- Department of Gynecology, Cancer Hospital of China Medical University, Liaoning Cancer Hospital & Institute, Shenyang, China
Objectives: The relationship between diet quality indices and risk of ovarian and endometrial cancers were unclear. We aimed at conducting a systematic review to evaluate the epidemiological evidence.
Methods: Embase, PubMed, Web of Science and Scopus databases were searched for eligible studies up to December 2020. Epidemiological studies reported the association of the diet quality with risk of ovarian and endometrial cancers were evaluated.
Results: Eleven eligible studies were identified, of which six studies were case-control studies, four were cohort studies, and one was case-cohort study. All studies were considered as high-quality with low risk of bias. Seven studies evaluated the association of diet quality with risk of ovarian cancer. Four studies reported null association for diet quality indices such as Healthy Eating Index (HEI)-2005, HEI-2010, Mediterranean Diet Score (MDS) and Recommended Foods Score (RFS). Two studies reported significantly inverse association for Alternate Healthy Eating Index (AHEI)-2010 and Healthy Diet Score (HDS) indices. One study reported significantly increased risk of ovarian cancer associated with higher level of Dietary Guidelines for Americans Index. Dose-response analysis showed pooled relative risks of 0.98 (95%Cl: 0.95, 1.01) and 0.94 (95%Cl: 0.77, 1.13) for each 10 points increase in the HEI-2005 and AHEI-2010 indices. Seven studies evaluated the association of diet quality with risk of endometrial cancer. Three studies reported significantly inverse association of diet quality as assessed by the MDS and Diet Score Quintiles with risk of endometrial cancer. Four studies reported null association for other diet quality indices including HEI-2005, HEI-2010, RFS and HDS. Dose-response analysis showed a pooled relative risk of 0.87 (95%CI: 0.81, 0.93) for one unit increment of the MDS.
Conclusion: This study suggests little evidence on the association between diet quality and risk of ovarian cancer. Adherence to high quality diet, as assessed by MDS, might be associated with lower the risk of endometrial cancer.
Introduction
Ovarian and endometrial cancers are two most common gynecological cancers and the leading cause of death due to gynecological cancer among women in Western countries (1). According to the GLOBOCAN cancer statistics, the estimated numbers of new cases due to ovarian and endometrial cancers worldwide were 295,414 and 382,069 in 2018, respectively (1). Thus, the identification of modifiable risk factors has continued being of clinical and public health importance to prevent ovarian and endometrial cancers.
Risk factors for ovarian cancer include absence of pregnancy, early age of menarche, late age at menopause, family history of ovarian cancer, smoking and benign gynecological conditions (2). Diet may play an important role in the etiology of ovarian cancer, but the associations between ovarian cancer risk and dietary factors such as black tea, milk, lactose and calcium were supported by weak evidence (2, 3). Well-established risk factors of endometrial cancer include nulliparous, higher body mass index and waist-to-hip ratio (4). However, dietary factors for ovarian cancer are still not apparent. Increased intake of coffee, monounsaturated fatty acid and fiber may be associated with lower risk of endometrial cancer, while western style pattern dietary intake may be associated with higher risk of endometrial cancer (4).
Although it is important to understand the role of individual dietary constituents, foods are not consumed in isolation. Diet quality indices such as the Healthy Eating Index-2005 (HEI-2005), Healthy Eating Index-2010 (HEI-2010), Alternate Healthy Eating Index-2010 (AHEI-2010) and Mediterranean diet score (MDS)/Alternate Mediterranean Diet Score (aMDS) address the complexity of the diet and the likely interaction between multiple diet components (5). Despite the various differences between these diet indices, a commonality is that they assess intake of desirable food groups such as fruits, vegetables, whole grains, nuts, and legumes (5). Diets that score highly on the HEI and AHEI were associated with a significant reduction in the risk of all-cause mortality, cardiovascular disease, cancer, type 2 diabetes, and neurodegenerative disease (6). The highest-quality diet as assessed by MDS was associated with reduced risks of breast and upper gastrointestinal cancers (7, 8). Previous epidemiological studies have evaluated the association between a variety of diet quality indices such as HEI, AHEI, MDS and other diet scores and risk of ovarian and endometrial cancers with inconsistent results (9–19). Several studies indicated that high quality diet was significantly associated with lower risk of these cancers (10, 12–14), whereas other studies suggested the null association (9, 11, 15–18). A US cohort study even reported an increased risk of ovarian cancer associated with higher adherence of the fifth edition of the Dietary Guidelines for Americans (19).
A thorough understanding of the relation between diet quality and risk of ovarian and endometrial cancers could facilitate the development of more effective strategy and recommendation on cancer prevention in women. Thus, we aimed at conducting a systematic review to evaluate the association between diet quality and risk of ovarian and endometrial cancers.
Materials and methods
This study was performed in adherence to PRISMA guidance (Supplementary Document 1) (20). Two researchers (YHZ and ZL) independently conducted the information collection including the literature search, study selection and information extraction. Whenever there is a discrepancy between the two authors, they first try to resolve it by an internal discussion; if consensus still cannot be reached, a third reviewer (MZT) acted as an arbitrator to make the final decision.
Literature Search
The Embase, PubMed, Web of Science and Scopus databases were searched up to Dec 2020, using the Mesh terms as well as the following words: (“diet quality” OR “diet score” OR “diet index” OR “healthy eating index” OR “Mediterranean diet” OR “dietary guidelines” OR “lifestyle index”) AND (ovarian OR ovary OR endometrial OR endometrium) AND (cancer OR tumor OR neoplasm OR carcinoma). We also searched Google Scholar for grey literature. Language of publication was restricted to English. Besides, we screened the reference lists of relevant studies to identify other potential studies. The search strategies were presented in Supplementary Document 2.
Study Selection
The inclusion criteria were as follows: (1) Study design should include cohort study, case-cohort or case-control study; (2) Studies should report diet quality indices as exposure of interest, such as HEI-2005, HEI-2010, AHEI-2010, MDS, other diet quality indices; (3) Studies should report ovarian or endometrial cancer as the outcome of interest; (5) Studies should report relative risk (RR), risk ratio, rate ratio, hazard ratio, odds ratio with the corresponding 95% confidence interval (CI) as the measure of association. When two or more studies covered the same study population, we selected the most recent one, or the most informative study, or extracted information from both studies as appropriate.
Data Extraction
A structured data extraction form was used to collect the study-specific information, which included the first author of the study, year of publication, study design, study location, study population, size of cohort/number of controls, age at baseline, exposures, exposure assessment methods, outcomes, outcome ascertainment, number of cases, follow-up time, risk estimates, and confounder adjustment. When there were multiple risk estimates in a study, we extracted the one most appropriately adjusted for the confounders in the analysis.
Study Quality Assessment
The study quality was assessed by two researchers (YHZ and ZL) independently. The Newcastle-Ottawa Scale, which was developed to evaluate the quality of observational studies, was used as the assessment tool (21). A study was judged on three broad perspectives: the selection of the study groups; the comparability of the groups; and the ascertainment of either the exposure or outcome of interest for case-control or cohort studies respectively. “High” quality choices were assigned with a maximum of two stars for items in “comparability” category, and with one star for other numbered items such as “selection of groups” and “ascertainment of the outcome or exposure”. Based on the criteria in previous studies (22, 23), a study with NOS score of ≥7 was considered as the high-quality study.
Statistical Analysis
Due to various types of dietary quality indices, as well as different ranges and categories of these indices in the population, there was significant heterogeneity across the studies regarding the risk estimates for highest category compared with the lowest category of dietary quality indices. Thus, we only attempted to conduct dose-response meta-analysis to pool the study-specific risk estimates for same dietary indices when more than one study reported the dose-response results. A dose-response meta-analysis may help reduce the heterogeneity, address the inconsistency of the individual studies and add further quantitative information for the review. Compared with risk estimate from a single study, a dose-response meta-analysis may tend to provide relatively precise risk estimates when the heterogeneity was low. The dose-response relation was estimated by using generalized least squares trend estimation, which was proposed by Greenland and Longnecker (24). We assigned the median value in each category of dietary indices to the corresponding RR for each study (25). If medians were not reported, we estimated approximate medians by using the midpoint of the lower and upper bounds (25). If the highest or lowest category of the studies was open-ended, we considered the range of the highest or lowest category to be equivalent to the difference in the closest adjacent category (25). We evaluated the heterogeneity across studies by using the I2 statistic (26). Statistical heterogeneity was indicated at an I2 of more than 50% (26). Statistical analyses were conducted using Stata 14.0.
Results
Study Selection
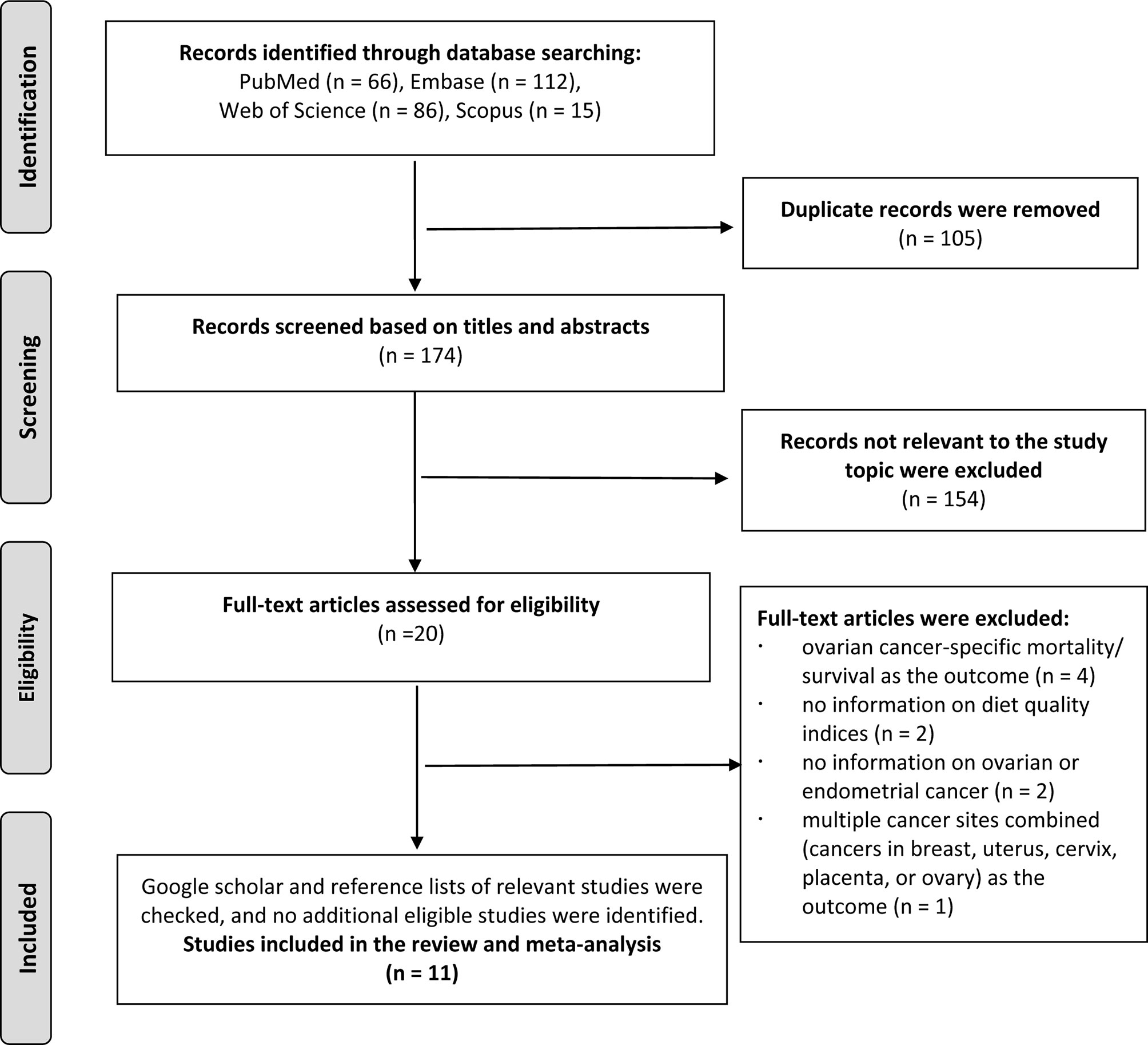
The literature search identified 279 total records from Embase, PubMed, Web of Science and Scopus databases. After we excluded 105 duplicates, 174 records remained for further screening. After screening the titles and abstracts, 154 non-relevant records were excluded, and 20 records were identified for further full-text review. During the full texts review stage, four studies were excluded because of reporting ovarian cancer-specific mortality/survival in women with ovarian cancer (27–30); two studies were excluded because of not reporting information on diet quality indices (31, 32); two studies were excluded because of not reporting information on ovarian or endometrial cancer (33, 34); one study was excluded because of reporting multiple cancer sites combined (cancers in breast, uterus, cervix, placenta, or ovary) as the outcome (35); Finally, we included eleven studies in the review (9–19) (Figure 1).
Study Characteristics
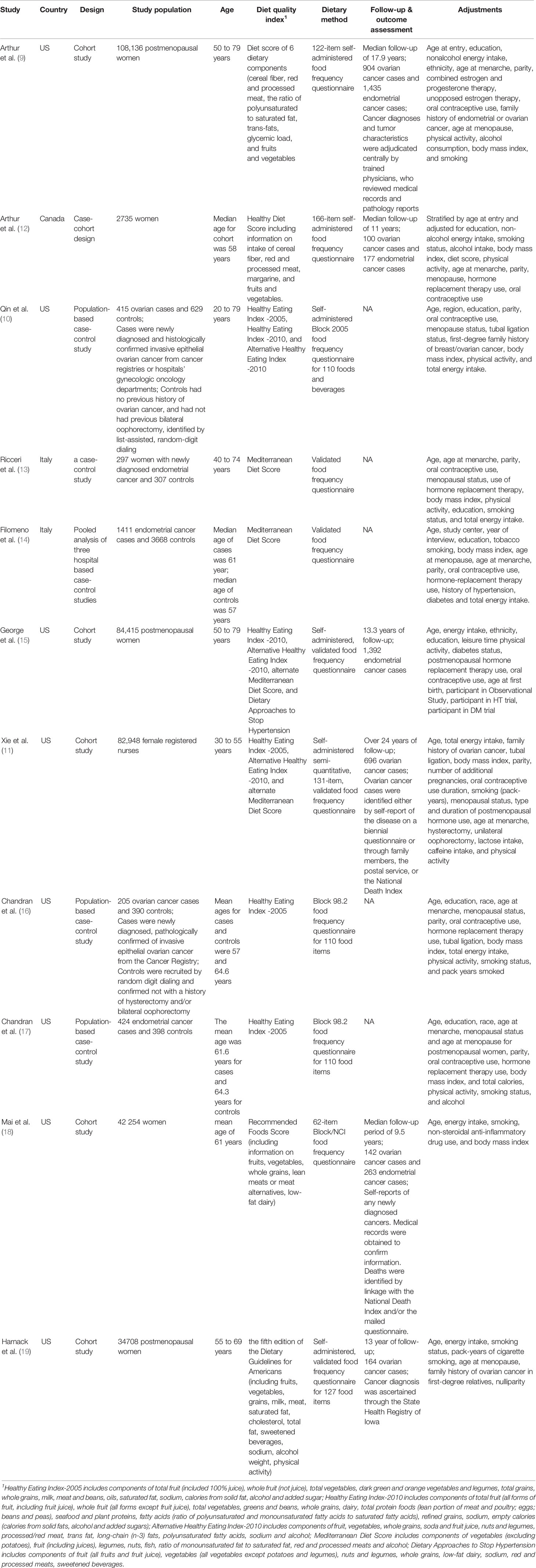
As shown in Table 1, among the eleven included studies, six studies were case-control studies, four were cohort studies, and one was case-cohort study. Most of the studies were conducted in Western countries, including US (n=8), Italy (n=2) and Canada (n=1). All the studies collected the diet information by food-frequency questionnaires. The diet quality was assessed by HEI-2005, HEI-2010, AHEI-2010, MDS/aMDS, DASH, Recommended Foods Score (RFS), Healthy Diet Score (HDS) and other diet quality indices. This study included 2626 and 3998 cases of ovarian and endometrial cancers, respectively. Information on cancer diagnosis was obtained from a variety of data sources including medical record review, patient contact, cancer or death registries. Most of the included studies reported risk estimates adjusted for the most potential confounders or risk factors such as age, body mass index, total energy intake, family history and smoking, etc. According to assessments from the Newcastle-Ottawa Scale, all the studies were considered as relatively high quality with low risk of bias (Supplementary Document 3).
Diet Quality and Ovarian Cancer Risk
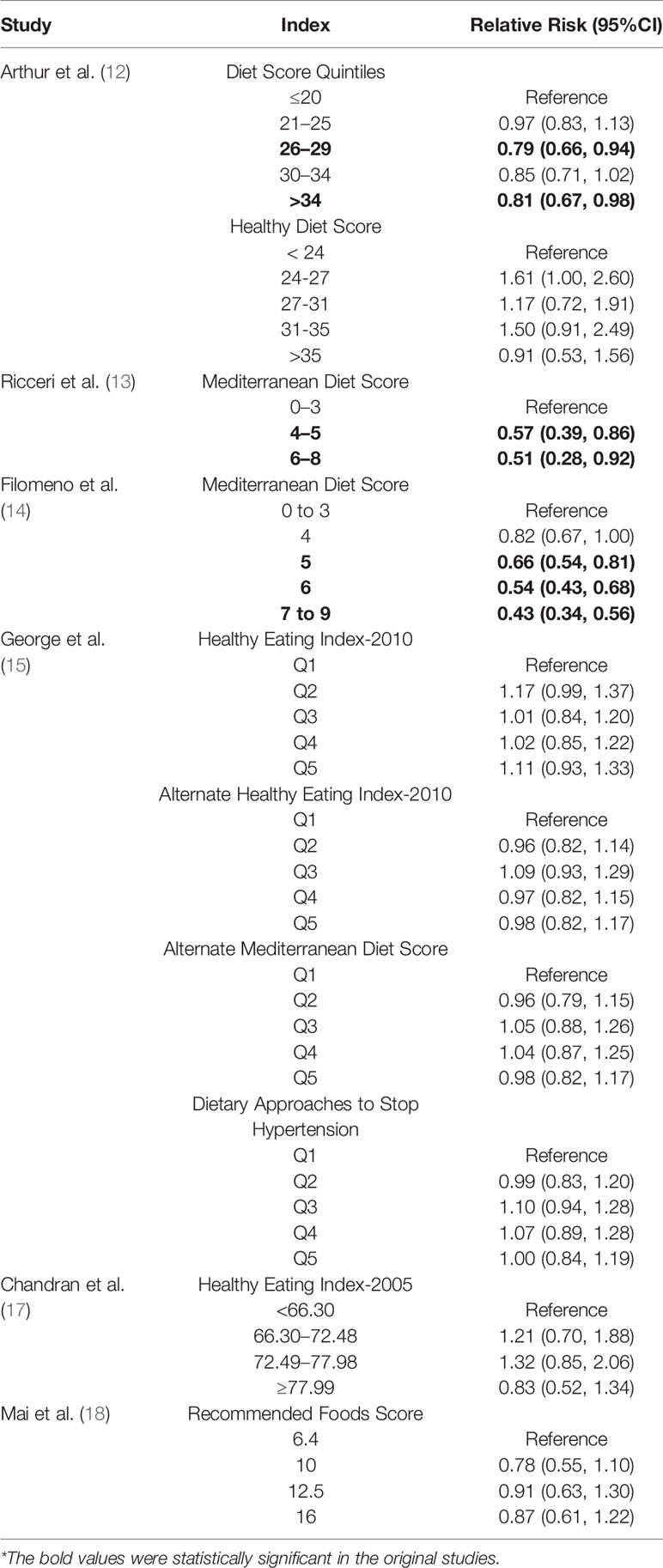
Seven studies evaluated the association of diet quality with risk of ovarian cancer. Two studies reported significantly inverse association of diet quality as assessed by AHEI-2010 and HDS with risk of ovarian cancer (Qin et al., 2017 study (10)): RR AHEI-2010 = 0.66, 95%CI: 0.45, 0.98; Arthur et al. (12) study: RR HDS = 0.50, 95%CI: 0.27, 0.92). One study reported significantly increased risk of ovarian cancer associated with high quality diet as assessed by “Dietary Guidelines for Americans Index” (RR = 2.05, 95%CI: 1.19, 3.52). Four studies reported null associations with RRs ranged from 0.76 (95%CI: 0.47, 1.22) to 1.03 (95%CI: 0.80, 1.34) for other diet quality indices such as HEI-2005, HEI-2010, aMDS and RFS. The main results for these seven included studies were shown in Table 2.
In the dose-response meta-analysis of three studies assessing diet quality with HEI-2005 index, the pooled RR for each 10 points increase was 0.98 (95%CI: 0.95, 1.01) without statistical heterogeneity (I2 = 0%, P heterogeneity = 0.968). Two studies assessed the diet quality using AHEI-2010 index, with pooled RR of 0.94 (95%CI: 0.77, 1.13) for each 10 points increase. Since limited number of studies were included in the dose-response results, these non-significant results should still be interpreted with caution due to lack of power.
Diet Quality and Endometrial Cancer Risk
Seven studies evaluated the association of diet quality with risk of endometrial cancer. Three studies reported significantly inverse association of diet quality as assessed by the MDS and Diet Score Quintiles with risk of endometrial cancer (Ricceri et al. (13) study: RR MDS = 0.51, 95%CI: 0.28, 0.92; Filomeno et al. (14) study: RR MDS = 0.43, 95%CI: 0.34, 0.56; Arthur et al. (9) study: RR Diet Score Quintiles = 0.81, 95%CI: 0.67, 0.98). Four studies reported null association with RRs ranged from 0.83 (95%CI: 0.52, 1.34) to 0.98 (95%CI: 0.82, 1.17) for other diet quality indices including HEI-2005, HEI-2010, RFS and HDS. The main results for the seven included studies were shown in Table 3. In the dose-response meta-analysis of two studies assessing diet quality with the MDS, the pooled RR for one unit increment of the MDS was 0.87 (95%CI: 0.81, 0.93).
Discussion
This review of epidemiological studies suggested little clear association of major diet quality indices, including HEI-2005, HEI-2010, AHEI-2010, aMDS and RFS, with risk of ovarian cancer. Of note, adherence to higher quality of diets, as assessed by MDS, may be associated with a lower risk of endometrial cancer. Dose-response analysis suggested a 13% reduction in risk of endometrial cancer for one unit increment in MDS in women. However, this inverse association with endometrial cancer was not observed for other diet quality indices including HEI-2005, HEI-2010 and RFS etc.
Assessment of the overall quality of diet instead of single nutrients can address the likely interaction between multiple diet components (5). Previous meta-analyses suggested high quality diets as assessed by the HEI, AHEI or DASH were associated with a significant reduction in the risk of total cancer (6, 36). However, concerning the ovarian cancer, the results were inconclusive since there is only one epidemiological study included in the previous study, and reported a null association (6). In the current review of seven studies, most studies still reported a null association. Although Qin et al., 2007 reported a reduced risk of ovarian cancer associated with the highest category of AHEI-2010 index, such significantly inverse association was not observed in the further dose-response meta-analysis. In addition, a population-based cohort study in China where the diet habits and pattern were different from the Western countries suggested that diet quality as assessed by Chinese food pagoda and modified DASH score was not associated with cancers in breast, uterus, cervix, placenta, or ovary combined, while adherence to modified AHEI-2010 was significantly associated with lower risk of these cancers combined (35). Compared with ovarian cancer, breast cancer cases accounted for a larger proportion. Thus, the inverse association was more likely to be due to a reduced risk of breast cancer rather than the ovarian cancer (35). Taken together, there was still no clear evidence indicating any association of diet quality with risk of ovarian cancer.
Our results suggested that, compared with other dietary indices HEI-2005, HEI-2010 and AHEI-2010, the MDS may capture aspects of diet more relevant to endometrial cancer. In a large case-control study in Italian population, there was a reduced risk of endometrial cancer for increasing adherence to the Mediterranean diet (14). The Mediterranean diet contains several antioxidants with important anti-inflammatory properties that have been inversely related with cancer risk (37). The Mediterranean diet is rich in vitamins, carotenoids, flavonoids and folates (mainly derived from vegetables and fruits), which have shown inverse relations with endometrial cancer in case-control studies (13, 14). Moreover, a large proportion of energy intake in the Mediterranean diet derives from cereals and other plant sources rather than from animal sources, which has been inversely associated with endometrial cancer risk (38). Besides, the richness of phytoestrogens in soy and whole grain products from the Mediterranean diet may exert protective effect on endometrial cancer (39). Since MDS takes into account the interactions among various combinations of foods and nutrients and their synergistic effects, Mediterranean diet as a whole may be a stronger determinant of endometrial cancer risk than the single dietary components (14).
There are several limitations in the study. Despite there are certain commonalities on the diet components for these diet quality indices, the weights of each components, assessment methods, and categories of the diet indices varied from study to study. The diet quality indices in these studies included HEI-2005, HEI-2010, AHEI-2010, aMDS and RFS, etc., Due to high heterogeneity of the diet quality as assessed by various diet quality indices, this review was mainly based on a systematic review of the current evidence, and little quantitative conclusion could be drawn. Although the dose-response meta-analyses for certain dietary indices were performed, the pooled risk estimates, especially the non-significant results, were still inconclusive due to the inclusion of a limited number of epidemiological studies. These results should still be interpreted with caution due to lack of statistical power. Further evidence from well-designed, large-scale cohort studies are still warranted before we could draw a confirmative conclusion. Furthermore, the epidemiological studies in the review were conducted in the Western population. As such, we should be more cautious in generalizing the results to other areas, especially where the dietary patterns and habits are different, such as Asia and Africa. In addition, non-English databases were not searched in the review, which may lead to publication bias.
In conclusion, this systematic review of the epidemiological studies suggests little evidence on the association between diet quality and risk of ovarian cancer. Adherence to high quality diets, as assessed by MDS, may be associated with lower risk of endometrial cancer. If a causal association could be confirmed by further well-designed studies, the adherence of the Mediterranean diet guidance might be encouraged for the prevention of endometrial cancer in women.
Data Availability Statement
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request. Requests to access these datasets should be directed to ZnVzYW4yMDIwQHNpbmEuY29t.
Author Contributions
Y-HZ developed the research design, interpreted the results, and also had primary responsibility for the final content. ZL and M-ZT analyzed the data and interpreted the results. Y-HZ drafted manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We appreciate Dr. Dan Zhao for her helpful suggestions on the statistical analysis of this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2021.659183/full#supplementary-material
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 countries. CA Cancer J Clin (2018) 68(6):394–424. doi: 10.3322/caac.21492
2. Lheureux S, Gourley C, Vergote I, Oza AM. Epithelial Ovarian Cancer. Lancet (2019) 393(10177):1240–53. doi: 10.1016/S0140-6736(18)32552-2
3. Sun H, Gong TT, Xia Y, Wen ZY, Zhao LG, Zhao YH, et al. Diet and Ovarian Cancer Risk: An Umbrella Review of Systematic Reviews and Meta-Analyses of Cohort Studies. Clin Nutr (2020) 2020:S0261–5614(20)30653-1. doi: 10.1016/j.clnu.2020.11.032
4. Raglan O, Kalliala I, Markozannes G, Cividini S, Gunter MJ, Nautiyal J, et al. Risk Factors for Endometrial Cancer: An Umbrella Review of the Literature. Int J Cancer (2019) 145(7):1719–30. doi: 10.1002/ijc.31961
5. Wirt A, Collins CE. Diet Quality–What is It and Does It Matter? Public Health Nutr (2009) 12(12):2473–92. doi: 10.1017/S136898000900531X
6. Schwingshackl L, Bogensberger B, Hoffmann G. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: an Updated Systematic Review and Meta-Analysis of Cohort Studies. J Acad Nutr Diet (2018) 118(1):74–100.e11. doi: 10.1016/j.jand.2017.08.024
7. Moazzen S, van der Sloot KWJ, Vonk RJ, de Bock GH, Alizadeh BZ. Diet Quality and Upper Gastrointestinal Cancers Risk: A Meta-Analysis and Critical Assessment of Evidence Quality. Nutrients (2020) 12(6):1863. doi: 10.3390/nu12061863
8. Du M, Liu SH, Mitchell C, Fung TT. Associations Between Diet Quality Scores and Risk of Postmenopausal Estrogen Receptor-Negative Breast Cancer: A Systematic Review. J Nutr (2018) 148(1):100–8. doi: 10.1093/jn/nxx015
9. Arthur R, Brasky TM, Crane TE, Felix AS, Kaunitz AM, Shadyab AH, et al. Associations of a Healthy Lifestyle Index with the Risks of Endometrial and Ovarian Cancer among Women in the Women’s Health Initiative Study. Am J Epidemiol (2019) 188(2):261–73. doi: 10.1093/aje/kwy249
10. Qin B, Moorman PG, Kelemen LE, Alberg AJ, Barnholtz-Sloan JS, Bondy M, et al. Dietary Quality and Ovarian Cancer Risk in African-American Women. Am J Epidemiol (2017) 185(12):1281–9. doi: 10.1093/aje/kwx022
11. Xie J, Poole EM, Terry KL, Fung TT, Rosner BA, Willett WC, et al. A Prospective Cohort Study of Dietary Indices and Incidence of Epithelial Ovarian Cancer. J Ovarian Res (2014) 7:112. doi: 10.1186/s13048-014-0112-4
12. Arthur R, Kirsh VA, Kreiger N, Rohan T. A Healthy Lifestyle Index and its Association with Risk of Breast, Endometrial, and Ovarian Cancer Among Canadian Women. Cancer Causes Control (2018) 29(6):485–93. doi: 10.1007/s10552-018-1032-1
13. Ricceri F, Giraudo MT, Fasanelli F, Milanese D, Sciannameo V, Fiorini L, et al. Diet and Endometrial Cancer: A Focus on the Role of Fruit and Vegetable Intake, Mediterranean Diet and Dietary Inflammatory Index in the Endometrial Cancer Risk. BMC Cancer (2017) 17(1):757. doi: 10.1186/s12885-017-3754-y
14. Filomeno M, Bosetti C, Bidoli E, Levi F, Serraino D, Montella M, et al. Mediterranean Diet and Risk of Endometrial Cancer: A Pooled Analysis of Three Italian Case-Control Studies. Br J Cancer (2015) 112(11):1816–21. doi: 10.1038/bjc.2015.153
15. George SM, Ballard R, Shikany JM, Crane TE, Neuhouser ML. A Prospective Analysis of Diet Quality and Endometrial Cancer Among 84,415 Postmenopausal Women in the Women’s Health Initiative. Ann Epidemiol (2015) 25(10):788–93. doi: 10.1016/j.annepidem.2015.05.009
16. Chandran U, Bandera EV, Williams-King MG, Paddock LE, Rodriguez-Rodriguez L, Lu SE, et al. Healthy Eating Index and Ovarian Cancer Risk. Cancer Causes Control (2011) 22(4):563–71. doi: 10.1007/s10552-011-9728-5
17. Chandran U, Bandera EV, Williams-King MG, Sima C, Bayuga S, Pulick K, et al. Adherence to the Dietary Guidelines for Americans and Endometrial Cancer Risk. Cancer Causes Control (2010) 21(11):1895–904. doi: 10.1007/s10552-010-9617-3
18. Mai V, Kant AK, Flood A, Lacey JV Jr., Schairer C, Schatzkin A. Diet Quality and Subsequent Cancer Incidence and Mortality in a Prospective Cohort of Women. Int J Epidemiol (2005) 34(1):54–60. doi: 10.1093/ije/dyh388
19. Harnack L, Nicodemus K, Jacobs DR Jr., Folsom AR. An Evaluation of the Dietary Guidelines for Americans in Relation to Cancer Occurrence. Am J Clin Nutr (2002) 76(4):889–96. doi: 10.1093/ajcn/76.4.889
20. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: E xplanation and Elaboration. PloS Med (2009) 6(7):e1000100. doi: 10.1371/journal.pmed.1000100
21. Wells GA SB OCD PJ, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. (2020). Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (Accessed December).
22. Jayedi A, Soltani S, Zargar MS, Khan TA, Shab-Bidar S. Central Fatness and Risk of all Cause Mortality: Systematic Review and Dose-Response Meta-Analysis of 72 Prospective Cohort Studies. BMJ (2020) 370:m3324. doi: 10.1136/bmj.m3324
23. Luo D, Cheng Y, Zhang H, Ba M, Chen P, Li H, et al. Association Between high Blood Pressure and long Term Cardiovascular Events in Young Adults: Systematic Review and Meta-Analysis. BMJ (2020) 370:m3222. doi: 10.1136/bmj.m3222
24. Greenland S, Longnecker MP. Methods for Trend Estimation From Summarized Dose-Response Data, with Applications to Meta-Analysis. Am J Epidemiol (1992) 135(11):1301–9. doi: 10.1093/oxfordjournals.aje.a116237
25. Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, et al. Fruit and Vegetable Consumption And Mortality From all Causes, Cardiovascular Disease, and Cancer: Systematic Review And Dose-Response Meta-Analysis of Prospective Cohort Studies. BMJ (2014) 349:g4490. doi: 10.1136/bmj.g4490
26. Higgins JP, Thompson SG. Quantifying Heterogeneity in a Meta-Analysis. Stat Med (2002) 21(11):1539–58. doi: 10.1002/sim.1186
27. Al Ramadhani RM, Nagle CM, Ibiebele TI, Grant P, Friedlander M, DeFazio A, et al. Pre- and Post-Diagnosis Diet Quality and Ovarian Cancer Survival. Cancer Epidemiol Biomarkers Prev (2021) 30(1):229–32. doi: 10.1158/1055-9965.EPI-20-1036
28. Hansen JM, Nagle CM, Ibiebele TI, Grant PT, Obermair A, Friedlander ML, et al. A Healthy Lifestyle and Survival Among Women with Ovarian Cancer. Int J Cancer (2020) 147(12):3361–9. doi: 10.1002/ijc.33155
29. Karavasiloglou N, Pestoni G, Faeh D, Rohrmann S. Post-Diagnostic Diet Quality and Mortality in Females with Self-Reported History of Breast or Gynecological Cancers: Results from the Third National Health and Nutrition Examination Survey (NHANES III). Nutrients (2019) 11(11):2558. doi: 10.3390/nu11112558
30. Thomson CA, EC T, Wertheim BC, Neuhouser ML, Li W, Snetselaar LG, et al. Diet Quality and Survival After Ovarian Cancer: Results From the Women’s Health Initiative. J Natl Cancer Inst (2014) 106(11):dju314. doi: 10.1093/jnci/dju314
31. Dalvi TB, Canchola AJ, Horn-Ross PL. Dietary patterns, Mediterranean Diet, and Endometrial Cancer Risk. Cancer Causes Control (2007) 18(9):957–66. doi: 10.1007/s10552-007-9037-1
32. Gallus S, Bosetti C, La Vecchia C. Mediterranean Diet and Cancer Risk. Eur J Cancer Prev (2004) 13(5):447–52. doi: 10.1097/00008469-200410000-00013
33. Romaguera D, Vergnaud AC, Peeters PH, van Gils CH, Chan DS, Ferrari P, et al. Is concordance with World Cancer Research Fund/American Institute for Cancer Research Guidelines for Cancer Prevention Related to Subsequent Risk of Cancer? Results from the EPIC Study. Am J Clin Nutr (2012) 96(1):150–63. doi: 10.3945/ajcn.111.031674
34. Moran LJ, Grieger JA, Mishra GD, Teede HJ. The Association of a Mediterranean-Style Diet Pattern with Polycystic Ovary Syndrome Status in a Community Cohort Study. Nutrients (2015) 7(10):8553–64. doi: 10.3390/nu7105419
35. Yu D, Zhang X, Xiang YB, Yang G, Li H, Gao YT, et al. Adherence to Dietary Guidelines and Mortality: A Report From Prospective Cohort Studies of 134,000 Chinese Adults in Urban Shanghai. Am J Clin Nutr (2014) 100(2):693–700. doi: 10.3945/ajcn.113.079194
36. Milajerdi A, Namazi N, Larijani B, Azadbakht L. The Association of Dietary Quality Indices and Cancer Mortality: A Systematic Review and Meta-Analysis of Cohort Studies. Nutr Cancer (2018) 70(7):1091–105. doi: 10.1080/01635581.2018.1502331
37. Schwingshackl L, Schwedhelm C, Galbete C, Hoffmann G. Adherence to Mediterranean Diet and Risk of Cancer: An Updated Systematic Review and Meta-Analysis. Nutrients (2017) 9(10):1063. doi: 10.3390/nu9101063
38. Gil A, Ortega RM, Maldonado J. Wholegrain Cereals and Bread: A Duet of the Mediterranean Diet for the Prevention of Chronic Diseases. Public Health Nutr (2011) 14(12A):2316–22. doi: 10.1017/S1368980011002576
Keywords: diet quality, ovarian cancer, edometrial cancer, risk factors, epidemiological studies
Citation: Zhang Y-H, Li Z and Tan M-Z (2021) Association Between Diet Quality and Risk of Ovarian and Endometrial Cancers: A Systematic Review of Epidemiological Studies. Front. Oncol. 11:659183. doi: 10.3389/fonc.2021.659183
Received: 27 January 2021; Accepted: 04 March 2021;
Published: 18 May 2021.
Edited by:
Qi-Jun Wu, ShengJing Hospital of China Medical University, ChinaCopyright © 2021 Zhang, Li and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu-Hua Zhang, ZnVzYW4yMDIwQHNpbmEuY29t
 Yu-Hua Zhang
Yu-Hua Zhang Zhuo Li
Zhuo Li