- Department of Clinical Child and Adolescent Psychology, Philipps University Marburg, Marburg, Germany
Children of parents with a mental illness are a particularly vulnerable group as they have a high risk to develop a mental disorder themselves and those are associated with high stigma. Moreover, just like primary recipients of stigma, they are affected by the social taboo surrounding mental illness: they do not receive enough information, are often left alone with their problems, and are thus considered “invisible children”. In previous research, family stigma has only been assessed through general questionnaires for all family members. What has not yet been adequately investigated is how stigma difficulties affect the children of parents with mental illness in particular. To address these limitations, we developed the Children of Parents with Mental Illness-Stigma-Questionnaire (COPMI-SQ), a self-report instrument for young people aged 12–19 years, designed to assess young people's stigma experiences in daily life. Based on a systematic review preceding the questionnaire, we identified relevant stigma dimensions for children of parents with a mental illness that resulted in 93 items that according to theory were assumed to load on four different scales: experienced stigma, anticipated stigma, self-stigma, and structural discrimination. An expert discussion, and a comprehensibility analysis with the target group followed. In this paper, we report on the development process and initial pilot data (N = 32) on the psychometric properties of the COPMI-SQ. Item analyses via an item difficulty index, discriminatory power, as well as internal consistency analysis resulted in a revised instrument reduced to 67 items. We observed very high internal consistencies (between α = 0.868 and α = 0.975) for the subscales. The approach taken to develop the COPMI-SQ followed scientifically accepted principles by ensuring different construction phases and is considered a solid basis for further reliability and validity studies. The study is ongoing and undergoing a further validation investigation; dimensionality and factor structure will also be examined.
Introduction
Approximately 17–25% of all children worldwide live with at least one parent who has a mental illness (1–4). Evidence shows that children of parents with a mental illness (COPMI) are exposed to serious and diverse risks compared to their peers of similar age (3). The high prevalence and known risks contrast with the very low visibility of these children (5). Mental illnesses of parents can influence the living environment of children and adolescents in many ways, and they carry various risks associated with reduced mental health, poorer academic achievement, and impaired social well-being (3, 6). Moreover, COPMI carry a significantly increased risk of developing mental health problems themselves (1). In addition to genetic factors and familial influences resulting from or accompanying the parental illness, there are environmental factors that contribute to whether children develop a mental illness themselves during their lives (1, 7). One social environment mechanism that influences the entire family system and is known to be relevant in terms of children's personal development, wellbeing, and help-seeking behavior is the stigma associated with a parent's mental illness (8, 9). Despite high prevalence rates of children of parents with a mental illness, they are remaining “invisible” due to the lack of recognition and formal identification within (adult) health systems (10, 11). Through the fear of stigma and negative repercussions of those children and their families, many of these children remain hidden (8, 9).
Although the appearance of stigma is liable to historical, cultural, and temporal changes, there is hardly a country, society, or culture in the world where mental illness is not stigmatized (12, 13). Stigma is an attribute leading to widespread social disapproval, and encompasses the negative effects of a label placed on any group (14, 15). It occurs in social situations, meaning that stigma does not reside in the person itself, but is the result of the social context and the perception of the public (16). People with a mental illness are frequently viewed as dangerous, unpredictable, incompetent, abnormal, and of weak character (17). While this is widely true for all types of mental disorders, the perception of different disorders varies and therefore the stigma attached to it: for instance, schizophrenia is associated with much more “dangerousness” than depression, resulting in greater social distancing from the public to the people it is associated with (18).
With regard to the stigma of mental illness, as with other stigmatized conditions, there is evidence that those affected themselves by mental illness are not the only individuals who suffer social stigma (19). Goffman, who raised the concept of stigma, has already outlined the phenomenon of the so-called courtesy stigma in 1963 (15). Nowadays, it is widely known as stigma by association (SBA) or family stigma, describing family members as also being exposed to stigma resulting from a family member's mental illness (20). An abnormality attributed to individual family members or the family as a whole is considered key to the development of family stigma (21). Another crucial factor in determining whether a SBA occurs appears to be the entitavity, i.e. the degree to which two or more people form a significant social unit (22, 23). The higher the entitavity, the greater the likelihood of being stigmatized on the basis of association (23). Intimate groups such as families are attributed the highest degree of entitavity (23)—the association with a stigmatized family member and one's own experience of stigmatization is therefore very likely.
Children and adolescents who grow up with parents with a mental illness are thus—due to their dependent and close relationship to the affected person—a particularly vulnerable group for stigma. They may face the stigma due to the parental mental illness itself, and due to associated peculiarities and “otherness” within their families as described above (21, 24, 25). Negative effects in the affected children and young people arise both from the actual stigma experienced as well as the fear of being stigmatized and the internalization of stigmatizing attitudes toward them and their families (24, 26, 27).
There are many theories clarifying the various facets of stigma for people with a mental illness. Yet there is no comprehensive theoretical model for SBA. Research suggests that family stigma is no monolithic phenomenon, because it varies depending on the relationship the family member has with the person with the mental illness: studies have shown that parents of children with a mental illness are more likely to experience the stigma of neglect and blame for their children's disease onset (12, 28), and the siblings of children with a mental illness and spouses of someone with a mental illness are more likely to experience the stigma of blame for the persistence of their relative's disease (12); COPMI are more likely to face the stigma of “contamination”—meaning that the general population believes that parental illness, and especially regarding COPMI, is passed on to children (29). However, studies in this regard are very sparse. By describing a “contamination” stigma, authors are often referring to the public perception of stigma toward COPMI [e.g., (30, 31)], and are thereby missing out to understand children's lived experiences. Thus, these studies possess little informative value if we hope to understand how children perceive and experience family stigma. A recent integrative review on the evidence of stigma concepts for children of parents with a mental illness has shed light on those limitations by identifying stigma-related experiences and outcomes as reported by parents and children (29). Nevertheless, this review shows that a concept which includes the various dimensions of stigma experiences of children whose parent has a mental illness is missing. The results of the review show that children report feelings of embarrassment, shame, and the need to hide their parental mental illness, but the authors do not integrate those findings into an overall framework of different stigma dimensions.
To fill this gap, we have conducted a systematic review to analyze the COPMI's experiences of stigma and to identify specific stigma dimensions and their characteristics for this specific target group (28). Our review resulted in four stigma dimensions: (1) Experienced SBA describes personally experienced prejudice and discrimination (32, 33); (2) anticipated SBA incorporates expectations that others will devalue and discriminate against them in the future (32); (3) affiliate stigma describes the self-stigma of people associated with a mental illness, i.e. the internalization of public stigma (34); and (4) structural discrimination, entailing social institutions and ideological systems that reproduce and maintain the stigmatized status (14).
In a literature search, we identified nine scales measuring mental illness SBA or family stigma (34–42) as well as one family-experiences interview with a stigma subscale (43). Most of the scales only measure the stigma component self-stigma/internalized stigma (34–36, 40). One of the scales was a slightly modified version of a scale constructed for primary stigma recipients, i.e., people with a mental illness (39). Another scale was developed to measure the SBA of relatives of patients with schizophrenia (42); the others were not restricted to a specific relative's mental illness. Six scales as well as the interview schedule stigma scale were designed for all family members, while two of the scales measure the stigma parents of children with a mental illness suffer from (40, 41). None of the scales was constructed or validated for minor children. The items' wording is often awkward [e.g., “Most people believe their friends would not visit them as often if a member of their family were hospitalized for serious mental illness” (37)]. In addition, the way the items are phrased often presuppose a great deal of basic knowledge of certain emotional and cognitive processes, such as “I feel emotionally disturbed because I have a family member with mental illness/intellectual disability” (34), or do not seem stigma-specific: “Having a family member with mental illness/intellectual disability imposes a negative impact on me” (34).
Furthermore, we know that stigma varies depending on the individual's role within the family, and none of the established instruments combines all the stigma dimensions highlighted in the review that are relevant to children with a mentally ill parent. Our systematic review has revealed aspects of stigma that are quite specific to their role as children, for example, being bullied and teased in school, being isolated because of feeling ashamed and therefore not inviting friends home, being afraid of passing on the illness to another generation, being responsible as a child for the parent's wellbeing when psychiatrists turn them away, having nobody to talk to, and not getting enough information about their parent's mental illness.
Overall, for children of parents with a mental illness, no suitable instrument exists yet to measure their stigma experiences, expectations, self-stigma and the stigma's structural dimensions—especially none considering the special role of children. The current study aimed to describe the development and initial pilot data on our newly developed Children of Parents with a Mental Illness—Stigma Questionnaire (COPMI-SQ). This scale can provide important information to better understand the complex phenomenon of stigma by association among young people and shed light on experiences and needs of this group in intervention studies or anti-stigma campaigns.
METHODS
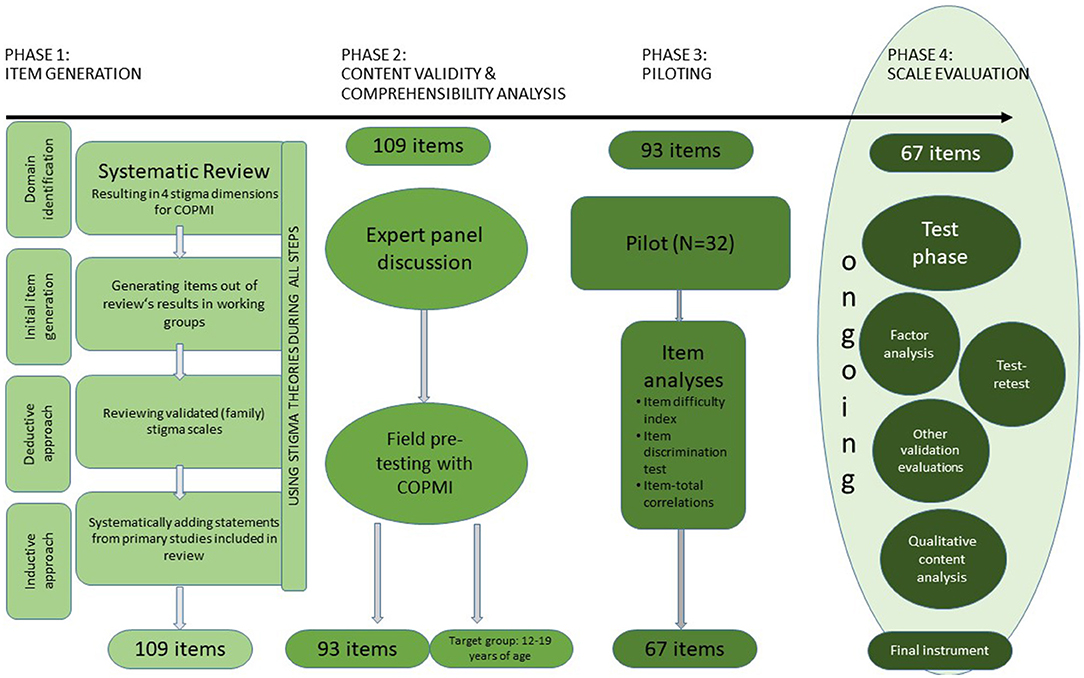
Figure 1 shows the different stages of development for the COPMI-SQ. We have oriented ourselves to two guidelines for the development of new scales (44, 45). We are currently reporting on phase 3 and present our pilot data. Phase 4 is still under way.
Ethics
Research with children and adolescents is always in a field of tension between the respect of the various rights of children and their special need for protection. In recent decades, a paradigm shift has occurred within research, in which children are now rather seen as “moral agents in their own right” (46). As a result, more research is now being conducted with children to increase their participation. Researchers and adults in general cannot assume that their view of the world is congruent with that of children (46). In order to comply with the UN Convention on the Rights of the Child, we consider it of fundamental importance to interview children and adolescents themselves when it comes to their life experiences and the intention to improve their living conditions. Since it can be assumed that stigma may affect a lot of children of parents with mental illness in particular, it is necessary to obtain their perspectives before interventions are directed past their needs.
In order to ensure the special protection of children under guardianship, we followed the guidelines of the Central Ethics Committee of the German Medical Association (47), which stipulates a need for an informed consent both from their parents with a mental disorder and the children themselves in age-appropriate language prior to study participation. We considered the costs and benefits of a survey, which could be potentially burdensome and concluded that the results of the survey offered great insights into the experiences of this population which could be beneficially used for further interventions for this population. However, since it can be assumed that children of parents with mental illness are particularly exposed to stresses that may also be related to stigmatizing experiences, they were offered to contact the persons responsible for the study, who are child and adolescent psychotherapists, at any time. In addition, they were advised to contact any trusted adult person in case of need. Furthermore, prior to study participation, they were informed that they could withdraw from their participation in the online study at any time and without giving reasons, up to when the data were analyzed.
The study was approved by the Ethics Committee of the Psychology Department of Philipps University of Marburg (study approval number: 2020-20).
Inclusion Criteria
Young people were eligible to participate in the study as long as they were between 12 and 19 years old and one or both parents had a mental illness. Information regarding the illness was obtained through a self-report by the parents. Otherwise, there were no exclusion criteria.
Phase 1: Item Generation
The first step toward designing this new instrument, the systematic review, resulted in four different dimensions of family stigma in COPMI, i.e. experienced SBA, anticipated SBA, affiliate stigma (self-stigma), and structural discrimination. Those findings were presented by a PhD student to 50 scientific collaborators in Clinical Psychology and Clinical Child and Adolescent Psychology working groups of Marburg University, Department of Psychology, including pre-, post-docs, and professors. Post-docs and professors further possessed licenses as psychotherapists and PhD students were psychotherapists in training. Quotes from primary studies based on a systematic review with the instruction to collect ideas for items for a survey were presented to all participants. Initial items that may be used in a survey for this population and for the different dimensions were generated through group discussions.
The inductively generated items were then compared with already validated instruments measuring (family) stigma (see above) to apply formulations already established whenever possible. Using the established stigma scales, the generated items were developed further and supplemented in their formulation.
To ensure that every aspect of stigma was covered, the first pool of items was then supplemented by adding further inductively formed items for every (sub-)sub-category identified in the review [for further information see Dobener et al. (28)]. Statements from the included primary studies were included also to reflect as accurately as possible the comments of the target group members themselves in the items. For each category identified in the review, 5–15 items were formed. A total of 109 items was generated in phase 1.
Phase 2: Content Validity and Comprehensibility Analysis
Expert Discussion
The entire item pool was then reviewed and discussed by a panel of experts from our and other known working groups, with knowledge in developing questionnaires as well as in the field of stigma. The experts were asked to rate all items according to the extent to which they seemed to be an appropriate measure of the intended construct. They were also asked to provide open-ended feedback. Items agreed upon by at least two of the three experts were retained or reworded according to their comments. This ensured that only items that were understandable and meaningful in terms of both content and language were used. Through this process, the item pool was reduced to 96 items since the expert panel revealed problems like overly complex wording, repetition, or other violations of “best-practices” regarding item structure (48).
Comprehensibility Analysis With Children
In a further step, five children and adolescents of different ages whose parents have a mental illness filled in the questionnaire to check comprehensibility. They completed the COPMI-SQ in the presence of the author L-MD, to enable immediate feedback on any difficulties in understanding. In addition to the comprehensibility check, this allowed us to see whether filling in the COPMI-SQ was associated with any mental stress when confronted with the effects of their parents' illness. According to the children's feedback, some items were reworded, and three were removed entirely.
At the end of this second phase, the item pool was reduced to 93 items, of which 91 were closed questions and two were open-ended. Due to the complexity of wording and the general need for any mental illness concept as well as children's feedback, we found our survey to be most suitable for children and adolescents aged 12–19 years. For younger children, the language and delivery as an online survey does not seem the right format.
Phase 3: Piloting
Our questionnaire was piloted in an online survey with a sample of children and adolescents having at least one parent with a mental illness.
The study was conducted using the online platform SosciSurvey (49) between March and May 2021. All participants were part of a convenience sample—either contacted as part of an ongoing study [COMPARE-family, see (4, 50), via university mailing lists or clinical institutions; e.g., psychiatric clinics, psychotherapy outpatient clinics]. Participants could participate in a raffle of several gifts as study reimbursement. Inclusion criteria for the COPMI-SQ-validation were having a parent with a mental illness and being 12–19 years of age. Participants were not excluded if they themselves had a mental illness.
Measures
Participants responded to questions pertaining to socio-demographic characteristics (age, school grade, living situation, etc.) and questions about their parent's mental illness and their own health status.
COPMI-SQ
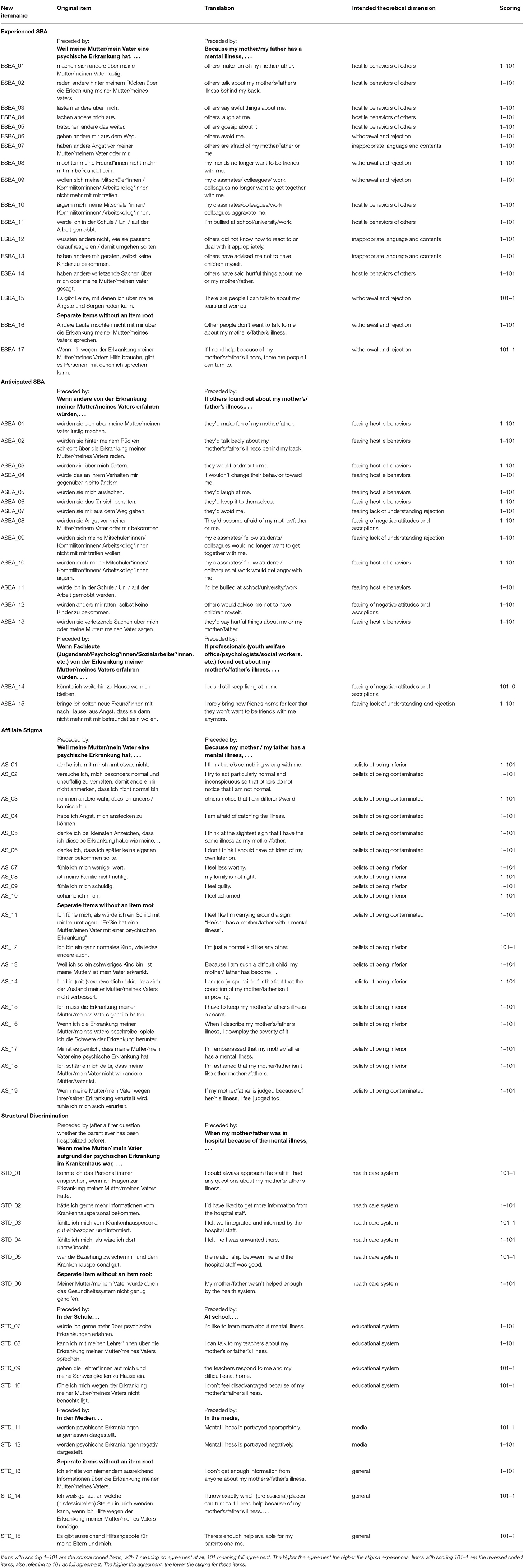
Stigma experiences in COPMI were measured via the 93 items in the newly developed COPMI-SQ. Participants were first asked to complete two open-ended sentences: “I think about people with a mental illness …” and “Others think about people with a mental illness …”. Afterwards, they were asked to rate each of the 91 closed items on a visual analog scale (VAS). The VAS consisted of a line with verbal anchors (“strongly disagree” on the far left and “strongly agree” on the far right). All of the items were scored from 1 to 101, with 1 meaning no agreement at all, 101 meaning full agreement. Most of the items were preceded by an item root like “Because my mother/my father has a mental illness,…”, others were presented separately. The questionnaire consists of 26 reversed coded items, whose agreement represented a low stigma experience to control for and identify acquiescence response bias (51), see Supplementary Table S1. For all other items, the higher the agreement, the greater the experience of stigma.
The first theoretically assumed dimension, experienced stigma by association (SBA), consisted of 18 items representing varied aspects of directly experienced stigmatization as a result of the parental mental illness; for example, experiencing rejection by others, inappropriate and hurtful language or warnings, and obviously discriminatory behavior such as bullying.
The second theoretically assumed dimension, anticipated SBA, was captured across 20 items and included fears of stigmatizing behavior or the attitudes of others if they found out about the parental mental illness.
For the third theoretically assumed dimension, self-stigma, 23 items were constructed to capture different facets of self-stigma: the feeling of being “contaminated” by the parental illness, the shame associated with the parental illness, feelings of guilt, and feeling generally inferior compared to other people.
The fourth and last theoretically assumed dimension represents the experienced structural discrimination and was captured by 30 items. This included discrimination in the education system, the health system, the media, and discrimination in society as a whole. Our instrument's entire structure and all its items are found in Supplementary Table S1.
Statistics
Sample Size
We aimed to recruit about 200 participants to validate the scale's psychometric properties. The sample size of 200 is considered adequate for validating an instrument, i.e., for item analyses, and factor analyses to examine the questionnaire's multidimensionality (52, 53).
Missing Values and Outliers
The online survey was designed so that all items had to be answered. Thus, none of the included cases had any missing values. However, there was a filter question addressing parental hospitalization. If this was answered positively, all the subsequent questions were posed only to COPMI whose parent(s) had been hospitalized; this group formed a smaller subsample of only 18 children. All items were analyzed for univariate outliers using boxplots. Conspicuous cases were assessed as realistic after examination and were in a generally inconspicuous range across the mean values achieved; thus they were not excluded from further analyses.
Item Analyses
General Procedure
The item analyses were carried out in three phases. In the first phase, items were checked at the subscale level for appropriate item difficulty and discriminatory power, and subscales were adjusted by removing inappropriate items. Due to content considerations, some psychometrically inappropriate items were retained. In the second phase, the adjusted subscales were combined into an overall scale, the items were rechecked for their characteristic values, and unsuitable items were removed accordingly to improve global consistency and increase the suitability of the overall instrument. In the third phase, the subscales of the COPMI-SQ were adapted to the structure of the final overall instrument, and the final instrument's internal consistency was calculated again. Statistical analyses were carried out using SPSS, version 20.
Item Difficulty Index
Given that the COPMI-SQ is intended to allow differentiation across a broad spectrum of trait values, we aimed for a distribution of item difficulties of 20 < Pi <80 [see (54)]. Since extremely difficult, or very easy items hardly allow differentiation between test persons, items with values below 20 and above 80 were considered more closely. Items of very low or extreme difficulty were checked for their discriminatory power and their retention or removal from the item pool was supplemented with content considerations. The exact reasons for retaining or deleting a given conspicuous item are provided in Supplementary Table S1.
Discriminatory Power
The item discrimination index was calculated using the corrected item-total-correlation. Values of rit between 0.3 and 0.5 were considered acceptable; 0.5 < rit <0.7 is considered good discriminatory power (54). All items whose discriminatory power was below 0.3 were scrutinized, and usually removed to ensure high internal consistency of the subscales and the overall instrument. However, those items with cut-off values below 0.3 were checked for their relevance to the content and either deleted or reformulated when evaluating strongly relevant content. They were then removed one after the other and new item-total correlations were calculated in each case to see how the items interacted. The order of removal of the items and content-related considerations is illustrated in Supplementary Table S1.
Internal Reliability
Cronbach's alpha was calculated to measure the COPMI-SQ's internal reliability (55). This should attain a value of at least 0.7 for the subscales—the widely accepted criterion for Cronbach's alpha [e.g., (56)].
Results
Sample
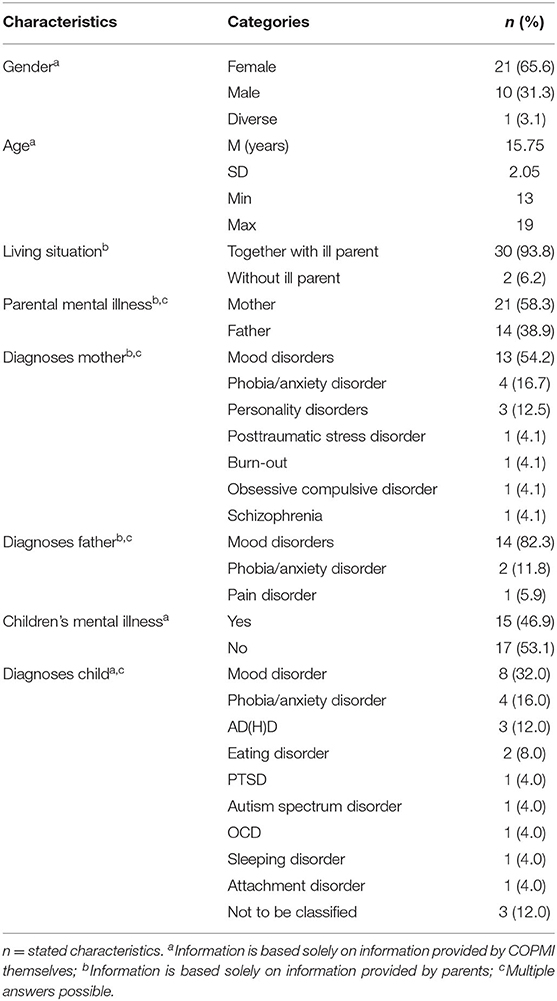
All participants (N = 32) were between 13 and 19 years of age (M = 15.75, SD = 2.05). Sixty-five percent of the participants were female. The COPMI usually lived together with their parent with a mental illness (93.8%). Three COPMIs reported having both parents with a mental illness. Mothers were most often affected (60%). The most common parental diagnosis was a mood disorder such as bipolar disorder and depression (maternal: 54.2%; paternal: 82.3%), followed by anxiety disorders (maternal: 16.7%; 11.8% paternal). Almost half of the children stated to have already suffered from a mental illness themselves (46.9%). These were, similar to the parental diagnoses, usually mood disorders (32%). All the sample characteristics are provided in Table 1.
As COPMI are an exceedingly difficult target group to reach (57, 58), we were unable to recruit enough COPMI to assess decisively the questionnaire's psychometric goodness of fit, despite intensive recruitment efforts. Nevertheless, according to Johanson and Brooks (59), 30 representative participants from the population of interest suffice for a pilot study to test a new instrument in terms of preliminary item analyses, estimates of internal consistency and proportions of people responding to specific options. For factor and further analyses, more participants are needed, so we focused on the item analyses, especially to reduce the number of items requiring further validation and evaluation of the COPMI-SQ, in order to make the questionnaire more practical and reduce participation thresholds as well as raise the quality of the instrument.
Item Analysis on Subscale Level
Experienced SBA Subscale
Initial Cronbach's alpha equalled 0.940 (see Table 4). In the experienced SBA scale, two items revealed low item difficulty, and one item a low item-total correlation. The item with the low item-total correlation was thus removed. However, the two items of low item difficulty were retained after content considerations. Both had a discriminatory power above 0.7. The item “Because my mother/my father has a mental illness, my friends no longer want to be friends with me” was retained because this aspect addressing the loss of friendship stood out in the review as a relevant experience for COPMI, and that aspect was not covered by any other item. Similar considerations applied to the item “Because my mother/my father has a mental illness, I'm bullied at school/university/work”: the aspect of bullying has been described in the literature, and as it is not covered by any other item in the questionnaire, we retained this item.
Anticipated SBA Subscale
In the anticipated SBA subscale (initial Cronbach's alpha of 0.927), four items revealed a low item-total-correlation; one of them also revealed low difficulty. The item with low discriminatory power and low difficulty was removed first. After considering the content, the other items with too little discriminatory power were also removed one after the other, because they were either covered by other items or classified as non-essential. The step-by-step removal of the items led to an increased item-total correlation within the subscale.
Affiliate Stigma Subscale
In the Affiliate Stigma subscale with an initial alpha of 0.904, two items were conspicuous due to low difficulty and two items due to low discriminatory power. The item with negative discriminatory power was removed first, as it seems to be misleading. Furthermore, its content was already covered by other items. The other item with low discriminatory power was also removed. The item “Because my mother/father has a mental illness, I don't think I should have children of my own later” was retained despite its low difficulty because it measures the belief in contamination, which has consequences for future plans, and is not covered by any other items. Furthermore, the other item of low difficulty “I feel like I'm carrying around a sign: He/she has a mother/father with a mental illness” was also retained because, it was adapted from an evaluated stigma scale and, additionally, the aspect of “contamination” is otherwise not sufficiently embodied in comparison to “inferiority.”
Structural Discrimination Subscale
Out of the Structural Discrimination subscale with an initial alpha of 0.817, 16 items revealed low discriminatory power. Of these, one had very high and one very low item difficulty. The first ones deleted stepwise were those three items with negative item-total correlation, indicating that they measured something completely different. Further items of very low discriminatory power were then successively removed, starting with those intended to measure discrimination within the mental health system. This was because it was clearly overrepresented compared to the other dimensions of the subscale.
The item “At school, I'd like to learn more about mental illness” was retained despite its low discriminatory power, firstly because it was on the edge of acceptance (rit = 0.295), secondly, in order to maintain the proportions to the other structural stigma dimensions to some extent, and thirdly, because the content of the item was attributed a special significance concerning possible interventions. For the media as a source of structural discrimination, the item “In the media, mental illness is portrayed negatively, which contributes to many people developing prejudices” was retained despite its low item-total-correlation; for the reason of having at least two items representing this source of discrimination. In addition, we reworded the item in order to avoid multidimensionality as follows “Mental illness is portrayed negatively in the media.”
Item Analysis on Total Scale
In the second phase of the item analyses, i.e., when assessing the internal reliability of the overall instrument, one item in the Affiliate Stigma scale and an item in the Structural Discrimination scale showed low item-total correlations and were therefore deleted. Supplementary Table S1 shows which items were affected.
Revised COPMI-SQ
Our instrument was reduced to a total of 67 items after the three phases of item analyses. The revised instrument is illustrated in Table 2. The final version of the Experienced SBA subscale now consists of 17 items, with Cronbach's alpha = 0.948 and item-total-correlations from good (lowest 0.395 for the item “There are people I can talk to about my fears and worries.”) to very high (highest 0.905 for item “Because my mother/father has a mental illness, my classmates/colleagues/work colleagues tease me.”). The final subscale Anticipated SBA (Cronbach's alpha = 0.949) shows item-total correlations between 0.426 (item “If others found out about my mother's/father's illness, it wouldn't change their behavior toward me”) and 0.877 (item “they'd bad-mouth me.”), see Supplementary Table S1. The final subscale of Affiliate Stigma consists of 19 items, with item-total correlations ranging between 0.449 (item: “I'm just a normal kid like any other.”) to 0.820 (item: “Because my mother/my father has a mental illness, I think there's something wrong with me”), and with Cronbach's alpha = 0.933. The item-total-correlations for the final subscale of Structural Discrimination (STD) are the lowest compared to the other subscales, and range from 0.282 (item “In media, mental illness is appropriately portrayed”), which is actually below acceptable discriminatory power, but will be kept to ensure the media source of discrimination is represented, to 0.705 (item: “In school, I don't feel disadvantaged because of my mother's/father's illness”). The revised STD subscale results in a Cronbach's alpha of 0.868.
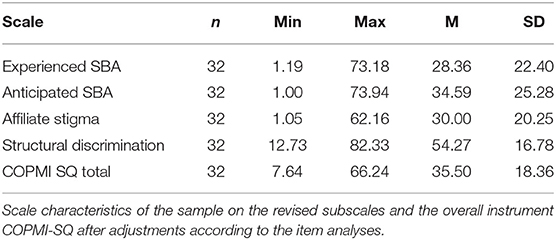
Table 3 shows our sample's scores on the final subscales and the overall COPMI-SQ instrument. Overall, the sample shows very similar average levels of family stigma on the subscales Experienced SBA, Anticipated SBA, Affiliate Stigma and the overall instrument. Here COPMI, with a mean score of 30, tend to be in the lower third of the possible values. On the STD subscale, COPMI are in the middle range of values. Supplementary Table 2 illustrates the intercorrelations of the final instrument scales. Overall, these tend to demonstrate small to very large correlations, all of which are significant.
Internal Reliability
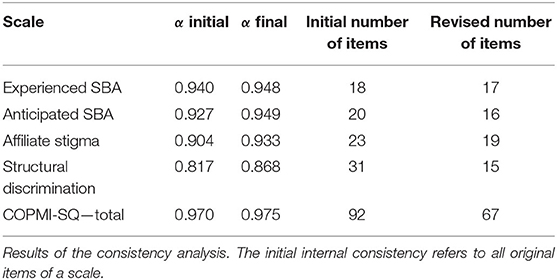
Table 4 shows the internal consistencies for both the initial subscales and subscales adjusted by the item analyses as described above. The internal consistencies for the overall instrument are also visible in Table 4. We observed an improvement in all the scales' consistencies. We detected internal consistencies between α = 0.868 and α = 0.975 across the scales.
Discussion
This study reports on the development and piloting of a questionnaire to assess stigma in children of parents with a mental illness. The COPMI-SQ is the first instrument incorporating different stigma by association dimensions tailored to the stigma experiences of children of parents with a mental illness. After reducing the item number, the final version of the COPMI-SQ consists of 67 items representing four subscales: experienced stigma (17 items), anticipated stigma (16 items), self-stigma (19 items) and structural discrimination (15 items). The COPMI-SQ, once validated, can be used to better understand the complex phenomenon of stigma by association among young people and also to target the experiences and needs of this group in intervention studies or anti-stigma campaigns. As the questionnaire also captures which parental condition in which parent is present, it can be used to create insights to the extent to which stigma experiences vary for different parental disorders. In addition, it could potentially support shedding light on the gendered theoretical landscape of parenting.
Developing the Instrument
The approach we took to develop the instrument followed scientifically accepted principles (20) by ensuring various construction phases. The construction process relied on (family) stigma theories (14, 20, 39, 60, 61), incorporated qualitative results from a comprehensive systematic review to best reflect the expressed stigma experiences of affected children (28), and included expert opinions on the initially constructed items. The COPMI-SQ is thus considered a solid basis for further reliability and validity studies.
Item Reduction
We ran into difficulty with item analyses due to the fact that it was not a test construction for which clear rules could be applied while considering the required item difficulties or discriminatory power. Although recommendations could be used as a guide, each change or reduction of the item pool had to be made by carefully considering the content. For example, the subscale “Structural Discrimination” represents a very heterogeneous set of items, as they were meant to represent different institutional sources of discrimination, for example the educational system, as well as the media and the health care system. In this respect, we had to assume that discrimination perceived in one societal structure does not necessarily go hand in hand with a high level of discrimination in another, as there are unintended public and private sector policies that restrict opportunities for some groups (62) and we do not yet know precisely how they interact (62, 63). This means that the item-total correlations it did for not have to meet the same requirements as did the other subscales. We also had to make sure we did not over- or under-represent some sub-aspects.
Nevertheless, a detailed explanation of the reasons for deleting or retaining the items ensures transparency, and very high item-total correlations were achieved overall. Only in the “Structural Discrimination” subscale one item with a low item-total-correlation, namely “In the media, mental illness is appropriately portrayed” remained in the questionnaire. This can be justified due to the item's relevance to the content and that its discriminatory power of 0.282 was only minimally below the acceptable limit of 0.3. Nevertheless, items of low discriminatory power or showing low item-total correlations must be examined more closely in the further validation course in a factor analysis.
The very high values regarding internal reliability and the increase in Cronbach's alpha in each subscale, as well as in the final instrument compared to its first version suggest that we made the right decisions here.
We detected overall very strong correlations between the various subscales in the questionnaire's revised form. This may be an initial indication that also a one factor model may be considered. In a further validation study, factor structure and dimensionality have to be examined.
Evaluating Reliability and Validity
The final COPMI-SQ's internal reliability can be considered as very good. It demonstrates good to excellent internal consistency in the subscales, as well as excellent internal reliability of the instrument as a whole. We ensured content validity through an expert panel, and evaluated the difficulty of understanding items with children themselves. However, due to the impossibility of conducting a factor analysis, whether these subscales are confirmed by the instrument's factor structure and multidimensionality cannot be assessed yet.
Test-retest reliability could not be assessed due to an insufficient sample size. However, we can assume that stigma experiences are also not constant variables. New experiences can always emerge, so that if test-retest reliability is to be measured, there should be a shorter time span between them. Furthermore, the mere questioning of these experiences could also lead to some young people, especially when confronted with the topic for the first time through the questionnaire, potentially being sensitized to subsequent experiences and accordingly revealing higher values at a later point in time.
Strengths and Limitations
The greatest strength of the present study is that the COPMI-SQ was theory-based and developed supported by an extensive systematic review. In addition, the various steps in its development are presented transparently and in detail.
There are several areas for improvement and further investigations. About half of the participants reported having a mental illness of their own—a good representation of the population of children of parents with mental illness (64), but this means that their responses may be cofounded by experiencing stigma due to their own illness. Due to recruitment difficulties, we were unable to identify enough participants to permit a factor analysis and investigate multidimensionality and factor structure. The assumed four factors are not supported by the very high inter-correlations of the assumed subscales, but they cannot be ruled out either. However, the study is still ongoing. With the reduced number of items due to the item analyses, we can reach our sample size more easily. Other recruitment strategies, such as recruiting via schools, must be integrated in the future to reach this vulnerable target group. Since this paper is concerned with the methodology of developing a new instrument, content-related considerations of the different dimensions of stigma have been marginalized. A more detailed discussion of the meaning and interconnectedness of the different dimensions can be found in the paper reporting the results of the systematic review (28).
Implications for Further Research and Use of the COPMI-SQ
In a further validation study, we will aim to recruit approximately 200 COPMI to examine our questionnaire's multidimensionality. In the first step, this should be examined via an exploratory factor analysis (EFA). An EFA is preferable to a confirmatory factor analysis (CFA), since it is possible that factor structures other than those expected might emerge (45). Especially as high inter-correlations between the subscales might indicate a one-factor structure, uni-dimensionality should also be checked. A CFA should then be conducted on a separate sample to confirm the structure of the scales resulting from the EFA.
A further validated COPMI-SQ could be used to help develop anti-stigma and general interventions for this population. Our first pilot data promises good reliability of the a priori assumed subscales. As our scale is constructed for young people aged 12–19, it can be used as a starting point to develop a scale addressing the same problem for younger children. A more creative and interactive way of getting those information from younger children, should be developed, to be able to incorporate younger children's views as well. Research in children's lived experiences is limited, and this is especially true for younger children.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Psychology Department of Philipps University of Marburg. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
L-MD designed and completed the study, involved as the main person in charge in all development and analyses steps, and wrote the manuscript. MS co-organized the data collection process and supported the writing of the manuscript by reviewing and editing. KV assisted with data collection and data analysis. HC supervised the study and preparation of the manuscript and supported the writing of the manuscript by reviewing and editing.
Funding
Funding was provided by the Working Group on Clinical Child and Adolescent Psychology, Department of Psychology, Philipps University of Marburg. The funding for the raffle was provided by COMPARE-family. COMPARE-family is funded by the Federal Ministry of Education and Research (BMBF) (01GL1748B). The funders did not influence the collection, analysis, and interpretation of data and played no role in writing the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank Simone Pfeiffer from the University of Landau and Cornelia Weise from Philipps University of Marburg for their crucial contributions regarding the formulation of the items, thanks to their expertise in the field of stigma and questionnaire development. The authors would also like to thank all the participating COPMI and their parents. We know it can be difficult and painful to provide information about such experiences. We hope to contribute to improving care and, above all, to breaking the silence.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.800037/full#supplementary-material
References
1. van Santvoort F, Hosman CMH, van Doesum KTM, Janssens JMAM, et al. Children of mentally ill parents participating in preventive support groups. Parental Diagnoses and Child Risk J Child Fam Stud. (2014) 23:67–75. doi: 10.1007/s10826-012-9686-x
2. Maybery DJ, Reupert AE, Patrick K, Goodyear M, Crase L. Prevalence of parental mental illness in Australian families. Psychiatr Bull. (2009) 33:22–6. doi: 10.1192/pb.bp.107.018861
3. Hosman CMH, van Doesum KTM, van Santvoort F. Prevention of emotional problems and psychiatric risks in children of parents with a mental illness in the Netherlands. I The scientific basis to a comprehensive approach. Aust e-J Adv Mental Health. (2009) 8:250–63. doi: 10.5172/jamh.8.3.250
4. Christiansen H, Reck C, Zietlow A-L, Otto K, Steinmayr R, Wirthwein L, et al. Children of mentally III parents at risk evaluation (COMPARE). Design and methods of a randomized controlled multicenter study-Part I. Front Psychiatry. (2019) 10:128. doi: 10.3389/fpsyt.2019.00128
5. Gladstone BM, Boydell KM, McKeever P. Recasting research into children's experiences of parental mental illness. Beyond risk and resilience. Soc Sci Med. (2006) 62:2540–50. doi: 10.1016/j.socscimed.2005.10.038
6. Radicke A, Barkmann C, Adema B, Daubmann A, Wegscheider K, Wiegand-Grefe S, et al. Children of parents with a mental illness. Predictors of health-related quality of life and determinants of child-parent agreement. Int J Environ Res Public Health. (2021) 18:379. doi: 10.3390/ijerph18020379
7. Reupert AE, Maybery J, Kowalenko D. Children whose parents have a mental illness. Prevalence, need and treatment. MJA Open. (2012) 1:7–9. doi: 10.5694/mjao11.11200
8. Cogan N, Riddell S, Mayes G. Children living with an affectively ill parent. How do they cope? Educ Child Psychol. (2005) 22:16–28.
9. Gladstone BM, Boydell KM, Seeman MV, McKeever PD. Children's experiences of parental mental illness. A literature review. Early Interv Psychiatry. (2011) 5:271–89. doi: 10.1111/j.1751-7893.2011.00287.x
10. Reedtz C, Lauritzen C, Stover YV, Freili JL, Rognmo K. Identification of children of parents with mental illness. A necessity to provide relevant support. Front Psychiatry. (2019) 9:358. doi: 10.3389/fpsyt.2018.00728
11. Maybery D, Reupert AE. The number of parents who are patients attending adult psychiatric services. Curr Opin Psychiatry. (2018) 31:358–62. doi: 10.1097/YCO.0000000000000427
12. Koschorke M, Evans-Lacko S, Sartorius N, Thornicroft G. Stigma in different cultures. In: Gaebel W, Roessler, Sartorius N, editors. The Stigma of Mental Illness - End of the Story?. Berlin: Springer International Publishing (2017). p. 67–82.
13. Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health. (2013) 103:777–80. doi: 10.2105/AJPH.2012.301056
14. Bos AER, Pryor JB, Reeder GD, Stutterheim SE. Stigma. Adv Theory Res Basic Appl Soc Psychol. (2013) 35:1–9. doi: 10.1080/01973533.2012.746147
16. Hebl MR, Dovidio JF. Promoting the “social” in the examination of social stigmas. Pers Soc Psychol Rev. (2005) 9:156–82. doi: 10.1207/s15327957pspr0902_4
17. Corrigan P, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. (2002) 1:16–20.
18. Rössler W. The stigma of mental disorders: A millennia-long history of social exclusion and prejudices. EMBO Rep. (2016) 17:1250–3. doi: 10.15252/embr.201643041
19. van der Sanden RLM, Bos AER, Stutterheim SE, Pryor JB, Kok G. Experiences of stigma by association among family members of people with mental illness. Rehabil Psychol. (2013) 58:73–80. doi: 10.1037/a0031752
20. Miller PW, Corrigan FE. Shame, blame, and contamination. A review of the impact of mental illness stigma on family members. J Mental Health. (2009) 13:537–48. doi: 10.1080/09638230400017004
21. Park S, Park KS. Family stigma. A concept analysis. Asian Nurs Res. (2014) 8:165–71. doi: 10.1016/j.anr.2014.02.006
22. Campbell DT. Common fate, similarity, and other indices of the status of aggregates of persons as social entities. Syst Res. (1958) 3:14–25. doi: 10.1002/bs.3830030103
23. Pryor JB, Reeder GD, Monroe AE. The infection of bad company. Stigma by association. J Pers Soc Psychol. (2012) 102:224–41. doi: 10.1037/a0026270
24. Dam K, Hall EOC. Navigating in an unpredictable daily life. A metasynthesis on children's experiences living with a parent with severe mental illness. Scand J Caring Sci. (2016) 30:442–57. doi: 10.1111/scs.12285
25. Griffiths J, Norris E, Stallard P, Matthews S. Living with parents with obsessive-compulsive disorder. Children's lives and experiences. Psychol Psychother. (2012) 85:68–82. doi: 10.1111/j.2044-8341.2011.02016.x
26. Blakeman M, Martin C, Gupta A. Making sense of growing up with a parent with psychosis. An interpretative phenomenological analysis study. Psychosis. (2019) 11:54–62. doi: 10.1080/17522439.2019.1573916
27. Wahl P, Otto C, Lenz A. “…dann würde ich traurig werden, weil alle über meinen Papa reden – Die Rolle des Stigmas in Familien mit psychisch erkranktem Elternteil („…I would be sad then, because they are all talking about my dad”—The Role of Stigma in Families Affected by Parental Mental Illness). Gesundheitswesen. (2017) 79:987–92. doi: 10.1055/s-0043-122234
28. Dobener L-M, Fahrer J, Purtscheller D, Paul J, Christiansen H. How do children of parents with mental illness experience stigma? A systematic mixed studies review. Front Psychiatry. (2022) 13:813519. doi: 10.3389/fpsyt.2022.813519
29. Reupert A, Gladstone B, Helena Hine R, Yates S, McGaw V, Charles G, et al. Stigma in relation to families living with parental mental illness. An integrative review. Int J Ment Health Nurs. (2021) 30:6–26. doi: 10.1111/inm.12820
30. Corrigan P, Watson AC, Miller FE. Blame, shame, and contamination. The impact of mental illness and drug dependence stigma on family members. J Fam Psychol. (2006) 20:239–46. doi: 10.1037/0893-3200.20.2.239
31. Koschade JE, Lynd-Stevenson RM. The stigma of having a parent with mental illness. Genetic attributions and associative stigma. Aust J Psychol. (2011) 63:93–9. doi: 10.1111/j.1742-9536.2011.00009.x
32. Fox AB, Earnshaw VA, Taverna EC, Vogt D. Conceptualizing and measuring mental illness stigma. The mental illness stigma framework and critical review of measures. Stig Health. (2018) 3:348–76. doi: 10.1037/sah0000104
33. Pescosolido BA, Martin JK. The stigma complex. Annu Rev Sociol. (2015) 41:87–116. doi: 10.1146/annurev-soc-071312-145702
34. Mak WWS, Cheung RYM. Affiliate stigma among caregivers of people with intellectual disability or mental illness. J Appl Res Intellect Disabil. (2008) 21:532–45. doi: 10.1111/j.1468-3148.2008.00426.x
35. Girma E, Möller-Leimkühler AM, Dehning S, Mueller N, Tesfaye M, Froeschl G, et al. Self-stigma among caregivers of people with mental illness. Toward caregivers' empowerment. J Multidiscip Healthc. (2014) 7:37–43. doi: 10.2147/JMDH.S57259
36. Morris E, Hippman C, Murray G, Michalak EE, Boyd JE, Livingston J, et al. Self-stigma in relatives of people with mental illness scale. Development and validation. Br J Psychiatry. (2018) 212:169–74. doi: 10.1192/bjp.2017.23
37. Struening EL, Perlick DA, Link BG, Hellman F, Herman D, Sirey JA, et al. Stigma as a barrier to recovery. The extent to which caregivers believe most people devalue consumers and their families. Psychiatr Serv. (2001) 52:1633–8. doi: 10.1176/appi.ps.52.12.1633
38. Werner P, Goldstein D, Heinik J. Development and validity of the Family Stigma in Alzheimer's disease Scale (FS-ADS). Alzheimer Dis Assoc Disord. (2011) 25:42–8. doi: 10.1097/WAD.0b013e3181f32594
39. Yin Y, Zhang W, Hu Z, Jia F, Li Y, Xu H, et al. Experiences of stigma and discrimination among caregivers of persons with schizophrenia in China. A field survey PLoS ONE. (2014) 9:e108527. doi: 10.1371/journal.pone.0108527
40. Zisman-Ilani Y, Levy-Frank I, Hasson-Ohayon I, Kravetz S, Mashiach-Eizenberg M, Roe D. Measuring the internalized stigma of parents of persons with a serious mental illness. The factor structure of the parents' internalized stigma of mental illness scale. J Nerv Ment Dis. (2013) 201:183–7. doi: 10.1097/NMD.0b013e3182845d00
41. Zuckerman KE, Lindly OJ, Reyes NM, Chavez AE, Cobian M, Macias K, et al. Parent perceptions of community autism spectrum disorder stigma. Measure validation and associations in a multi-site sample. J Autism Dev Disord. (2018) 48:3199–209. doi: 10.1007/s10803-018-3586-x
42. Yıldız M, İncedere A, Kiras F, Abut FB, Kircalı A, İpçi K. Development of self-stigma inventory for families of the patients with schizophrenia (SSI-F). Validity and reliability study. Psychiatry Clin Psychopharmacol. (2019) 29:463–71. doi: 10.1080/24750573.2018.1480858
43. Tessler RC. Family Experiences With Mental Illness. Westport, Conn: Richard Tessler and Gail Gamache (2000).
44. Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. (2018) 6:149. doi: 10.3389/fpubh.2018.00149
45. Carpenter S. Ten steps in scale development and reporting. A guide for researchers. Commun Methods Measures. (2017) 12:25–44. doi: 10.1080/19312458.2017.1396583
46. Bell N. Ethics in child research: rights, reason and responsibilities. Children's Geogr. (2008) 6:7–20. doi: 10.1080/14733280701791827
47. Zentrale Ethikkommission. Stellungnahme der Zentralen Kommission zur Wahrung ethischer Grundsätze in der Medizin und ihren Grenzgebieten (Zentrale Ethikkommission) bei der Bundesärztekammer zur Forschung mit Minderjährigen. Deutsches Ärzteblatt. (2004) 101:1613–1617.
48. Hinkin TR. A brief tutorial on the development of measures for use in survey questionnaires. Organ Res Methods. (1998) 1:104–21. doi: 10.1177/109442819800100106
49. Leiner DJ. SoSci Survey (Version 3, 1.06). (2019). Available online at: https://www.soscisurvey.de (accessed September 22, 2021).
50. Stracke M, Gilbert K, Kieser M, Klose C, Krisam J, Ebert DD, et al. COMPARE Family (Children of Mentally Ill Parents at Risk Evaluation). Study protocol for a preventive intervention for children of mentally ill parents (Triple P, evidence-based program that enhances parentings skills, in addition to gold-standard cbt with the mentally ill parent) in a multicenter RCT-Part II. Front Psychiatry. (2019) 10:54. doi: 10.3389/fpsyt.2019.00054
51. Herche J, Engelland B. Reversed-polarity items and scale unidimensionality. J Acad Market Sci. (1996) 24:366–74. doi: 10.1177/0092070396244007
52. Guadagnoli E. The Relationship of Sample Size to the Stability of Component Patterns: A Simulation Study. University of Rhode Island, Open Access Master's Theses. Paper 1575 (1984). Available online at: https://digitalcommons.uri.edu/theses/157
53. Comrey AL. Factor-analytic methods of scale development in personality and clinical psychology. J Consult Clin Psychol. (1988) 56:754–61. doi: 10.1037/0022-006X.56.5.754
55. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. (1951) 16:297–334. doi: 10.1007/BF02310555
56. Hossiep R. Cronbachs alpha. In: Wirtz MA, editor. Lexikon der Psychologie. Bern: Hogrefe (2021).
57. Grové C. Using social networking sites in research. An emerging approach to engaging with young people who have a parent with a mental illness and/or substance abuse disorder. Front Psychiatry. (2019) 10:76. doi: 10.3389/fpsyt.2019.00281
58. van Doesum KTM, Riebschleger J, Carroll J, Grové C, Lauritzen C, Mordoch E, et al. Successful recruitment strategies for prevention programs targeting children of parents with mental health challenges. An international study. Child Youth Serv. (2016) 37:156–74. doi: 10.1080/0145935X.2016.1104075
59. Johanson GA, Brooks GP. Initial scale development. Sample size for pilot studies. Educ Psychol Meas. (2010) 70:394–400. doi: 10.1177/0013164409355692
60. Fife B, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and Cancer. J Health Soc Behav. (2000) 41:50–67.
61. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. (2001) 27:363–85. doi: 10.1146/annurev.soc.27.1.363
62. Corrigan PW, Markowitz FE, Watson AC. Structural levels of mental illness stigma and discrimination. Schizophr Bull. (2004) 30:481–91. doi: 10.1093/oxfordjournals.schbul.a007096
63. Hatzenbuehler ML. Structural stigma. Research evidence and implications for psychological science. Am Psychol. (2016) 71:742–51. doi: 10.1037/amp0000068
Keywords: children of parents with a mental illness, stigma by association, family stigma, COPMI-SQ, questionnaire, instrument development, piloting
Citation: Dobener L-M, Stracke M, Viehl K and Christiansen H (2022) Children of Parents With a Mental Illness—Stigma Questionnaire: Development and Piloting. Front. Psychiatry 13:800037. doi: 10.3389/fpsyt.2022.800037
Received: 22 October 2021; Accepted: 04 February 2022;
Published: 08 April 2022.
Edited by:
Anja Wittkowski, The University of Manchester, United KingdomReviewed by:
Emma Maynard, University of Portsmouth, United KingdomKate Blake-Holmes, University of East Anglia, United Kingdom
Andrea Reupert, Monash University, Australia
Copyright © 2022 Dobener, Stracke, Viehl and Christiansen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lisa-Marie Dobener, bGlzYS1tYXJpZS5kb2JlbmVyQHVuaS1tYXJidXJnLmRl
 Lisa-Marie Dobener
Lisa-Marie Dobener Markus Stracke
Markus Stracke Kathrin Viehl
Kathrin Viehl Hanna Christiansen
Hanna Christiansen