- 1Department of Psychiatry, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 2Department of Nursing, College of Health Science, Woldia University, Woldia, Ethiopia
- 3Department of Psychiatry, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 4Department of Medical Nursing, School of Nursing, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 5Department of Psychiatry, College of Health Science, Mettu University, Mettu, Ethiopia
Background: Poor sleep quality significantly impacts academic performance in university students. However, inconsistent and inconclusive results were found in a study on sleep among university students in several African nations. Therefore, this study aimed to estimate the pooled prevalence and associated factors of poor sleep quality among university students in Africa.
Methods: The databases PubMed, Scopus, Cochrane Library, Science Direct, African Journal Online, and Google Scholar were searched to identify articles. A total of 35 primary articles from 11 African countries were assessed and included in this systematic review and meta-analysis. Data were extracted by using a Microsoft Excel spreadsheet and exported to STATA version 14 for analysis. The I2 test was used to assess the statistical heterogeneity. A random effect meta-analysis model was employed with 95% confidence intervals. Funnel plots analysis and Egger regression tests were used to check the presence of publication bias. A subgroup analysis and a sensitivity analysis were done.
Results: A total of 16,275 study participants from 35 studies were included in this meta-analysis and systematic review. The overall pooled prevalence of poor sleep quality among university students in Africa was 63.31% (95% CI: 56.91-65.71) I2 = 97.2. The subgroup analysis shows that the combined prevalence of poor sleep quality in East, North, West, and South Africa were 61.31 (95% CI: 56.91-65.71), 62.23 (95% CI: 54.07-70.39), 54.43 (95% CI: 47.39-61.48), and 69.59 (95% CI: 50.39-88.80) respectively. Being stressed (AOR= 2.39; 95% CI: 1.63 to 3.51), second academic year (AOR= 3.10; 95% CI: 2.30 to 4.19), use of the electronic device at bedtime (AOR= 3.97 95% CI: 2.38 to 6.61)) and having a comorbid chronic illness (AOR = 2.71; 95% CI: 1.08, 6.82) were factors significantly associated with poor sleep quality.
Conclusion: This study shows that there is a high prevalence of poor sleep quality among university students in Africa. Being stressed, in the second year, using electronic devices at bedtime, and having chronic illness were factors associated with poor sleep quality. Therefore, addressing contributing factors and implementing routine screenings are essential to reduce the burden of poor sleep quality.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42023493140.
Introduction
Sleep is a naturally recurring physiological process that is important for psychological, physical, and emotional well-being (1). Sleep is also an important role in cognitive functions like judgment and memory consolidation, and vital for academic performance (2). Sleep quality is a combination of quantitative and qualitative aspects, including duration and subjective feeling of restfulness upon awakening (3). Africa is a continent that is bounded by the Mediterranean Sea to the north, the Indian and Atlantic Oceans to the east, the Atlantic Ocean to the west, and the confluence of the two oceans to the south (4). According to recent studies, non-communicable illnesses (NCDs), such as sleep disorders, are becoming more common at an alarming rate across Africa, placing a strain on healthcare resources in addition to communicable diseases (5). Due to factors including urbanization, socioeconomic development, and globalization, NCDs are becoming more common among young Africans. Taking care of these risk factors in today’s youth can drastically change how NCDs are expected to develop in Africa (5–8). Nowadays, the majority of young individuals sleep for shorter periods of time than what is advised by science (9). Good sleep quality at night facilitates the brain’s physiological repair processes and nerve cell growth. Regular engagement in these processes enhances an individual’s memory and learning capacity (10, 11). Due to a lack of resources for education, young adults in Africa typically perform worse academically, especially if they live in rural areas (12). However, African students with lesser academic standing may experience sleep disturbances as a result, particularly if they attempt to find work and their grades fall short of most employer imposed requirements (13).
Poor sleep quality is a common problem for university students, and it has a detrimental effect on their academic performance (14, 15). Compared to the general population, university students had a twofold higher prevalence of poor quality of sleep (16). This is brought on by the change from high school to college, the lessening of the role of parents, and higher expectations for academic achievement (17, 18). Poor sleep quality was found to be highly prevalent among medical students 55.64% according to a global meta-analysis study (19). A cross-sectional study was carried out in seven countries the Dominican Republic, Egypt, Guyana, India, Mexico, Pakistan, and Sudan, and the prevalence of sleep quality among university students was found to be 73.5% (20). These rates are greater than those of the general population (21, 22). A complicated interaction between genetics, academic load, technology, environmental conditions, and comorbidities is blamed for this problem. In general, it has been noted that a sizable percentage of students have trouble sleeping, which may be connected to stress from their studies (22, 23).
Poor sleep quality among university students can lead to mental and physical health issues (24). Students who have poor quality of sleep typically report common mental health issues, which many will probably need to get support for in order to successfully resolve. Poor quality of sleep has an impact on several aspects of behavior, including executive function, hormone balance, emotional control, and attentiveness. Numerous studies that involved depriving small groups of healthy individuals of all sleep for one or two nights revealed a wide range of specific abnormalities (24–26). Among the findings in the field of emotional regulation is a rise in psychopathology symptoms, like depression (27–31), anxiety (28, 29), and stress (32–34) including substance use (18, 35). Sleep is also crucial for learning and memory processes. Nonetheless, there is still much to learn about the specifics of the connection between sleep and memory formation. According to the dual process theory, declarative memory may require non-REM sleep, and procedural memory may require rapid eye movement (REM) sleep. This is because different forms of memory are associated with different sleep states (36, 37). Therefore, poor sleep can impair attention, concentration, and memory and all this leads to poor academic performance (2, 36, 38, 39). It also leads to metabolic, hormonal, and immunologic effects, causing immune suppression (40–42). Undergraduate students often experience poor sleep quality due to various factors, including irregular sleep schedules fatigue, and co-morbid chronic illness (43, 44). Sleep disturbances can worsen a person’s quality of life in addition to contributing to the early onset of chronic diseases (45). Factors such as internet addiction, substance use, depression, stress, and poor academic performance (20, 35, 46–48) are associated with poor sleep quality. New social and academic environments, reduced parental supervision, and increased academic demands contribute to poor sleep quality among this population (18, 22, 49).
Poor sleep quality among college students in African countries is a significant issue, with mixed findings across studies. It is crucial to investigate patterns of poor sleep quality to create efficient interventions and reduce the likelihood of the detrimental effects associated with poor sleep quality, such as school dropout, poor academic performance, suicide, burnout, depression, and anxiety. To date, no meta-analysis, and systematic review has been carried out to investigate the prevalence of poor sleep quality among this population. To better understand the prevalence and associated factors of poor sleep quality among university students in African countries, we did a thorough meta-analysis and systematic review study.
Research questions
● What is the estimated pooled prevalence of poor sleep quality among university students in Africa?
● What are the associated factors for poor sleep quality among university students in Africa?
Materials and methods
The current meta-analysis and systematic review was registered (ID CRD42023493140) in the Prospective Register of Systemic Review (PROSPERO). Our search strategy and selection of publication for the review were conducted according to the (PRISMA 2020) guideline (50) (Additional File 1).
Searching strategy
This study was conducted to determine the sleep quality and associated factors among university students in Africa. A search of published articles was found by using the following databases: EMBASE, PubMed, African Journals Online, Psychiatry Online, Scopus, World Health Organization (WHO) reports, Cochrane Library, and other gray literature from Google. A search strategy was developed for each database by using a combination of free texts and controlled vocabularies (Mesh). The search for these articles was carried out until January 2, 2024. The following search items were used (“prevalence” OR “magnitude” OR “epidemiology), AND (“poor sleep quality” OR “poor sleep” OR “sleep quality”) AND (“associated factors” OR “risk factors” OR “determinants” OR “predictors” OR “correlate”) AND (“University” OR “College” AND using African search filter developed by Pienaar et al. to identify prevalence studies (51). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed in conducting this systematic review and meta-analysis.
Eligibility criteria
Inclusion criteria
Cross-sectional studies that reported the prevalence of poor sleep quality among university students published in peer-reviewed journals in English language only, conducted in the continent of Africa were included. The tool used was the Pittsburg Sleep Quality Index only to diagnose poor sleep quality, and published from March 2011 to June 2023 were included in this review and meta-analysis.
Exclusion criteria
Studies were excluded if they did not report the prevalence of poor sleep quality, case reports, reviews, poster presentations, and editorial letters. Studies published in non-English languages, and conducted outside the continent of Africa were excluded. Besides this studies without access to the full data and duplicated studies were also excluded.
Outcome of interest
The primary outcome of this review was to determine the pooled prevalence of poor sleep quality among university students in Africa. The second outcome was to identify the pooled effects of factors associated with poor sleep quality. STATA version 14.0 was used to determine the pooled prevalence of depression, and the odds ratio (OR) was used to identify the pooled effect size of factors associated with poor sleep quality.
Study selection and quality assessment
The articles that were retrieved were imported into EndNote X7 (Clarivate, London, UK) for gathering and arranging search results as well as eliminating duplicate entries. Three authors (GK, YAW, and GMT) evaluated the quality of the primary studies using the Joanna Briggs Institute (JBI) quality appraisal criteria. There are nine items on this quality assessment checklist, ranging from 0 to 9 (0–4 low, 5-7 medium, and 8 and above good quality (52). Those articles with high and medium quality (greater than or equal to 5) were included in the final analysis.
Data extraction
Using a standardized data extraction format, four reviewers (FA, MM, SF, and GR) independently extracted all the necessary data from primary articles. After a careful review of the article titles, abstracts, and full texts, this was arranged using Microsoft Excel. Finally, articles approved by the four reviewers in the selection processes were included in the study, and any disagreements were resolved through discussions with other authors to reach a consensus. For instance, the first author’s name, study design, study year, publication year, country/region in which the study was conducted, a screening tool used to examine sleep quality, type of students, sample size, and prevalence of poor sleep quality were extracted. The combined estimated effects of the related covariates and prevalence of sleep quality together with their 95% confidence intervals (CIs) and odd ratios were also extracted.
Statistical procedure
The extracted data were entered into a Microsoft Excel spreadsheet and then exported to STATA version 14.0 for analysis. The pooled prevalence of poor sleep quality along with the 95% confidence intervals was visually displayed using a forest plot. The degree of heterogeneity among the included articles was determined by the index of heterogeneity (I2 statistics) (53). A random-effect meta-analysis model was used to determine the pooled effect size of all the included studies due to variations of effects from individual studies. The potential sources of heterogeneity were identified using sub-group, and sensitivity analysis and meta regression. Subgroup analyses were done by using study area (Country), Region, and type of population (medical students only, health science students, and general university students). Publication bias was assessed by using both observation of the symmetry in the funnel plots and Egger weighted regression tests (54, 55). A p-value of <0.05 in Egger’s test was considered to have statistically significant publication bias.
Results
Identified studies
A total of 1978 articles were retrieved through database literature searching, including manual searching. Of these, 658 articles were excluded due to duplication, and 1277 unrelated articles were excluded by their title and abstract. The remaining 43 full-text articles were assessed for inclusion; of them, 8 full-text articles were excluded with reasons. Despite the fact that these 8 articles included a complete skeleton, the necessary information like the outcome of interest (the prevalence of poor sleep quality), and the sample size was missing. Finally, all 35 studies were included in the final meta-analysis (Figure 1).
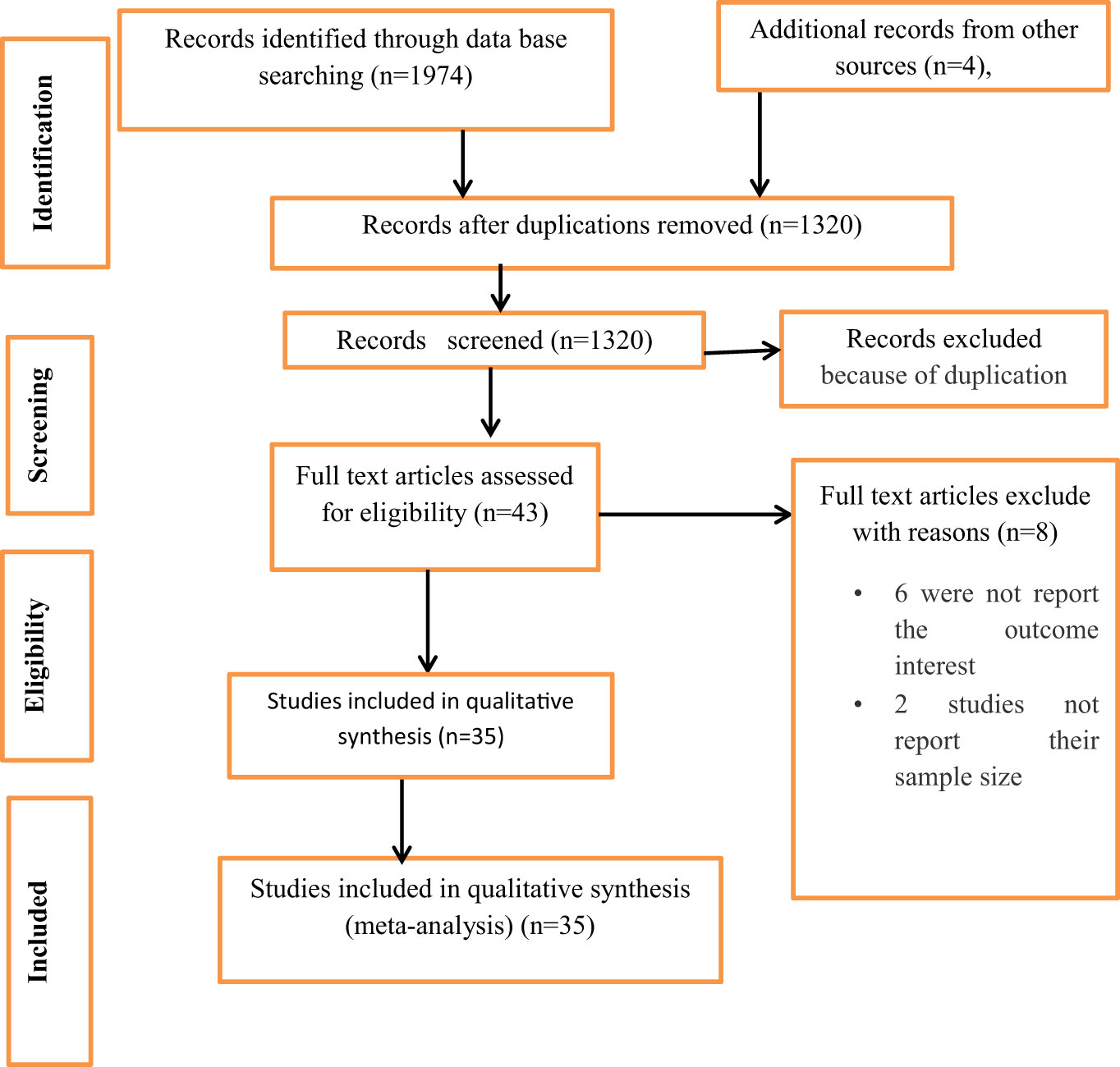
Figure 1 Flow charts to describe the selection of studies for the systematic review and meta-analysis on the prevalence of poor sleep quality among university students in Africa.
Characteristics of included studies
A total of 35 published articles from 11 countries among 16,275 university students were included in this review. All the articles included in these studies were a cross-sectional study design and the sleep quality was assessed with the Pittsburgh Sleep Quality Index. Of the 35 studies included, six studies were conducted in Nigeria, 6 in Ethiopia, 5 in Egypt, 4 in Tunisia, 3 in Ghana, 3 in Sudan, 2 in Kenya, 2 in Zambia, 2 in Morocco, 1 in Rwanda, and 1 in Libya. The study period of 25 articles were reported and conducted between March 2010 and March 2022 whereas ten studies did not report the study period. The included study was also published between March 2011 and June 2023. In terms of the study population that was involved, out of the total number of studies done, twenty-three were specifically undertaken among medical students, eight studies were conducted among general university students, and four studies were conducted among students studying health sciences (Table 1).
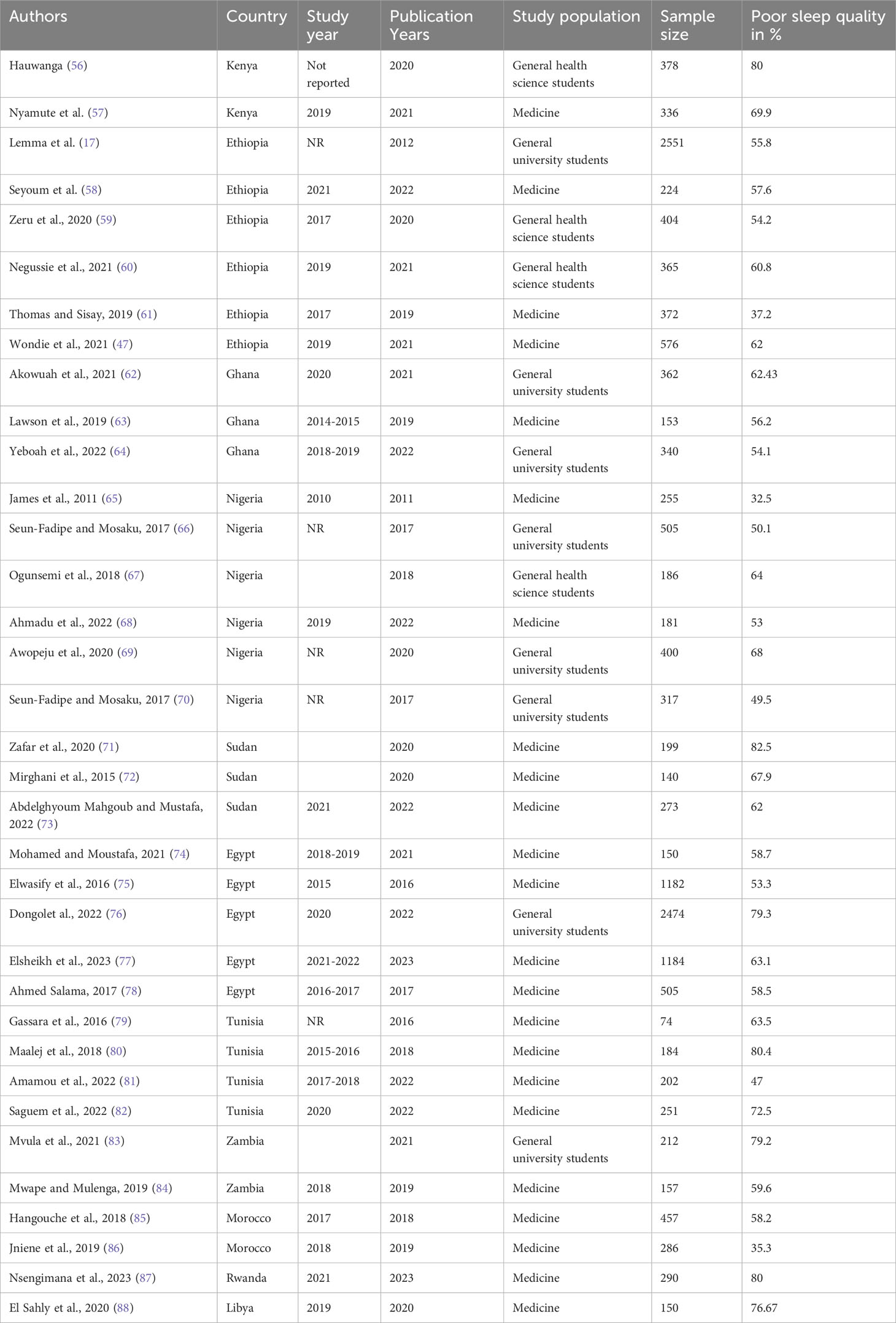
Table 1 Characteristics of original articles included in this systematic review and meta-analysis on poor sleep quality among university students in Africa.
Prevalence of poor sleep quality
Thirty-five published articles were included in this systematic review and meta-analysis to estimate the pooled prevalence of poor sleep quality among university students. The minimum prevalence of the included study was 32.5% from Nigeria and the maximum was 82.5% from Sudan. The pooled prevalence of poor sleep quality was found to be 63.31% (95%CI: 56.91-65.71). The I2 test result showed higher heterogeneity (I2 = 97.2, P= 0.000) (Figure 2). Therefore, a random effect meta-analysis model was computed to estimate the pooled prevalence of poor sleep quality. To identify the possible sources of heterogeneity, different factors associated with the heterogeneity such as study areas that is countries and regions, and type of study population were investigated by using univariate meta-regression models.
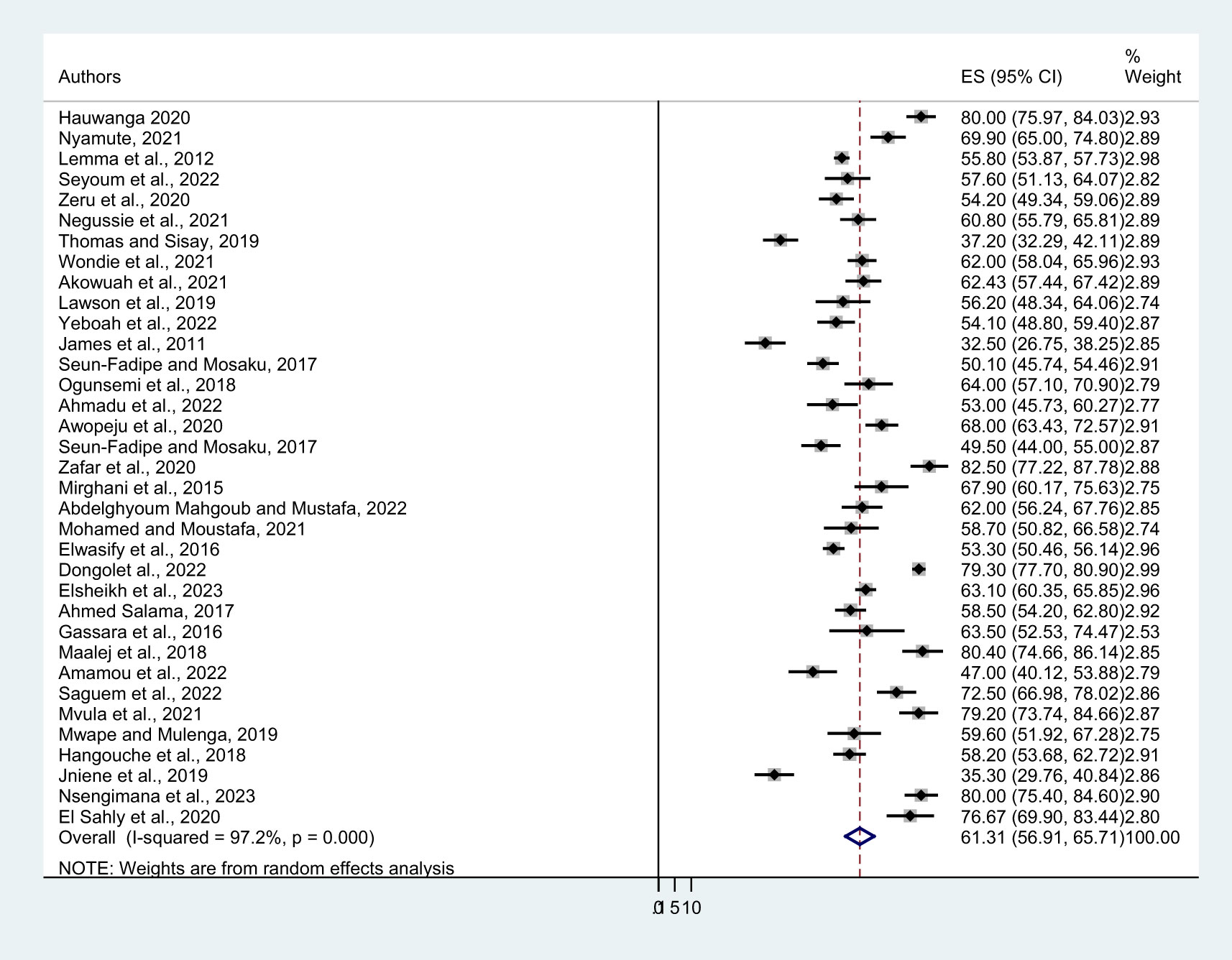
Figure 2 Forest plot showing the pooled prevalence of poor sleep quality among university students in Africa.
Publication bias
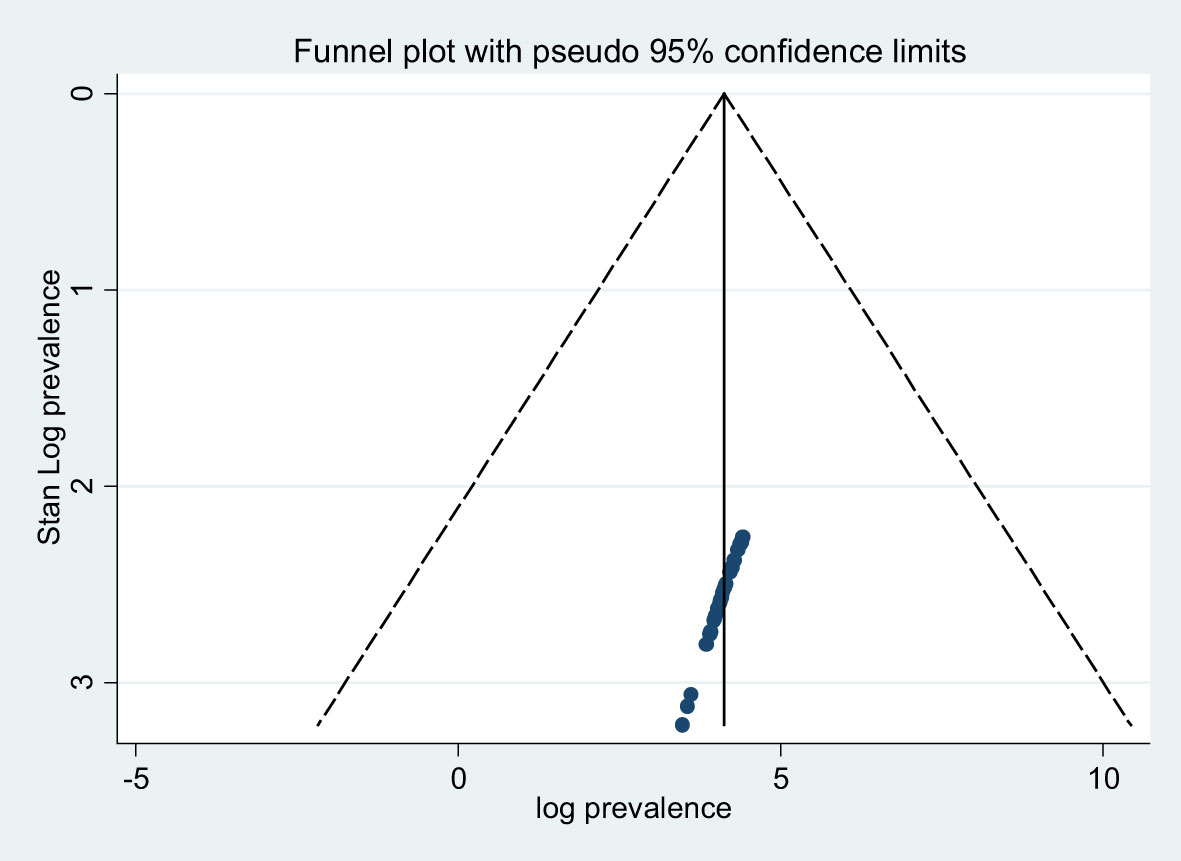
A funnel plot and Egger’s regression test were used to check the existence of potential publication bias. The result of the funnel plot triangle indicates a symmetric distribution indicating the absence of publication bias within the included studies (Figure 3). The Egger’s regression weighted test for publication bias revealed also no statistically significant evidence (P = 0.099) (Table 2).
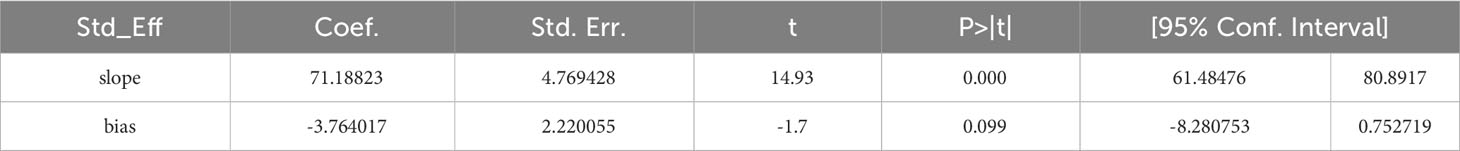
Subgroup analysis
To identify the possible source of heterogeneity, a subgroup analysis was performed based on the region, study area (country) where studies were conducted, and the type of study population of the included study. Accordingly, the combined prevalence of poor sleep quality in East, North, West, and South Africa were 61.31 (95% CI: 56.91-65.71), 62.23 (95% CI: 54.07-70.39), 54.43 (95% CI: 47.39-61.48), and 69.59 (95% CI: 50.39-88.80) respectively. Across countries relatively high prevalence of poor sleep quality were observed in Rwanda and Libya, Kenya, and Sudan, which results in 78.95 (95% CI: 75.14-82.75), 75.05 (95% CI: 65.155-84.946), 70.89 (95% CI: 57.60-84.17) respectively and the minimum was in Morocco (46.81 (95% CI: 24.37-69.25)). A sub-group analysis based on the study population also shows that the prevalence of poor sleep quality among health science students was 64.81 (95% CI: 52.36-77.25) whereas specifically among medical students was 60.33 (95% CI: 54.96-65.69) (Table 3).
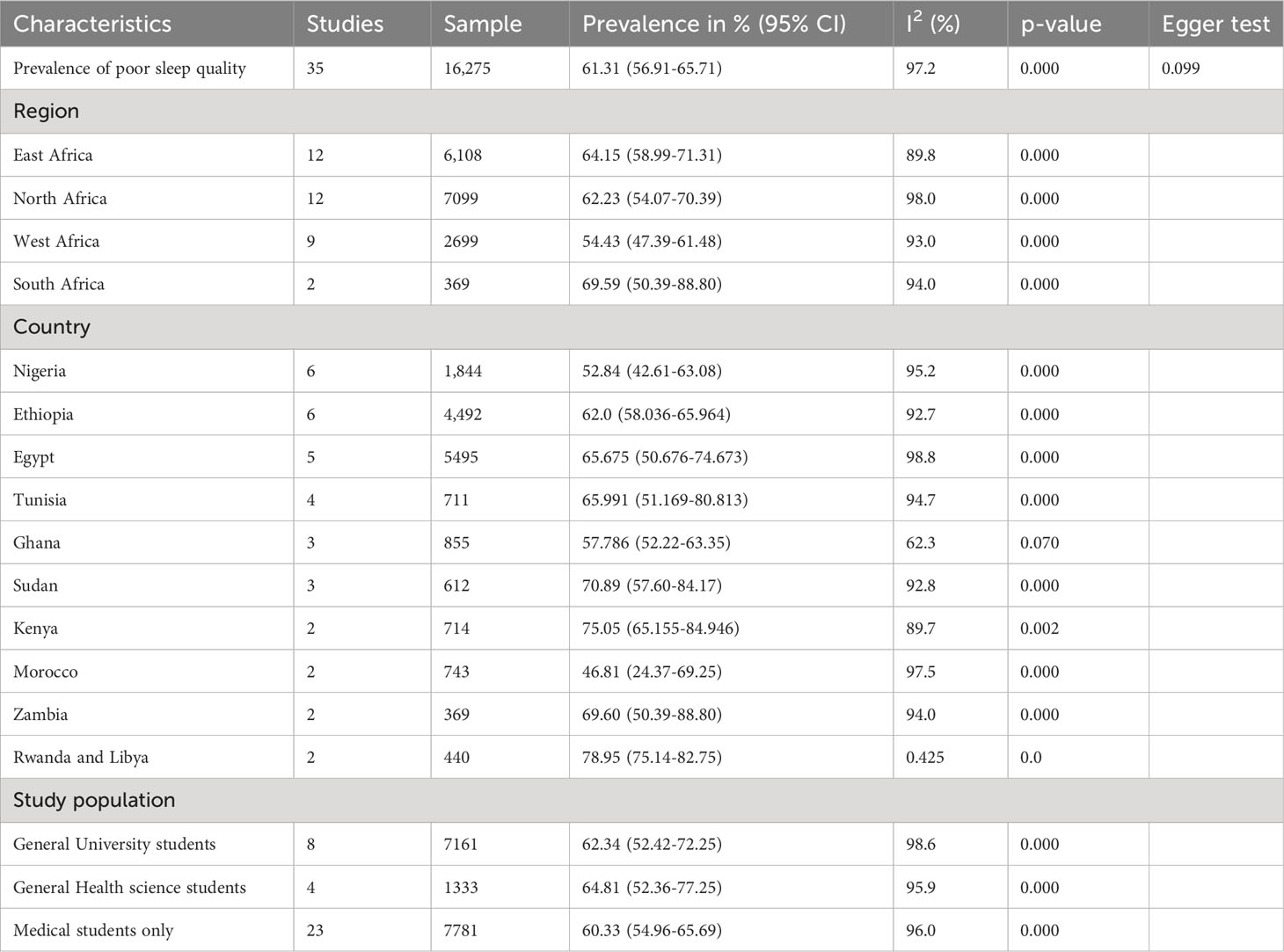
Sensitivity analysis
The sensitivity analysis was conducted to examine the heterogeneity of those studies and determine the impact of each study’s findings on the overall prevalence of poor sleep quality. The result showed that all values are within the estimated 95% CI, indicating that the omission of one study had no significant impact on the prevalence of this meta-analysis (Table 4).
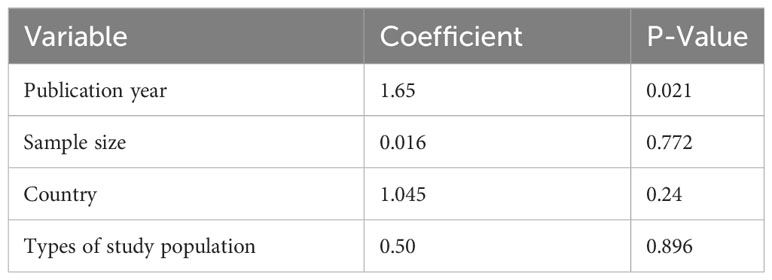
Meta regression
In this study, meta-regression was done on continuous covariates including years of publication, type of study populations (general university students, general health science students, and medical students only), sample size, and countries. The results showed that only publication year (p = 0.021) was a source of heterogeneity for this study. However, the pooled prevalence of poor sleep quality was not associated with sample size (p = 0.772), countries (p = 0.24), and types of study populations (p = 0.896) (Table 5).
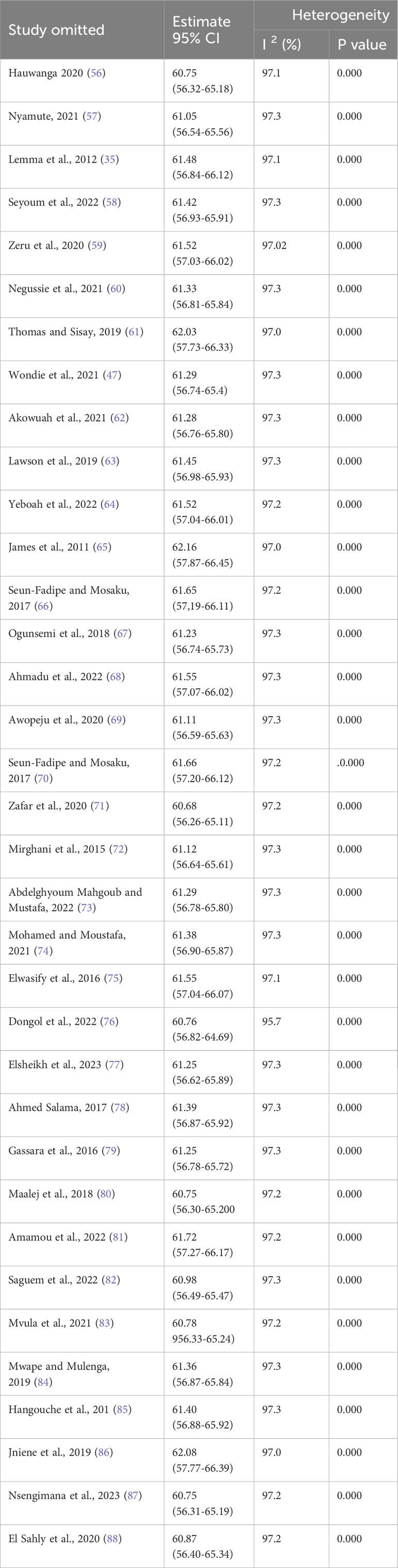
Associated factors of poor sleep quality among university students
From the included primary studies, there are different factors associated with poor sleep quality among university students, but we include those reported in more than one study. For instance, being stressed, having poor sleep hygiene, second year, using electronic devices at bedtime, and having comorbid chronic illness were factors reported and associated with poor sleep quality among university students more than once. The result of this meta-analysis indicated that being stressed is 2.4 times more likely to have poor sleep quality than not being stressed (AOR= 2.39; 95% CI: 1.63 to 3.51). The pooled odds ratio (AOR) demonstrated that the odds of poor sleep quality were 3.1 higher in participants who were in the second academic year (AOR= 3.10; 95% CI: 2.30 to 4.19) than students in other academic years. In addition, participants who use electronic devices at bedtime (AOR= 3.97 95% CI: 2.38 to 6.61) were nearly 4 times to have poor sleep quality than their counterparts. The current meta-analysis also shows that having a comorbid chronic illness was about 2.7 (AOR = 2.71; 95% CI: 1.08, 6.82) times more likely to have poor sleep quality than students who have not (Figure 4).

Figure 4 The forest plot shows associated factors of poor sleep quality among university students in Africa.
Discussion
Sleep is an important physiological process for humans. University students in African countries often report poor quality of Sleep due to changing social opportunities and increasing academic demands. However, the results of poor sleep quality among university students across nations and in between different studies vary. This systematic review and meta-analysis of 35 studies aimed to estimate the pooled prevalence and associated factors of poor sleep quality among university students in 11 African countries.
In this meta-analysis and systematic review, the pooled prevalence of poor sleep quality was found to be 63.31% with a 95% CI (56.91-65.71). This result is in line with findings from other studies. According to a systematic review and meta-analysis, which was done to determine the global prevalence rate of poor sleep quality among university students, the result was 57% (89). The current finding is also comparable with a systematic review and a meta-analysis study conducted among Korean University Students yielded 59.2% (90). A global systematic and meta-analysis study of the general population found that 57.3% of respondents had poor sleep quality, which was consistent with the findings of the current study (91).The results of a systematic review of twelve studies among Indian university students range from 25 to 72%, which is consistent with the findings of the current meta-analysis on poor sleep quality among students in Africa (92).
On the contrary, the current finding was significantly higher than with a different systematic review and meta-analysis study that was carried out at a different period. For instance, in a global systematic review and meta-analysis study conducted on sleep disruption in medicine students and its relationship with impaired academic performance, 39.8% of them reported having poor sleep quality (93). The prevalence of poor sleep quality was 51.45% in the global systematic review and meta-analysis study on the prevalence of sleep problems among 59427 medical students from 109 Studies (19). However, the sub-group analysis in the current meta-analysis studies showed that the prevalence of poor sleep quality, specifically among African medical students was 60.33 (95% CI: 54.96-65.69). In a comprehensive meta-analysis of observational studies among 24,884 medical students across 50 studies, the prevalence of poor sleep quality was 52.7% (94). The current finding is also higher than the results of previous meta-analyses that were carried out in 28 different countries, with results of 9.6% (95), 55.6% in a global meta-analysis (19), 53% in the Ethiopian population (96), 51.0% in Brazil (97), 24.1% in China (98), and 43.4% in US college students (99). A review of the causes of poor sleep quality in African young dults indicates that poor sleep quality is higher in Africa than other continents (45). When young African people do manage to get into committed partnerships, they often wind up spending a large portion of their evenings on social media (100). Some of them may indulge in drug and alcohol abuse with several partners, frequent clubs, or spend a significant portion of their sleep hours in sexual activities (100, 101). Because of this, most young adults may suffer from sleep deprivation and excessive daytime sleepiness as their bodies attempt to harmonize their naturally delayed schedule with their daily social schedules and activities at school (102). The other possible reason could be the impact that an individual’s race or ethnicity has on the quality of their sleep. It follows that mental health concerns and sleep disturbances are related health problems. According to two studies, black people are more likely to have sleep problems, which raises the likelihood of poor sleep quality in Africa (45, 103, 104).
Poor sleep quality among university students is also higher in Africa than in other studies because of the different genes involved in sleep activity (105–107), and the immune system (108–110) that Africans have. The other explanation could be because health care providers, insurance companies, governments, and the general population in Africa have little knowledge about sleep disorders and the grave repercussions they can have. One of the main problems in many African countries is the state of the health and insurance systems. The low socioeconomic level is frequently accompanied by a lack of sleep labs, clinics, and diagnostic equipment as well as a high cost of medications (111, 112).
However, the current finding is lower than a multinational cross-sectional study involving medical students during the COVID-19 pandemic, which found that 73.5% of students had poor sleep quality (20). The COVID-19 pandemic has led to increased stress, anxiety, and psychological distress among students, potentially affecting their sleep quality. The restrictions and fear of infection also led to a negative mood, which can negatively impact sleep quality. The virus primarily targets the respiratory system, and sudden outbreaks, rising death counts, and social disruptions have contributed to a decline in sleep quality. The pandemic indirectly affects college students’ moods and sleep quality (113–117).
Regarding factors affecting poor sleep quality among university students, three of the included studies in this meta-analysis study disclosed that students who have been stressed were more likely to have poor sleep quality as compared with non-stressed. The pooled result of this meta-analysis indicated that stressed students were about 1.4 times more likely to have poor sleep quality as compared to their counterparts. University students’ various activities and stressors, including studying during the night, can lead to poor sleep quality due to psychological distress (118). Compared to other students, especially medical students, they experience stress more frequently. Medical students face a stressful environment due to academic requirements and workload. They often reduce sleep to cope with the demands, leading to poor mental and physical health. Factors such as on-call duties, disease contact, and examinations contribute to this stress. Consequently, they may not prioritize sleep, leading to poor sleeping quality (34, 119). Stress plays a big role in how well people sleep, and many stresses from daily lifeare associated with poor sleep. For example, a longitudinal study of people with good sleep quality at baseline found that the most significant predictors of disrupted sleep at follow-up were daytime stress level and nighttime worries (120). Similar to this, as measured by polysomnography, healthy volunteers who experienced higher levels of stress at work had substantially more fragmented sleep and lower sleep efficiency (121). Chronic activation of stress responses, such as the sympathetic-adrenal-medullary axis and hypothalamic-pituitary-adrenal axis, can produce epinephrine and cortisol, known as stress hormones. This stress hormone has a negative effect on students sleep quality and their academic performances (118, 122). Uncontrollable worries about stress events trigger emotional arousal, leading to cognitive biases and distorted evaluations, resulting in subjective sleep quality decline (123–126).
In this meta-analysis, the year of study is also one of the factors contributing to poor sleep quality among university students. The year 2 students were more than 3 times to have poor sleep quality compared with students in other academic years. Several other investigations also discovered that the distribution of sleep quality varied across the years of study. A study in Saudi Arabian and Brazilian students showed that the odds of having poor sleep were significantly higher among second and fourth-year students (127, 128). However, according to a study in Greece, sixth-year medical students were more odds to have poor sleep quality than other students (129). A study conducted at a Chinese university revealed that fifth-year students were more negatively impacted by sleep deprivation (130), while other studies found no differences in the general quality of sleep by academic years (131). This variety may be the result of variations in the curriculum used in different countries and universities, as well as differences in social and academic demands (58, 132).
University students who use electronic devices at bedtime had approximately four times higher rates of poor sleep quality than their counterparts. This study is supported by a global meta-analysis study in which using electronic devices like smartphones was associated with poor sleep quality (133). Excessive use of electronic devices is significantly associated with poor sleep quality, according to two further global meta-analyses, one of which was conducted on medical students and the other on adolescents (89, 134). The quality of sleep is greatly impacted by using electronic devices before and during bedtime, including computers, music players, televisions, social networking sites, and cell phones. Intimate relationship-seeking young adults in Africa often find themselves interacting with their partners on mobile social media platforms like Facebook, Instagram, Snapchat, WhatsApp, and TikTok late at night, before going to bed early the next day (135, 136). Regular use of such material thus increases the likelihood of prolonged sleep onset, short duration, and extended start latency (136–138). There are physiological changes in students’ circadian rhythm and homeostatic sleep patterns. Because of this, the majority of young adults may experience sleep deprivation and excessive fatigue during the day as their bodies try to adjust to their naturally delayed schedule in order to fit in with their everyday social routines and academic obligations (102, 139). Researchers have hypothesized that using mobile devices also affects the quality of one’s sleep through a variety of mechanisms, including electromagnetic fields emitted by the device, which change melatonin rhythms, cerebral blood flow, and other related brain activities recorded in waking electroencephalograms (136, 140–142).
In this systematic review and meta-analysis study, a substantial association between having comorbid medical illness and poor sleep quality was also found. The prevalence of poor sleep quality among students was 2.7 times more common among students who had comorbid medical illnesses than those who did not. This was supported by a worldwide investigation involving seven nations as well as a US study on multi-campus students (20, 99). Poor sleep quality can also be brought on by the stress of a chronic condition. Heartburn, which is brought on by stomach acid backing up into the esophagus, is frequently linked to trouble sleeping. Uncontrolled diabetes can also contribute to trouble sleeping through night sweats, and frequent urination. Students with heart failure may experience dyspnea when they wake up in the middle of the night. People with arthritis pain may find it difficult to go off to sleep. Furthermore, a variety of over-the-counter and prescription drugs used to address these and other health issues might lower the quality of sleep (143–145).
Strengths and limitations of the study
The study’s strength lies in its pooled effect of multiple studies (35 articles) and large sample size of 16,275 university students. Additionally, we included articles from all regions of Africa (North, South, East, and West) to help generalize the findings throughout the continent. The study’s limitations include the fact that the age range was not adequately defined in the primary studies included in the review and meta-analysis and that only English-language publications were taken into consideration because of language bias. This review revealed significant between-study heterogeneity. Other than the ones currently listed, there may be more factors contributing to heterogeneity.
Conclusion and recommendations
According to this study, there is a high pooled prevalence of poor sleep quality among university students in Africa. Being stressed, using electronic devices in bed, being a second year, and having concomitant medical conditions were all associated with poor sleep quality. Thus, early detection and adequate intervention are important for improving sleep quality among university students. The establishment of academic counseling centers with an emphasis on improving sleep quality, bolstering students’ study skills, and helping them cope with their stressful surroundings is advised for the management of the sleep quality of university students. University students can also benefit from improved physical health and reduced stress levels to get better sleep. Students are also recommended to limit their use of electronic devices, such as smartphones, right before bed.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
GN: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. GMT: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. GR: Methodology, Writing – original draft, Writing – review & editing. FA: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. TT: Methodology, Writing – original draft. MAK: Data curation, Investigation, Writing – original draft. GT: Formal analysis, Writing – original draft, Writing – review & editing. SF: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. YW: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. TS: Formal analysis, Methodology, Writing – original draft. GK: Formal analysis, Investigation, Writing – original draft, Writing – review & editing. MM: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to acknowledge the authors of the included primary articles as they helped as the groundwork for this systematic review and meta-analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1370757/full#supplementary-material
Abbreviations
AOR, Adjusted odd ratio; CI, Confidence interval; COVID, Corona Virus Disease; NCD, Non-Communicable Disease; REM, Rapid Eye Movement; WHO, World Health Organization.
References
1. Colten HR, Altevogt BM. Sleep physiology. Sleep disorders and sleep deprivation: An unmet public health problem. Washington, DC: National Academies Press (US (2006).
2. Diekelmann S, Wilhelm I, Born J. The whats and whens of sleep-dependent memory consolidation. Sleep Med Rev. (2009) 13:309–21. doi: 10.1016/j.smrv.2008.08.002
3. Giri PA, Baviskar MP, Phalke DB. Study of sleep habits and sleep problems among medical students of Pravara Institute of Medical Sciences Loni, Western Maharashtra, India. Ann Med Health Sci Res. (2013) 3:51–4. doi: 10.4103/2141-9248.109488
4. Nunn N, Puga D. Ruggedness: The blessing of bad geography in Africa. Rev Economics Statistics. (2012) 94:20–36. doi: 10.1162/REST_a_00161
5. Gyasi RM, Phillips DR. Aging and the rising burden of noncommunicable diseases in sub-Saharan Africa and other low-and middle-income countries: a call for holistic action. Gerontologist. (2020) 60:806–11. doi: 10.1093/geront/gnz102
6. Curbing N. Noncommunicable diseases in africa: youth are key to curbing the epidemic and achieving sustainable development. Washington: Population Reference Bureau (2015).
7. Li Y, Fan X, Wei L, Yang K, Jiao M. The impact of high-risk lifestyle factors on all-cause mortality in the US non-communicable disease population. BMC Public Health. (2023) 23:1–9. doi: 10.1186/s12889-023-15319-1
8. Saran R, Randolph E, Omollo KL. Addressing the global Challenge of NCDs using a Risk Factor approach: voices from around the world. FASEB BioAdvances. (2021) 3:259. doi: 10.1096/fba.2020-00131
9. Chaput J-P, Dutil C, Featherstone R, Ross R, Giangregorio L, Saunders TJ, et al. Sleep duration and health in adults: an overview of systematic reviews. Appl Physiology Nutrition Metab. (2020) 45:S218–S31. doi: 10.1139/apnm-2020-0034
11. Saksvik-Lehouillier I, Saksvik SB, Dahlberg J, Tanum TK, Ringen H, Karlsen HR, et al. Mild to moderate partial sleep deprivation is associated with increased impulsivity and decreased positive affect in young adults. Sleep. (2020) 43:zsaa078. doi: 10.1093/sleep/zsaa078
12. Suardiaz-Muro M, Ortega-Moreno M, Morante-Ruiz M, Monroy M, Ruiz MA, Martín-Plasencia P, et al. Sleep quality and sleep deprivation: relationship with academic performance in university students during examination period. Sleep Biol Rhythms. (2023) 21:1–7. doi: 10.1007/s41105-023-00457-1
13. Chen W-L, Chen J-H. Consequences of inadequate sleep during the college years: Sleep deprivation, grade point average, and college graduation. Prev Med. (2019) 124:23–8. doi: 10.1016/j.ypmed.2019.04.017
14. Ghoreishi A, Aghajani A. Sleep quality in Zanjan university medical students. Tehran Univ Med J TUMS publications. (2008) 66:61–7.
15. Lemma S, Berhane Y, Worku A, Gelaye B, Williams MA. Good quality sleep is associated with better academic performance among university students in Ethiopia. Sleep Breathing. (2014) 18:257–63. doi: 10.1007/s11325-013-0874-8
16. Brown FC, Soper B, Buboltz WC Jr. PREVALENCE OF DELAYED SLEEP PHASE SYNDROME IN UNIVERSITY STUDENTS. Coll student J. (2001) 35.
17. Lemma S, Gelaye B, Berhane Y, Worku A, Williams MA. Sleep quality and its psychological correlates among university students in Ethiopia: a cross-sectional study. BMC Psychiatry. (2012) 12:1–7. doi: 10.1186/1471-244X-12-237
18. Taylor DJ, Bramoweth AD. Patterns and consequences of inadequate sleep in college students: substance use and motor vehicle accidents. J Adolesc Health. (2010) 46:610–2. doi: 10.1016/j.jadohealth.2009.12.010
19. Binjabr MA, Alalawi IS, Alzahrani RA, Albalawi OS, Hamzah RH, Ibrahim YS, et al. The Worldwide Prevalence of Sleep Problems Among Medical Students by Problem, Country, and COVID-19 Status: a Systematic Review, Meta-analysis, and Meta-regression of 109 Studies Involving 59427 Participants. Curr Sleep Med Rep. (2023) 9:1–19. doi: 10.1007/s40675-023-00258-5
20. Tahir MJ, Malik NI, Ullah I, Khan HR, Perveen S, Ramalho R, et al. Internet addiction and sleep quality among medical students during the COVID-19 pandemic: A multinational cross-sectional survey. PloS One. (2021) 16:e0259594. doi: 10.1371/journal.pone.0259594
21. Hinz A, Glaesmer H, Brähler E, Löffler M, Engel C, Enzenbach C, et al. Sleep quality in the general population: psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Med. (2017) 30:57–63. doi: 10.1016/j.sleep.2016.03.008
22. Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, et al. Sleep disturbances among medical students: a global perspective. J Clin sleep Med. (2015) 11:69–74. doi: 10.5664/jcsm.4370
23. Brick CA, Seely DL, Palermo TM. Association between sleep hygiene and sleep quality in medical students. Behav sleep Med. (2010) 8:113–21. doi: 10.1080/15402001003622925
24. Sutton EL. Psychiatric disorders and sleep issues. Med Clinics. (2014) 98:1123–43. doi: 10.1016/j.mcna.2014.06.009
25. Romier A, Maruani J, Lopez-Castroman J, Palagini L, Serafini G, Lejoyeux M, et al. Objective sleep markers of suicidal behaviors in patients with psychiatric disorders: A systematic review and meta-analysis. Sleep Med Rev. (2023) 101760. doi: 10.1016/j.smrv.2023.101760
26. Minkel J, Htaik O, Banks S, Dinges D. Emotional expressiveness in sleep-deprived healthy adults. Behav sleep Med. (2011) 9:5–14. doi: 10.1080/15402002.2011.533987
27. Moo-Estrella J, Pérez-Benítez H, Solís-Rodríguez F, Arankowsky-Sandoval G. Evaluation of depressive symptoms and sleep alterations in college students. Arch Med Res. (2005) 36:393–8. doi: 10.1016/j.arcmed.2005.03.018
28. Eller T, Aluoja A, Vasar V, Veldi M. Symptoms of anxiety and depression in Estonian medical students with sleep problems. Depression anxiety. (2006) 23:250–6. doi: 10.1002/da.20166
29. Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. (1996) 39:411–8. doi: 10.1016/0006-3223(95)00188-3
30. Chang PP, Ford DE, Mead LA, Cooper-Patrick L, Klag MJ. Insomnia in young men and subsequent depression: The Johns Hopkins Precursors Study. Am J Epidemiol. (1997) 146:105–14. doi: 10.1093/oxfordjournals.aje.a009241
31. Trockel M, Manber R, Chang V, Thurston A, Tailor CB. An e-mail delivered CBT for sleep-health program for college students: effects on sleep quality and depression symptoms. J Clin Sleep Med. (2011) 7:276–81. doi: 10.5664/JCSM.1072
32. Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. (2010) 46:124–32. doi: 10.1016/j.jadohealth.2009.06.016
33. Sahraian A, Javadpour A. Sleep disruption and its correlation to psychological distress among medical students. Shiraz E-Medical J. (2010) 11:12–7.
34. Waqas A, Khan S, Sharif W, Khalid U, Ali A. Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. PeerJ. (2015) 3:e840. doi: 10.7717/peerj.840
35. Lemma S, Patel SV, Tarekegn YA, Tadesse MG, Berhane Y, Gelaye B, et al. The epidemiology of sleep quality, sleep patterns, consumption of caffeinated beverages, and khat use among Ethiopian college students. Sleep Disord. (2012) 2012. doi: 10.1155/2012/583510
36. Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. (2006) 10:323–37. doi: 10.1016/j.smrv.2005.11.001
37. Rauchs G, Desgranges B, Foret J, Eustache F. The relationships between memory systems and sleep stages. J sleep Res. (2005) 14:123–40. doi: 10.1111/j.1365-2869.2005.00450.x
38. Shehata YA, Sharfeldin AY, El Sheikh GM. Sleep Quality as a Predictor for Academic Performance in Menoufia University Medical Students. Egyptian J Hosp Med. (2022) 89:5101–5. doi: 10.21608/ejhm.2022.261794
39. Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med Rev. (2010) 14:179–89. doi: 10.1016/j.smrv.2009.10.004
40. Ali T, Choe J, Awab A, Wagener TL, Orr WC. Sleep, immunity and inflammation in gastrointestinal disorders. World J gastroenterology: WJG. (2013) 19:9231. doi: 10.3748/wjg.v19.i48.9231
41. AlDabal L, BaHammam AS. Metabolic, endocrine, and immune consequences of sleep deprivation. Open Respir Med J. (2011) 5:31. doi: 10.2174/1874306401105010031
42. Hua J, Jiang H, Wang H, Fang Q. Sleep duration and the risk of metabolic syndrome in adults: a systematic review and meta-analysis. Front Neurology. (2021) 12:635564. doi: 10.3389/fneur.2021.635564
43. Haseli-Mashhadi N, Dadd T, Pan A, Yu Z, Lin X, Franco OH. Sleep quality in middle-aged and elderly Chinese: distribution, associated factors and associations with cardio-metabolic risk factors. BMC Public Health. (2009) 9:1–11. doi: 10.1186/1471-2458-9-130
44. Wang F, Bíró É. Determinants of sleep quality in college students: A literature review. Explore. (2021) 17:170–7. doi: 10.1016/j.explore.2020.11.003
45. Owens J, Group ASW, Adolescence Co, Au R, Carskadon M, Millman R, et al. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. (2014) 134:e921–e32. doi: 10.1542/peds.2014-1696
46. Hansen DA, Ramakrishnan S, Satterfield BC, Wesensten NJ, Layton ME, Reifman J, et al. Randomized, double-blind, placebo-controlled, crossover study of the effects of repeated-dose caffeine on neurobehavioral performance during 48 h of total sleep deprivation. Psychopharmacology. (2019) 236:1313–22. doi: 10.1007/s00213-018-5140-0
47. Wondie T, Molla A, Mulat H, Damene W, Bekele M, Madoro D, et al. Magnitude and correlates of sleep quality among undergraduate medical students in Ethiopia: cross–sectional study. Sleep Sci Practice. (2021) 5:1–8. doi: 10.1186/s41606-021-00058-2
48. Modarresi MR, Faghihinia J, Akbari M, Rashti A. The relation between sleep disorders and academic performance in secondary school students. J Isfahan Med School. (2012) 30.
49. Preišegolavičiūtė E, Leskauskas D, Adomaitienė V. Associations of quality of sleep with lifestyle factors and profile of studies among Lithuanian students. Medicina. (2010) 46:482. doi: 10.3390/medicina46070070
50. Moher D, Liberati A, Tetzlaff J, Altman DG, Group* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Internal Med. (2009) 151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
51. Pienaar E, Grobler L, Busgeeth K, Eisinga A, Siegfried N. Developing a geographic search filter to identify randomised controlled trials in Africa: finding the optimal balance between sensitivity and precision. Health Inf Libraries J. (2011) 28:210–5. doi: 10.1111/j.1471-1842.2011.00936.x
52. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. JBI Evidence Implementation. (2015) 13:147–53. doi: 10.1097/XEB.0000000000000054
53. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
54. Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Chinese edition). J Chin Integr Med. (2009) 7:889–96. doi: 10.3736/jcim20090918
55. Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. (2001) 54:1046–55. doi: 10.1016/S0895-4356(01)00377-8
56. Hauwanga LN. Prevalence and factors associated with sleep quality among undergraduate students at the college of health sciences, University of Nairobi, Kenya. Kenya: University of Nairobi (2020).
57. Nyamute L, Mathai M, Mbwayo A. Quality of sleep and burnout among undergraduate medical students at the university of Nairobi, Kenya. BJPsych Open. (2021) 7:S279–S. doi: 10.1192/bjo.2021.742
58. Seyoum M, Dege E, Gelaneh L, Eshetu T, Kemal B, Worku Y. Sleep quality and associated factors during COVID-19 pandemic among medical students of St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia MJH. Millennium Journal of Health (2022), 2790–1378.
59. Zeru M, Berhanu H, Mossie A. Magnitude of poor sleep quality and associated factors among health sciences students in Jimma University, Southwest Ethiopia, 2017. Biomed J Sci Tech Res. (2020) 25:19145–53. doi: 10.26717/BJSTR.2020.25.004202
60. Negussie BB, Emeria MS, Reta EY, Shiferaw BZ. Sleep deprivation and associated factors among students of the Institute of Health in Jimma University, Southwest Ethiopia. Front Nursing. (2021) 8:303–11. doi: 10.2478/fon-2021-0031
61. Thomas S, Sisay M. Prevalence of Poor Quality of Sleep and Associated Factors among Medical Students at Haramaya University. Int J Neurological Nursing. (2019) 5:47–62. doi: 10.37628/ijnn.v5i1.1017
62. Akowuah PK, Nti AN, Ankamah-Lomotey S, Frimpong AA, Fummey J, Boadi P, et al. Digital device use, computer vision syndrome, and sleep quality among an African undergraduate population. Adv Public Health. (2021) 2021:1–7. doi: 10.1155/2021/6611348
63. Lawson HJ, Wellens-Mensah JT, Attah Nantogma S. Evaluation of sleep patterns and self-reported academic performance among medical students at the University of Ghana School of Medicine and Dentistry. Sleep Disord. (2019) 2019. doi: 10.1155/2019/1278579
64. Yeboah K, Dodam KK, Agyekum JA, Oblitey JN. Association between poor quality of sleep and metabolic syndrome in Ghanaian university students: A cross-sectional study. Sleep Disord. (2022) 2022. doi: 10.1155/2022/8802757
65. James BO, Omoaregba JO, Igberase OO. Prevalence and correlates of poor sleep quality among medical students at a Nigerian university. Ann Nigerian Med. (2011) 5:1. doi: 10.4103/0331-3131.84218
66. Seun-Fadipe CT, Mosaku KS. Sleep quality and psychological distress among undergraduate students of a Nigerian university. Sleep Health. (2017) 3:190–4. doi: 10.1016/j.sleh.2017.02.004
67. Ogunsemi O, Afe T, Deji-Agboola M, Osalusi B, Adeleye O, Ale A, et al. Quality of sleep and psychological morbidity among paramedical and medical students in Southwest Nigeria. Res J Health Sci. (2018) 6:63–71. doi: 10.4314/rejhs.v6i2.3
68. Ahmadu I, Garba NA, Abubakar MS, Ibrahim UA, Gudaji M, Umar MU, et al. Quality of sleep among clinical medical students of Bayero university, Kano, Nigeria. Med J Dr DY Patil University. (2022) 15:524–8. doi: 10.4103/mjdrdypu.mjdrdypu_185_20
69. Awopeju O, Adewumi A, Adewumi A, Adeboye O, Adegboyega A, Adegbenro C, et al. (2020). Sleep Hygiene Awareness, Practice, and Sleep Quality Among Nigerian University Students. America: American Thoracic Society pp. A4136–A.
70. Seun-Fadipe CT, Mosaku KS. Sleep quality and academic performance among Nigerian undergraduate students. J Syst Integr Neurosci. (2017) 3:1–6. doi: 10.15761/JSIN.1000179
71. Zafar M, Omer EO, Hassan ME, Ansari K. Association of sleep disorder with academic performance among medical students in Sudan. Russian Open Med J. (2020) 9:208. doi: 10.15275/rusomj.2020.0208
72. Mirghani HO, Mohammed OS, Almurtadha YM, Ahmed MS. Good sleep quality is associated with better academic performance among Sudanese medical students. BMC Res notes. (2015) 8:1–5. doi: 10.1186/s13104-015-1712-9
73. Mahgoub AA, Mustafa SS. Correlation between physical activity, Sleep Components and Quality: in the Context of Type and Intensity: A Cross-Sectional study among Medical Students. (2022). doi: 10.21203/rs.3.rs-2061067/v1
74. Mohamed RA, Moustafa HA. Relationship between smartphone addiction and sleep quality among faculty of medicine students Suez Canal University, Egypt. Egyptian Family Med J. (2021) 5:105–15. doi: 10.21608/efmj.2021.27850.1024
75. Elwasify M, Barakat DH, Fawzy M, Elwasify M, Rashed I, Radwan DN. Quality of sleep in a sample of Egyptian medical students. Middle East Curr Psychiatry. (2016) 23:200–7. doi: 10.1097/01.XME.0000490933.67457.d4
76. Dongol E, Shaker K, Abbas A, Assar A, Abdelraoof M, Saady E, et al. Sleep quality, stress level and COVID-19 in university students; the forgotten dimension. Sleep Sci. (2022) 15:347. doi: 10.5935/1984-0063.20210011
77. Elsheikh AA, Elsharkawy SA, Ahmed DS. Impact of smartphone use at bedtime on sleep quality and academic activities among medical students at Al-Azhar University at Cairo. J Public Health. (2023), 1–10. doi: 10.1007/s10389-023-01964-8
78. Ahmed Salama A. Sleep Quality in Medical Students, Menoufia University, Egypt. Egyptian Family Med J. (2017) 1:1–21. doi: 10.21608/efmj.2017.67520
79. Gassara I, Ennaoui R, Halwani N, Turki M, Aloulou J, Amami O. Sleep quality among medical students. Eur Psychiatry. (2016) 33:S594. doi: 10.1016/j.eurpsy.2016.01.2216
80. Maalej M, Guirat M, Mejdoub Y, Omri S, Feki R, Zouari L, et al. Quality of sleep, anxiety and depression among medical students during exams period: a cross sectional study. J OF SLEEP Res. (2018).
81. Amamou B, Ben Saida I, Bejar M, Messaoudi D, Gaha L, Boussarsar M. Stress, anxiety, and depression among students at the Faculty of Medicine of Sousse (Tunisia). La Tunisie medicale. (2022) 100:346–52.
82. Saguem B, Nakhli J, Romdhane I, Nasr S. Predictors of sleep quality in medical students during COVID-19 confinement. L'encephale. (2022) 48:3–12. doi: 10.1016/j.encep.2021.03.001
83. Mvula JS, Muchindu YS, Kijai J. The Influence of Sleep Practices, Chronotype, and Life-Style Variables on Sleep Quality among Students at Rusangu University, Zambia. " forsch!"-Studentisches Online-Journal der Universität Oldenburg. (2021) 1:124–37.
84. Mwape RK, Mulenga D. Consumption of energy drinks and their effects on sleep quality among students at the Copperbelt University School of Medicine in Zambia. Sleep Disord. (2019) 2019. doi: 10.1155/2019/3434507
85. Hangouche AJE, Jniene A, Aboudrar S, Errguig L, Rkain H, Cherti M, et al. Relationship between poor quality sleep, excessive daytime sleepiness and low academic performance in medical students. Adv Med Educ Pract. (2018) 9:631–8. doi: 10.2147/AMEP.S162350
86. Jniene A, Errguig L, El Hangouche AJ, Rkain H, Aboudrar S, El Ftouh M, et al. Perception of sleep disturbances due to bedtime use of blue light-emitting devices and its impact on habits and sleep quality among young medical students. BioMed Res Int. (2019) 2019. doi: 10.1155/2019/7012350
87. Nsengimana A, Mugabo E, Niyonsenga J, Hategekimana JC, Biracyaza E, Mutarambirwa R, et al. Sleep quality among undergraduate medical students in Rwanda: a comparative study. Sci Rep. (2023) 13:265. doi: 10.1038/s41598-023-27573-9
88. El Sahly RA, Ahmed AM, Amer SEA, Alsaeiti KD. Assessment of insomnia and sleep quality among medical students-benghazi university: A cross-sectional study. Apollo Med. (2020) 17:73–7. doi: 10.4103/am.am_22_20
89. Leow MQH, Chiang J, Chua TJX, Wang S, Tan NC. The relationship between smartphone addiction and sleep among medical students: A systematic review and meta-analysis. PloS One. (2023) 18:e0290724. doi: 10.1371/journal.pone.0290724
90. Hwang E, Shin S. Prevalence of sleep disturbance in Korean university students: a systematic review and meta-analysis. Korean J Health Promotion. (2020) 20:49–57. doi: 10.15384/kjhp.2020.20.2.49
91. Limongi F, Siviero P, Trevisan C, Noale M, Catalani F, Ceolin C, et al. Changes in sleep quality and sleep disturbances in the general population from before to during the COVID-19 lockdown: A systematic review and meta-analysis. Front Psychiatry. (2023) 14:1166815. doi: 10.3389/fpsyt.2023.1166815
92. Dunn C, Goodman O, Szklo-Coxe M. Sleep duration, sleep quality, excessive daytime sleepiness, and chronotype in university students in India: A systematic review. J Health Soc Sci. (2022) 7. doi: 10.19204/2022/SLPD3
93. Seoane HA, Moschetto L, Orliacq F, Orliacq J, Serrano E, Cazenave MI, et al. Sleep disruption in medicine students and its relationship with impaired academic performance: a systematic review and meta-analysis. Sleep Med Rev. (2020) 53:101333. doi: 10.1016/j.smrv.2020.101333
94. Rao W-W, Li W, Qi H, Hong L, Chen C, Li C-Y, et al. Sleep quality in medical students: a comprehensive meta-analysis of observational studies. Sleep Breathing. (2020) 24:1151–65. doi: 10.1007/s11325-020-02020-5
95. Pengpid S, Peltzer K. Fruit and vegetable consumption is protective from short sleep and poor sleep quality among university students from 28 countries. Nat Sci sleep. (2020) 12:627–33. doi: 10.2147/NSS.S263922
96. Manzar MD, Bekele BB, Noohu MM, Salahuddin M, Albougami A, Spence DW, et al. Prevalence of poor sleep quality in the Ethiopian population: a systematic review and meta-analysis. Sleep Breathing. (2020) 24:709–16. doi: 10.1007/s11325-019-01871-x
97. Pacheco JP, Giacomin HT, Tam WW, Ribeiro TB, Arab C, Bezerra IM, et al. Mental health problems among medical students in Brazil: a systematic review and meta-analysis. Braz J Psychiatry. (2017) 39:369–78. doi: 10.1590/1516-4446-2017-2223
98. Li L, Wang YY, Wang SB, Zhang L, Li L, Xu DD, et al. Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. Journal of Sleep Research (2018) 27. doi: 10.1111/jsr.12648
99. Hagedorn RL, Olfert MD, MacNell L, Houghtaling B, Hood LB, Roskos MRS, et al. College student sleep quality and mental and physical health are associated with food insecurity in a multi-campus study. Public Health Nutr. (2021) 24:4305–12. doi: 10.1017/S1368980021001191
100. Das-Friebel A, Lenneis A, Realo A, Sanborn A, Tang NK, Wolke D, et al. Bedtime social media use, sleep, and affective wellbeing in young adults: an experience sampling study. J Child Psychol Psychiatry. (2020) 61:1138–49. doi: 10.1111/jcpp.13326
101. Semelka M, Wilson J, Floyd R. Diagnosis and treatment of obstructive sleep apnea in adults. Am Family physician. (2016) 94:355–60.
102. Uccella S, Cordani R, Salfi F, Gorgoni M, Scarpelli S, Gemignani A, et al. Sleep deprivation and insomnia in adolescence: implications for mental health. Brain Sci. (2023) 13:569. doi: 10.3390/brainsci13040569
103. Kingsbury JH, Buxton OM, Emmons KM, Redline S. Sleep and its relationship to racial and ethnic disparities in cardiovascular disease. Curr Cardiovasc Risk Rep. (2013) 7:387–94. doi: 10.1007/s12170-013-0330-0
104. Johnson DA, Jackson CL, Williams NJ, Alcántara C. Are sleep patterns influenced by race/ethnicity–a marker of relative advantage or disadvantage? Evidence to date. Nat Sci sleep. (2019) 11:79–95. doi: 10.2147/NSS.S169312
105. Adenekan B, Pandey A, McKenzie S, Zizi F, Casimir GJ, Jean-Louis G. Sleep in America: role of racial/ethnic differences. Sleep Med Rev. (2013) 17:255–62. doi: 10.1016/j.smrv.2012.07.002
106. Bhatia G, Patterson N, Pasaniuc B, Zaitlen N, Genovese G, Pollack S, et al. Genome-wide comparison of African-ancestry populations from CARe and other cohorts reveals signals of natural selection. Am J Hum Genet. (2011) 89:368–81. doi: 10.1016/j.ajhg.2011.07.025
107. Arnardottir ES, Nikonova EV, Shockley KR, Podtelezhnikov AA, Anafi RC, Tanis KQ, et al. Blood-gene expression reveals reduced circadian rhythmicity in individuals resistant to sleep deprivation. Sleep. (2014) 37:1589–600. doi: 10.5665/sleep.4064
108. Krueger JM. The role of cytokines in sleep regulation. Curr Pharm design. (2008) 14:3408–16. doi: 10.2174/138161208786549281
109. Grandner MA, Buxton OM, Jackson N, Sands-Lincoln M, Pandey A, Jean-Louis G. Extreme sleep durations and increased C-reactive protein: effects of sex and ethnoracial group. Sleep. (2013) 36:769–79. doi: 10.5665/sleep.2646
110. Christian LM, Glaser R, Porter K, Iams JD. Stress-induced inflammatory responses in women: effects of race and pregnancy. Psychosomatic Med. (2013) 75:658. doi: 10.1097/PSY.0b013e31829bbc89
111. BaHammam AS. Sleep medicine in Saudi Arabia: Current problems and future challenges. Ann Thorac Med. (2011) 6:3–10. doi: 10.4103/1817-1737.74269
112. Komolafe MA, Sanusi AA, Idowu AO, Balogun SA, Olorunmonteni OE, Adebowale AA, et al. Sleep medicine in Africa: past, present, and future. J Clin Sleep Med. (2021) 17:1317–21. doi: 10.5664/jcsm.9218
113. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
114. Romero-Blanco C, Rodríguez-Almagro J, Onieva-Zafra MD, Parra-Fernández ML, Prado-Laguna M, Hernández-Martínez A. Sleep pattern changes in nursing students during the COVID-19 lockdown. Int J Environ Res Public Health. (2020) 17:5222. doi: 10.3390/ijerph17145222
115. Mandelkorn U, Genzer S, Choshen-Hillel S, Reiter J, Meira e Cruz M, Hochner H, et al. Escalation of sleep disturbances amid the COVID-19 pandemic: a cross-sectional international study. J Clin Sleep Med. (2021) 17:45–53. doi: 10.5664/jcsm.8800
116. Zhang Y, Zhang H, Ma X, Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int J Environ Res Public Health. (2020) 17:3722. doi: 10.3390/ijerph17103722
117. Shi L, Lu Z-A, Que J-Y, Huang X-L, Liu L, Ran M-S, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA network Open. (2020) 3:e2014053–e. doi: 10.1001/jamanetworkopen.2020.14053
118. Amaral AP, Soares MJ, Pinto AM, Pereira AT, Madeira N, Bos SC, et al. Sleep difficulties in college students: The role of stress, affect and cognitive processes. Psychiatry Res. (2018) 260:331–7. doi: 10.1016/j.psychres.2017.11.072
119. Wear D. “Face-to-face with it”: medical students' narratives about their end-of-life education. Acad Med. (2002) 77:271–7. doi: 10.1097/00001888-200204000-00003
120. Garett R, Liu S, Young SD. A longitudinal analysis of stress among incoming college freshmen. J Am Coll Health. (2017) 65:331–8. doi: 10.1080/07448481.2017.1312413
121. Kim E-J, Dimsdale JE. The effect of psychosocial stress on sleep: a review of polysomnographic evidence. Behav sleep Med. (2007) 5:256–78. doi: 10.1080/15402000701557383
122. Almojali AI, Almalki SA, Alothman AS, Masuadi EM, Alaqeel MK. The prevalence and association of stress with sleep quality among medical students. J Epidemiol Global Health. (2017) 7:169–74. doi: 10.1016/j.jegh.2017.04.005
123. Li H-J, Hou X-H, Liu H-H, Yue C-L, Lu G-M, Zuo X-N. Putting age-related task activation into large-scale brain networks: a meta-analysis of 114 fMRI studies on healthy aging. Neurosci Biobehav Rev. (2015) 57:156–74. doi: 10.1016/j.neubiorev.2015.08.013
124. Bartel KA, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Med Rev. (2015) 21:72–85. doi: 10.1016/j.smrv.2014.08.002
125. Short MA, Gradisar M, Lack LC, Wright HR, Dohnt H. The sleep patterns and well-being of Australian adolescents. J adolescence. (2013) 36:103–10. doi: 10.1016/j.adolescence.2012.09.008
126. Zhang L, Li D, Yin H. How is psychological stress linked to sleep quality? The mediating role of functional connectivity between the sensory/somatomotor network and the cingulo-opercular control network. Brain Cognition. (2020) 146:105641. doi: 10.1016/j.bandc.2020.105641
127. Siddiqui AF, Al-Musa H, Al-Amri H, Al-Qahtani A, Al-Shahrani M, Al-Qahtani M. Sleep patterns and predictors of poor sleep quality among medical students in King Khalid University, Saudi Arabia. Malaysian J Med sciences: MJMS. (2016) 23:94. doi: 10.21315/mjms2016.23.6.10
128. Kobbaz TM, Bittencourt LA, Pedrosa BV, Fernandes B, Marcelino LD, Pires de Freitas B, et al. The lifestyle of Brazilian medical students: What changed and how it protected their emotional wellbeing during the COVID-19 pandemic. Aust J Gen Practice. (2021) 50:668–72. doi: 10.31128/AJGP-03-21-5886
129. Eleftheriou A, Rokou A, Arvaniti A, Nena E, Steiropoulos P. Sleep quality and mental health of medical students in Greece during the COVID-19 pandemic. Front Public Health. (2021) 9:775374. doi: 10.3389/fpubh.2021.775374
130. Xie J, Li X, Luo H, He L, Bai Y, Zheng F, et al. Depressive symptoms, sleep quality and diet during the 2019 novel coronavirus epidemic in China: a survey of medical students. Front Public Health. (2021) 8:588578. doi: 10.3389/fpubh.2020.588578
131. Tsai L-L, Li S-P. Sleep patterns in college students: Gender and grade differences. J psychosomatic Res. (2004) 56:231–7. doi: 10.1016/S0022-3999(03)00507-5
132. Chick CF, Singh A, Anker LA, Buck C, Kawai M, Gould C, et al. A school-based health and mindfulness curriculum improves children’s objectively measured sleep: a prospective observational cohort study. J Clin Sleep Med. (2022) 18:2261–71. doi: 10.5664/jcsm.9508
133. Yang J, Fu X, Liao X, Li Y. Association of problematic smartphone use with poor sleep quality, depression, and anxiety: A systematic review and meta-analysis. Psychiatry Res. (2020) 284:112686. doi: 10.1016/j.psychres.2019.112686
134. Mei X, Zhou Q, Li X, Jing P, Wang X, Hu Z. Sleep problems in excessive technology use among adolescent: a systemic review and meta-analysis. Sleep Sci practice. (2018) 2:1–10. doi: 10.1186/s41606-018-0028-9
135. Hershner SD, Chervin RD. Causes and consequences of sleepiness among college students. Nat Sci sleep. (2014) 6:73–84. doi: 10.2147/NSS.S62907
136. Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. (2007) 8:602–12. doi: 10.1016/j.sleep.2006.12.002
137. Figueiro MG, Bierman A, Plitnick B, Rea MS. Preliminary evidence that both blue and red light can induce alertness at night. BMC Neurosci. (2009) 10:1–11. doi: 10.1186/1471-2202-10-105
138. Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. (2010) 11:735–42. doi: 10.1016/j.sleep.2010.02.006
139. Tarokh L, Raffray T, Van Reen E, Carskadon MA. Physiology of normal sleep in adolescents. Adolesc medicine: state art Rev. (2010) 21:401–17, vii. doi: 10.1542/9781581105803-physiology
140. Demirci K, Akgönül M, Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav addictions. (2015) 4:85–92. doi: 10.1556/2006.4.2015.010
141. Tamura H, Nishida T, Tsuji A, Sakakibara H. Association between excessive use of mobile phone and insomnia and depression among Japanese adolescents. Int J Environ Res Public Health. (2017) 14:701. doi: 10.3390/ijerph14070701
142. Heo J-Y, Kim K, Fava M, Mischoulon D, Papakostas GI, Kim M-J, et al. Effects of smartphone use with and without blue light at night in healthy adults: A randomized, double-blind, cross-over, placebo-controlled comparison. J Psychiatr Res. (2017) 87:61–70. doi: 10.1016/j.jpsychires.2016.12.010
143. Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. J psychosomatic Res. (2004) 56:497–502. doi: 10.1016/j.jpsychores.2004.02.010
144. Hyyppä MT, Kronholm E. Quality of sleep and chronic illnesses. J Clin Epidemiol. (1989) 42:633–8. doi: 10.1016/0895-4356(89)90006-1
Keywords: sleep quality, university students, systematic review, meta-analysis, Africa
Citation: Nakie G, Takelle GM, Rtbey G, Andualem F, Tinsae T, Kassa MA, Tadesse G, Fentahun S, Wassie YA, Segon T, Kibralew G and Melkam M (2024) Sleep quality and associated factors among university students in Africa: a systematic review and meta-analysis study. Front. Psychiatry 15:1370757. doi: 10.3389/fpsyt.2024.1370757
Received: 15 January 2024; Accepted: 27 February 2024;
Published: 11 March 2024.
Edited by:
Guanhu Yang, Ohio University, United StatesReviewed by:
Jemal Seid, Wollo University, EthiopiaXingfang Liu, Swiss University of Traditional Chinese Medicine, Switzerland
Copyright © 2024 Nakie, Takelle, Rtbey, Andualem, Tinsae, Kassa, Tadesse, Fentahun, Wassie, Segon, Kibralew and Melkam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Girum Nakie, Z2lydW1uYWtpZUBnbWFpbC5jb20=
 Girum Nakie
Girum Nakie Girmaw Medfu Takelle
Girmaw Medfu Takelle Gidey Rtbey
Gidey Rtbey Fantahun Andualem
Fantahun Andualem Techilo Tinsae
Techilo Tinsae Mulat Awoke Kassa
Mulat Awoke Kassa Gebresilassie Tadesse
Gebresilassie Tadesse Setegn Fentahun
Setegn Fentahun Yilkal Abebaw Wassie
Yilkal Abebaw Wassie Tesfaye Segon5
Tesfaye Segon5 Getasew Kibralew
Getasew Kibralew Mamaru Melkam
Mamaru Melkam