- 1Department of Preventive Medicine, North Sichuan Medical College, Nanchong, China
- 2Applied Biostatistics Laboratory, University of Michigan School of Nursing, Ann Arbor, MI, United States
Background: The potential effects of excess weight status in childhood on later adult cardiometabolic risk factors have been undetermined in a Chinese population. Additionally, the potential mitigation of these effects if adult weight status returns to normalcy has been unresolved. Accordingly, we aimed to assess the association of childhood excess weight status and its long-term change with adult cardiometabolic risk factors.
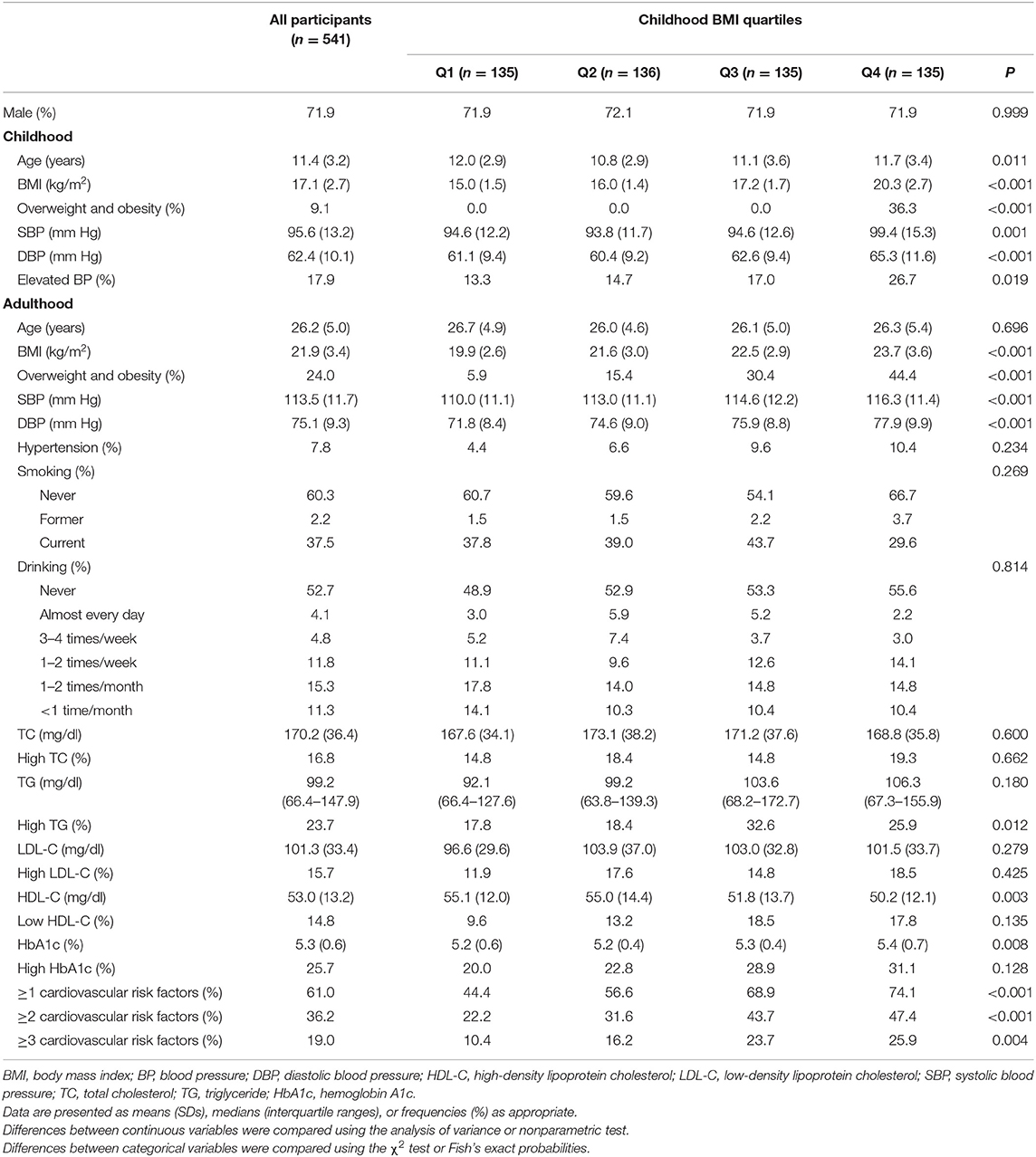
Methods: A cohort study from the China Health and Nutrition Survey 1991–2009 consisted of 541 participants who were measured in childhood (≥6 and <18 years) and underwent laboratory assessment in adulthood (≥18 years). In childhood, the participants were classified into four groups as age-sex-specific body mass index (BMI) z-score quartiles. The adult cardiometabolic risk factors included overweight and obesity, hypertension, high total cholesterol, high triglyceride, low high-density lipoprotein cholesterol, high low-density lipoprotein cholesterol, and high hemoglobin A1c.
Results: The prevalence was 61.0, 36.2, and 19.0% for ≥1, 2, and 3 cardiometabolic risk factors, respectively, with a mean 14.9-year follow-up. There was a significant trend in the progression of the number of adult cardiometabolic risk factors across childhood BMI quartiles (P < 0.001). Additionally, participants with childhood BMI z-scores ≥ 75th percentile and adult BMI z-scores < 75th percentile did not have increased cardiometabolic risks compared with those with both childhood and adulthood BMI z-scores < 75th percentile.
Conclusions: Our findings revealed that child excess weight status increased adult cardiometabolic risks. However, the effects of excess weight status in childhood on adult cardiometabolic risk factors were mitigated if adult weight status returned to normalcy.
Introduction
Cardiovascular disease (CVD) remains the leading cause of mortality across the globe (1). Cardiometabolic risk factors increase the risk of CVD, which results in a future burden of CVD (2). Controlling the epidemic of cardiometabolic risk factors has proven to be one effective strategy for the prevention of CVD.
Cardiometabolic risk factors tend to cluster and include excess weight status, high blood pressure, dyslipidemia, and hyperglycemia (3–5). Excess weight status causes inflammation and insulin resistance, which play a key role in the onset and clustering of cardiometabolic risk factors (6). Excess weight status is the easiest cardiometabolic risk factor to identify, and often is attained in early life (3–6).
The worldwide prevalence of childhood excess weight status has increased at an alarming rate in recent years (7). Observational studies have shown that children with excess weight status have an increased risk of cardiometabolic risk factors in adulthood (8, 9). Furthermore, evidence regarding the impact of the change in weight status from childhood to adulthood on health consequences has revealed that the adverse health consequences can be reversed if children with excess weight status attain normal weight as adults (10–13). However, few similar studies have been conducted in China. As industrialization and urbanization have accelerated and the population has aged, CVD has become a major public health challenge in China. Reliable information is essential for the development of national health policies for the prevention and control of CVD (14). Consequently, we aimed to assess the association of childhood weight status and its long-term change with cardiometabolic risk factors in early adulthood based on the China Health and Nutrition Survey (CHNS).
Materials and Methods
Study Population
Launched in 1989, the CHNS is an ongoing, open, and population-based longitudinal cohort study that is designed to examine health and nutrition status in the Chinese population (15). The survey sample was drawn with the use of a stratified multistage cluster method. As part of the CHNS, a follow-up survey is conducted every 2–4 years. Participants are asked to complete an interview questionnaire and a physical examination at each survey instance (15). Notably, fasting blood was collected for the first time in the 2009 survey (16, 17). The survey procedures used for the CHNS are described in detail elsewhere (15). This study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill, Institute of Nutrition and Food Safety, China Centers for Disease Control, and the China-Japan Friendship Hospital, Ministry of Health and China. All participants or their guardians provided written informed consent.
We established a cohort study from childhood (≥6 and <18 years) to adulthood (≥18 years) based on the CHNS. To ensure adequate follow-up length, individuals with a full record of key information (sex, age, blood pressure, weight, and height) on the first measurement during childhood, collected before the 2009 survey, were included in the present study. The follow-up survey was conducted among adult participants in the 2009 survey. In total, 660 participants were eligible. However, 119 participants did not undergo laboratory assessment in 2009. As a result, the cohort consisted of 541 individuals with a full record of key information during childhood before 2009, and had a full record of key information and had undergone laboratory assessment during adulthood in 2009.
General Examinations and Laboratory Assessment
Sex, age, and adult risk factors (smoking and alcohol consumption) were collected by self-administered questionnaire. Weight and height were measured by trained workers, respectively. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Blood pressure (BP) was measured using certified mercury sphygmomanometers. Three consecutive BP measurements were obtained, and the average of the latter two measurements was used for further analyses.
Fasting blood was collected in the 2009 survey. The methods of blood sample collection and preservation, the measurement procedures, the measurement equipment, and the test method are described in detail in several previous publications (16, 17). Total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and hemoglobin A1c (HbA1c) were measured.
Definitions
BMI was used to evaluate childhood weight status (18). Childhood overweight and obesity were defined as BMI ≥ corresponding sex- and age-specific overweight cutoffs presented in the national reference for Chinese children (19). Adulthood overweight and obesity were defined as BMI ≥ 24 kg/m2 (20). Childhood elevated BP was defined as BP ≥ 90th percentile for sex, age, and height or 120/80 mm Hg as per the BP reference for Chinese children (21, 22). Adulthood hypertension was defined as BP ≥ 140/90 mm Hg or taking anti-hypertension medications according to the 2018 Chinese Guidelines for Prevention and Treatment of Hypertension (21). Adulthood high TC was defined as TC ≥ 200 mg/dL, high TG as ≥150 mg/dL, high LDL-C as ≥130 mg/dL, and low HDL-C as <40 mg/dL in terms of the 2016 Chinese Guidelines for the Prevention and Treatment of Dyslipidemia in adults (23). High HbA1c was defined as ≥5.6% (16). The number of individual cardiovascular risk factors (overweight and obesity, hypertension, high TC, high TG, high LDL-C, low HDL-C, and high HbA1c) in adulthood was calculated to assess the cardiovascular risk profile.
Statistical Analysis
After adjusting for sex and age by regression residual analyses, childhood BMI was standardized using the Z-transformation (mean = 0, SD = 1). The participants were categorized into four groups as quartiles of childhood BMI z-scores. The data between groups were presented as means (SDs), medians (interquartile ranges), or frequencies (%) as appropriate. The differences between groups were tested using either analysis of variance, the chi-square test, Fish's exact probabilities, or the nonparametric test. Poisson models with robust standard errors were used to calculate relative risks (RRs) and 95% confidence intervals (CIs) with adjustment for covariates, and to investigate the relation of childhood weight status to cardiovascular risk factors in adulthood (24). The trend across the quartiles was tested using quartiles as a continuous ordinal variable.
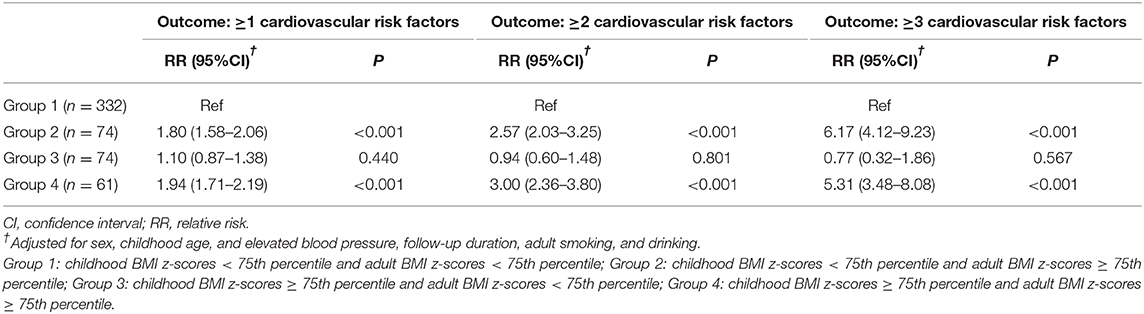
Individuals were classified into 4 groups based on combinations of childhood and adulthood weight status: childhood BMI z-scores < 75th percentile and adult BMI z-scores < 75th percentile (Group 1), childhood BMI z-scores < 75th percentile and adult BMI z-scores ≥ 75th percentile (Group 2), childhood BMI z-scores ≥ 75th percentile and adult BMI z-scores < 75th percentile (Group 3), childhood BMI z-scores ≥ 75th percentile and adult BMI z-scores ≥ 75th percentile (Group 4). Differences in the number of cardiovascular risk factors between groups were tested using the chi-square test. Covariate-adjusted Poisson models were used to assess the association between weight status change from childhood to adulthood and the number of cardiovascular risk factors in adulthood.
We used SAS 9.4 (SAS Institute Inc., Cary, NC, USA) to conduct the analyses and considered a two-tailed P < 0.05 to be statistically significant.
Results
The present study included 541 participants (males, 71.9%) from the CHNS 1991–2009. The participants' age ranged from 6 to 17 years (mean age, 11.4 years) in childhood and from 18 to 35 years (mean age, 26.2 years) in adulthood. The mean follow-up duration was 14.9 years (median, 16.0 years; range, 3–19 years).
Table 1 summarizes the characteristics of all participants. The prevalence of overweight and obesity in childhood and adulthood was 9.1 and 24.0%, respectively. Adult hypertension, high TC, high TG, high LDL-C, low HDL-C, and high HbA1c prevalences were 7.8, 16.8, 23.7, 15.7, 14.8, and 25.7%, respectively. 61.0, 36.2, and 19.0% of all individuals had ≥1, ≥2, and ≥3 cardiovascular risk factors in adulthood, respectively. Additionally, compared with individuals in the first quartile of childhood BMI, those in the fourth quartile tended to have more cardiovascular risk factors in adulthood.
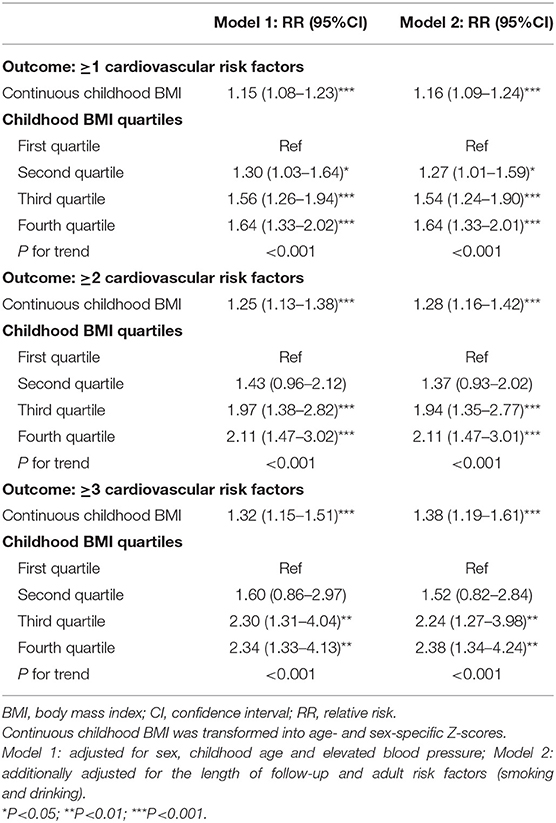
Table 2 presents the association between childhood BMI and adult cardiometabolic risk profile. Participants in the fourth quartile of childhood BMI had an increased risk of cardiovascular risk factors in comparison with those in the first quartile after adjusting for sex, childhood age, and elevated BP (Model 1). RR did not vary significantly after adjusting further for the follow-up duration, adult smoking, and drinking (Model 2). There was a significant trend in the progression of the number of adult cardiometabolic risk factors across the quartiles of childhood BMI in the fully adjusted model (P for trend <0.001).
Figure 1 describes the prevalence of cardiometabolic risk factors among the four groups as defined in the combinations of childhood and adulthood weight status. Interestingly, the difference in the prevalence of cardiometabolic risk factors between the participants with both child and adult BMI z-scores < 75th percentile and those with child BMI z-scores ≥ 75th percentile and adult BMI z-scores < 75th percentile was not significant (P > 0.05).
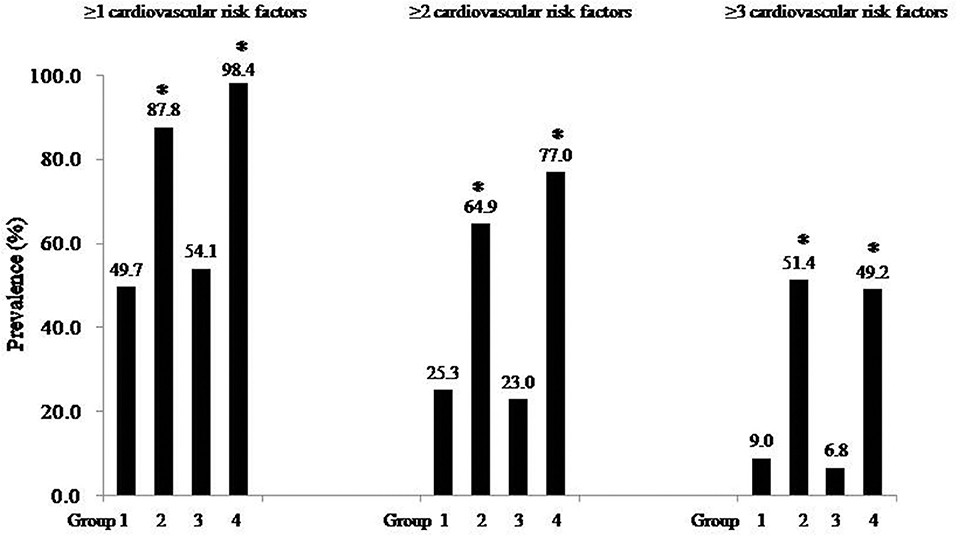
Figure 1. Prevalence of cardiometabolic risk factors among four groups. Group 1: childhood BMI z-scores < 75th percentile and adult BMI z-scores < 75th percentile; Group 2: childhood BMI z-scores < 75th percentile and adult BMI z-scores ≥ 75th percentile; Group 3: childhood BMI z-scores ≥ 75th percentile and adult BMI z-scores < 75th percentile; Group 4: childhood BMI z-scores ≥ 75th percentile and adult BMI z-scores ≥ 75th percentile. *P < 0.001 (Compared with group 1).
Table 3 shows the impact of weight status change from childhood to early adulthood on cardiometabolic risk factors. In comparison with the participants who had both child and adult BMI z-scores < 75th percentile, those with child BMI z-scores ≥ 75th percentile and adult BMI z-scores < 75th percentile had no increased risk of adult cardiometabolic risk factors (all Ps > 0.05).
We excluded 134 participants with child elevated BP or overweight (including obesity) to perform a sensitivity analysis. The sensitivity analysis results were similar (Tables S1, S2). In addition, we used the national reference for Chinese children and Asia adult reference (BMI ≥ 24 kg/m2) to define child and adult overweight (including obesity), respectively (19, 20). We performed a sensitivity analysis and obtained similar results (Table S3).
Discussion
We revealed that childhood excess weight status increased adult cardiometabolic risks based on a cohort study with a mean 14.9-year follow-up from the CHNS 1991–2009. Moreover, our results suggested that the effects of excess weight status in childhood on adult cardiometabolic risk factors were mitigated if adult weight status returned to normalcy. Our findings have important implications for the prevention and control of CVD in the Chinese population.
Child excess weight status increased the risk of early-onset and clustering of future cardiometabolic risk factors (10). Previous studies reported that the number of cardiometabolic risk factors increased with the extent of childhood excess weight status (8). Our results were consistent with the previous findings, indicating that childhood excess weight status was an important determinant in the development of cardiometabolic risk factors. In addition, several prospective cohort studies began in childhood presented BMI trajectory and incremental area under the growth curve to obtain similar findings (25, 26). Moreover, childhood excess weight status predicted significantly future CVD and both cardiovascular and all-cause mortality across the life span (9, 27–29).
Maintaining an ideal weight in early life is an effective means for the prevention and control of future CVD. The International Childhood Cardiovascular Cohort (i3C) Consortium pooled data from four prospective cohort studies in the Western population, and revealed that children with excess weight status who achieved an ideal weight in adulthood did not have an increased risk of cardiovascular risk factors (10). Moreover, ample evidence demonstrated that the effect of childhood adiposity on cardiometabolic profile was mediated by current BMI (11–13). Consistent with previous publications, the present study showed that the long-term adverse effects of childhood excess weight status can be reversed if weight status returned to normalcy in adulthood in the Chinese population. Our findings were also supported by existing evidence from the Chinese population, which showed that a decrease in excess weight status from childhood to adulthood was related to significant reductions in the risks of hypertension, metabolic syndrome, nonalcoholic fatty liver disease, subclinical atherosclerosis, arterial stiffness, and left ventricular hypertrophy (30–33).
There were several limitations in our study. First, data regarding blood glucose and lipid levels in childhood were not collected, which may affect our results. However, the sensitivity analysis results did not vary significantly after excluding 134 participants with childhood elevated BP or overweight (including obesity). In addition, pediatric overweight and obesity were equivalent to metabolic syndrome in terms of the power to predict adult adverse health consequence (9). Second, this observational study was not able to assess the causality between weight status change from childhood to adulthood and cardiometabolic risk factors. Third, 18% (119/660) of participants were lost to follow-up. However, no significant difference in childhood characteristics, except systolic BP, was observed between those who were included in the present study and those who were lost to follow-up (Table S4). Fourth, the sample size was insufficient to perform stratification analysis. Fifth, the number of female participants was small, which may affect our findings.
In conclusion, the current study demonstrated that childhood excess weight status is positively associated with adult cardiometabolic risk factors. Given that China is facing an excess weight epidemic in childhood (34), our results underscore the importance for weight management in early life in regard to the prevention and control of adult cardiometabolic risk factors and CVD.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation, to any qualified researcher.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board at the University of North Carolina at Chapel Hill, Institute of Nutrition and Food Safety, China Centers for Disease Control and the China-Japan Friendship Hospital, Ministry of Health and China. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
HF conceptualized and designed the study, carried out the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript. QZ and XZ critically reviewed and revised the manuscript. All authors approved the final manuscript for submission.
Funding
This study was supported by the PhD Funding Program of North Sichuan Medical College (CBY18-QD02) and the Key Subject Development Program of North Sichuan Medical College (NSMC-M-18-19), and the 2018-2020 MCUBE 3.0 Program from the University of Michigan.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the National Institute for Nutrition and Health, China Center for Disease Control and Prevention, Carolina Population Center (P2C HD050924, T32 HD007168), the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350, R24 HD050924, and R01-HD38700), and the NIH Fogarty International Center (D43 TW009077, D43 TW007709) for financial support for the CHNS data collection and analysis files.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2020.00301/full#supplementary-material
Abbreviations
BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; DBP, diastolic blood pressure; HbA1c, hemoglobin A1c; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol; TG, triglycerides.
References
1. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
2. GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1923–94. doi: 10.1016/S0140-6736(18)32225-6
3. Tanrikulu MA, Agirbasli M, Berenson G. Primordial prevention of cardiometabolic risk in childhood. Adv Exp Med Biol. (2017) 956:489–96. doi: 10.1007/5584_2016_172
4. Turer CB, Brady TM, de Ferranti SD. Obesity, hypertension, and dyslipidemia in childhood are key modifiable antecedents of adult cardiovascular disease: a call to action. Circulation. (2018) 137:1256–59. doi: 10.1161/CIRCULATIONAHA.118.032531
5. Camhi SM, Katzmarzyk PT. Tracking of cardiometabolic risk factor clustering from childhood to adulthood. Int J Pediatr Obes. (2010) 5:122–9. doi: 10.3109/17477160903111763
6. Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, et al. Pediatric obesity-assessment, treatment, and prevention: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. (2017) 102:709–57. doi: 10.1210/jc.2017-00561
7. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2014) 384:766–81. doi: 10.1016/S0140-6736(14)60460-8
8. Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. (2015) 373:1307–17. doi: 10.1056/NEJMoa1502821
9. Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR, et al. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation. (2010) 122:1604–11. doi: 10.1161/CIRCULATIONAHA.110.940809
10. Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. (2011) 365:1876–85. doi: 10.1056/NEJMoa1010112
11. Magnussen CG, Koskinen J, Juonala M, Chen W, Srinivasan SR, Sabin MA, et al. A diagnosis of the metabolic syndrome in youth that resolves by adult life is associated with a normalization of high carotid intima-media thickness and type 2 diabetes mellitus risk: the Bogalusa heart and cardiovascular risk in young Finns studies. J Am Coll Cardiol. (2012) 60:1631–39. doi: 10.1016/j.jacc.2012.05.056
12. Araújo J, Severo M, Barros H, Mishra GD, Guimarães JT, Ramos E. Developmental trajectories of adiposity from birth until early adulthood and association with cardiometabolic risk factors. Int J Obes. (2015) 39:1443–9. doi: 10.1038/ijo.2015.128
13. Parker ED, Sinaiko AR, Kharbanda EO, Margolis KL, Daley MF, Trower NK, et al. Change in weight status and development of hypertension. Pediatrics. (2016) 137:e20151662. doi: 10.1542/peds.2015-1662
14. Agirbasli M, Tanrikulu AM, Berenson GS. Metabolic syndrome: bridging the gap from childhood to adulthood. Cardiovasc Ther. (2016) 34:30–6. doi: 10.1111/1755-5922.12165
15. Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: The China Health and Nutrition Survey—monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol. (2010) 39:1435–40. doi: 10.1093/ije/dyp322
16. Adair LS, Gordon-Larsen P, Du SF, Zhang B, Popkin BM. The emergence of cardiometabolic disease risk in Chinese children and adults: consequences of changes in diet, physical activity and obesity. Obes Rev. (2014) 15 (Suppl. 1):49–59. doi: 10.1111/obr.12123
17. Yan S, Li J, Li S, Zhang B, Du S, Gordon-Larsen P, et al. The expanding burden of cardiometabolic risk in China: the China Health and Nutrition Survey. Obes Rev. (2012) 13:810–21. doi: 10.1111/j.1467-789X.2012.01016.x
18. Fan H, Zhu Q, Medrano-Gracia P, Zhang X. Comparison of child adiposity indices in prediction of hypertension in early adulthood. J Clin Hypertens. (2019) 21:1858–62. doi: 10.1111/jch.13734
19. National Health Commission of the People's Republic of China. Data From: Screening for Overweight and Obesity Among School-Age Children and Adolescents. (2018). Available online at:http://www.nhc.gov.cn/ewebeditor/uploadfile/2018/03/20180329094554367.pdf (accessed October 1, 2019).
20. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363:157–63. doi: 10.1016/S0140-6736(03)15268-3
21. Joint Committee for Guideline Revision. 2018 Chinese Guidelines for prevention and treatment of hypertension-A report of the Revision Committee of Chinese Guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. (2019) 16:182–241. doi: 10.11909/j.issn.1671-5411.2019.03.014
22. Fan H, Hou D, Liu J, Yan Y, Mi J. Performance of 4 definitions of childhood elevated blood pressure in predicting subclinical cardiovascular outcomes in adulthood. J Clin Hypertens. (2018) 20:508–14. doi: 10.1111/jch.13201
23. Joint Committee for Guideline Revision. 2016 Chinese Guidelines for prevention and treatment of adult dyslipidemia. Chin Circ J. (2016) 33:937–50. doi: 10.3969/j.issn.1000-3614.2016.10.001
24. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. (2004) 159:702–6 doi: 10.1093/aje/kwh090
25. Berentzen NE, van Rossem L, Gehring U, Koppelman GH, Postma DS, de Jongste JC, et al. Overweight patterns throughout childhood and cardiometabolic markers in early adolescence. Int J Obes. (2016) 40:58–64. doi: 10.1038/ijo.2015.196
26. Chen W, Srinivasan SR, Li S, Xu J, Berenson GS. Clustering of long-term trends in metabolic syndrome variables from childhood to adulthood in Blacks and Whites: the Bogalusa Heart Study. Am J Epidemiol. (2007) 166:527–33. doi: 10.1093/aje/kwm105
27. Baker JL, Olsen LW, Sørensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. (2007) 357:2329–37. doi: 10.1056/NEJMoa072515
28. Twig G, Yaniv G, Levine H, Leiba A, Goldberger N, Derazne E, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med. (2016) 374:2430–40. doi: 10.1056/NEJMoa1503840
29. Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. (2010) 362:485–93. doi: 10.1056/NEJMoa0904130
30. Liang Y, Hou D, Zhao X, Wang L, Hu Y, Liu J, et al. Childhood obesity affects adult metabolic syndrome and diabetes. Endocrine. (2015) 50:87–92. doi: 10.1007/s12020-015-0560-7
31. Yan Y, Hou D, Zhao X, Liu J, Cheng H, Wang Y, et al. Childhood adiposity and nonalcoholic fatty liver disease in adulthood. Pediatrics. (2017) 139:e20162738. doi: 10.1542/peds.2016-2738
32. Hou Y, Wang M, Yang L, Zhao M, Yan Y, Xi B. Weight status change from childhood to early adulthood and the risk of adult hypertension. J Hypertens. (2019) 37:1239–43. doi: 10.1097/HJH.0000000000002016
33. Yan Y, Hou D, Liang Y, Zhao X, Hu Y, Liu J, et al. Tracking body mass index from childhood to adulthood for subclinical cardiovascular diseases at adulthood. J Am Coll Cardiol. (2016) 67:1006–7. doi: 10.1016/j.jacc.2015.12.013
Keywords: weight status, cardiometabolic risk factors, childhood, adulthood, cohort
Citation: Fan H, Zhu Q and Zhang X (2020) Child Excess Weight Status, Adult Excess Weight Status, and Cardiometabolic Risk Profile. Front. Pediatr. 8:301. doi: 10.3389/fped.2020.00301
Received: 08 December 2019; Accepted: 11 May 2020;
Published: 09 June 2020.
Edited by:
Oswin Grollmuss, Université Paris-Sud, FranceReviewed by:
Shengxu Li, Tulane University, United StatesDimpna Calila Albert-Brotons, King Faisal Specialist Hospital & Research Centre, Saudi Arabia
Copyright © 2020 Fan, Zhu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Fan, MTU3NzM3MTM5OUBxcS5jb20=; Xingyu Zhang, emhhbmd4eXVAbWVkLnVtaWNoLmVkdQ==
 Hui Fan
Hui Fan Qi Zhu
Qi Zhu Xingyu Zhang
Xingyu Zhang