- 1Department of Dermatology, Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 2Institute of Dermatology, Shanghai Academy of Traditional Chinese Medicine, Shanghai, China
Background: The use of Chinese herbal medicine (CHM) for the treatment of atopic dermatitis (AD) has gained attention. This quantitative study systematically evaluated the efficacy and safety of CHM for the treatment of AD in eight high-level clinical trials, resulting in a high level of clinical evidence.
Methods: Several databases were searched, including PubMed, Embase, Cochrane Library, Web of Science, China National Knowledge Infrastructure (CNKI), the Chongqing VIP Chinese Science (VIP), and Wanfang Database. High-quality randomized controlled trials (RCTs) comparing CHM with placebo were included. The 95% confidence interval (CI) of the risk ratio (RR) was calculated using software (RevMan 5.3) and a meta-analysis was performed. Evidence level evaluation using GRADE Profiler 3.6.
Results: In total, 662 patients (322 in the experimental group and 340 in the control group) were included. The response rate of the Eczema Area and Severity Index (EASI) −90 was higher in the CHM group than in the placebo group (RR, 3.72; 95% CI, 1.76 to7.83; p = 0.01). Furthermore, the scoring of atopic dermatitis (SCORAD) (RR, −10.20), body surface area (BSA) (RR, −2.01), surface damage score (RR, −2.25), visual analog scale (VAS) (RR, −1.90), and sleep score (RR, −2.16), improvement of investigator’s global assessment (IGA) (RR, 2.94) improved in the CHM group. The results showed no statistical difference between CHM and placebo (MD, −0.47; 95% CI, −1.30, 0.37; p = 0.27) in improving the Dermatology Life Quality Index (DLQI) or children’s DLQI (CDLQI). There was also no significant difference in the IgE level between the two groups (MD, −62.76; 95% CI, −809.58, 684.05; p = 0.87). However, the adverse events (AEs) rate was slightly higher in patients treated with CHM than in those treated with placebo (RR, 1.42; 95% CI, 1.06–1.90; p = 0.02).
Conclusion: CHM improved the size and severity of the skin lesions and sleep quality in patients with AD. Comparing the adverse effects between the two groups, CHM is safe. However, CHM does not improve the quality of life or the patient’s IgE levels.
1 Introduction
Atopic dermatitis (AD) is a dermatological disease characterized by chronic inflammation (Damour, et al., 2020). Studies have found that more than 20% of children and 3% of adults worldwide suffer from atopic dermatitis (Nutten, 2015). Epidemiological studies in the United States and Europe over the past 20 years have shown a prevalence of atopic dermatitis of up to 25%, with an increasing trend over the years (Sybilski, et al., 2015). The basic clinical features are intensely pruritic dry, or eczema-like skin lesions (Lacouture and Sibaud 2018). Patients with AD often have other atopic diseases such as allergic rhinitis and asthma. These conditions can lead to sleep deprivation, depression, anxiety, social embarrassment, and other psychosocial concerns (Nutten, 2015).
The etiology of AD is unclear. Genetic factors, allergen stimulation (food, inhalation, etc.), autoantigens, infection, or skin dysfunction are all associated with the development of AD (Avena-Woods, 2017). In healthy humans, there is a dynamic balance in the Th1/Th2 cells. For AD patients with AD, there is an imbalance in the Th1/Th2 cells. This has emerged as an important mechanism in the pathogenesis of AD and is thought to be an important factor in disease progression. This imbalance is mainly caused by the overexpression of Th2 cytokines such as IL-4, IL-13, and IL-31 (Huang, et al., 2013). Secretion of thymic stromal lymphopoietin (TSLP) by epithelial cells, expressed in epithelial and stromal cells, is also a major allergenic cytokine in AD (Wilson, et al., 2013). Additionally, IgE is considered a hallmark antibody for allergic diseases such as AD. IgE is elevated in approximately 50%–80% of patients with atopic dermatitis and is one of the indicators for the diagnosis of atopic dermatitis (Furue, et al., 2017).
Traditional treatments for AD include antihistamines, topical corticosteroids, and immunosuppressants (Czarnowicki, et al., 2019). However, antihistamines are unsatisfactory for treating pruritus (Gholyaf, et al., 2020), and glucocorticoids cannot be used long-term because of their potential side effects (Ronchetti, et al., 2021), biologics are expensive, and relapse is common after withdrawal. Because of the chronic and relapsing nature of AD, treatment must be effective and have few side effects.
Chinese herbal medicine (CHM) has considerable benefits and low toxicity for the treatment of skin diseases and has a complete theoretical basis (Luo et al., 2021). Currently, there is growing interest in Chinese herbal medicine (CHM) as a potential complementary and alternative therapy (Cao, et al., 2015). The treatment of atopic dermatitis with CHM is diverse and mainly divided into internal and external treatments, all of which are reported to have good efficacy (Lin, et al., 2019). This may be related to the that many herbs and their active ingredients have anti-inflammatory, anti-allergic, antioxidant, and anti-angiogenic effects, and can mitigate the effects of AD by restoring the skin barrier while balancing Th1/Th2 cell levels and regulating the expression of cytokines and chemokines through a variety of mechanisms with few side effects (Yan, et al., 2020).
CHM has also been questioned as complementary and alternative medicine for the treatment of AD (Berke, et al., 2012). Several systematic reviews about the efficacy of CHM in the treatment of AD have been published (Gu, et al., 2013; Tan, et al., 2013). However, all of them lack high-level clinical evidence and a substantial amount of new trials have been published. So, this review aimed to systematically evaluate the efficacy and safety of CHM as a treatment for AD, based on high-quality clinical studies.
2 Methods
This study was conducted according to the Cochrane Handbook on Systematic Review of Interventions and Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines (Liberati, et al., 2009) (Supplementary Table S1).
2.1 Search strategy
We searched seven databases, PubMed, Embase, Cochrane Library, Web of Science, China National Knowledge Infrastructure (CNKI), the Chongqing VIP Chinese Science (VIP), and Wanfang Database from inception to 15 February 2022. We used free text words for the search in the title and abstract. The search formula is as follows (“Atopic dermatitis” OR “Eczema” OR “Dermatitis”) and (“Traditional Chinese Medicine” OR “Chinese drug” OR “Chinese herbal drug” OR “herbal”) and (“Clinical” OR “trial” OR “Clinical trial”) (Supplementary Table S2).
2.2 Inclusion and exclusion criteria
The inclusion criteria for the study were: 1) patients diagnosed according to diagnostic criteria; 2) randomized controlled trials (RCTs) comparing CHM with placebo for AD, 3) RCTs with a Jadad score ≥4 (Jadad, et al., 1996), and 4) studies must report adverse effects and efficacy outcome indicators.
The exclusion criteria were 1) the two groups had different modes of drug delivery method, and 2) combination intervention using drugs other than CHM in the trial group.
2.3 Data extraction
Two researchers (X.C. Cai, and X.Y. Sun) carefully screened eligible articles based on the inclusion and exclusion criteria. Two researchers (S.G. Hong and J. Wang) completed separate tables for data extraction, including author name, publication year, sample characteristics (size, age, sex, and duration), interventions in the experiment (specific drug names, composition, and dosage), and control groups. The inconsistencies were confirmed by a third investigator (L. Liu).
2.4 Outcome measures
The primary outcome was the number of patients whose EASI scores decreased by 50%/75%/90% or more from baseline. EASI scores is a composite score that allows the assessment of lesion severity and area. A dermatologist evaluated the clinical presentation score (erythema, induration or population, excoriation, and lichenification), lesion area size score, and body surface area score and then calculated the EASI score. Scoring Atopic Dermatitis (SCORAD) clinical tool, which includes the assessment of clinical signs and symptoms and the patient’s self-assessment of pruritus and sleep, was used as a secondary outcome. Other secondary outcomes included body surface area (BSA), surface damage score, Investigator’s Global Assessment decreased by 1/2 points (IGA 1/IGA 2), Dermatology Quality of Life Index/Children’s Dermatology Quality of Life Index (DLQI/CDLQI), visual analog scale (VAS), sleep score, IgE, and adverse events (AEs).
2.5 Risk of bias
To assess the quality of the clinical trials, two investigators (J.L.Chen, and M. Zhang) completed the Jadad scale for each of the included studies. When the two authors disagreed, a third investigator (C.X. Wang) was consulted. The Jadad scale has four dimensions (randomization, concealment, blind method, and reports of withdrawals), with a total of seven scores. Trials scoring ≥ 4 points were considered high quality (Jadad, et al., 1996).
2.6 Statistical analysis
We used RevMan5.3 software provided by the Cochrane Collaboration, to synthesize the results of the meta-analysis. When we extracted date from the included articles and found that several articles report three levels of EASI score (90/75/50), for which we set up a subgroup analysis to obtain more complete results. Risk ratios (RR) with 95% confidence intervals (CI) were assessed for dichotomous data, continuous data, mean differences (MD), and standard mean differences (SMD). Throughout the experiment, if homogeneity was present (p > 0.1, I2<50%), a fixed-effects model was used; otherwise, a random-effects model was used. Statistical significance was set at p < 0.05. Evidence level evaluation using GRADE Profiler 3.6.
3 Results
3.1 Included studies
After searching five databases, we initially identified 490 studies and 26 articles from relevant references. Of these, 217 duplicate articles were excluded and 189 irrelevant articles were removed after reviewing the title and abstract. Of the 84 remaining studies, 76 were excluded (six did not have full text or protocols, 13 used medicinal alternatives that were not CHM, 14 were not RCTs, and 30 were not placebo-controlled). Finally, the remaining 21 studies were assessed using the Jadad score, of which 8 studies met the inclusion criteria (Jadad score ≥4) (Hon, et al., 2007; Sun, 2009; Cheng, et al., 2011; Gu, et al., 2018; Huang, et al., 2019; Tian, 2019; Lin, et al., 2020; Liu, 2021). Five trials were published in English and three in Chinese. Figure 1 shows a flowchart of the screening process.
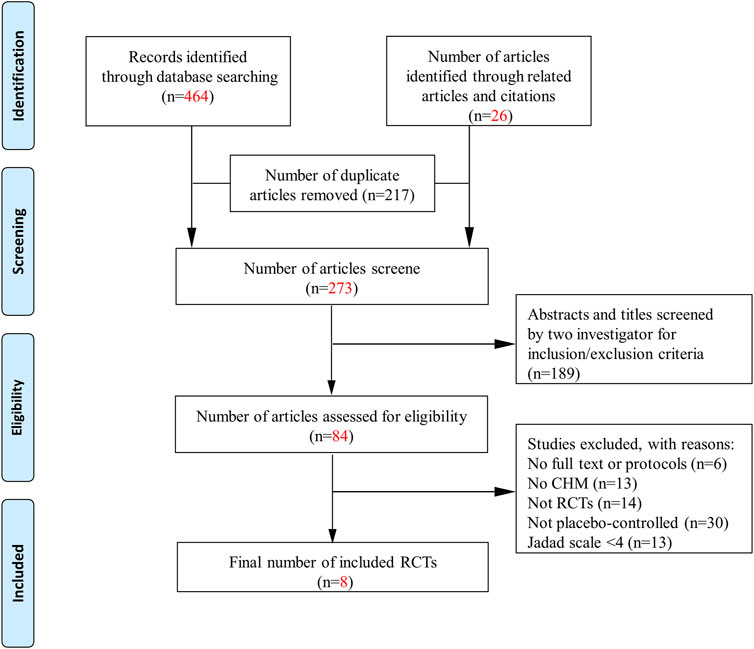
FIGURE 1. Flowchart. CHM, Chinese herbal medicine; RCTs: randomized control trials; AEs, adverse events.
3.2 Study characteristics
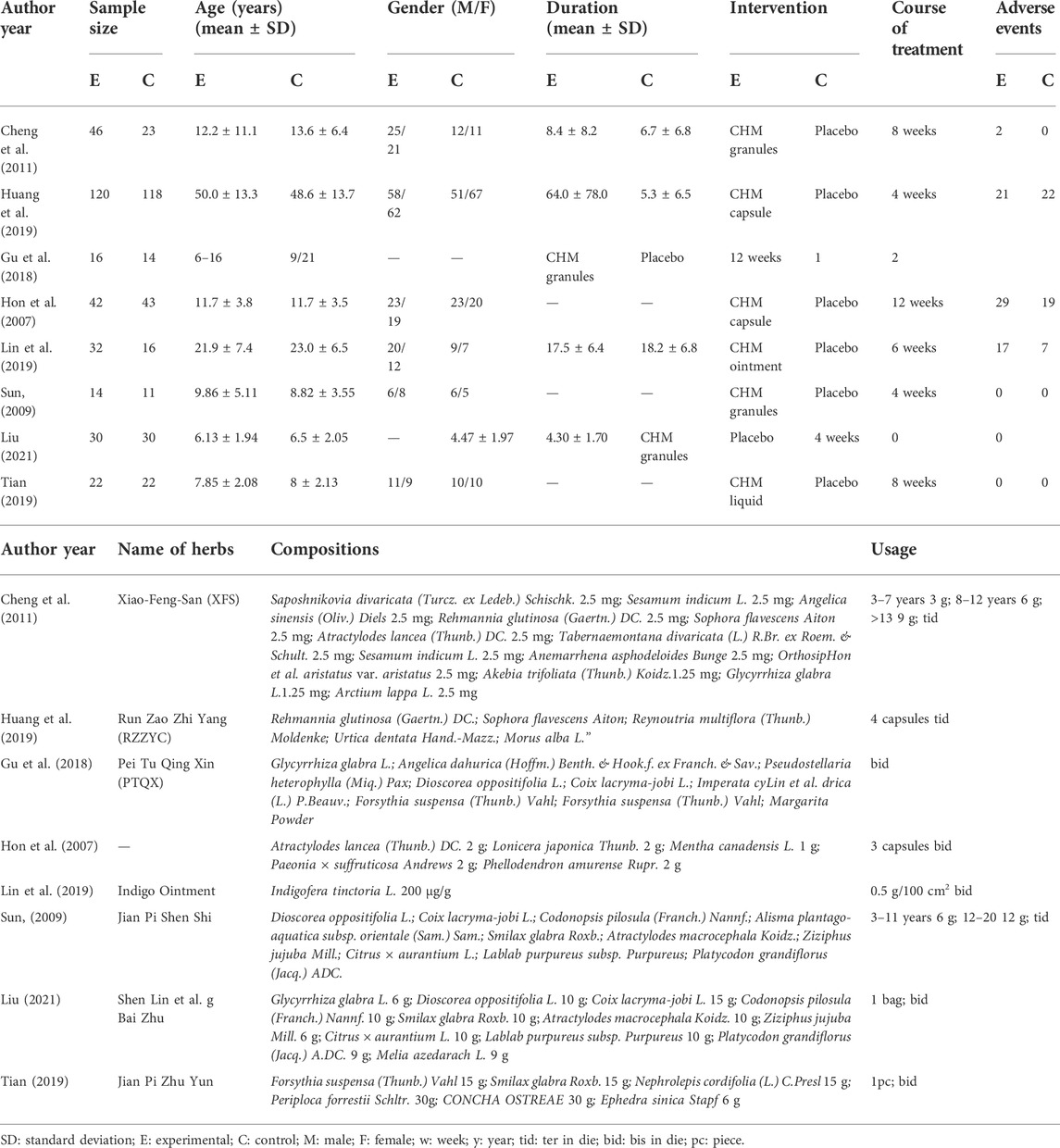
In total, 662 patients (322 in the experimental group and 340 in the control group) were included. A placebo was used in the control group in all eight trials. However, the intervention drugs were not identical. Four trials (Sun, 2009; Cheng, et al., 2011; Gu, et al., 2018; Liu, 2021) used granules, two (Hon, et al., 2007; Huang, et al., 2019) used capsules, and one (Lin, et al., 2020) used ointments, and one (Tian, 2019) used liquids. The treatment duration varied from 4 to 12 weeks. Four (Sun, 2009; Tian, 2019; Lin, et al., 2020; Liu, 2021) reported the number of patients achieving EASI-90 at the end of treatment, three (Sun, 2009; Lin, et al., 2020; Liu, 2021) reported on EASI-75, and four (Sun, 2009; Tian, 2019; Lin, et al., 2020; Liu, 2021) reported on EASI-50, which signifies an EASI score reduction of at least 90, 75, and 50%, respectively. Three trials (Sun, 2009; Tian, 2019; Liu, 2021) assessed SCORAD, four (Sun, 2009; Tian, 2019; Lin, et al., 2020; Liu, 2021) measured the BSA score, and three (Sun, 2009; Tian, 2019; Liu, 2021) reported on the surface damage score, two (Huang, et al., 2019; Lin, et al., 2020) used IGA 1 or IGA 2, four trials (Gu, et al., 2018; Huang, et al., 2019; Tian, 2019; Lin, et al., 2020) assessed DLQI/CDLQI, five (Sun, 2009; Huang, et al., 2019; Tian, 2019; Lin, et al., 2020; Liu, 2021) measured VAS scores, two (Sun, 2009; Tian, 2019) reported sleep scores, and two (Cheng, et al., 2011; Liu, 2021) detected cytokine IgE levels. Adverse events were reported in all eight trials. The names of the CHMs, drug composition, doses, and dosages are listed in Table 1.
3.3 Introduction of Chinese herbs
Forty-two herbs were used in the eight studies. More than three times use were Glycyrrhiza glabra L.; Dioscorea oppositifolia L.; Coix lacrymal-Jobi L.; Smilax glabra Roxb.
3.4 Risk of bias
Methodological quality was evaluated using Jadad scores, and the eight included trials were high-quality articles with Jadad scores ≥4. Sensitivity analysis was done for Jadad scores ≥4 and <4 (Supplementary Figure S1). All articles were performed by random and assigned concealment, but two studies (Sun, 2009; Huang, et al., 2019) did not report how the random sequence was generated, and three articles (Sun, 2009; Huang, et al., 2019; Liu, 2021) did not provide details of the concealment process. Although all articles utilized blinding, one article (Tian, 2019) did not specify whether the study was double-blinded, and one article (Sun, 2009) did not provide details regarding the placebo (Supplementary Table S3).
3.5 Primary outcome
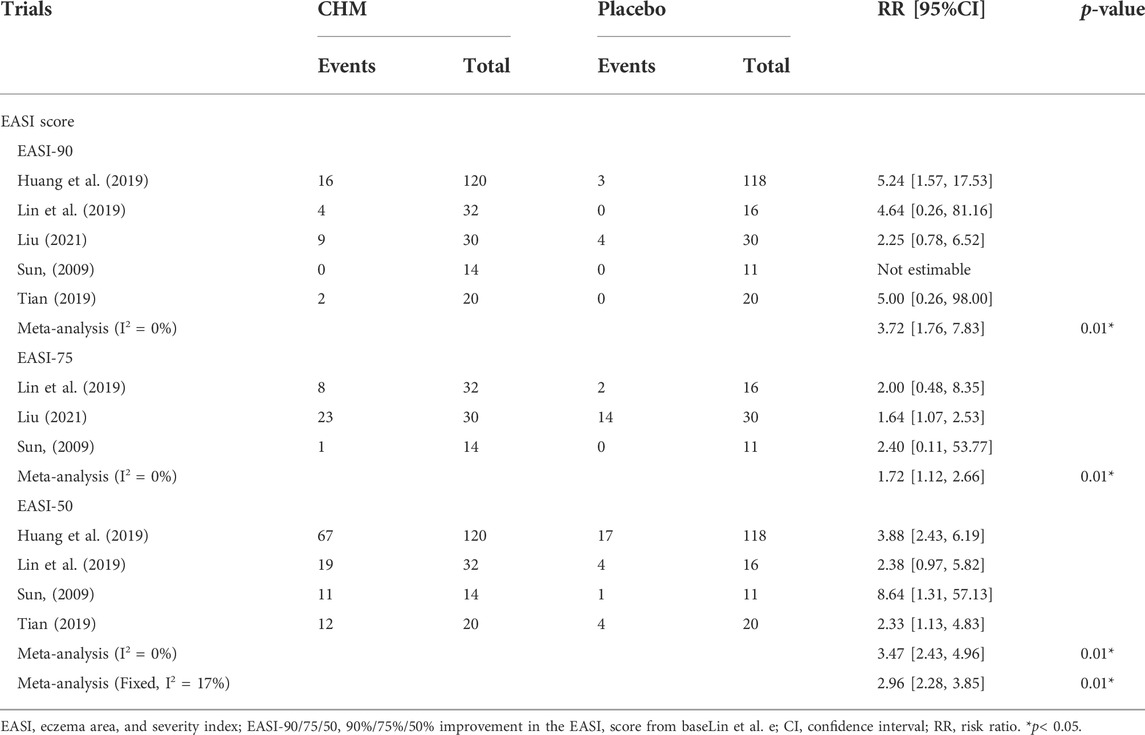
3.5.1 EASI 90/75/50
We performed a subgroup analysis of the different EASI score decline rates. The EASI-90 response rate was higher in the CHM group than in the placebo group (EASI-90: RR, 3.72; 95% CI, 1.76 to 7.83; p = 0.01) (Table 2; Supplementary Figure S2). For the EASI-75 and EASI-50, the results were not statistically significant (EASI-75: RR, 1.72; 95% CI, 1.12 to 2.66; p = 0.01; EASI-50: RR, 3.47; 95% CI, 2.28 to 3.85; p = 0.01).
3.6 Secondary outcome
3.6.1 Scoring of atopic dermatitis (SCORAD)
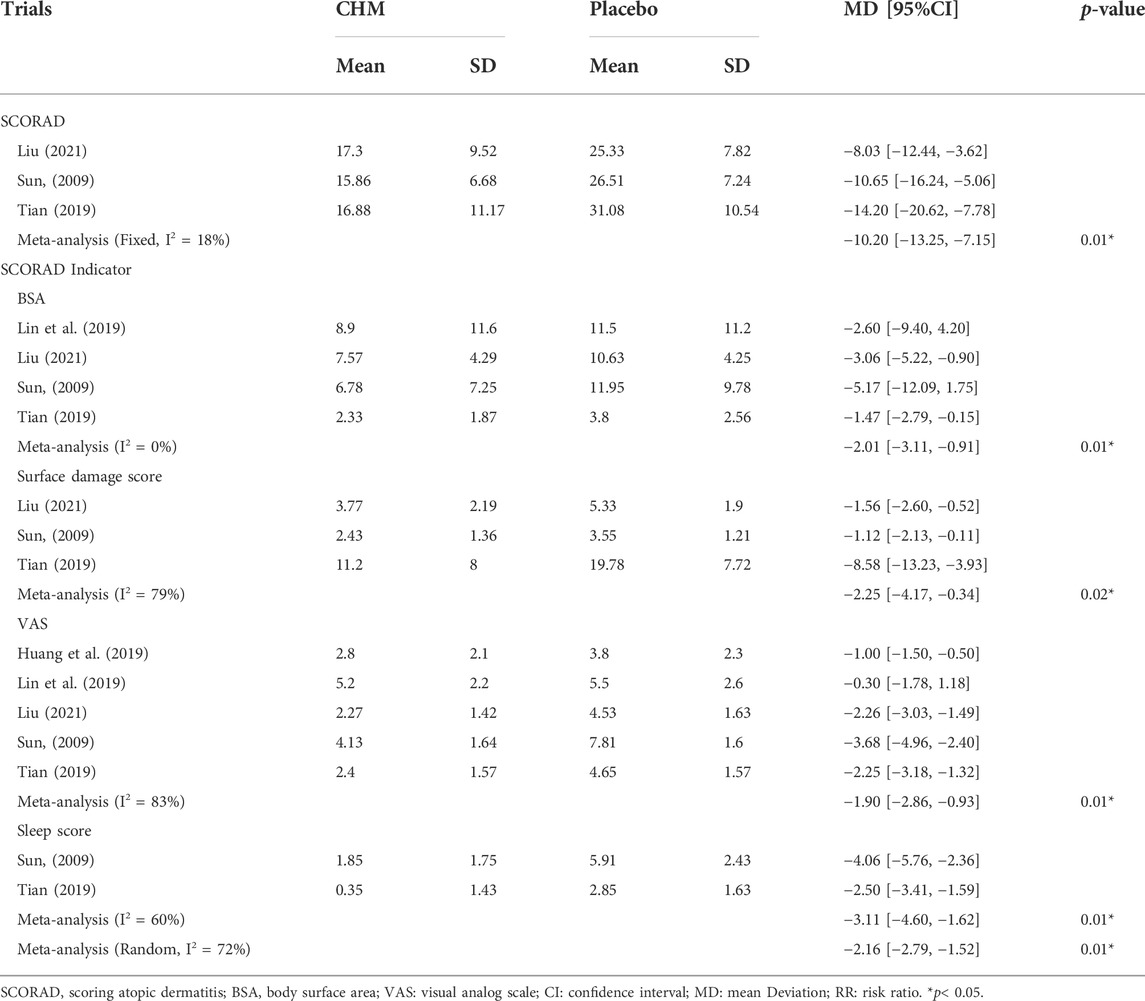
Patients receiving CHM had a lower SCORAD than those taking placebo (MD, −10.20; 95% CI, −13.25 to −7.15; p = 0.01) (Table 3; Supplementary Figure S3).
3.6.2 Body surface area (BSA)
Compared to the placebo group, BSA was lower in patients receiving CHM (MD, −2.01; 95% CI, −3.11 to −0.91; p = 0.01) (Table 3; Supplementary Figure S3).
3.6.3 Surface damage score
The surface damage score was lower in patients receiving CHM than patients in the placebo group (MD, −2.25; 95% CI, −4.17 to −0.34; p = 0.02) (Table 3; Supplementary Figure S3).
3.6.4 Visual analog scale (VAS)
The visual analog scale (VAS) was used to assess the pruritus severity. The CHM group had lower VAS scores than the control group (MD, −1.90; 95% CI, −2.86 to −0.93; p = 0.01) (Table 3; Supplementary Figure S3).
3.6.5 Sleep score
Two trials applied sleep scores to assess the sleep quality of patients with AD. Our meta-analysis indicated that the CHM group had lower scores than did the control group (MD, −3.11; 95% CI, −4.60 to −1.62; p = 0.01) (Table 3; Supplementary Figure S3).
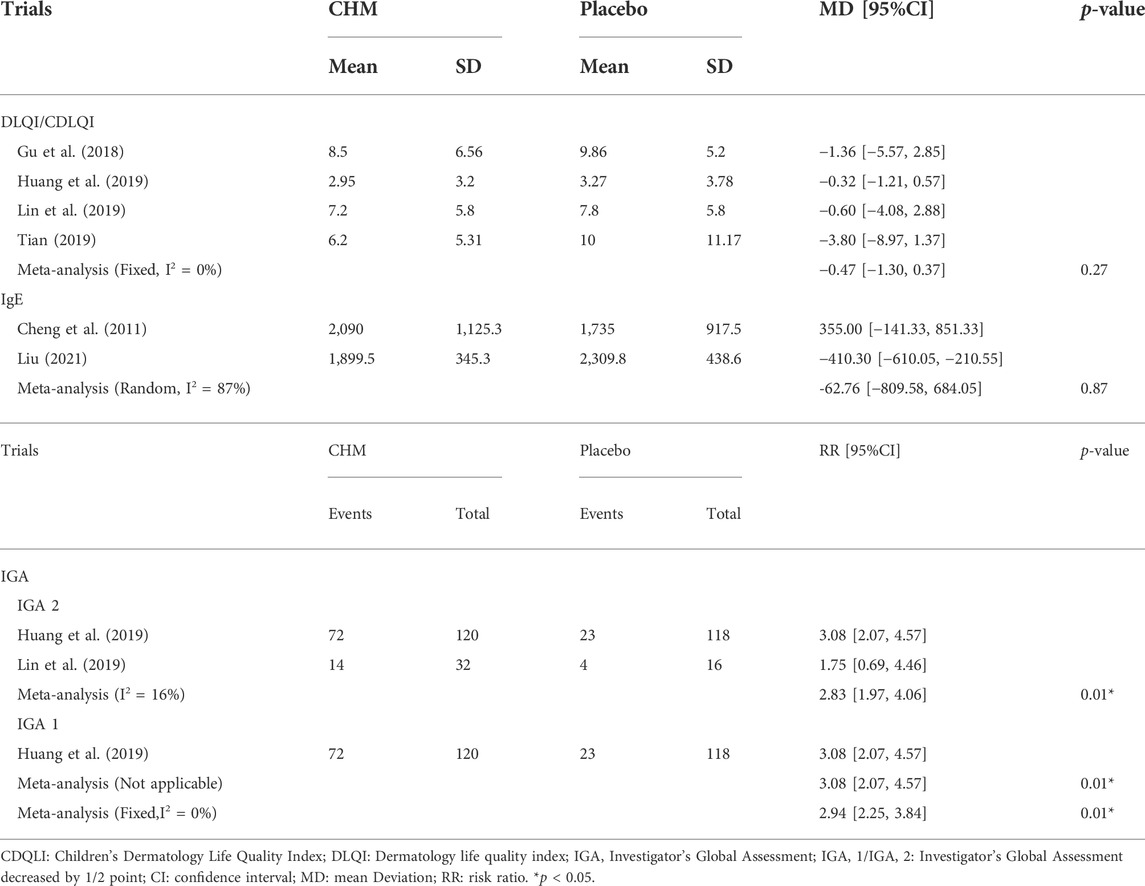
3.6.6 DLQI/CDLQI
Four trials applied the Dermatology Life Quality Index/Children’s Dermatology Life Quality Index to assess the quality of life of patients with AD. The results suggested no significant difference between CHM and placebo (MD, -0.47; 95% CI, −1.30 to 0.37; p = 0.27) (Table 4; Supplementary Figure S3).
3.6.7 IgE
The IgE level is important in patients with AD. The results suggested no significant difference between CHM and placebo (MD, −62.76; 95% CI, −809.58 to 684.05; p = 0.87) (Table 4; Supplementary Figure S3).
3.6.8 Investigator’s global assessment (IGA)
There were more patients in the herbal group with IGA2 (Investigator’s Global Assessment decreased by two points) than in the placebo group (RR, 2.83; 95% CI, 1.97–4.06; p = 0.01). For IGA1 (the Investigator’s Global Assessment decreased by 1 point), the number of patients in the CHM group was higher than that in the placebo group (RR, 3.08; 95% CI, 2.07–4.57; p = 0.01), and overall (RR, 2.94; 95% CI, 2.25–3.84; p = 0.01) (Table 4; Supplementary Figure S3).
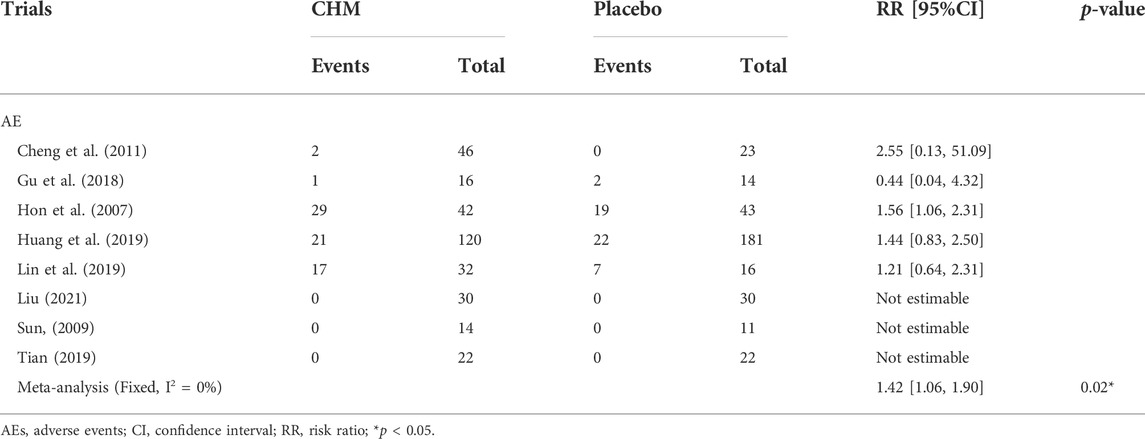
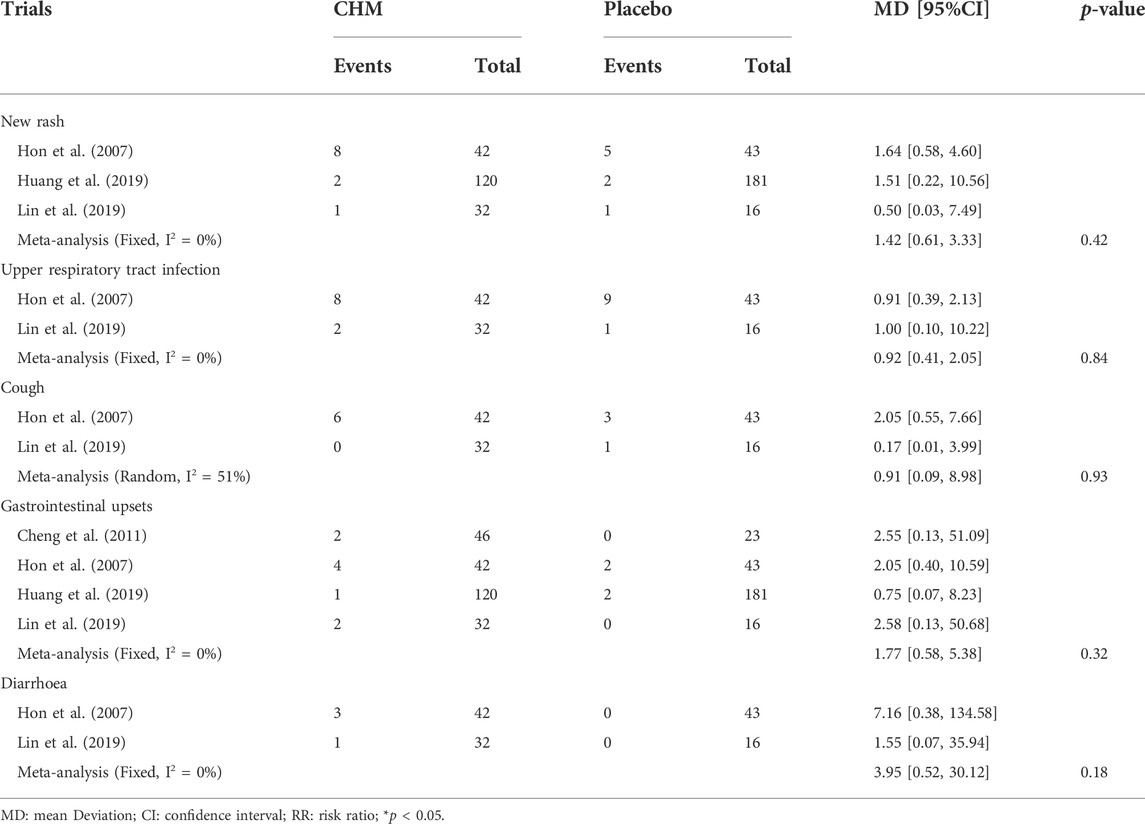
3.6.9 Safety
All trials assessed adverse events (AEs). The reported AEs included a new rash, upper respiratory tract infection, cough, gastrointestinal upsets, and diarrhea. Our results demonstrated that the incidence of AEs in patients treated with CHM was slightly higher than that in the placebo group (RR, 1.42; 95% CI, 1.06–1.90; p = 0.02) (Table 5; Supplementary Figure S4). We also classified the AEs into different body systems, including the neurological, dermatologic, respiratory, digestive, and reproductive systems (Figure 2).
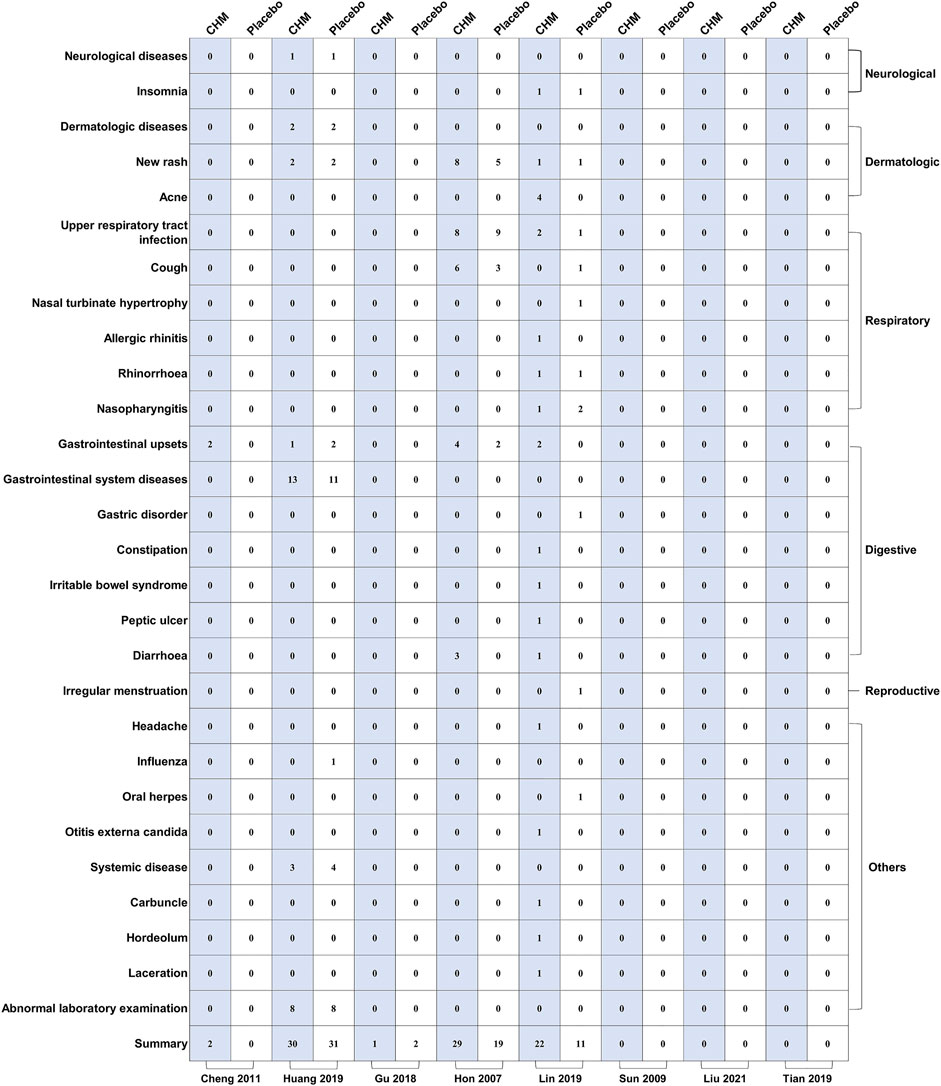
FIGURE 2. The mapping of specific adverse events between biological agents and control groups. MTX: methotrexate.
We evaluated five adverse reactions: new rash (RR, 1.42; 95% CI, 0.61–3.33; p = 0.42), upper respiratory tract infection (RR, 0.92; 95% CI, 0.41–2.05; p = 0.84), cough (RR, 0.91; 95% CI, 0.09–8.89; p = 0.93), gastrointestinal upsets (RR, 1.77; 95% CI, 0.58–5.38; p = 0.32), and diarrhea (RR, 3.95; 95% CI, 0.52–30.12; p = 0.18) (Table 6; Supplementary Figure S5).
3.6.10 Evidence level
EASI-50, DLQI/CDLQI, VAS, New rush, Cough, gastrointestinal upsets, and total AE were moderate. Because the IgE result inconsistency was very serious, so the rating is low, and the rest are of high quality (Supplementary Figure S6).
4 Discussion
This systematic review included eight high-quality RCTs that evaluated the efficacy and safety of CHM for AD. Our study data showed an improvement in the CHM group compared to the placebo group. For the EASI-90, the arrival rate in the CHM group was higher (RR, 3.72) than that in the placebo group. This indicates that herbs are more likely to clear AD lesions than placebos are. In addition, other efficacy indicators such as SCORAD (RR, −10.20), BSA (RR, −2.01), surface damage score (RR, −2.25), VAS (RR, −1.90), sleep score (RR, −2.16), and IGA (RR, 2.94) improved to different degrees in the CHM group. These results indicate that Chinese medicine has better efficacy than placebo in many respects.
However, our systematic evaluation showed that CHM did not improve the DLQI/CDLQI (RR, −0.47) or IgE (RR, −62.76) levels in patients with AD. A possible reason for the lack of improvement in quality of life following CHM treatment may be that the patients reported only mild to moderate eczema that did not significantly impact their lives and work. Moreover, basic management strategies, such as the application of moisturizing creams, may reduce pruritus to some extent (Huang, et al., 2019). Cell-mediated immunity is also involved in AD pathogenesis. However, only two articles reported IgE levels and high heterogeneity (I2 = 87) in this analysis. These results indicate that herbal medicines did not reduce IgE.
Some studies have shown that certain herbs have anti-inflammatory effects. For example, the alcoholic extract of Coix lacrymal-Jobi L. has been shown to reduce the cellular secretion of inflammatory factors IL-4, IL-6, and TNF-α, and inhibit allergic reactions by regulating the expression of the ERK signaling pathway (Chen, et al., 2010). The volatile oil of agrimony inhibits the NF-κB pathway and reduces the inflammatory response. Platycodon grandiflorus (Jacq.) A. DC. contains platycodon saponins, flavonoids, phenolic acids, and other chemicals with anti-inflammatory, antitumor, and other desirable pharmacological effects (Ting, 2017; Chen, et al., 2020). The exact mechanism of action of polyherbal preparations is unclear. This may explain the stochastic efficacy of herbal medicines in the regulation of the expression of inflammatory factors, and provides a marker for future new directions in the treatment of atopic dermatitis.
There was slightly higher in patients treated with CHM than in those treated with placebo. But no difference in the safety between the CHM and placebo groups in a new rash, upper respiratory tract infection, cough, gastrointestinal upsets, and diarrhea. Therefore, CHM can be safely used to treat AD.
This study has several limitations. First, sufficiently high-quality trials are limited. Moreover, even if a study showed that CHM is more effective than placebo, it was difficult to standardize the included trials in terms of drug composition, dose, and treatment course, which may have affected the validity of our results. Although we list the herbs that were used more than 3 times, it remains unclear which CHM or herbal combination should be used in the clinical setting.
5 Conclusion
In summary, CHM improved the size and severity of the skin lesions and sleep quality in patients with AD. All included studies reported adverse events. Comparing the adverse effects between the CHM and placebo groups, CHM was safe. However, CHM does not improve the quality of life or patients’ IgE levels.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
XC and XS designed the study. YZ, SH, and JW performed the literature search and data extraction. JC, CW, and MZ performed a quality evaluation of the included articles and data analysis. XC and NL drafted the original manuscript, and RX and XL contributed to the manuscript revision. All the authors have read and approved the final manuscript.
Funding
National Natural Science Foundation of China (grant nos. 81874470 and 82074427), National Key Research and Development Program of China (grant no. 2018YFC1705302), Xinglin Scholar, Shanghai University of Traditional Chinese Medicine (No. RY411.14.12), Shanghai Pujiang Talent Program (No. 2020PJD067), Science and Technology Commission of Shanghai Municipality (Nos. 21Y21920100, 21Y21920102), and Shanghai Municipal Commission of Economy and Information Technology (No. 2020-RGZN-02038).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.927304/full#supplementary-material
Abbreviations
AD, Atopic Dermatitis; AEs, adverse events; BSA, body surface area; CDQLI, Children’s Dermatology Life Quality Index; CHM, Chinese herbal medicine; CNKI, China national knowledge infrastructure; CI, confidence intervals; DLQI, Dermatology Life Quality Index; EASI, Eczema Area and Severity Index; EASI 50/75/90, EASI score decreases more than 50%/75%/90% from baseline; HD, High dose; IGA, Investigator’s Global Assessment; IGA 1/IGA 2, Investigator’s Global Assessment decreased by 1/2 point; IL-4, interleukin-4; IL-13, interleukin-13; IL-31, interleukin-31; LD, Low dose; MD, mean difference; MTX, methotrexate; PRISMA, Preferred Reporting Items for Systematic Review and Meta-Analysis; RCTs, randomized control trials; RR, Risk ratios; SCORAD, Scoring Atopic Dermatitis; SD: Standard Deviation; SMD, standard mean difference; TH1, T helper type 1 cells; TH2, T helper type 2 cells; TSLP, Thymic Stromal Lymphopoietin; VAS, visual analog scale.
References
Berke, R., Singh, A., and Guralnick, M. (2012). Atopic dermatitis: An overview. Am. Fam. Physician 86 (1), 35–42.
Cao, H., Yang, G., Wang, Y., Liu, J. P., Smith, C. A., Luo, H., et al. (2015). Complementary therapies for acne vulgaris. Cochrane Database Syst. Rev. 1, CD009436. doi:10.1002/14651858.CD009436.pub2
Chen, D. D., Hong, T., Wang, D., and Yang, Y. S. (2020). Overview of research on chemical composition and its pharmacological effects of Platycodon grandifloras. Drug Eval. 17 (15), 9–11.
Chen, H. J., Shih, C. K., Hsu, H. Y., and Chiang, W. (2010). Mast cell-dependent allergic responses are inhibited by ethanolic extract of adlay (Coix lachryma-jobi L. var. ma-yuen Stapf) testa. J. Agric. Food Chem. 58 (4), 2596–2601. doi:10.1021/jf904356q
Cheng, H. M., Chiang, L. C., Jan, Y. M., Chen, G. W., and Li, T. C. (2011). The efficacy and safety of a Chinese herbal product (Xiao-Feng-San) for the treatment of refractory atopic dermatitis: A randomized, double-blind, placebo-controlled trial. Int. Arch. Allergy Immunol. 155 (2), 141–148. doi:10.1159/000318861
Czarnowicki, T., He, H., Krueger, J. G., and Guttman-Yassky, E. (2019). Atopic dermatitis endotypes and implications for targeted therapeutics. J. Allergy Clin. Immunol. 143 (1), 1–11. doi:10.1016/j.jaci.2018.10.032
Damour, A., Garcia, M., Seneschal, J., Lévêque, N., and Bodet, C. (2020). Eczema herpeticum: Clinical and pathophysiological aspects. Clin. Rev. Allergy Immunol. 59 (1), 1–18. doi:10.1007/s12016-019-08768-3
Furue, M., Chiba, T., Tsuji, G., Ulzii, D., Kido-Nakahara, M., Nakahara, T., et al. (2017). Atopic dermatitis: Immune deviation, barrier dysfunction, IgE autoreactivity, and new therapies. Allergol. Int. 66 (3), 398–403. doi:10.1016/j.alit.2016.12.002
Gholyaf, M., Sheikh, V., Yasrebifar, F., Mohammadi, Y., Mirjalili, M., and Mehrpooya, M. (2020). Effect of mirtazapine on pruritus in patients on hemodialysis: A cross-over pilot study. Int. Urol. Nephrol. 52 (6), 1155–1165. doi:10.1007/s11255-020-02473-3
Gu, S. X., Mo, X., Zhang, A. L., Liu, J., Coyle, M. E., Ye, S., et al. (2018). A Chinese herbal medicine preparation (pei tu qing xin) for children with moderate-to-severe atopic eczema: A pilot randomized controlled trial. Br. J. Dermatol. 179 (6), 1404–1405. doi:10.1111/bjd.16988
Gu, S., Yang, A. W., Xue, C. C., Li, C. G., Pang, C., Zhang, W., et al. (2013). Chinese herbal medicine for atopic eczema. Cochrane Database Syst. Rev. (9), CD008642. doi:10.1002/14651858.CD008642.pub2
Hon, K. L., Leung, T. F., Ng, P. C., Lam, M. C., Kam, W. Y., Wong, K. Y., et al. (2007). Efficacy and tolerability of a Chinese herbal medicine concoction for treatment of atopic dermatitis: A randomized, double-blind, placebo-controlled study. Br. J. Dermatol. 157 (2), 357–363. doi:10.1111/j.1365-2133.2007.07941.x
Huang, D., Chen, K., Zhang, F. R., Yang, S., Guo, Q., Xu, J. H., et al. (2019). Efficacy and safety of run zao zhi yang capsule on chronic eczema: A multiple-center, randomized, double-blind, placebo-controlled clinical study. J. Dermatol. Treat. 30 (7), 677–684. doi:10.1080/09546634.2019.1571267
Huang, H., Lu, Z., Jiang, C., Liu, J., Wang, Y., and Xu, Z. (2013). Imbalance between Th17 and regulatory T-Cells in sarcoidosis. Int. J. Mol. Sci. 14 (11), 21463–21473. doi:10.3390/ijms141121463
Jadad, A. R., Moore, R. A., Carroll, D., Jenkinson, C., Reynolds, D. J., Gavaghan, D. J., et al. (1996). Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 17 (1), 1–12. doi:10.1016/0197-2456(95)00134-4
Lacouture, M., and Sibaud, V. (2018). Toxic side effects of targeted therapies and immunotherapies affecting the skin, oral mucosa, hair, and nails. Am. J. Clin. Dermatol. 19 (1), 31–39. doi:10.1007/s40257-018-0384-3
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 339, b2700. doi:10.1136/bmj.b2700
Lin, H., Li, Z., and Peng, J. (2019). New progress in the treatment of atopic dermatitis with traditional Chinese medicine. J. Liaoning Univ. Tradit. Chi. Med (11), 29–32.
Lin, Y. K., Chang, S. H., Yang, C. Y., See, L. C., Lee, B. H., and Shih, I. H. (2020). Efficacy and safety of indigo naturalis ointment in treating atopic dermatitis: A randomized clinical trial. J. Ethnopharmacol. 250, 112477. doi:10.1016/j.jep.2019.112477
Liu, M. Q. (2021). Clinical effect of shenlingbaizhu powder on spleen deficiency type Atopic dermatitis and its influence on intestinal floraeczema. Jiangxi Univ. Chin. Med.
Luo, Y., Chen, J., Kuai, L., Zhang, Y., Ding, X., Luo, Y., et al. (2021). Chinese herbal medicine for psoriasis: Evidence from 11 high-quality randomized controlled trials. Front. Pharmacol. 11, 599433. doi:10.3389/fphar.2020.599433
Nutten, S. (2015). Atopic dermatitis: Global epidemiology and risk factors. Ann. Nutr. Metab. 66 (1), 8–16. doi:10.1159/000370220
Ronchetti, S., Ayroldi, E., Ricci, E., Gentili, M., Migliorati, G., and Riccardi, C. (2021). A glance at the use of glucocorticoids in rare inflammatory and autoimmune diseases: Still an indispensable pharmacological tool? Front. Immunol. 11, 613435. doi:10.3389/fimmu.2020.613435
Sun, X. D. (2009). Evaluation of the efficacy of Jian spleen and dampness granules in the treatment of atopic dermatitis and its effect on recurrence. Chin. J. integr. Dermatolo. Venereolo. 8 (06), 335–337.
Sybilski, A. J., Raciborski, F., Lipiec, A., Tomaszewska, A., Lusawa, A., Samel-Kowalik, P., et al. (2015). Epidemiology of atopic dermatitis in Poland according to the Epidemiology of Allergic Disorders in Poland (ECAP) study. J. Dermatol. 42 (2), 140–147. doi:10.1111/1346-8138.12731
Tan, H. Y., Zhang, A. L., Chen, D., Xue, C. C., and Lenon, G. B. (2013). Chinese herbal medicine for atopic dermatitis: A systematic review. J. Am. Acad. Dermatol. 69 (2), 295–304. doi:10.1016/j.jaad.2013.01.019
Tian, X. Y. (2019). Clinical observation and mechanism of action of the formula of strengthening the spleen and helping transportation in the treatment of pediatric atopic dermatitis. Beijing Univ. Tradit. Chin. Med.
Ting, Z. (2017). Effects and mechanisms of volatile oil of amomi fructus on drug-induced intestinal mucositis. Yunnan college of tradit. Chin. Med.
Wilson, S. R., Thé, L., Batia, L. M., Katibah, G. E., McClain, S. P., Pellegrino, M., et al. (2013). The epithelial cell-derived atopic dermatitis cytokine TSLP activates neurons to induce itch. Cell 155 (2), 285–295. doi:10.1016/j.cell.2013.08.057
Keywords: Chinese herbal medicine, atopic dermatitis, randomized controlled trials, safety, efficacy
Citation: Cai X, Sun X, Liu L, Zhou Y, Hong S, Wang J, Chen J, Zhang M, Wang C, Lin N, Li S, Xu R and Li X (2022) Efficacy and safety of Chinese herbal medicine for atopic dermatitis: Evidence from eight high-quality randomized placebo-controlled trials. Front. Pharmacol. 13:927304. doi: 10.3389/fphar.2022.927304
Received: 24 April 2022; Accepted: 29 August 2022;
Published: 27 September 2022.
Edited by:
Anna Rita Bilia, University of Florence, ItalyReviewed by:
Jianping Liu, Beijing University of Chinese Medicine, ChinaBojun Chen, Guangzhou University of Chinese Medicine, China
Copyright © 2022 Cai, Sun, Liu, Zhou, Hong, Wang, Chen, Zhang, Wang, Lin, Li, Xu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rong Xu, bWFycnl4dTc3QDE2My5jb20=; Xin Li, MTM2NjE5NTYzMjZAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Xiaoce Cai
Xiaoce Cai Xiaoying Sun
Xiaoying Sun Liu Liu
Liu Liu Yaqiong Zhou
Yaqiong Zhou Seokgyeong Hong
Seokgyeong Hong Jiao Wang
Jiao Wang Jiale Chen
Jiale Chen Miao Zhang
Miao Zhang Chunxiao Wang
Chunxiao Wang Naixuan Lin
Naixuan Lin Su Li
Su Li Rong Xu
Rong Xu Xin Li
Xin Li