- 1Center for Health Promotion and Prevention Research, School of Public Health, The University of Texas Health Science Center at Houston, Houston, TX, United States
- 2Department of Clinical Sciences, University of Texas Southwestern Medical Center, Dallas, TX, United States
Introduction: Effective interventions to increase HPV vaccination are needed to reach national vaccination goals and to reduce later HPV-related cancer disparities. We used Intervention Mapping (IM) to develop and adapt a theory- and evidence-based educational intervention targeting parents of Hispanic adolescents to increase HPV vaccination.
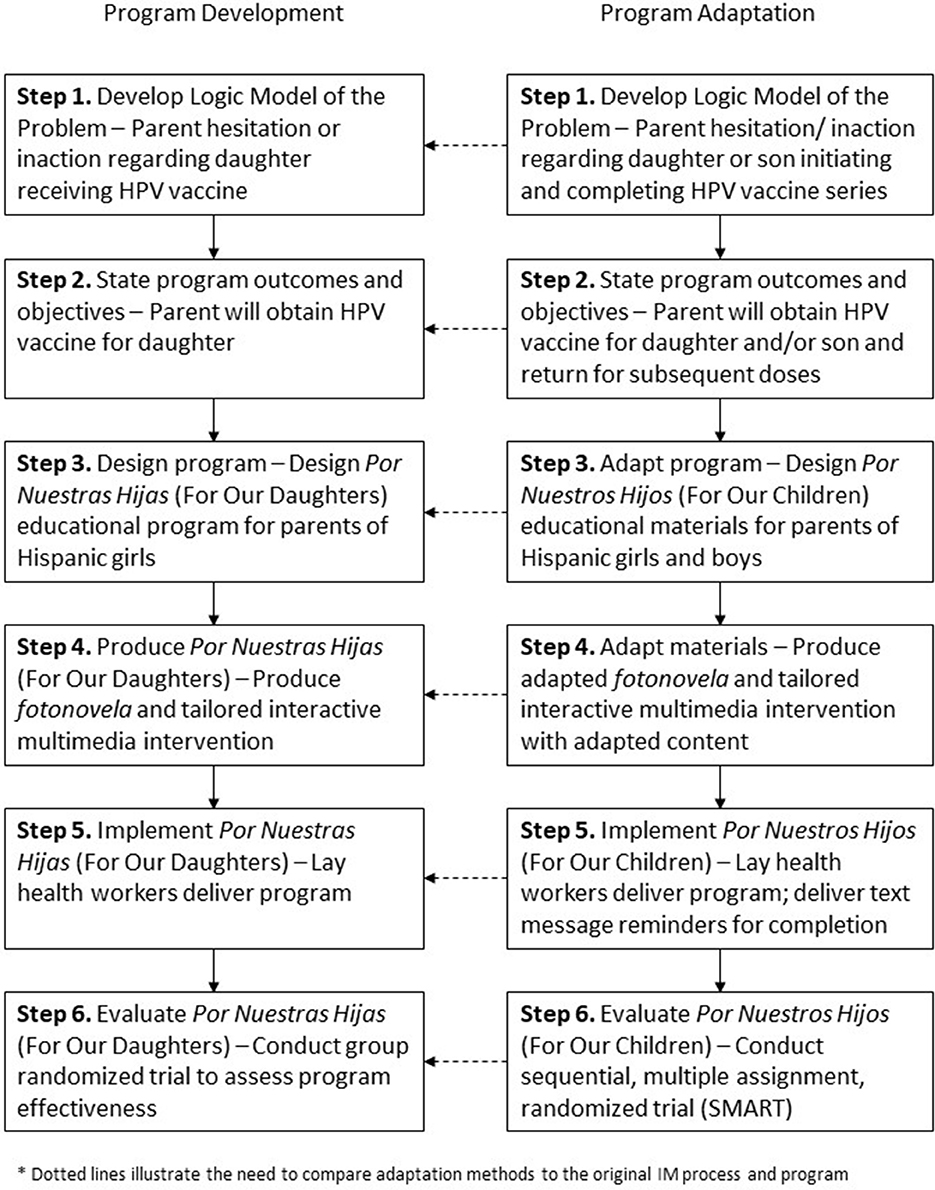
Methods: We followed IM steps 1–6 to: (1) develop a logic model and identify modifiable factors associated with vaccination among Hispanic adolescents by conducting literature reviews, focus groups, and in-depth interviews with Hispanic parents; (2) develop outcomes, write performance objectives, and develop a matrix of change objectives; (3) develop and identify a program theme, program components, theoretical methods, and practical applications; (4) develop an intervention design plan; (5) develop implementation strategies; and (6) develop an evaluation plan. We completed Steps 1–6 for to develop an intervention targeting parents of females, and we followed the steps again to adapt the program once HPV vaccine recommendations included males.
Results: The program Por Nuestras Hijas (For Our Daughters) included two components: a print fotonovela and a tailored interactive multimedia intervention (TIMI). The program utilized the methods tailoring, targeting, framing, anticipated regret, modeling, skill building, and education and counseling to target the following determinants: parental knowledge, attitudes, self-efficacy, skills, perceived benefits/barriers, perceived susceptibility, perceived norms, and outcome expectations as modifiable factors influencing HPV vaccination. Lay health workers implemented the program in community clinics. A logic model of change guided evaluation planning. We later adapted the outcome and intervention content for parents of Hispanic adolescent males and changed the theme to Por Nuestros Hijos (For Our Children). Throughout the development and adaptation processes, we relied on theory, empirical evidence, and new data to make decisions.
Discussion: IM provided a systematic methodology for program development and adaptation. Tasks in each step built upon one another integrating findings from the literature, previous research, qualitative findings, and theory to develop two educational programs for parents to increase HPV vaccination. The systematic process allowed us to develop messages and materials targeting factors beyond HPV knowledge or awareness to create behavior change.
Introduction
Persistent human papillomavirus (HPV) infection can lead to anogenital cancers, oropharyngeal cancer, and genital warts (1). In 2017, cervical cancer was the most prevalent HPV-related cancer with nearly 12,000 new cases per year in the United States (2). Cervical cancer disproportionality affects Hispanic women who have higher cervical cancer rates than their non-Hispanic counterparts and who have the second highest cervical cancer mortality rate after Black women (3, 4). Hispanic women also have lower cervical cancer screening rates than non-Hispanic women contributing to cervical cancer morbidity and mortality disparities (5).
The HPV vaccine can protect against the types of HPV that can lead to cervical cancer, other anogenital cancers, oropharyngeal cancer, and genital warts in both men and women. The Centers for Disease Control Advisory Committee for Immunization Practices (ACIP) recommends providers administer the HPV vaccine to adolescent males and females at ages 11–12 (6). While HPV vaccination rates in the United States have improved incrementally over the last several years, they remain below national benchmarks (7). Specifically among Hispanic adolescents, 68% of females aged 13–17 years, and 59% of males aged 13–17 years initiated the vaccine in 2015. However, only 46% of females and 35% of males completed the vaccine series (8). Theory- and evidence-based HPV vaccination interventions aimed at increasing series initiation and completion by targeting the multiple factors influencing vaccination rates are needed for Hispanic adolescent populations to reduce later cancer disparities (5, 9).
Theory- and evidence-based interventions have been shown to be more effective than non-theory based interventions (10). Intervention Mapping (IM) is a systematic framework for developing, implementing, and adapting theory- and evidence-based interventions (11). Cancer control and prevention researchers and program planners have used IM to develop interventions focused on sun safety and skin cancer prevention (12), smoking cessation (13) cervical cancer and breast cancer screening (14–19), and colorectal cancer screening (20). IM also provides a framework for developing implementation strategies for the adoption and implementation of interventions (21) and clinical guidelines (22) and for systematically adapting existing evidence-based programs (23).
This paper describes the use of IM to develop and adapt two interventions for parents aimed at increasing HPV vaccine uptake among Hispanic adolescents. These interventions were developed as part of a larger comparative effectiveness study to develop and evaluate a print vs. tailored intervention delivered by lay health workers in clinic settings. Initially, we followed IM to develop interventions focused exclusively on parents of Hispanic female adolescents to increase HPV vaccination among this population. The interventions, packaged as Por Nuestras Hijas (For Our Daughters), included a print fotonovela and a tailored interactive multimedia intervention (TIMI) delivered as an application on a tablet. Fotonovelas are brief print stories with pictures and dialog popular among Hispanic populations in conveying health information. Once recommendations changed and included HPV vaccination for boys, we used IM to adapt the interventions, repackaged as Por Nuestros Hijos (For Our Children).
Methods
Intervention Mapping guides program planners through six steps from needs assessment to program evaluation. The steps include: (1) developing a logic model of the problem, (2) identifying program outcomes and objectives, (3) designing the program, (4) producing the program, (5) planning for program implementation, and (6) planning for evaluation (11). Below we detail IM Steps 1–6 methods to develop and adapt two educational interventions for Hispanic parents of adolescents aged 11–17 years (Figure 1). While we briefly described the IM Step 6 in terms of evaluation planning, evaluation outcomes are not described as the effectiveness trial is currently ongoing. The University of Texas Health Science Center at Houston Institutional Review Board approved all research conducted during program development and adaptation.
Por Nuestras Hijas Program Development
Step 1. Develop a Logic Model of the Problem
The purpose of IM Step 1 is to conduct a needs assessment and develop a logic model of the problem (parent hesitation or inaction regarding adolescent child's HPV vaccination). To inform our needs assessment and logic model, we identified the following: (1) the burden of cervical cancer among low income or underinsured Hispanic women; (2) rates of HPV vaccination among low income and underinsured Hispanic female adolescents; (3) Hispanic parental beliefs, barriers, or attitudes toward the HPV vaccine amon; (4) and parental decision-making processes for obtaining the vaccine for their daughters.
IM recommends first forming a planning group made up of community stakeholders, members of the target population, and potential program implementers who work collaboratively with intervention developers to identify health problems and work together to develop solutions (11). Our planning group consisted of academic researchers and intervention planners, community leaders, and a prominent promotora (health worker) association to help guide program development, implementation, and adaptation decisions.
The team conducted a literature review to identify factors related to parental acceptance of the HPV vaccine and parental beliefs and attitudes related to HPV vaccine decision-making. A medical librarian skilled in designing systematic reviews developed our search, which included MeSH terms related to HPV vaccination, parent decision-making and vaccinations, parental acceptance of the HPV vaccine, and parental beliefs and attitudes toward the HPV vaccine for their daughters. Studies conducted in the United States between 2001 and 2010 published in English were included in the search. Studies were not limited to those with Hispanic participants only.
Finally, focus groups and in-depth interviews were conducted with Hispanic parents of adolescent females aged 11–17 years to further understand parental acceptance of the HPV vaccine for their daughters and beliefs and attitudes related to the vaccination. Research staff placed recruitment flyers in local community centers and clinics serving predominantly Hispanic populations. Parent eligibility requirements included: (1) identify as Hispanic/Latina/o; and (2) report having a daughter aged 11–17 years. Bilingual facilitators trained in qualitative research methods conducted a total of four focus groups and two in-depth interviews. All focus groups and interviews were recorded and later transcribed for analysis. All participants completed informed consent documents prior to the focus group or interview, and all received a $25 gift card for participating.
Step 2. Identify Program Outcomes and Objectives—Logic Model of Change
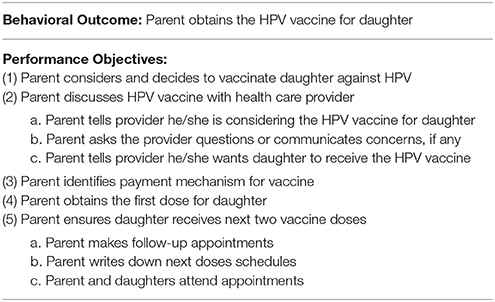
The purpose of IM Step 2, is to state program outcomes and objectives and develop a matrix of change objectives to guide program development. During this step, we stated the overall behavioral outcome to be accomplished as a result of our intervention and developed a detailed list of performance objectives, or sub-behaviors needed in order to achieve the outcome (11).
To construct the matrix of change objectives, performance objectives were included as row headings and modifiable factors positively associated with vaccine decision-making (determinants) as column headings. IM Step 1 findings informed the selection of determinants for the matrix. We crossed performance objectives and determinants to produce change objectives. Change objectives describe what must change in the determinant in order for an individual to perform the performance objective (11). The matrix of change objectives served as a blueprint for further program development and guided the selection of intervention methods, practical applications, and messages. Step 2 elements were organized into a logic model of change illustrating the expected change mechanisms leading to the desired behavior—HPV vaccine uptake.
Step 3. Design Por Nuestras Hijas
The purpose of IM Step 3 is to develop a program theme, identify program components, map change objectives and determinants to theoretical methods, and develop practical applications to operationalize methods. Our team collaborated with the planning group to develop a theme for the intervention, identify program components, decide on tangible products for parents, and discuss how parents would interact with the intervention. Guided by tables of methods to address specific determinant in the Intervention Mapping text (11), the group selected theoretical methods to influence specific determinants. Theoretical methods are techniques for influencing determinants to ultimately create behavior change (11). We then developed practical applications, or the specific ways we would operationalize the theoretical methods. The setting (clinics), feasibility of delivery, literacy level of parents, and preferences for educational material were considered throughout this process.
Step 4. Produce Por Nuestras Hijas
For both program development and adaptation, a production plan guided the creation and adaptation of materials. The plan included detailed flowcharts, developed mock-ups, created content, and produced all materials. To produce materials, collaborators included an application design team, a graphic designer, a talent consultant and agency, a video production team, actors, video editors, and a photographer.
Step 5. Implement Por Nuestras Hijas
In IM Step 5 for both program development and adaptation, we developed implementation strategies to build lay health worker capacity to deliver the program. To do so, we completed IM Steps 1–4 again with lay health workers in mind. This included identifying specific steps lay health workers would have to do in order to implement the interventions, determinants that may influence lay health workers' abilities to implement, theoretical methods to influence those determinants, and materials needed to deliver the interventions.
Step 6. Evaluate Por Nuestras Hijas
As a first evaluation step in both program development and adaptation, we validated that program content was consistent with the program plan by comparing content with the matrix of change. Creating a table with all determinants, change objectives, theoretical methods, and practical applications enabled us to assess whether the interventions addressed each change objective.
Next, we designed a comparative effectiveness study to assess the intervention effect on increasing vaccination uptake among Hispanic adolescents. Previous IM Steps informed the evaluation in several ways. First, the matrix of change objectives guided measurement development since they clearly describe the specific changes expected because of the program. The logic model guided development of indicators and measures to identify predictors, mediators, and moderators of HPV vaccination. The logic model of change also guided the evaluation of program implementation and informed our process evaluation. A complete description of the group randomized controlled trial including results is forthcoming. However, in short, thirty federally qualified health centers and community clinics to participate in the study. Lay health workers recruited participants from within the clinics and followed protocols to assess eligibility, obtain informed consent, administer surveys, and implement the interventions.
Por Nuestros Hijos Program Adaptation
Step 1. Develop a Logic Model of the Problem
During program adaptation Step 1, the aim was to identify factors associated with parental vaccine decision-making for males that may differ from those identified for parents of females. If significant differences existed, the program would likely require more extensive adaptations. Similar to methods in Step 1 for program development, we described the disease burden among the target population, parental barriers to obtaining the HPV vaccine for their sons, and the parental decision-making process for vaccinating sons.
An updated literature search was conducted in PubMed for studies assessing the following: (1) correlates of HPV vaccination in boys; (2) parents' acceptance or intention to vaccinate their sons against HPV; (3) parents' attitudes, knowledge, and acceptability of the HPV vaccine for male adolescents; and (4) barriers to HPV vaccination for male adolescents. The search was limited to US populations and to studies published in English through January 2015.
Step 1 also included three focus groups and five individual interviews with 20 Hispanic parents of males ages 11–17 recruited from local community centers and clinics. The purpose was to understand parental beliefs about the HPV vaccine for males and to understand parental decision-making to vaccinate their sons. Trained bilingual facilitators conducted the focus groups and interviews, which lasted between 60 and 85 min each. All sessions were conducted in Spanish. Facilitators obtained informed consent from each participant prior to each session, and all sessions were recorded and transcribed for analysis. Parents received $20 gift cards for participating.
Step 2. Identify Program Outcomes and Objectives—Logic Model of Change
Throughout the adaptation process, we considered whether the adapted intervention needed a new behavioral outcome and whether steps parents took to obtain the HPV vaccine for sons different from steps for obtaining the vaccine for daughters. All steps outlined above were followed to state the adapted behavioral outcome, identify adapted performance objectives, and create an adapted matrix of change objectives.
Step 3. Design Por Nuestros Hijos
During program adaptation, we reexamined the program theme, components, and theoretical methods, and practical applications to assess applicability to our new population. To ensure all content was relevant, we compared change objectives from the matrices for males to the materials previously developed for females. For example, if a change objective stated specific knowledge a parent should have, all materials were checked for that content. For all change objectives not addressed in the materials, we created new content.
Results
For Our Daughters Program Development
Step 1. Develop a Logic Model of the Problem
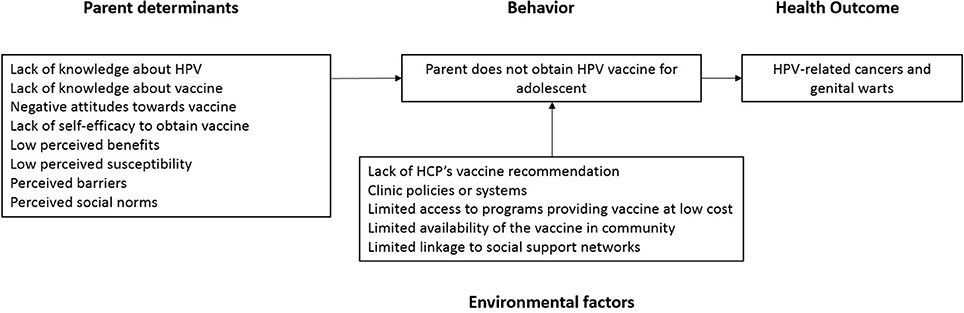
The literature search resulted in 30 studies examining factors associated with HPV vaccination among adolescent females. Modifiable factors associated with HPV vaccination included knowledge, attitudes toward the HPV vaccine, self-efficacy and communication skills, perceived benefits of the vaccine, perceived barriers to vaccination, HPV risk perception, and concerns about HPV vaccine safety (24–26). Non-modifiable factors included income, parental history of sexually transmitted infections, mother's Pap testing history, and parental education level (25, 27–29). The literature review also elucidated information sources where parents learned about HPV and the HPV vaccine including pamphlets, brochures, the internet, television media, and health care providers (30).
Findings from the focus groups and interviews confirmed that the modifiable factors identified in the literature search were applicable to our population. For example, Hispanic parents had low knowledge and awareness about HPV and the HPV vaccine, and parents expressed concerns about vaccine safety and side effects. Importantly, parents wanted information on how to speak with their daughter's provider about HPV and the HPV vaccine.
Our complete logic model of the problem included the behavior of interest (lack of HPV vaccination), the related health consequences (HPV-related cancers and genital warts), and determinants, or parental factors associated with the decision not to vaccinate (Figure 2).
Step 2. Identify Program Outcomes and Objectives—Logic Model of Change
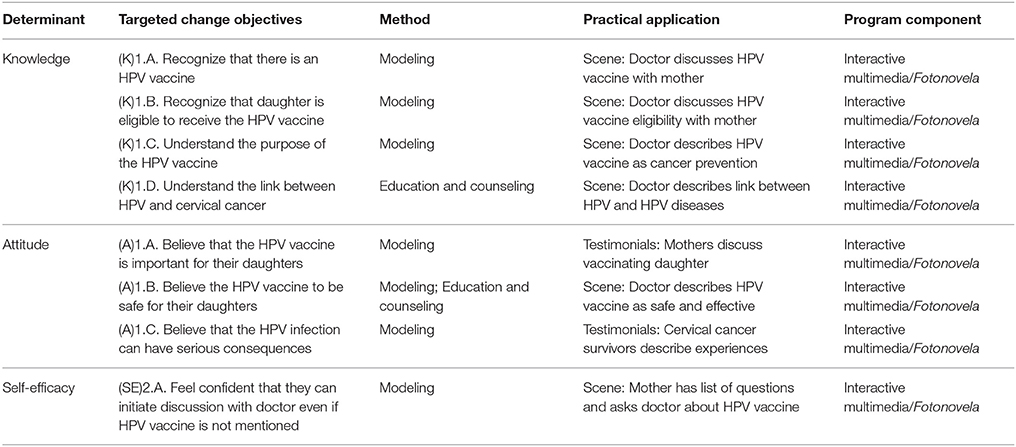
The overall behavioral outcome focused on parents: Parent will obtain the HPV vaccine for daughter. We identified five performance objectives associated with the outcome (Table 1). Determinants to increase vaccination behaviors identified in Step 1 included knowledge, attitudes toward the HPV vaccine, self-efficacy and communication skills, perceived benefits of the vaccine, perceived barriers to vaccination, HPV risk perception, and concerns about HPV vaccine safety. The matrix of change objectives described the changes in determinants needed for each specified performance objective (Table 2).
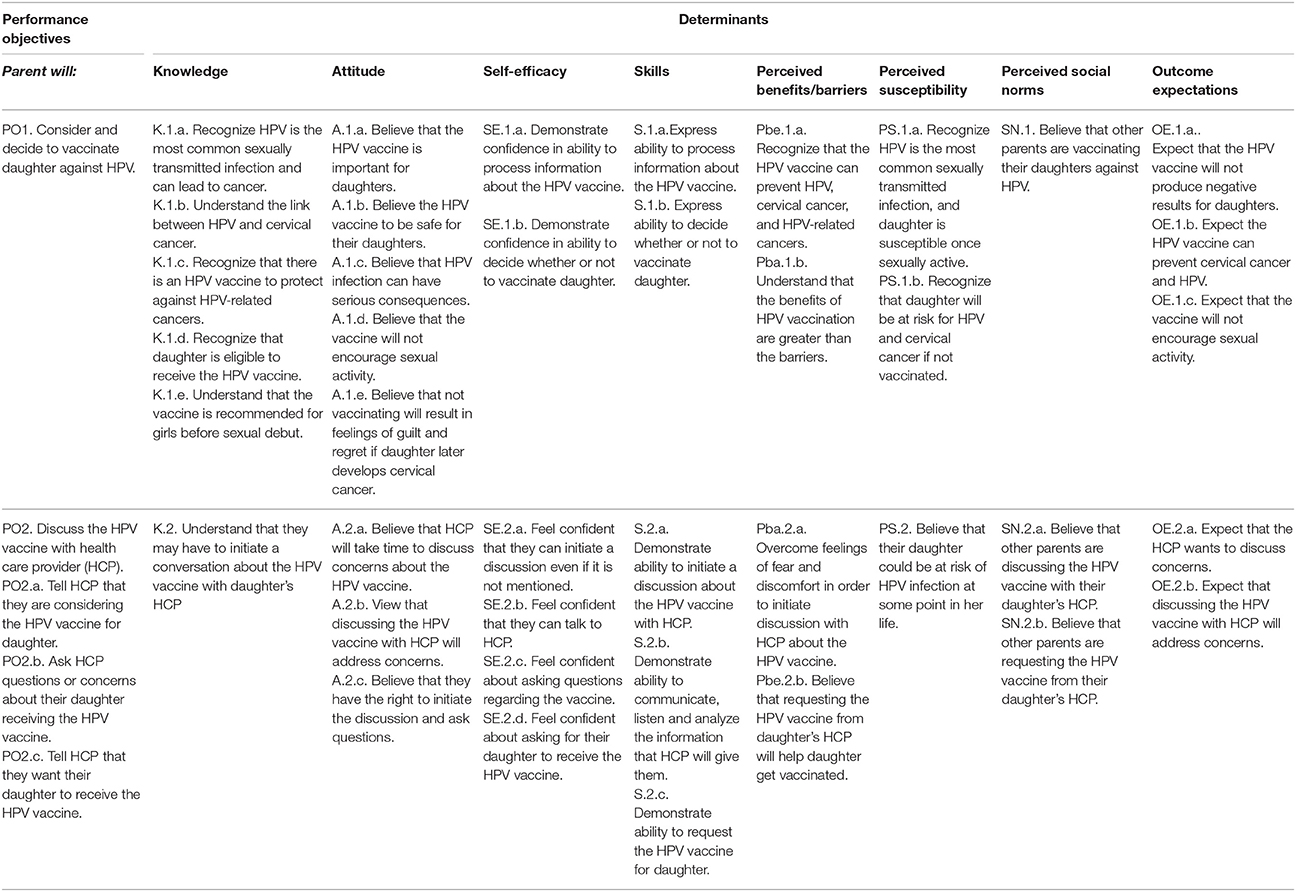
Table 2. Intervention mapping partial matrix for the behavioral outcome “parent obtains the HPV vaccine for daughter.”
Step 3. Design Por Nuestras Hijas
Program theme
The team developed the theme “Por Nuestras Hijas (For Our Daughters)” to convey a message of protection. Throughout the program, the theme was interwoven in two ways: (1) highlight that the HPV vaccine protects daughters from the human papillomavirus; and (2) highlight that parents protect their daughters from cancer by obtaining the HPV vaccine for them. The intervention follows the story of a mother gathering information about the HPV vaccine and making the decision to vaccinate her daughter to protect her against cancer. This protective framework is effective for this population. Messages that specifically frame the HPV virus as a threat to daughters and mothers as protectors increase Hispanic mothers' intentions to vaccinate their daughters (31).
Program components
Based on our previous work (32), we developed two program components: a print fotonovela and a tailored interactive multimedia intervention (TIMI) delivered on a tablet. The two components conveyed the story of the mother in both video and print format. Print fotonovelas are illustrated brief stories with pictures and dialog accompanying the images. Fotonovelas are soap-opera style stories, popular in Spanish-speaking societies and are often used to describe and educate Hispanic audiences about health topics. They often employ theory and evidence-based methods such as social modeling and vicarious learning, and have been shown to be effective in helping individuals personalize health issues, identify with and internalize the information being presented, and engage in positive health behaviors (33, 34).
Theoretical methods
Tailoring and targeting, modeling, skill building, and education and counseling were identified as key theoretical methods to address determinants influencing Hispanic parents' decision-making regarding the HPV vaccine. Tailoring presents messages or interventions based on characteristics unique to an individual. Targeting is broader and involves developing messages and interventions for a subpopulation or group with shared characteristics (35, 36). These methods were operationalized as practical applications in multiple ways. First, program components were presented in English and Spanish and used actors resembling the audience (see IM Step 4). Next, self-tailoring and automatic-tailoring pause points were included throughout the TIMI. At self-tailoring points, parents chose information they wanted to see. For example, one pause point listed common questions parents have about the HPV vaccine. Parents were able to choose all of the questions they had, and the program tailored the subsequent content accordingly. Automatic-tailoring included pause points where the program asked questions based on specific determinants. Depending on the response, the application showed different messages.
We also incorporated framing and anticipatory regret in the intervention. Gain-framing and loss-framing may be used to emphasize the advantages or disadvantages of performing a behavior, such as vaccination (37). Using loss framing, we emphasized the negative consequences of not vaccinating to elicit anticipatory regret. For low-frequency behaviors such as HPV vaccination, loss-framed messages have been found to be associated with greater behavioral intentions (38). These framing methods targeted perceived susceptibility, perceived vaccine efficacy, and behavioral intentions.
Modeling, a method from the Social Cognitive Theory (39), targeted multiple determinants such as self-efficacy and skills, and reinforced desired behaviors outlined in the performance objectives. As stated above, the theme following the story of a mother as she decides to vaccinate her daughter. Scenes in the program showed the mother modeling behaviors aligned with the performance objectives that we wanted parents to emulate.
Additional methods included education and counseling and skill building as we aimed to educate parents about the virus, the HPV vaccine, and how to request the vaccine for their adolescents. By identifying participant-specific barriers to initiation and completion through tailoring, the program provided tools and information necessary to build skills and overcome those barriers. For example, participants had the opportunity to write down questions they had for their provider after viewing content. Additionally, lay health workers clarified information that was unclear to participants and provided additional sources of information as needed.
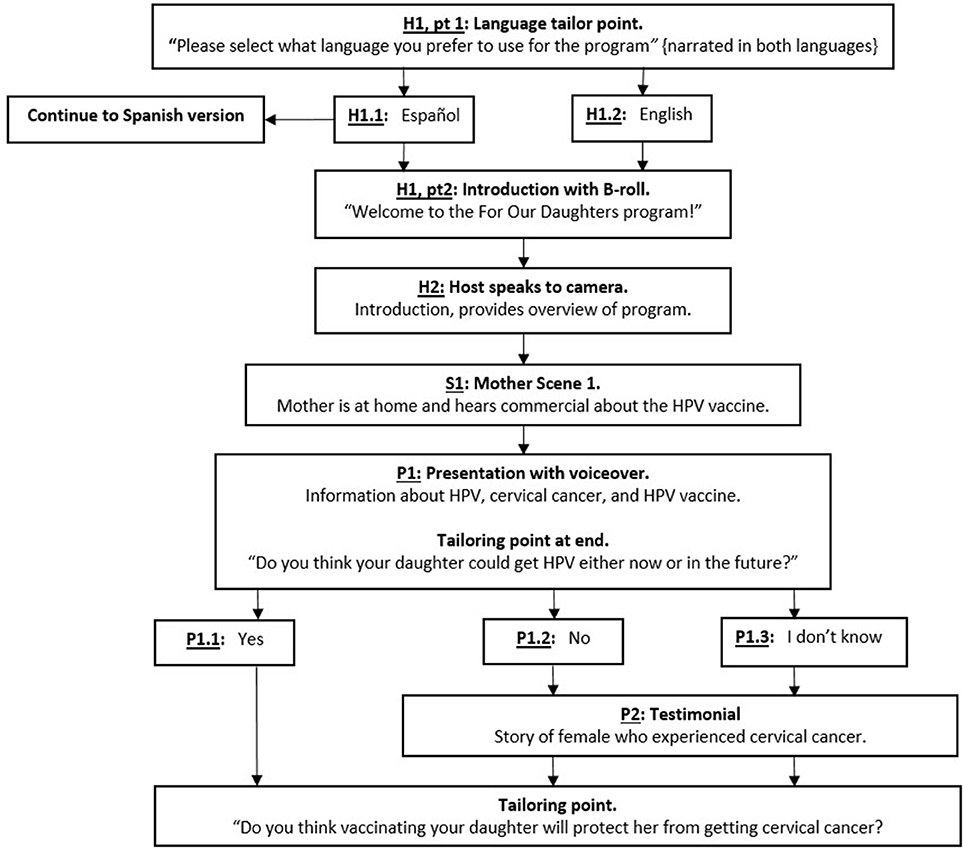
Step 4. Produce Por Nuestras Hijas
Design documents shared with the TIMI design team included a flowchart, mock-up presentations, and scripts. A detailed flowchart of the TIMI included all tailoring points and detailed the placement of all video vignettes (Figure 3). Mock-ups of presentations with voiceover were created for TIMI graphic designers. Presentations included illustrations, such as abnormal cells leading to cervical cancer, a presentation on HPV prevalence, and information about free vaccination programs. Scripts were in both English and Spanish. Simple, direct sentences free of jargon were used to accommodate a low-literacy population.
Actors for the TIMI and fotonovela were bilingual Hispanic actors with experience in health-related productions. It was important to hire actors resembled our target population and to film in locations that were culturally appropriate for our target audience (e.g., community-based clinics serving predominantly low-income populations). A video production team with experience in health-related productions filmed and produced all scenes, and a graphic designer created presentations with voiceover for the TIMI. The design team received all material and created the tablet-based application (Figure 4).
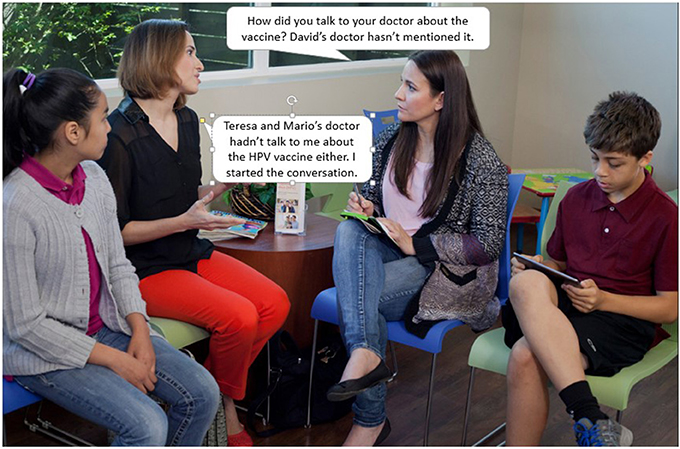
We created a storyboard for the fotonovela based on scripts used in the TIMI. Similar to a comic book or illustrated novel, each page of the fotonovela contained short text bubbles along with a relevant image from a relevant video scene (Figure 5). In addition to the story of a mother learning about the HPV vaccine and deciding to vaccinate her daughter, the fotonovela contained the following content: (1) a list of resources available to help cover the cost of the vaccine; (2) information about HPV and the HPV vaccine; (3) a calendar to help parents keep track of dosing schedules; and (4) a place for mothers to write down questions about the vaccine to ask their health care provider.
The cost of developing the TIMI and fotonovela have previously been reported (40). As reflected in the development steps outlined here, a substantial proportion of personnel time was associated with program development. Cost analyses indicate that the personnel time cost to plan and create the fotonovela-based education (41%) was less than the iPad-based TIMI (67%) education intervention.
Step 5. Implement Por Nuestras Hijas
For implementation, the target behavior was “Lay health worker will deliver the educational interventions with fidelity,” and performance objectives included (1) adopting the role of lay health worker, (2) locating eligible parents, and (3) conducting sessions with parents. Determinants included knowledge, skills and self-efficacy, attitudes, perceived norms, and outcome expectations. After completing the matrix of change objectives, we identified the following theoretical methods: information, modeling, feedback, reinforcement, and active learning for use in the implementation intervention. These methods were operationalized through presentations, activities, and practice sessions during a 2-day training session at Pro Salud, the lay health worker program headquarters. As a part of the training, medical experts presented information about HPV, the HPV vaccine, and cervical cancer. Each presentation ended with a question and answer session. The goal was to provide the lay health workers with a working knowledge of HPV, cervical cancer, and the HPV vaccine. We also used skills training and modeling approaches to prepare the lay health workers for their role in educating parents. Lay health workers learned how to use the program materials and how to respond to participant questions or concerns through both didactic presentations and facilitated practice session. Lay health workers took turns administering the program materials to build skills and self-efficacy. During this time, research staff circulated around the room to observe, assist, and offer feedback and reinforcement. Additional training topics pertained to evaluation efforts (see IM Step 6).
Step 6. Evaluate Por Nuestras Hijas
To assess content validity, we created a table mapping all program components back to change objectives and determinants (Table 3). The table illustrates the expected mechanisms of change. For example, in IM Step 1 we identified self-efficacy as a modifiable factor associated with behavior change to increase HPV vaccination. Parents needed increased self-efficacy to discuss the HPV vaccine with providers. In order to increase self-efficacy and to address each change objective associated with the determinant, the program included scenes with a mother modeling the behavior. As part of the content analysis, we went back to the table to ensure all appropriate change objectives were included in that scene.
We recruited 1,398 parents of adolescent females in participating clinics as part of the group randomized controlled trial to assess the effectiveness of the two interventions. Trained, bilingual data collectors approached parents in clinic waiting rooms, assessed eligibility, and obtained informed consent from those agreeing to participate. Data collectors administered baseline surveys to all participants and lay health workers administered the interventions to those in the fotonovela and TIMI study arms. We conducted follow up surveys and accessed patient vaccination records to assess vaccination status at 6 months after baseline. Results are forthcoming. During program development and implementation, we also assessed the cost-effectiveness of developing and implementing the interventions (40, 41). Finally, a sequential, multiple assignment, randomized trial to assess the effectiveness of Por Nuestros Hijos (described below) is currently underway.
Por Nuestros Hijos Program Adaptation
Step 1. Develop a Logic Model of the Problem
During the literature review, thirty-two relevant articles were identified after screening 1,032 title and abstracts. Similar to female adolescents, determinants for vaccinating adolescent males included parental knowledge, self-efficacy, skills, perceived benefits of the HPV vaccine, perceived susceptibility to HPV, perceived social norms, outcome expectations, and HPV vaccination attitudes. Parental intentions to vaccinate their sons were higher if they had daughters who were previously vaccinated against HPV (42, 43). Further, parents of males often believed their adolescent sons may soon become sexually active, and they believed vaccinating their sons could prevent the transmission of HPV to their female partners in the future (43–45). This finding was different from parents of females who perceived their daughters to be too young for the vaccine and not at risk for HPV because they did not perceive their daughters to be sexually active in the near future.
Focus groups and interviews revealed knowledge gaps about HPV-related cancers among males. Some parents were also unaware the HPV vaccine was available for males. Other knowledge gaps included parents confusing HPV with the herpes simplex virus (HSV) and parents now knowing condoms do not provide complete protection against HPV. Finally, parents reported receiving conflicting information about HPV from multiple sources. These results informed new content included in the adapted intervention.
Step 2. Identify Program Outcomes and Objectives—Logic Model of Change
The adapted program focused on a new outcome (HPV vaccination of sons). However, the target population, Hispanic parents, and the desired behavior, HPV vaccination, remained the same. Therefore, performance objectives were unchanged, and the matrix of change included most of the same change objectives. Minor changes included updating the knowledge change objectives to include male cancers and genital warts and removing change objectives regarding concerns about sexual disinhibition. For parents of daughters, we originally included content that assured parents daughters were not more likely to initiate sex at a younger age or to engage in risky sexual behaviors after vaccination. For parents of sons, we did not emphasize this point since it was not an identified barrier in the literature review or focus groups and interviews.
Step 3. Design Por Nuestros Hijos
Our original theme and program title Por Nuestras Hijas (For Our Daughters) was changed to Por Nuestros Hijos (For Our Children) to reflect that the program now contained information for parents of daughters and sons. The adapted program included the original story of a mother of a daughter and included a new story following a mother gathering information and deciding to vaccinate her son. The adapted program used the same program components, methods, strategies, and practical applications with one addition. Text message reminders, or cues to action, were added as a during Por Nuestros Hijos (For Our Children) to target HPV vaccine series completion behaviors.
Step 4. Produce Por Nuestros Hijos
To adapt the TIMI, we modified the original flowchart to include gender as an additional tailoring point. The flowchart depicted the two-arm program with one arm tailored for parents with daughters and one arm tailored for parents with sons. A third arm for parents with both daughters and sons is currently under development. We also revised the original scripts and multimedia presentations to provide information relevant to HPV-related cancers in males. As before, the program includes culturally appropriate actors. We followed the same process as in the development phase to produce the fotonovela aimed at parents of Hispanic males. Language in text message reminders to increase series completion were based on our previous work regarding linguistic agency and HPV vaccination intentions (31).
Step 5. Implement Por Nuestros Hijos
Our implementation plan for delivering Por Nuestros Hijos (For Our Children) did not change from Por Nuestras Hijas (For Our Daughters). Lay health workers continued to implement the program. The two primary adaptations to training content included: (1) providing information about HPV-related cancers affecting males, and (2) describing the updated ACIP recommendations to include HPV vaccination for adolescent males.
Discussion
We used Intervention Mapping (IM) to systematically develop and adapt two interventions for parents of Hispanic adolescents to increase HPV vaccine uptake. We first followed IM to develop Por Nuestras Hijas (For Our Daughters), an intervention targeting parents of Hispanic females. The process relied on evidence and theory to drive development of the logic model of the problem, program outcomes and objectives, program design, program production, development of an implementation intervention, and evaluation. As guidelines changed to include HPV vaccination for males (46), we used IM to assess and adapt the original program to the needs of parents of Hispanic males. We repeated IM Steps 1–6 systematically assessing the original intervention and identifying key elements that needed adapting.
Our program adapted for Hispanic parents of adolescent males required minimal adaptations. IM can guide program planners in making adaptations that are more significant by systematically guiding decision-making throughout the process. This is helpful as program planners identify evidence-based interventions developed in one context and adapt them for another (23). Changes may include a new priority population, a different setting, or a new health behavior. IM then provides the framework to assess and adapt the building blocks of each intervention to determine the level of adaptation needed.
Por Nuestros Hijos required mostly surface-adaptations since the behavioral outcome, determinants, and performance objectives were similar to the original program. Surface adaptations are smaller adaptations that tailor a program to a new audience, but do not necessarily add new program components or address new determinants. In Por Nuestros Hijos, example surface adaptations included changing characters to include males, altering scripts to include HPV-related cancers related to males, and updating the HPV guidelines to include males. Some program planners may follow IM and find that deeper adaptations, or more extensive changes to the original program, are needed to adapt an existing program for a new population. For example, IM Step 1 may identify a new determinant relevant to the new target population. This would then add to the matrix of change objectives. Planners would then identify new methods to target that determinant, new practical applications, and new intervention materials addressing the new change objectives—activities associated with more extensive adaptations to the original program.
Further, IM assists program planners in identifying the most salient methods, applications, or program components critical to program effectiveness. For example, in Por Nuestras Hijas (For Our Daughters), we used modeling to address parental self-efficacy in asking the provider questions, requesting the vaccine, and scheduling subsequent doses. We also used modeling to address parental outcome expectations. In this way, and based on the IM logic model of change, modeling was a critical method for creating parental behavior change. Modeling was the mechanism through which we expected to increase self-efficacy, to create positive outcome expectations, and to ultimately increase vaccination behaviors. In adapting the program, we retained modeling as a method since determinants were identical, and we adapted the original scripts to include language relevant to parents of males to operationalize the method.
Interventions targeting multiple factors associated with a health behavior are critical to behavior change, and interventions specifically targeting HPV vaccination sometimes fail to address more than one factor associated with parental decision-making. Interventions to increase HPV vaccination among adolescents often provide only educational information or cues to action (e.g., reminder letters, text messages) for parents (47). Educational interventions and materials, including those produced by the CDC, aim to increase parental knowledge about HPV, HPV-related cancers, and the HPV vaccine (48). While it is important to increase parental knowledge, focusing solely on this factor may not be enough to change behavior, particularly for unmotivated parents (49). Systematically identifying and addressing multiple factors associated with HPV vaccination, such as attitudes, beliefs, or self-efficacy, allows intervention planners to move beyond simply providing information or cues to action to create behavior change.
The steps that guided program development and adaptation are applicable to a broad group of researchers, program planners, and public health professionals. IM was specifically designed for use in public health settings, not just academic research settings, providing public health practitioners the tools and resources to develop theory- and evidence-based interventions specific to their context (11). IM provides a systematic process, appropriate for any population or behavior of interest, that result in interventions targeting determinants specific to the population and behavior. Public health practitioners and health educators in health departments and hospital settings (50, 51), workplace settings (52), and community organizations (23) have successfully developed theory- and evidence-based interventions using IM. As exemplified by Por Nuestras Hijas (For Our Daughters) and Por Nuestros Hijos (For Our Children), IM provides a user-friendly, iterative stepped approach to facilitate development and adaptation guiding researchers and public health practitioners every step of the way.
Future studies should evaluate the Por Nuestras Hijas (For Our Daughters) and Por Nuestros Hijos (For Our Children) interventions to assess their efficacy in increasing HPV vaccination in Hispanic adolescents and in changing psychosocial determinants. These studies will provide important information regarding the effect the interventions on the knowledge, beliefs and attitudes that influence HPV vaccination along with information about the efficacy of the two program components. If the interventions are effective in increasing vaccination, they could be adapted for other populations using the process we outline in this paper.
There are limitations to our development and adaptation process using IM. Participants in the focus groups and interviews self-selected to be a part of our needs assessment work. Their attitudes toward the HPV vaccine may differ from those of other parents who did not participate. We therefore may not have captured all determinants relevant to our target population. While we conducted systematic reviews of the literature to also identify determinants, the qualitative nature of the needs assessment process may limit generalizability. Additionally, the program is limited in reach since participants were low income and underinsured Hispanic parents in an urban setting. The programs may not be effective among Hispanics in other settings, and messages may not resonate for other race/ethnicity populations. Further, while our team had resources to train and implement the intervention using lay health workers, clinics and other organizations utilizing this program in the future may not be able to employ this implementation strategy. This potentially limits program reach. Similarly, clinics or other organizations may not have capacity to implement text message reminders to target HPV vaccine series completion. Our development and adaptation processes and outcomes did not account for these differences in resources for future program adopters.
Ethics Statement
This study was carried out in accordance with the recommendations of UTHealth Science Center at Houston with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the University of Texas Health Science Center at Houston Institutional Review Board.
Author Contributions
MF, SV, LS: Study and manuscript conceptualization; SR: Background, methods, results, discussion; AR, LS, and MF: Contributed to background, methods, results, discussion; DL: Contributed to methods.
Funding
This research was funded by the Cancer Prevention Research Institute of Texas (CPRIT) grants RP100865 and RP130459. SR was supported by a Predoctoral Fellowship from the University of Texas School of Public Health Cancer Education and Career Development Program supported by the National Cancer Institute/NIH Grant R25 CA57712 and partially supported by the UTHealth School of Public Health Department of Health Promotion and Behavioral Sciences. AR is supported an NIH Career Development award, K01CA181437. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Cancer Prevention Research Institute of Texas, the National Cancer Institute, or the National Institutes of Health.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Natalie Fernandez-Espada, Erica Lipizzi, Jennifer Villamar, and Milet Serna for their support developing Por Nuestras Hijas (For Our Daughters) and adapting the program to become Por Nuestros Hijos (For Our Children). The authors would also like to acknowledge study Co-Investigators Drs. Paula Cuccaro, Elizabeth Baumler, and David Lairson.
References
1. Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MCB, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, (2008). Sex Transm Dis. (2013) 40:187–93. doi: 10.1097/OLQ.0b013e318286bb53
2. Centers for Disease Control and Prevention (CDC). Human Papillomavirus – Associated Cancers — United States, 2004 – 2008. Morb Mortal Wkly Rep. (2012) 61:258–61. doi: 10.15585/mmwr.mm6526a1
3. Viens LJ, Henley SJ, Watson M, Markowitz LE, Thomas CC. Human Papillomavirus – associated cancers — United States, 2008 – 2012. Morb Mortal Wkly Rep. (2016) 65:2008–12. doi: 10.15585/mmwr.mm6526a1
4. Centers for Disease Control and Prevention. HPV-Associated Cervical Cancer Rates by Race and Ethnicity (2017). Available online at: https://www.cdc.gov/cancer/hpv/statistics/cervical.htm
5. Shoemaker ML, White MC. Breast and cervical cancer screening among Hispanic subgroups in the USA: estimates from the National Health Interview Survey 2008, 2010, and 2013. Cancer Causes Control (2016) 27:453–7. doi: 10.1007/s10552-016-0718-5
6. Markowitz LE, Dunne EF, Saraiya M, Chesson HW, Curtis CR, Gee J, et al. Human Papillomavirus vaccination recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. (2014) 63:1–30. Available online at: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6305a1.htm
7. U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020: Immunization and Infectious Diseases [Internet]. (2016) Available online at: https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases (Accessed September 29, 2016).
8. Reagan-Steiner S, Yankey D, Jeyarajah J, Elam-Evans LD, Curtis CR, MacNeil J, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13-17 Years - United States, 2015. Morb Mortal Wkly Rep. (2016) 65:850–8. doi: 10.15585/mmwr.mm6533a4
9. Centers for Disease Control and Prevention. Cervical Cancer Rates by Race and Ethnicity. (2016). Available online at: http://www.cdc.gov/cancer/cervical/statistics/race.htm
10. Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Heal. (2010) 31:399–418. doi: 10.1146/annurev.publhealth.012809.103604
11. Bartholomew Eldredge LK, Markham CM, Ruiter RAC, Fernandez ME, Kok G, Parcel GS. Planning Health Promotion Programs: An Intervention Mapping Approach. 4th ed. San Francisco, CA: Jossey-Bass (2016).
12. Tripp MK, Herrmann NB, Parcel GS, Chamberlain RM, Gritz ER. Sun protection is fun! A skin cancer prevention program for preschools. J Sch Health (2000) 70:395–401. doi: 10.1111/j.1746-1561.2000.tb07226.x
13. Brendryen H, Kraft P, Schaalma H. Looking inside the black box: using intervention mapping to describe the development of the automated smoking cessation intervention “Happy Ending.” J Smok Cessation. (2010) 5:29–56. doi: 10.1375/jsc.5.1.29
14. Fernández ME, Gonzales A, Tortolero-Luna G, Partida S, Bartholomew LK. Using Intervention mapping to develop a breast and cervical cancer screening program for Hispanic farmworkers: cultivando la salud. Health Promot Pract. (2005) 6:394–404. doi: 10.1177/1524839905278810
15. Hou S-I, Fernandez ME, Parcel GS. Development of a cervical cancer educational program for chinese women using intervention mapping. Health Promot Pract. (2004) 5:80–7. doi: 10.1177/1524839903257311
16. Vernon SW, Del Junco DJ, Tiro JA, Coan SP, Perz CA, Bastian LA, et al. Promoting regular mammography screening II. Results from a randomized controlled trial in US women veterans. J Natl Cancer Inst. (2008) 100:347–58. doi: 10.1093/jnci/djn026
17. Byrd TL, Wilson KM, Smith JL, Heckert A, Orians CE, Vernon SW, et al. Using intervention mapping as a participatory strategy: development of a cervical cancer screening intervention for Hispanic women. Heal Educ Behav. (2012) 39:603–11. doi: 10.1177/1090198111426452
18. Scarinci IC, Bandura L, Hidalgo B, Cherrington A. development of a theory-based (PEN-3 and Health Belief Model), culturally relevant intervention on cervical cancer prevention among latina immigrants using intervention mapping. Health Promot Pract. (2012) 13:29–40. doi: 10.1177/1524839910366416
19. Fernández ME, Gonzales A, Tortolero-Luna G, Williams J, Saavedra-Embesi M, Chan W, et al. Effectiveness of Cultivando la Salud: A breast and cervical cancer screening promotion program for low-income hispanic women. Am J Public Health (2009) 99:936–43. doi: 10.2105/AJPH.2008.136713
20. Fernández ME, Savas LS, Carmack CC, Chan W, Lairson DR, Byrd TL, et al. A randomized controlled trial of two interventions to increase colorectal cancer screening among Hispanics on the Texas–Mexico border. Cancer Causes Control (2015) 26:1–10. doi: 10.1007/s10552-014-0472-5
21. Donaldson A, Poulos RG. Planning the diffusion of a neck-injury prevention programme among community rugby union coaches. Br J Sports Med. (2014) 48:151–9. doi: 10.1136/bjsports-2012-091551
22. Pressel S, Bartholomew LK, Cushman W, Whelton P, Nwachuku C. Disseminating Clinical Trial Results: Case Study From the Antihypertensive and Lipid-Lowering Treatment to Prevention Heart Attack Trial (ALLHAT). Presentation. Portland, OR: Society for Clinical Trials. (2005).
23. Highfield L, Hartman MA, Mullen PD, Rodriguez SA, Fernandez ME, Bartholomew LK. Intervention mapping to adapt evidence-based interventions for use in practice: increasing mammography among African American women. Biomed Res Int. (2015) 2015:160103. doi: 10.1155/2015/160103
24. Dempsey AF, Abraham LM, Dalton V, Ruffin M. Understanding the reasons why mothers do or do not have their adolescent daughters vaccinated against human Papillomavirus. Ann Epidemiol. (2009) 19:531–8. doi: 10.1016/j.annepidem.2009.03.011
25. Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Prev Med. (2007) 45:107–14. doi: 10.1016/j.ypmed.2007.05.013
26. Fernández ME, Allen JD, Mistry R, Kahn JA. Integrating clinical, community, and policy perspectives on human papillomavirus vaccination. Annu Rev Public Health (2010) 31:235–52. doi: 10.1146/annurev.publhealth.012809.103609
27. Chao C, Slezak JM, Coleman KJ, Jacobsen SJ. Papanicolaou screening behavior in mothers and human papillomavirus vaccine uptake in adolescent girls. Am J Public Health (2009) 99:1137–42. doi: 10.2105/AJPH.2008.147876
28. Gerend MA, Weibley E, Bland H. Parental response to human papillomavirus vaccine availability: uptake and intentions. J Adoles Health (2009) 45:528–31. doi: 10.1016/j.jadohealth.2009.02.006
29. Yeganeh N, Curtis D, Kuo A. Factors influencing HPV vaccination status in a Latino population; and parental attitudes towards vaccine mandates. Vaccine (2010) 28:4186–91. doi: 10.1016/j.vaccine.2010.04.010
30. Watts L A, Joseph N, Wallace M, Rauh-Hain J A, Muzikansky A, Growdon WB, et al. HPV vaccine: A comparison of attitudes and behavioral perspectives between Latino and non-Latino women. Gynecol Oncol. (2009) 112:577–82. doi: 10.1016/j.ygyno.2008.12.010
31. McGlone MS, Stephens KK, Rodriguez SA, Fernandez ME. Persuasive texts for prompting action: Linguistic agency assignment in HPV vaccination reminders. Vaccine (2017) 5:4295–7. doi: 10.1016/j.vaccine.2017.06.080
32. Kreuter MW, Fernandez ME, Brown M, Cofta-Woerpel L, Pfeiffer D, Adams-Piphus B, et al. Increasing information-seeking about human Papillomavirus vaccination through community partnerships in African American and Hispanic communities. Fam Commun Health (2012) 35:15–30. doi: 10.1097/FCH.0b013e3182385d13
33. Holmes M, Bacon T, Dobson L, McGorty E, Silberman P, DeWalt D, et al. Addressing health literacy through improved patient-practitioner communication. N C Med J. (2007) 68:319–26.
34. Auger S, Verbiest S. Lay health educators' roles in improving patient education. North Carolina Med J. (2007) 68:333–5.
35. Kreuter MW, Farrell D, Olevitch L, Brennan L. Tailoring Health Messages: Customizing Communication with Computer Technology. New York, NY: Routledge (2000).
36. Schmid KL, Rivers SE, Latimer AE, Salovey P. Targeting or tailoring? Mark Health Serv. (2008) 28:32–7.
37. Van 't Riet J, Cox AD, Cox D, Zimet GD, De Bruijn GJ, Van den Putte B, et al. Does perceived risk influence the effects of message framing? Revisiting the link between prospect theory and message framing. Health Psychol Rev. (2016) 10:447–59. doi: 10.1080/17437199.2016.1176865
38. Gerend MA, Shepherd JE, Monday KA. Behavioral frequency moderates the effects of message framing on HPV vaccine acceptability. Ann Behav Med. (2008) 35:221–9. doi: 10.1007/s12160-008-9024-0
39. Kelder S, Hoelscher D, Perry CL. How individuals, environments, and health behavior inteact: Social Cognitive Theory. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior: Theory, Research, and Practice. 5th ed. San Francisco, CA: Jossey-Bass (2015). p. 285–325.
40. Karanth SS, Lairson DR, Savas LS, Vernon SW, Fernández ME. The cost of developing a computerized tailored interactive multimedia intervention vs. a print based Photonovella intervention for HPV vaccine education. Eval Program Plann. (2017) 63:1–6. doi: 10.1016/j.evalprogplan.2017.02.009
41. Karanth SS, Lairson DR, Huang D, Savas LS, Vernon SW, Fernándezb ME. The cost of implementing two small media interventions to promote HPV vaccination. Prev Med. (2017) 99:277–81. doi: 10.1016/j.ypmed.2017.03.002
42. Reiter PL, McRee A-L, Kadis J A, Brewer NT. HPV vaccine and adolescent males. Vaccine (2011) 29:5595–602. doi: 10.1016/j.vaccine.2011.06.020
43. Reiter PL, McRee AL, Gottlieb SL, Brewer NT. HPV vaccine for adolescent males: acceptability to parents post-vaccine licensure. Vaccine (2010) 28:6292–7. doi: 10.1016/j.vaccine.2010.06.114
44. Dempsey AF, Butchart A, Singer D, Clark S, Davis M. Factors associated with parental intentions for male human papillomavirus vaccination: results of a National survey. Sex Transm Dis. (2011) 38:769–76. doi: 10.1097/OLQ.0b013e318211c248
45. Schuler CL, DeSousa NS, Coyne-Beasley T. Parents' decisions about HPV vaccine for sons: the importance of protecting sons' future female partners. J Commun Health (2014) 39:842–8. doi: 10.1007/s10900-014-9859-1
46. Centers for Disease Control and Prevention Advisory Committee on Immunization Practices. Recommendations on the Use of Quadrivalent Human Papillomavirus Vaccine in Males — Advisory Committee on Immunization Practices (ACIP), (2011). MMWR Morb Mortal Wkly Rep. (2011) 60:1705–8.
47. Walling EB, Benzoni N, Dornfeld J, Bhandari R, Sisk BA, Garbutt J, et al. Interventions to improve hpv vaccine uptake: a systematic review. Pediatrics (2016) 138:e20153863. doi: 10.1542/peds.2015-3863
48. Centers for Disease Control and Prevention.. Materials for Parents [Internet] (2016). Available online at: https://www.cdc.gov/hpv/partners/outreach-parents/materials-parents.html (Accessed June 30, 2017).
49. Montano DE, Kasprzyk D. Theory of Reasoned Action, Theory of Planned Behavior, an the Integrated Behavioral Model. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior: Theory, Research, and Practice. 5th ed. San Francisco, CA: Jossey-Bass (2015). p. 95–124.
50. Schmid AA, Andersen J, Kent T, Williams LS, Damush TM. Using intervention mapping to develop and adapt a secondary stroke prevention program in Veterans Health Administration medical centers. Implement Sci. (2010) 5:97. doi: 10.1186/1748-5908-5-97
51. Durks D, Fernandez-Llimos F, Hossain LN, Franco-Trigo L, Benrimoj SI, Sabater-Hernández D. Use of intervention mapping to enhance health care professional practice: a systematic review. Heal Educ Behav. (2017) 44:524–35. doi: 10.1177/1090198117709885
Keywords: HPV vaccination, Hispanic adolescents, intervention development, intervention adaptation, Intervention Mapping
Citation: Rodriguez SA, Roncancio AM, Savas LS, Lopez DM, Vernon SW and Fernandez ME (2018) Using Intervention Mapping to Develop and Adapt Two Educational Interventions for Parents to Increase HPV Vaccination Among Hispanic Adolescents. Front. Public Health 6:164. doi: 10.3389/fpubh.2018.00164
Received: 01 July 2017; Accepted: 14 May 2018;
Published: 15 June 2018.
Edited by:
Shane Andrew Thomas, Shenzhen International Primary Healthcare Research Institute, ChinaReviewed by:
Paolo Giorgi Rossi, Azienda Sanitaria Unità Locale di Reggio Emilia, ItalyAnna Chapman, Deakin University, Australia
Copyright © 2018 Rodriguez, Roncancio, Savas, Lopez, Vernon and Fernandez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Serena A. Rodriguez, c2VyZW5hLnJvZHJpZ3VlekB1dHNvdXRod2VzdGVybi5lZHU=
 Serena A. Rodriguez
Serena A. Rodriguez Angelica M. Roncancio1
Angelica M. Roncancio1 Lara S. Savas
Lara S. Savas Maria E. Fernandez
Maria E. Fernandez