Abstract
Objective:
To construct and validate a nomogram prediction model for anxiety and depression in chemotherapy patients with multiple myeloma (MM).
Methods:
From May 2021 to May 2023, 333 MM chemotherapy patients treated at our hospital were selected. The patients were randomly divided into a modeling group and a validation group in a 7:3 ratio (using a random number table method). According to whether the modeling group patients had anxiety and depression, they were grouped into a non-anxiety and depression group and an anxiety and depression group; a nomogram model constructed using R software was built to evaluate the predictive performance of the model. Clinical decision curves (DCA) were used to assess the value of the clinical application of the model.
Results:
Out of the 233 patients in this study, 66 experienced anxiety and depression, with an incidence rate of 28.33%. There were great differences in gender, economic income, education level, tumor staging, complications, and treatment plans between the anxiety and depression group and the non-anxiety and depression group (P<0.05). The results of multivariate Logistic regression analysis showed that gender, education level, tumor stage, complications, and treatment plan were risk factors for anxiety and depression in MM chemotherapy patients (P<0.05), while economic income served as a protective factor (P<0.05). The AUC of the modeling group was 0.945, and the H-L test was χ2 = 8.579, P = 0.674, with good agreement. The AUC of the validation group was 0.967, and the H-L test was χ2 = 7.315, P = 0.698, with good consistency. The DCA curve shows that the probability of assessing anxiety and depression in patients undergoing MM chemotherapy is higher for clinical use when the probability is between 0.05 and 0.95.
Conclusion:
Gender, education, tumor stage, comorbidities and treatment regimen were risk factors for anxiety and depression in MM chemotherapy patients, while financial income was a protective factor for anxiety and depression in MM chemotherapy patients, and the constructed nomogram visually predicted the risk of anxiety and depression in MM chemotherapy patients.
1 Introduction
Multiple Myeloma (MM) is a common clinical malignancy, most frequently seen in middle-aged and elderly people. MM can suppress the body’s immune function, increasing the risk of bacterial infections, and the body is also prone to kidney damage, hypercalcemia, all of which have a serious impact on the patient’s health (1, 2). Clinical chemotherapy is an important method for treating MM, which can effectively improve the prognosis of patients and extend their survival time. However, during the chemotherapy process, while the drugs kill tumor cells, they may also damage normal cells, causing patients to experience various side effects such as nausea, vomiting, hair loss, which adversely affect physical and mental health, and are prone to anxiety and depression (3, 4). There are many factors affecting anxiety and depression in patients with malignant tumors. Promptly identifying and intervening in the relevant factors is particularly important for improving patient prognosis. A nomogram is a risk prediction model that converts influencing factors into numerical probabilities of clinical events, predicting the risk of occurrence and assisting clinicians in formulating preventive measures (5). A visual obesity risk prediction system based on machine learning has been developed, demonstrating good predictive performance and interpretability. The system directly provides users with their obesity risk level and identifies corresponding intervention priorities, helping physicians formulate personalized health management plans and achieving comprehensive and accurate obesity management (6). Based on the CHARLS cohort study, a visual risk prediction system for sarcopenia in the elderly was constructed using machine learning. This system supports early identification and scientific intervention of sarcopenia in older adults, with significant clinical value and application potential (7). A risk prediction system for depression in middle-aged and elderly individuals was also established using machine learning and visualization techniques. By providing early detection and evidence-based interventions for depression in this population, it establishes a new health management paradigm and has the potential to improve quality of life (8). Currently, there are few reports on the risk prediction research of anxiety and depression in MM chemotherapy patients, therefore, this study mainly aims to construct and verify a nomogram prediction model for anxiety and depression in MM chemotherapy patients.
2 Subjects and methods
2.1 Study subjects
333 MM chemotherapy patients treated in our hospital from May 2021 to May 2023 were selected, aged 54-86 years. Sample size calculation was performed using PASS 15 software (two-sided test, α = 0.05, power = 90%, d = 0.50), the total required sample size was calculated to be 301. Considering a 10% dropout rate, at least 333 participants need to be enrolled. The enrollees were randomly divided into a modeling group (233 cases) and a validation group (100 cases) at a 7:3 ratio (using a random number table method), and according to whether patients in the modeling group experienced anxiety and depression, they were divided into an anxiety-depression group and a non-anxiety-depression group. The case-selection flowchart is shown in Figure 1. Inclusion criteria: ① Conforming to the relevant diagnostic criteria for MM (9), confirmed by imaging; ② All receiving chemotherapy; ③ Stable condition, with no abnormal organ function (except for the kidneys); ④ Complete data. Exclusion criteria: ① Severe condition; ② Communication barriers; ③ History of alcohol or drug dependence; ④ Severe physical illness; ⑤ Stressful events occurring before admission. Patients signed a consent form, and this study was approved by the ethics committee of our hospital.
Figure 1

Flow chart of case collection.
2.2 Criteria for assessing anxiety and depression in MM chemotherapy patients
Anxiety and depression are assessed using the Hospital Anxiety and Depression Scale (HADS) (10) (two subscales for anxiety and depression), each consisting of 7 items scored from 0 to 3. A total score of ≤7 points (no anxiety or depression) is classified as the non-anxiety and depression group, while scores of 8-10 points (possible anxiety or depression) and >10 points (definite anxiety or depression) are classified as the anxiety and depression group.
2.3 Collection of clinical data
Data collected includes patient’s age, Body Mass Index (BMI), gender, place of residence, economic income (grouped by the median value for statistical analysis), family support, marital status, educational level, method of medical expense payment, employment status, tumor staging, complications(anemia, bone pain, hyperviscosity syndrome, and renal impairment), treatment regimen (MPT regimen: Melphalan + Prednisone + Thalidomide; VDT regimen: Bortezomib + Dexamethasone + Thalidomide), coping strategies (assessed using a simple coping style questionnaire with a four-level scoring system, including positive and negative coping), and the Social Support Rating Scale (SSRS) to assess social support (with a maximum score of 62, higher scores indicating greater social support).
2.4 Method of data collection
All personnel in this study were uniformly trained to ensure consistent understanding of the questionnaire items. Data collection was mainly done through the hospital’s electronic medical record system on computer terminals, using specially designed pathology data collection forms. The data collectors, proficient in using the electronic medical record system and with over five years of experience and research capability, compiled the survey contents item by item to ensure the validity and authenticity of the data.
2.5 Statistical processing
Data were analyzed using SPSS 25.0. Count data were tested with the χ2 chi-square test and expressed as cases (%). Quantitative data (conforming to normal distribution) were tested with the t-test and expressed as (mean ± standard deviation). Multifactorial logistic regression analysis (enter method) was used to analyze the risk factors for anxiety and depression in MM chemotherapy patients; The identified risk factors were then introduced into R3.6.3 software using the rms package to construct a nomogram model for predicting anxiety and depression in MM chemotherapy patients. The nomogram model was generated to visually represent the contribution of each independent variable to the predicted probability of anxiety and depression, allowing for an intuitive assessment of risk for each patient based on their clinical characteristics. ROC curves were drawn to evaluate the discriminative ability of the nomogram model for predicting anxiety and depression in MM chemotherapy patients; calibration curves were drawn to assess the consistency of the model. The clinical decision curve analysis (DCA) was used to evaluate the clinical application value of the nomogram model. P<0.05 was considered statistically significant.
3 Results
3.1 Anxiety status in MM chemotherapy patients
The results of this study show that 167 patients had no anxiety or depression, 41 possibly affected, and 25 had definite anxiety or depression. The depression score for the anxiety and depression group is (9.40 ± 1.30) points, and the anxiety score is (10.60 ± 1.40) points.
3.2 Comparison of clinical data between modeling and validation groups
There were no significant differences (P>0.05) in clinical data such as age, BMI, gender, place of residence, economic income, family support, marital status, educational level, method of medical expense payment, employment status, tumor staging, complications, treatment regimen, coping methods, and SSRS scores between the modeling and validation groups. Details are shown in Table 1.
Table 1
| Factor | Modeling group (n=233) | Validation groups(n=100) | t/χ2 | P |
|---|---|---|---|---|
| Age(year) | 0.455 | 0.500 | ||
| ≥60 | 167(71.67) | 68(68.00) | ||
| <60 | 66(28.33) | 32(32.00) | ||
| BMI(kg/m2) | 23.61 ± 4.28 | 23.59 ± 4.29 | 0.039 | 0.969 |
| Gender | 0.231 | 0.631 | ||
| man | 144(61.80) | 59(59.00) | ||
| woman | 89(38.20) | 41(41.00) | ||
| Place of residence | 0.284 | 0.594 | ||
| town | 147(63.09) | 60(60.00) | ||
| countryside | 86(36.91) | 40(40.00) | ||
| Economic income (10,000 yuan/year) | 1.003 | 0.317 | ||
| ≥5 | 135(57.94) | 52(52.00) | ||
| <5 | 98(42.06) | 48(48.00) | ||
| Family support situation | 0.053 | 0.819 | ||
| support | 129(55.36) | 54(54.00) | ||
| Not supported | 104(44.64) | 46(46.00) | ||
| Marital status | 0.510 | 0.475 | ||
| married | 163(69.96) | 66(66.00) | ||
| Unmarried/divorced/widowed | 70(30.04) | 34(34.00) | ||
| Educational level | 0.176 | 0.675 | ||
| Junior high school and below | 106(45.49) | 43(43.00) | ||
| High school and above | 127(54.51) | 57(57.00) | ||
| Payment methods for medical expenses | 0.160 | 0.689 | ||
| No health insurance | 49(21.03) | 23(23.00) | ||
| Medical Health Insurance | 184(78.97) | 77(77.00) | ||
| Working conditions | 0.124 | 0.725 | ||
| incumbency | 137(58.80) | 56(56.00) | ||
| retire | 96(41.20) | 44(44.00) | ||
| Tumor staging | 0.177 | 0.674 | ||
| I~II | 127(54.51) | 52(52.00) | ||
| III | 106(45.49) | 48(48.00) | ||
| Complication | 0.139 | 0.710 | ||
| Yes | 103(44.21) | 42(42.00) | ||
| No | 130(55.79) | 58(58.00) | ||
| Treatment regimen | 0.018 | 0.892 | ||
| MPT scheme | 96(41.20) | 42(42.00) | ||
| VDT scheme | 137(58.80) | 58(58.00) | ||
| Coping | 0.104 | 0.747 | ||
| Be proactive | 121(51.93) | 50(50.00) | ||
| Negative coping | 112(48.07) | 50(50.00) | ||
| SSRS Score (points) | 0.089 | 0.765 | ||
| <40 | 109(46.78) | 45(45.00) | ||
| ≥40 | 124(53.22) | 55(55.00) |
Comparison of clinical data between the modeling group and the validation group.
3.3 Comparison of clinical data between anxiety and depression group and non-anxiety and depression group
Statistically, among the 233 patients in this study, 66 had anxiety or depression, with an incidence rate of 28.33%. There were differences (P<0.05) in gender, economic income, educational level, tumor staging, complications, and treatment regimen between the anxiety and depression group and the non-anxiety and depression group. There were no differences (P>0.05) in age, BMI, place of residence, family support, marital status, method of medical expense payment, employment status, coping methods, and SSRS scores between the two groups. See Table 2.
Table 2
| Factor | Anxiety and depression group(n=66) | No anxiety and depression group(n=167) | t/χ2 | P |
|---|---|---|---|---|
| Age(year) | 1.929 | 0.165 | ||
| ≥60 | 43(65.15) | 124(74.25) | ||
| <60 | 23(34.85) | 43(25.75) | ||
| BMI(kg/m2) | 23.67 ± 4.30 | 23.59 ± 4.27 | 0.129 | 0.898 |
| Gender | 28.339 | <0.001 | ||
| man | 23(34.85) | 121(72.46) | ||
| woman | 43(65.15) | 46(27.54) | ||
| Place of residence | 0.632 | 0.426 | ||
| town | 39(59.09) | 108(64.67) | ||
| countryside | 27(40.91) | 59(35.33) | ||
| Economic income (10,000 yuan/year) | 15.207 | <0.001 | ||
| ≥5 | 25(37.88) | 110(65.87) | ||
| <5 | 41(62.12) | 57(34.13) | ||
| Family support situation | 0.203 | 0.652 | ||
| support | 35(53.03) | 94(56.29) | ||
| Not supported | 31(46.97) | 73(43.71) | ||
| Marital status | 0.138 | 0.710 | ||
| married | 45(68.18) | 118(70.66) | ||
| Unmarried/divorced/widowed | 21(31.82) | 49(29.34) | ||
| Educational level | 12.223 | <0.001 | ||
| Junior high school and below | 42(63.64) | 64(38.32) | ||
| High school and above | 24(36.36) | 103(61.68) | ||
| Payment methods for medical expenses | 0.572 | 0.449 | ||
| No health insurance | 16(24.24) | 33(19.76) | ||
| Medical Health Insurance | 50(75.76) | 134(80.24) | ||
| Working conditions | 0.124 | 0.725 | ||
| incumbency | 40(60.61) | 97(58.08) | ||
| retire | 26(39.39) | 70(41.92) | ||
| Tumor staging | 24.563 | <0.001 | ||
| I~II | 19(28.79) | 108(64.67) | ||
| III | 47(71.21) | 59(35.33) | ||
| Complication | 14.095 | <0.001 | ||
| Yes | 42(63.64) | 61(36.53) | ||
| No | 24(36.36) | 106(63.47) | ||
| Treatment regimen | 24.648 | <0.001 | ||
| MPT scheme | 44(66.67) | 52(31.14) | ||
| VDT scheme | 22(33.33) | 115(68.86) | ||
| Coping | 0.045 | 0.833 | ||
| Be proactive | 35(53.03) | 86(51.50) | ||
| Negative coping | 31(46.97) | 81(48.50) | ||
| SSRS Score (points) | 0.107 | 0.743 | ||
| <40 | 32(48.48) | 77(46.11) | ||
| ≥40 | 34(51.52) | 90(53.89) |
Comparison of clinical data between the anxiety and depression groups and the non-anxiety and depression groups.
3.4 Logistic regression analysis of anxiety and depression in MM chemotherapy patients
Taking whether MM chemotherapy patients had anxiety or depression as the dependent variable (yes=1, no=0), and gender(female=1, male=0), economic income(<50,000 yuan/year=1,≥50,000 yuan/year=0), educational level(below high school=1, high school or above=0), tumor staging(Stage I–II=0, Stage III–IV=1), complications(yes=1, no=0), and treatment regimen(VDT regimen=0, MPT regimen= 1) as independent variables for analysis. The results of the multivariate logistic regression analysis show that gender (OR:5.215, 95%CI:1.78915.202), educational level (OR:13.381, 95%CI:4.45140.228), tumor staging (OR:4.666, 95%CI:1.46814.837), complications (OR:7.063, 95%CI:2.52419.763), and treatment regimen (OR:3.629, 95%CI:1.20710.905) were risk factors for anxiety and depression in MM chemotherapy patients (P<0.05), and economic income (OR:0.578, 95%CI:0.4260.785) was a protective factor (P<0.05). See Table 3.
Table 3
| Variable | β value | SE value | Wald χ2 value | P value | OR value | 95%CI |
|---|---|---|---|---|---|---|
| Gender | 1.651 | 0.546 | 9.152 | 0.002 | 5.215 | 1.789~15.202 |
| Economic income | -0.548 | 0.156 | 12.348 | <0.001 | 0.578 | 0.426~0.785 |
| Educational level | 2.594 | 0.562 | 21.333 | <0.001 | 13.381 | 4.451~40.228 |
| Tumor staging | 1.540 | 0.590 | 6.812 | 0.009 | 4.666 | 1.468~14.837 |
| Complication | 1.955 | 0.525 | 13.864 | <0.001 | 7.063 | 2.524~19.763 |
| Treatment regimen | 1.289 | 0.561 | 5.270 | 0.02 | 3.629 | 1.207~10.905 |
| Constant | -5.163 | 0.708 | 53.109 | <0.001 | 0.006 | – |
Logistic regression analysis of anxiety and depression in patients undergoing MM chemotherapy.
3.5 Establishment of a nomogram model for anxiety and depression in MM chemotherapy patients
The identified risk factors were introduced into R software to establish a nomogram model for predicting anxiety and depression in MM chemotherapy patients. The nomogram was constructed to visually quantify the contribution of each independent factor to the predicted risk. Each variable is assigned a specific number of points: educational level contributes the most, followed by complications, gender, economic income, tumor staging, and treatment regimen. By summing the scores of each variable and calculating the total score, the risk of anxiety and depression in MM chemotherapy patients can be predicted. It is evident that in this model, the most important factor affecting the score is the level of education, followed by complications, gender, economic income, tumor staging, and treatment regimen. Figure 2 displays the nomogram.
Figure 2
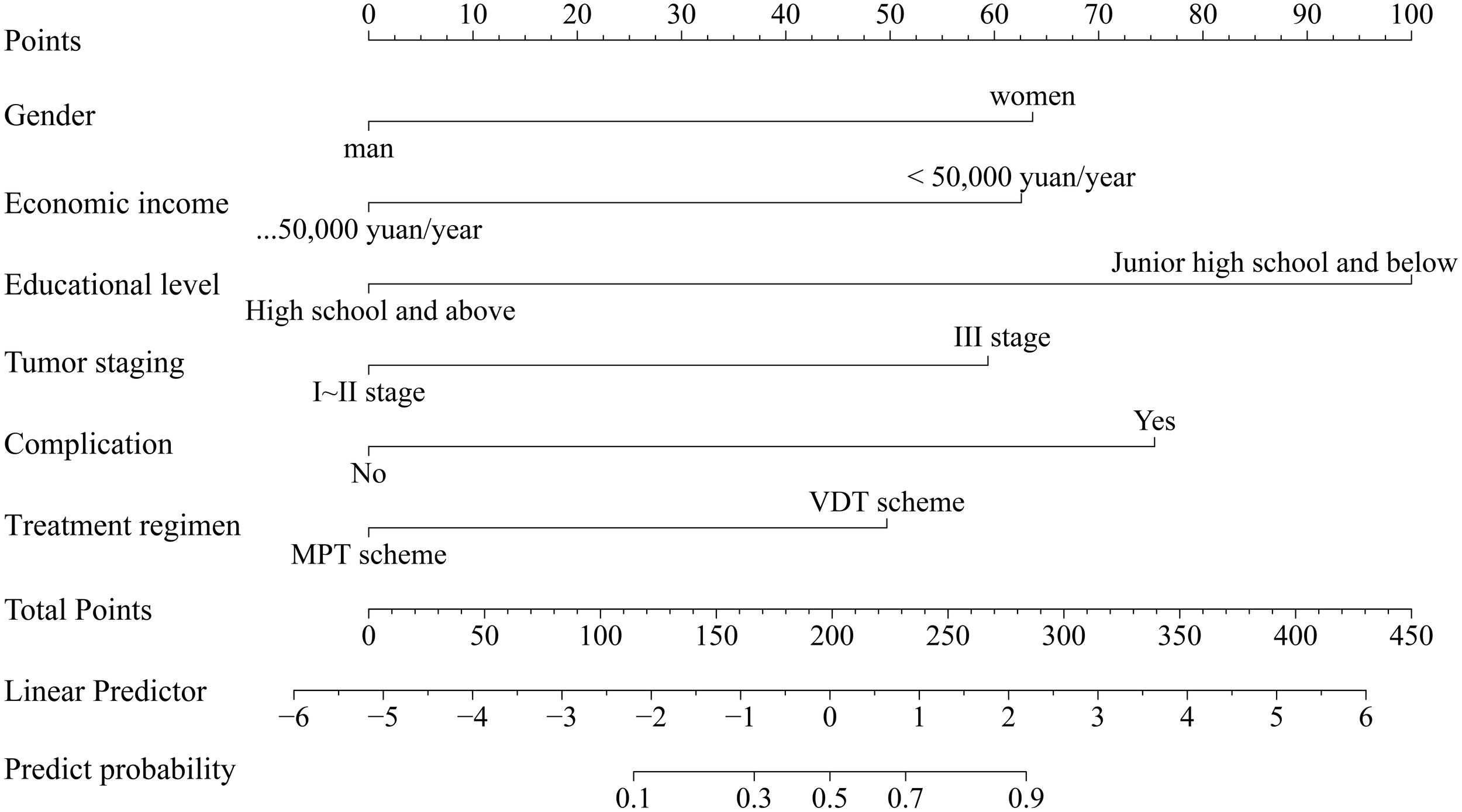
Nomogram for predicting anxiety and depression in MM chemotherapy patients.
3.6 Internal validation of the nomogram model for anxiety and depression in MM chemotherapy patients
For the modeling group, the Area Under the Curve (AUC) of the ROC curve was 0.945 (95%CI: 0.913~0.981) (see Figure 3A). The calibration curve slope was close to 1 (see Figure 3B), and the Hosmer-Lemeshow (H-L) test yielded a χ2=8.579, P = 0.674, indicating good consistency.
Figure 3

Internal validation of the anxiety and depression nomogram model in patients with MM chemotherapy (A) ROC curves of the modeling group; (B) Calibration curves of the modeling group.
3.7 External validation of the nomogram model for anxiety and depression in MM chemotherapy patients
The AUC for external validation was 0.967 (95% CI: 0.913~0.989) (Figure 4A). The calibration curve slope was close to 1 (Figure 4B), and the H-L test yielded a χ2=7.315, P = 0.698, indicating good consistency.
Figure 4

External validation of the anxiety and depression nomogram model in patients with MM chemotherapy (A) ROC curves of the verify group; (B) Calibration curve of the verification group.
3.8 DCA curve of the nomogram model
As observed from the DCA curve, when the probability ranges from 0.05 to 0.95, the nomogram provided high clinical utility for assessing anxiety and depression risk in MM chemotherapy patients (Figure 5).
Figure 5
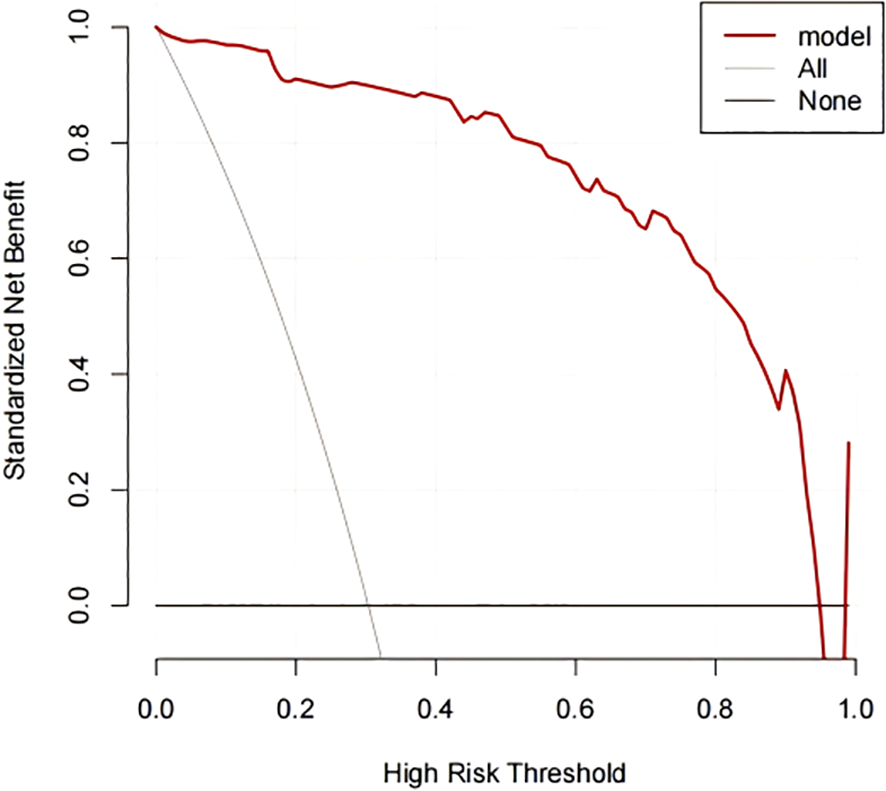
DCA curves for nomogram model. The X-axis represents the continuum of potential threshold probabilities for early recurrence, and the Y-axis represents the net benefit. The red line indicates the nomogram model predicting anxiety and depression in MM chemotherapy patients. The gray line represents the strategy of intervening in all patients, while the thin black line represents the strategy of intervening in none.
4 Discussion
The incidence of MM is increasing with the aggravation of aging. With the advancement in medical standards and the continuous development of new drugs, the survival period of MM patients has been extended, but this can also create additional physical and psychological burdens (11). Apart from the disease itself, chemotherapy drugs can cause adverse effects such as fatigue and hair loss in patients. Moreover, the proliferation of plasma cells in the body secretes a large number of cytokines, activating osteoclasts and leading to bone pain and limited mobility in patients. Such physical discomfort and restricted activity easily lead to anxiety and depression in patients (12, 13). Therefore, it is important to pay attention to the emotional state of patients during clinical treatment to effectively improve their prognosis. The results of this study show that the incidence of anxiety and depression in MM patients is 28.33%, and the presence of anxiety and depression severely affects the psychological state of patients. Thus, constructing a risk prediction model for anxiety and depression in MM chemotherapy patients is very important for clinical intervention.
Clinically, risk management for anxiety and depression in MM chemotherapy patients can be strengthened based on risk factors. This study identified six influencing factors: gender, economic income, educational level, tumor staging, complications, and treatment regimen. Analysis: ① Compared with male patients, female patients-due to a more family-centered role orientation and potentially lower psychological tolerance-are more likely to develop adverse emotions after falling ill. They are more emotional, and the side effects of chemotherapy, such as endocrine disorders, hair loss and diarrhea, can exacerbate feelings of anxiety and depression (14, 15). ② MM requires long-term treatment, and the high cost of medical care adds to the family burden. Patients may also worry about becoming a burden to their family, leading to anxiety and depression, especially when facing elderly spouses or adult children occupied with work (16, 17). ③ Patients with higher educational levels can more thoroughly understand educational content, have stronger learning abilities, and can acquire treatment-related knowledge through various channels. By contrast, patients with a lower level of education have less ability to understand disease information and may not fully understand health education provided by medical staff, leading to increased anxiety (18, 19). ④ Patients with advanced tumor stages and complications may worry about the incurability of their condition due to disease progression. Complications can exacerbate the disease, and adjustments in the treatment regimen can increase drug dosage and side effects, further aggravating physical discomfort and causing anxiety and depression (20–22). ⑤ The VDT treatment regimen based on Bortezomib can effectively delay the growth of MM. After treatment, it has cytotoxic effects on tumor cells, inhibits the proteasome, and blocks the degradation of target cells through the ubiquitin-proteasome pathway, reducing the adhesion and secretion of tumor cells, leading to their death. Combined with Dexamethasone and Thalidomide, it increases the synergistic effect, inhibits the proliferation of myeloma cells, prolongs survival, and may help alleviate anxiety and depression (23, 24). Nursing interventions can be implemented to address the above influencing factors. During health education, use simple and easy-to-understand language, provide examples of successful cases to increase treatment confidence, and for patients experiencing financial pressure, introduce social assistance programs to alleviate economic burdens.
The nomogram transforms complex regression equations into visual representations, making the results of the predictive model more intuitive and facilitating clinicians’ assessment of patients. In this study, the constructed nomogram yielded AUC values of 0.945 and 0.967 for the two groups, with good fit in the H-L test, indicating strong predictive capability. Additionally, the DCA curve showed that when the high-risk threshold probability ranged from 0.05 to 0.95, the nomogram model had high clinical utility. This model can assist healthcare professionals in predicting the risk of anxiety and depression in MM chemotherapy patients based on risk factors and enable early intervention.
In conclusion, gender, educational level, tumor staging, complications, and treatment regimen are risk factors for anxiety and depression in MM chemotherapy patients, while economic income is a protective factor. The constructed nomogram model has good discriminative ability and consistency, and can visually predict the risk of anxiety and depression in MM chemotherapy patients. This study has limitations, including a relatively small sample size, as well as potential self-report bias from patients diagnosed with anxiety and depression, which may limit generalizability. Future studies should expand sample size and optimize diagnostic procedures for further validation.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Ganzhou People’s Hospital and the Ethics Committee of Guangzhou Hospital of Integrated Traditional and Western Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LW: Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. YL: Data curation, Investigation, Methodology, Writing – original draft. HL: Writing – original draft, Writing – review & editing.
Funding
The author(s) declared that financial support was received for this work and/or its publication. This study was supported by the 2024 Huadu District Basic and Applied Basic Research Joint Funding Project of Guangzhou Hospital of Integrated Traditional Chinese and Western Medicine (No. 24HDQYLH20).
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Rajkumar SV . Multiple myeloma: 2022 update on diagnosis, risk stratification, and management. Am J Hematol. (2022) 97:1086–107. doi: 10.1002/ajh.26590
2
Cowan AJ Green DJ Kwok M Lee S Coffey DG Holmberg LA et al . Diagnosis and management of multiple myeloma: A review. JAMA. (2022) 327:464–77. doi: 10.1001/jama.2022.0003
3
Cho Y-R Yoo Y-S . Factors influencing supportive care needs of multiple myeloma patients treated with chemotherapy. Support Care Cancer. (2020) 28:1783–91. doi: 10.1007/s00520-019-04984-x
4
Selvy M Kerckhove N Pereira B Barreau F Nguyen D Busserolles J et al . Prevalence of chemotherapy-induced peripheral neuropathy in multiple myeloma patients and its impact on quality of life: A single center cross-sectional study. Front Pharmacol. (2021) 12:637593. doi: 10.3389/fphar.2021.637593
5
Zhou H Jian Y Du J Liu J Zhang Z Yang G et al . Prognostic nomogram for multiple myeloma early relapse after autologous stem cell transplant in the novel agent era. Cancer Med. (2023) 12:9085–96. doi: 10.1002/cam4.5630
6
Du J Yang S Zeng Y Ye C Chang X Wu S . Visualization obesity risk prediction system based on machine learning. Sci Rep. (2024) 14:22424. doi: 10.1038/s41598-024-73826-6
7
Du J Tao X Zhu L Wang H Qi W Min X et al . Development of a visualized risk prediction system for sarcopenia in older adults using machine learning: a cohort study based on CHARLS. Front Public Health. (2025) 13:1544894. doi: 10.3389/fpubh.2025.1544894
8
Du J Tao X Zhu L Qi W Min X Deng H et al . A risk prediction system for depression in middle-aged and older adults grounded in machine learning and visualization technology: a cohort study. Front Public Health. (2025) 13:1606316. doi: 10.3389/fpubh.2025.1606316
9
Rajkumar SV . Updated diagnostic criteria and staging system for multiple myeloma. Am Soc Clin Oncol Educ Book. (2016) 35:e418–e23. doi: 10.1200/EDBK_159009
10
Shi H Ren H Tian Y Chen Z Xu C Lu L et al . Pain as a risk factor of depression and anxiety symptoms with multiple myeloma during maintenance therapy. Front Psychol. (2022) 13:1015497. doi: 10.3389/fpsyg.2022.1015497
11
Joshua DE Bryant C Dix C Gibson J Ho J . Biology and therapy of multiple myeloma. Med J Aust. (2019) 210:375–80. doi: 10.5694/mja2.50129
12
Fischer J Knop S Danhof S Einsele H Keller D Löffler C . The influence of baseline characteristics, treatment and depression on health-related quality of life in patients with multiple myeloma: a prospective observational study. BMC Cancer. (2022) 22:1032. doi: 10.1186/s12885-022-10101-9
13
Kang H-Y Choi E-Y . Factors influencing quality of life in patients with multiple myeloma. Contemp Nurse. (2019) 55:109–21. doi: 10.1080/10376178.2019.1623699
14
Dweik A Dweik H Mian H Mohan M Schinke C Al Hadidi S . Gender disparities in multiple myeloma publications. EJHaem. (2022) 3:966–9. doi: 10.1002/jha2.470
15
Bangolo AI Fwelo P Trivedi C Sagireddy S Aljanaahi H Auda A et al . Interaction between age and gender on survival outcomes in extramedullary multiple myeloma over the past two decades. World J Clin Oncol. (2023) 14:179–89. doi: 10.5306/wjco.v14.i4.179
16
Hong YD Mullins CD Onukwugha E Yared JA Zheng Z Slejko JF . Association of individual low-income status and area deprivation with mortality in multiple myeloma. J Geriatr Oncol. (2023) 14:101415. doi: 10.1016/j.jgo.2022.12.003
17
Chamoun K Firoozmand A Caimi P Fu P Cao S Otegbeye F et al . Socioeconomic factors and survival of multiple myeloma patients. Cancers (Basel). (2021) 13:1–12. doi: 10.3390/cancers13040590
18
Xu L Wang X Pan X Wang X Wang Q Wu B et al . Education level as a predictor of survival in patients with multiple myeloma. BMC Cancer. (2020) 20:737. doi: 10.1186/s12885-020-07178-5
19
Hsieh RW Go RS Abeykoon JP Kapoor P Kumar SK Gertz MA et al . Characteristics of long-term survivors with multiple myeloma: A National Cancer Data Base analysis. Cancer. (2019) 125:3574–81. doi: 10.1002/cncr.32357
20
Padala SA Barsouk A Barsouk A Rawla P Vakiti A Kolhe R et al . Epidemiology, staging, and management of multiple myeloma. Med Sci (Basel). (2021) 9:1–14. doi: 10.3390/medsci9010003
21
Zhong L Hao P Zhang Q Jiang T Li H Xiao J et al . Revised International Staging System (R-ISS) stage-dependent analysis uncovers oncogenes and potential immunotherapeutic targets in multiple myeloma (MM). Elife. (2022) 11:1–24. doi: 10.7554/eLife.75340
22
Bridoux F Leung N Belmouaz M Royal V Ronco P Nasr SH et al . Management of acute kidney injury in symptomatic multiple myeloma. Kidney Int. (2021) 99:570–80. doi: 10.1016/j.kint.2020.11.010
23
Voorhees PM Kaufman JL Laubach J Sborov DW Reeves B Rodriguez C et al . Daratumumab, lenalidomide, bortezomib, and dexamethasone for transplant-eligible newly diagnosed multiple myeloma: the GRIFFIN trial. Blood. (2020) 136:936–45. doi: 10.1182/blood.2020005288
24
McCaughan GJ Gandolfi S Moore JJ Richardson PG . Lenalidomide, bortezomib and dexamethasone induction therapy for the treatment of newly diagnosed multiple myeloma: a practical review. Br J Haematol. (2022) 199:190–204. doi: 10.1111/bjh.18295
Summary
Keywords
multiple myeloma, chemotherapy, anxiety and depression, nomogram, influence factor
Citation
Wu L, Li Y and Li H (2026) Construction and validation of nomogram prediction model for anxiety and depression in chemotherapy patients with multiple myeloma. Front. Psychiatry 16:1578132. doi: 10.3389/fpsyt.2025.1578132
Received
17 February 2025
Revised
20 November 2025
Accepted
30 November 2025
Published
12 January 2026
Volume
16 - 2025
Edited by
Lamyae Benzakour, University of Geneva, Switzerland
Reviewed by
Kuanjun He, Inner Mongolia University for Nationalities, China
Fillipe Pereira, Federal University of São Carlos, Brazil
Updates
Copyright
© 2026 Wu, Li and Li.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Li, hpinggzhou88@sina.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.