- 1Department of Integrative Cardiology, China-Japan Friendship Hospital, Beijing, China
- 2Department of Pediatrics, Beijing Fangshan District Liangxiang Hospital, Beijing, China
- 3Department of Pediatrics, Guang’ Anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China
Aim: To assess the individual effects of overweight/obesity and tobacco exposure, and their combined effects on hypertension in children.
Methods: This cross-sectional study included 6,339 children aged 6–17 years from National Health and Nutrition Examination Surveys 1999–2018. Participants’ height, weight and blood pressure (BP) were measured by trained technicians. Hypertension was defined as: mean systolic BP (SBP) and/or diastolic BP (DBP) ≥ 90th percentile for sex, age, and height (for children aged 1–13 years), and SBP ≥120 mmHg and/or a DBP ≥80 mmHg (for adolescents aged 13–17 years); or self-reported having been diagnosed with hypertension or taking antihypertensive medication. Gender- and age-specific body mass index (BMI) cut-points were used to define overweight/obesity: “overweight” was defined as a BMI > 1 standard deviation (SD); “obesity” was defined as BMI > 2SD; and “thinness” was defined as BMI < −2SD. Tobacco exposure was defined as having serum cotinine levels >0.05 µg/L or reporting the presence of at least one smoker in the household. Weighted univariate and multivariate logistic regression models were used to assess overweight/obesity and tobacco exposure with the odds of hypertension, and the combined effects of overweight/ obesity and tobacco exposure on hypertension, followed by strata-specific analyses. Odds ratios (OR) with 95% confidence intervals (CI) were calculated.
Results: The prevalence of overweight/obesity and tobacco exposure was significantly higher in the hypertension group than in the non-hypertension group. Overweight/obesity (OR = 1.67, 95%CI: 1.26–2.21/ OR = 2.38, 95%CI: 1.67–3.39) and tobacco exposure (OR = 1.58, 95%CI: 1.16–2.14) were associated with a higher odd of hypertension in children, respectively. Additionally, we also observed the combined effect between overweight (OR = 3.05, 95%CI: 1.96–4.75)/obesity (OR = 3.68, 95%CI: 2.24–6.03) and tobacco exposure were related to hypertension odds in children, with a significant effect in different populations.
Conclusion: There may exist joint effect of overweight/obesity and tobacco exposure on the odds of hypertension in American children. These findings offer an insight that early weight control and reduction of tobacco exposure may be important to reduce odds of hypertension in children.
Introduction
Hypertension in children has become a major global public health problem (1). A large amount of research evidence shows that childhood hypertension is closely related to hypertension and cardiovascular disease in adults (2, 3). Therefore, it is important to prevent and manage the development of hypertension in children.
The occurrence of hypertension in children is influenced by many factors. Previous research has shown that overweight and obese children were more likely to develop hypertension than underweight or normal-weight children (4, 5). A meta-analysis also concluded that childhood overweight and obesity were associated with elevated blood pressure (BP), and controlling childhood obesity is beneficial in lowering BP (6). Tobacco exposure dramatically increases BP by activating the sympathetic nervous system (7). Recent evidence suggests that tobacco exposure plays an important role in the development of hypertension (8, 9). In the study of Levy RV, et al, they found that tobacco exposure was associated with both elevated BP and hypertension in children and adolescents (10). Liu SH, et al., also reported that higher diastolic blood pressure (DBP) in association with secondhand tobacco smoke exposure during childhood (11).
Interestingly, several studies have found a combined effect of body fat/overweight and tobacco exposure on hypertension in adults. A cross-sectional study showed that there was an interaction between lipid accumulation product (LAP) and smoking on hypertension risk, and the risk of hypertension in male with higher LAP and smoking was 3.32 times that of men with lower LAP and non-smoking (12). Shen et al. observed that the synergistic effect of secondhand smoke exposure and vitamin D deficiency on hypertension was influenced by body mass index (BMI), and the synergistic effect was particularly pronounced in overweight women (13). This interactive effect may be due to the shared effects of obesity and tobacco exposure on airway or systemic oxidative stress and inflammation (12, 13). However, there was few studies to explore the joint effect of overweight/obesity and tobacco exposure on the odds of hypertension risk in children and adolescents.
Here, this study intends to explore the combined effects of overweight/ obesity and tobacco exposure on children’s hypertension, which provided a scientific basis for the prevention and management of hypertension in children.
Participants and methods
Study participants
In this cross-sectional study, we analyzed publicly available data from the National Health and Nutrition Examination Survey (NHANES) between 1999 and 2018. NHANES is a program of studies conducted by the National Center for Health Statistics (NCHS). The survey combines interviews (demographic, socioeconomic, dietary, and health-related questions) and physical examinations (medical, dental, physiological measurements and laboratory tests) (13). Since our study was a secondary analysis for NHANES public database, ethical approval from Guang’ anmen Hospital, China Academy of Chinese Medical Sciences was not required for this study. Informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
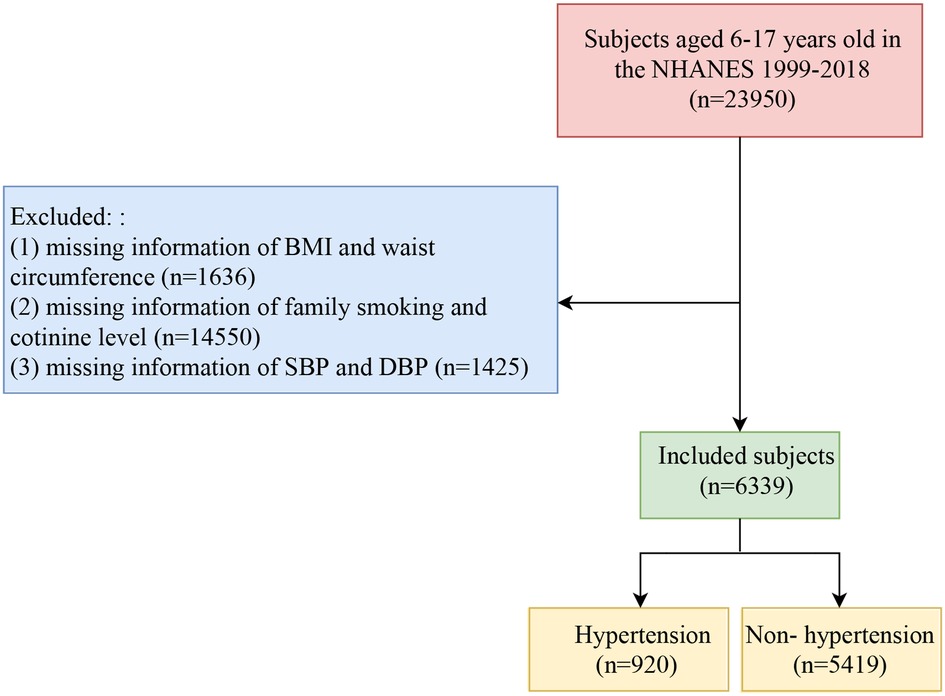
In the current analysis, the inclusion criterion was subjects aged 6–17 years. The exclusion criteria were as follows: (1) subjects with missing information of BMI and waist circumference (n = 1,636); (2) subjects with missing information of family smoking and cotinine level (n = 14,550); (3) subjects with missing information of systolic blood pressure (SBP) and diastolic blood pressure (DBP) (n = 1,425). Finally, a total of 6,339 subjects were included in this study. The flow chart of population selection was shown in Figure 1.
Definition of hypertension
For participants in the NHANES database, three consecutive BP measurements (SBP and DBP; Baumanometer® calibrated mercury true gravity wall model sphygmomanometer) were taken after a trained BP examiner asked the participants to sit quietly and rest for five minutes (14). For participants with three measurements, the BP record is the average of the last two measurements; for those with two or one measurement, the BP record is based on the last measurements. All BP measurements (systolic and diastolic) were conducted in a Mobile Examination Center (MEC). Hypertension is defined as: (1) mean SBP and/or DBP ≥90th percentile for sex, age, and height (for children aged 1–13 years), and SBP ≥120 mmHg and/or a DBP ≥80 mmHg (for adolescents aged 13–17 years) according to the 2017 American Academy of Pediatrics guidelines (15). (2) self-reported having been diagnosed with hypertension or taking antihypertensive medication. Either of these two conditions can be diagnosed as hypertension.
Assessment of overweight/obesity and tobacco exposure
In the NHANES database, measurements of participants’ height (Stadiometer) and weight (Digital weight scale) were collected by trained health technicians in the MEC. Participants of all ages reported their weight in kilograms, while those aged 2 and older recorded their height in centimeters (https://wwwn.cdc.gov/Nchs/Nhanes/2009−2010/BMX_F.htm). BMI are calculated for NHANES participants follows: weight (kg) divided by the square of height (m). According to the World Health Organization (WHO 2007 Z-score) and the International Obesity Task Force (IOTF2000), gender- and age-specific BMI cut-points were used to define overweight/obesity (16): “overweight” was defined as a BMI > 1 standard deviation (SD); “obesity” was defined as BMI > 2SD; and “thinness” was defined as BMI < −2SD.
Cotinine serves as the primary metabolite of nicotine. In this study, we employed both objective and self-reported measures to evaluate tobacco exposure (17). Subjects were categorized as tobacco exposure if their serum cotinine levels were >0.05 µg/L or if they reported the presence of at least one smoker in their household; subjects were classified as non-tobacco exposure if their serum cotinine levels were ≤0.05 µg/L and no smokers were reported in the household.
Data collection
Some variables of the participants were extracted: age (years), gender, race, education level, BMI (kg/m2), waist circumference (cm), income, screen time (h/day), energy intake, maternal smoking during pregnancy, birth weight (pounds), childhood smoking (active smoking, passive smoking), cotinine (µg/l). Screen time was considered as the time spent watching TV/videos and playing computer games (18); and the screen time was categorized as high-level group (≥3 h/day) and low-level group (<3 h/day).
Statistical analysis
In this study, Continuous variables with normal distribution were described as weighted mean (standard error) [Mean (SE)], and independent samples t-test for comparison between two groups. Categorical variables were described as weighted percentages and frequencies [n (%)], and the chi-square test was used for the comparison between groups; rank data required the use of rank sum test. Statistical analyses were performed using SAS 9.4 software (SAS Institute Inc., Cary, NC, USA), R 4.2.2 software and Python 3.9.12 software. P < 0.05 was considered statistically significant.
We used the weighted univariate and multivariate logistic regression models to examine the association of overweight/obesity and tobacco exposure with the odds of hypertension in children, respectively. The multivariate logistic regression model adjusted for gender, education level, waist circumference, maternal smoking during pregnancy and birth weight. Importantly, we assessed the combined effects of overweight/ obesity and tobacco exposure on hypertension in children. Odds ratios (OR) with 95% confidence intervals (CI) were calculated. Simultaneously, this joint effect has also been investigated in different populations. In this study, random forest interpolation method was used to fill the missing variables, and the difference analysis was conducted on the data before and after interpolation (Supplementary Table S1).
Results
Basic characteristics
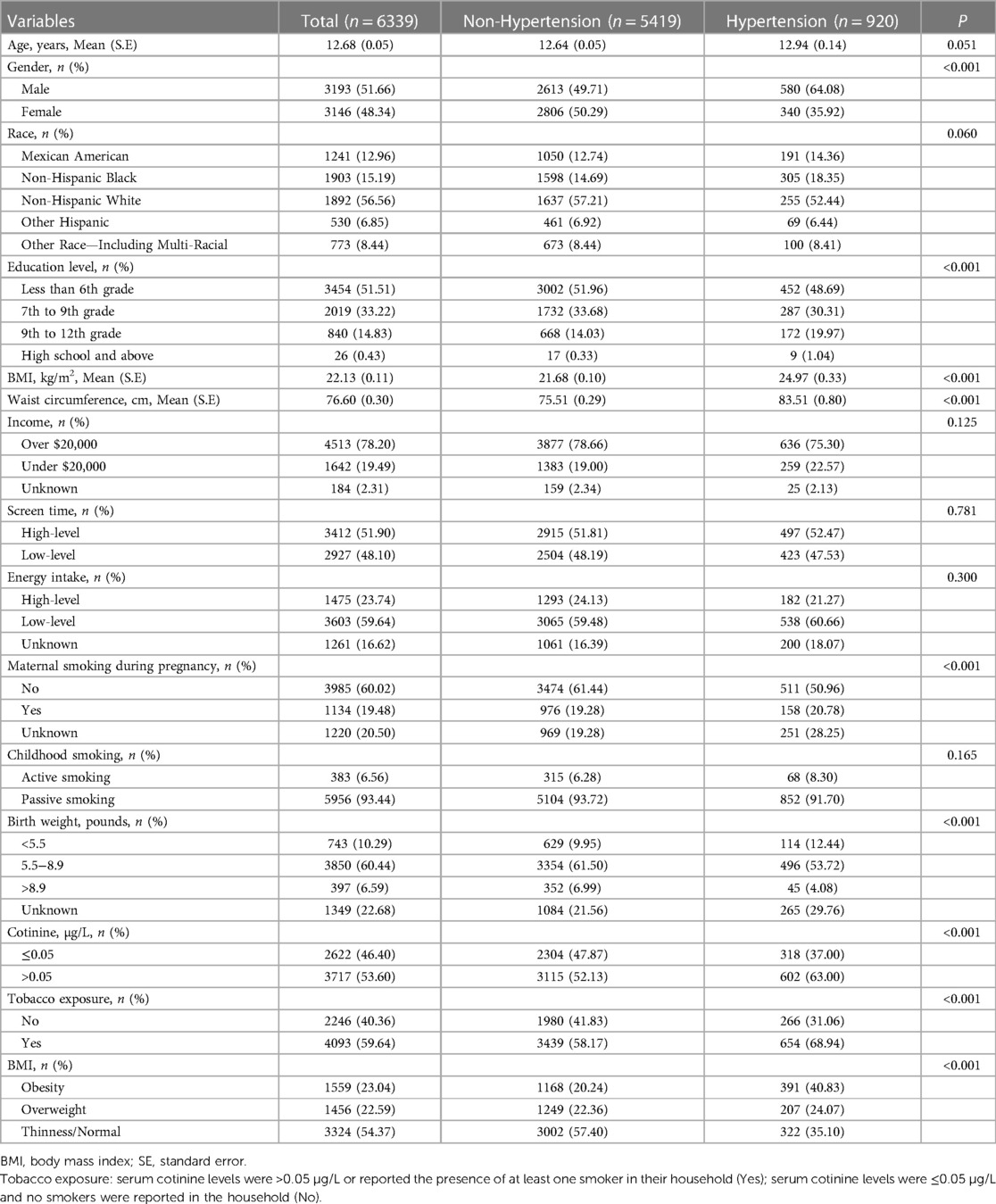
Table 1 presents the basic characteristics of all eligible participants (n = 6,339). The mean age was 12.68 years old, and 51.66% were males. In this population, the prevalence of hypertension was approximately 14.51%. We compared the differences in characteristics between the hypertension group and non-hypertension group. Individuals with hypertension had a higher rate of overweight/obesity than those without hypertension (24.07%/40.83 vs. 22.36%/20.24, P < 0.001), as well as the rate of maternal smoking during pregnancy (20.78% vs. 19.28%, P < 0.001). Compared with participants without hypertension, those with hypertension tended to the tobacco exposure (P < 0.001). Additionally, we found significant differences between the two groups for some variables, including gender, education level, waist circumference, maternal smoking during pregnancy and birth weight, which were also considered as confounding factors in this study.
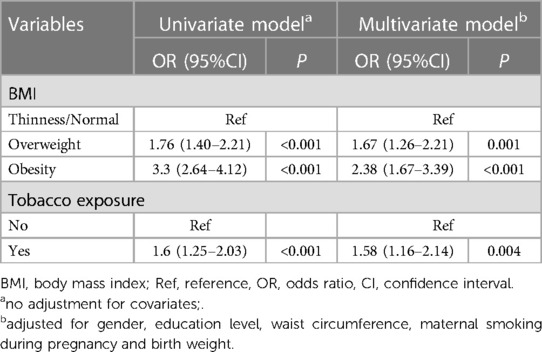
The association of overweight/obesity and tobacco exposure with the risk of hypertension in children
As shown in Table 2, we assessed the association of overweight/obesity and tobacco exposure on hypertension, respectively. In the weighted univariate logistic regression model, compared with thinness/normal group, the OR for the relationship of overweight and hypertension odds was 1.76 (95%CI: 1.40−2.21); and the OR for the relationship of obesity and hypertension odds was 3.30 (95%CI: 2.64−4.12). After adjusting confounding factors, overweight (OR = 1.67, 95%CI: 1.26−2.21, P = 0.001) and obesity (OR = 2.38, 95%CI: 1.67−3.39, P < 0.001) remained associated with odds of hypertension in children. Similarly, tobacco exposure has been found to be related to the odds of hypertension in children in the weighted multivariate logistic regression model (OR = 1.58, 95%CI: 1.16−2.14, P = 0.004).
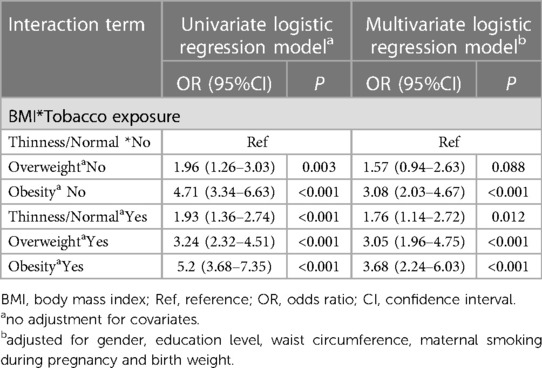
Combined effects analysis
We divided the entire population into six groups based on gender- and age-specific BMI level and whether tobacco exposure was present (group 1: thinness/normal and non-tobacco exposure; group 2: overweight and non-tobacco exposure; group 3: obesity and non-tobacco exposure; group 4: thinness/normal and tobacco exposure; group 5: overweight and tobacco exposure; group 6: obesity and tobacco exposure). As expressed in Table 3, using thinness/normal and non-tobacco exposure (group 1) as the reference, the OR for the relationship of the other five groups and hypertension risk was 1.96 (95%CI: 1.26−3.03, P = 0.003, group 2), 4.71 (95%CI: 3.34−6.63, P < 0.001, group 3), 1.93 (95%CI: 1.36−2.74, P < 0.001, group 4), 3.24 (95%CI: 2.32, P < 0.001, group 5) and 5.20 (95%CI: 3.68−7.35, P < 0.001, group 6), respectively. After adjusting confounding factors, “obesity and non-tobacco exposure” (OR = 3.08, 95%CI: 2.03−4.67, P < 0.001, group 3), “thinness/normal and tobacco exposure” (OR = 1.76, 95%CI: 1.14−2.72, P = 0.012, group 4), “overweight and tobacco exposure” (OR = 3.05, 95%CI: 1.96−4.75, P < 0.001, group 5) and “obesity and tobacco exposure” (OR = 3.68, 95%CI: 2.24−6.03, P < 0.001, group 6) were still associated with the odds of hypertension in children. The result also indicated that the combined effects of overweight/obesity and tobacco exposure were associated with the odds of hypertension among children.
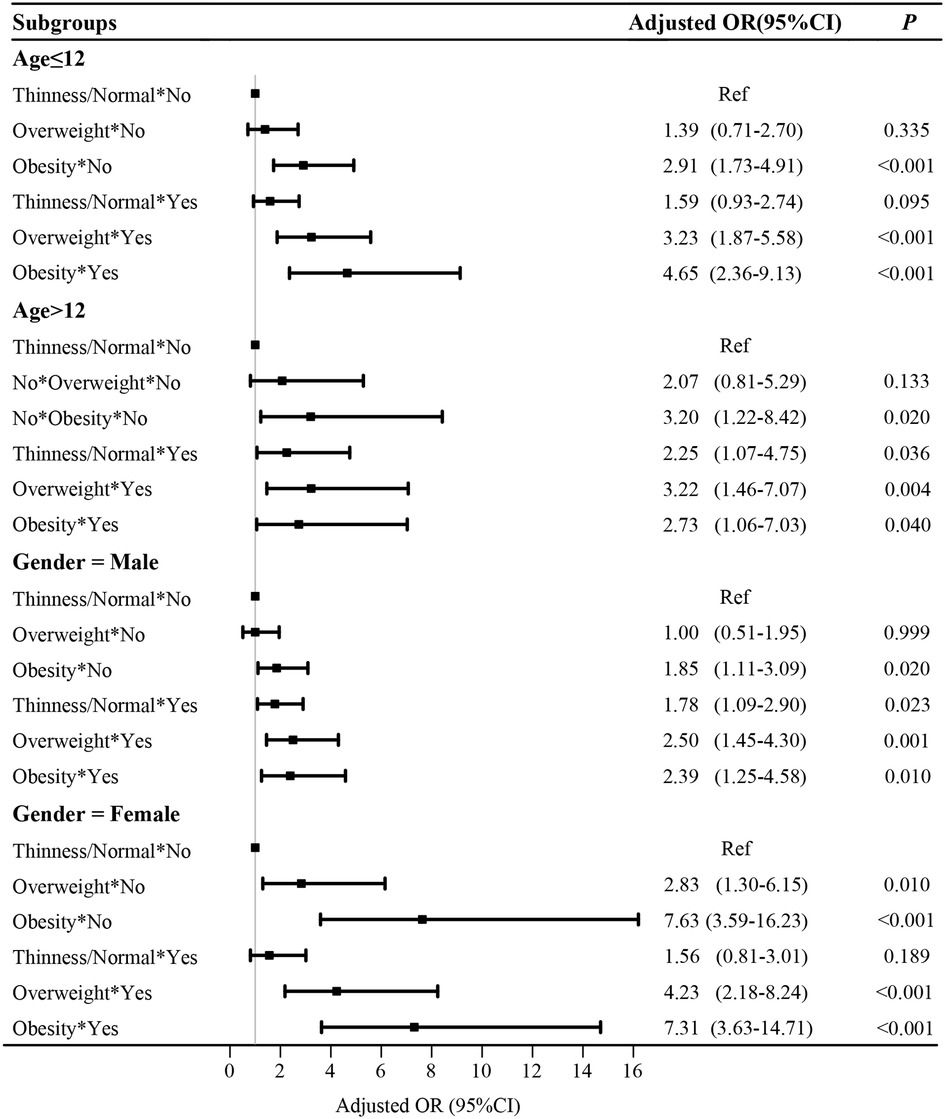
Subgroup analysis based on age and gender
After adjusting confounding factors, the combined effects of overweight/ obesity and tobacco exposure with the odds of hypertension were assessed in different populations (Figure 2). In the age ≤12 years group, “obesity and non-tobacco exposure”, “overweight and tobacco exposure” and “obesity and tobacco exposure” were associated with the odds of hypertension in children. In the age >12 years group, “obesity and non-tobacco exposure”, “thinness/normal and tobacco exposure”, “overweight and tobacco exposure” and “obesity and tobacco exposure” were associated with the odds of hypertension in children. In the stratification by gender, we also observed the combined effects of overweight/obesity and tobacco exposure on the odds of hypertension in children.
Discussion
Our study suggested the independent relationship between overweight/obesity, tobacco exposure and the odds of children’s hypertension. More importantly, this study indicated the joint effect between overweight/obesity and tobacco exposure towards the odds of hypertension in children. These findings offer a new insight that early weight control and reduction of tobacco exposure may be important to reduce the odds of hypertension in children.
In this study, the prevalence of overweight, obesity and hypertension were approximately 22.59%, 23.04% and 14.51%, respectively. Studies conducted in China reported that the prevalence rates of childhood overweight and obesity were 10.90% and 8.70%, respectively (19); while the prevalence rate of hypertension was approximately 13.56% (20). The difference in prevalence may be related to variations in dietary habits across different countries. Our study is one of those supporting the evidence that overweight/ obesity was related to the odds of hypertension in children. Several mechanisms might be used to explain this relationship: For overweight/ obesity populations, adipocytes produce a hormone called leptin, which can bind to leptin receptors in the central nervous system to increase sympathetic nerve activity, leading to hypertension development (21, 22). Obesity can lead to increased sympathetic nervous system activity (23). In addition, dietary factors, endothelial and vascular dysfunction, neuroendocrine imbalances, metabolic, sodium retention, and inflammation have all been identified as potential mechanisms for the association of obesity with hypertension (24–26). Several researchers have proposed a relationship between tobacco exposure and the odds of hypertension (10, 27, 28). The result of our study was consistent with previous studies. Skipina TM, et al. also pointed out that cigarette smoke is able to induce cardiovascular mitochondrial oxidative stress, promote endothelial dysfunction, and contribute to the development of hypertension (8). In this study, we found that there was a higher rate of tobacco exposure in the hypertension group than non-hypertension group. After adjusting confounding factors, tobacco exposure was considered to be related to the odds of hypertension in children. It is worth mentioning that, “thinness/normal and tobacco exposure” was also found to be associated with the odds of hypertension in children, which also means that tobacco exposure has an effect on hypertension in children regardless of BMI level.
A recent cross-sectional study reported that there was an interactive effect between secondhand smoke exposure and overweight on the prevalence of hypertension among non-smoking Chinese coke oven workers and NHANES participants (29). To our knowledge, there has been no clear conclusion about the overweight/obesity and tobacco exposure on hypertension odds in children and adolescents so far. In the present study, we observed the joint effect between overweight/obesity and tobacco exposure with hypertension odds in children. Potential mechanisms may involve the effects of airway or systemic oxidative stress and inflammation (12, 13, 29). Not only that, the results of subgroup analysis based on age and gender also indicated that the joint effect of thinness/normal and tobacco exposure on the risk of hypertension was not significant among children younger than 12 years old and female children. The reason may be related to the lower level of tobacco exposure in this population.
Nevertheless, this study had certain limitations. Firstly, this was a cross-sectional study, we were unable to assess the causal relationship between overweight/ obesity, tobacco exposure and hypertension in children. Secondly, although we controlled for some potential confounders, some possible confounders that were not included in the NHANES database, such as parental hypertension and obesity status, remained. Lastly, the study had a limited sample size of active smoking children, and the gender and age of active smokers were not included in the analysis. Further prospective studies are needed to confirm these findings.
Conclusion
In summary, overweight/obesity and tobacco exposure were associated with higher odds of hypertension in children, respectively. There exist joint effect of overweight/obesity and tobacco exposure on the odds of hypertension in American children. These findings offer a new insight that early weight control and reduction of tobacco exposure may be important to reduce odds of hypertension in children.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: NHANES database, https://wwwn.cdc.gov/nchs/nhanes/.
Ethics statement
Ethical approval was not provided for this study on human participants because our study was a secondary analysis for NHANES public database. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
HG and JL designed the study. HG wrote the manuscript. LH and ML collected, analyzed, and interpreted the data. JL critically reviewed, edited, and approved the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the China Academy of Chinese Medical Sciences Innovation Fund (No.CI2020A02509) and China Center for Evidence Based Traditional Chinese Medicine (No.49425).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1188417/full#supplementary-material
References
1. Flynn JT, Urbina EM, Brady TM, Baker-Smith C, Daniels SR, Hayman LL, et al. Ambulatory blood pressure monitoring in children and adolescents: 2022 update: a scientific statement from the American heart association. Hypertension. (2022) 79(7):e114–24. doi: 10.1161/hyp.0000000000000215
2. Song P, Zhang Y, Yu J, Zha M, Zhu Y, Rahimi K, et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr. (2019) 173(12):1154–63. doi: 10.1001/jamapediatrics.2019.3310
3. de Simone G, Mancusi C, Hanssen H, Genovesi S, Lurbe E, Parati G, et al. Hypertension in children and adolescents. Eur Heart J. (2022) 43(35):3290–301. doi: 10.1093/eurheartj/ehac328
4. Nguyen T, Lau DC. The obesity epidemic and its impact on hypertension. Can J Cardiol. (2012) 28(3):326–33. doi: 10.1016/j.cjca.2012.01.001
5. Zhao W, Mo L, Pang Y. Hypertension in adolescents: the role of obesity and family history. J Clin Hypertens (Greenwich). (2021) 23(12):2065–70. doi: 10.1111/jch.14381
6. Cai L, Wu Y, Wilson RF, Segal JB, Kim MT, Wang Y. Effect of childhood obesity prevention programs on blood pressure: a systematic review and meta-analysis. Circulation. (2014) 129(18):1832–9. doi: 10.1161/circulationaha.113.005666
7. Huntington-Moskos L, Turner-Henson A, Rice M. Tobacco exposure, weight status, and elevated blood pressure in adolescents. J Community Health. (2014) 39(4):653–9. doi: 10.1007/s10900-014-9839-5
8. Dikalov S, Itani H, Richmond B, Vergeade A, Rahman SMJ, Boutaud O, et al. Tobacco smoking induces cardiovascular mitochondrial oxidative stress, promotes endothelial dysfunction, and enhances hypertension. Am J Physiol Heart Circ Physiol. (2019) 316(3):H639–h646. doi: 10.1152/ajpheart.00595.2018
9. Bernabe-Ortiz A, Carrillo-Larco RM. Second-hand smoking, hypertension and cardiovascular risk: findings from Peru. BMC Cardiovasc Disord. (2021) 21(1):576. doi: 10.1186/s12872-021-02410-x
10. Levy RV, Brathwaite KE, Sarathy H, Reidy K, Kaskel FJ, Melamed ML. Analysis of active and passive tobacco exposures and blood pressure in US children and adolescents. JAMA Netw Open. (2021) 4(2):e2037936. doi: 10.1001/jamanetworkopen.2020.37936
11. Liu SH, Liu B, Sanders AP, Saland J, Wilson KM. Secondhand smoke exposure and higher blood pressure in children and adolescents participating in NHANES. Prev Med. (2020) 134:106052. doi: 10.1016/j.ypmed.2020.106052
12. Song J, Zhao Y, Nie S, Chen X, Wu X, Mi J. The effect of lipid accumulation product and its interaction with other factors on hypertension risk in Chinese han population: a cross-sectional study. PLoS One. (2018) 13(6):e0198105. doi: 10.1371/journal.pone.0198105
13. Shen Q, Xu Q, Li G, Ren L, Zhang Z, Zhang Y, et al. Joint effect of 25-hydroxyvitamin D and secondhand smoke exposure on hypertension in non-smoking women of childbearing age: nHANES 2007−2014. Environ Health. (2021) 20(1):117. doi: 10.1186/s12940-021-00803-1
14. Wu Z, Wu Y, Rao J, Hu H, Wang C, Wu J, et al. Associations among vitamin D, tobacco smoke, and hypertension: a cross-sectional study of the NHANES 2001−2016. Hypertens Res. (2022) 45(12):1986–96. doi: 10.1038/s41440-022-01023-x
15. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. (2017) 140:3. doi: 10.1542/peds.2017-1904
16. de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. (2007) 85(9):660–7. doi: 10.2471/blt.07.043497
17. Fan Z, Gong X, Xu H, Wang H, Zeng N, Li L, et al. Gender differences in the associations between tobacco smoke exposure and depressive symptoms among U.S. Adults: NHANES 2007−2018. J Psychiatr Res. (2022) 146:249–57. doi: 10.1016/j.jpsychires.2021.11.013
18. Ahluwalia N, Frenk SM, Quan SF. Screen time behaviours and caffeine intake in US children: findings from the cross-sectional national health and nutrition examination survey (NHANES). BMJ Paediatr Open. (2018) 2(1):e000258. doi: 10.1136/bmjpo-2018-000258
19. Dong J, Guo XL, Lu ZL, Cai XN, Wang HC, Zhang JY, et al. Prevalence of overweight and obesity and their associations with blood pressure among children and adolescents in shandong, China. BMC Public Health. (2014) 14:1080. doi: 10.1186/1471-2458-14-1080
20. Chen C, Lu M, Wu Y, Zhang Z, Hu J, Yin J, et al. The prevalence of hypertension and elevated blood pressure and its correlation with overweight/obesity among students aged 6−17 years in suzhou. J Pediatr Endocrinol Metab. (2021) 35(3):341–8. doi: 10.1515/jpem-2021-0033
21. Hall JE, da Silva AA, do Carmo JM, Dubinion J, Hamza S, Munusamy S, et al. Obesity-induced hypertension: role of sympathetic nervous system, leptin, and melanocortins. J Biol Chem. (2010) 285(23):17271–6. doi: 10.1074/jbc.R110.113175
22. Pan WW, Myers MG Jr. Leptin and the maintenance of elevated body weight. Nat Rev Neurosci. (2018) 19(2):95–105. doi: 10.1038/nrn.2017.168
23. Tanaka M. Improving obesity and blood pressure. Hypertens Res. (2020) 43(2):79–89. doi: 10.1038/s41440-019-0348-x
24. DeMarco VG, Aroor AR, Sowers JR. The pathophysiology of hypertension in patients with obesity. Nat Rev Endocrinol. (2014) 10(6):364–76. doi: 10.1038/nrendo.2014.44
25. Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity, kidney dysfunction and hypertension: mechanistic links. Nat Rev Nephrol. (2019) 15(6):367–85. doi: 10.1038/s41581-019-0145-4
26. Yun M, Zhang T, Li S, Wang X, Fan L, Yan Y, et al. Temporal relationship between body mass index and uric acid and their joint impact on blood pressure in children and adults: the bogalusa heart study. Int J Obes (Lond). (2021) 45(7):1457–63. doi: 10.1038/s41366-021-00810-9
27. Skipina TM, Soliman EZ, Upadhya B. Association between secondhand smoke exposure and hypertension: nearly as large as smoking. J Hypertens. (2020) 38(10):1899–908. doi: 10.1097/hjh.0000000000002478
28. Zhang Q, Zeng G, Wang X, Wu KH. Associations of exposure to secondhand smoke with hypertension risk and blood pressure values in adults. Environ Health Prev Med. (2021) 26(1):86. doi: 10.1186/s12199-021-01009-0
29. Zhao X, Guo S, Zhang R, Liu L, Guo L, Liu G, et al. The interaction effects of secondhand smoke exposure and overweight on the prevalence of hypertension in Chinese coke oven workers and NHANES participants (2013−2016). Chemosphere. (2022) 303(Pt 2):135120. doi: 10.1016/j.chemosphere.2022.135120
Keywords: children, overweight/ obesity, tobacco exposure, hypertension, joint effect
Citation: Gu H, Hao L, Li M and Li J (2023) Joint effect of overweight/obesity and tobacco exposure on hypertension in children aged 6–17 years: a cross-sectional study. Front. Pediatr. 11:1188417. doi: 10.3389/fped.2023.1188417
Received: 17 March 2023; Accepted: 14 June 2023;
Published: 30 June 2023.
Edited by:
Giulio Maltoni, Sant'Orsola-Malpighi Polyclinic, ItalyReviewed by:
Yolanda Flores-Peña, Autonomous University of Nuevo León, MexicoAna Maria Salinas Martínez, Autonomous University of Nuevo León, Mexico
© 2023 Gu, Hao, Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ji Li bGlqZGN0QG91dGxvb2suY29t
 Huan Gu1
Huan Gu1 Ji Li
Ji Li