- 1Black Dog Institute, Prince of Wales Hospital, Sydney, NSW, Australia
- 2Faculty of Medicine, University of New South Wales, Sydney, NSW, Australia
Background: Schools play an important role in supporting young people’s mental health, but face challenges identifying and responding to students in need of care. To assist secondary schools, the Black Dog Institute has developed an online, school-based, mental health service (Smooth Sailing). Delivered in the classroom, Smooth Sailing uses a website to screen, assess, allocate, and deliver care for depression and anxiety. The service is based on the principles of stepped care, offering treatments with varied intensity and follow-up by a school counselor when necessary. The current study aimed to evaluate the feasibility, acceptability, and safety of this new type of service among secondary school students.
Methods: Between February and June 2017, a single-arm, pre-post, pilot study was conducted among students from four NSW secondary schools. Schools were given access to the service for 6 weeks. Feasibility measures (consent rates and step allocations), acceptability measures (service use and satisfaction) and safety measures (deterioration in help-seeking intention scores and mental health symptoms) were assessed at baseline and completion of the 6-week trial period.
Results: A total of 59 students took part in the service pilot (mean age, 14.57 years; SD, 0.89 years; range, 13-16 years). At baseline, 18.64% of students were found to require follow-up from the school counselor, and 80% of these were new cases. Although completion of the online modules was low, service satisfaction was high. At 6 weeks, the mean scores for help-seeking, depression, and anxiety remained relatively stable or improved.
Conclusions: The current study presents important findings for the development and implementation of an online mental health service that screens students’ mental health and allocates care accordingly, all within the school setting. Although the findings provide some support for the feasibility, acceptability, and safety, service improvements are needed. The modifications outlined are likely to improve the quality of the service and its effectiveness.
Trial Registration: Australian New Zealand Clinical Trials Registry (ANZCTR):
ACTRN12617000977370
Introduction
Given that half of all mental disorders emerge between the ages of 12 and 18 years (1), secondary schools play an important role in supporting the mental health of young people. Delivering mental health services in schools has the potential to address barriers to care, including accessibility, costs, and stigma (2). Many secondary schools employ counselors or psychologists to address student mental health, but up to one third report that their workload is unmanageable (3). A meta-analysis of face-to-face mental health services delivered to students found that targeted, selective, and universal programs were all effective for reducing mental health problems among students (4). Other initiatives, such as classroom-based online cognitive behavioral therapy (5–7) and curriculum-embedded mental health content (8) were also effective for improving symptoms and mental health literacy. However, wide-scale uptake is challenged by low levels of awareness of the effective mental health programs, competing priorities, time constraints, and limited resources (9). Despite the potential, schools remain underutilized, under resourced, and lack the capacity to appropriately manage students’ mental health needs.
Stepped care has been proposed as a service model for the treatment of depression and anxiety (10) that may increase engagement with care, reduce symptoms, and allow for better distribution of resources (11). Stepped care is considered well suited to depression and anxiety as these disorders are highly prevalent, have varied degrees of severity, are responsive to light-touch interventions, and the shortage of trained clinicians and specialist services hinders access to face-to-face care (12). Although there is no consistent definition of stepped care, it typically involves a process of screening and assessment to determine individuals’ symptoms and treatment needs (13). In some models, initial treatment is matched to the severity of symptoms whereas in others, all individuals begin at the same “step” of intervention, regardless of symptom severity. Individuals who fail to respond to their allocated treatment in the set time are then stepped up to the subsequent level of care (14). Most models do not incorporate stepping down. In accordance with clinical guidelines (15), stepped care for depression may involve several components including psychoeducation, self-directed online therapy, individual face-to-face therapy, medication, and monitoring. It has been argued that when fully realized, stepped care could maximize clinical outcomes while minimizing provider costs (13).
While the cost-effectiveness of stepped care has been supported (16–18), there is only emerging evidence of treatment effectiveness. A meta-analysis of 10 randomized trials among depressed adults found moderate treatment effects for stepped care, but limited evidence to support its use as the dominant treatment model (19). In a review of primary care trials, stepped care for depression was found to be as effective as treatment as usual (20); however, its clinical superiority was undetermined. Few formal evaluations of stepped care have been conducted among youth. When comparing standard care to stepped care for the treatment of clinical anxiety, no significant difference in symptom reduction was found (17). In contrast, young adults living with HIV who received stepped care for depression had significantly greater improvements in symptoms compared to those receiving treatment as usual (21). This is consistent with Mufson et al. (22) who found stepped care to be more effective for reducing depression among adolescents in primary care when compared to treatment-as-usual. This suggests that the superiority of stepped care may be dependent on the degree of intervention provided by the treatment comparator. As such, stepped care may be ideal for school settings where treatment as usual is minimal.
In Australia and other high-income countries, most schools operate on a wait-to-act model in which school staff instigate referral to mental health support only after observing certain behaviors or students’ self-disclosures (23). As help-seeking is low among youth, and teachers are not always trained to identify those in need (24), a proactive model like stepped care which detects symptoms and stratifies care accordingly may assist schools in caring for students. Components of stepped care have already been implemented in schools with some success. School based screening has been found to identify a significantly greater proportion of students to be in need of mental health services than would have been identified without screening (25). School based screening has also resulted in increased rates of referral, improved help-seeking behavior, and greater access to services for students (26). Australian schools are well-placed to provide professional follow-up due to the availability and employment of school counselors and school psychologists. Although other components of stepped care, such as triage and brief intervention, have been tested in school settings with promising results (27), it remains unknown whether Australian schools have the capacity to integrate a stepped care model for depression and anxiety. Given the emergence of mental illness in adolescence, the low levels of help-seeking, and limited school resources, evaluating stepped care and its promise is timely.
The Smooth Sailing Service
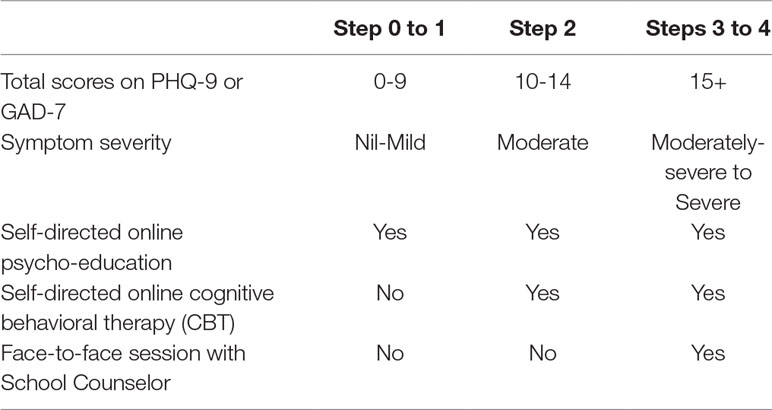
The Black Dog Institute has developed an online, schools-based, mental health service called Smooth Sailing. Based on the principles of stepped care, Smooth Sailing uses a website to screen, assess, allocate, and deliver psychological interventions to improve help-seeking for mental health problems and reduce depressive and anxiety symptoms among secondary school youth. Brief, validated, self-report measures of depression and anxiety (28, 29) are used to accurately determine students’ symptoms and required level of care. The service has three degrees of treatment intensity which are matched to students’ initial symptom severity categorization (i.e. nil-mild, moderate, moderately severe to severe). The model is consistent with Australian Clinical Practice Guidelines (30) and conservative due to the novelty of the service. Self-directed, web-based, psycho-education is provided for students with nil to mild symptoms. Self-directed, web-based, cognitive behavioral therapy (CBT) is provided for students with moderate symptoms (5, 7). A direct link to face-to-face care with a school counselor is provided for students with moderately severe to severe symptoms or thoughts of death/harming one’s self. School counselors are instructed to provide their usual care, consistent with school guidelines and policies. Students’ symptoms are monitored fortnightly by an email or SMS check-in, which also includes a reminder to use the service and an automated login link. Every 6 weeks, students complete a step assessment from which care is reallocated based on their results.
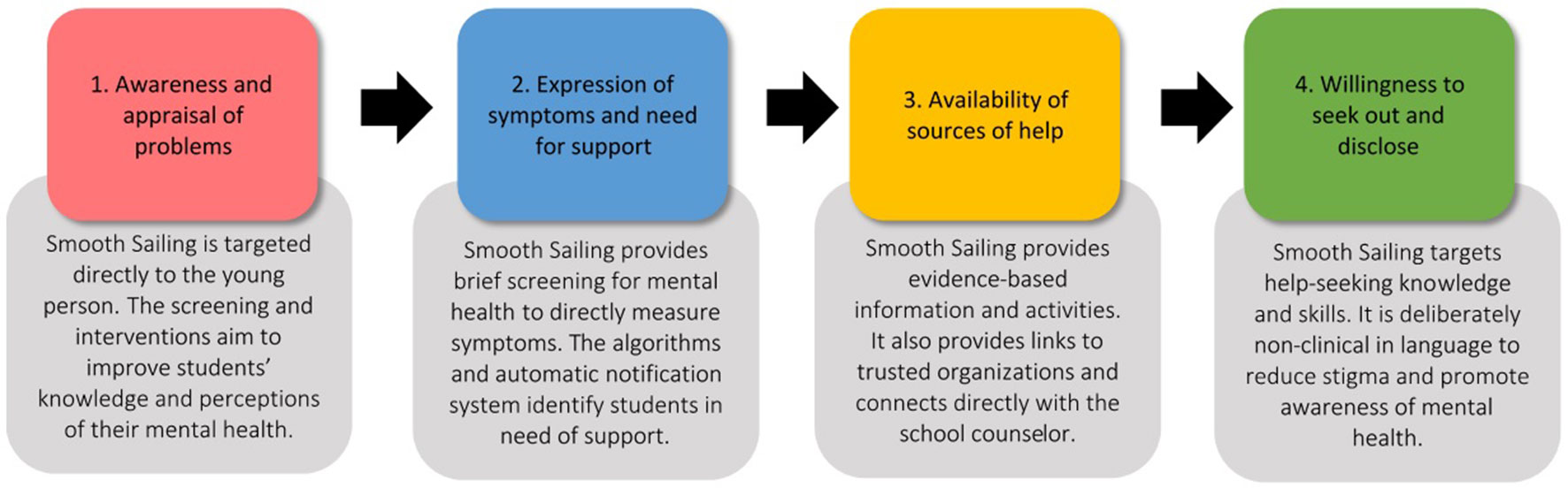
The Smooth Sailing service is based on Rickwood et al. (31) help-seeking model. As outlined in Figure 1, Smooth Sailing directly targets each of the stages of help seeking through varied content and features. Smooth Sailing utilizes the Internet to address resource shortages and provide young people with evidence-based information and resources (32, 33). A major strength of the current service is that it links directly to face-to-face care, improving the likelihood of actual and future help-seeking (34).
The Smooth Sailing service was designed in partnership with students, school counselors (3), teachers, General Practitioners (GPs; 35), and parents (36). These stakeholders strongly endorsed the service due to perceptions of its usefulness in detecting symptoms and providing care, the suitability of the school setting for reaching youth, and young people’s preferences for digital technology. However, key concerns also emerged including the privacy and confidentiality of students’ information, Internet accessibility, and the availability of face-to-face care. School counselors felt students may try to avoid follow-up by answering the screening questions dishonestly and that students may forget or lack motivation to complete the online modules. School staff felt that gaining parental consent would be a potential barrier, although conversely, parents endorsed the service due to the prevalence and impacts of poor mental health among youth. While these concerns have been raised in similar studies of school-based computerized programs for mental health (37–41), broad uptake and successful implementation of the service is unlikely unless issues related to feasibility and acceptability are addressed.
Aims
The current study aimed to evaluate the feasibility, acceptability, and safety of the Smooth Sailing service among secondary school students. Feasibility was determined by the willingness of students to take part and the capacity of school counselors to initiate and manage follow-ups. Acceptability was determined by the extent to which students used the service, barriers to service use, and students’ perceptions of service satisfaction (42, 43). The safety profile of the service was determined based on the deterioration in students’ help-seeking intentions and symptoms after using the service. Although the study was not powered to detect significance (44, 45), measuring the change in these scores determined whether the service was likely to have an effect in an appropriately powered trial. The current study enabled service improvements to be defined and actioned, including important resource considerations. It also provided the initial data needed to develop future trial protocols, including sample size calculations and recruitment targets. Given the limited number of studies on school-based mental health services, and the lack of evaluation of stepped care for adolescent mental health, the current pilot may help researchers and clinicians to design more effective and integrative school-based service models.
Method
Study Design
A single-arm, pre-post, 6-week uncontrolled pilot trial was conducted. The study was approved by UNSW Human Research Ethics Committee (#167424), the NSW State Education Research Application Process (#2016471), and the necessary Catholic Education Offices. The study was undertaken in NSW, Australia, between February and June 2017. The recruitment target was set at a minimum of 50 students in total from 4 schools. This target was based on recommendations for pilot research (46, 47) and was conservative to minimize the number of notifications and potential overburden on the participating school counselors. A convenience sample of schools who had expressed interest in the service during the design phase was used. School principals were emailed an information letter inviting the school counselor and two class groups from each school to participate. For school consent, schools were asked to provide a signed letter of support from the school principal. This letter was then forwarded to the governing ethics bodies to confirm school participation. Upon receipt of the signed school letter of support, student information and consent forms were mailed to each school. These forms were then distributed to the selected class groups by school staff. Interested students were required to return their consent form with signed parental consent by the day of the first school researcher visit. There were no other exclusion criteria. The study information sheet and consent form informed the students that taking part was completely voluntary, and that they were free to withdraw from the study at any time, without penalty, and without having to give a reason. Students could withdraw by emailing the research team or notifying the researchers at the school visits. Parents could also withdraw their child at any time using the same methods or by contacting their child’s school.
Implementing the Service
At baseline, researchers visited the school to deliver the service in class time. Researchers reviewed students’ consent forms and provided them with instructions to register to the service. Registration involved visiting the service website (https://smoothsailing.blackdoghealth.org.au) and completing an online Gillick Competency measure—six multiple choice questions to test students’ capacity to provide informed consent and their understanding of the service. During registration, students provided their name, study code, email, mobile phone number, gender, and date of birth. They were asked to report their current employment status (part-time/casual, nil), whether they identified as lesbian, gay, bisexual, trans, or intersex (LGBTI) (answered yes, no, I’d rather not say) or as Aboriginal or Torres Strait Islander (ATSI) (answered yes, no, I’d rather not say). They were also asked to report whether they knew someone with a mental illness; cared for someone with a mental illness; had a mental illness themselves; or had used the Internet to find information about a mental health problem (all answered yes, no). This information was collected to determine the demographics of the sample alongside their experience and exposure to mental health problems.
The self-report mental health screener consisted of two validated measures: the nine-item Patient Health Questionnaire (PHQ-9; 28) for depressive symptoms and the seven-item self-report Generalized Anxiety Disorder Scale (GAD-7; 29) for generalized anxiety symptoms. Each of these questionnaires listed symptoms, and students were asked to rate how frequently they had experienced these, in the past 2 weeks, using a four-point Likert scale ranging from not at all (0) to nearly every day (4). The service automatically calculated a total score for each scale. Using whichever total score was the highest, students’ symptoms were classified as “nil-mild” (i.e. total score on PHQ-9 or GAD-7 equaling 0-9), “moderate” (i.e., total score of PHQ-9 or GAD-7 between 10 and 14), or “moderately severe to severe” (i.e., total score of PHQ-9 or GAD-7 between 15 and 27). To measure the impact of their symptoms on overall functioning, one additional item asked students to rate how difficult their symptoms had made their daily life and relationships. Participants answered using a four-point Likert scale ranging from not at all (0) to very (4).
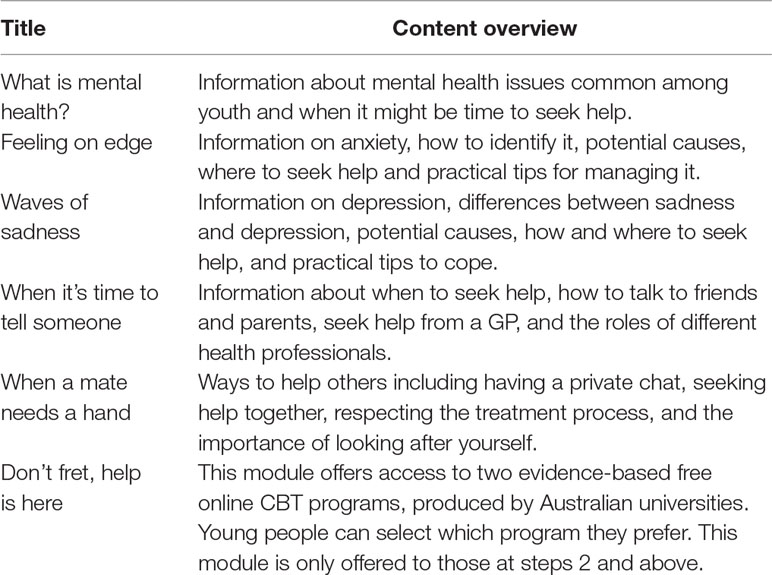
After completing the screener, the service automatically allocated students to a step of care that matched their symptom severity (see Table 1). The Smooth Sailing service produced a personalized dashboard which provided students with an overview of the recommended modules to complete in their own time (see Table 2). The online psycho-education consisted of five 10-minute modules which provided information about anxiety, depression, and help-seeking. The modules were created specifically for the Smooth Sailing service and were reviewed in the co-design process by young people as well as a clinical psychologist. The content was also edited by a copywriter to ensure it was written at an appropriate reading level. The modules are complemented by animations and illustrations as well as hyperlinks to other credible youth mental health services and websites. All modules are designed to be self-directed, self-paced, and can be completed in any order. Module 6 includes referral to two web-based, publicly available, free, evidence-based CBT programs for depression and anxiety (5, 48, 49). MoodGym (5) comprises of five modules in which young people learn strategies to identify and manage unhelpful patterns of thinking, connect their thoughts and feelings, improve self-esteem and interpersonal relationships, and relaxation exercises to de-stress. The BRAVE Program (48, 49) includes ten 1-hour self-directed sessions that are usually completed over 10 weeks, that teach young people to identify anxiety and stress, develop relaxation and problem-solving skills, and reframe negative thinking. Before ending the visit, researchers advised students to use the website as much as they wished for the next 6 weeks.
Students who were allocated to steps 3 and 4 (i.e. moderately severe to severe symptoms) and/or reported thoughts of that they would be better off dead or of harming themselves in the past two weeks (i.e. score ≥ 1 on item-9 of the PHQ-9) automatically triggered a notification to the school counselor for follow-up through a secure, deidentified, email. Using the study ID codes, this email outlined that a student required follow-up from the school counselor within two days. School counselors were provided with a paper list of student names and matching study ID codes to ensure follow-up could be facilitated. The screening was only conducted on days when the school counselors were onsite. After conducting the student session, researchers met with the school counselor to review the email notifications. This took no more than 30 minutes. School counselors were provided with a list of local mental health services to support their follow-up. Two days after the school visit, the research team contacted the school counselor to confirm that all students had been followed up and to monitor any adverse events. This procedure was repeated at 6 weeks. All data were collected via the Smooth Sailing service e-platform which is hosted on university servers at the Black Dog Institute, University of New South Wales, Sydney, Australia.
Outcome Measures
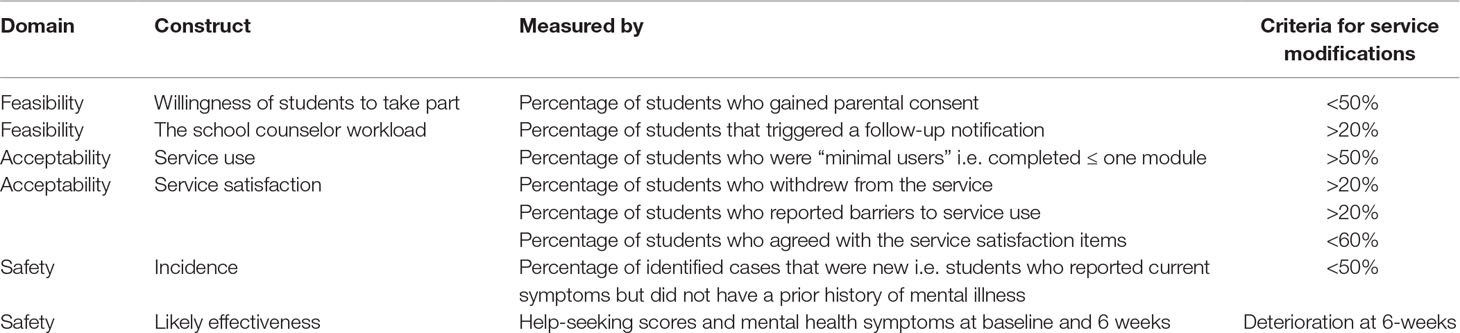
Table 3 presents the key outcome measures and the criterion used to determine whether service modifications and improvements to procedure were needed.
Feasibility
Consent rate: This was measured by the percentage of students who gained parental consent to participate and determined the likelihood of service uptake among students. The service was deemed feasible if >50% of invited students took part, based on the uptake of previous Australian school-based mental health programs (50, 51). Non-consenting students were asked to complete a short anonymous questionnaire outlining their reasons and to indicate whether an incentive would encourage participation.
Step allocations and follow-up notifications: This was the percentage of students who were allocated to each step and the percentage who required follow-up from the school counselor. This was measured to provide an estimate of the prevalence of mental health issues among students and the capacity required of school counselors. Based on prior recommendations for school-based screening, the service was deemed feasible if no more than 20% of students triggered a follow-up notification (52).
Acceptability
Service use: Based on a recent review of uptake and use of digital health interventions (53), service modifications were needed if the majority of students (>50%) were minimal users (i.e. completed one or less of the prescribed modules).
Barriers to service use: Service barriers were identified using an 18-item list delivered at 6-weeks. Students were asked to report whether they experienced any of the listed service barriers throughout the pilot (e.g. “I forgot how to access Smooth Sailing,” answered yes or no). If >20% of students reported experiencing the same barrier, service modifications were needed.
Service satisfaction: Satisfaction was measured using service dropout - the percentage of students who withdrew from the service throughout the pilot period. Based on dropout rates for mental health treatment, service modifications were needed if dropout was >20% (54). Satisfaction was also measured using students’ responses to an 11-item questionnaire delivered at 6 weeks. Students were asked to agree or disagree with a list of statements about the service (e.g. “Smooth Sailing was easy to understand”). Service modifications were needed if <60% of students agreed with each of the statements.
Safety
Incidence: This was the number of new cases identified by the service i.e. the percentage of students who required follow-up but had no history of mental health problems or illness. Service modifications would be needed if <50% of the identified cases were new.
Likely effectiveness: This was determined based on the deterioration in help seeking and symptom scores at 6 weeks. Help-seeking intentions for mental health were assessed at baseline and 6 weeks using an adapted version of the General Attitudes to Help-Seeking Questionnaire (GHSQ; 55). Students were asked to rate how likely they were to seek help when faced with a mental health problem from 12 different sources including informal (e.g. parents, friends, other adults), formal (e.g. GP, mental health professional), school-based (e.g. teacher, school counselor), and technology (e.g. mental health websites, telephone helplines, Internet activities). Each item was answered using a 5-point scale ranging from “extremely unlikely’’ to “extremely likely.” Answers were summed to create a total score with higher scores indicating a greater likelihood of seeking help. As outlined, the service also measured students’ depression and anxiety symptoms at baseline and 6 weeks using the Patient Health Questionnaire (PHQ-9; 28) and the Generalized Anxiety Disorder Scale (GAD-7; 29). Higher scores indicated greater symptom severity.
Results
Feasibility
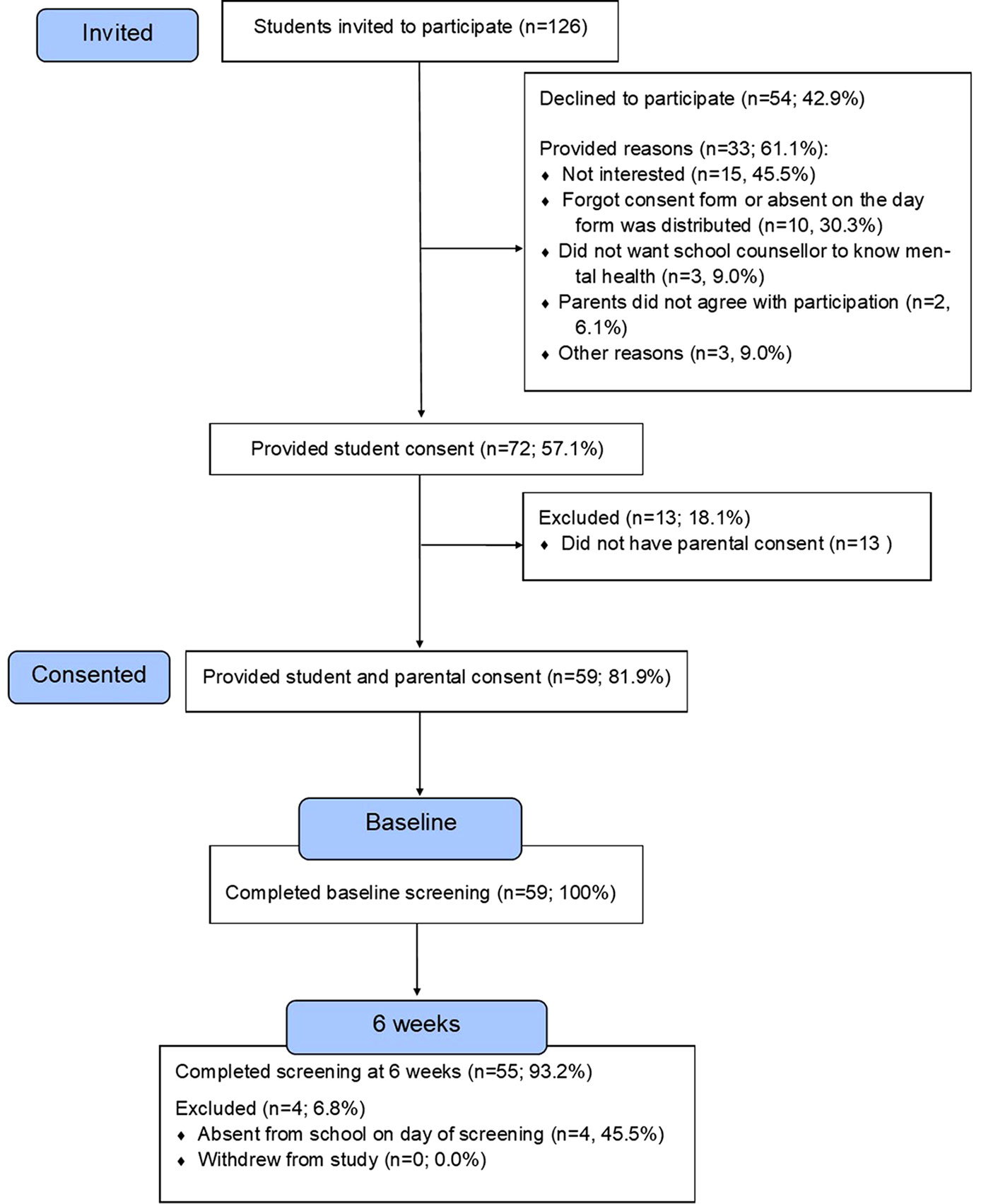
Consent rate:Figure 2 outlines the participant recruitment and flow.
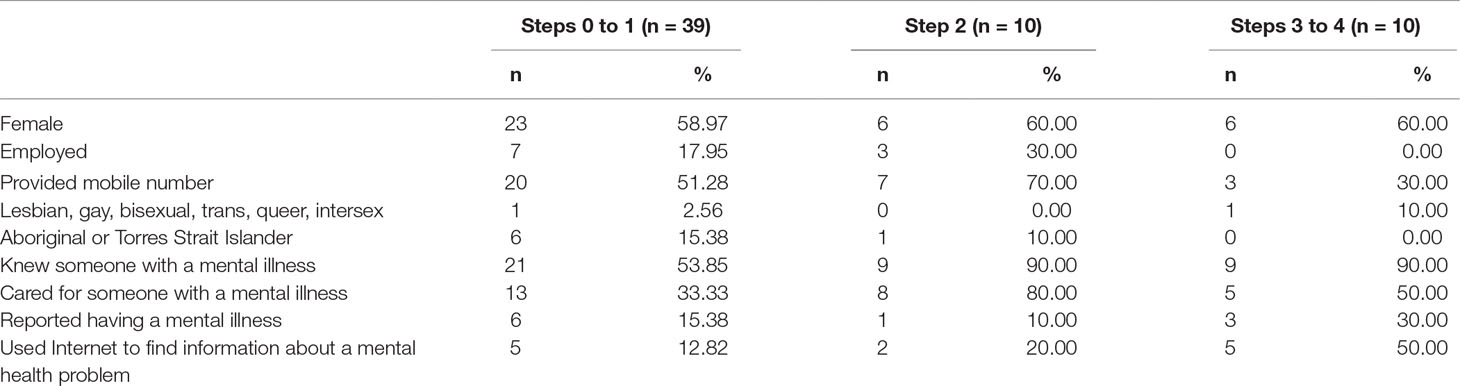
A total of 126 students from the 4 participating schools were invited to take part in the service and 72 provided their consent (57.14%, n = 72/126). Of these, 59 gained parental permission. This gave an overall consent rate of 46.83% (n = 59/126). A total of 33 non-consenting students completed the feedback form. Of these, half were male (n = 18/33, 54.54%) and over half reported feeling sad, worried, or stressed for more than two weeks at a time (54.54%, n = 18/33). Figure 2 outlines the reasons for non-participation. When asked about the use of an incentive for future participation, 24.24% (n = 8/33) said they would not participate regardless, 39.39% (n = 13/33) preferred a gift voucher, and 36.36% (n = 12/33) gave no response. Participant characteristics of the final sample are presented in Table 4, stratified according to baseline step allocation.
Step allocations and follow-up notifications: Displayed in Figure 3, two thirds (66.10%, n = 39) of the sample reported nil to mild symptoms at baseline and were allocated to steps 0 and 1; 16.94% (n = 10) reported moderate symptoms and were allocated to step 2; and a further 16.94% (n = 10) reported moderately severe to severe symptoms and were allocated to steps 3 and 4. A total of 18.64% of the sample (n = 11/59, 7 female) triggered a follow-up notification at baseline. There was a downward shift in symptom severity at 6-weeks with reductions in the number of students at the highest steps. However, there was no change in the total number of students who required follow-up at 6 weeks because five students with nil-mild symptoms reported thoughts of death and/or self-harm.
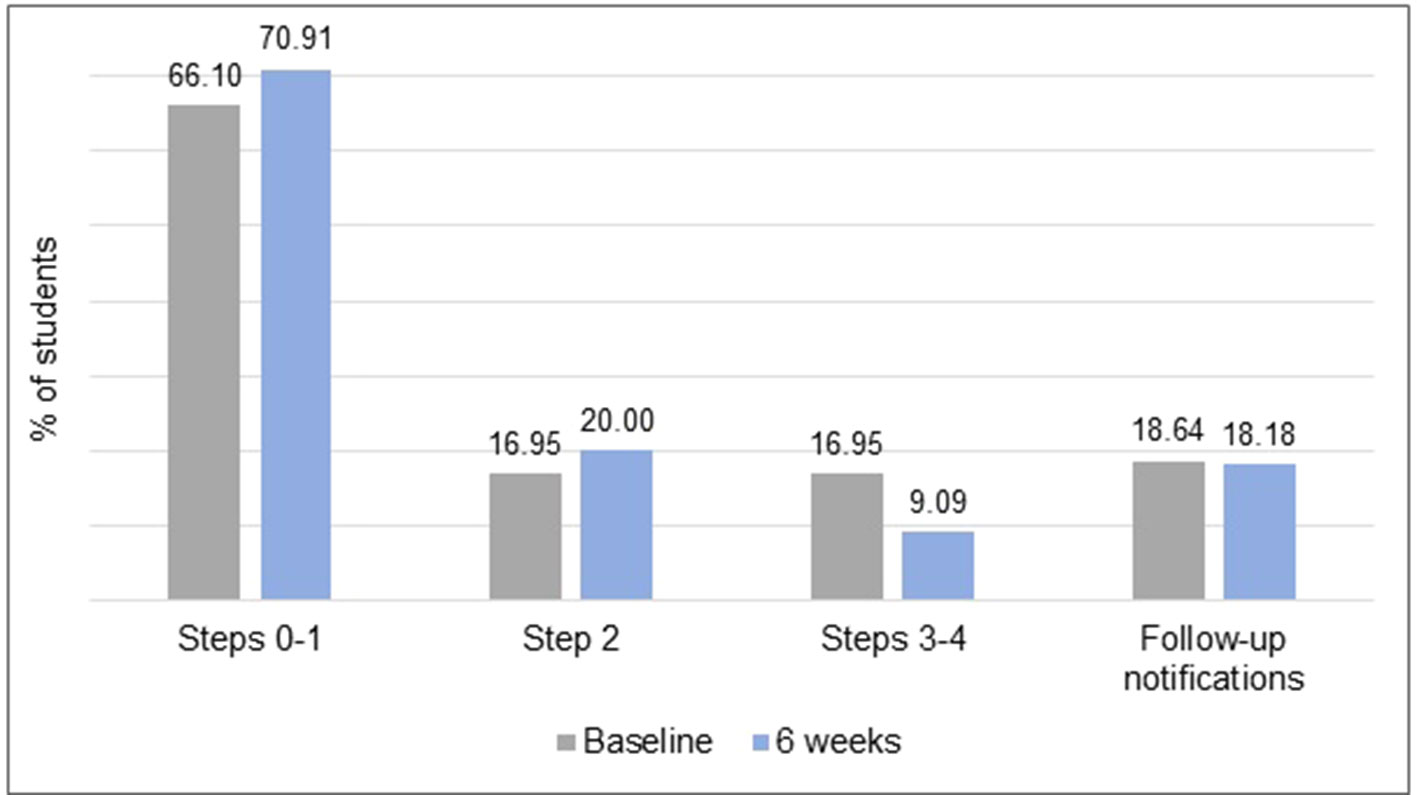
Figure 3 The frequencies of the step allocations and follow-up notifications at baseline and 6 weeks.
Acceptability
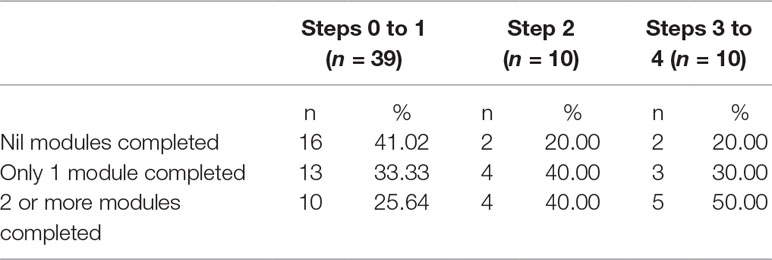
Service use: Although module completion was higher among the students with more severe symptoms at baseline, the majority were minimal users (range: 50.00-74.35%, see Table 5).
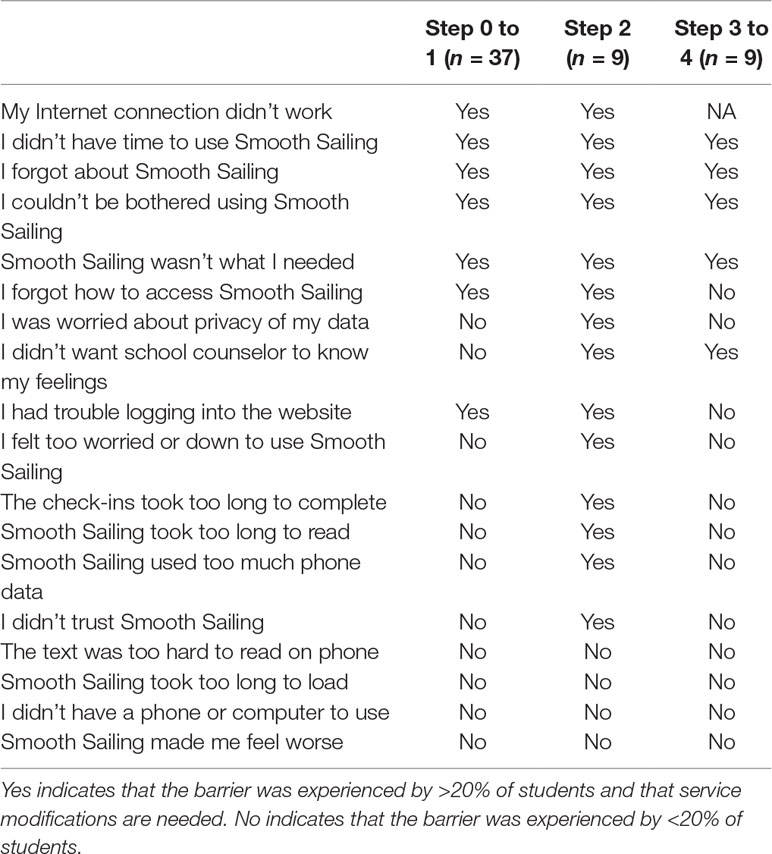
Barriers to service use: Outlined in Table 6, service barriers differed according to baseline step allocation. Students at step 2 experienced more barriers than others, reporting problems with Internet connectivity, lack of time, forgetfulness, low motivation, worry about the privacy of data, content taking too long to read and complete, using too much phone data, not trusting the service, feeling too worried or down to use the service, and not wanting the school counselor to know their feelings.
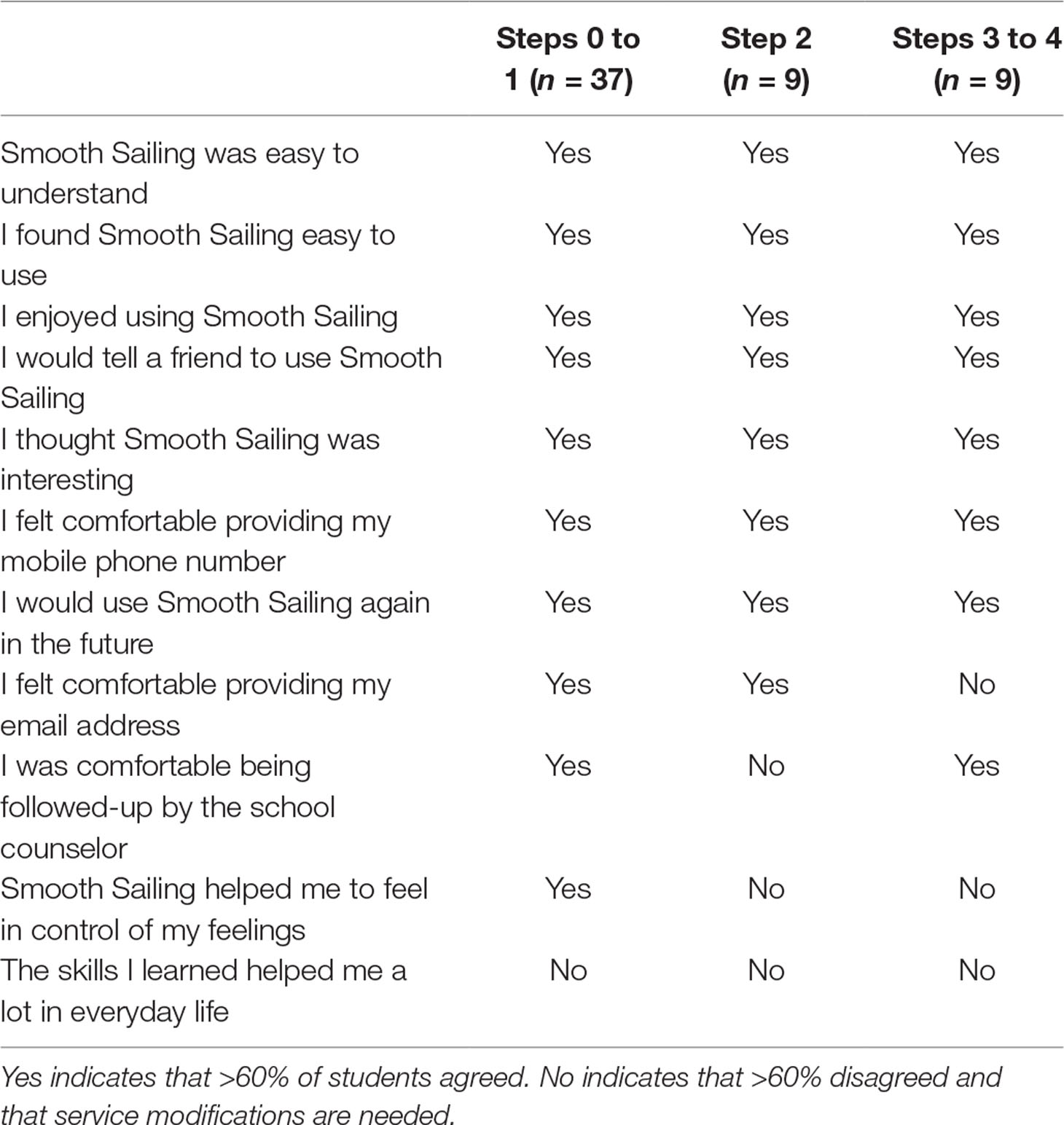
Service satisfaction: There were no active withdrawals during the service pilot and 55 of the 59 students were present for the 6-week assessment (93.22% retention). As outlined in Table 7, most of the students (range: 60–100%) felt that Smooth Sailing was easy to understand, easy to use, interesting and enjoyable, regardless of their baseline step allocation. The majority also felt comfortable providing their mobile phone number, agreed that they would tell a friend to use the service, and would use the service again in the future. The students allocated to steps 3 and 4 were comfortable with school counselor follow-up but less comfortable providing their email address. There was also disparity in students’ responses to whether Smooth sailing helped them “feel in control of their feelings” and “helped them a lot in everyday life,” with lower levels of agreeance among those allocated to the higher steps.
Safety
Incidence: Sixteen of the 20 (80%) students who required follow-up did not report a history of mental health problems or mental illness.
Likely effectiveness: The mean scores for help-seeking intentions, depression, and anxiety appeared stable or improved throughout the pilot, across all levels of symptom severity (see Table 8).
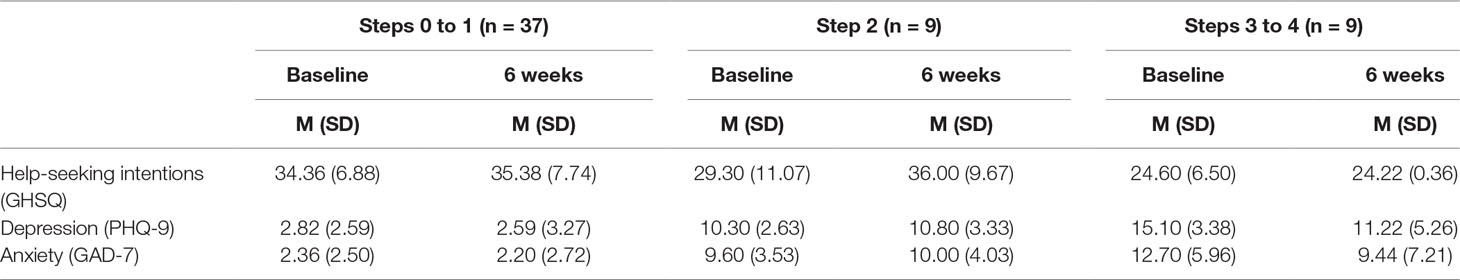
Table 8 Help-seeking intentions (GHSQ), depression (PHQ-9), and anxiety (GAD-7) scores at baseline and 6 weeks (N = 55).
Discussion
This study aimed to determine the feasibility, acceptability, and initial safety profile of an online mental health service for improving help seeking and mental health symptoms in NSW secondary school students. The findings revealed that some modifications to the service and its procedure are needed if a future controlled trial is to be successful.
Feasibility
Uptake of the service among students was low with less than half consenting to take part. Importantly however, the main barrier to consent appeared to be administrative: one quarter of the non-participating students had forgotten their consent forms and others were absent on the day forms were distributed. A more streamlined approach such as using passive “opt out” consent for parents and collecting student consent on the day of registration may improve uptake. This is likely to be supported by school communities as only a small proportion of parents did not want their child to participate in the service, although this would need to be evaluated further. Other strategies to increase uptake of the service among students may include broader promotion and marketing, utilizing school champions (56), increasing teacher awareness and support, and using incentives (57, 58). To better understand reasons for non-participation, future trials would benefit from implementing a consent form which all students are required to return, regardless of whether they choose to participate. This would allow more accurate rates of uptake to be measured and to better capture the reasons for non-participation. This is particularly important to address any concerns students have about using the service, the potential follow-up from the school counselor, and privacy protection.
This pilot also confirmed that the feasibility of the service is significantly impacted by the availability of school counselors to conduct the student follow-ups. In the initial screening, the service found that nearly one in four students experienced symptoms of depression and anxiety that warranted being seen by the school counselor. These rates are likely to increase the workload of school counselors. Based on the current study, school counselors would be required to initiate consultations with approximately 20% of all students screened. This has implications for delivering the service to larger samples, which would be needed for an effectiveness trial. In preparation for service implementation, schools would need to increase school counseling resources during the screening periods to ensure that all students requiring follow-up are seen in a timely manner. This would allay the concerns that students would not have access to face-to-face care if needed (3, 36). The service may lead to fewer follow-ups in the future; however, this would need to be investigated. Implementing the service over a longer period would enable researchers to evaluate the preventative and early intervention effects of the proposed stepped care model. As school counselors have already reported feeling time poor and vulnerable to burnout (3), future studies would need to monitor the impact of the increased workload on school counselors’ well-being and job stress.
Acceptability
There was no drop-out throughout the pilot, signifying the support for this type of service among the participating youth. However, service use was low with most students failing to complete more than one module. This is problematic, particularly for the students allocated to step 2 (i.e. moderate symptoms) as they were symptomatic but failed to engage with the therapeutic content. Students at step 2 also faced more barriers to service use, such as poor Internet connectivity, failure to remember passwords, and forgetfulness. Time constraints also impacted students’ use. Although email and SMS reminders were used, these did not appear to increase engagement. While SMS reminders are more likely than emails to be actioned (59), only half of the students chose to provide their mobile phone number. Service use may be improved by schools allocating class time for module completion as Neil et al. (60) found this resulted in a threefold increase. Other strategies could include publishing promotional material throughout the schools, inserting a web link to the Smooth Sailing service on schools’ websites and students’ desktops, introducing multiple options for restoring access and password retrieval (e.g. one-time pin codes, email verification links, use of secret questions) and utilizing student leaders to promote the service. A future trial may also benefit from using multi-modal methods of reminders including ones that are classroom-based, as well as customizable electronic reminders via SMS and email. Highlighting the brief time commitment required to work through the online modules may also increase module completion. Engagement is a challenge for many Internet programs and interventions, with the relationship between adherence and effect still unclear (61). However, as greater adherence can lead to stronger effects (62), modifications to the service may be necessary to increase acceptability and effectiveness.
Service satisfaction was high. Most students reported that they enjoyed using the service and found it easy to use. The online delivery mode may have contributed to this, with young people commonly reporting positive experiences with Internet activities for mental health (63). However, for stepped care models to be effective, participants need to be motivated and engaged with their allocated treatment (64, 65). The findings suggest that the current service model may need to be modified to include additional support or interaction, particularly for those at step 2 because motivation and capacity to engage with the self-directed content was low. This confirms school counselors’ prior concerns that symptomatic students may have difficulties engaging with this type of delivery (3). In studies among adults, adherence to online therapies has been greater when external support or guidance was provided (66). The current service model may be improved by the addition of human contact for youth allocated to step 2. Further, many students reported that the service was not what they needed, despite many having symptoms. Students’ lack of awareness of their mental health may have negatively impacted their engagement with the service. This is supported by Gould et al. (67) who found that students’ perceptions about their need for treatment impacted their service use. The service may benefit from improving the registration process to better educate students about its purpose and include symptom feedback to help students understand their needs. Providing more information about the effectiveness of e-mental health programs to students (68) and utilizing parents or peers for support (69) may help increase service use and satisfaction. In addition, redefining the expectations of students who have nil-minimal symptoms and implementing a curriculum-embedded mental health program (8) may help to supplement the online modules and increase overall acceptability.
Safety
A key question of this study was to establish the initial safety profile of a service which overtly identified students in need, provided care, and referred them to the school counselor when appropriate. The service was successful at detecting new cases of mental health problems, with four of five of the students identified not having a history of mental illness. Prior concerns about Internet-delivered screening and programs for school students have been related to them being untruthful or joking with their responses (3, 36). This study found no evidence of this behavior in students. On the contrary, it appeared that the service was perceived as trustworthy, encouraging honest disclosures of mental health history, symptoms, and help-seeking behavior. However, future studies would benefit from measuring the outcomes of student follow-ups, to determine whether the positively identified cases were genuine and whether referrals to other mental health services were made. The mean scores at baseline and 6 weeks suggested that the service did not worsen students’ intentions or symptoms, and positive significance may be found with a larger sample. Importantly, most students were comfortable being followed up by the school counselor, and even those who were not remained in the service. These findings provide some initial support for the effectiveness of the proposed model, but the low rates of module completion suggest improvements are needed before effects can be confirmed in a larger clinical trial. Future studies would benefit from increasing the sample size, using a control group, and implementing the service over a longer period. This would help determine genuine improvements in help-seeking behavior and symptoms.
Conclusion
The current study presents important findings for the development and implementation of an online mental health service that screens students’ mental health and allocates care accordingly, all within the school setting. Although the findings provide some support for the feasibility, acceptability, and safety, service improvements are needed. Modifying consent procedures, ensuring school counselor availability, improving completion of modules, and removing service barriers related to accessibility will significantly improve the quality of the service and its likely effectiveness. The current study confirms the potential of this new type of service model for identifying new cases of mental health problems in students, which may halt symptom progression and prevent the onset of serious mental illness. A randomized controlled trial comparing this service to school as usual would determine the genuine effects and benefits for students. Future studies should also examine the impact of the service on school counselors, school culture, and parents. This would help to understand the broader implications of this new type of service delivery model.
Ethics Statement
This study was carried out in accordance with the recommendations of the National Health and Medical Research Council's National Statement on Human Research with written informed consent from all subjects in accordance with the Declaration of Helsinki. The protocol was approved by UNSW Human Research Ethics Committee (#167424), the NSW State Education Research Application Process (#2016471), and the necessary Catholic Education Offices. Written consent was obtained from participants and their parents
Author Contributions
BO’D and HC conceived the study. BO’D prepared the protocol and initiated the trial. HC and NC approved protocol and supervised trial activities. BO’D, CK, and MS-K contributed to the coordination of the trial. BO’D and CK contributed to data analysis. BO’D led the authorship of the paper alongside all co-authors. MA completed formatting and referencing. All authors read and approved the final manuscript.
Funding
This project was funded by Hong Kong and Shanghai Banking Corporation (HSBC) and the Graf Family Foundation.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
(CBT), Cognitive Behavioral Therapy; (PHQ-9), Patient Health Questionnaire-9; (GAD-7), Generalized Anxiety Disorder 7-item; (UNSW), University of New South Wales; (GHSQ), General Attitudes to Help-Seeking Questionnaire; (AHSQ), Actual Help-Seeking Questionnaire; (LGBTI), Lesbian, Gay, Bisexual, Transsexual or Intersex; (ATSI), Aboriginal and Torres Strait Islander.
Acknowledgments
Sam Scopelliti developed the Smooth Sailing images.
References
1. Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry (2007) 20:359. doi: 10.1097/YCO.0b013e32816ebc8c
2. Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry (2010) 10:113. doi: 10.1186/1471-244X-10-113
3. O’Dea B, King C, Subotic-Kerry M, O’Moore K, Christensen H. School counselors’ perspectives of a web-based stepped care mental health service for schools: cross-sectional online survey. J Med Internet Res – Ment Health (2017) 4:e55. doi: 10.2196/mental.8369
4. Sanchez AL, Cornacchio D, Poznanski B, Golik AM, Chou T, Comer JS. The effectiveness of school-based mental health services for elementary-aged children: a meta-analysis. J Am Acad Child Adolesc Psychiatry (2018) 57:153–65. doi: 10.1016/j.jaac.2017.11.022
5. Calear AL, Christensen H, Mackinnon A, Griffiths KM, O’kearney R. The youth mood project: a cluster randomized controlled trial of an online cognitive behavioral program with adolescents. J Consult Clin Psychol (2009) 77:1021–32. doi: 10.1037/a0017391
6. Wong N, Kady L, Mewton L, Sunderland M, Andrews G. Preventing anxiety and depression in adolescents: a randomised controlled trial of two school based Internet-delivered cognitive behavioural therapy programmes. Internet Interv (2014) 1:90–4. doi: 10.1016/j.invent.2014.05.004
7. Perry Y, Werner-Seidler A, Calear A, Mackinnon A, King C, Scott J, et al. Preventing depression in final year secondary students: school-based randomized controlled trial. J Med Internet Res (2017) 19:e369. doi: 10.2196/jmir.8241
8. Perry Y, Petrie K, Buckley H, Cavanagh L, Clarke D, Winslade M, et al. Effects of a classroom-based educational resource on adolescent mental health literacy: a cluster randomised controlled trial. J Adolesc (2014) 37:1143–51. doi: 10.1016/j.adolescence.2014.08.001
9. Langley AK, Nadeem E, Kataoka SH, Stein BD, Jaycox LH. Evidence-based mental health programs in schools: barriers and facilitators of successful implementation. Sch Ment Health (2010) 2:105–13. doi: 10.1007/s12310-010-9038-1
10. Kendall PC, Makover H, Swan A, Carper MM, Mercado R, Kagan E, et al. What steps to take? How to approach concerning anxiety in youth. Clin Psychol Sci Pract (2016) 23:211–29. doi: 10.1111/cpsp.12156
11. Ho FY, Yeung W, Ng TH, Chan CS. The efficacy and cost-effectiveness of stepped care prevention and treatment for depressive and/or anxiety disorders: a systematic review and meta-analysis. Sci Rep (2016) 6:29281. doi: 10.1038/srep29281
12. Cross S, Hickie I. Transdiagnostic stepped care in mental health. Public Health Res Pract (2017) 27:e2721712. doi: 10.17061/phrp2721712
13. Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency: narrative literature review. Br J Psychiatry (2005) 186:11–7. doi: 10.1192/bjp.186.1.11
14. Gunlicks-Stoessel M, Mufson L, Westervelt A, Admiral D, Murphy S. A pilot SMART for developing an adaptive treatment strategy for adolescent depression. J Clin Child Adolesc Psychol (2016) 45:480–94. doi: 10.1080/15374416.2015.1015133
15. Zuckerbrot RA, Cheung AH, Jensen PS, Stein RE, Laraque D. Guidelines for adolescent depression in primary care (GLAD-PC): I. identification, assessment, and initial management. Pediatrics (2007) 120:e1299–312. doi: 10.1542/peds.2007-1144
16. Salloum A, Wang W, Robst J, Murphy TK, Scheeringa MS, Cohen JA, et al. Stepped care versus standard trauma-focused cognitive behavioral therapy for young children. J Child Psychol Psychiatry (2016) 57:614–22. doi: 10.1111/jcpp.12471
17. Rapee RM, Lyneham HJ, Wuthrich V, Chatterton ML, Hudson JL, Kangas M, et al. Comparison of stepped care delivery against a single, empirically validated Cognitive-Behavioral Therapy program for youth with anxiety: a randomized clinical trial. J Am Acad Child Adolesc Psychiatry (2017) 56:841–8. doi: 10.1016/j.jaac.2017.08.001
18. Meeuwissen J.A.C., Feenstra TL, Smit F, Blankers M, Spijker J, Bockting CLH, et al. The cost-utility of stepped-care algorithms according to depression guideline recommendations—results of a state-transition model analysis. J Affect Disord (2018) 1:244–54. doi: 10.1016/j.jad.2018.08.024
19. Van Straten A, Hill J, Richards DA, Cuijpers P. Stepped care treatment delivery for depression: a systematic review and meta-analysis. Psychol Med (2014) 45:231–46. doi: 10.1017/S0033291714000701
20. Firth N, Barkham M, Kellett S. The clinical effectiveness of stepped care systems for depression in working age adults: a systematic review. J Affect Disord (2015) 170:119–30. doi: 10.1016/j.jad.2014.08.030
21. Brown LK, Kennard BD, Emslie GJ, Mayes TL, Whiteley LB, Bethel J, et al. Effective treatment of depressive disorders in medical clinics for adolescents and young adults living with HIV: a controlled trial. J. Acquir Immune Defic Syndr (2016) 71:38–46. doi: 10.1097/QAI.0000000000000803
22. Mufson L, Rynn M, Yanes-Lukin P, Choo TH, Soren K, Stewart E, et al. Stepped care interpersonal psychotherapy treatment for depressed adolescents: a pilot study in pediatric clinics. Adm Policy Ment Health Ment Health Serv Res (2018) 45:417–31. doi: 10.1007/s10488-017-0836-8
23. Briesch AM, Chafouleas SM, Chaffee RK. Analysis of state-level guidance regarding school-based, universal screening for social, emotional, and behavioral risk. Sch Ment Health (2018) 10:147–62. doi: 10.1007/s12310-017-9232-5
24. Moon J, Williford A, Mendenhall A. Educators perceptions of youth mental health: implications for training and the promotion of mental health services in schools. Child Youth Serv Rev (2017) 73:384–91. doi: 10.1016/j.childyouth.2017.01.006
25. Husky MM, Kaplan A, Mcguire L, Flynn L, Chrostowski C, Olfson M. Identifying adolescents at risk through voluntary school-based mental health screening. J Adolesc (2011) 34:505–11. doi: 10.1016/j.adolescence.2010.05.018
26. Green JG, Mclaughlin KEA, Alegría M, Costello EJ, Gruber MJ, Hoagwood K, et al. School mental health resources and adolescent mental health service use. J Am Acad Child Adolesc Psychiatry (2013) 52:501–10. doi: 10.1016/j.jaac.2013.03.002
27. Bruns EJ, Pullmann MD, Nicodimos S, Lyon AR, Ludwig K, Namkung N, et al. Pilot test of an engagement, triage, and brief intervention strategy for school mental health. Sch Ment Health (2018) 11:148–62. doi: 10.1007/s12310-018-9277-0
28. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
29. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
30. Mcdermott B, Baigent M, Chanen A, Fraser L, Graetz B, Hayman N, et al. Clinical Practice Guidelines: Depression in adolescents and young adults. Melbourne: beyondblue: the national depression initiative (2010).
31. Rickwood D, Deane FP, Wilson CJ, Ciarrochi J. Young people’s help-seeking for mental health problems. Australian e-J Adv Ment Health (2005) 4:218–51. doi: 10.5172/jamh.4.3.218
32. Lawrence D, Johnson S, Hafekost J, De Haan KB, Sawyer M, Ainley J, et al. The mental health of children and adolescents: Report on the second Australian child and adolescent survey of mental health and wellbeing. Canberra: Department of Health (2015).
33. Bullot A, Cave L, Fildes J, Hall S, Plummer J. Mission Australia’s 2017 Youth Survey Report,. Australia: Mission Australia (2017).
34. Bradford S, Rickwood D. Adolescent’s preferred modes of delivery for mental health services. Child Adolesc Ment Health (2014) 19:39–45. doi: 10.1111/camh.12002
35. Subotic-Kerry M, King C, O’Moore K, Achilles M, O’Dea B. General Practitioners’ attitudes toward a web-based mental health service for adolescents: implications for service design and delivery. J Med Internet Res Hum Factors (2018) 5:e12. doi: 10.2196/humanfactors.8913
36. O’Dea B, Leach C, Achilles M, King C, Subotic-Kerry M, O’Moore K. Parental attitudes towards an online, school-based, mental health service: implications for service design and delivery. Adv Ment Health (2018) 17:146–60. doi: 10.1080/18387357.2018.1514269
37. Stallard P, Velleman S, Richardson T. Computer use and attitudes towards computerised therapy amongst young people and parents attending child and adolescent mental health services. Child Adolesc Ment Health (2010) 15:80–4. doi: 10.1111/j.1475-3588.2009.00540.x
38. Glasheen K, Campbell MA, Shochet I. Opportunities and challenges: school guidance counsellors’ perceptions of counselling students online. J Psychol Couns Sch (2013) 23:222–35. doi: 10.1017/jgc.2013.15
39. Glasheen K, Campbell M, Shochet I. School counsellors and students attitudes to online counselling: a qualitative study. J Relatsh Res (2015) 6:e12. doi: 10.1017/jrr.2015.8
40. Sweeney GM, Donovan CL, March S, Laurenson SD. Logging into therapy: parent attitudes and intentions to use computer-based therapies for youth mental health. Internet Interv (2015) 2:437–45. doi: 10.1016/j.invent.2015.11.001
41. Clarke AM, Chambers D, Barry MM. Bridging the digital disconnect: exploring the views of professionals on using technology to promote young people’s mental health. Sch Psychol Int (2017) 38:380–97. doi: 10.1177/0143034317700937
42. Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health Ment Health Serv Res (2011) 38:65–76. doi: 10.1007/s10488-010-0319-7
43. Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res (2017) 17:88. doi: 10.1186/s12913-017-2031-
44. Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol (2010) 10:1. doi: 10.1186/1471-2288-10-1
45. Lancaster GA. Pilot and feasibility studies come of age! Pilot and Feasibility Studies (2015) 1:1. doi: 10.1186/2055-5784-1-1
46. Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract (2004) 10:307–12. doi: 10.1111/j..2002.384.doc.x
47. Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol (2012) 65:301–8. doi: 10.1016/j.jclinepi.2011.07.011
48. Spence SH, Holmes JM, March S, Lipp OV. The feasibility and outcome of clinic plus internet delivery of cognitive-behavior therapy for childhood anxiety. J Consult Clin Psychol (2006) 74:614. doi: 10.1037/0022-006X.74.3.614
49. Spence SH, Donovan CL, March S, Gamble A, Anderson RE, Prosser S, et al. A randomized controlled trial of online versus clinic-based CBT for adolescent anxiety. J Consult Clin Psychol (2011) 79:629. doi: 10.1037/a0024512
50. Kowalenko N, Rapee RM, Simmons J, Wignall A, Hoge R, Whitefield K, et al. Short-term effectiveness of a school-based early intervention program for adolescent depression. Clin Child Psychol. Psychiatry (2005) 10:493–507. doi: 10.1177/1359104505056311
51. Sheffield JK, Spence SH, Rapee RM, Kowalenko N, Wignall A, Davis A, et al. Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents. J Consult Clin Psychol (2006) 74:66. doi: 10.1037/0022-006X.74.1.66
52. Reinke WM, Thompson A, Herman KC, Holmes S, Owens S, Cohen D, et al. The county schools mental health coalition: a model for community-level impact. Sch Ment Health (2018) 10:173–80. doi: 10.1007/s12310-017-9227-2
53. Fleming T, Bevin L, Lucassen M, Stasiak K, Hopkins S, Merry S. Beyond the trial: systematic review of real-world uptake and engagement with digital self-help interventions for depression, low mood, or anxiety. J Med Internet Res (2018) 20:e199. doi: 10.2196/jmir.9275
54. Edlund MR, Wang PS, Berglund PA, Katz SJ, Lin E, Kessler RC. Dropping out of mental health treatment: patterns and predictors among epidemiological survey respondents in the United States and Ontario. Am J Psychiatry (2002) 159:845–51. doi: 10.1176/appi.ajp.159.5.845
55. Wilson CJ, Deane FP, Ciarrochi JV, Rickwood D. Measuring help seeking intentions: properties of the general help seeking questionnaire. Can J Couns (2005) 39:15–28. doi: 10.1037/t42876-000
56. Moore JB, Carson RL, Webster CA, Singletary CR, Castelli DM, Pate RR, et al. The application of an implementation science framework to comprehensive school physical activity programs: be a champion! Front Public Health (2018) 5:354. doi: 10.3389/fpubh.2017.00354
57. Blom-Hoffman J, Leff SS, Franko DL, Weinstein E, Beakley K, Power TJ. Consent procedures and participation rates in school-based intervention and prevention research: using a multi-component, partnership-based approach to recruit participants. Sch Ment Health (2009) 1:3–15. doi: 10.1007/s12310-008-9000-7
58. Dunne T, Bishop L, Avery S, Darcy S. A review of effective youth engagement strategies for mental health and substance use interventions. J Adolesc Health (2017) 60:487–512. doi: 10.1016/j.jadohealth.2016.11.019
59. Bentley F, Church K, Harrison B, Lyons K, Rafalow M. Three hours a day: understanding current teen practices of smartphone application use. ArXiv. Available from: https://arxiv.org/abs/1510.05192 (Accessed August 12, 2019).
60. Neil AL, Batterham P, Christensen H, Bennett K, Griffiths KM. Predictors of adherence by adolescents to a Cognitive Behavior Therapy website in school and community-based settings. J. Med. Internet Res (2009) 11:e6. doi: 10.2196/jmir.1050
61. Donkin L, Christensen H, Naismith SL, Neal B, Hickie IB, Glozier N. A systematic review of the impact of adherence on the effectiveness of e-therapies. J Med Internet Res (2011) 13:e52. doi: 10.2196/jmir.1772
62. Calear AL, Christensen H, Mackinnon A, Griffiths KM. Adherence to the mood gym program: outcomes and predictors for an adolescent school-based population. J Affect Disord (2013) 147:338–44. doi: 10.1016/j.jad.2012.11.036
63. Kauer SD, Mangan C, Sanci L. Do online mental health services improve help-seeking for young people? A systematic review. J Med Internet Res (2014) 16:e66. doi: 10.2196/jmir.3103
64. Van Straten A, Seekles W, Van’t Veer-Tazelaar NJ, Beekman AT, Cuijpers P. Stepped care for depression in primary care: what should be offered and how? Med J Aust (2010) 192:S36. doi: 10.5694/j.1326-5377.2010.tb03691.x
65. Alfonsson S, Olsson E, Linderman S, Winnerhed S, Hursti T. Is online treatment adherence affected by presentation and therapist support? A randomized controlled trial. Comp Human Behav (2016) 60:550–8. doi: 10.1016/j.chb.2016.01.035
66. Beatty L, Binnion C. A Systematic review of predictors of, and reasons for, adherence to online psychological interventions. Intern J Behav Med (2016) 23:776–94. doi: 10.1007/s12529-016-9556-9
67. Gould MS, Marrocco FA, Hoagwood K, Kleinman M, Amakawa L, Altschuler E. Service use by at-risk youths after school-based suicide screening. J Am Acad Child Adolesc Psychiatry (2009) 48:1193–201. doi: 10.1097/CHI.0b013e3181bef6d5
68. Casey LM, Joy A, Clough BA. The impact of information on attitudes toward e-mental health services. Cyberpsychol Behav Soc Netw (2013) 16:593–8. doi: 10.1089/cyber.2012.0515
Keywords: school, student, mental health, stepped care, online, help-seeking, depression, anxiety
Citation: O’Dea B, King C, Subotic-Kerry M, Achilles MR, Cockayne N and Christensen H (2019) Smooth Sailing: A Pilot Study of an Online, School-Based, Mental Health Service for Depression and Anxiety. Front. Psychiatry 10:574. doi: 10.3389/fpsyt.2019.00574
Received: 23 November 2018; Accepted: 22 July 2019;
Published: 20 August 2019.
Edited by:
Mario Alvarez-Jimenez, The University of Melbourne, AustraliaReviewed by:
Pia Jeppesen, Mental Health Services, DenmarkNicola Reavley, The University of Melbourne, Australia
Copyright © 2019 O’Dea, King, Subotic-Kerry, Achilles, Cockayne and Christensen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bridianne O’Dea, Yi5vZGVhQGJsYWNrZG9nLm9yZy5hdQ==
 Bridianne O’Dea
Bridianne O’Dea Catherine King1,2
Catherine King1,2 Mirjana Subotic-Kerry
Mirjana Subotic-Kerry Melinda Rose Achilles
Melinda Rose Achilles Helen Christensen
Helen Christensen