- 1Nursing Department, The Second Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China
- 2Rehabilitation Department, The Second Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China
- 3Anesthesiology Department, The Second Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China
- 4Ear, Nose, Throat, Head and Neck Surgery, The Second Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China
- 5Party Committee Office, The Second Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China
Objective: The purpose of this study was to understand the relationship between the multiple chronic conditions (MCC), mental health and cognitive function of older adults in the community, and to propose a hypothesis that depressive symptom mediate the number of chronic diseases and cognitive impairment in older adults.
Method: Participants aged 65 years and older from 35 communities in 14 cities in Guangxi, China were recruited. The residents’ depressive symptom (PHQ-9) and cognitive status (AD-8) were evaluated, Chi-square test was used to explore the effects of different socio-demographic characteristics on depressive symptom and cognitive impairment. Pearson correlation analysis and the process model 4 were used to explore the relationship between the number of chronic diseases, depressive symptom and cognitive impairment.
Result: A total of 11,582 older adults were included in our analysis. The rate of MCC reaching 26.53%. Hypertension combined with diabetes accounts for the highest proportion of two chronic diseases (13.2%). Among the combination of three chronic diseases, the highest incidence of coexisting hypertension combined with cervical/lumbar spondylosis, and rheumatoid arthritis (7.1%). In this study, depression symptoms accounted for 12.9% of older adults aged 65 and above, and cognitive impairment accounted for 27.4%. Female, older age, reside in urban areas, lower educational levels, no spouse, live alone, and MCC were risk factors for depressive symptom and cognitive impairment in older adults (P<0.05). Depressive symptom had a mediating effect in the number of chronic diseases and cognitive impairment, and the mediating effect (1.109) accounted for 44.13% of the total effect (0.247).
Conclusion: The mental health of the older adult needs to be taken seriously, and improving depressive symptom can reduce the occurrence of cognitive impairment in older patients with MCC to a certain extent.
1 Introduction
With the deepening of aging society, cognitive impairment has become a silent epidemic among the older adult. The fight against Alzheimer’s disease (AD) is considered a public health priority by the World Health Organization (WHO) (1). As of 2019, there are at least 50 million AD patients worldwide, and it is expected to reach 152 million by 2050, while China will reach 28.98 million (2). Mild cognitive impairment (MCI) is a cognitive stage between normal cognition and dementia, and is the primary sign of cognitive change. Its further development will significantly increase the risk of AD and other dementia, and gradually evolve into functional disorders and irreversible severe cognitive damage (3). Changes in cognitive function in the older adult will have a huge impact on their quality of life and family burden, and also pose an increasingly large challenge to healthcare systems worldwide (4, 5). It is urgent to screen the older adult for cognitive impairment in the community and design targeted early intervention programs.
One-third of AD cases worldwide can be attributed to potentially modifiable risk factors. There is Level 1 evidence that depressive symptom can significantly increase the risk of AD (6). And the conversion rate from MCI patients with depressive symptom to AD (31.0%) is significantly higher than that of MCI patients without depressive symptom (13.5%) (7). Long-term use of certain antidepressants such as anticholinergic drugs may also increase the risk of AD (8). In addition, the severity of cognitive impairment was positively correlated with the frequency of depression in a dose-response relationship (9). Studies have shown that older MCI patients are often accompanied by symptoms of depression, which is also an important reason for the decline in their quality of life, and it is necessary to pay attention to the synergistic intervention of the two (10).
Currently, medical services for the older adult are shifting from a disease-centered single-disease model to a patient-centered multi-disease model. How to improve the quality of life of older adult patients with MCC is a major issue in the aging society (11). Multiple chronic conditions (MCC) mean that one patient has two or more chronic diseases (12), and the prevalence rate of MCC among the older adult in China is 65.14% (13). Compared with a single chronic disease, patients with MCC have a rapid decline in physical function, a continuous decline in quality of life, including a 94% increased risk of functional limitation and a 73% increased risk of death (14). Research shows that MCC such as hypertension, diabetes, and chronic kidney disease have common etiological mechanisms such as vascular and metabolic factors, which increases the risk of cognitive impairment (15, 16), indicating that there may be synergy between various chronic diseases on the impact of cognitive function. It is particularly important to explore the common type of chronic diseases among older adults living in the community and further study the co-pathogenesis of MCC and cognitive impairment.
Existing research has mainly focused on exploring the cognitive function of specific chronic disease patients, while overlooking the impact of MCC on cognition. Although some scholars have demonstrated a close relationship between cognitive function and depressive symptom, the combined effect of MCC and depressive symptom on cognition has not been considered. The influence of older adult’s mental health on the relationship between the coexistence of multiple chronic diseases and cognitive impairment remains is unclear. Our study hypothesizes that depressive symptom may mediate the number of chronic diseases and cognitive dysfunction in the older adult. Based on the perspective of cognitive impairment in older adults with MCC, we seek to provide a reference for the development of targeted, multidisciplinary comprehensive prevention and management measures.
2 Materials and methods
2.1 Sample
This study is a cross-sectional study that recruited older adults at 35 community and village committee health centers in 14 cities in Guangxi, China, from March to October 2023. Health examinations and questionnaire surveys were conducted, and some objective information was provided by their primary caregivers. The eligible samples for inclusion were (1) 65 years old and older, (2) resident population living in the sampled community. And exclusion criteria were (1) the presence of conditions affecting the assessment, such as congenital or acquired developmental delays, corrected vision/hearing abnormalities, (2) did not complete all investigations and withdrew midway. All data were evaluated and collected by health professionals who have undergone unified training. A total of 12769 older adult’s health data were collected. All information is entered into the database through the electronic questionnaire system. During data cleaning, we excluded objects with missing data in three categories: chronic disease status, depressive symptom and cognitive function. Finally, a total of 11582 participants (90.7%) were included in this study for analysis. This study was approved by the Research Ethics Committee of the Second Affiliated Hospital of Guangxi Medical University (No. 2023-KY0905) and received informed consent from all participants.
2.2 Data measurement
2.2.1 Measurement of chronic diseases
Data on chronic diseases were obtained through the following question: “Have you ever been informed by a doctor or other healthcare professional that you have the following chronic diseases?” Older adults and their caregivers answered yes or no. The list of chronic diseases was designed based on the 10th revision of the International Classification of Disease, 10th Revision (ICD-10). According to previous epidemiological research and prevalence rates (17), we selected the following 20 chronic diseases and symptoms: hypertension, heart disease/coronary heart disease, diabetes, cerebrovascular disease, chronic bronchitis, cancer, kidney disease, liver disease, gastroenteritis or other digestive diseases, tuberculosis, rheumatoid arthritis, cervical/lumbar spondylosis, reproductive system diseases, prostate disease, urinary system diseases, glaucoma or cataracts, osteoporosis, emotional and mental problems, neurological diseases, and hearing loss. If any one of these diseases was diagnosed by a hospital, the participant was defined as having a chronic disease. Those with two or more chronic diseases were considered as having MCC, while those with less than 2 chronic diseases were considered as non-MCC patients (18).
2.2.2 Measurement of depressive symptom
The Patient Health Questionnaire-9 (PHQ-9) is an effective scale for assessing depressive symptom based on the Diagnostic and Statistical Manual of Mental Disorders (DSM)-V. It measures participants’ depressive symptom over the past two weeks and scores 9 items from 0 (not at all) to 3 (nearly every day), with a total score of 27. A score of ≥5 indicates the presence of depressive symptom (19).
2.2.3 Measurement of mild cognitive impairment
We use the Ascertain dementia-8 (AD-8) to measure cognitive function in the older adult and invited their primary caregivers to fill out this questionnaire. The AD-8 is a simple and rapid screening tool that is sensitive to early cognitive changes in many common dementia diseases (20). The AD-8 includes eight items that evaluate the judgment, daily living ability, initiative, orientation, and memory, and each item is scored as 0 or 1. The total score of the AD-8 ranges from 0 to 8, with higher scores indicating greater cognitive impairment. A score of ≥2 indicates the possible presence of cognitive impairment (21).
2.3 Statistical analysis
All analyses were conducted using SPSS 23. Measurement data is expressed as mean and standard deviation, while count data is expressed as frequency and percentage. The Chi-square test was used to explore the effects of different socio-demographic characteristics on depressive symptom and cognitive impairment. Pearson correlation coefficient was used to conduct bivariate correlation analysis, and Model 4 in the Process program was used to examine the mediating role of depressive symptom between the number of chronic diseases and cognitive function in the older adult. Significance tests were two-tailed with a significance level of 0.05. Bootstrapping was used for significance testing for the mediation analysis.
3 Results
3.1 Characteristics of study population
A total of 11582 participants were included in analysis with the age of 65 and over. Among them, there are 5118 males (44.2%) and 6464 females (55.8%). The mean age was (73.74 ± 6.87) years old. There are 6223 (53.7%) residing in urban areas and 5359 (46.3%) residing in rural areas. The average length of schooling was (5.19 ± 3.92) years. More than half of participants have a spouse (68.7%) and a small percentage (8.4%) are living alone.
3.2 Common type of MCC in the older adults
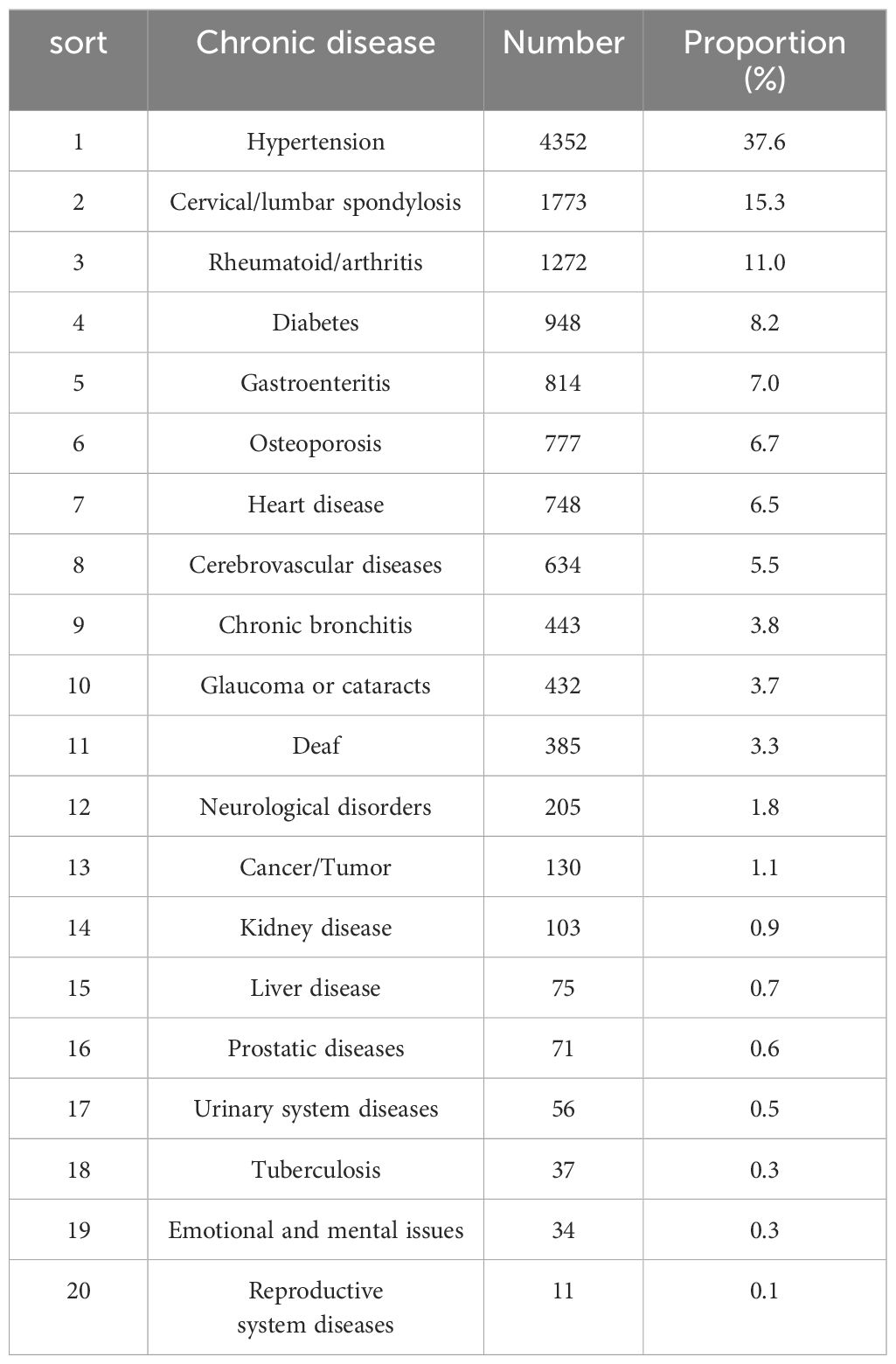
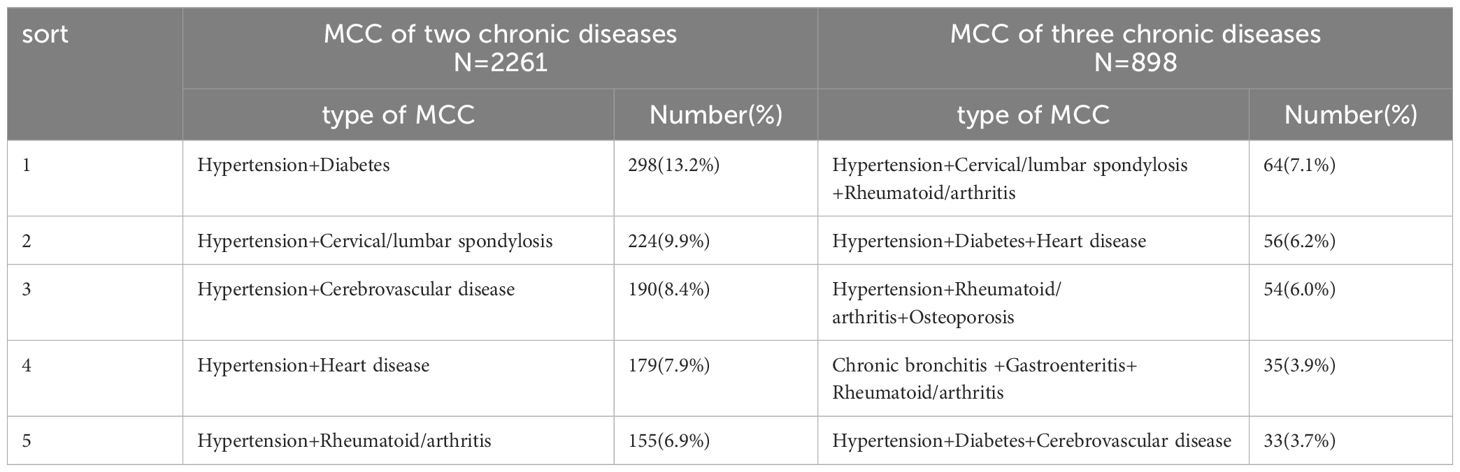
Among the 20 chronic diseases surveyed, the top three with the highest prevalence were hypertension (37.6%), cervical/lumbar spondylosis (15.3%), and rheumatoid arthritis/joint disease (11.0%), while the remaining 17 were all below 10% (Table 1). The incidence rate of MCC was 26.53%, with the number of older adults suffering from 0, 1, 2, 3, and more than 4 chronic diseases were 3677 (31.7%), 4332 (37.4%), 2261 (19.5%), 898 (7.8%), and 414 (3.6%), respectively. Among the combinations of chronic diseases, there were 138 types of two chronic diseases, the three combinations with the highest proportion were hypertension with diabetes (13.2%), hypertension with cervical/lumbar spondylosis (9.9%), and hypertension with cerebrovascular disease (8.4%). It’s worth noting that the top five all contain hypertension. There were 192 types of three chronic diseases, with the highest prevalence combination were hypertension combined with cervical/lumbar spondylosis and rheumatoid arthritis/joint disease (7.1%), hypertension combined with diabetes and heart disease (6.2%) (Table 2).
3.3 The prevalence and influencing factors of depressive symptom and cognitive impairment in older adults
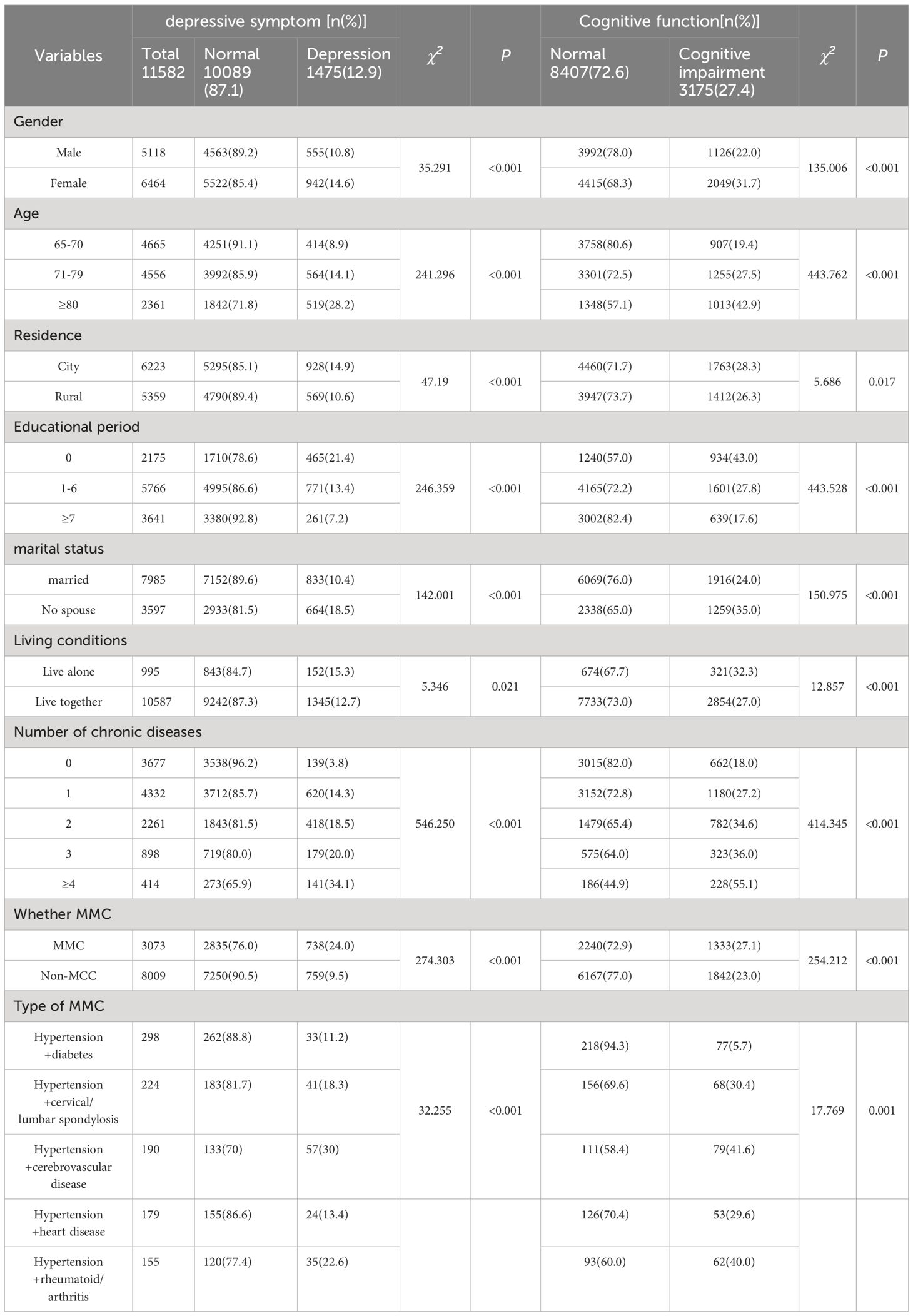
In this study, depressive symptom accounted for 12.9% of older adults aged 65 and above, and cognitive impairment accounted for 27.4%. In the univariate analysis, female, older age, reside in urban areas, lower educational levels, no spouse, live alone, and MCC were risk factors for depressive symptom and cognitive impairment, and the difference is statistically significant (p < 0.05) (Table 3).
3.4 Correlation of the number of chronic diseases, depressive symptom and cognitive impairment in the older adult
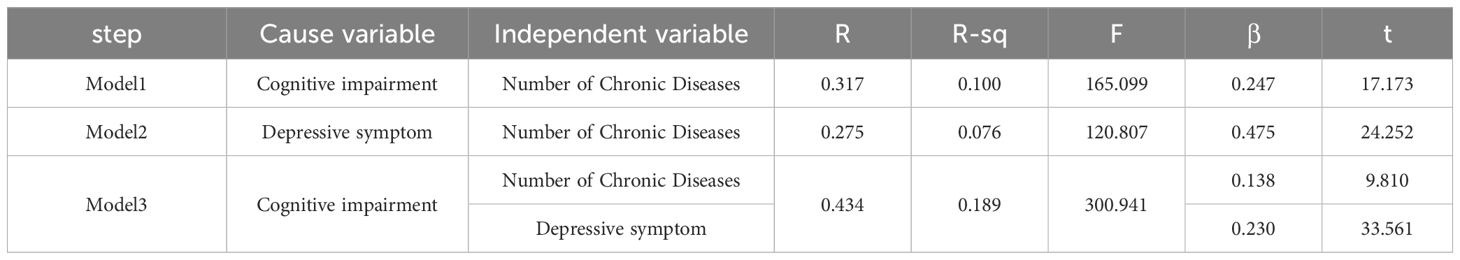
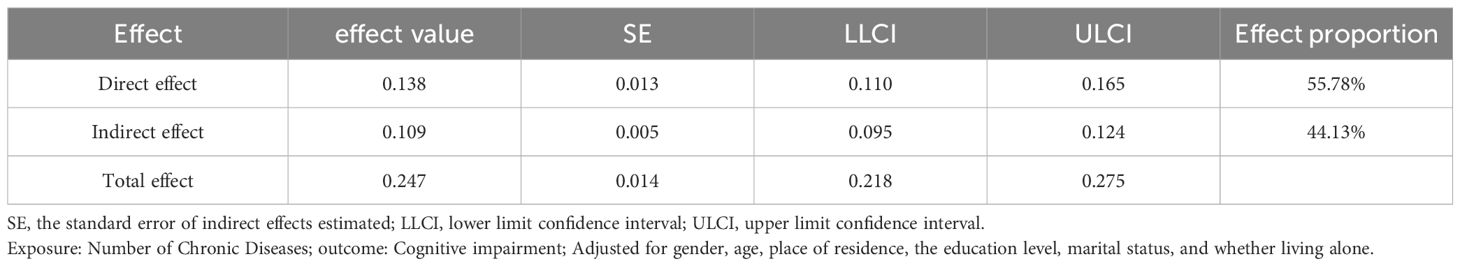
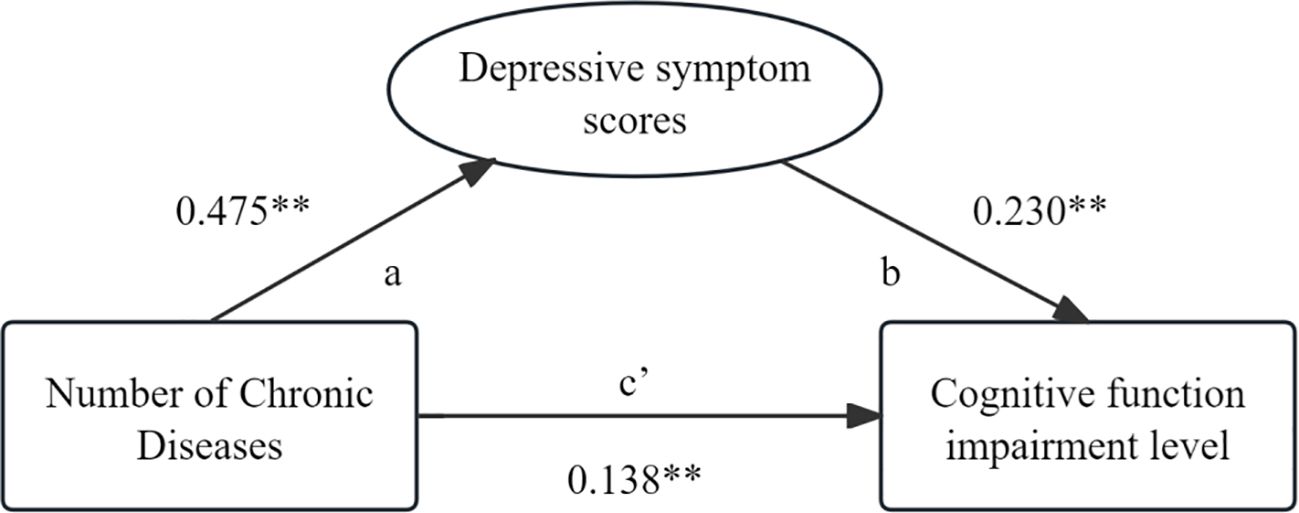
The statistical analysis result shows that the number of chronic diseases is positively correlated with depressive symptom and cognitive function (p<0.05), and depressive symptom are also positively correlated with cognitive impairment (p<0.05) Table 4. After controlling for six variables that have an impact on cognitive impairment, including gender, age, place of residence, the education level, marital status, and whether living alone, a three-step test was conducted to examine the mediating effect of depressive symptom between the number of chronic diseases and cognitive impairment. In Model 1 test, the number of chronic diseases had a significant predictive effect on cognitive impairment(β=0.247, p<0.001) indicates that the total effect is valid. In the test of Model 2, the number of chronic diseases has a significant impact on depressive symptom(β=0.475, p<0.001) indicates that path a is valid. Finally, in the Model 3 test, after controlling for the influence of the mediating variable (depressive symptom), the number of chronic diseases had a significant direct effect on cognitive function (β=0.138, p<0.001), indicating that path c’ was effective. After controlling for the effect of the number of chronic diseases, the mediating variable (depressive symptom) had a significant effect on cognitive impairment (β=0.230, p<0.001), suggesting that path b was effective (Table 5). In conclusion, the mediating effect of depressive symptom between the number of chronic diseases and the impairment of cognitive function are established, and the mediating effect (0.109) accounted for 44.13% of the total effect (0.247) (Table 6; Figure 1).
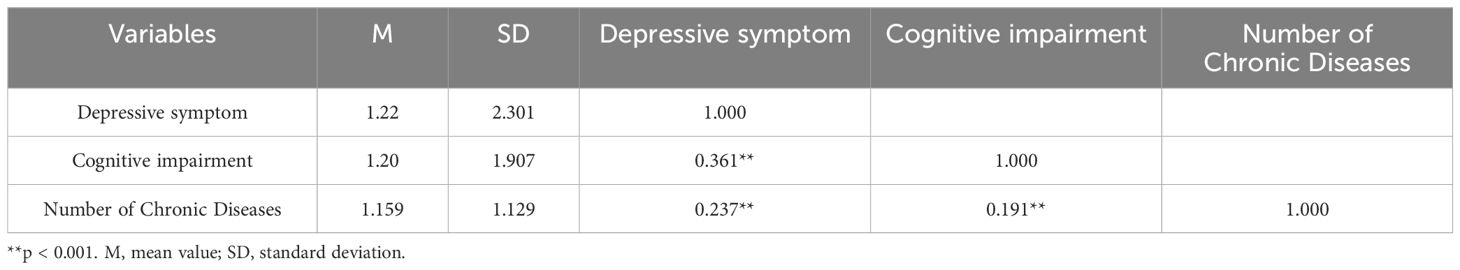
Table 4 The correlation between number of chronic diseases, depressive symptom and cognitive impairment.
4 Discussion
In this survey, in addition to the most commonly occurring hypertension, musculoskeletal diseases (neck/lumbar spine disease, rheumatoid arthritis/arthritis, osteoporosis) were reported the most. These diseases are closely related to physical activity and can cause significant difficulties in the daily life of the older adults (22). In future research, more attention should be paid to chronic damage to the skeletal muscles of the older adult and the development of exercise rehabilitation plans to alleviate pain. In the type of MCC, older adults with hypertension combined with cerebrovascular disease have the highest proportion of depressive symptom and cognitive impairment, followed by hypertension combined with rheumatoid arthritis. The reason may be that patients with cerebrovascular diseases and musculoskeletal diseases have to constantly endure the pain caused by the disease in their daily activities. If it worsens, they also face a high risk of disability. The accumulation of stress and emotions can worsen the patient’s mental health (23). The changes in cerebral blood vessels and inflammatory factors are both potential mechanisms for cognitive impairment (24). Meanwhile, the ranking of depressive symptom and cognitive impairment in each type of MCC is basically the same, which lays a foundation for the hypothesis made in this study.
There is a significant correlation between the number of chronic diseases, depressive symptom, and cognitive impairment in the older adult, and depressive symptom partially mediates the relationship between the number of chronic diseases and cognitive impairment. The coexistence of multiple chronic diseases can accelerate the functional decline of various systems in the body, leading to a sustained state of chronic consumption, which reduces the body’s resistance and tolerance to the external environment (25, 26). Moreover, the long-term evolution of diseases can cause damage to the body’s vessels and nerves, leading to a decline in cognitive function (27). The results of this study showed that the higher number of chronic diseases, the higher incidence of depression, which is consistent with a longitudinal study of older adults in China, and shows a dose-response relationship (28). Studies have shown that the potential pathogenesis of cognitive decline, such as non-physiological in aging, cerebrovascular disease, and leukoaraiosis, is related to the pathogenesis of depression (29–31). Ruan (32)suggested that depression can cause the body to produce various chronic inflammatory factors, which through the blood-brain barrier cause an increase in amyloid precursor proteins in the brain, leading to a decline in cognitive function. And there is data to suggest that depression still exists on the devastating role of on basic cognitive capacities in older adults without other comorbid disorders (33). To sum up, the hypothesis of this study is valid and can be explained. Due to the survey targeting older adults in the community, comorbidity index was not calculated, and the impact of comorbidity severity on depressive symptom could not be determined. In summary, older adults with MCC are plagued by various diseases and complications for a long time. Persistent physical symptoms combined with reduced social participation have a negative impact on their mental health (34). Adverse emotions such as depression can reduce the subjective memory and cognitive flexibility of the older adult, leading to cognitive changes (35).
Therefore, older adults healthcare workers should not only treat the disease itself, but also pay more attention to the psychological state of patients to reduce the occurrence of cognitive impairment. The factors related to depressive symptom in this study showed that female, advanced age, low education, and no spouse were risk factors. Similar to previous research results (36, 37), it suggests that we should fully consider the impact of different age groups on psychological distress (38) and take proactive and effective measures for precise intervention. Targeted health education should be provided during free clinics or physical examinations for the older adult to improve their health literacy and compensate for the psychological impact of low education (39). Encourage older adults to actively participate in social activities and help them build a positive social support network. In this study, the detection of depressive symptom in older adults living in urban areas was higher than in rural areas, which is inconsistent with previous studies (40). The reason may be that rural older adults have been in a relatively difficult environment for a long time, are more easily satisfied with themselves and the environment, have strong independence and autonomy, which may enhance their psychological resilience and adaptability, thereby reducing psychological distress (41).
Finally, this study has certain limitations. As is well known, cognitive symptoms are associated with some clinical variables, such as the disease course, acute onset, or remission period, at the same time the proportion of chronic disease types may also have an impact on the outcome of the mediating effect, but unfortunately, we did not consider these factors. Therefore, research should be conducted on the impact of the severity of MCC on depressive symptom and cognitive impairment to further confirm these findings. Secondly, this study adopts a cross-sectional design and only analyzes the mediating effect of the occurrence of cognitive impairment in the older adult, without elaborating the causal relationship. Finally, because this study was conducted in the community through interviews, older adult’s memories of diseases may not be comprehensive enough, resulting in recall bias. And the assessment of depression and cognitive impairment may be subjective by investigators, which may affect the accuracy of the data. In the future, further related intermediary studies can be conducted in hospitals on older adults with MCC.
5 Conclusions
It is challenging for older adults with MCC to implement cognitive interventions considering multiple chronic diseases at the same time. It is necessary to identify modifiable intermediate variables for secondary prevention in order to reduce or delay the onset of cognitive impairment. Our study found that depressive symptom has a mediating effect between the number of chronic diseases and cognitive impairment. Therefore, focusing on the mental health of older adults can reduce the occurrence of cognitive impairment in MCC old adults. In the process of policy implementation, cognitive impairment screening should be coordinated with chronic disease management, emphasizing the prevention and intervention of cognitive related diseases, and promoting the development of healthy aging.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Second Affiliated Hospital of Guangxi Medical University Ethical Review Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. The manuscript presents research on animals that do not require ethical approval for their study.
Author contributions
L-CL: Writing – original draft, Investigation. DMH: Data curation, Writing – original draft. JP: Investigation, Writing – original draft. X-YC: Investigation, Writing – original draft. X-LF: Investigation, Writing – original draft. P-YT: Formal analysis, Writing – review & editing. XP: Formal analysis, Writing – review & editing. Q-NP: Methodology, Writing – review & editing. D-JF: Methodology, Writing – review & editing. S-YL: Methodology, Writing – original draft. C-LL: Writing – review & editing. Y-FP: Writing – review & editing. P-XD: Investigation, Writing – original draft. Y-DC: Investigation, Writing – original draft. P-H: Investigation, Writing – original draft. H-CW: Investigation, Writing – original draft. H-QH: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Guangxi Philosophy and Social Science Research Project (22FRK004), Guangxi Medical University Youth Science Fund Project (GXMUYSF202379), Self-funded project by Guangxi Health Commission (Z-A20230629), Self-funded project by Guangxi Health Commission (Z-A20220653).
Acknowledgments
The authors would like to thank all the older adults who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mehra A, Suri V, Kumari S, Avasthi A, Grover S. Association of mild cognitive impairment and metabolic syndrome in patients with hypertension. Asian J Psychiatr. (2020) 53:102185. doi: 10.1016/j.ajp.2020.102185
2. Zhu Z, Zheng Z, Zhou C, Cao L, Zhao G. Trends in prevalence and disability-adjusted life-years of alzheimer's disease and other dementias in China from 1990 to 2019. Neuroepidemiology. (2023) 57:206–17. doi: 10.1159/000530593
3. Qin Y, Han H, Li Y, Cui J, Jia H, Ge X, et al. Estimating bidirectional transitions and identifying predictors of mild cognitive impairment. Neurology. (2023) 100:e297–307. doi: 10.1212/WNL.0000000000201386
4. GBD 2016 Dementia Collaborators. Global, regional, and national burden of Alzheimer's disease and other dementias, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. (2019) 18:88–106. doi: 10.1016/S1474-4422(18)30403-4
5. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
6. Xu W, Tan L, Wang HF, Jiang T, Tan MS, Tan L, et al. Meta-analysis of modifiable risk factors for Alzheimer's disease. J Neurol Neurosurg Psychiatry. (2015) 86:1299–306. doi: 10.1136/jnnp-2015-310548
7. Ma L. Depression, anxiety, and apathy in mild cognitive impairment: current perspectives. Front Aging Neurosci. (2020) 12:9. doi: 10.3389/fnagi.2020.00009
8. Jacob L, Bohlken J, Kostev K. Risk of dementia in German patients treated with antidepressants in general or psychiatric practices. Int J Clin Pharmacol Ther. (2017) 55:322–8. doi: 10.5414/CP202754
9. Kriesche D, Woll C, Tschentscher N, Engel RR, Karch S. Neurocognitive deficits in depression: a systematic review of cognitive impairment in the acute and remitted state. Eur Arch Psychiatry Clin Neurosci. (2023) 273:1105–28. doi: 10.1007/s00406-022-01479-5
10. Stites SD, Karlawish J, Harkins K, Rubright JD, Wolk D. Awareness of mild cognitive impairment and mild alzheimer's disease dementia diagnoses associated with lower self-ratings of quality of life in older adults. J Gerontol B Psychol Sci Soc Sci. (2017) 72:974–85. doi: 10.1093/geronb/gbx100
11. Makovski TT, Schmitz S, Zeegers MP, Stranges S, van den Akker M. Multimorbidity and quality of life: Systematic literature review and meta-analysis. Ageing Res Rev. (2019) 53:100903. doi: 10.1016/j.arr.2019.04.005
12. Palladino R, Pennino F, Finbarr M, Millett C, Triassi M. Multimorbidity and health outcomes in older adults in ten european health systems, 2006-15. Health Aff (Millwood). (2019) 38:613–23. doi: 10.1377/hlthaff.2018.05273
13. Yanna L, Yiqiao W. Prevalence and patterns of multimorbidity among chinese elderly people. Chin Gen Pract. (2021) 24:3955–62.
14. Chunzi C, Tubao Y. The exploration of the prevalence and the determinants of the chronic disease multimorbidity patterns among chinese middle-aged and elderly population:Based on hierarchical clustering analysis and apriori algorithm. Chin J Health Stat. (2023) 40:172–7.
15. Rundek T, Tolea M, Ariko T, Fagerli EA, Camargo CJ. Vascular cognitive impairment (VCI). Neurotherapeutics. (2022) 19:68–88. doi: 10.1007/s13311-021-01170-y
16. Murtaza A, Dasgupta I. Chronic kidney disease and cognitive impairment. J Stroke Cerebrovasc Dis. (2021) 30:105529. doi: 10.1016/j.jstrokecerebrovasdis.2020.105529
17. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
18. Aguado A, Moratalla-Navarro F, Lopez-Simarro F, Moreno V. MorbiNet: multimorbidity networks in adult general population. Analysis of type 2 diabetes mellitus comorbidity. Sci Rep. (2020) 10:2416. doi: 10.1038/s41598-020-59336-1
19. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
20. Maya G, Sarto J, Compta Y, Balasa M, Ximelis T, Aldecoa I, et al. Assessment of cognitive symptoms in brain bank-registered control subjects: feasibility and utility of a telephone-based screening. J Alzheimers Dis. (2022) 85:1107–13. doi: 10.3233/JAD-215444
21. Ham Y, Bae S, Lee H, Ha Y, Choi H, Park JH, et al. Item-level psychometrics of the ascertain dementia eight-item informant questionnaire. PloS One. (2022) 17:e270204. doi: 10.1371/journal.pone.0270204
22. Jahan S, Islam R, Rahman T, Kabir MF, Islam MW, Hossain K, et al. The assessment of musculoskeletal disorders, quality of life, and comorbidities in older people in Bangladesh. Front Public Health. (2023) 11:1269444. doi: 10.3389/fpubh.2023.1269444
23. GBD 2019 Bangladesh Burden of Disease Collaborators. The burden of diseases and risk factors in Bangladesh, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Glob Health. (2023) 11:e1931–42. doi: 10.1016/S2214-109X(23)00432-1
24. Gonzales MM, Garbarino VR, Pollet E, Palavicini JP, Kellogg DL Jr, Kraig E, et al. Biological aging processes underlying cognitive decline and neurodegenerative disease. J Clin Invest. (2022) 132(10):e158453. doi: 10.1172/JCI158453
25. Streit WJ, Khoshbouei H, Bechmann I. The role of microglia in sporadic alzheimer's disease. J Alzheimers Dis. (2021) 79:961–8. doi: 10.3233/JAD-201248
26. Cunningham C, Wilcockson DC, Campion S, Lunnon K, Perry VH. Central and systemic endotoxin challenges exacerbate the local inflammatory response and increase neuronal death during chronic neurodegeneration. J Neurosci. (2005) 25:9275–84. doi: 10.1523/JNEUROSCI.2614-05.2005
27. Morley JE. White matter lesions (leukoaraiosis): a major cause of falls. J Am Med Dir Assoc. (2015) 16:441–3. doi: 10.1016/j.jamda.2015.03.023
28. Bi YH, Pei JJ, Hao C, Yao W, Wang HX. The relationship between chronic diseases and depression in middle-aged and older adults: A 4-year follow-up study from the China Health and Retirement Longitudinal Study. J Affect Disord. (2021) 289:160–6. doi: 10.1016/j.jad.2021.04.032
29. Hansen N, Singh A, Bartels C, Brosseron F, Buerger K, Cetindag AC, et al. Hippocampal and hippocampal-subfield volumes from early-onset major depression and bipolar disorder to cognitive decline. Front Aging Neurosci. (2021) 13:626974. doi: 10.3389/fnagi.2021.626974
30. Salwierz P, Thapa S, Taghdiri F, Vasilevskaya A, Anastassiadis C, Tang-Wai DF, et al. Investigating the association between a history of depression and biomarkers of Alzheimer's disease, cerebrovascular disease, and neurodegeneration in patients with dementia. Geroscience. (2024) 46:783–93. doi: 10.1007/s11357-023-01030-x
31. Marawi T, Zhukovsky P, Rashidi-Ranjbar N, Bowie CR, Brooks H, Fischer CE, et al. Brain-cognition associations in older patients with remitted major depressive disorder or mild cognitive impairment: A multivariate analysis of gray and white matter integrity. Biol Psychiatry. (2023) 94:913–23. doi: 10.1016/j.biopsych.2023.05.018
32. Ruan Q, Xiao F, Gong K, Zhang W, Zhang M, Ruan J, et al. Prevalence of cognitive frailty phenotypes and associated factors in a community-dwelling elderly population. J Nutr Health Aging. (2020) 24:172–80. doi: 10.1007/s12603-019-1286-7
33. Giannouli V, Stamovlasis D, Tsolaki M. Longitudinal study of depression on amnestic mild cognitive impairment and financial capacity. Clin Gerontol. (2022) 45:708–14. doi: 10.1080/07317115.2021.2017377
34. Read JR, Sharpe L, Modini M, Dear BF. Multimorbidity and depression: A systematic review and meta-analysis. J Affect Disord. (2017) 221:36–46. doi: 10.1016/j.jad.2017.06.009
35. Chu CS, Sun IW, Begum A, Liu SI, Chang CJ, Chiu WC, et al. The association between subjective memory complaint and objective cognitive function in older people with previous major depression. PloS One. (2017) 12:e173027. doi: 10.1371/journal.pone.0173027
36. Maier A, Riedel-Heller SG, Pabst A, Luppa M. Risk factors and protective factors of depression in older people 65+. A systematic review. PloS One. (2021) 16:e251326. doi: 10.1371/journal.pone.0251326
37. Zhou F, He S, Shuai J, Deng Z, Wang Q, Yan Y. Social determinants of health and gender differences in depression among adults: A cohort study. Psychiatry Res. (2023) 329:115548. doi: 10.1016/j.psychres.2023.115548
38. Banihashemi N, Robillard R, Yang J, Carpenter JS, Hermens DF, Naismith SL, et al. Quantifying the effect of body mass index, age, and depression severity on 24-h activity patterns in persons with a lifetime history of affective disorders. BMC Psychiatry. (2016) 16:317. doi: 10.1186/s12888-016-1023-2
39. Jennings CS, Astin F, Prescott E, Hansen T, Gale Chris P, De Bacquer D. Illness perceptions and health literacy are strongly associated with health-related quality of life, anxiety, and depression in patients with coronary heart disease: results from the EUROASPIRE V cross-sectional survey. Eur J Cardiovasc Nurs. (2023) 22:719–29. doi: 10.1093/eurjcn/zvac105
40. Abdoli N, Salari N, Darvishi N, Jafarpour S, Solaymani M, Mohammadi M, et al. The global prevalence of major depressive disorder (MDD) among the elderly: A systematic review and meta-analysis. Neurosci Biobehav Rev. (2022) 132:1067–73. doi: 10.1016/j.neubiorev.2021.10.041
Keywords: multiple chronic conditions (MCC), depressive symptom, cognitive impairment, older adults, mediating effect
Citation: Lai L-C, Huang D-M, Peng J, Cao X-Y, Feng X-L, Tao P-Y, Pan X, Pan Q-N, Fan D-J, Lu S-Y, Li C-L, Pan Y-F, Dong P-X, Chai Y-D, Huang P, Wu H-C and Huang H-Q (2024) Depressive symptom mediates the association between the number of chronic diseases and cognitive impairment: a multi-center cross-sectional study based on community older adults. Front. Psychiatry 15:1404229. doi: 10.3389/fpsyt.2024.1404229
Received: 20 March 2024; Accepted: 27 June 2024;
Published: 17 July 2024.
Edited by:
Maria Basta, University Hospital of Heraklion, GreeceReviewed by:
Alejandra Mondragón-Maya, National Autonomous University of Mexico, MexicoYijun Pan, The University of Melbourne, Australia
Copyright © 2024 Lai, Huang, Peng, Cao, Feng, Tao, Pan, Pan, Fan, Lu, Li, Pan, Dong, Chai, Huang, Wu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui-Qiao Huang, aGhxQHNyLmd4bXUuZWR1LmNu
 Li-Chong Lai
Li-Chong Lai Dong-Mei Huang2
Dong-Mei Huang2