- 1Lab LRI Division of Isotopic Medicine, Pediatric and Adult Physiology, University of Antananarivo, Antananarivo, Madagascar
- 2ARCIM Institute, Department of Pediatrics, Filderklinik, University of Tübingen, Filderstadt, Germany
- 3ARCIM Institute, Department of Neonatology, Filderklinik, University of Tübingen, Filderstadt, Germany
Editorial on the Research Topic
Case reports in pediatric gastroenterology, hepatology and nutrition 2022
Introduction
The combined fields of gastroenterology, hepatology, and nutrition form a holistically evolving foundation with segmented subspecialties linked around the gastrointestinal (GI) tract and its appendages. Another key driver is macro/micro nutrition, closely linked to interplaying with the gut-immune system and the GI microbiome extended to the gut-brain axis, these subfields benefit from the technical support of functional GI assessments, super-resolution multimodal imaging and child-sized diagnostic/interventional endoscopy (Int-Endosc). The dynamics of the field stimulate translational research, inspiring thriving publications, including Clinical Case Reports (CCRs).
While much of the scientific interest during the COVID-19 pandemic focused on the importance of randomized controlled trials (RCTs), large case series, and meta-analyses (1) addressing SARS, Cov-2 and vaccines, it is now time to refocus on other “thematic organ systems,” including underutilized scientific approaches such as CCRs (2). These typically have the potential to describe novel discoveries and cutting-edge treatment modalities, providing a valuable source of new concepts and suscitating questioning knowledge for clinical care in the broad field of pediatric gastroenterology.
Previously, CCRs in Frontiers in Pediatrics were scattered among different sections. In 2022, the Editorial Board initiated this Research Topic (RT) to focus explicitly on CCRs, to which we have brought our collective interest and expertise. The aim of this RT was to gather outstanding findings and advances in pediatric gastroenterology and related fields.
Results
Five CCRs were accepted after a rigorous interactive blinded peer review process involving 75 experts from various countries.
Jing Sun et al. reported a case of Caroli's disease (CD), a rare congenital malformation with intrahepatic bile duct dilatation that presents a challenging diagnostic process. This 13-year-old boy presented with an unexplained and recurrent fever, non-specific abdominal pain, and episodic jaundice. He was started on an appropriate antibiotic regimen for suspected suppurative cholangitis. He underwent an extensive work-up, including magnetic resonance cholangiopancreatography (MRCP), which showed specific features of CD biliary ectasia. This relatively early diagnosis has avoided serious complications that can include extensive hepatic abscess, biliary infection, pancreatitis, and, in late stages, cholangiocarcinoma in the case of an erroneous or delayed diagnosis. This CCR outlines the relevance of MRCP, an imaging tool with highly discriminative diagnostic performance, to expedite the challenging characterization of malformed hepatic bile ducts. Its early application avoids a “diagnostic odyssey” and the poor outcome of a child with CD condemned to liver transplantation (3).
In mid-2022, Yujiao Zhou et al. reported a case of acute hepatitis in a 10-year-old-boy with no history of COVID-19. The boy presented with abdominal pain, hepatic splenomegaly (confirmed by ultrasound), and jaundice associated with high bilirubin levels and elevated transaminases (alanine-aminotransferase 2,330 U/L and aspartate-aminotransferase 1,326 U/L). MRCP showed edema of the periportal region and a stenotic choledochus. A comprehensive search for common etiologies was undertaken. This excluded standard viral infections (e.g., SARS COV-2, 41-adenovirus, Epstein-Barr, herpes simplex virus, and cytomegalovirus) and autoimmune hepatitis. The authors reached a diagnosis of non-AE hepatitis (WHO criteria). Next-generation sequencing, metagenomic NGS, and hepatic biopsy unexpectedly revealed Torque-Teno Virus (TTV) in the blood and liver. Plasmapheresis with a boost of corticosteroids improved hepatic function leading to his discharge. This CCR addressed the hot topic of mystery hepatitis by identifying, for the first time, TTV as a potential cause of this liver immune dysregulation during the omicron Covid-19 wave (4).
The case report by Kakiuchi et al. describes an interesting case of GI bleeding in a 7-year-old boy with Peutz-Jeghers syndrome (PJS) and hypofibrinogenemia following Int-Endosc mucosal resection of small intestinal polyps. Genetic characterization of this fibrinogen disorder revealed a heterozygous pathogenic mutation in exon 10 of the fibrinogen gamma chain. In this case, we see the unusual occurrence of two separate monogenic diseases in one individual. This CCR expands our understanding of conditions that may be associated with PJS and outlines key aspects of the diagnosis of PJS and congenital abnormalities of fibrinogen. The key learning point from this CCR was the importance of taking steps to prevent postoperative bleeding during polypectomy in individuals with PJS. Hypofibrinogenemia should be considered a risk factor for such bleeding (5).
Hanhua Zhang et al. describe the first case of a 12-year-old boy diagnosed simultaneously with two rare conditions: (i) acute pandysautonomia (A-PDA), a post-ganglionic sympathetic and parasympathetic failure, and (ii) distal esophageal spasm (DES), a motility disorder. Without any relevant family history, this boy presented with recurrent dysphagia, nausea, vomiting and autonomic instability (e.g., decreased lacrimation and sweating but over-salivation, pupillary dilation, and urinary retention).
After considering the differential diagnoses, A-PDA was confirmed by MR imaging, which showed enhancement of the lumbar nerve root in the left fiber endings. This case of A-PDA did not respond to treatment with intravenous immunoglobulin. A combination of oryzanol, mecobalamin, and lorazepam improved his vomiting. However, he still exhibited dysphagia and residual postprandial vomiting with growth retardation requiring nasogastric feeding. Upper GI endoscopy revealed a contraction of the lower esophagus with a contractile ring. Results of high-resolution esophageal manometry and barium swallowing confirmed the diagnosis of DES. His family refused plasmapheresis, even though it is recommended for such a condition. The selected treatment option was per oral endoscopic myotomy (POEM), a minimally invasive procedure that has gained more popularity in adults than in children. POEM resulted in a significant relief of the patient's symptoms, as exemplified by a reduction in the commonly used Ekcardt score from 9 to 2 postoperatively. This CCR highlights the first use of a cutting-edge technique (POEM) for DES in a child who was also diagnosed with A-PDA, another rare condition (6).
A 6-year-old boy with autism, acute malnutrition, and undiagnosed scurvy experienced a pulmonary arterial hypertension (PAH) crisis that resulted in cardiac arrest during endoscopic assessment, as reported by Quinn et al. The risk of experiencing anesthesia in a patient can be greatly increased by life-threatening cardiovascular events due to a hidden selective malnutrition. In addition, a severe but reversible form of PAH has been linked to vitamin C deficiency. The authors undertook a comprehensive review of the relevant literature, proposed a novel clinical algorithm for risk stratification and mitigation prior to anesthesia in patients at high risk for scurvy and associated PAH, and discussed how to take the next step toward better patient outcomes. This CCR raises awareness of the importance of considering pre-anesthesia micronutrient assessment in children (7).
Concluding remarks
This RT focusing on digestive CCRs in Frontiers Pediatrics follows the trend of o the renowned journals to set aside a separate location for the collection of CCR (8, 9). This RT is noteworthy because it addresses various topics spanning the GI, hepatic, Int-Endosc, and nutritional fields, particularly a secular micronutrient deficiency. Each CCR is rich in key takeaways for readers and clinicians, which makes them so interesting.
Overall, CCRs are a useful way to expand knowledge about rare and unusual complications of common or orphan diseases. Furthermore, a re-evaluation of collections of CCRs may even bring to light valuable data with practical real-life implications (10). The CCR platform is also of great interest to busy gastroenterologists searching for a specific topic.
This RT hopefully serves to justify the publication of CCRs, an often-undervalued format at the bottom of the pyramid of scientific studies (Figure 1). The use of current methodological quality requirements should further enhance the value of CCRs, allowing them to continue to contribute to advances in clinical practice (11–14).
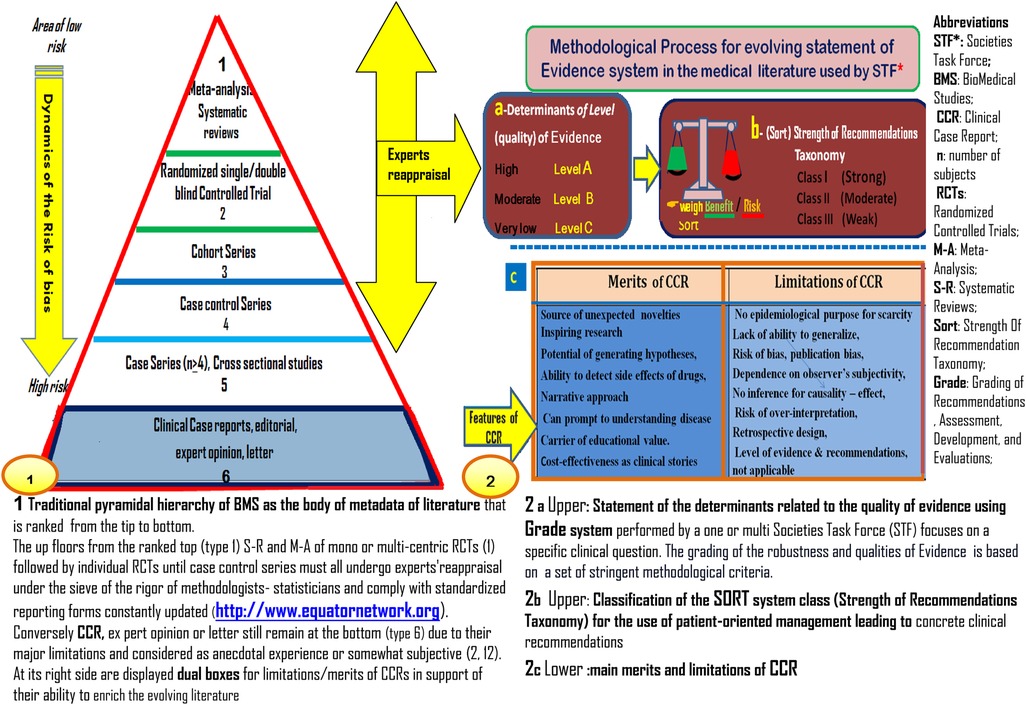
Figure 1. Schematic representation of biomedical studies for use in clinical practice guidelines and recommendations.
Author contributions
Each author has contributed to the handling success of this RT in providing the abstract of their respective topic. BR and JV wrote the first overall draft. BR designed the figure and its associated legend. Both authors contributed equally to refine the scope of this editorial along and shorten the legend in accordance with their respective expertise. Both did the final polishing in English. BR, as the corresponding author, prepared a fairly well-documented response to the reviewer. Both authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to express our gratitude to all the contributors and reviewers for their full commitment to this research topic. Special thanks go to the Frontiers editorial team and staff managers for their technical editorial assistance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1206993/full#supplementary-material.
References
1. Gurevitch J, Koricheva J, Nakagawa S, Stewart G. Meta-analysis and the science of research synthesis. Nature. (2018) 555(7695):175–82. doi: 10.1038/nature25753
2. Vandenbroucke JP. In defense of case reports and case series. Ann Intern Med. (2001) 134(4):330–4. doi: 10.7326/0003-4819-134-4-200102200-00017
3. Ananthakrishnan AN, Saeian K. Caroli’s disease: identification and treatment strategy. Curr Gastroenterol Rep. (2007) 9(2):151–5. doi: 10.1007/s11894-007-0010-7
4. Reshetnyak VI, Maev IV, Burmistrov AI, Chekmazov IA, Karlovich TI. Torque teno virus in liver diseases: on the way towards unity of view. World J Gastroenterol. (2020) 26(15):1691–707. doi: 10.3748/wjg.v26.i15.1691
5. Latchford A, Cohen S, Auth M, Scaillon M, Viala J, Daniels R, et al. Management of Peutz-Jeghers syndrome in children and adolescents: a position paper from the ESPGHAN polyposis working group. J Pediatr Gastroenterol Nutr. (2019) 68(3):442–52. doi: 10.1097/MPG.0000000000002248
6. Mencin AA, Sethi A, Barakat MT, Lerner DG. Peroral endoscopic myotomy (POEM) in children: a state of the art review. J Pediatr Gastroenterol Nutr. (2022) 75(3):231–6. doi: 10.1097/MPG.0000000000003503
7. Trapani S, Rubino C, Indolfi G, Lionetti P. A narrative review on pediatric scurvy: the last twenty years. Nutrients. (2022) 14(3):684. doi: 10.3390/nu14030684
8. Coles A, Mukherjee M, Compston A. Case reports in the lancet. Lancet. (2003) 361(9364):1230. doi: 10.1016/S0140-6736(03)12946-7
9. Akers KG. New journals for publishing medical case reports. J Med Libr Assoc. (2016) 104(2):146–9. doi: 10.3163/1536-5050.104.2.010
10. Rakotoambinina B, Hiffler L, Gomes F. Pediatric thiamine deficiency disorders in high-income countries between 2000 and 2020: a clinical reappraisal. Ann N Y Acad Sci. (2021) 1498(1):57–76. doi: 10.1111/nyas.14669
11. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. (2018) 23(2):60–3. doi: 10.1136/bmjebm-2017-110853
12. Nissen T, Wynn R. The clinical case report: a review of its merits and limitations. BMC Res Notes. (2014) 7:264. doi: 10.1186/1756-0500-7-264
13. Alsaywid BS, Abdulhaq NM. Guideline on writing a case report. Urol Ann. (2019) 11(2):126–31. doi: 10.4103/UA.UA_177_18
Keywords: pandysautonomia, distal esophageal spasm, peutz-Jeghers syndrome, fibrinogen disorders, caroli disease, torque teno virus related hepatitis, scurvy, pediatric digestive clinical case report
Citation: Rakotoambinina B and Vagedes J (2023) Editorial: Case reports in pediatric gastroenterology, hepatology and nutrition 2022. Front. Pediatr. 11:1206993. doi: 10.3389/fped.2023.1206993
Received: 16 April 2023; Accepted: 26 April 2023;
Published: 25 May 2023.
Edited and Reviewed by: Andrew S. Day, University of Otago, New Zealand
© 2023 Rakotoambinina and Vagedes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benjamin Rakotoambinina YWJyLnNjaWVuY2FAZ21haWwuY29t UHJiZW5qYS5pbW1AaG90bWFpbC5jb20=
 Benjamin Rakotoambinina
Benjamin Rakotoambinina Jan Vagedes
Jan Vagedes