Function of Endocytosis in Wnt Signaling. Cell Mol Life Sci 75 (5), 785–795. doi:10.1007/s00018-017-2654-2
Burrage, P. S., Mix, K. S., and Brinckerhoff, C. E. (2006). Matrix Metalloproteinases: Role in Arthritis. Front. Biosci. 11, 529–543. doi:10.2741/1817
Caballero-Ortega, H., Pereda-Miranda, R., and Abdullaev, F. I. (2007). HPLC Quantification of Major Active Components from 11 Different Saffron (Crocus Sativus L.) Sources. Food Chem. 100 (3), 1126–1131. doi:10.1016/j.foodchem.2005.11.020
CADTH Common Drug Reviews (2015). In Golimumab (Simponi) IV: In Combination with Methotrexate (MTX) for the Treatment of Adult Patients with Moderately to Severely Active Rheumatoid Arthritis. Ottawa (On) Can. Agency Drugs Tech. Health Copyright © CADTH, 26962595.
Cao, P. C., Xiao, W. X., Yan, Y. B., Zhao, X., Liu, S., Feng, J., et al. (2014). Preventive Effect of Crocin on Osteoporosis in an Ovariectomized Rat Model. Evid. Based Complement. Alternat Med. 2014, 825181. doi:10.1155/2014/825181
Chen, D., Shen, J., Zhao, W., Wang, T., Han, L., Hamilton, J. L., et al. (2017a). Osteoarthritis: toward a Comprehensive Understanding of Pathological Mechanism. Bone Res. 5, 16044. doi:10.1038/boneres.2016.44
Chen, Z., Bachhuka, A., Han, S., Wei, F., Lu, S., Visalakshan, R. M., et al. (2017b). Tuning Chemistry and Topography of Nanoengineered Surfaces to Manipulate Immune Response for Bone Regeneration Applications. ACS Nano 11 (5), 4494–4506. doi:10.1021/acsnano.6b07808
Chen, Z., Ni, S., Han, S., Crawford, R., Lu, S., Wei, F., et al. (2017c). Nanoporous Microstructures Mediate Osteogenesis by Modulating the Osteo-Immune Response of Macrophages. Nanoscale 9 (2), 706–718. doi:10.1039/C6NR06421C
de Sousa, L. M., dos Santos Alves, J. M., da Silva Martins, C., Pereira, K. M. A., Goes, P., and Gondim, D. V. (2019). Immunoexpression of Canonical Wnt and NF-Κb Signaling Pathways in the Temporomandibular Joint of Arthritic Rats. Inflamm. Res. 68, 889–900. doi:10.1007/s00011-019-01274-4
Deng, M., Li, D., Zhang, Y., Zhou, G., Liu, W., Cao, Y., et al. (2018). Protective Effect of Crocin on Ultraviolet B-induced D-ermal F-ibroblast P-hotoaging. Mol. Med. Rep. 18 (2), 1439–1446. doi:10.3892/mmr.2018.9150
Dimitriou, R., Jones, E., McGonagle, D., and Giannoudis, P. V. (2011). Bone Regeneration: Current Concepts and Future Directions. BMC Med. 9, 66. doi:10.1186/1741-7015-9-66
Ding, Q., Zhong, H., Qi, Y., Cheng, Y., Li, W., Yan, S., et al. (2013). Anti-arthritic Effects of Crocin in Interleukin-1β-Treated Articular Chondrocytes and Cartilage in a Rabbit Osteoarthritic Model. Inflamm. Res. 62 (1), 17–25. doi:10.1007/s00011-012-0546-3
do Prado, A. D., Bisi, M. C., Piovesan, D. M., Bredemeier, M., Batista, T. S., Petersen, L., et al. (2016). Ultrasound Power Doppler Synovitis Is Associated with Plasma IL-6 in Established Rheumatoid Arthritis. Cytokine 83, 27–32. doi:10.1016/j.cyto.2016.03.014
Dreher, M., Kosz, M., and Schwarting, A. (2019). Physical Activity, Exercise and Nutrition in Rheumatism : Adjuvant Treatment Options for Inflammatory-Rheumatic Diseases. Orthopade 48 (11), 917–926. doi:10.1007/s00132-019-03808-4
Dubin, A. (2016). Managing Osteoarthritis and Other Chronic Musculoskeletal Pain Disorders. Med. Clin. North. Am. 100 (1), 143–150. doi:10.1016/j.mcna.2015.08.008
Duesterdieck-Zellmer, K. F., Driscoll, N., and Ott, J. F. (2012). Concentration-dependent Effects of Tiludronate on Equine Articular Cartilage Explants Incubated with and without Interleukin-1β. Am. J. Vet. Res. 73 (10), 1530–1539. doi:10.2460/ajvr.73.10.1530
Ebadi, M. (2006). Pharmacodynamic Basis of Herbal Medicine. 2nd Ed. Boca Raton, Florida, United States: CRC Press.
Ebrahimi, B., Vafaei, S., Rastegar-Moghaddam, S. H. R., Hosseini, M., Tajik Yabr, F., and Mohammadipour, A. (2021). Crocin Administration from Childhood to Adulthood Increases Hippocampal Neurogenesis and Synaptogenesis in Male MiceJournal of Kerman University of Medical Sciences. J. Kerman Univ. Med. Sci. 28 (3), 243–251. doi:10.22062/jkmu.2021.91664
Ehinger, M., Vestberg, M., Johansson, A. C., Johannesson, M., Svensson, A., and Holmdahl, R. (2001). Influence of CD4 or CD8 Deficiency on Collagen-Induced Arthritis. Immunology 103 (3), 291–300. doi:10.1046/j.1365-2567.2001.01257.x
Fan, J. J., Cao, L. G., Wu, T., Wang, D. X., Jin, D., Jiang, S., et al. (2011). The Dose-Effect of Icariin on the Proliferation and Osteogenic Differentiation of Human Bone Mesenchymal Stem Cells. Molecules 16 (12), 10123–10133. doi:10.3390/molecules161210123
Feldmann, M. (2001). Pathogenesis of Arthritis: Recent Research Progress. Nat. Immunol. 2 (9), 771–773. doi:10.1038/ni0901-771
Filaire, E., and Toumi, H. (2012). Reactive Oxygen Species and Exercise on Bone Metabolism: Friend or Enemy? Jt. Bone Spine 79 (4), 341–346. doi:10.1016/j.jbspin.2012.03.007
Friedman, M. S., Long, M. W., and Hankenson, K. D. (2006). Osteogenic Differentiation of Human Mesenchymal Stem Cells Is Regulated by Bone Morphogenetic Protein-6. J. Cel Biochem 98 (3), 538–554. doi:10.1002/jcb.20719
Fu, L., Pan, F., and Jiao, Y. (2017). Crocin Inhibits RANKL-Induced Osteoclast Formation and Bone Resorption by Suppressing NF-Κb Signaling Pathway Activation. Immunobiology 222 (4), 597–603. doi:10.1016/j.imbio.2016.11.009
Furman, B. D., Mangiapani, D. S., Zeitler, E., Bailey, K. N., Horne, P. H., Huebner, J. L., et al. (2014). Targeting Pro-inflammatory Cytokines Following Joint Injury: Acute Intra-articular Inhibition of Interleukin-1 Following Knee Injury Prevents post-traumatic Arthritis. Arthritis Res. Ther. 16 (3), R134. doi:10.1186/ar4591
Giacomelli, R., Ruscitti, P., Alvaro, S., Ciccia, F., Liakouli, V., Di Benedetto, P., et al. (2016). IL-1β at the Crossroad between Rheumatoid Arthritis and Type 2 Diabetes: May We Kill Two Birds with One Stone? Expert Rev. Clin. Immunol. 12 (8), 849–855. doi:10.1586/1744666x.2016.1168293
Gilston, V., Jones, H. W., Soo, C. C., Coumbe, A., Blades, S., Kaltschmidt, C., et al. (1997). NF-kappa B Activation in Human Knee-Joint Synovial Tissue during the Early Stage of Joint Inflammation. Biochem. Soc. Trans. 25 (3), 518. doi:10.1042/bst025518s
Gismondi, A., Serio, M., Canuti, L., and Canini, A. (2012). Biochemical, Antioxidant and Antineoplastic Properties of Italian Saffron (Crocus Sativus L. %J Am. J. Plant Sci. 03 (11), 8. doi:10.4236/ajps.2012.311190
Gohari, A. R., Saeidnia, S., and Mahmoodabadi, M. K. (2013). An Overview on Saffron, Phytochemicals, and Medicinal Properties. Pharmacogn Rev. 7 (13), 61–66. doi:10.4103/0973-7847.112850
Goldring, M. B. (2000). Osteoarthritis and Cartilage: the Role of Cytokines. Curr. Rheumatol. Rep. 2 (6), 459–465. doi:10.1007/s11926-000-0021-y
Haeri, P., Mohammadipour, A., Heidari, Z., and Ebrahimzadeh-Bideskan, A. (2019). Neuroprotective Effect of Crocin on Substantia Nigra in MPTP-Induced Parkinson's Disease Model of Mice. Anat. Sci. Int. 94 (1), 119–127. doi:10.1007/s12565-018-0457-7
Hamerman, D. (1966). New Thoughts on the Pathogenesis of Rheumatoid Arthritis. Am. J. Med. 40 (1), 1–9. doi:10.1016/0002-9343(66)90181-1
Hatziagapiou, K., Kakouri, E., Lambrou, G. I., Bethanis, K., and Tarantilis, P. A. (2019). Antioxidant Properties of Crocus Sativus L. And its Constituents and Relevance to Neurodegenerative Diseases; Focus on Alzheimer's and Parkinson's Disease. Curr. Neuropharmacol 17 (4), 377–402. doi:10.2174/1570159x16666180321095705
Hemshekhar, M., Sebastin Santhosh, M., Sunitha, K., Thushara, R. M., Kemparaju, K., Rangappa, K. S., et al. (2012). A Dietary Colorant Crocin Mitigates Arthritis and Associated Secondary Complications by Modulating Cartilage Deteriorating Enzymes, Inflammatory Mediators and Antioxidant Status. Biochimie 94 (12), 2723–2733. doi:10.1016/j.biochi.2012.08.013
Hosseinzadeh, H., Mehri, S., Heshmati, A., Ramezani, M., Sahebkar, A., and Abnous, K. (2014). Proteomic Screening of Molecular Targets of Crocin. Daru 22 (1), 5. doi:10.1186/2008-2231-22-5
Hosseinzadeh, H., and Nassiri-Asl, M. (2013). Avicenna's (Ibn Sina) the Canon of Medicine and Saffron (Crocus Sativus): a Review. Phytother Res. 27 (4), 475–483. doi:10.1002/ptr.4784
Hreggvidsdottir, H. S., Noordenbos, T., and Baeten, D. L. (2014). Inflammatory Pathways in Spondyloarthritis. Mol. Immunol. 57 (1), 28–37. doi:10.1016/j.molimm.2013.07.016
Hu, Y., Cheng, W., Cai, W., Yue, Y., Li, J., and Zhang, P. (2013). Advances in Research on Animal Models of Rheumatoid Arthritis. Clin. Rheumatol. 32 (2), 161–165. doi:10.1007/s10067-012-2041-1
Hu, Y., Liu, X., Xia, Q., Yin, T., Bai, C., Wang, Z., et al. (2019). Comparative Anti-arthritic Investigation of Iridoid Glycosides and Crocetin Derivatives from Gardenia Jasminoides Ellis in Freund's Complete Adjuvant-Induced Arthritis in Rats. Phytomedicine 53, 223–233. doi:10.1016/j.phymed.2018.07.005
Hunter, D. J., and Sambrook, P. N. (2000). Bone Loss. Epidemiology of Bone Loss. Arthritis Res. 2 (6), 441–445. doi:10.1186/ar125
Imenshahidi, M., Razavi, M., Faal, A., Gholampoor, A., Mousavi, S., and Hosseinzadeh, H. (2015). The Effect of Chronic Administration of Safranal on Systolic Blood Pressure in Rats. Iranian J. Pharm. Res. 14 (2), 585–590. doi:10.22037/ijpr.2015.1669
Jalili, C., Tabatabaei, H., Kakaberiei, S., Roshankhah, S., and Salahshoor, M. R. (2015). Protective Role of Crocin against Nicotine-Induced Damages on Male Mice Liver. Int. J. Prev. Med. 6, 92. doi:10.4103/2008-7802.165203
Javad, B., Tayebe, R., Shahrokhabadi Khadijeh, N., and Maryam, N. (2014). Effects of Crocus Sativus Lextract and Vitamin D3 on In Vitro Osteogenesis of Mecenchymal Stem Cells. Int. J. Cell Mol. Biotechnol. 2014, 1–10. doi:10.5899/2014/ijcmb-00012
Johnell, O., and Kanis, J. A. (2006). An Estimate of the Worldwide Prevalence and Disability Associated with Osteoporotic Fractures. Osteoporos. Int. 17 (12), 1726–1733. doi:10.1007/s00198-006-0172-4
Kacsur, C., Mader, R., Ben-Amotz, A., and Levy, Y. (2002). Plasma Anti-oxidants and Rheumatoid Arthritis. Harefuah 141 (2), 148–223.
Kalalinia, F., Ghasim, H., Amel Farzad, S., Pishavar, E., Ramezani, M., and Hashemi, M. (2018). Comparison of the Effect of Crocin and Crocetin, Two Major Compounds Extracted from Saffron, on Osteogenic Differentiation of Mesenchymal Stem Cells. Life Sci. 208, 262–267. doi:10.1016/j.lfs.2018.07.043
Knight, M. N., and Hankenson, K. D. (2013). Mesenchymal Stem Cells in Bone Regeneration. Adv. Wound Care (New Rochelle) 2 (6), 306–316. doi:10.1089/wound.2012.0420
Korani, S., Korani, M., Sathyapalan, T., and Sahebkar, A. (2019). Therapeutic Effects of Crocin in Autoimmune Diseases: A Review. Biofactors 45 (6), 835–843. doi:10.1002/biof.1557
Koski, C., Sarkar, N., and Bose, S. (2020). Cytotoxic and Osteogenic Effects of Crocin and Bicarbonate from Calcium Phosphates for Potential Chemopreventative and Anti-inflammatory Applications In Vitro and In Vivo. J. Mater. Chem. B 8 (10), 2048–2062. doi:10.1039/c9tb01462d
Krasnokutsky, S., Samuels, J., and Abramson, S. B. (2007). Osteoarthritis in 2007. Bull. NYU Hosp. Jt. Dis. 65 (3), 222–228.
Largo, R., Alvarez-Soria, M. A., Díez-Ortego, I., Calvo, E., Sánchez-Pernaute, O., Egido, J., et al. (2003). Glucosamine Inhibits IL-1beta-induced NFkappaB Activation in Human Osteoarthritic Chondrocytes. Osteoarthritis Cartilage 11 (4), 290–298. doi:10.1016/s1063-4584(03)00028-1
Lei, M., Guo, C., Hua, L., Xue, S., Yu, D., Zhang, C., et al. (2017). Crocin Attenuates Joint Pain and Muscle Dysfunction in Osteoarthritis Rat. Inflammation 40 (6), 2086–2093. doi:10.1007/s10753-017-0648-8
Li, B., Qin, K., Wang, B., Liu, B., Yu, W., Li, Z., et al. (2020). Crocin Promotes Osteogenesis Differentiation of Bone Marrow Mesenchymal Stem Cells. In Vitro Cel Dev Biol Anim 56 (8), 680–688. doi:10.1007/s11626-020-00487-w
Li, C., Wei, G. J., Xu, L., Rong, J. S., Tao, S. Q., and Wang, Y. S. (2017). The Involvement of Senescence Induced by the Telomere Shortness in the Decline of Osteogenic Differentiation in BMSCs. Eur. Rev. Med. Pharmacol. Sci. 21 (5), 1117–1124.
Li, G., Wu, Y., Jia, H., Tang, L., Huang, R., Peng, Y., et al. (2016). Establishment and Evaluation of a Transgenic Mouse Model of Arthritis Induced by Overexpressing Human Tumor Necrosis Factor Alpha. Biol. Open 5 (4), 418–423. doi:10.1242/bio.016279
Li, J., Lei, H. T., Cao, L., Mi, Y. N., Li, S., and Cao, Y. X. (2018). Crocin Alleviates Coronary Atherosclerosis via Inhibiting Lipid Synthesis and Inducing M2 Macrophage Polarization. Int. Immunopharmacol 55, 120–127. doi:10.1016/j.intimp.2017.11.037
Li, K., Li, Y., Ma, Z., and Zhao, J. (2015). Crocin Exerts Anti-inflammatory and Anti-catabolic Effects on Rat Intervertebral Discs by Suppressing the Activation of JNK. Int. J. Mol. Med. 36 (5), 1291–1299. doi:10.3892/ijmm.2015.2359
Li, L., Zhang, H., Jin, S., and Liu, C. (2018). Effects of Crocin on Inflammatory Activities in Human Fibroblast-like Synoviocytes and Collagen-Induced Arthritis in Mice. Immunol. Res. 66 (3), 406–413. doi:10.1007/s12026-018-8999-2
Li, S., Liu, X., Lei, J., Yang, J., Tian, P., and Gao, Y. (2017). Crocin Protects Podocytes against Oxidative Stress and Inflammation Induced by High Glucose through Inhibition of NF-Κb. Cell Physiol Biochem 42 (4), 1481–1492. doi:10.1159/000479212
Li, X., Huang, T., Jiang, G., Gong, W., Qian, H., and Zou, C. (2013). Synergistic Apoptotic Effect of Crocin and Cisplatin on Osteosarcoma Cells via Caspase Induced Apoptosis. Toxicol. Lett. 221 (3), 197–204. doi:10.1016/j.toxlet.2013.06.233
Li, X., Jiang, C., and Zhu, W. (2017). Crocin Reduces the Inflammation Response in Rheumatoid Arthritis. Biosci. Biotechnol. Biochem. 81 (5), 891–898. doi:10.1080/09168451.2016.1263145
Liakopoulou-Kyriakides, M., and Kyriakidis, D. A. (2002). “Croscus Sativus-Biological Active Constitutents,”. Editor R. Atta ur (Amsterdam, Netherlands: Elsevier), Vol. 26, 293–312. doi:10.1016/s1572-5995(02)80009-6Studies in Natural Products Chemistry
Liang, J. J., Li, H. R., Chen, Y., Zhang, C., Chen, D. G., Liang, Z. C., et al. (2019). Diallyl Trisulfide Can Induce Fibroblast-like Synovial Apoptosis and Has a Therapeutic Effect on Collagen-Induced Arthritis in Mice via Blocking NF-Κb and Wnt Pathways. Int. Immunopharmacol 71, 132–138. doi:10.1016/j.intimp.2019.03.024
Lim, H. A., Song, E. K., Seon, J. K., Park, K. S., Shin, Y. J., and Yang, H. Y. (2017). Causes of Aseptic Persistent Pain after Total Knee Arthroplasty. Clin. Orthop. Surg. 9 (1), 50–56. doi:10.4055/cios.2017.9.1.50
Linton, M. F., and Fazio, S. (2003). Macrophages, Inflammation, and Atherosclerosis. Int. J. Obes. Relat. Metab. Disord. 27 (Suppl. l), S35–S40. doi:10.1038/sj.ijo.0802498
Liu, W., Sun, Y., Cheng, Z., Guo, Y., Liu, P., and Wen, Y. (2018). Crocin Exerts Anti-inflammatory and Anti-arthritic Effects on Type II Collagen-Induced Arthritis in Rats. Pharm. Biol. 56 (1), 209–216. doi:10.1080/13880209.2018.1448874
Lv, B., Huo, F., Zhu, Z., Xu, Z., Dang, X., Chen, T., et al. (2016). Crocin Upregulates CX3CR1 Expression by Suppressing NF-Κb/yy1 Signaling and Inhibiting Lipopolysaccharide-Induced Microglial Activation. Neurochem. Res. 41 (8), 1949–1957. doi:10.1007/s11064-016-1905-1
Makarov, S. S. (2001). NF-kappa B in Rheumatoid Arthritis: a Pivotal Regulator of Inflammation, Hyperplasia, and Tissue Destruction. Arthritis Res. 3 (4), 200–206. doi:10.1186/ar300
Marcus, R. (2002). An Expanded Overview of Postmenopausal Osteoporosis. J. Musculoskelet. Neuronal Interact 2 (3), 195–197.
Marzona, L., and Pavolini, B. (2009). Play and Players in Bone Fracture Healing Match. Clin. Cases Miner Bone Metab. 6 (2), 159–162.
Meki, A. R., Hamed, E. A., and Ezam, K. A. (2009). Effect of green tea Extract and Vitamin C on Oxidant or Antioxidant Status of Rheumatoid Arthritis Rat Model. Indian J. Clin. Biochem. 24 (3), 280–287. doi:10.1007/s12291-009-0053-7
Melnyk, J. P., Wang, S., and Marcone, M. F. (2010). Chemical and Biological Properties of the World's Most Expensive Spice: Saffron. Food Res. Int. 43 (8), 1981–1989. doi:10.1016/j.foodres.2010.07.033
Miao, C., Bai, L., Yang, Y., and Huang, J. (2021). Dysregulation of lncRNAs in Rheumatoid Arthritis: Biomarkers, Pathogenesis and Potential Therapeutic Targets. Front. Pharmacol. 12, 652751. doi:10.3389/fphar.2021.652751
Min, B. W., Kang, C. S., Lee, K. J., Bae, K. C., Cho, C. H., Choi, J. H., et al. (2018). Radiographic Progression of Osteoarthritis after Rotational Acetabular Osteotomy: Minimum 10-Year Follow-Up Outcome According to the Tönnis Grade. Clin. Orthop. Surg. 10 (3), 299–306. doi:10.4055/cios.2018.10.3.299
Mohamadpour, A. H., Ayati, Z., Parizadeh, M. R., Rajbai, O., and Hosseinzadeh, H. (2013). Safety Evaluation of Crocin (A Constituent of Saffron) Tablets in Healthy Volunteers. Iran J. Basic Med. Sci. 16 (1), 39–46.
Mollazadeh, H., Emami, S. A., and Hosseinzadeh, H. (2015). Razi's Al-Hawi and Saffron (Crocus Sativus): a Review. Iran J. Basic Med. Sci. 18 (12), 1153–1166.
Mostafa, N. Z., Fitzsimmons, R., Major, P. W., Adesida, A., Jomha, N., Jiang, H., et al. (2012). Osteogenic Differentiation of Human Mesenchymal Stem Cells Cultured with Dexamethasone, Vitamin D3, Basic Fibroblast Growth Factor, and Bone Morphogenetic Protein-2. Connect. Tissue Res. 53 (2), 117–131. doi:10.3109/03008207.2011.611601
Mostafavinia, S. E., Khorashadizadeh, M., and Hoshyar, R. (2016). Antiproliferative and Proapoptotic Effects of Crocin Combined with Hyperthermia on Human Breast Cancer Cells. DNA Cel Biol 35 (7), 340–347. doi:10.1089/dna.2015.3208
Mulherin, D., Fitzgerald, O., and Bresnihan, B. (1996). Synovial Tissue Macrophage Populations and Articular Damage in Rheumatoid Arthritis. Arthritis Rheum. 39 (1), 115–124. doi:10.1002/art.1780390116
Murphy, C. A., Langrish, C. L., Chen, Y., Blumenschein, W., McClanahan, T., Kastelein, R. A., et al. (2003). Divergent Pro- and Antiinflammatory Roles for IL-23 and IL-12 in Joint Autoimmune Inflammation. J. Exp. Med. 198 (12), 1951–1957. doi:10.1084/jem.20030896
Nakken, B., Papp, G., Bosnes, V., Zeher, M., Nagy, G., and Szodoray, P. (2017). Biomarkers for Rheumatoid Arthritis: From Molecular Processes to Diagnostic Applications-Current Concepts and Future Perspectives. Immunol. Lett. 189, 13–18. doi:10.1016/j.imlet.2017.05.010
Nam, K. N., Park, Y. M., Jung, H. J., Lee, J. Y., Min, B. D., Park, S. U., et al. (2010). Anti-inflammatory Effects of Crocin and Crocetin in Rat Brain Microglial Cells. Eur. J. Pharmacol. 648 (1-3), 110–116. doi:10.1016/j.ejphar.2010.09.003
NHI (2001). Osteoporosis Prevention, Diagnosis, and Therapy. Jama 285 (6), 785–795. doi:10.1001/jama.285.6.785
Nie, Z., Deng, S., Zhang, L., Chen, S., Lu, Q., and Peng, H. (2019). Crocin Protects against Dexamethasone-induced O-steoblast A-poptosis by I-nhibiting the ROS/Ca2+-mediated M-itochondrial P-athway. Mol. Med. Rep. 20 (1), 401–408. doi:10.3892/mmr.2019.10267
Noh, J.-Y., Yang, Y., and Jung, H. (2020). Molecular Mechanisms and Emerging Therapeutics for Osteoporosis. Ijms 21, 7623. doi:10.3390/ijms21207623
Ordoudi, S. A., Kyriakoudi, A., and Tsimidou, M. Z. (2015). Enhanced Bioaccessibility of Crocetin Sugar Esters from Saffron in Infusions Rich in Natural Phenolic Antioxidants. Molecules 20 (10), 17760–17774. doi:10.3390/molecules201017760
Pennock, A. T., Robertson, C. M., Emmerson, B. C., Harwood, F. L., and Amiel, D. (2007). Role of Apoptotic and Matrix-Degrading Genes in Articular Cartilage and Meniscus of Mature and Aged Rabbits during Development of Osteoarthritis. Arthritis Rheum. 56 (5), 1529–1536. doi:10.1002/art.22523
Pfander, H., and Schurtenberger, H. (1982). Biosynthesis of C20-Carotenoids in Crocus Sativus. Phytochemistry 21 (5), 1039–1042. doi:10.1016/S0031-9422(00)82412-7
Poursamimi, J., Shariati-Sarabi, Z., Tavakkol-Afshari, J., Mohajeri, S. A., Ghoryani, M., and Mohammadi, M. (2020). Immunoregulatory Effects of Krocina, a Herbal Medicine Made of Crocin, on Osteoarthritis Patients: A Successful Clinical Trial in Iran. Ijaai 19 (3), 253–263. doi:10.18502/ijaai.v19i3.3453
Radhakrishnan, A., Tudawe, D., Chakravarthi, S., Chiew, G. S., and Haleagrahara, N. (2014). Effect of γ-tocotrienol in Counteracting Oxidative Stress and Joint Damage in Collagen-Induced Arthritis in Rats. Exp. Ther. Med. 7 (5), 1408–1414. doi:10.3892/etm.2014.1592
Rathore, B., Jaggi, K., Thakur, S., Mathur, A., and Mahdi, A. A. (2015). Anti-inflammatory Activity of Crocus Sativus Extract in Experimental Arthritis. Int. J. Pharm. Sci. Res. 6, 1473–1478. doi:10.13040/IJPSR.0975-8232.6(4).1473-78
Redlich, K., and Smolen, J. S. (2012). Inflammatory Bone Loss: Pathogenesis and Therapeutic Intervention. Nat. Rev. Drug Discov. 11 (3), 234–250. doi:10.1038/nrd3669
Ríos, J. L., Recio, M. C., Giner, R. M., and Máñez, S. (1996). An Update Review of Saffron and its Active Constituents. Phytother. Res. 10 (3), 189–193. doi:10.1002/(SICI)1099-1573(199605)10:3<189:AID-PTR754>3.0.CO;2-C
Roman-Blas, J. A., and Jimenez, S. A. (2006). NF-kappaB as a Potential Therapeutic Target in Osteoarthritis and Rheumatoid Arthritis. Osteoarthritis Cartilage 14 (9), 839–848. doi:10.1016/j.joca.2006.04.008
Roodman, G. D. (2006). Regulation of Osteoclast Differentiation. Ann. N. Y Acad. Sci. 1068, 100–109. doi:10.1196/annals.1346.013
Ross, F. P. (2006). M-CSF, C-Fms, and Signaling in Osteoclasts and Their Precursors. Ann. N. Y Acad. Sci. 1068 (1), 110–116. doi:10.1196/annals.1346.014
Sakkas, L. I., and Platsoucas, C. D. (2007). The Role of T Cells in the Pathogenesis of Osteoarthritis. Arthritis Rheum. 56 (2), 409–424. doi:10.1002/art.22369
Salahshoor, M. R., Khashiadeh, M., Roshankhah, S., Kakabaraei, S., and Jalili, C. (2016). Protective Effect of Crocin on Liver Toxicity Induced by Morphine. Res. Pharm. Sci. 11 (2), 120–129.
Shafiee, M., Moghaddam, N. S. A., Tousi, M., Avan, A., Ryzhikov, M., et al. (2017). Saffron against Components of Metabolic Syndrome: Current Status and Prospective. J. Agric. Food Chem. 65 (50), 10837–10843. doi:10.1021/acs.jafc.7b03762
Shafiee, M., Arekhi, S., Omranzadeh, A., and Sahebkar, A. (2018). Saffron in the Treatment of Depression, Anxiety and Other Mental Disorders: Current Evidence and Potential Mechanisms of Action. J. Affect Disord. 227, 330–337. doi:10.1016/j.jad.2017.11.020
Sheng, L., Qian, Z., Zheng, S., and Xi, L. (2006). Mechanism of Hypolipidemic Effect of Crocin in Rats: Crocin Inhibits Pancreatic Lipase. Eur. J. Pharmacol. 543 (1-3), 116–122. doi:10.1016/j.ejphar.2006.05.038
Shi, L., Zhao, S., Chen, Q., Wu, Y., Zhang, J., and Li, N. (2018). Crocin Inhibits RANKL induced Osteoclastogenesis by Regulating JNK and NFκB Signaling Pathways. Mol. Med. Rep. 17 (6), 7947–7951. doi:10.3892/mmr.2018.8835
Silverwood, V., Blagojevic-Bucknall, M., Jinks, C., Jordan, J. L., Protheroe, J., and Jordan, K. P. (2015). Current Evidence on Risk Factors for Knee Osteoarthritis in Older Adults: a Systematic Review and Meta-Analysis. Osteoarthritis Cartilage 23 (4), 507–515. doi:10.1016/j.joca.2014.11.019
Sinkov, V., and Cymet, T. (2003). Osteoarthritis: Understanding the Pathophysiology, Genetics, and Treatments. J. Natl. Med. Assoc. 95 (6), 475–482.
Srivastava, R., Ahmed, H., Dixit, R. K., Dharamveer, , and Saraf, S. A. (2010). Crocus Sativus L.: A Comprehensive Review. Pharmacogn Rev. 4 (8), 200–208. doi:10.4103/0973-7847.70919
Sugerman, D. T., and Jin, J. (2014). JAMA Patient page. Talking to Your Doctor about Tests, Treatments, and Their Costs. JAMA 312 (1), 2178. doi:10.1001/jama.2013.28300910.1001/jama.2014.3693
Suh, K. S., Chon, S., Jung, W. W., and Choi, E. M. (2019). Crocin Attenuates Methylglyoxal-Induced Osteoclast Dysfunction by Regulating Glyoxalase, Oxidative Stress, and Mitochondrial Function. Food Chem. Toxicol. 124, 367–373. doi:10.1016/j.fct.2018.12.031
Szekanecz, Z., Kerekes, G., Végh, E., Kardos, Z., Baráth, Z., Tamási, L., et al. (2016). Autoimmune Atherosclerosis in 3D: How it Develops, How to Diagnose and what to Do. Autoimmun. Rev. 15 (7), 756–769. doi:10.1016/j.autrev.2016.03.014
Takaishi, H., Kimura, T., Dalal, S., Okada, Y., and D'Armiento, J. (2008). Joint Diseases and Matrix Metalloproteinases: a Role for MMP-13. Curr. Pharm. Biotechnol. 9 (1), 47–54. doi:10.2174/138920108783497659
Takayanagi, H., Iizuka, H., Juji, T., Nakagawa, T., Yamamoto, A., Miyazaki, T., et al. (2000). Involvement of Receptor Activator of Nuclear Factor kappaB Ligand/osteoclast Differentiation Factor in Osteoclastogenesis from Synoviocytes in Rheumatoid Arthritis. Arthritis Rheum. 43 (2), 259–269. doi:10.1002/1529-0131(200002)43:2<259:Aid-anr4>3.0.Co;2-w
Tardif, G., Reboul, P., Pelletier, J. P., and Martel-Pelletier, J. (2004). Ten Years in the Life of an Enzyme: the story of the Human MMP-13 (Collagenase-3). Mod. Rheumatol. 14 (3), 197–204. doi:10.1007/s10165-004-0292-7
Teitelbaum, S. L. (2000). Bone Resorption by Osteoclasts. Science 289 (5484), 1504–1508. doi:10.1126/science.289.5484.1504
Todd, J. A., and Robinson, R. J. (2003). Osteoporosis and Exercise. Postgrad. Med. J. 79 (932), 320–323. doi:10.1136/pmj.79.932.320
Tsimidou, M., and Tsatsaroni, E. (1993). Stability of Saffron Pigments in Aqueous Extracts. J. Food Sci. 58 (5), 1073–1075. doi:10.1111/j.1365-2621.1993.tb06116.x
Udagawa, N., Takahashi, N., Jimi, E., Matsuzaki, K., Tsurukai, T., Itoh, K., et al. (1999). Osteoblasts/stromal Cells Stimulate Osteoclast Activation through Expression of Osteoclast Differentiation Factor/RANKL but Not Macrophage colony-stimulating Factor: Receptor Activator of NF-Kappa B Ligand. Bone 25 (5), 517–523. doi:10.1016/S8756-3282(99)00210-0
Udalamaththa, V. L., Jayasinghe, C. D., and Udagama, P. V. (2016). Potential Role of Herbal Remedies in Stem Cell Therapy: Proliferation and Differentiation of Human Mesenchymal Stromal Cells. Stem Cel Res Ther 7 (1), 110. doi:10.1186/s13287-016-0366-4
Vafaei, S., Motejaded, F., and Ebrahimzadeh-bideskan, A. (2020). Protective Effect of Crocin on Electromagnetic Field-Induced Testicular Damage and Heat Shock Protein A2 Expression in Male BALB/c Mice. Iran J. Basic Med. Sci. 23 (1), 102–110. doi:10.22038/ijbms.2019.38896.9229
Walsh, N. C., and Gravallese, E. M. (2010). Bone Remodeling in Rheumatic Disease: a Question of Balance. Immunol. Rev. 233 (1), 301–312. doi:10.1111/j.0105-2896.2009.00857.x
Wang, J. F., Xu, H. J., He, Z. L., Yin, Q., and Cheng, W. (2020). Crocin Alleviates Pain Hyperalgesia in AIA Rats by Inhibiting the Spinal Wnt5a/β-Catenin Signaling Pathway and Glial Activation. Neural Plast. 2020, 4297483. doi:10.1155/2020/4297483
Winterhalter, P., and Straubinger, M. (2000). Saffron-renewed Interest in an Ancient Spice. Food Rev. Int. 16 (1), 39–59. doi:10.1081/FRI-100100281
Wu, T., Zhang, J., Geng, M., Tang, S. J., Zhang, W., and Shu, J. (2017). Nucleoside Reverse Transcriptase Inhibitors (NRTIs) Induce Proinflammatory Cytokines in the CNS via Wnt5a Signaling. Sci. Rep. 7 (1), 4117. doi:10.1038/s41598-017-03446-w
Xie, Y., He, Q., Chen, H., Lin, Z., Xu, Y., and Yang, C. (2019). Crocin Ameliorates Chronic Obstructive Pulmonary Disease-Induced Depression via PI3K/Akt Mediated Suppression of Inflammation. Eur. J. Pharmacol. 862, 172640. doi:10.1016/j.ejphar.2019.172640
Xu, F., and Teitelbaum, S. L. (2013). Osteoclasts: New Insights. Bone Res. 1 (1), 11–26. doi:10.4248/BR201301003
Yamaguchi, T. (2014). Updates on Lifestyle-Related Diseases and Bone Metabolism. The Metabolic Syndrome and Bone Metabolism. Clin. Calcium 24 (11), 1599–1604.
Yamashita, T., Takahashi, N., and Udagawa, N. (2012). New Roles of Osteoblasts Involved in Osteoclast Differentiation. World J. Orthop. 3 (11), 175–181. doi:10.5312/wjo.v3.i11.175
Yasuda, H., Shima, N., Nakagawa, N., Yamaguchi, K., Kinosaki, M., Mochizuki, S., et al. (1998). Osteoclast Differentiation Factor Is a Ligand for Osteoprotegerin/osteoclastogenesis-Inhibitory Factor and Is Identical to TRANCE/RANKL. Proc. Natl. Acad. Sci. U S A. 95 (7), 3597–3602. doi:10.1073/pnas.95.7.3597
Yokota, K., Sato, K., Miyazaki, T., Kitaura, H., Kayama, H., Miyoshi, F., et al. (2014). Combination of Tumor Necrosis Factor α and Interleukin-6 Induces Mouse Osteoclast-like Cells with Bone Resorption Activity Both In Vitro and In Vivo. Arthritis Rheumatol. 66 (1), 121–129. doi:10.1002/art.38218
Yoo, J. H., Oh, H. C., Park, S. H., Kim, J. K., and Kim, S. H. (2018). Does Obesity Affect Clinical and Radiological Outcomes in Minimally Invasive Total Knee Arthroplasty? Minimum 5-Year Follow-Up of Minimally Invasive TKA in Obese Patients. Clin. Orthop. Surg. 10 (3), 315–321. doi:10.4055/cios.2018.10.3.315
Yu, Y., Mu, J., Fan, Z., Lei, G., Yan, M., Wang, S., et al. (2012). Insulin-like Growth Factor 1 Enhances the Proliferation and Osteogenic Differentiation of Human Periodontal Ligament Stem Cells via ERK and JNK MAPK Pathways. Histochem. Cel Biol 137 (4), 513–525. doi:10.1007/s00418-011-0908-x
Yuan, S., Shi, Y., Guo, K., and Tang, S. J. (2018). Nucleoside Reverse Transcriptase Inhibitors (NRTIs) Induce Pathological Pain through Wnt5a-Mediated Neuroinflammation in Aging Mice. J. Neuroimmune Pharmacol. 13 (2), 230–236. doi:10.1007/s11481-018-9777-6
Yuan, X., Cao, H., Wang, J., Tang, K., Li, B., Zhao, Y., et al. (2017). Immunomodulatory Effects of Calcium and Strontium Co-doped Titanium Oxides on Osteogenesis. Front. Immunol. 8, 1196. doi:10.3389/fimmu.2017.01196
Zaminy, A., Ragerdi Kashani, I., Barbarestani, M., Hedayatpour, A., Mahmoudi, R., and Farzaneh Nejad, A. (2008). Osteogenic Differentiation of Rat Mesenchymal Stem Cells from Adipose Tissue in Comparison with Bone Marrow Mesenchymal Stem Cells: Melatonin as a Differentiation Factor. Iran Biomed. J. 12 (3), 133–141.
Zheng, Y. Q., Liu, J. X., Wang, J. N., and Xu, L. (2007). Effects of Crocin on Reperfusion-Induced Oxidative/nitrative Injury to Cerebral Microvessels after Global Cerebral Ischemia. Brain Res. 1138, 86–94. doi:10.1016/j.brainres.2006.12.064
Zhou, J., Zhang, Q., Yuan, X., Wang, J., Li, C., Sheng, H., et al. (2013). Association between Metabolic Syndrome and Osteoporosis: a Meta-Analysis. Bone 57 (1), 30–35. doi:10.1016/j.bone.2013.07.013
Zhu, J., Yamane, H., and Paul, W. E. (2010). Differentiation of Effector CD4 T Cell Populations (*). Annu. Rev. Immunol. 28, 445–489. doi:10.1146/annurev-immunol-030409-101212
Keywords: crocin, bone, cartilage, inflammation, cell differentiation
Citation: Vafaei S, Wu X, Tu J and Nematollahi-mahani SN (2022) The Effects of Crocin on Bone and Cartilage Diseases. Front. Pharmacol. 12:830331. doi: 10.3389/fphar.2021.830331
Received: 07 December 2021; Accepted: 28 December 2021;
Published: 19 January 2022.
Edited by:
Longhuo Wu, Gannan Medical University, ChinaReviewed by:
Yujie Deng, Guangzhou Regenerative Medicine and Health Guangdong Laboratory, ChinaAlbert Hoi Hung Cheung, The Chinese University of Hong Kong, China
Chen Zhu, Anhui Provincial Hospital, China
Copyright © 2022 Vafaei, Wu, Tu and Nematollahi-mahani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiajie Tu, dHVqaWFqaWVAYWhtdS5lZHUuY24=; Seyed Noureddin Nematollahi-mahani, bm5lbWF0b2xsYWhpQGttdS5hYy5pcg==
 Shayan Vafaei
Shayan Vafaei Xuming Wu2
Xuming Wu2 Jiajie Tu
Jiajie Tu