- 1Department of Pediatrics, NYU Long Island School of Medicine, Mineola, NY, United States
- 2Department of Community Health and Social Medicine, The City University of New York (CUNY) School of Medicine, New York, NY, United States
Objective: The aim of this study was to examine the prevalence of bandemia in confirmed respiratory viral infections in febrile infants and children presenting to the emergency department.
Methods: An observational retrospective study from January 1, 2016, through December 31, 2016, was conducted in patients between the ages of ≥ 1 month and ≤ 5 years presenting to the emergency room with fever and who had a complete blood cell count performed. Patients were separated into seven groups based on the type of respiratory viral infection. Inclusion criteria strictly counted children with viral infections and absence of clinical and laboratory evidence of a bacterial coinfection.
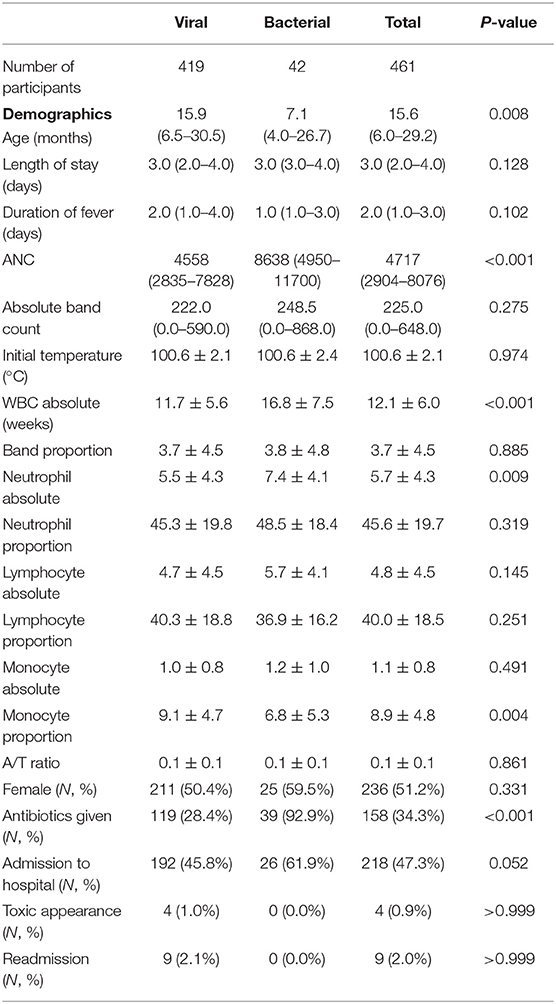
Results: A total of 419 patients had a documented viral infection. A significant proportion of these children were found to have bandemia; children with adenovirus (17%), respiratory syncytial virus (RSV) (14.9%), human metapneumovirus (hMPV) (13%), and parainfluenza virus (7.9%) had the highest prevalence when the cutoff for bandemia was set at 10%. The prevalence increased to 35.3, 30.9, 40.3, and 15.8% for adenovirus, RSV, hMPV, and parainfluenza virus, respectively, when this cutoff was lowered further to 5%.
Conclusion: Band neutrophils are detected frequently in confirmed respiratory viral infections particularly during early stages.
Introduction
Respiratory viral infections, either confirmed or presumed, account for the majority of febrile illnesses in healthy infants and young children (1, 2). Common viral presentations include fever with upper respiratory signs and symptoms, clinical bronchiolitis, or fever without localizing signs (3). The diagnosis of a viral infection is mainly based on clinical grounds. The multiplex molecular respiratory panel (respiratory PCR assay) has enabled better identification of these respiratory viral infections and provides objective data. Many of these children would get non-specific laboratory markers performed, i.e., complete blood count (CBC), C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) to investigate a concomitant bacterial infection (4). Since the 1990's, there have been multiple studies and guidelines on the management of febrile infants, which indicated a low, but non-negligible, risk of serious bacterial infections (5–7). Infants > 1 month of age who present to the emergency room (ER) often get a CBC as part of the workup. This study sought to investigate the prevalence of bandemia in a cohort of children with confirmed viral infection.
Methods
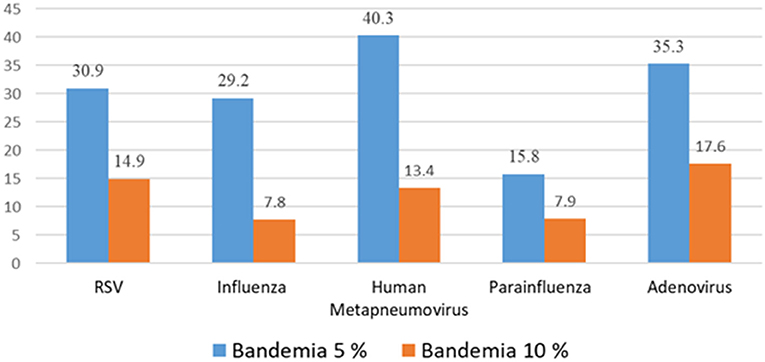
We conducted a retrospective study from January 1, 2016, through December 31, 2016, in children between the ages of ≥ 1 month and ≤ 5 years. These children presented to our Children's Medical Center, which is a suburban, tertiary-care academic hospital in the Northeast United States with 95 pediatric inpatient beds and 19,000 pediatric ED visits per year. They presented with documented fevers defined as a temperature of 100.4° Fahrenheit (38° C) or greater and had a complete blood cell count performed using Beckman Coulter ® LH 780 electric cell counter. A manual differential count of the peripheral blood smear was performed on every patient, which is standard protocol in patients 5 years or younger in our institution (Figure 3). Febrile children with confirmed viral infections (BioFire FilmArray® multiplex PCR) were included in the study. We excluded patients with chronic conditions (sickle cell disease, malignancy, and inflammatory bowel disease), immunodeficiencies, patients with diagnosed bacterial infections, and toxic appearing children as documented by attending physicians. We also excluded children with documented signs of acute otitis media because it is difficult to distinguish between viral or bacterial etiology. Cases where the chest x-ray was read as focal infiltrates due to atelectasis by the attending radiologists were included in the viral infection group and cases with chest x-ray findings of consolidation, effusion, or empyema were excluded to ensure that patients did not have a bacterial coinfection.
Cases with confirmed viral infections had nasopharyngeal specimens obtained and tested positive for Respiratory syncytial virus (RSV), adenovirus, influenza, parainfluenza, and human metapneumovirus (hMPV) on the Filmarray® multiplex PCR system. We excluded enterovirus and rhinovirus because of difficulty in distinguishing symptomatic infections from asymptomatic prolonged shedding. Also, results are reported together as enterovirus/rhinovirus (both are picornavirus) and it is difficult to determine which virus is the culprit. We also excluded coronavirus (non-SARS or MERS) as a majority of the cases were either asymptomatic or had mild upper respiratory symptoms.
In addition we collected data on a small sample of patients who presented to the ER with fever and were diagnosed with a bacterial infection, such as bacteremia, meningitis, bacterial gastroenteritis, and urinary tract infection (UTI). Bacteremia was defined as a positive blood culture (excluding contaminants: bacillus species [non-anthrax and non-cereus] coagulase negative staphylococcus or corynebacterium sp.). Meningitis was confirmed with positive CSF culture and enteritis with stool culture growth of a bacterial pathogen. Cases of urinary tract infection were diagnosed based on pyuria (>5 WBC on automated urinalysis) and >50,000 CFU of a single uropathogen.
The study was approved by the Institutional Review Board.
Statistical Analysis
Continuous variables, assumed to be normal, were analyzed using two-sample t-test and summarized using mean ± standard deviation. Continuous variables with skewed distribution were analyzed using the Wilcoxon rank-sum test and summarized using median and interquartile range. Categorical variables were summarized using frequency and percent, and analyzed using the Pearson's chi-square test of independence. When the asymptotic assumption of the chi-square distribution was violated, an exact chi-square p-value was computed. All analyses were done using SAS 9.4®, and p-value < 0.05 were considered significant for all analyses except for the planned comparisons within the viral group where significance was set at 0.025 after Bonferroni correction.
Results
A total of 419 pediatric patients were included in the study (Figure 1). They all had documented viral infections with no evidence of bacterial coinfection: adenovirus (54), parainfluenza (114), influenza (77), hMPV (68), and RSV (175). Forty five of the cases were combination of the above.
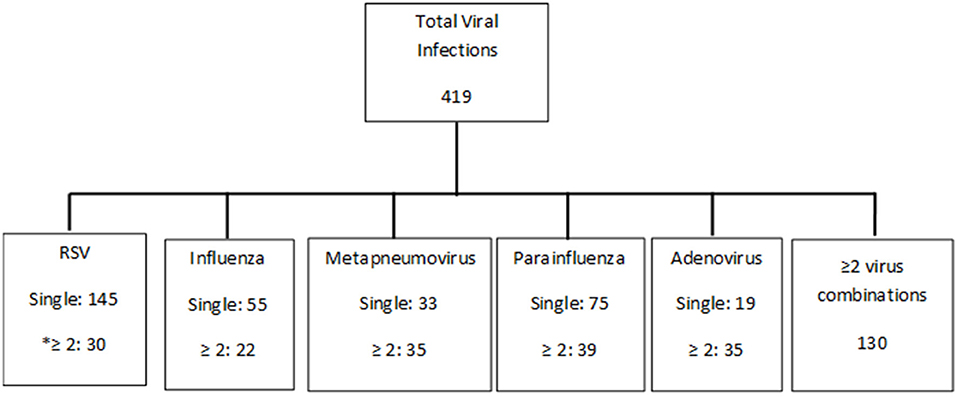
Figure 1. Breakdown of viruses. *≥2 includes of combinations of viruses (most common combination was with enterovirus, rhinovirus, and coronavirus addition to be a combination of the above five viruses).
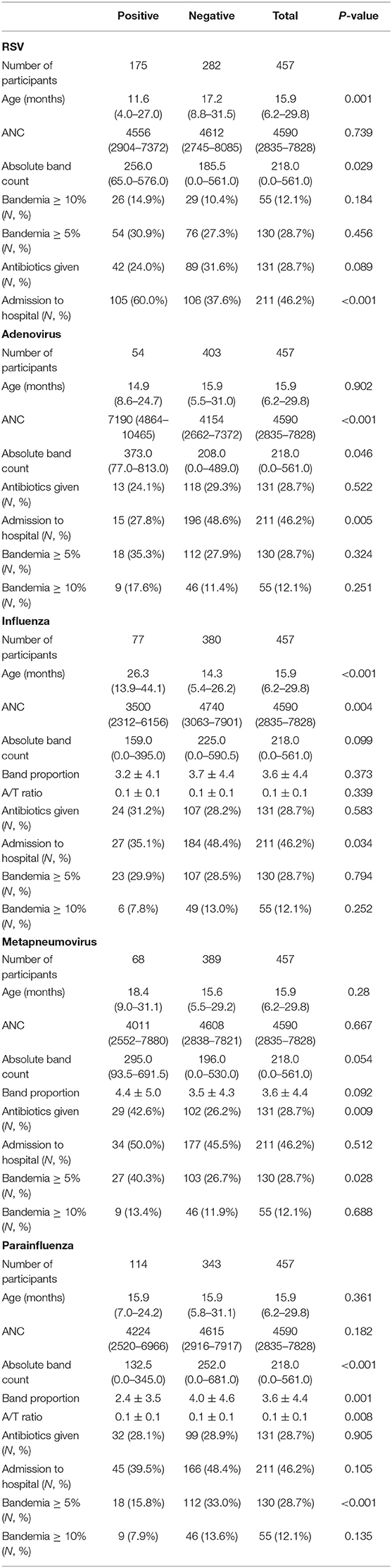
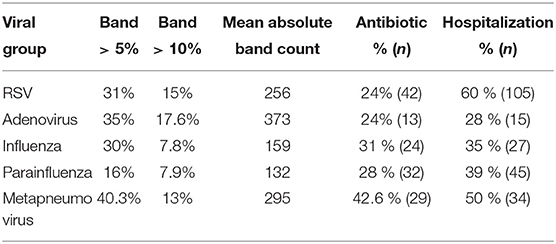
Viral Group With Band ≥ 10% (Table 1)
In the viral group, patients with band proportions ≥10% had a significantly higher mean absolute neutrophil count (ANC), mean temperature, exposure to antibiotics, and rate of admission than their viral counterpart with band proportions <10%. Furthermore, these patients had significantly lower mean lymphocyte counts and lower mean lymphocyte proportions.
RSV Patients With Band ≥ 10% (Table 2)
Patients who were positive for RSV were significantly younger, had lower body temperature, were less likely to receive antibiotics, and were more likely to be admitted to the hospital than those negative for RSV.
Adenovirus Patients With Band ≥ 10%
Patients who were positive for adenovirus had higher ANC, body temperature, WBC, absolute neutrophil counts, and absolute monocyte counts. In addition, they were less likely to be admitted to the hospital than patients negative for adenovirus.
Parainfluenza Patients With Band ≥ 10%
Patients who were positive for parainfluenza virus had lower rates of admission to the hospital, and lower rate of patients with bandemia ≥ 10% when compared to patients negative for parainfluenza. Of note, these patients had higher lymphocyte proportions.
Influenza Patients With Band ≥ 10%
Patients who were positive for influenza were older and had lower WBC, absolute lymphocyte counts, and absolute monocyte counts than patients negative for influenza.
Metapneumovirus Patients With Band ≥ 10%
Patients who were positive for hMPV had higher band proportions and exposure to antibiotics when compared to patients negative for hMPV.
Combination Group With Band ≥ 10%
Patients who were positive for 2 or more viruses had higher ANC, temperature, and WBC but had shorter length of stay in the hospital when compared to those positive with only one virus.
Bacterial vs. Viral Group
In our sample of 42 patients diagnosed with bacterial infections, there were urinary tract infections (36), Streptococcus pneumonia meningitis (2), bacteremia Escherichia coli (2), and Shigella enteritis (2).
We compared characteristics between the bacterial group and the viral group. Patients with a bacterial infection were significantly younger than patients with a viral infection. Patients with a bacterial infection had significantly higher mean ANC, mean WBC, mean neutrophil count, and higher exposure to antibiotics than their viral counterparts (Table 3). When comparing the absolute band count and band proportion between the viral group and the bacterial group, there was no statistically significant difference. When comparing the WBC and ANC between the viral group and the bacterial group, the bacterial group had a higher WBC and ANC which was significant (p <0.001).
Discussion
Bandemia or elevated immature neutrophil count (left shift) was detected in a cohort of febrile children presenting to the emergency department with confirmed respiratory viral infection without a concomitant bacterial infection. In our study, a significant proportion of these children were found to have bandemia. Adenovirus (17%), RSV (14.9%), human metapneumovirus (13%), and parainfluenza (7.9%) had the highest prevalence when the cutoff for bandemia was set at 10%. The prevalence increased to 35.3, 30.9, 40.3, and 15.8% for adenovirus, RSV, hMPV, and PIV, respectively when this cutoff was lowered further to 5%, which is the cutoff used by our institution (Figure 2).
Over the past decade, use of multiplex molecular respiratory panel has enabled better identification of respiratory viral infections. As a result, this information has allowed us to investigate the differential white blood cell count in common childhood viral infections (8). We reviewed the different cell lines, including immature neutrophils (bands), lymphocytes, and monocytes. We found that adenovirus had significantly (p <0.001) higher ANC when compared to the other viruses with a mean value of 7,190.
Although identification of bandemia may represent a serious underlying bacterial infection (SBI) (9, 10) immature neutrophils are also associated with certain viral infections (11). Of note, in our study, we found viral cases with band proportions >10% which had significantly higher exposure to antibiotics and hospital admission rates (p <0.001). The study results suggest that the traditional belief of bandemia and its association with SBI may persist in clinical practice.
What is bandemia? WBC is a component of the CBC. The WBC's differential measures the absolute number and proportion of granulocytes, lymphocytes, monocytes, basophils, and eosinophils (12). A neutrophil is a mature granulocyte and part of the innate immune system. Band is the most “mature” of the immature stages in the development of a neutrophil (Figure 3). In older children and adults, the normal blood circulation has 3–5% of bands which will mature into neutrophils in the circulation. However, the majority of blasts undergo maturation in the marrow storage compartment. Any stress, whether an infection, inflammation, or a hypermetabolic state will lead to an increase in band count or bandemia (>10%) (13–15).
In our study, all differentials were performed manually. Manual band count requires the additional time-consuming, labor-intensive process of slide preparation and manual leukocyte tabulation. The interpretation is technician dependent, and its enumeration is associated with inaccuracy and imprecision. In addition, there exists a wide variation in reference ranges of bandemia (16). It has been reported in the literature that the percentage and absolute band count in healthy children between the ages of 15 days and 2 years of age is similar, but the response to infection may be different in young children of different ages (16).
What does presence of bandemia in viral infections mean? Bandemia has been reported in children with viral infections notably with lower respiratory tract infections, enteroviral infections, and rotavirus infections (6, 11, 17). Bandemia has also been reported in association with influenza and RSV infections (18).
We found bandemia (>10%) in about a quarter of cases of respiratory viral infections in the absence of concomitant bacterial infection (confirmed or presumed): RSV (14.9% 26/175), adenovirus (17.6% 9/54), hMPV (13.4% 9/68), influenza (7.8% 6/77), and parainfluenza virus (7.9% 9/114). The cutoff for bandemia in our laboratory is 5% which further increases the percentage of children classified with bandemia. This implies that a relatively higher band count is seen in viral infections that primarily cause lower respiratory tract disease and are associated with more parenchymal inflammation at the time of ER presentation. In addition, our study is the first to report the prevalence of bandemia in hMPV infections.
In reviewing our data we noticed that patients admitted with a known viral infection, but high band count, were likely to receive antibiotics. Antibiotic exposure was seen in one quarter of the patients infected with hMPV (40.3%), followed by influenza (31%), parainfluenza (28%), RSV (24%), and adenovirus (17.6%). This lower antibiotic use in adenovirus can be attributed to the known association of bandemia in adenovirus by clinicians (Table 4).
We compared the bacterial group with the viral group and did not find a statistically significant difference in bandemia when comparing viral with bacterial infections in infants and young children. However, the bacterial group was a considerably smaller sample size so when comparing the groups, the results should be taken cautiously. Nevertheless, when comparing the absolute band count, band proportion, and A/T ratio between the viral group and the bacterial group, there was no statistical significant difference.
This study has several limitations. First, it is a retrospective review conducted in a single center. Second, there were fewer patients in the bacterial group in comparison to the viral group; therefore, the incidence of true bandemia in the bacterial group might be under represented. In addition, we included only well-appearing children with confirmed viral infections, thus we cannot generalize our results to ill appearing patients.
Conclusions
Elevated band counts are seen in lower respiratory viral infections and clinicians should be aware of this association. While absolute neutrophil count and white blood cell count are reliable markers of bacterial infection, bandemia may also be present in viral infections. This is the first study comparing bandemia among different viral infections. We observed an elevated band count in many viral infections, specifically RSV, adenovirus, hMPV, influenza, and parainfluenza. Bandemia in well-appearing children with confirmed viral infections can be an area of opportunity to limit the use of antibiotics.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by NYU Long Island School of Medicine IRB Department. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
EN, AN, and RR was involved in manuscript writing and data collection of viral infections. JC was involved in data collection of bacterial infections. RC performed statistical analysis. NS was involved in manuscript writing, and LK supervised the project and was involved in revision of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
Clinical research grants were paid to LK's institution, NYU Long Island School of Medicine, by AstraZeneca (Medimmune), Regeneron, and Sanofi Pasteur. These three companies had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2020.576676/full#supplementary-material
Abbreviations
CBC, complete blood count; WBC, white blood cell count; ANC, absolute neutrophil count; RSV, Respiratory syncytial virus; hMPV, human metapneumovirus; ER, emergency room; SBI, serious bacterial infection; PCR, polymerase chain reaction.
References
1. Byington CL, Enriquez FR, Hoff C, Tuohy R, Taggart EW, Hillyard DR, et al. Serious bacterial infections in febrile infants 1 to 90 days old with and without viral infections. Pediatrics. (2004) 113:1662. doi: 10.1542/peds.113.6.1662
2. Hall CB, Weinberg GA, Iwane MK, Blumkin AK, Edwards KM, Staat MA, et al. The burden of RSV infection in young children. N Engl J Med. (2009) 360:588–98. doi: 10.1056/NEJMoa0804877
3. Colvin JM, Muenzer JT, Jaffe DM, et al. Detection of viruses in young children with fever without an apparent source. Pediatrics. (2012) 130:e1455–62. doi: 10.1542/peds.2012-1391
4. Librizzi J, McCulloh R, Koehn K, Alverson B. Appropriateness of testing for serious bacterial infection in children hospitalized with bronchiolitis. Hosp Pediatr. (2014) 4:33–8. doi: 10.1542/hpeds.2013-0073
5. Baker MD, Bell LM, Avner JR. Outpatient management without antibiotics of fever in selected infants. N Engl J Med. (1993) 329:1437–41. doi: 10.1056/NEJM199311113292001
6. Blaschke AJ, Korgenski EK, Wilkes J, Presson AP, Thorell EA, Pavia AT, et al. Rhinovirus in febrile infants and risk of bacterial infection. Pediatrics. (2018) 141:e20172384. doi: 10.1542/peds.2017-2384
7. Baraff LJ, Oslund SA, Schriger DL, Stephen ML. Probability of bacterial infections in febrile infants less than three months of age: a meta-analysis. Pediatr Infect Dis J. (1992) 11:257–64. doi: 10.1097/00006454-199204000-00001
8. Echavarría M, Marcone DN, Querci M, Seoane A, Ypas M, Videla C, et al. Clinical impact of rapid molecular detection of respiratory pathogens in patients with acute respiratory infection. J Clin Virol. (2018) 108:90–5. doi: 10.1016/j.jcv.2018.09.009
9. Hornik CP, Benjamin DK, Becker KC, Benjamin DK Jr, Li J, Clark RH, et al. Use of the complete blood cell count in early-onset neonatal sepsis. Pediatr Infect Dis J. (2012) 31:799–802. doi: 10.1097/INF.0b013e318256905c
10. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee. American college of chest physicians/society of critical care medicine. Chest. (1992) 101:1644–55. doi: 10.1378/chest.101.6.1644
11. Kuppermann N, Walton EA. Immature neutrophils in the blood smears of young febrile children. Arch Pediatr Adolesc Med. (1999) 153:261–6. doi: 10.1001/archpedi.153.3.261
12. Sacher RA, McPherson RA, Campos JM, Widmann FK. Widmann's Clinical Interpretation of Laboratory Tests. 11th ed. Philadelphia, PA: Davis (2000).
13. Morens DM. WBC count and differential. AJDC. (1979) 133:25–27. doi: 10.1001/archpedi.1979.02130010031003
14. Baines KJ, Simpson JL, Gibson PG. Biology of neutrophils. Middletons Allergy Princ. Pract. 17:280–291. doi: 10.1016/B978-0-323-08593-9.00018-8
15. Mare TA, Treacher DF, Shankar-Hari M, Beale R, Lewis SM, Chambers DJ, et al. The diagnostic and prognostic significance of monitoring blood levels of immature neutrophils in patients with systemic inflammation. Crit Care. (2015) 19:57. doi: 10.1186/s13054-015-0778-z
16. Joanne Cornbleet P. Clinical utility of the band count. Clin Lab Med. (2002) 22:1. doi: 10.1016/S0272-2712(03)00069-6
17. Portnoy B, Hanes B, Salvatore MA, Eckert HL. The peripheral white blood count in respirovirus infection. J Peditrics. (1966) 68:181–8. doi: 10.1016/S0022-3476(66)80148-8
Keywords: bandemia, respiratory viral infections, fever, complete blood cell (CBC) count, absolute neutrophil count (ANC), absolute band count, film array
Citation: Noyola E, Noor A, Sweeney N, Chan J, Ramesh R, Calixte R and Krilov LR (2020) Prevalence of Bandemia in Respiratory Viral Infections: A Pediatric Emergency Room Experience. Front. Pediatr. 8:576676. doi: 10.3389/fped.2020.576676
Received: 26 June 2020; Accepted: 16 November 2020;
Published: 29 December 2020.
Edited by:
Cristiana Nascimento-Carvalho, Federal University of Bahia, BrazilReviewed by:
Eitan Naaman Berezin, Santa Casa of São Paulo, BrazilWilliam Curtis, Assistance Publique Hopitaux De Paris, France
Copyright © 2020 Noyola, Noor, Sweeney, Chan, Ramesh, Calixte and Krilov. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Asif Noor, YXNpZi5ub29yQG55dWxhbmdvbmUub3Jn
 Estela Noyola
Estela Noyola Asif Noor
Asif Noor Nicole Sweeney1
Nicole Sweeney1 Joshua Chan
Joshua Chan Rose Calixte
Rose Calixte Leonard R. Krilov
Leonard R. Krilov