- 1Department of Cell and Molecular Biology, Rowan-Virtua School of Osteopathic Medicine, Rowan University, Stratford, NJ, United States
- 2Department of Psychiatry, Medstar Georgetown University Hospital, Washington, DC, United States
Problem based learning (PBL) is based on the idea that learning is “grounded by experience. ” PBL curriculums in medical school highlight the importance of engaging students and allowing students to be the driver of their education. This mimics their work in the hospital where answers are rarely suited to a multiple-choice question, but a myriad of complex clinical questions, ethical decisions, and cost barriers. Teaching medical students from the start of medical school to handle multiple variables is an important aspect of their learning. Studies indicate that PBL students consistently score at or above the national average on board exams compared to their peers. Furthermore, evaluations of competence during clinical rotations show statistically significant advantages for PBL students in areas such as critical thinking, social and cognitive interactions, and patient comfort. Studies highlight a notable advantage in interpersonal skills among PBL students. Additionally, geographical access plays a critical role in enrollment, and personal responsibilities can hinder potential applicants from pursuing medical school. PBL can be utilized to create an environment where location-based barriers are minimized to increase the number of individuals entering the medical profession. This approach could ultimately reduce the healthcare burden and enhance medical services in underserved areas of the country. Here, we present a concise review of resources and approaches including online and digital platforms to facilitate curriculum development and implementation of flipped classrooms and independent learning that are well-suited for PBL.
Introduction
Problem based learning (PBL) programs are being utilized by many medical schools around the world (Kinkade, 2005; Frambach et al., 2019). Here, we describe fundamental aspects of how the PBL process developed and its current use in medical education. We also describe currently available PBL implementation platforms, virtual patient cases, and effects of PBL on educational accessibility.
Methodology
This review is based on empirical research. The authors have experience as PBL instructors and students graduating from medical school using a PBL based curriculum. A dynamic network of PBL medical students and faculty were also solicited for feedback regarding their experience with available resources, what aspects they found helpful, and what they felt could be improved. All websites and platforms referred to were directly evaluated to the fullest extent possible. Comprehensive literature searches were also performed with terms including but not limited to “PBL,” “medical education,” “virtual patients,” “flipped classroom,” and “experiential learning.”
PBL historical roots
Throughout history, educators have sought innovative ways to improve the learning experience, aiming to help students acquire knowledge more effectively. From traditional lecture-based learning to modern flipped classrooms, the landscape of education has evolved to accommodate a variety of learning needs. These efforts have led to the development of various teaching methods, each designed to cater to different learning styles, disciplines, and educational goals (Trullas et al., 2022; Saqr et al., 2020; Ng et al., 2014).
Fundamental aspects of PBL can be traced back to renowned Chinese and Greek philosophers. For example, the Chinese philosopher and scientist Confucius (551-479 BC; see Figure 1a) engaged his students with debates, which is an active part of the PBL process. The Greek philosopher Socrates (470-399 BC; see Figure 1b) believed in teaching his students how to think rather than simply retain knowledge. This approach to teaching—known as the Socratic Method—shares many similarities with modern day PBL. Socrates aimed not to impart information, but rather to foster critical thinking skills, emphasizing questions over facts (Wang et al., 2008). This was not appreciated by society at the time as evidenced by Socrates being sentenced to suicide by poison rather than submitting to social and geographical ostracism (Plato, 2000). A contemporary of Socrates, Hippocrates is often regarded as the father of modern medicine. He is credited with formulating the Hippocratic Oath, which outlines ethical standards for physicians from ancient times to today (Mesko and Spiegel, 2022).
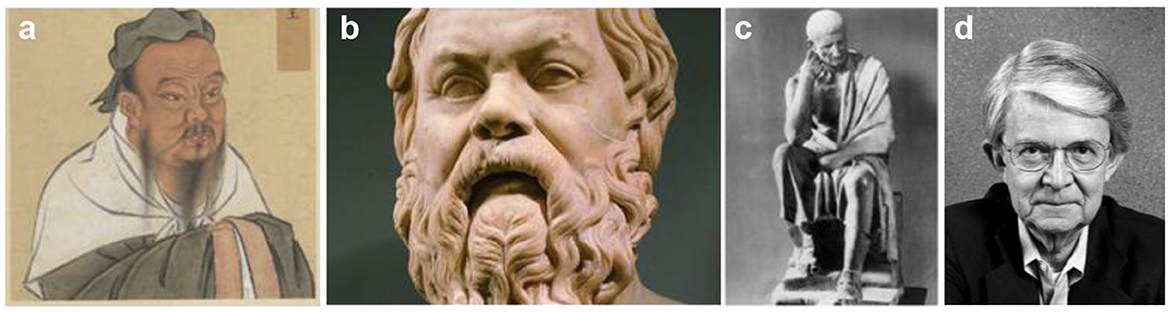
Figure 1. Images of Confucius, Socrates, and Aristotle. (a) Artist rendition of Confucius during the Yuan dynasty, artist unknown (ca. 1279–1368; National Palace Museum, 2025), (b) Herm of Greek philosopher Socrates on display in Capitoline Museum in Rome, artist unknown (ca. 450-301 BCE; kraut, 2025), (c) Bronze Statue of Greek philosopher Aristotle on display at the British Museum, artist unknown (384-322 BCE; Dunn, 2006), (d) Photograph of Dr. Howard Barrows (Howard Barrows, 2025).
This Socratic method encourages active learning by asking open-ended questions that prompt students to think critically and reflect on the material. Rather than simply delivering information, as traditional didactic methods do, the teacher in this model acts as a facilitator, guiding students through their thought processes and enabling students to find points of weakness in their argument. This type of questioning promotes an interactive learning environment where students are not passive recipients of knowledge, but active participants in their education (Ho et al., 2023).
Plato was a student of Socrates and later taught Aristotle (see Figure 1c), who became one of the most influential figures in Athens during his time. Aristotle was a dynamic scientist and philosopher who taught pupils including Alexander the Great. Aristotle is considered to be a founder of western thought. His influence on medicine and biological classifications are still relevant today (Dunn, 2006). He studied animal cadavers to discover important similarities between different species. Aristotle believed in the process of learning by doing, which is embraced by modern day “experiential approaches” to learning (Bernacer and Murillo, 2014).
Notable educational influencers after Aristotle include Alhazen (965–1040) from an area located in current day Iraq. Alhazen (also known as Ibn al-Haytham) is considered a father of the “scientific method.” He promoted question based learning which is foundational to the PBL process (Omar, 1979). John Amos Comenius (1592–1670) from an area located in the current day Czech Republic, emphasized the importance of experiential learning and student interest in education which are essential components of PBL (Goss, 2009). Jean-Jacques Rousseau (1712–1778) and Johann Heinrich Pestalozzi (1746–1827) from Switzerland and Herbert Spencer (1820–1903) from England promoted the roles of exploration and problem solving in education which are also fundamental properties of PBL (Hall, 1973; Heafford, 2016; Mead, 2008). John Dewey and his student William Heard Kilpatrick (1859–1952) from the USA also promoted learning through experience and problem solving which supported the advent of experiential education and inquiry based learning which form the foundation of PBL (Hmelo-Silver, 2004; Fallace, 2008).
PBL in medicine today
The introduction of modern day PBL curriculums in medical education is attributed to John Evans and William Spaulding at McMaster University in Canada in the 1960s. They felt that traditional medical education was inadequate to prepare medical students for actual practice. For example, they believed that traditional didactic teaching did not effectively promote knowledge retention and utilization (Azzahrani, 2024).
Dr. Howard Barrows (see Figure 1d) took over the PBL curriculum at McMaster in the 1970s and is generally credited with developing PBL as a new approach for medical education. He noticed that traditional didactic lectures did not fully prepare students for the practical, problem-solving demands of medicine (Wood, 2003). Dr. Barrows pioneered the use of PBL as a complete preclinical curriculum with instructors that do not need to be content experts in a simple uniform format. Essential to the PBL approach was the use of small groups which foster interpersonal dynamics that encourage peer-peer interaction and promote student centered learning (Kraft et al., 1997). Additionally, the original PBL approach was not focused on assessments in order to most efficiently support the learning process. The success of these seminal programs was instrumental in the adoption of the curriculum to other schools (Camp, 2016).
PBL curriculums have been widely adopted in U.S. medical schools since its introduction in the late 1960s. Over 70% of U.S. medical schools incorporated PBL into their curricula by the early 1990s. Subsequent studies confirm that at least 70% of medical schools in the USA currently utilize PBL in their preclinical years (Kinkade, 2005). Additionally, PBL has since spread internationally to other countries in the Americas, Europe, and Asia (Frambach et al., 2019).
Modern PBL vs. traditional didactic learning
Traditional didactic learning remains the most common approach to medical education, where instructors acquire and deliver structured content to relatively large groups of students in a classroom setting as shown in Figure 2a (Alaagib et al., 2019). Assessments are usually integral to didactic curriculums in order to identify weakness in the learner's mastery of subject material. Didactic presentations are often given adjacent to a slide deck which students can review before and after lectures. Didactic lectures allow for material to be covered within a structured timeframe. However, didactic teaching is a passive learning style which does not always result in long term retention of subject matter (Timmer et al., 2020).
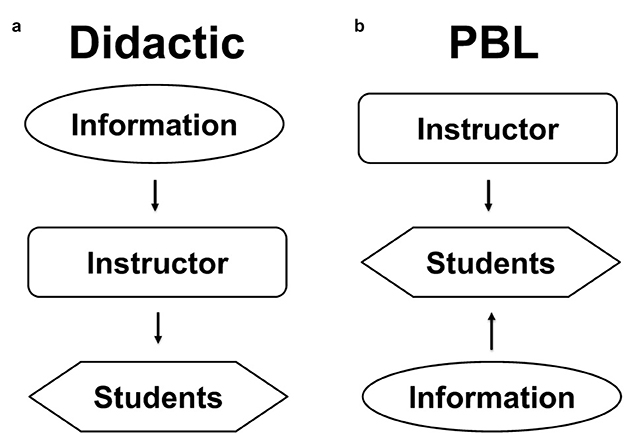
Figure 2. Comparison of traditional didactic and PBL methods of teaching. (a) Traditional didactic methods involve an instructor acquiring and feeding knowledge from a variety of resources to a group of students. (b) PBL methods involve an instructor that contributes to the students ability to acquire information from a variety of resources.
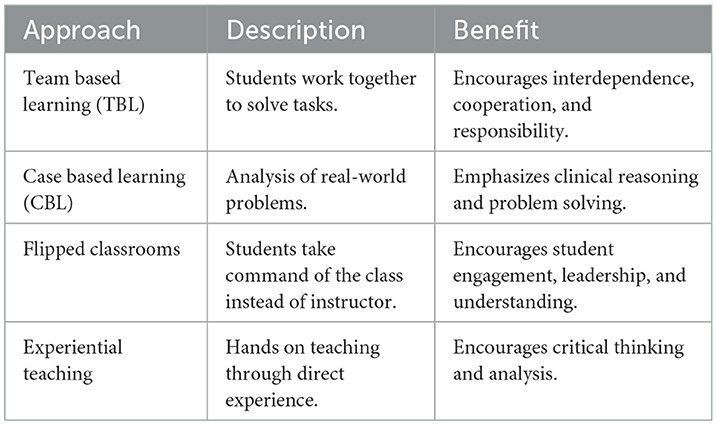
In contrast to didactic learning, PBL incorporates team based learning (TBL), case based learning (CBL), flipped classrooms, and experiential teaching methods to more actively engage students in their learning process as shown in Figure 2b (Vieira, 2025; Wang et al., 2025; Zhu et al., 2025). Each of these approaches offers advantages as shown in Table 1.
• Team based learning involves students working collaboratively—in teams—to solve problems and apply knowledge. This process develops collaborative and communication skills needed in medicine (Punja et al., 2014).
• Case based learning utilizes case studies and real-world scenarios to drive students to develop cognitive and problem-solving skills through student engagement (Kumar et al., 2022).
• Flipped classrooms force students to run learning sessions without significant guidance from their instructors. This process promotes active learning during class through problem solving activities and group discussions (Kumar et al., 2022).
• Experiential learning employs direct experiences such as internships and fieldwork to develop skills that prepare students for practical challenges (Yardley et al., 2012). This approach mirrors Aristotle's teaching methods by focusing on mastery of applied skills. PBL integrates these learning methods to empower students to develop skills that are useful in their careers (Dolmans et al., 2005; Ghani et al., 2021).
Advantages of PBL are evidenced by results from medical board exams. For example, PBL students outperformed didactic learners in 11 out of 12 years on board exams and scored above the national average all 12 years (Zaveri et al., 2019). Didactic instruction trains students to passively absorb facts presented to them by a central instructor. In contrast, in the PBL classroom, students work in small groups to analyze and solve case-based or scenario-driven problems. This process is facilitated by instructors, but students typically lead the discussion by identifying their learning objectives, conducting independent study or research, and applying what they learn to case scenarios. The instructor acts more as a guide than a teacher in a traditional lecture format. PBL instructors, often called “facilitators” or “coordinators,” assist in keeping the students on track, encourage discussion or debate, and ensure that students accomplish their learning objectives without providing direct answers (Servant-Miklos, 2020; Lim, 2023).
PBL engages medical students by having them apply their existing knowledge to realistic cases or scenarios that expose gaps in their understanding. These specific learning objectives are often referred to as “learning issues.” These gaps are then addressed through self-study, enabling students to deepen their knowledge to solve problems. More than team based learning (TBL), which places greater emphasis on group collaboration from the outset, PBL focuses on critical thinking and reasoning, requiring students to adopt evidence-based approaches to diagnostic and treatment challenges. This ability is highly valued in medical education (Trullas et al., 2022; Wood, 2003). PBL encourages deeper learning and helps students apply knowledge in context, as they must come to class prepared to contribute meaningfully to discussions. This collaborative environment fosters skills including teamwork, communication, and problem solving, all essential in clinical and interdisciplinary settings. Studies have shown that students trained in PBL demonstrate strong independence by the end of their preclinical years, reflecting significant interpersonal growth attributable to the PBL curriculum (Richards et al., 1996).
PBL implementation platforms
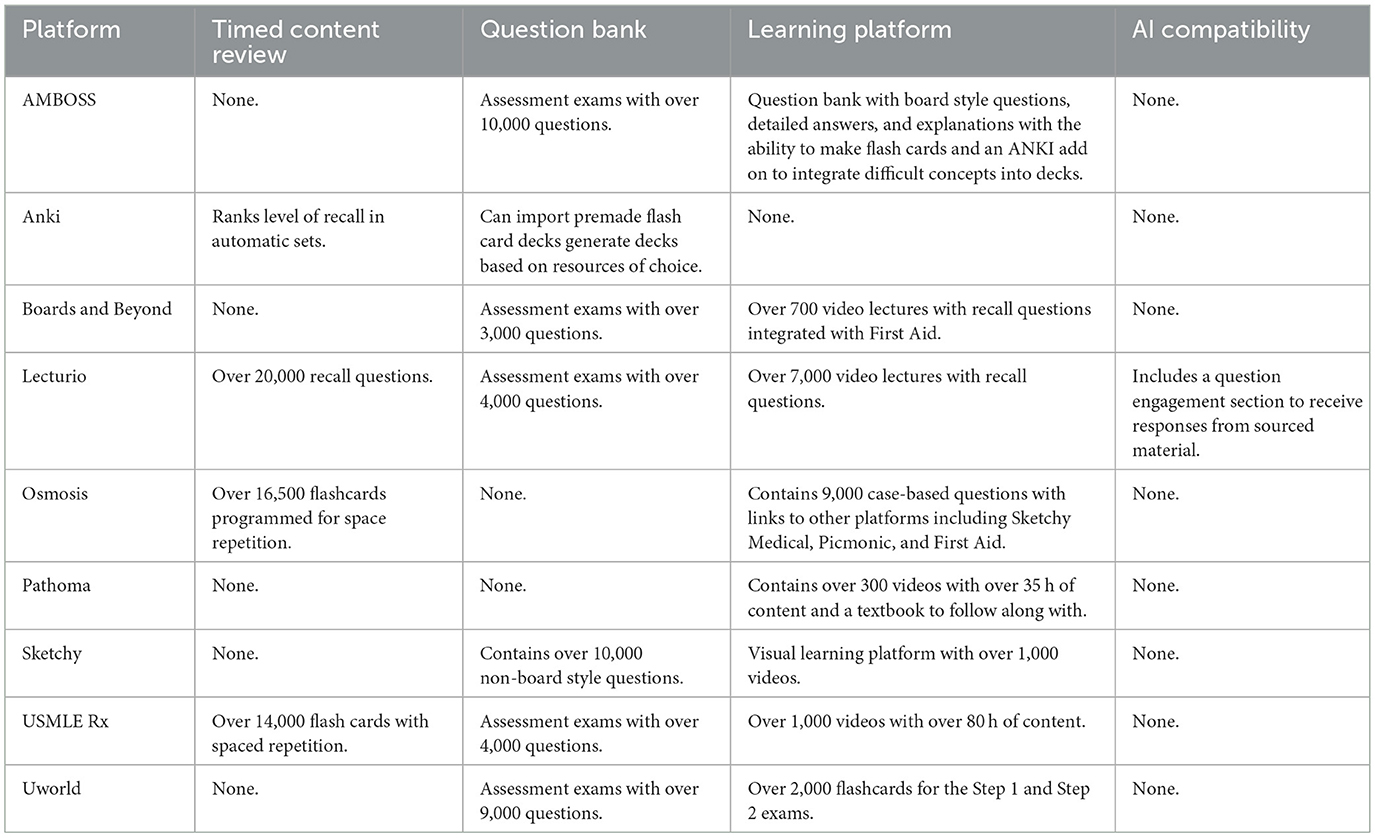
At least 70% of medical schools in the USA employ PBL in their preclinical years (Kinkade, 2005; Servant-Miklos, 2020; Jonas et al., 1992), with comparative advantages of PBL over traditional didactic teaching (Trullas et al., 2022; Sharma et al., 2023). A number of platforms have been developed to support PBL curriculums as shown in Table 2. Many students use multiple platforms and resources to supplement their learning. Some of the most widely used online learning platforms include: AMBOSS, Anki, Boards and Beyond, Lecturio, Osmosis, Pathoma, Sketchy, USMLE Rx, and UWorld.
• AMBOSS (www.amboss.com) is an integrated digital learning platform that serves as a medical knowledge base and a question bank with over 2,000 questions, videos and clinically focused topic summaries (AMBOSS, 2025). The platform also features a mobile application that can be utilized as a real time reference during problem-based learning (PBL) sessions and clinical rotations. Additionally, AMBOSS and Anki (see below) collaborated to generate an AMBOSS Anki Add-On tool which allows the learner to export information from the AMBOSS platform onto Anki flashcards that can be used for spaced repetition and recall. AMBOSS offers search functionality, mobile accessibility, and question based assessments that make it a versatile tool for academic preparation and clinical problem solving. Empirical analysis of user engagement supports its educational value. In a study involving over 23,000 users, the number of learning cards reviewed, and questions answered positively correlated with higher examination scores, suggesting that increased interaction with the platform contributes to improved academic performance (Bientzle et al., 2019).
• Anki (www.apps.ankiweb.net) is an open-source flashcard application developed by programmer Damien Elmes to facilitate language learning through spaced repetition. It has since been widely adopted in medical education due to its efficiency in promoting long term retention of large volumes of information. The program allows users to create custom flashcards or download premade decks, many of which are shared by other students and tailored to specific lectures, textbooks, and exam content (Anki, 2025). Notably, educational platforms such as AMBOSS have partnered with Anki to develop integrated decks that reinforce challenging medical topics as described above. Studies indicate that first year medical students who used Anki demonstrated significantly higher performance on course examinations and a comprehensive basic science exam compared to non-users (Gilbert et al., 2023). These findings suggest that Anki's spaced repetition system can meaningfully enhance academic outcomes in medical training.
• Boards & Beyond (www.boardsbeyond.com), developed by cardiologist Dr. Jason Ryan, is an online educational platform featuring comprehensive video lectures with over 500 h of content designed to supplement preclinical medical curricula and board exam preparation by covering subjects including anatomy, biochemistry, pharmacology, and pathology (Boards and Beyond, 2025). The videos are supplemented with reference slides and practice questions designed to reinforce key concepts. The platform includes Power Point based visuals that accompany each lecture, along with questions designed to help students assess their comprehension and retention of material. Boards & Beyond has been widely adopted during the early years of medical education, with nearly half of first year medical students reporting regular use of the resource (Finn et al., 2022). However, its usage tends to decline during the dedicated USMLE Step 1 study period with less than 20% of those students continuing to use it as a primary review tool (Finn et al., 2022). This pattern suggests that while Boards & Beyond is highly valued for building foundational knowledge, many students transition to more targeted or high yield resources as they prepare for board exams.
• Lecturio (www.lecturio.com) has built a platform that enables students to utilize curated content that supports virtual patient cases (pblmed.lecturio.com). This content includes over 6,000 video lectures that cover anatomy, physiology, pharmacology, and other subjects related to medical and clinical training (Lecturio, 2025). The platform also offers an extensive library of medical concept study pages designed to enhance understanding of complex medical topics. Lecturio also offers a question bank with over 6,000 questions with an “adaptive review” system and an “spaced repetition algorithm” with “tutor” and timed modes linked to video lessons and other references that are customized to prepare for board exams. This enhances the PBL curriculum by embracing a flipped classroom approach giving the students effective tools to succeed in their cases and career (Sharma et al., 2023). The Lecturio platform also offers faculty accounts that can be used to evaluate student progress through content including videos and questions. This enables faculty to identify individual student needs and help guide them through the learning process.
• Osmosis (www.osmosis.org) is a comprehensive multimedia learning platform designed to support medical education through a combination of concise instructional videos, flashcards, and a question bank with over 2,000 questions covering topics including anatomy, physiology, pharmacology and pathology (Osmosis, 2025). Its content spans basic science and clinical topics and is organized into user friendly formats such as decision making trees and topic specific summary pages. Osmosis also offers a mobile application to readily access information. The platform is well-received in preclinical curricula with over 80% of first year medical students finding Osmosis videos helpful for understanding cardiovascular physiology, with many preferring them over traditional lectures (Tackett et al., 2021). Although Osmosis is particularly popular during the early phases of medical training, its use tends to decline during board exam preparation, with one survey reporting a drop in usage from over 50% in the first year to 11% during USMLE Step 1 study (Finn et al., 2022). Despite this trend, Osmosis remains a valuable tool for reinforcing foundational knowledge, enhancing engagement, and supporting multiple learning styles in preclinical education.
• Pathoma (www.pathoma.com) is a pathology-focused educational resource developed by Dr. Husain Sattar, consisting of the widely used textbook Fundamentals of Pathology and approximately 35 h of corresponding online video lectures (O'Hanlon and Laynor, 2019; Sattar, 2025). Designed to support medical students during their preclinical years, Pathoma emphasizes high yield pathology content presented in a concise and accessible format. Students are encouraged to follow along with the textbook while viewing the lectures to promote engagement and reinforce learning. Pathoma has become particularly popular for USMLE Step 1 preparation with over 80% of first year medical students using the platform during dedicated board exam study periods (Finn et al., 2022). Its clarity, organization, and focused coverage of essential pathology topics have led many students to regard it as a core resource for mastering pathology.
• Sketchy (www.sketchy.com) is a visual and auditory learning platform that employs story based animated scenes and artist designed sketches to support memory retention through vivid, mnemonic based learning (Sketchy, 2025). Originally developed to teach microbiology, it contains over 1,200 microbiology learning cards. Sketchy has expanded to cover a range of subjects including pharmacology and pathology using imaginative visual metaphors and recurring symbols to present clinically relevant information (O'Hanlon and Laynor, 2019). This distinctive approach has garnered widespread popularity among medical students with over 60% of first year students using Sketchy, and over 70% continuing to use it during USMLE Step 1 preparation (Finn et al., 2022).
• USMLE-Rx (www.usmle-rx.com) is a digital learning platform created by the authors of First Aid for the USMLE. This platform features a board relevant question bank with over 2,300 “Qmax” practice questions, a “Flash Facts” flashcard system, and video lectures as part of their “Rx260 program” designed to reinforce high yield content of the First Aid textbook through active recall and self-assessment (USMLE-Rx, 2025). Some of the videos contain clinically relevant case discussions to help students apply learning material to real life scenarios. Despite its structured alignment with First Aid, USMLE-Rx is used by a relatively small proportion of students during Step 1 preparation with less than 15% of students using it regularly (Finn et al., 2022).
• UWorld (www.uworld.com) is a widely recognized and extensively utilized online question bank. It features over 2,000 questions geared to the USMLE Step 1 exam and over 2,000 questions geared to the USMLE step 2 exam. The questions bank also provides a subset of questions geared toward osteopathic students geared to the COMLEX level 1 and 2 exams. This question banks offers tutor and timed modes to give students the option to simulate time constraints during exams. A central strength of UWorld lies in its integration of in-depth feedback through its detailed answer explanations, which reinforce learning and help solidify key concepts across physiology, pathology, pharmacology, and clinical management. Consequently, UWorld is frequently used as a primary learning resource during preclinical and clinical training as well as a test preparation tool. Its widespread adoption is evidenced by survey data indicating that over 95% of medical students use UWorld during their dedicated Step 1 study period (Finn et al., 2022). The platform offers a mobile application for students to access as well as flashcard capability (UWorld, 2025).
Studies indicate that integration of online video resources with PBL classes can enhance medical education. For example, first year medical students provided with curated online videos to provide preparatory material before engaging in PBL sessions exhibited deeper understanding and improved engagement with complex medical concepts than students not provided these videos (Hamilton et al., 2023). This study highlighted synergistic effects of these learning modalities, emphasizing how curated content serves as a scaffold to help students focus on critical thinking and application during PBL sessions. This blended approach aligns with contemporary pedagogical trends in medical education, advocating for technology enhanced active learning strategies to meet the evolving needs of diverse learner populations.
PBL patient cases
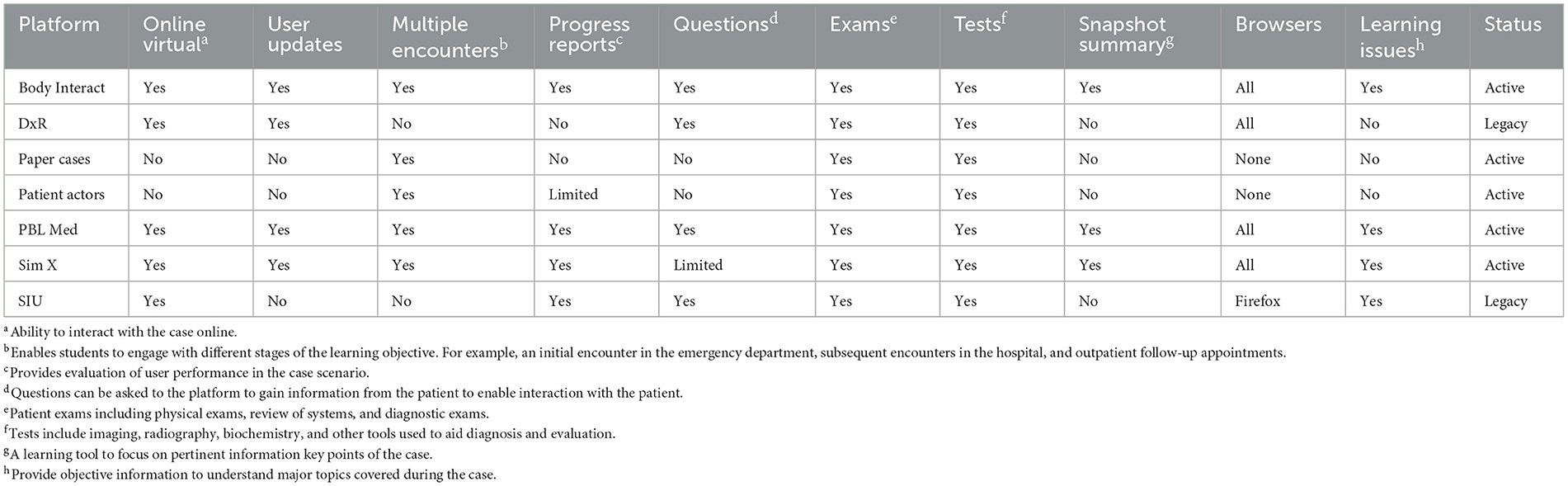
PBL curriculums in medical education use patient cases to allow students to apply their knowledge, review key teaching points, and gain a deeper understanding of the concepts that arise from realistic scenarios. There are different means of delivering cases. The three most utilized methods rely on: (1) actors, (2) paper cases, and (3) virtual cases.
Actors can be either virtual or in person. Typically, actors are individuals who are provided with a script prior to the class. During the session, students engage in various questions to understand the clinical presentation and courses of action. However, since the actor is not likely to have extensive medical training, and the students are still in their preclinical years, questions regarding symptoms and other patient presentations might be answered incorrectly. This process can mislead student learning objectives, and result in inaccurate learning. In addition, patient actors do not readily provide clear reports, imaging, and other content that is available with other methods of case presentations.
Paper cases are another option for presenting PBL patients. These cases are typically stored in a binder, with one student reading through the case while the rest of the group listens. This process is awkward since the reader is expected to read through the case in real time while students are waiting for answers. In addition, the cases are not easily updated to reflect current research and clinical guidelines. Shorter written cases or “vignettes” are also used in PBL classes. These can present specific points to cover in relatively short time frames. However, they also tend to rely on instructor knowledge to maintain accuracy of the material involved in each case.
Virtual methods for presenting PBL cases have become an important part of many PBL teaching curriculums. These cases can be accessed in classrooms and virtually online. These virtual cases allow for discourse and interactions between the learner and the case which enhances the learning experience. Virtual cases can also be updated to ensure current and accurate information. Virtual platforms have become the cornerstone of PBL in medical education. Common virtual case platforms used by medical schools include Body Interact, DxR, PBL Med, Sim X, and SIU. These platforms present various advantages and limitations as shown in Table 3.
Body Interact (at www.bodyinteract.com) offers scenarios across more than fifty specialties and is available in eight different languages. The platform features various settings, including street scenes, ambulances, and follow-up outpatient care. It provides real-time patient monitoring and includes over 80 physical exam findings, allowing students to practice conducting a full physical exam. Additionally, the platform offers more than 290 tests, including labs and imaging. Moreover, Body Interact includes over 200 interventions, enabling students to alter patient positioning, administer oxygen, perform life support, and more. While this platform is not generally used in PBL curriculums, it provides an alternative to mannequins used in medical school simulation centers.
DxR (Diagnostic Clinical Reasoning Program at www.dxrgroup.com) is an online platform with patient cases to help students develop clinical reasoning skills. In addition, DxR provides immediate feedback to students based on what they do in the platform. For example, if a student orders an inappropriate test, the platform will engage the student and explain why that test is not needed. The platform also has cases in different medical scenarios which broadens student exposure to various clinical complaints. The cases can also be updated so that the information reflects current research and clinical guidelines. Additionally, the platform has multimedia access allowing students the ability to listen to physical exam findings and see relevant imaging among other capabilities. However, the system does not offer multiple encounters with the same patient to track and understand disease progression. Also, progress reports are not incorporated into the application which also does not offer snapshot summaries, mapped resources, or learning issues. In general, the DxR platform is geared best to student assessment more than learning.
PBLMed (PBL Medicine at www.pblmed.com) is another online platform that offers virtual patient presentations. The PBLMed platform offers features including user updates and multimedia access. The platform also offers multiple encounters with the same patient to learn about disease progression and patient progress. PBLMed also includes snapshot summaries that offer learners an organized overview of each case. Additionally, the platform provides progress reports to help keep learners on track, as well as learning issues that guide students to focus on specific topics after each case. The platform features over 220 questions that reflect patient responses to clinical inquiries, along with medical, social, and family history prompts. It also includes over 130 exams that cover various organ systems and over 640 tests representing a wide range of imaging and lab value tests that students can order (Hamilton et al., 2023). PBLMed is compatible with all browsers to ensure broad accessibility. Moreover, PBLMed is set up to integrate each case with educational materials provided by Lecturio. This feature enables students to review relevant content while engaging with cases in order to enhance student learning objectives. Additionally, students can review learning issues and quiz themselves after completing cases in order to reinforce and reflect on the material more effectively.
Sim X Virtual Manikin (at www.simxvr.com) is a virtual reality platform designed to simulate clinical encounters. It features over 425 different patient models, over 1,000 simulated tools, and over 470 unique settings. Users can request custom clinical scenarios by altering lab findings and results, allowing for tailored practice opportunities. Educators can assess students as they engage with the platform, providing valuable insights into their performance. The platform offers flexibility by enabling trainees to work on cases on campus or remotely. Learners interact with virtual patients directly, without needing to select items from dropdown menus or lists. Additionally, Sim X supports collaborative training, allowing learners to work together on a single patient (SpaceRef, 2023).
SIU (Southern Illinois University at www.siumed.edu) offers a platform that enables students to engage with clinical cases in a virtual setting, allowing them to collaborate as they work through each case. Like other platforms, the interface allows students to view patient charts and ask preselected questions with predefined answers. This includes the ability to inquire about physical exam findings and test results. However, students are restricted from asking questions beyond the preformatted list. Other limitations of the SIU platform are that the cases are static and cannot be updated, and that the platform does not allow access to multimedia resources such as heart sounds and dynamic imaging results. As a result, the information cannot be refreshed to align with evolving clinical guidelines. In addition, SIU cases do not feature multiple patient encounters, though progress reports are available to the learner throughout the cases. A notable downside is that the platform is only compatible with Firefox, and it does not provide snapshot summaries or mapped resources. However, SIU cases do offer some deep insights into each case and present suggested learning issues. Each case aims to help students develop diagnostic reasoning and prepare treatment plans based on the information provided.
PBL accessibility
Accessibility has long been a concern in medical education, and digital platforms offer promising avenues to mitigate these challenges. It is well-recognized that medical training is expensive, both for institutions (which must invest in faculty, facilities, and materials) and for students (who face tuition fees and the cost of textbooks, review courses, etc.; Walsh, 2018). PBL, while pedagogically effective, can further increase instructional burden since it typically requires small tutor-to-student ratios, significant faculty development, and adequate infrastructure to support group learning (Clark, 2006). Traditional PBL curricula thus demand substantial resources. The strategic use of digital technology has been proposed as a way to deliver high-quality education. E-learning platforms can potentially reduce the need for physical materials (e.g., replacing some textbooks with online content) and allow one instructor to reach a large and geographically dispersed audience. As one commentary notes, there is enthusiasm for e-learning as a method that can deliver worthwhile outcomes, with studies showing that online learning can produce outcomes comparable to face-to-face instruction (Walsh, 2018). For example, instead of hiring additional lecturers or purchasing numerous cadavers for anatomy teaching, a medical program might use a combination of virtual anatomy software and online modules. Similarly, integrating an online PBL platform can offer reusable digital case materials that do not need to be printed or physically distributed. From the student perspective, digital resources can provide a comprehensive repository of lectures, question banks, and reference materials. Additionally, educational content including open-access medical journals, online question sets, and educational internet channels can be used to supplement formal learning (Walsh, 2018).
Accessibility is a critical dimension where digital platforms have a transformative impact. Online learning removes geographical barriers, allowing students in remote or underserved regions to access quality educational content that was once limited to those in major academic centers. Digital PBL sessions can connect learners from different hospitals, cities, or countries, fostering a more diverse exchange of knowledge and experiences. According to recent perspectives, online learning has the potential to enhance open and equitable access to medical education resources globally (Han and Kumwenda, 2025). A medical student with an internet connection can, in principle, watch lectures from experts worldwide, participate in virtual case discussions, or use the same question banks as students in top-tier universities. This democratization of knowledge is a significant step toward reducing disparities in educational opportunities. For instance, a student in a developing country might not have local access to specialized instructors or libraries, but through digital platforms, they can learn content and practice as well as their peers in other places. Moreover, digital resources support on-demand learning, meaning students can engage with materials at times that suit their work schedule or personal circumstances. This flexibility is particularly beneficial for those who may be working part-time, have family responsibilities, or are otherwise unable to attend live classes regularly.
However, it is important to acknowledge that digital solutions are not a panacea for all accessibility issues. They come with their own challenges, such as the requirement of reliable internet access and devices, and the need for digital literacy. In some cases, if not proactively addressed, online education can inadvertently widen the gap—a phenomenon referred to as the “digital divide” (Han and Kumwenda, 2025). Students or institutions in low-resource settings might struggle with bandwidth limitations and software access. To truly mitigate educational inequalities, stakeholders must invest in improving internet infrastructure and provide support to those who need to access learning platforms. Encouragingly, many organizations and academic consortia are working on open-access materials and sharing digital curricula freely, which can help bridge these gaps. Furthermore, as noted by (Lim 2023), achieving the full benefit of PBL (digital or otherwise) requires appropriate infrastructure and faculty training. This implies that careful planning and resource allocation are needed to ensure that digital PBL implementations are sustainable and equitable. When implemented thoughtfully, digital platforms can greatly increase the reach of medical education, standardize the quality of content delivered, and reduce burdens associated with traditional teaching methods. The continued effort to expand connectivity and create inclusive digital learning environments will determine how broadly these advantages are felt across different regions and socioeconomic groups.
Additional considerations
Despite many strengths, PBL curricula have intrinsic drawbacks and challenges. Class success depends heavily on active student participation and attentive faculty. Unprepared or engaged students can hinder the learning experience for the entire class. Moreover, instructors must be able to encourage discussion and also ensure that each student has the opportunity to participate. It can be challenging for instructors to prevent some participants from dominating group conversations while nurturing enthusiasm and positive group dynamics. In addition, PBL classes often utilize small groups to enhance active learning. However, these small groups also require more instructors than larger classes. Therefore, small group PBL classes can increase administrative expenses for faculty and infrastructure including classrooms and technologies needed to cases and online platforms (Lim, 2023; Tefera et al., 2024).
Conclusion
Medical education has evolved over time, with PBL assuming a leading role in many curriculum. In particular, PBL addresses concerns that arise from cost effective training, independent learning, and retention of clinical knowledge. Here, we describe several platforms that currently exist to support this approach. However, more platforms and dynamic learning methods are bound to be developed as technology advances. The need for more physicians is clearly evident and PBL is well-positioned to addressed this situation by increasing access to medical training for more students around the world.
Author contributions
AG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. GG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded in part by NIH grant R15CA271044 to GG. GG is a founder and owner of the PBLMed platform, but has not received any payment for its use and was not involved in platform evaluations for this report to mitigate potential conflict of interest related to this relationship.
Acknowledgments
We are grateful to Manuel Mendive, Svetoslav Denev, and Stefan Wisbauer (Lecturio GmbH, Germany), Shumin Guo (PBLMed, USA), and Peter Stein (Rowan-SOM, USA) for technical assistance and helpful conversations.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alaagib, N. A., Musa, O. A., and Saeed, A. M. (2019). Comparison of the effectiveness of lectures based on problems and traditional lectures in physiology teaching in Sudan. BMC Med. Educ. 19:365. doi: 10.1186/s12909-019-1799-0
AMBOSS (2025). Available online at: https://www.amboss.com (accessed March 26, 2025).
Anki (2025). Powerful, Intelligent Flashcards. Available online at: https://apps.ankiweb.net/ (accessed March 27, 2025).
Azzahrani, M. (2024). Problem-based learning for interprofessional education: a review of the concept and its application in a geriatric team. Cureus 16:e63055. doi: 10.7759/cureus.63055
Bernacer, J., and Murillo, J. I. (2014). The Aristotelian conception of habit and its contribution to human neuroscience. Front. Hum. Neurosci. 8:883. doi: 10.3389/fnhum.2014.00883
Bientzle, M., Hircin, E., Kimmerle, J., Knipfer, C., Smeets, R., Gaudin, R., et al. (2019). Association of online learning behavior and learning outcomes for medical students: large-scale usage data analysis. JMIR Med. Educ. 5:e13529. doi: 10.2196/13529
Boards and Beyond (2025). Available online at: https://www.boardsbeyond.com (accessed March 28, 2025).
Camp, G. (2016). Problem-based learning: a paradigm shift or a passing fad? Med. Educ. Online 1. doi: 10.3402/meo.v1i.4282
Clark, C. E. (2006). Problem-based learning: how do the outcomes compare with traditional teaching? Br. J. Gen. Pract. 56, 722–723.
Dolmans, D. H., Grave, W. D. e, Wolfhagen, I. H., and van der Vleuten, C. P. (2005). Problem-based learning: future challenges for educational practice and research. Med. Educ. 39, 732–741. doi: 10.1111/j.1365-2929.2005.02205.x
Dunn, P. M. (2006). Aristotle (384-322 BC): philosopher and scientist of ancient Greece. Arch. Dis. Child. Fetal Neonatal Ed. 91, F75–F77. doi: 10.1136/adc.2005.074534
Fallace, T. D. (2008). John Dewey and the savage mind: uniting anthropological, psychological, and pedagogical thought, 1894-1902. J. Hist. Behav. Sci. 44, 335–349. doi: 10.1002/jhbs.20328
Finn, E., Ayres, F., Goldberg, S., and Hortsch, M. (2022). Brave new E-world: medical students' preferences for and usage of electronic learning resources during two different phases of their education. FASEB Bioadv. 4, 298–308. doi: 10.1096/fba.2021-00124
Frambach, J. M., Talaat, W., Wasenitz, S., and Martimianakis, M. A. T. (2019). The case for plural PBL: an analysis of dominant and marginalized perspectives in the globalization of problem-based learning. Adv. Health Sci. Educ. Theory Pract. 24, 931–942. doi: 10.1007/s10459-019-09930-4
Ghani, A. S. A., Rahim, A. F. A., Yusoff, M. S. B., and Hadie, S. N. H. (2021). Effective learning behavior in problem-based learning: a scoping review. Med. Sci. Educ. 31, 1199–1211. doi: 10.1007/s40670-021-01292-0
Gilbert, M. M., Frommeyer, T. C., Brittain, G. V., Stewart, N. A., Turner, T. M., Stolfi, A., et al. (2023). A Cohort study assessing the impact of anki as a spaced repetition tool on academic performance in medical school. Med. Sci. Educ. 33, 955–962. doi: 10.1007/s40670-023-01826-8
Goss, D. A. (2009). Johannes Amos Comenius (1592-1670) and his depiction of lenses and spectacles in the first children's picture book. Hindsight 40, 25–28.
Hall, J. C. (1973). Rousseau: An Introduction to his Political Philosophy. Cambridge, MA: Schenkman.
Hamilton, K. L., Kuo, Y. C., Horneffer, P., Stein, T. P., and Goldberg, G. S. (2023). Video didactic preparation augments problem-based learning for first year medical students. J. Med. Educ. Curric. Dev. 10:23821205231177862. doi: 10.1177/23821205231177862
Han, S. P., and Kumwenda, B. (2025). Bridging the digital divide: promoting equal access to online learning for health professions in an unequal world. Med. Educ. 59, 56–64. doi: 10.1111/medu.15455
Heafford, M. R. (2016). Pestalozzi: His Thought and Its Relevance Today. London: Routledge. doi: 10.4324/9781315441405
Hmelo-Silver, C. E. (2004). Problem-based learning: what and how do students learn. Educ. Psychol. Rev. 16, 235–266. doi: 10.1023/B:EDPR.0000034022.16470.f3
Ho, Y. R., Chen, B. Y., and Li, C. M. (2023). Thinking more wisely: using the Socratic method to develop critical thinking skills amongst healthcare students. BMC Med. Educ. 23:173. doi: 10.1186/s12909-023-04134-2
Howard Barrows (2025). Available online at: https://en.wikipedia.org/wiki/Howard_Barrows (accessed May 16, 2025).
Jonas, H. S., Etzel, S. I., and Barzansky, B. (1992). Educational programs in US medical schools. JAMA 268, 1083–1090. doi: 10.1001/jama.1992.03490090025009
Kinkade, S. (2005). A snapshot of the status of problem-based learning in U. S. medical schools, 2003-04. Acad. Med. 80, 300–301. doi: 10.1097/00001888-200503000-00021
Kraft, S. K., Honebein, P. C., Prince, M. J., and Marrero, D. G. (1997). The SOCRATES curriculum: an innovative integration of technology and theory in medical education. J. Audiov. Media Med. 20, 166–171. doi: 10.3109/17453059709063100
kraut (2025). Socrates. Available online at: https://www.britannica.com/biography/Socrates (accessed February 6, 2025).
Kumar, T., Sakshi, P., and Kumar, C. (2022). Comparative study between “case-based learning” and “flipped classroom” for teaching clinical and applied aspects of physiology in “competency-based UG curriculum”. J. Family Med. Prim. Care 11, 6334–6338. doi: 10.4103/jfmpc.jfmpc_172_22
Lecturio (2025). Available online at: https://www.lecturio.com/ (accessed March 26, 2025).
Lim, W. K. (2023). Problem based learning in medical education: handling objections and sustainable implementation. Adv. Med. Educ. Pract. 14, 1453–1460. doi: 10.2147/AMEP.S444566
Mesko, B., and Spiegel, B. (2022). A revised hippocratic oath for the era of digital health. J. Med. Internet Res. 24:e39177. doi: 10.2196/39177
National Palace Museum (2025). Available online at: https://theme.npm.edu.tw/exh106/Confucius/en/page-2.html (accessed February 25, 2025).
Ng, M. L., Bridges, S., Law, S. P., and Whitehill, T. (2014). Designing, implementing and evaluating an online problem-based learning (PBL) environment–a pilot study. Clin. Linguist. Phon. 28, 117–130. doi: 10.3109/02699206.2013.807879
O'Hanlon, R., and Laynor, G. (2019). Responding to a new generation of proprietary study resources in medical education. J. Med. Libr. Assoc. 107, 251–257. doi: 10.5195/jmla.2019.619
Omar, S. (1979). Ibn Al-Haytham's theory of knowledge and its significance for later science. Arab. Stud. Q. 1, 67–82.
Osmosis (2025). Available online at: www.osmosis.org (accessed March 25, 2025).
Plato (2000). Apology. Indianapolis: Hackett Publishing Company, Readings in Ancient Greek Philosophy: from Thales to Aristotle.
Punja, D., Kalludi, S. N., Pai, K. M., Rao, R. K., and Dhar, M. (2014). Team-based learning as a teaching strategy for first-year medical students. Australas. Med. J. 7, 490–499. doi: 10.4066/AMJ.2014.2244
Richards, B. F., Ober, K. P., Cariaga-Lo, L., Camp, M. G., Philp, J., McFarlane, M., et al. (1996). Ratings of students' performances in a third-year internal medicine clerkship: a comparison between problem-based and lecture-based curricula. Acad. Med. 71, 187–189. doi: 10.1097/00001888-199602000-00028
Saqr, M., Nouri, J., Vartiainen, H., and Malmberg, J. (2020). What makes an online problem-based group successful? A learning analytics study using social network analysis. BMC Med. Educ. 20:80. doi: 10.1186/s12909-020-01997-7
Sattar, H. (2025). Pathoma. Available online at: www.pathoma.com (accessed March 27, 2025).
Servant-Miklos, V. (2020). Problem-oriented project work and problem-based learning: “mind the gap!”. Interdiscipl. J. Probl. Based Learn. 14. doi: 10.14434/ijpbl.v14i1.28596
Sharma, S., Saragih, I. D., Tarihoran, D., and Chou, F. H. (2023). Outcomes of problem-based learning in nurse education: a systematic review and meta-analysis. Nurse Educ. Today 120:105631. doi: 10.1016/j.nedt.2022.105631
Sketchy (2025). Available online at: www.sketchy.com (accessed March 27, 2025).
SpaceRef (2023). SimX Awarded U.S. Space Force Contract to Adapt VR Medical Simulation Training for Astronaut Recovery and Space Launch Medicine. Alexandria, VA: spacenews.com.
Tackett, S., Green, D., Dyal, M., O'Keefe, E., Thomas, T. E., Nguyen, T., et al. (2021). Use of commercially produced medical education videos in a cardiovascular curriculum: multiple cohort study. JMIR Med. Educ. 7:e27441. doi: 10.2196/27441
Tefera, A. S., Melaku, E. E., Urgie, B. M., Hassen, E. M., Tamene, T. D., Gebeyaw, E. D., et al. (2024). Barriers to implementing problem-based learning at the school of medicine of Debre Berhan University, Ethiopia. BMC Med. Educ. 24:501. doi: 10.1186/s12909-024-05252-1
Timmer, M. C. J., Steendijk, P., Arend, S. M., and Versteeg, M. (2020). Making a lecture stick: the effect of spaced instruction on knowledge retention in medical education. Med. Sci. Educ. 30, 1211–1219. doi: 10.1007/s40670-020-00995-0
Trullas, J. C., Blay, C., Sarri, E., and Pujol, R. (2022). Effectiveness of problem-based learning methodology in undergraduate medical education: a scoping review. BMC Med. Educ. 22:104. doi: 10.1186/s12909-022-03154-8
USMLE-Rx (2025). Available online at: www.usmle-rx.com (accessed March 26, 2025).
UWorld (2025). Available online at: https://www.uworld.com/ (accessed March 27, 2025).
Vieira, M. L. (2025). Bringing microbiology to life: problem-based learning activities enhance student engagement and clinical reasoning in the early medical curriculum. FEMS Microbiol. Lett. 372:fnaf075. doi: 10.1093/femsle/fnaf075
Walsh, K. (2018). Cost and value in e-learning: the perspective of the learner. BMJ Simul. Technol. Enhanc. Learn. 4, 201–202. doi: 10.1136/bmjstel-2017-000239
Wang, A. Y., Zhao, H. C., Song, Y. W., Xiong, B. L., Guo, Z. Y., Sun, X. D., et al. (2025). Application of PBL in combination with the SP teaching method in the clinical teaching of orthopedics and traumatology. BMC Med. Educ. 25:1113. doi: 10.1186/s12909-025-07658-x
Wang, S. Y., Tsai, J. C., Chiang, H. C., Lai, C. S., and Lin, H. J. (2008). Socrates, problem-based learning and critical thinking — a philosophic point of view. Kaohsiung J. Med. Sci. 24, S6–13. doi: 10.1016/S1607-551X(08)70088-3
Yardley, S., Teunissen, P. W., and Dornan, T. (2012). Experiential learning: AMEE guide No. 63. Med. Teach. 34, e102–e115. doi: 10.3109/0142159X.2012.650741
Zaveri, N., Coty, M., McCarver, V., Vidic, C., Nolan, T., Nath, S., et al. (2019). Changes to an active learning curriculum in osteopathic medical education: effects on exam outcomes and board scores. Med. Sci. Educ. 29, 215–222. doi: 10.1007/s40670-018-00674-1
Keywords: PBL, problem based learning, education, virtual patients, online platforms
Citation: Greenspan AA, Goldberg GS and Hamilton KL (2025) Problem-based learning and digital platforms in medical education. Front. Educ. 10:1631337. doi: 10.3389/feduc.2025.1631337
Received: 19 May 2025; Accepted: 28 August 2025;
Published: 15 September 2025.
Edited by:
Yu-Tung Kuo, North Carolina Agricultural and Technical State University, United StatesReviewed by:
Ivan Šoša, University of Rijeka, CroatiaVenkataramana Kandi, Prathima Institute of Medical Sciences, India
Copyright © 2025 Greenspan, Goldberg and Hamilton. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gary S. Goldberg, Z29sZGJlZ2FAcm93YW4uZWR1
 Amanda A. Greenspan1
Amanda A. Greenspan1 Gary S. Goldberg
Gary S. Goldberg Kelly L. Hamilton
Kelly L. Hamilton