- 1Second Affiliated Middle School International Department, Beijing Normal University, Beijing, China
- 2College of Physical Education and Sports, Beijing Normal University, Beijing, China
- 3Department of Sport Arts, Heibei Sport University, Shijiazhuang, China
Objective: In recent years, the prevalence of autism spectrum disorder (ASD) has been increasing year by year, bringing huge economic and mental burdens to society and families. Ayres Sensory Integration Intervention (ASI) is a widely used approach in the treatment of ASD. A more common sensory integration approach in China is called sensory integration-based intervention (SIBI), which is developed based on ASI. This study systematically analyzes the effects of SIBI on the sensory integration abilities and autism-related behaviors of autistic children.
Methods: We searched PubMed, Cochrane Library, Web of Science, EBSCO, and CNKI databases from inception to February 2025. Randomized controlled trials (RCTs) using SIBI to improve autistic children were included. After selection, data were extracted on author, year, country, sample size, age, intervention type and duration, and outcome indicators. Quality assessment and data extraction were conducted independently by two researchers. Statistical analyses were performed in Stata 17, including forest plots, funnel plots with Egger’s test for publication bias, and meta-regression for heterogeneity.
Results: A total of 16 studies with 1319 samples were included. The results showed that compared to the control group, SIBI had a positive effect on the total score of sensory integration ability scales for autistic children [mean difference (MD), 11.53; 95% confidence interval (CI) (10.53, 12.53); P<0.5]. Compared to the control group, SIBI also positively improved the total score of the ATEC scale [MD, -16.12; 95% CI (-22.61, -9.64); P<0.05] and the total score of the ABC scale [MD, -16.12; 95% CI (-22.61, -9.64); P<0.05]. The results from Egger’s test and the funnel plot indicated no publication bias. Due to the high heterogeneity (I²>50%) in the results of SIBI intervention on the total ABC score, a meta-regression analysis was conducted. The results of the meta-regression analysis indicated that age was not the source of heterogeneity, while the intervention duration was found to be the source of heterogeneity (β=-0.51, P<0.05, 95% CI [-1.01, -0.01]).
Conclusion: SIBI can effectively improve the sensory integration ability and autism-related behaviors of autistic children.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD420250639991.
1 Introduction
Autism spectrum disorder (ASD) is a common, highly heritable, and heterogeneous neurodevelopmental disorder that encompasses conditions such as autism, Asperger syndrome, and pervasive developmental disorder. These disorders are characterized by underlying cognitive features and frequently co-occur with other conditions (1). The core symptoms of ASD include social communication difficulties and repetitive patterns of behavior, interests, or activities. It is often accompanied by sensory integration disorders, emotional issues, and language communication difficulties (2). The etiology of ASD is complex and not yet fully understood, involving a combination of genetic and environmental factors (3). Early environmental insults may lead to abnormal brain structure and function, affecting neurodevelopmental processes and increasing the risk of ASD (4). At present, the prevalence of ASD is increasing annually, with the World Health Organization (WHO) estimating a global prevalence of 0.76% (5). In 2023, the Centers for Disease Control and Prevention (CDC) reported a prevalence rate of 1 in 36 among 8-year-old children in the United States (6). In China, epidemiological studies indicate that the prevalence of ASD among school-aged children (6–12 years) is 0.7%, suggesting that nearly 700, 000 children in China are affected by ASD (7). The increasing incidence of ASD, with its early and often lifelong onset, places an enormous economic and emotional burden on families and society. The “Analysis of the Current Situation of Autistic Children in China” report highlights that the monthly rehabilitation costs for children with ASD account for half of a family’s total expenditure. Currently, there are no specific pharmacological treatments for ASD, with medications such as risperidone and aripiprazole being used primarily for symptom management. As a result, ASD interventions mainly rely on non-pharmacological approaches, including Applied Behavior Analysis (ABA), the Early Start Denver Model, Ayres Sensory Integration® (ASI) and so on, which form an essential component of the overall treatment strategy (8, 9).
Sensory integration is a process that involves combining sensory information received from various senses in the human body. After this information is processed and integrated into the central nervous system, it enables individuals to perceive their internal and external environments and triggers appropriate physical responses. However, individuals with sensory integration dysfunction may make errors in processing sensory stimuli accurately. While sensory factors are not specific elements for diagnosing autism, they can affect the vast majority of autistic children (10, 11). Sensory integration dysfunction mainly includes tactile defensive disorder, motor difficulties, auditory language disorders, vestibular balance dysfunction, and spatial and structural perception disorders (12). The sensory system issues in autistic children are significant factors affecting other behavioral problems, such as social skills, social engagement, and academic performance (13). Therefore, improving the sensory system function in autistic children is also a crucial measure to enhance the overall treatment effectiveness.
ASI, developed by A. Jean Ayres, is a therapeutic approach designed to enhance sensory integration functions by influencing the way the brain processes and organizes sensory information through the provision of controlled sensory stimuli in the context of playful and meaningful activities (14). ASI is a clinical-based approach that focuses on the relationship between the therapist and the child, using play-based sensory-motor activities aimed at improving sensory processing and integration (15). Currently, ASI has been widely applied in research involving children with various diseases, with ASD being one of them (16–18). ASI can effectively improve the social skills and self-care abilities of autistic children (19, 20).At the same time, occupational therapy using the principles of ASI is one of the most requested services by parents of autistic children (21). A survey of occupational therapists also showed that 82% of respondents indicated they ‘always’ use sensory integration methods in their treatment when working with autistic children (22). Several systematic reviews have examined the impact of ASI on autistic children, focusing on issues such as the fidelity of intervention implementation, the strength and certainty of the available evidence, and the reproducibility of intervention procedures (23–25). In China, a more commonly used sensory integration approach is referred to as sensory integration-based intervention (SIBI), which was developed based on the ASI framework. However, despite its widespread application, research conducted in China remains limited in both quality and consistency, characterized by relatively small sample sizes and variability in outcome measurement tools. Therefore, our review aims to contribute by providing quantitative evidence specific to Chinese populations, thereby complementing the broader international literature.
Therefore, to address this potential issue, this meta-analysis conducted searches in both Chinese and English databases to supplement the lack of sufficient RCTs, with the hope of providing a theoretical basis for the effects of SIBI interventions on autistic children. This study aims to synthesize published research to analyze the impacts of SIBI on the sensory integration abilities and behaviors of autistic children, exploring the specific effects of SIBI on this population.
2 Methods
Meta-analysis is performed according to the preferred reporting items in the System Review and Meta-analysis (PRISMA) guide (26).(CRD420250639991).
2.1 Literature search strategy
The studies search was performed for the related research studies, mainly from the following databases: PubMed, Cochrane Library, Web of Science, EBSCO, CNKI. The search keywords we used were (“ayres sensory integration intervention OR sensory integration therapy OR ayres sensory integration OR sensory integration training” OR SIT OR SII OR AIT OR “sensory integration”) AND (autism OR ASD OR autism spectrum disorder) AND (RCT OR random OR random controlled trial). This is limited to February 2025.
2.2 Inclusion and exclusion criteria
The following PICOS criteria were employed for the selection of studies included in the research.
Participant (p): Inclusion criteria for research subjects are children under the age of 18 diagnosed with ASD in hospitals. Also does not include other mental illnesses.
Intervention (I): using SIBI therapy to intervene in ASD.
Comparison (C): In the control group, autistic children only received standard care or did not receive any intervention.
Outcomes (O): outcomes indicators containing ABC (Autism Behavior Checklist)OR ATEC (Autism Treatment Evaluation Checklist) OR SIS(Sensory Integration Scale).
Study design (S): Randomized Controlled Trials, Controlled Studies, Studies with.
Criteria for exclusion: (1) observational designs rather than randomized controlled trials; (2) involved non-human subjects include rats, mice, etc.; (3) included children with ADHD or other neurodevelopmental disorders instead of ASD; (4) The outcome measures do not include ATEC, ABC, SIS; and (5) inability to extract outcome indicators.
2.3 Data extraction
Two authors independently screened the abstracts and full-text articles of the selected works, extracted and cross-verified the data. In instances of disagreement, a third researcher was consulted to mediate and reach consensus. During the studies screening process, the initial step involved reading the titles and abstracts, followed by a thorough examination of the full texts to determine the studies to be excluded.
2.4 Quality assessment
Two researchers independently screened literature, extracted relevant data, and conducted cross checks. Disagreements were resolved through discussion or, if necessary, with the assistance of a third researcher. The extracted data includes basic research information, characteristics of research participants, specific details of interventions, measured outcome indicators, and research quality. Evaluating the methodological quality of included studies using the Physical Therapy Evidence Database (PEDro) scale(https://pedro.org.au/simplified-chinese/resources/pedro-scale/)There are a total of 11 evaluation items. Meeting each standard earns 1 point and does not meet or apply any standards earns 0 points. Research with a score of 0–3 is classified as low-quality, 4–7 as moderate quality, and 8–11 as high-quality (27).
2.5 SIBI description
The SIBI currently used and most widely practiced in China are culturally adapted programs derived from Ayres’ sensory integration approach (14, 28). These interventions were originally developed in 1992 through a collaboration between the Institute of Mental Health at Peking Medical University and Professor Wen-De Chen, who analyzed and modified Ayres’ model to create an integrated program suited to the Chinese context (28).
2.6 Statistical analysis
We used Stata 17.0 to conduct a meta-analysis on the data from all included studies. All outcome indicators selected in this study were continuous variables, and there were no differences among the outcome measurement tools used in individual studies. Therefore, the weighted mean difference (MD) was used for calculation. The criteria for judging heterogeneity were as follows: When I² ≤ 50%, it indicates that the meta-analysis results show low heterogeneity, and a fixed-effect model should be applied. When I² > 50%, it indicates that the meta-analysis results have high heterogeneity, and a random-effect model should be used (29). Additionally, we conducted a meta-regression analysis on results with high heterogeneity to explore the sources of that heterogeneity. Subsequently, a funnel plot was constructed, and Egger’s test was used to analyze publication bias. If publication bias was detected, the trim and fill method was used to correct it.
3 Result
3.1 Search results
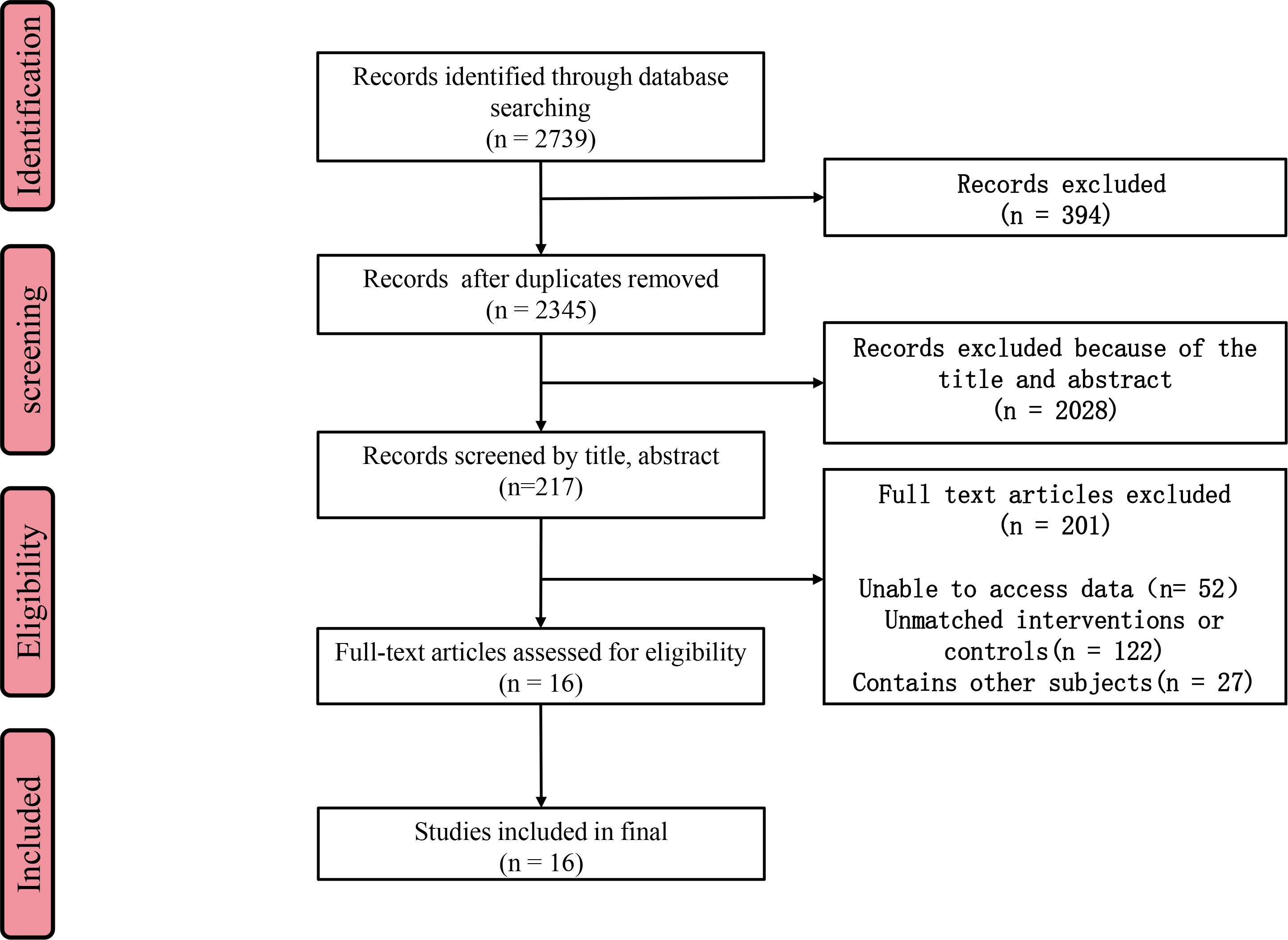
A total of 2739 studies were initially collected from the database for meta-analysis. After removing 394 duplicate studies, 2345 studies remained. Following the evaluation of titles and abstracts, 2028 studies were excluded. Subsequently, a full-text review of 217 potentially relevant studies was conducted, during which 201 studies were deemed ineligible. Ultimately, only 16 publications met the inclusion criteria. Figure 1 provides the steps involved in the screening procedure.
3.2 Study characteristics
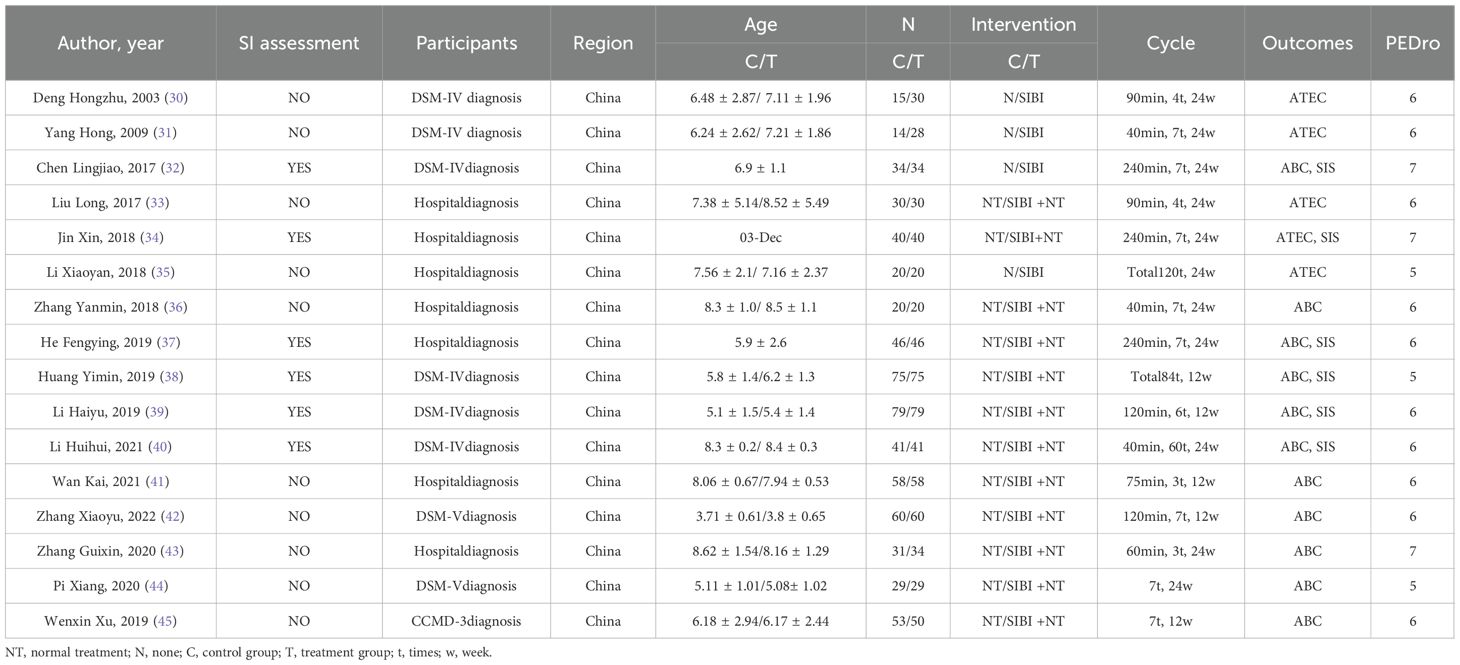
A total of 16 studies included 1, 319 ASD patients, with 645 in the control group and 674 in the intervention group. All ASD patients were diagnosed in hospitals or through specialized diagnostic scales, with an average age of under 10 years. The duration of SIBI ranged from 12 to 24 weeks, with the frequency of intervention sessions varying from 3 to 7 times per week, and each session lasting between 40 and 240 minutes. Five studies used the ATEC as an outcome measure, eleven studies used the ABC as an outcome measure, and six studies used the SIS as an outcome measure (Table 1). The PEDro results indicate that the quality scores of all literature ranged from 5 to 7, suggesting medium-quality literature (Supplementary Table 1). The specific components of the SIBI applied in the included studies are presented in Supplementary Table 2.
3.3 The effect of SIBI on SIS in autistic children
The SIS is used to assess children’s sensory integration abilities and includes three dimensions, vestibular balance, tactile defensiveness, and proprioception. SIS was used as an outcome measure to evaluate the effect of SIBI on sensory integration ability in autistic children. The SIS was developed by Professor Zheng Xinxiong from Taiwan, based on the checklist presented in “Sensory Integration and the Child” from the University of Southern California (46). The SIS has since been widely applied in clinical and research settings across China. In terms of total SIS scores, 3 studies met the inclusion criteria, with 136 participants receiving SIBI and 136 participants assigned to the control group. (Figure 2A). Due to statistically insignificant heterogeneity (I2 = 0%, P>0.05), a fixed-effect model was applied in the meta-analysis. Considering the combined effects, a statistically significant improvement was observed [MD = 11.53, 95% CI (10.53, 12.53)]. A diamond-shaped square on the right side of the zero line crosses it, indicating that compared to the control group, the SIBI effectively enhances sensory integration ability in children with ASD.
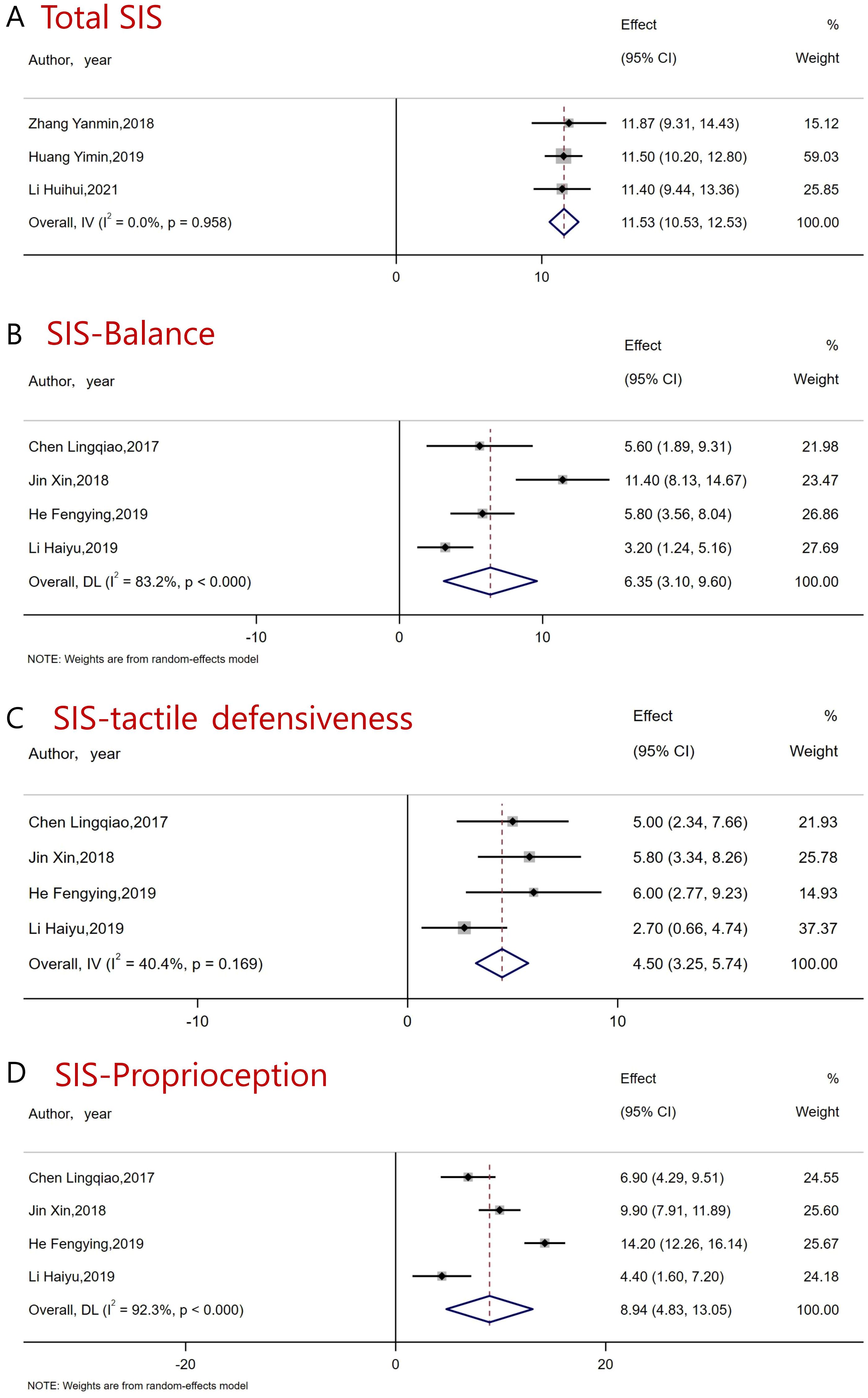
Figure 2. Forest plot of the effects of SIBI intervention on sensory integration abilities in autistic children. (A) Total SIS (B) Balance (C) Tactile defensiveness (D) Proprioception.
First, in the balance dimension, a total of 4 studies met the inclusion criteria and were included. Due to statistically significant heterogeneity (I2 = 83.2%, P<0.05), a random-effect model was applied in the meta-analysis. The results showed that balance ability in autistic children was significantly improved after SIBI [MD = 6.35, 95% CI (3.10, 9.60)] (Figure 2B). Then, in the dimension of tactile defensiveness, a total of four studies met the inclusion criteria and were included. Due to statistically insignificant heterogeneity (I2 = 40.4%, P>0.05), a fixed-effect model was applied in the meta-analysis. The results showed that tactile defensiveness in autistic children was significantly improved after SIBI [MD = 5.50, 95% CI (3.25, 5.47)] (Figure 2C). Finally, in the proprioception dimension, a total of four studies met the inclusion criteria and were included. Due to statistically significant heterogeneity (I2 = 92.3%, P<0.05), a random-effects model was applied in the meta-analysis. The results showed that proprioception in autistic children significantly improved after SIBI [MD = 8.94, 95% CI (4.83, 13.50)] (Figure 2D). Overall, although high heterogeneity was observed in the balance and proprioception subdimensions, the results for the total SIS score were robust with low heterogeneity. This indicates that SIBI can significantly enhance the sensory integration abilities of autistic children.
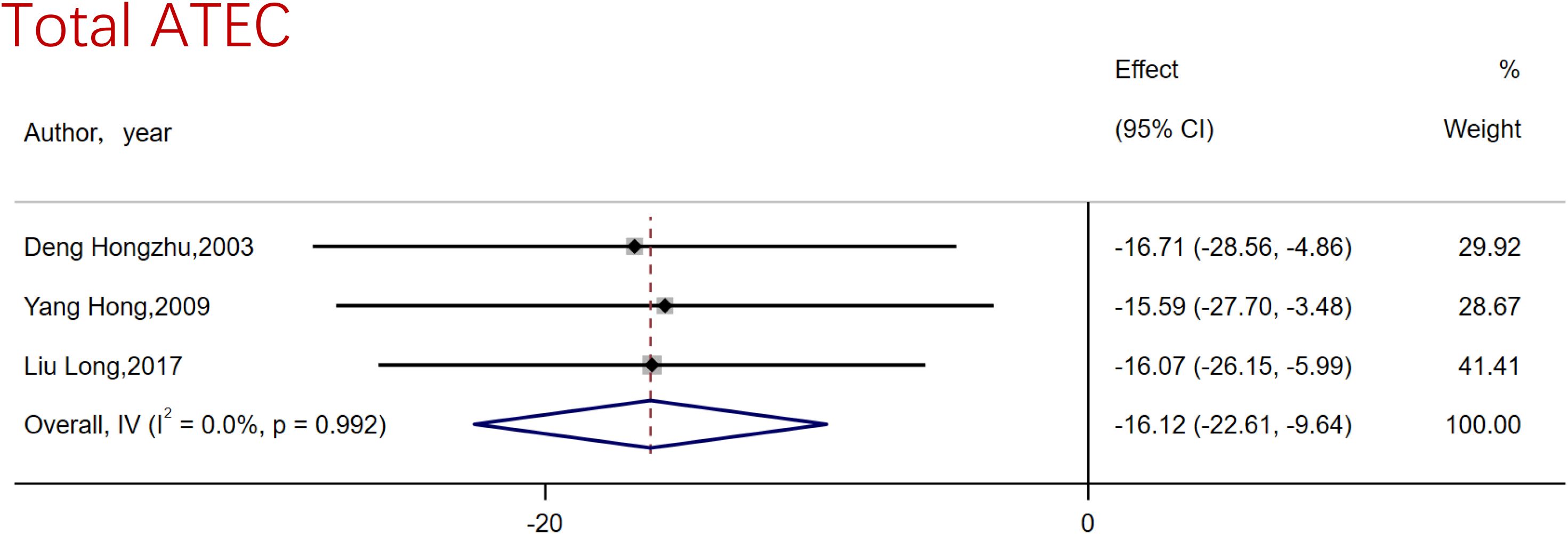
3.4 The effect of SIBI on ATEC in autistic children
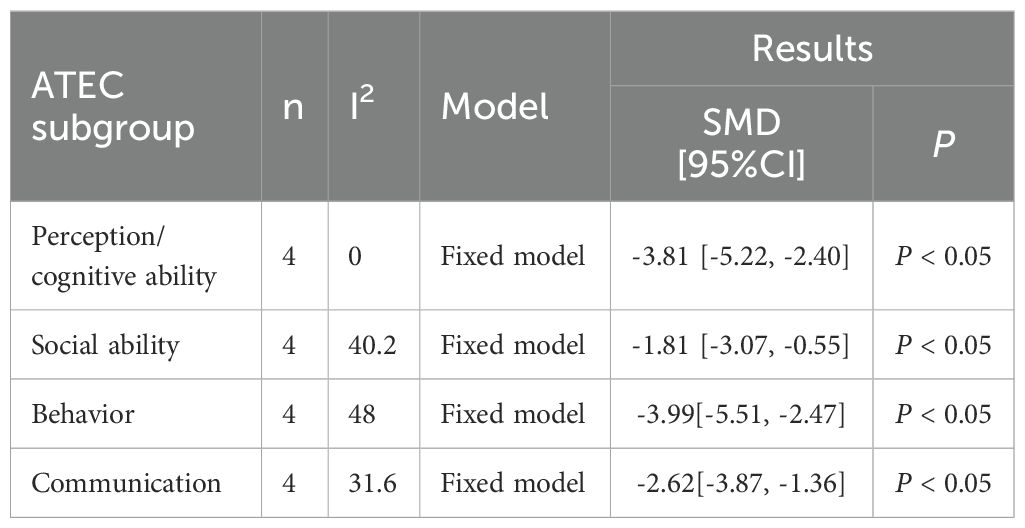
The ATEC assessment scale is a tool for evaluating symptoms and treatment effects in autistic children. It covers the performance of autistic children in perception/cognitive ability, social ability, behavior, and communication aspects. Regarding the total ATEC score, 3 studies met the inclusion criteria, with 90 participants receiving SIBI intervention and 59 participants assigned to the control group. (Figure 3). On account of statistically insignificant heterogeneity (I2 = 0%, P>0.05), a fixed-effect model was used for meta-analysis. The results showed that SIBI effectively reduced the total ATEC score of autistic children [MD=-16.12, 95%CI (-22.61, -9.64)], indicating that SIBI has a significant alleviating effect on autism-related behaviors in autistic children. Firstly, in perception/cognitive ability, due to statistically insignificant heterogeneity (I2 = 0%, P>0.05), a fixed-effect model was used for meta-analysis. The results showed that SIBI effectively improved the perception/cognitive ability score of autistic children [MD=-3.81, 95%CI (-5.22, -2.40)]. Secondly, in social ability, 4 studies met the inclusion criteria. Due to statistically insignificant heterogeneity (I2 = 0%, P>0.05), a fixed-effect model was used for meta-analysis. The results showed that SIBI could effectively improve the social ability of autistic children [MD=-1.81, 95%CI (-3.07, -0.55)]. Thirdly, regarding behavior, 4 studies met the inclusion criteria. Due to statistically insignificant heterogeneity (I2 = 0%, P>0.05), a fixed-effect model was used for meta-analysis. The results showed that SIBI could effectively improve the behavioral abilities of autistic children [MD=-3.99, 95%CI (-5.51, -2.47)]. Finally, in terms of communication skills, 4 studies met the inclusion criteria. Due to statistically insignificant heterogeneity (I2 = 0%, P>0.05), a fixed-effect model was used for meta-analysis. The results showed that SIBI could effectively improve the communication skills of autistic children [MD=-2.62, 95%CI (-3.87, -1.36)] (Table 2). Overall, SIBI has a significant effect on improving the total scores of ATEC and the scores of various sub-dimensions in autistic children, with low heterogeneity and robust results. This indicates that SIBI can significantly improve the autistic behaviors of autistic children.
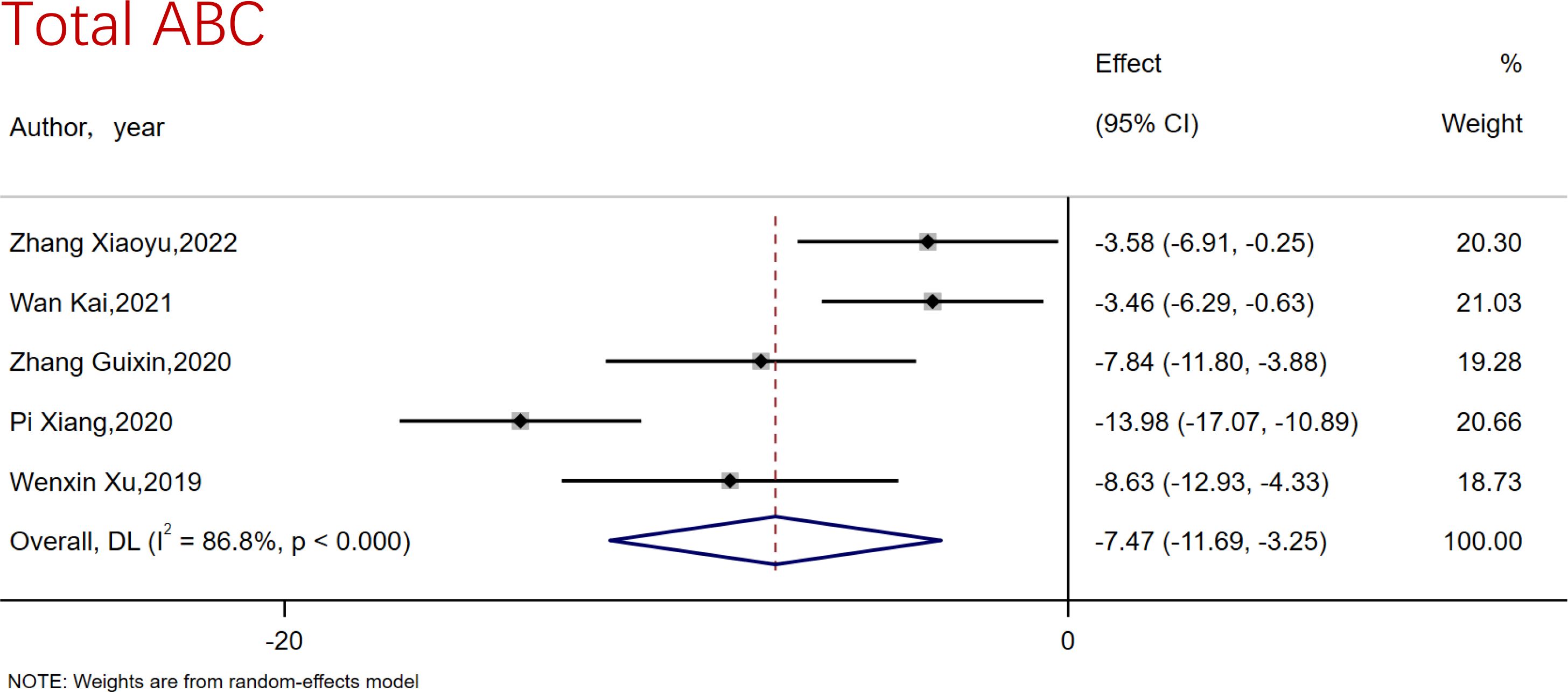
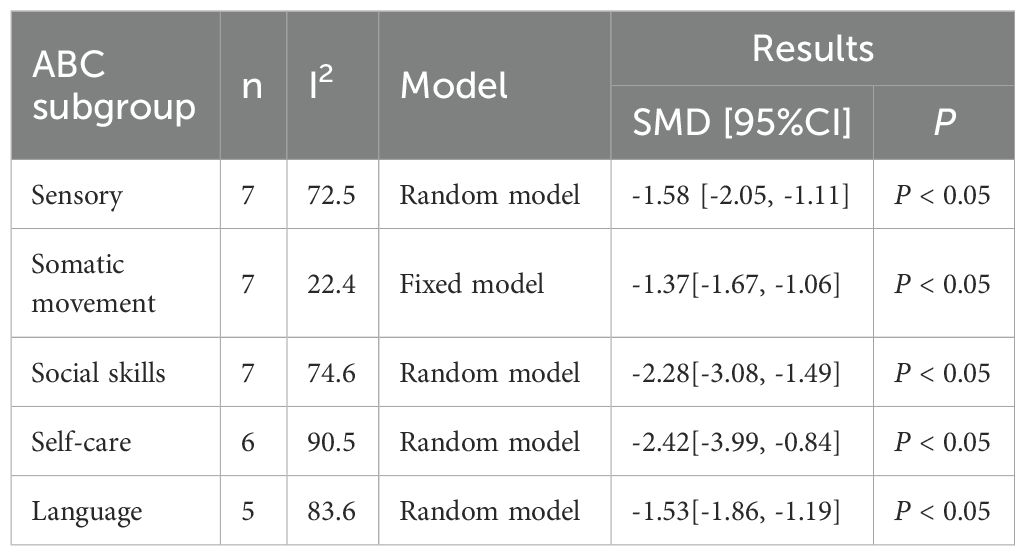
3.5 The effect of SIBI on ABC in autistic children
The ABC assessment scale serves as a tool to evaluate the severity of autistic children, encompassing sensory, physical movement, social skills, self-care, and language abilities. Concerning the total ABC score, 5 studies met the inclusion criteria, with 231 participants receiving SIBI and 231 participants assigned to the control group. The result of heterogeneity analysis indicated significant heterogeneity (I2 = 86.8%) (Figure 4). A random-effects model was employed for meta-analysis. The findings reveal that SIBI effectively reduces the total ABC score in autistic children [MD=-16.12, 95%CI (-22.61, -9.64)], suggesting that SIBI beneficially modifies autistic behaviors in these children (Figure 4). Firstly, in the area of Sensory, a total of 7 studies met the inclusion criteria. The heterogeneity results indicated statistically significant heterogeneity (I2 = 72.5%, P<0.05), and a random-effects model was employed for the meta-analysis. The results showed that SIBI can effectively reduce sensory issues in autistic children [MD=-1.58, 95%CI (-2.05, -1.11)]. Secondly, regarding Somatic movement, 7 studies met the inclusion criteria. The results indicated insignificant heterogeneity (I2 = 22.4%, P>0.05), and a fixed-effects model was used for statistical analysis. The results demonstrated that SIBI can significantly improve Somatic movement issues in autistic children [MD=-1.37, 95%CI (-1.67, -1.06)]. Thirdly, in the domain of social skills, 7 studies met the inclusion criteria. The results revealed significant heterogeneity (I2 = 74.6%, P>0.05), and a random-effects model was applied for statistical analysis. The findings showed that SIBI can significantly alleviate social skills issues in autistic children [MD=-2.28, 95%CI (-3.08, -1.49)]. Then, in terms of Self-care, 6 studies met the inclusion criteria. The results indicated significant heterogeneity (I2 = 90.5%, P<0.05), and a random-effects model was utilized for statistical analysis. The results demonstrated that SIBI can significantly enhance Self-care issues in autistic children [MD=-2.42, 95%CI (-3.99, -0.84)]. Finally, in the area of language, 5 studies met the inclusion criteria. The results showed significant heterogeneity (I2 = 83.6%, P<0.05), and a random-effects model was employed for statistical analysis. The findings indicated that SIBI can significantly improve language issues in autistic children [MD=-1.53, 95%CI (-1.86, -1.19)] (Table 3). Overall, SIBI has a significant effect on improving the total scores of ABC and the scores of various sub-dimensions in autistic children, but there is high heterogeneity, and the results are not robust, with only the Somatic movement sub-dimension showing low heterogeneity.
3.6 Publication bias detection
In this study, the Egger test and funnel plots were utilized to assess publication bias. Regarding the improvement of SIS by SIBI, the Egger test results indicated p>0.05, suggesting no evidence of publication bias. In the context of SIBI’s effect on improving the total ATEC score, the Egger test results also showed p>0.05, indicating no publication bias. Similarly, for the improvement of the total ABC score by SIBI, the Egger test results revealed p>0.05, signifying no publication bias. Concurrently, the analysis of the funnel plot yielded consistent results, as illustrated in Figure 5.
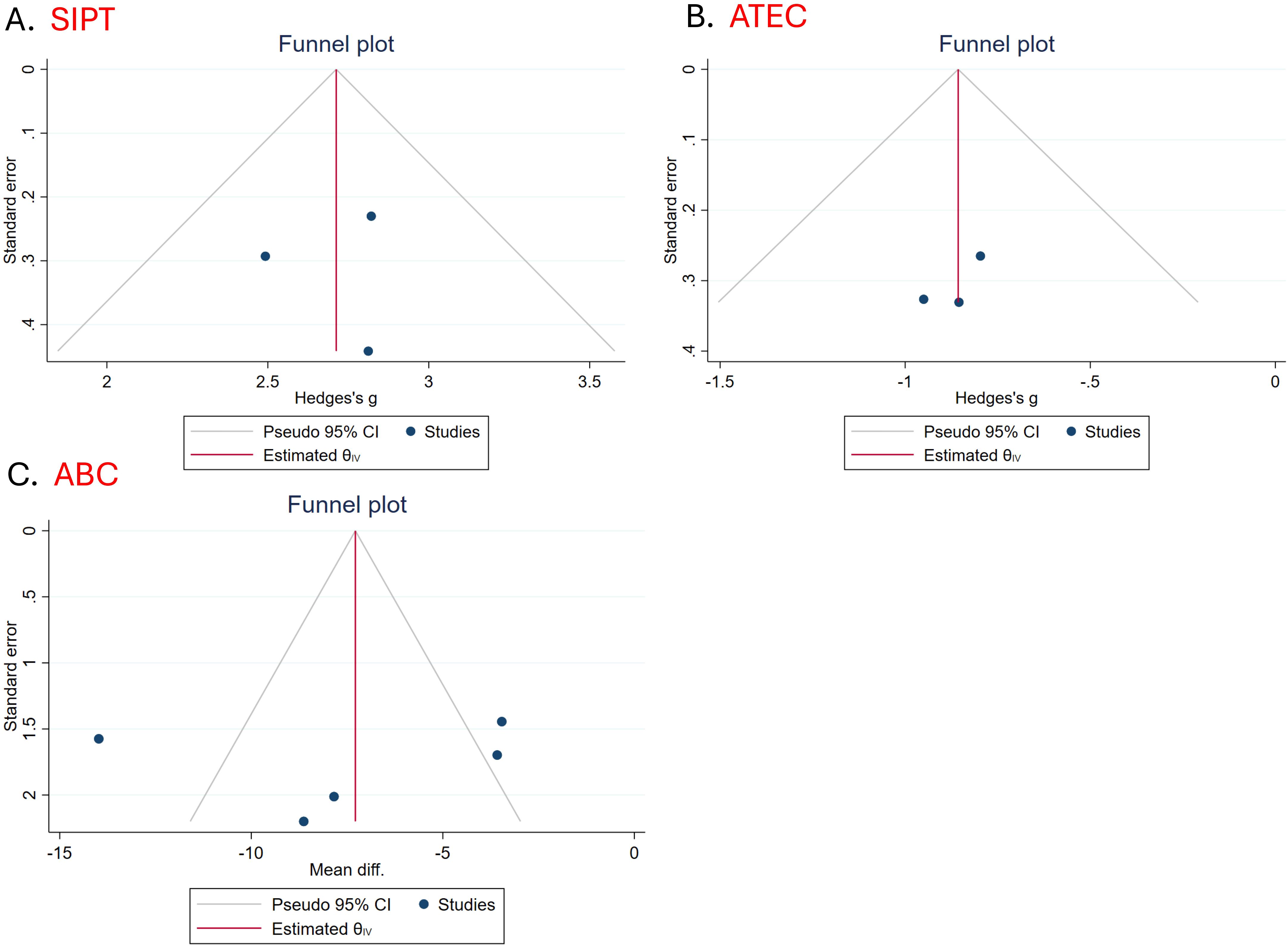
Figure 5. Funnel plot (A) Funnel plot of the impact of SIBI on SIS (B) Funnel plot of the impact of SIBI on ATEC (C) Funnel plot of the impact of SIBI on ABC.
3.7 Meta regression analyses
In order to examine the heterogeneity of the effects of SIBI on the total ABC score in autistic children, a meta-regression analysis was conducted to identify variables that may influence the intervention outcomes. The results of the regression analysis indicated that age did not have a significant effect on the total score of the ABC scale improved by SIBI in autistic children (β=0.33, P>0.05, 95%CI[-2.33, 3.00]) (Figure 6B). However, the number of intervention weeks had a significant impact on the effectiveness of SIBI in reducing the total ABC score, demonstrating that a longer duration of intervention weeks was associated with a greater reduction in the total ABC score (β=-0.51, P<0.05, 95%CI[-1.01, -0.01]) (Figure 6A).
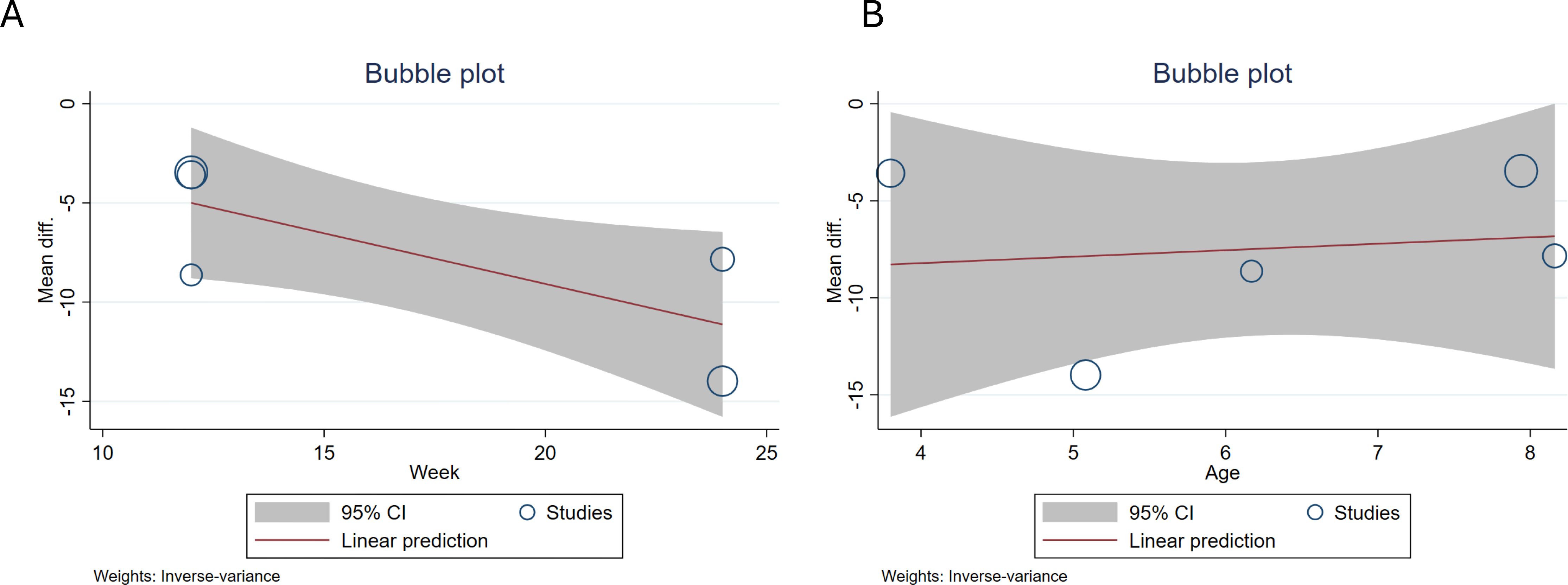
Figure 6. Meta-regression analysis bubble plot of the effects of SIBI on ABC in autistic children (A) The impact of the number of intervention weeks on the results. (B) The impact of age on the results.
4 Discussion
This meta-analysis investigated the impact of SIBI on sensory processing abilities and autism-related behaviors in autistic children. The analysis provides empirical evidence regarding the efficacy of SIBI in enhancing sensory processing capabilities and ameliorating autism-related behaviors.
Our research findings indicate that SIBI can effectively enhance the sensory integration abilities of autistic children in three aspects: balance, tactile defensiveness, and proprioception. Additionally, the heterogeneity test results show that the improvement of the total SIS score for autistic children through SIBI is robust (I2<50%). In normally developing children, sensory integration dysfunction significantly impacts learning, behavior, and social communication. This phenomenon can be ameliorated through targeted interventions (47). SIBI is a method that helps individuals regulate their neurological functions and promotes the integration and processing of environmental information through systematic intervention. This approach is based on the principles of neuroplasticity, facilitating the brain’s hierarchical processing of multisensory signals by integrating information received from different sensory modalities (19). As a result, it coordinates the body’s adaptive responses to external environmental stimuli and internal physiological states. By reinforcing the information integration capabilities of the nervous system through targeted training, SIBI can effectively enhance children’s behavioral organization levels, specifically reflected in improvements in joint attention, increased proactivity in social interactions, enhanced motor coordination, and improved sensory discrimination skills (48). The SIS scale encompasses sensory integration ability assessments across three dimensions: balance, tactile defensiveness, and proprioception. Maintaining balance necessitates the integration of diverse information from the vestibular, visual, and proprioceptive systems to effectively sustain equilibrium (49). Individuals with autism face greater challenges in balance (50). Further research indicates that postural and balance difficulties are related to other autistic characteristics, such as social communication deficiencies and repetitive behaviors (51, 52). SIBI appears to have a compensatory effect on sensory input deficits in children with ASD, particularly in the areas of visual, vestibular perception, and proprioception. SIBI can enhance the balance abilities of children with ASD by modulating the corresponding posture control mechanisms in different brain regions (25). Moreover, fNIRS evidence indicates that the enhanced neural activation in specific regions of the PFC highlights the role of SIBI in cognitive improvement, including inhibitory control and cognitive flexibility (53). However, this emerging compensatory effect deserves further exploration in future studies utilizing more sophisticated neuroscientific instruments.
Sensory integration disorder is not exclusive to individuals with ASD, but it is crucial to study SIBI in ASD children because this anomaly is commonly found in ASD patients and has a relatively high prevalence. Some atypical sensory behaviors can be clearly observed in autistic children in the early stages of life (around 1 year old), and these behaviors are more common in infancy and childhood than in adulthood (54). Research has shown that children with ASD exhibit several different atypical sensory patterns, including hyperresponsiveness (HYPER), hyporesponsiveness (HYPO), and sensory interests, repetitions, and seeking behaviors (SIRS), as well as the potential role of sensory processing as a crucial component of higher social and cognitive functions. Additionally, the atypical sensory behaviors displayed by individuals with sensory integration disorder are also part of the diagnostic criteria for core symptoms of autism spectrum disorder in DSM-5. Individuals with ASD exhibit abnormalities in central sensory processing, and these atypical characteristics related to the integration of somatosensory information are associated with an increase in autistic traits, further supported by the neurobiological characteristics of ASD (55, 56). The sensory processing abnormalities in children with ASD not only impair their sensory integration abilities but also have a significant impact on their behavioral issues, including core symptoms (12). Therefore, improving the sensory integration abilities of individuals with ASD may have significant benefits for the improvement of their core symptoms.
SIBI is a program that can enhance their sensory integration abilities. In individuals with autism, SIBI can reduce stereotypical behaviors, improve self-care and social interaction abilities, and positively influence motor skills, socialization, attention, behavior control, reading skills, participation in play activities, and the achievement of personal goals (16, 20). The meta-analysis results also found similar outcomes. SIBI not only improves sensory integration abilities in autistic children but also alleviates their autistic behaviors. SIBI can effectively reduce the total scores of the ATEC scale and the ABC scale in autistic children. The ATEC scale includes four dimensions: perception/cognitive ability, social ability, behavior, and communication. The results show that SIBI can effectively reduce both the total score and the symptom scores of each sub-dimension on the ATEC scale, and importantly, the results are robust (I2 < 50%). Additionally, the ABC scale, which is an autistic behavior assessment scale that can be used by parents, includes 5 dimensions: Sensory, Somatic Movement, Social Skills, Self-Care, and Language. The meta-analysis also found that the SIBI can reduce the total score of the ABC scale and the scores of each sub-dimension for autistic children. However, the results of the meta-analysis showed high heterogeneity. We then used meta-regression to examine the sources of heterogeneity, and the results indicated that the intervention cycle of SIBI is a source of heterogeneity affecting the overall score of the ABC scale. At the same time, this result highlights that a longer intervention cycle is associated with better improvement effects on the total score of the ABC. These results indicate that SIBI can not only directly improve the sensory integration ability of children with autism but also enhance their social cognitive function by reinforcing these fundamental abilities, thereby improving their social skills, language skills, and self-care abilities. The potential mechanism underlying these results may be due to the continuous SIBI providing comfortable sensory stimulation for children with autism, enabling them to reach an appropriate level of arousal through sensory input, and that SIBI stimulation can develop their visual processing abilities, influencing changes in their psychological and social functions through changes in physical abilities (57, 58).
These findings underscore the importance of SIBI in enhancing sensory integration processing abilities and improving autism-related behaviors, providing support for non-pharmacological interventions in autism treatment based on neuroplasticity. However, there are still some difficulties in the implementation of SIBI for ASD currently, such as the distinction between SIBI and sensory-based interventions in practical applications. SIBI is an important rehabilitation approach for ASD and must be strictly performed according to ASI principles to ensure the effectiveness of the intervention.
Recent international systematic reviews and empirical studies on ASI have provided increasing evidence that this intervention can improve social participation, communication, and sensory processing in autistic children across different cultural contexts (23). Our findings based on Chinese studies are generally consistent with these outcomes, particularly in demonstrating improvements in core autistic behaviors and sensory integration function. However, several differences are noteworthy. First, the version of SIBI applied in China is an adaptation developed by Professor Wen-De Chen in collaboration with Peking Medical University, based on ASI and modified to fit the Chinese cultural context. Next, compared with international studies, Chinese trials often focus on symptom reduction scales such as the ABC or SIS rather than on functional outcomes. In contrast, contemporary international research has increasingly emphasized ecologically valid measures, including Goal Attainment Scaling (GAS), activities of daily living (ADLs), social skills, and reductions in caregiver burden. These similarities and differences suggest that while ASI holds promise in the Chinese context, future research would benefit from adopting internationally recognized fidelity measures and incorporating more functional outcome indicators. Such efforts would not only enhance the comparability of Chinese studies with global evidence but also provide stronger guidance for clinical practice.
Current guidelines for ASI research emphasize that assessment of ASI concerns should be conducted prior to intervention to ensure appropriate participant inclusion and accurate evaluation of treatment effects. However, in this review, we found that several included studies did not perform formal SI assessments before intervention, and some provided insufficient information regarding assessment procedures. This inconsistency reflects the fact that a number of studies were conducted before such standards were widely adopted. The absence of standardized pre-intervention SI assessment represents a major limitation of the present review and highlights the need for future studies to implement rigorous assessment protocols to enhance the validity of intervention outcomes. Although praxis difficulties are known to occur in a large proportion of children with autism and represent a core aspect of sensory integration, most of the studies included in this review did not specifically assess or report praxis-related outcomes. Consequently, the absence of praxis assessment limits the ability to fully evaluate the intervention’s effectiveness, and future studies should incorporate standardized measures of praxis to provide a more comprehensive understanding of sensory integration-based interventions in children with autism.
5 Conclusion
This study aims to provide theoretical evidence for the effectiveness of SIBI by exploring its impact on children with autism. The results indicate that SIBI can effectively improve the sensory integration ability and autism-related behaviors of autistic children. Furthermore, the intervention effects gradually increase with the duration of SIBI. Additionally, this study has some limitations, including that the sample comprised only Chinese children with autism, the number of studies included is relatively small, and dissertations were excluded. Future research needs to include larger samples and high-quality RCT experiments from an international perspective to support these findings.
6 Limitation
All randomized controlled trials were conducted in China. Therefore, these findings may have limited generalizability to other regions and cultural backgrounds.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author contributions
BL: Data curation, Writing – original draft, Software. YB: Software, Data curation, Formal Analysis, Writing – original draft, Methodology. DM: Formal Analysis, Methodology, Writing – original draft. NL: Formal Analysis, Data curation, Writing – original draft, Funding acquisition. LF: Methodology, Conceptualization, Funding acquisition, Writing – review & editing, Writing – original draft. YX: Writing – review & editing, Writing – original draft, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1623149/full#supplementary-material
References
1. Lord C, Brugha TS, Charman T, Cusack J, Dumas G, Frazier T, et al. Autism spectrum disorder. Nat Rev Dis Primers. (2020) 6:5. doi: 10.1038/s41572-019-0138-4
2. Levy SE, Mandell DS, and Schultz RT. Autism. Lancet. (2009) 374:1627–38. doi: 10.1016/S0140-6736(09)61376-3
3. Lord C, Elsabbagh M, Baird G, and Veenstra-Vanderweele J. Autism spectrum disorder. Lancet. (2018) 392:508–20. doi: 10.1016/S0140-6736(18)31129-2
4. Emberti Gialloreti L, Mazzone L, Benvenuto A, Fasano A, Alcon AG, Kraneveld A, et al. Risk and protective environmental factors associated with autism spectrum disorder: evidence-based principles and recommendations. J Clin Med. (2019) 8:217. doi: 10.3390/jcm8020217
5. Baxter AJ, Brugha TS, Erskine HE, Scheurer RW, Vos T, and Scott JG. The epidemiology and global burden of autism spectrum disorders. psychol Med. (2015) 45:601–13. doi: 10.1017/S003329171400172X
6. Maenner MJ, Warren Z, Williams AR, Amoakohene E, Bakian AV, Bilder DA, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2020. Mmwr Surveill Summ. (2023) 72:1–14. doi: 10.15585/mmwr.ss7202a1
7. Zhou H, Xu X, Yan W, Zou X, Wu L, Luo X, et al. Prevalence of autism spectrum disorder in China: A nationwide multi-center population-based study among children aged 6 to 12 years. Neurosci Bull. (2020) 36:961–71. doi: 10.1007/s12264-020-00530-6
8. Tateno Y, Kumagai K, Monden R, Nanba K, Yano A, Shiraishi E, et al. The efficacy of early start denver model intervention in young children with autism spectrum disorder within Japan: A preliminary study. Soa Chongsonyon Chongsin Uihak. (2021) 32:35–40. doi: 10.5765/jkacap.200040
9. Warren Z, Veenstra-VanderWeele J, Stone W, Bruzek JL, Nahmias AS, Foss-Feig JH, et al. “Therapies for Children with Autism Spectrum Disorders,” in Therapies for Children with Autism Spectrum Disorders. United states: Rockville (MD (2011).
10. Leekam SR, Nieto C, Libby SJ, and Gould J. Describing the sensory abnormalities of children and adults with autism. J Autism Dev Disord. (2007) 37:894–910. doi: 10.1007/s10803-006-0218-7
11. Rogers SJ and Ozonoff S. Annotation: What do we know about sensory dysfunction in autism? A critical review of the empirical evidence. J Child Psychol Psychiatry. (2005) 46:1255–68. doi: 10.1111/j.1469-7610.2005.01431.x
12. Cummins RA. Sensory integration and learning-disabilities - ayres factor-analyses reappraised. J Learn Disabil. (1991) 24:160–8. doi: 10.1177/002221949102400304
13. Weitlauf AS, Sathe N, McPheeters ML, and Warren ZE. Interventions targeting sensory challenges in autism spectrum disorder: A systematic review. Pediatrics. (2017) 139:e20170347. doi: 10.1542/peds.2017-0347
14. Ayres AJ. Sensory integration and learning disorder. CA: Western PsychologicalServices, Los Angeles (1972).
15. Oh S, Jang JS, Jeon AR, Kim G, Kwon M, Cho B, et al. Effectiveness of sensory integration therapy in children, focusing on Korean children: A systematic review and meta-analysis. World J Clin cases. (2024) 12:1260–71. doi: 10.12998/wjcc.v12.i7.1260
16. May-Benson TA and Koomar JA. Systematic review of the research evidence examining the effectiveness of interventions using a sensory integrative approach for children. Am J Occup Ther. (2010) 64:403–14. doi: 10.5014/ajot.2010.09071
17. Schoen SA, Lane SJ, Mailloux Z, May-Benson T, Parham LD, Roley SS, et al. A systematic review of ayres sensory integration intervention for children with autism. Autism Res. (2019) 12:6–19. doi: 10.1002/aur.2046
18. Tzang RF, Chang YC, Kao KL, Huang YH, Huang HC, Wang YC, et al. Increased risk of developing psychiatric disorders in children with attention deficit and hyperactivity disorder (ADHD) receiving sensory integration therapy: a population-based cohort study. Eur Child Adoles Psy. (2019) 28:247–55. doi: 10.1007/s00787-018-1171-7
19. Pfeiffer BA, Koenig K, Kinnealey M, Sheppard M, and Henderson L. Effectiveness of sensory integration interventions in children with autism spectrum disorders: a pilot study. Am J Occup Ther. (2011) 65:76–85. doi: 10.5014/ajot.2011.09205
20. Schaaf RC, Benevides T, Mailloux Z, Faller P, Hunt J, Van Hooydonk E, et al. An intervention for sensory difficulties in children with autism: a randomized trial. J Autism Dev Disord. (2014) 44:1493–506. doi: 10.1007/s10803-014-2111-0
21. Goin-Kochel RP, Mackintosh VH, and Myers BJ. Parental reports on the efficacy of treatments and therapies for their children with autism spectrum disorders. Res Autism Spectr Disord. (2009) 3:528–37. doi: 10.1016/j.rasd.2008.11.001
22. Watling R, Deitz J, Kanny EM, and McLaughlin JF. Current practice of occupational therapy for children with autism. Am J Occup Ther. (1999) 53:498–505. doi: 10.5014/ajot.53.5.498
23. Acuña C, Gallegos-Berrios S, Barfoot J, Meredith P, and Hill J. Ayres sensory integration® With children ages 0 to 12: A systematic review of randomized controlled trials. Am J Occup Ther. (2025) 79:7903205180. doi: 10.5014/ajot.2025.051023
24. Parham LD, Roley SS, May-Benson TA, Koomar J, Brett-Green B, Burke JP, et al. Development of a fidelity measure for research on the effectiveness of the ayres sensory integration® Intervention. Am J Occup Ther. (2011) 65:133–42. doi: 10.5014/ajot.2011.000745
25. Schoen SA, Lane SJ, Mailloux Z, May-Benson T, Parham LD, Smith Roley S, et al. A systematic review of ayres sensory integration intervention for children with autism. Autism Res. (2019) 12:6–19. doi: 10.1002/aur.2046
26. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Internal Med. (2015) 162:777–84. doi: 10.7326/M14-2385
27. Elkins MR, Moseley AM, Sherrington C, Herbert RD, and Maher CG. Growth in the Physiotherapy Evidence Database (PEDro) and use of the PEDro scale. Br J Spts Med. (2013) 47:188–9. doi: 10.1136/bjsports-2012-091804
28. Wende C. Guidebook for children with learning difficulties: positive sensory integration therapy. China: China Children’s Publishing House (1996).
29. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
30. Hongzhu D, Xiaobing Z, Chun T, Jianying L, Yuuanyuan Z, Yuehua Y, et al. A study on the recent efficacy of sensory integration training in the treatment of childhood autism. J Pract Med. (2003) 19:984–6. doi: 10.3969/j.issn.1006-5725.2003.09.021
31. Hong Y. Analysis of factors influencing the efficacy of sensory integration training in treating childhood loneliness syndrome. HL Med J. (2009) 33:35–7. doi: 10.3969/j.issn.1004-5775.2009.01.011
32. Lingjiao C, Wenhui H, and Mian C. The improvement effect of sensory integration therapy on sensory dysfunction and behavioral symptoms in children with autism. Chin J Rural Med Pharm. (2017) 24:37–8. doi: 10.19542/j.cnki.1006-5180.001134
33. Long L. Analysis of the therapeutic effect of sensory integration therapy on autism in children. Guide China Med. (2017) 15:186. doi: 10.15912/j.cnki.gocm.2017.10.145
34. Xin J. The improvement effect of sensory integration training on sensory dysfunction and behavioral symptoms in children with autism. Diet Health. (2018) 5:65–6.
35. Xiaoyan L. Analysis of the therapeutic effect of sensory integration training on autism in children. Clin J Traditional Chin Med. (2018) 30:2117–9. doi: 10.3969/j.issn.2095-8439.2018.14.076
36. Yanmin Z and Qing S. Observation of the application effect of sensory integration training in the rehabilitation of children with autism. Med J Chin People’s Health. (2018) 30:78–83. doi: 10.3969/j.issn.1672-0369.2018.23.037
37. Fengying H, Xiaoying L, Xiaoyan L, Cuifang Z, Hongguang M, and Lanying H. The improvement effect of sensory integration training on sensory dysfunction and behavioral symptoms in children with autism. Special Health. (2019) 16:219–20. doi: 10.3969/j.issn.2095-6851.2019.16.284
38. Yimin H. The impact of sensory integration training on the rehabilitation outcomes of children with autism. Pract Clin J Integr Traditional Chin West Med. (2019) 19:107–8. doi: 10.13638/j.issn.1671-4040.2019.10.053
39. Haiyu L. Analysis of the application effect of sensory integration training in children with autism. Pract Clin J Integr Traditional Chin West Med. (2019) 19:103–4. doi: 10.13638/j.issn.1671-4040.2019.12.053
40. Huihui L. Analysis of the impact of sensory integration training on children with autism. China Cont Med Educ. (2021) 13:93–6. doi: 10.3969/j.issn.1674-9308.2021.17.026
41. Kai W, Qing S, Jingjie L, and Caiyun M. The effect of sensory integration training on the balance ability and ABC, CARS scores of children with autism. Chin J Pract Med. (2021) 48:53–6. doi: 10.3760/cma.j.cn115689-20210715-02319
42. Xiaoyu Z and Yanlei Z. The impact of sensory integration training based on the Denver model on the social skills and parental parenting pressure of children with autism spectrum disorder aged 2–5 years old. Chin Pediatr Integr Traditional West Med. (2022) 14:41–4. doi: 10.3969/j.issn.16743865.2022.01.011
43. Guixin Z and Yao W. Application of sensory integration training in the treatment of children with high functioning autism spectrum disorder. Henan Med Res. (2020) 29:5269–71. doi: 10.3969/j.issn.1004-437X.2020.28.035
44. Xiang P. The application effect of sensory integration training on cognitive and motor development in children with autism. China Mod Med. (2020) 27:103–6. doi: 10.3969/j.issn.1674-4721.2020.12.030
45. Xu W, Yao J, and Liu W. Intervention effect of sensory integration training on the behaviors and quality of life of children with autism. Psych Danub. (2019) 31:340–6. doi: 10.24869/psyd.2019.340
46. Xinxiong Z. Children’s sensory development checklist. Taiwan, China: Psychology Publishing House. p. (1998).
47. Critz C, Blake K, and Nogueira E. Sensory processing challenges in children. Jnp-J Nrs Pract. (2015) 11:710–6. doi: 10.1016/j.nurpra.2015.04.016
48. Watling R and Hauer S. Effectiveness of ayres sensory integration(R) and sensory-based interventions for people with autism spectrum disorder: A systematic review. Am J Occup Ther. (2015) 69:6905180030p1–12. doi: 10.5014/ajot.2015.018051
49. Bojanek EK, Wang Z, White SP, and Mosconi MW. Postural control processes during standing and step initiation in autism spectrum disorder. J Neurodev Disord. (2020) 12:1. doi: 10.1186/s11689-019-9305-x
50. Travers BG, Lee L, Klans N, Engeldinger A, Taylor D, Ausderau K, et al. Associations among daily living skills, motor, and sensory difficulties in autistic and nonautistic children. Am J Occup Ther. (2022) 76:7602205020. doi: 10.5014/ajot.2022.045955
51. Travers BG, Powell PS, Klinger LG, and Klinger MR. Motor difficulties in autism spectrum disorder: linking symptom severity and postural stability. J Autism Dev Disord. (2013) 43:1568–83. doi: 10.1007/s10803-012-1702-x
52. Radonovich KJ, Fournier KA, and Hass CJ. Relationship between postural control and restricted, repetitive behaviors in autism spectrum disorders. Front Integr Neurosci. (2013) 7:28. doi: 10.3389/fnint.2013.00028
53. Deng J, Lei T, and Du X. Effects of sensory integration training on balance function and executive function in children with autism spectrum disorder: evidence from Footscan and fNIRS. Front Psychol. (2023) 14:1269462. doi: 10.3389/fpsyg.2023.1269462
54. Ramappa S, Anderson A, Jung J, Chu R, Cummings KK, Patterson G, et al. An observed assessment of sensory responsivity in autism spectrum disorders: associations with diagnosis, age, and parent report. J Autism Dev Disord. (2023) 53:3860–72. doi: 10.1007/s10803-022-05653-5
55. Crane L, Goddard L, and Pring L. Sensory processing in adults with autism spectrum disorders. Autism. (2009) 13:215–28. doi: 10.1177/1362361309103794
56. Minshew NJ and Williams DL. The new neurobiology of autism: cortex, connectivity, and neuronal organization. Arch Neurol. (2007) 64:945–50. doi: 10.1001/archneur.64.7.945
57. Tanaka JW and Sung A. The “Eye avoidance” Hypothesis of autism face processing. J Autism Dev Disord. (2016) 46:1538–52. doi: 10.1007/s10803-013-1976-7
Keywords: autism spectrum disorder, sensory integration-based intervention, meta-analysis, children, systematic review
Citation: Lyu B, Ba Y, Ma D, Liu N, Fu L and Xue Y (2025) Effectiveness of sensory integration-based intervention in autistic children, focusing on Chinese children: a systematic review and meta-analysis. Front. Psychiatry 16:1623149. doi: 10.3389/fpsyt.2025.1623149
Received: 06 May 2025; Accepted: 22 October 2025;
Published: 19 November 2025.
Edited by:
Antonio Narzisi, Stella Maris Foundation (IRCCS), ItalyReviewed by:
Teresa A. May-Benson, TMB Educational Enterprises, LLC, United StatesSambasivamoorthy Sivayokan, University of Jaffna, Sri Lanka
Copyright © 2025 Lyu, Ba, Ma, Liu, Fu and Xue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Limin Fu, ZnVsaW1pbkBoZXBlYy5lZHUuY24=; Yaqi Xue, eHVleWFxaTU1NUBtYWlsLmJudS5lZHUuY24=
 Bingchen Lyu1
Bingchen Lyu1 Yaqi Xue
Yaqi Xue