- 1Hubert School of Global Health, Emory University Rollins School of Public Health, Atlanta, GA, United States
- 2Research Institute, NorthShore University HealthSystem, Evanston, IL, United States
- 3Rush Medical College of Rush University Medical Center, Chicago, IL, United States
- 4Department of Psychiatry & Behavioral Sciences, Rush University Medical Center, Chicago, IL, United States
Objective: To investigate maternal and parental factors associated with changes in children's body mass index percentile (BMI-P) from 12 to 24 months.
Methods: Data from a prospective cohort of racially and ethnically diverse mothers, fathers, and children (n = 245) were used. Changes in BMI-P from 12 to 24 months of age were examined using height and weight measurements collected at both times. Separate longitudinal mixed-effects models with maximum likelihood were introduced to examine the determinants introduced by mothers and determinants from both parents among all children, and by race and ethnicity.
Results: Models that examine maternal and parental factors showed that children's overall BMI-P decreased from 12 to 24 months [β = −4.85, 95% confidence interval (CI), −7.47 to −2.23]. Stratified tests showed that White children whose parents graduated high school or completed a 4-year college degree or higher had greater decreases in BMI-P than White children born to parents with less than high school education (β = −60.39, 95% CI, −115.05 to −5.72; β = −61.49, 95% CI, −122.44 to −0.53). Among Hispanic/Latinx children, mean BMI-P significantly decreased from 12 to 24 months (β = −7.12, 95% CI, −11.59 to −2.64). Mother's older age (β = 1.83, 95% CI, 0.29–3.36) and child female sex (β = 11.21, 95% CI, 1.61–20.82) were associated with gains in children's BMI-P, while father's older age was associated with decreases (β = −1.19, 95% CI, −2.30 to −0.08).
Conclusions: Parental determinants associated with children's early growth varied by children's sex and racial and ethnic background. Results highlight the importance of understanding racial and ethnicity-specific obesity risks and including fathers in research.
Introduction
In the United States, by the time Hispanic/Latinx and non-Hispanic Black children enter kindergarten, they already bear a higher prevalence of elevated body mass index percentile (BMI-P) than White children (1). Excessive weight gain during the first years of life often continues into adulthood triggering the development of racial and ethnic disparities in cardiometabolic diseases (2). Children who experienced rapid weight gain—particularly during the first 24 months of life—are more likely to develop obesity and adverse cardiometabolic health by early adolescence, than children who never exceeded the 85th BMI-P in the first 2 years of life (3, 4).
Maternal traits, such as mother's BMI, and social determinants of health, such as education and socioeconomic status, are strong predictors of childhood obesity (5–7). Beyond these maternal determinants, studies examining other familial factors yielded inconsistent findings (7–9). The inconsistency in findings may stem from differences across racial and ethnic groups in both child growth patterns and the contribution of social determinants to excessive weight gain in early life (7). Previous research has shown that higher income and education is associated with a lower BMI among White but not Black or Mexican American adults (10). Similarly, Black and Hispanic/Latinx youth experienced diminishing returns in health with increasing parental socioeconomic status relative to White youth (10–13). These differences may begin early in life. Several studies conducted with the Early Childhood Longitudinal Study Birth Cohort (ECLS-B) dataset, a nationally representative cohort of US children, showed that growth trajectories of US 4–6-year-old children vary by race and ethnic background and language spoken at home (14). Among Hispanic/Latina girls, weight differences were mostly explained by the difference in socioeconomic status when compared with their White counterparts (14). Rapid weight gain during the first 9 months of life was the biggest predictor of obesity at kindergarten entrance for White and Black children, but not for Hispanic/Latinx children (15). Notably, the characterization of household socioeconomic status in the ECLS-B study accounted for father's educational attainment, occupation, and prestige. Undoubtedly, although fathers exert an important influence in children's lives and obesity risks, the influence of fathers’ social determinants on children's health is much less understood (16). There are data suggesting that maternal–paternal combined traits would allow improved prediction of early childhood obesity (17), but research of paternal determinants remains limited (16).
These research gaps are a critical barrier to the development of effective obesity prevention strategies for racially and ethnically diverse children, particularly in the first 2 years of life. During the period from 12 to 24 months of age, children with healthy growth trajectories display a decrease in adiposity after they begin to walk and expend more energy (18, 19). In contrast, children who gain excessive weight during this period are at increased risks for delayed motor development (18), future obesity (2, 20), elevated cardiometabolic risk (3, 4), and associated premature diseases and morbidity in older ages (21). While rapid weight gain is considered a critical risk factor during the first 2 years of life, research suggest that weight gain after the first 12 months of life could have more profound effects than weight gains in earlier periods of infancy. In a previous study, researchers found that weight gain during the first 4 months of life was not associated with future obesity risks (22). In contrast, weight gain from birth to 12 months was associated with higher likelihood of obesity by 3 years of age (22). The authors did not examine the impact of weight gain after 12 months. Further information is needed to better understand children's BMI-P dynamics during the period from 12 to 24 months of age and identify differences in the risk factors associated with excessive weight gain among racial and ethnic minority children (23).
The purpose of this study is to investigate maternal and paternal determinants associated with changes in BMI-P from 12 to 24 months. We hypothesize that race- and ethnicity-stratified models will reveal differences in the benefits conferred by parental socioeconomic resources, and that when compared with models examining maternal determinants only, assessment of maternal–paternal combined determinants will introduce additional factors associated with changes in child's BMI-P from 12 to 24 months of age. In addition, we expect maternal and paternal BMI changes (when their child transitions from infancy to toddler ages) will be associated with their child changes in BMI-P from 12 to 24 months of age.
Methods
Study design and participants
Data from the Community Child Health Research Network (CCHN), a 5-year, multi-site prospective cohort study, were used. The CCHN study recruited African American/Black, Hispanic/Latinx, and White mothers and fathers of newborns at the time of delivery and followed them over 2 years. Participants were recruited in Washington, DC; Baltimore, MD; and Lake County, IL. Interviews were conducted when children were about 6, 12, and 24 months of age. Our analytical sample included data from the families that included three participants (mother, father, and child), with complete demographic data collected at baseline, and child BMI-P measurements collected at both the 12- and 24-month follow-up visits (n = 245). Fathers not cohabitating with mothers who agreed to participate in the study were included. Families with children born preterm, mothers not living with or actively in contact with the child delivered at the time of recruitment, and fathers reported as unknown, unavailable (e.g., incarcerated), or unwilling to participate in the study were excluded from the analytical sample.
Ethics approval was sought from and given by the Institutional Review Boards at the respective institutions affiliated with each of the study sites. Mother and father participants provided a written informed consent, which included permission to collect and access health information of themselves and their child. Additional details of the study have been published elsewhere (24).
Measures
Outcome
Children's BMI-P measured at 12 and 24 months
Children's height and weight were measured when children were about 12 months old and a second time at about 24 months of age. Measurements were collected by trained field interviewers who followed a standardized protocol. Children's BMI-P was calculated based on World Health Organization (WHO) age- and sex-specific growth charts. Data of children who did not participate in the 12-month follow-up (n = 14) were imputed using measurements from the 6-month follow-up for estimations. Sensitivity analyses excluding these children are included in the Supplementary Materials. None of the children in our analytical sample were missing the 24-month height and weight measurements.
Independent variables
Parent's race, ethnicity, and nativity
Mothers and fathers were asked to self-identify their race and ethnicity using the following categories: African American or Black, White or Caucasian, and Hispanic or Latinx. Parents who did not report a single race were considered multiracial and combined with the “Other race” category. For nativity, mothers and fathers were asked to report if they were US or foreign-born. Responses were used to classify nativity using a dichotomous indicator for US vs. foreign-born.
Parent's BMI from children's 12–24 months of age
Trained interviewers measured mother's and father's height and weight when their child was 12 and 24 months old following a standardized protocol that included light clothing and no shoes. Height and weight measurements were used to compute BMI-P for sex and age. A BMI-P of 85th to under 95th percentile was considered overweight and 95th percentile and higher as obesity. BMI-P measurements were examined using continuous time-varying variables.
Cohabitation or marital status
Mothers were asked their cohabitation status and marital status with the child's father during first year of study. The responses of cohabitation or marital status were combined into two categories for “not married or living together” and “married or living together.”
Mother and father's level of education
Mothers and fathers were asked about their maximum level of education completed. Responses were combined in four categories for (1) less than high school; (2) high school, GED certificate, or technical school; (3) some college but not a 4-year degree; and (4) 4-year degree or higher, with less than high school as a reference. In the models that examined maternal and paternal predictors together, the highest level of education of both parents was used to examine the influence of parental education.
Family's poverty level
Mothers and fathers were asked to report their income. Individual's income was used to calculate family's income and corresponding poverty level. Poverty level was calculated based on percentage of Federal Poverty Level (FPL) for the aggregated family income and household size. Measurements were classified into three categories for ≤100% FPL, >100% to 200% FPL, and >200% FPL.
Covariates
Maternal and paternal age and children's demographic characteristics, specifically child's age, sex, and birth weight, were included as covariates. Data on these covariates were computed based on data obtained during the baseline interview.
Statistical analysis
Baseline characteristics were examined overall and compared by children's race and ethnicity (White, Black, Latinx, and Other). Children's race was categorized based on the combined mother and father's race and ethnicity. Baseline categorical variables are displayed as frequency counts with percentages and were compared using chi-squared test or Fisher's exact test. Continuous variables are shown as means with standard deviations and were compared using ANOVA tests. Significant changes in continuous BMI-P of children from 12 to 24 months of age were examined using a set of longitudinal mixed-effects models with maximum likelihood estimating method and unstructured covariance. Data were fitted with random effects of intercept and time, which allowed us to account for multiple sources of variability in BMI-P changes from 12 to 24 months of age. Multivariable models examined the association of maternal predictors and predictors from both parents with changes in BMI-P from 12 to 24 months of age. Separate models were introduced to identify the contribution of mothers and the contribution from both parents. Tests included all children with complete families in our sample first, and in secondary analyses, we estimated models stratified by race and ethnicity. Given the sample size limitations, stratified tests were only conducted among White and Hispanic/Latinx children. Sensitivity analyses were conducted with a subsample (n = 231) that excluded 14 children for whom BMI-P was imputed. Characteristics of the subsample are introduced in Supplementary Table S1. Post-hoc power estimates revealed the analyses conducted with a sample of 231 families had a power of 77% to detect a difference of 0.15 in BMI-P while using an F-test with a significance level of 0.05 and adjusting for nine covariates. All statistical analyses were conducted in SAS 9.4 (SAS Institute, Cary, NC, United States).
Results
Characteristics of the study sample
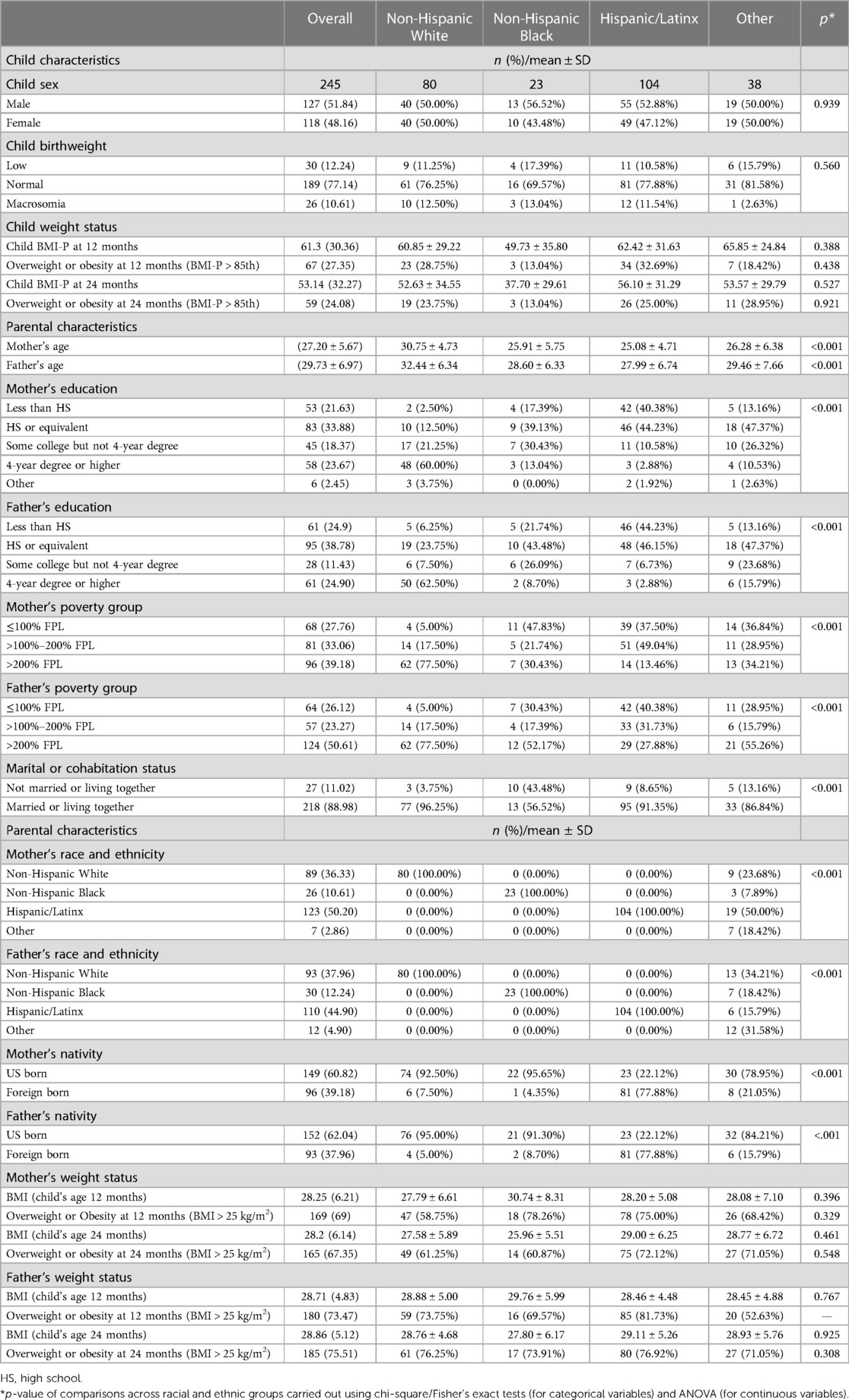
Table 1 provides descriptive characteristics of the sample overall and by race and ethnicity. At 12 months, the mean (standard deviation) BMI-P of children was 61.3 (30.36), and 27.4% had a BMI-P at or above the 85th percentile. By 24 months, the mean BMI-P of children was 53.1 (32.3), and about 24.1% had a BMI-P at or above the 85th percentile. There were no significant differences in children's sex, birthweight, and weight status at 12 and at 24 months across racial and ethnic groups. Mothers’ and fathers’ mean age, nativity, level of completed education, poverty level, and marital status differ significantly by race and ethnicity.
Parental factors associated with change in children's BMI-P from 12 to 24 months
Table 2 presents the association of changes in children's BMI-P from 12 to 24 months with maternal factors separately and maternal and paternal factors combined. Models that examined maternal factors exclusively showed that when compared to being born to White mothers, children born to Hispanic/Latinx mothers had a significant increase in mean BMI-P from 12 to 24 months [β = 11.86, 95% confidence interval (CI), 0.75–22.97, p = 0.04]. Changes in children's BMI-P were associated with children's birthweight (β = 2.09, 95% CI, 0.00–4.18, p < 0.05), but not with changes in their mother's mean BMI over the same period of time (β = 0.36, 95% CI, −0.13 to 0.86, p = 0.15). Sensitivity analyses presented in Supplementary Table S2 showed that both associations were attenuated when examined in a subsample (n = 231) that excluded children for whom BMI-P was imputed in the 12-month visit.
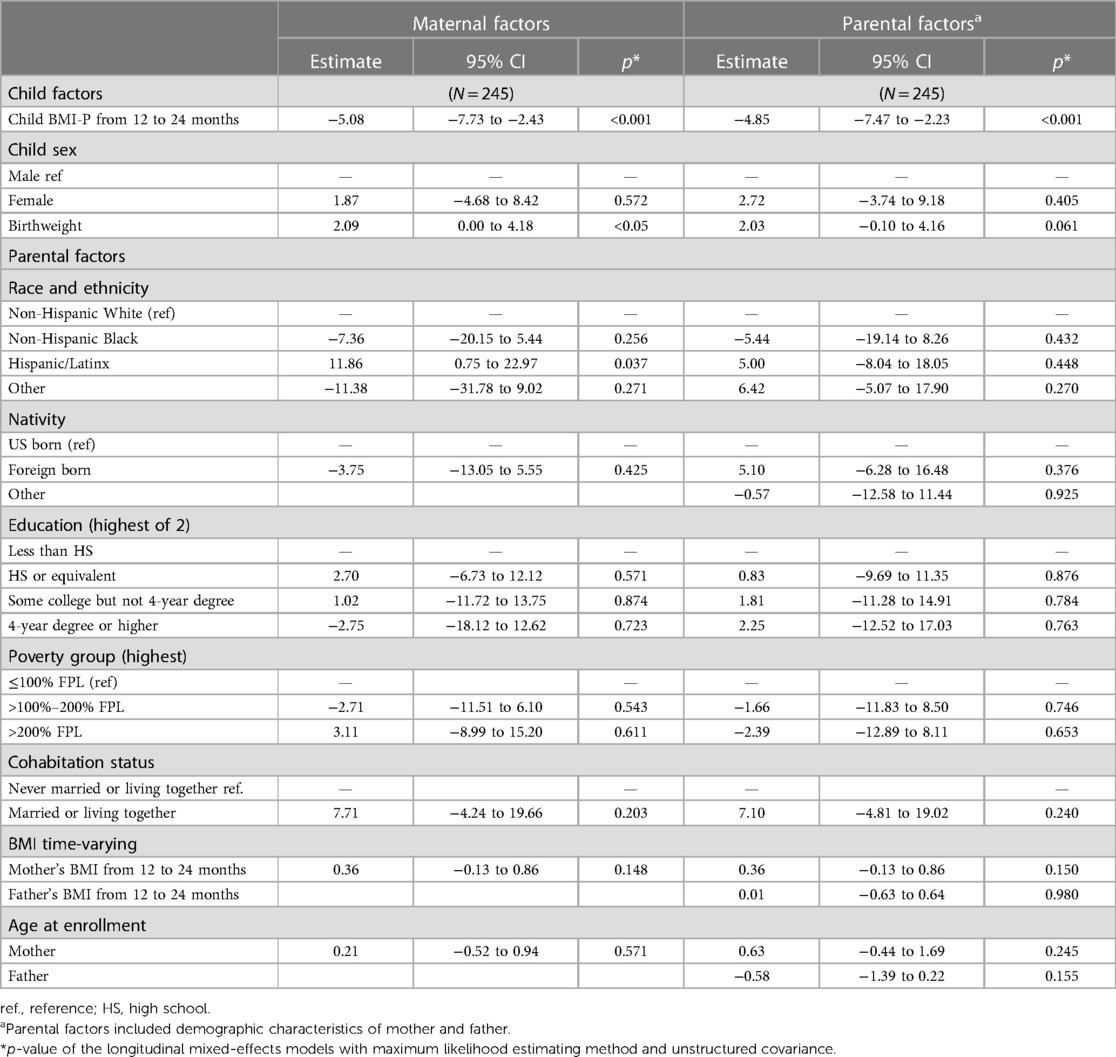
Table 2. Association of changes in children's age- and sex-adjusted body mass index percentile (BMI-P) from 12 to 24 months with maternal factors and parental factors.
Models that examined mothers’ and fathers’ predictors combined confirmed that children's overall mean BMI-P significantly decreased from 12 to 24 months (β = −4.85, 95% CI, −7.47 to −2.23, p < 0.01). Parent's age, race and ethnicity, nativity, level of completed education, poverty level, marital or cohabitation status, and changes on mother's or father's BMI from children's 12–24 months of age were not significantly associated with changes in children's mean BMI-P (p > 0.05). Sensitivity tests confirmed these findings.
Parental factors associated with change in children's BMI-P from 12 to 24 months
Table 3 shows the tests of the association of maternal factors exclusively and maternal and paternal factors combined with changes in their children's BMI-P from 12 to 24 months stratified by race and ethnicity. Within race tests showed that among White children, mean BMI-P did not significantly change from 12 to 24 months (p > 0.05). Tests of maternal predictors exclusively revealed that White children whose mothers completed a 4-year college degree or higher had a significant decrease in BMI-P (β = −46.43, 95% CI, −90.08 to −2.77, p = 0.04). Furthermore, when compared to White children born to parents with less than high school education, White children whose parents graduated high school or completed a 4-year college degree or higher had a significant decrease in BMI-P (β = −60.39, 95% CI, −115.05 to −5.72, p = 0.03 for high school graduates; β = −61.49, 95% CI, −122.44 to −0.53, p < 0.05 for college graduates). This association was confirmed in the tests that included the highest level of education achieved by both parents, but not in the sensitivity analyses that excluded children with imputed 12-month BMI-P measurements presented in Supplementary Table S3A. White mothers' or fathers' poverty group, cohabitation status, and BMI were not significantly associated with changes in their children's BMI-P from 12 to 24 months (p > 0.05).
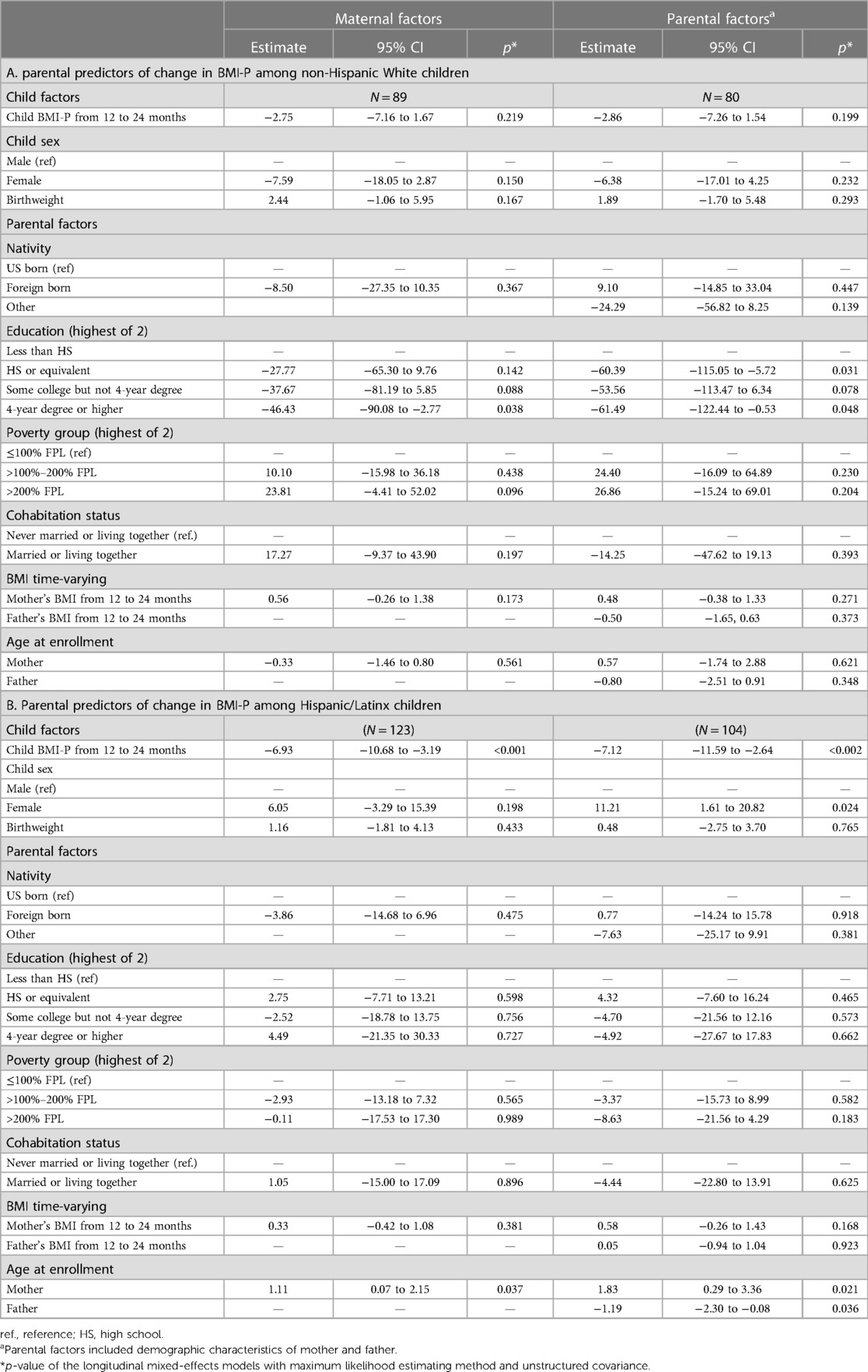
Table 3. Tests of the association of maternal factors exclusively and maternal and paternal factors combined with changes in their children's BMI-P from 12 to 24 months stratified by race and ethnicity.
Parental factors associated with change in Hispanic/Latinx children's BMI-P from 12 to 24 months
Table 3 provides the coefficients of the tests of maternal and maternal and paternal predictors and confirms that among Hispanic/Latinx children, BMI-P significantly decreased from 12 to 24 months. Tests of maternal predictors exclusively showed that mother's older age is associated with increases in their children's BMI-P from 12 to 24 months (β = 1.11, 95% CI, 0.07–2.15, p = 0.04). This association was consistent in the test that included maternal and paternal predictors and in the sensitivity analyses presented in Supplementary Table S3B. Tests with determinants from both parents showed that mother's older age was significantly associated with gain in children's BMI-P from 12 to 24 months (β = 1.83, 95% CI, 0.29–3.36, p = 0.02). Meanwhile, father's older age was associated with decreases in children's BMI-P from 12 to 24 months (β = −1.19, 95% CI, −2.30 to −0.08, p = 0.04). Tests including data from both parents showed that when compared with Hispanic/Latino males, mean BMI-P of Hispanic/Latina females significantly increased from 12 to 24 months (β = 11.21, 95% CI, 1.61–20.82, p = 0.02). Parent's nativity, level of completed education, poverty level, marital or cohabitation status, and changes in parent's BMI were not significantly associated with changes in Hispanic/Latinx children's BMI-P from 12 to 24 months (p > 0.05). Sensitivity analyses confirmed these findings.
Discussion
The first 2 years of life are known to be a critical period with important health consequences for future health; yet, information of children's growth in very early ages, particularly of racial and ethnic diverse children, remains limited. Childhood obesity rates have not plateaued in the United States. Data from 2015 to 2016 showed a sharp increase in obesity prevalence among children aged 2–5 years (25). These alarming increases highlight the need to improve the identification of children at risk for excessive weight gain during the first 2 years of life, when prevention may be more effective. To this end, this study advances our understanding of growth in early childhood using current data from a diverse sample of children and examining determinants from mothers and both parents. Findings revealed that, when assessing all children's growth from 12 to 24 months of age, BMI-P decreased. However, changes in BMI-P suggest that racial/ethnic disparities between Hispanic/Latinx and White children may begin in the first year of life. Analyses including only maternal demographic factors showed that having a Hispanic/Latinx mother and higher birthweight was associated with gain in BMI-P from 12 to 24 months. Racial and ethnicity-stratified analyses revealed that among White children, higher parental education, particularly having at least one parent graduate from high school or from a 4-year college or higher, was associated with greater BMI-P decreases during the first year of life in relationship with less than high school education. Notably, higher parental education achievement did not afford the same benefits to Hispanic/Latinx children. It was also noted that the inclusion of paternal predictors in the models helped identify factors that were not associated with children's BMI-P changes in the model that examined the contribution of maternal factors. Together, these findings highlight the importance of increasing representation of racial and ethnic diverse families in research and the urgent need to also consider the contributions of paternal determinants to child health outcomes, not instead of but in addition to the mothers.
A recent study showed that in the United States, trajectories and precursors of excessive weight gain from birth to 9 years of age vary by race and ethnicity (7). Our findings confirm that racial and ethnic differences in children's growth, and the factors that influence their growth, begin early in life. A better understanding of the racial and ethnicity-specific determinants associated with weight changes is urgently needed to inform culturally grounded obesity prevention strategies.
In the analyses of comparisons within White children, the level of education completed by their mother and the highest level of education completed by either parent, specifically having graduated from high school or college, was associated with decreases in children’s BMI-P from 12 to 24 months. A systematic review that examined data from the 27 richest countries suggested that parental education is a stronger indicator of child and adolescent weight status than income and/or occupation (26). This review suggested that the association can be attributed to healthier lifestyles in homes where parents have higher education levels (26). However, the association of parental educational achievement with children's optimal growth is not consistent. Previous studies conducted with older children have shown that having a parent with higher education attainment was associated with lower obesity risks among White, but not among Black, youth (27, 28). This is consistent with the diminishing return hypothesis that poses that the effects of socioeconomic achievement are not uniform across diverse racial and ethnic individuals (10). Our findings expand this literature by evidencing that racial and ethnic differences in the association of parental education attainment with children's optimal growth were present from very early ages and influenced White, but not Hispanic/Latinx, children. We hypothesize that persistent racial and ethnic inequalities and discrimination experiences may explain the lack of health benefits observed among children born to Hispanic/Latinx parents. For example, it has been documented that racial and ethnic minority parents with higher educational achievements, particularly first-generation college graduates, earn less than their White counterparts (29). As a result of the payment gap, it can be presumed that the offspring of Hispanic/Latinx parents who achieved higher levels of education received only a fraction of the benefits than higher education introduced to their White counterparts.
Comparisons within the subsample of Hispanic/Latinx children showed that mothers older age was associated with higher BMI-P in children, while father's older age was associated with lower BMI-P. A previous study showed that maternal age below 25 or above 35 years was associated with higher obesity risks for their offspring (30). However, the association of maternal age with offspring weight gain is not always consistent. In a sample of White children living in New Zealand, researchers found that children born to mothers over 35 years old were about 0.5 cm taller and had 13% lower adiposity than the offspring of mothers aged less than 30 years (31). We were not able to find previous studies that included Hispanic/Latino fathers and examined the impact of fathers’ age on children's obesity risks. This is likely attributed to the lower representation of fathers in research and lack of examinations of father's age as a covariate. We hypothesized that the association of parental age with changes in children's BMI-P after the first year of life is likely due to differences in parental feeding styles and socioeconomic resources. Older Hispanic/Latinx mothers may be more likely to sooth a fussy baby with food than their younger counterparts. In the case of older Hispanic/Latinx fathers, we hypothesize that they may be more financially stable than their younger counterparts. A previous study conducted with nationally representative data found that a lower socioeconomic status in early childhood predicted obesity at age 4, particularly among children with Hispanic/Latinx mothers (32). There is a lack of knowledge about the fathers’ determinants that contribute to childhood obesity risks, particularly among racial/ethnic minority families. As Hispanic/Latinx women and men continue to postpone fertility, it is important to better understand the potential contribution to child obesity risks that may be attributed to mothers' and fathers' age at the time of birth.
Models of Hispanic/Latinx children that included information from both parents suggested that when compared with males, females were more likely to experience increases in BMI-P from 12 to 24 months, a period of life when BMI-P is expected to decrease (33). Previous studies have shown that sex differences in older ages are contrary to our findings. Among White and Hispanic/Latinx children aged 2–5 years old, prevalence of obesity is higher among males than females (34). Further research is needed to further examine sex differences in BMI-P gains among Hispanic/Latinx children in early childhood.
Contrary to our hypotheses, parent's change in BMI-P was not associated with children's change in BMI-P from 12 to 24 months. Several studies have found that childhood BMI-P gains and obesity risks are greatly influenced by the weight status of mothers and fathers (35). However, important variations in the association suggest variations by children's age, family socioeconomic status, parental weight status, and, in the United States, race and ethnicity (35–37).
In the United States, the intergenerational transmission of obesity appears to be greater when examining maternal influences and present most often among White children than racial and ethnic minorities, particularly in families with older parents and higher socioeconomic status (36–38). We speculate the demographics of our sample and younger age of children at the time of the assessment may explain the lack of an association. These null findings support previous studies that suggested that intergenerational transmission of obesity is mostly attributable to behavioral, social, and environmental factors rather than biological differences, and are consequentially preventable.
Studies that use more precise indicators of adiposity have recognized that the ability of the current BMI-P cut-off recommendations to identify youth with excess body fatness and cardiometabolic risks varies by race/ethnicity (39). In nationally representative samples of US youth, studies have shown that non-Hispanic Black youth have significantly lower percentage of body fat for BMI than non-Hispanic White youth; meanwhile, Asian and Mexican American or Hispanic youth have higher fatness (39, 40). Higher fatness at similar levels of BMI is associated with higher cardiometabolic risks among Asian and Mexican American adults (41). When compared with other ethnic/racial groups in the United States, both Mexican American and Asian adults had a higher percent of body fat and metabolic syndrome at similar BMI levels (41). In response to the evidence of increased cardiometabolic risks at lower BMI cut-off points documented among Asian adults, the World Health Organization introduced population-specific BMI cut-off criteria for overweight and obesity (42). However, to date, population-specific recommendations have not been issued for Asian children or adolescents and Hispanic/Latinx children or adults. Race- and ethnicity-specific cut-off values (43) along with unique sociocultural measurements (44, 45) are needed to improve researchers’ and clinicians' ability to prevent, monitor, and treat obesity and obesity-related comorbidities among racial and ethnic minority children.
To our knowledge, this is among the first studies to include data collected with a racial and ethnic diverse sample of both mothers and fathers in the assessments of changes in BMI-P after the first year of life, a critical age for future obesity risks. A recent systematic review examining the inclusion of fathers in childhood obesity research found that fathers were included only in less than 10% of studies (18). In our study, the inclusion of maternal predictors and combined maternal and paternal determinants elucidated important differences in risk factors affecting children's BMI-P changes in early life. Overall models showed that considering father's educational attainment, poverty level, and age, along with mother's demographics attenuated the association of children's birthweight and mothers’ Hispanic/Latinx background with children's BMI-P change from 12 to 24 months of age. These associations were also attenuated in our sensitivity analyses presented in the Supplementary Tables, further suggesting lower robustness.
Findings of this study should be interpreted with caution in the context of the sample limitations. The study included a racial and ethnic diverse sample of predominantly low-income families. Thus, findings are not nationally representative and should be interpreted in the context of the large proportion White families with high education and Hispanic/Latinx with low education attainment who participated in the study. The limited number of African American/Black families who participated in the 24-month examination is also a key limitation that precluded the inclusion of this important racial minority in our stratified analyses. The early-life parental predictors of changes in BMI-P identified are not necessarily cause of obesity. Rather, factors are associated with children's probability of increases and decreases in BMI-P from 12 to 24 months. Although we examined multiple maternal and paternal predictors, lurking and unexamined variables (e.g., breastfeeding status, social determinants of health, timing of introduction to solids, parenting and feeding style, etc.) may explain the observed differences by race and ethnicity and the associations identified.
In conclusion, our results highlight the importance of increasing representation of racial and ethnic minorities in research and considering the influence of social determinants influencing the lives of both mothers and fathers in analyses of BMI-P changes during early life. Our findings suggest that higher levels of parental education were associated with greater reductions in BMI-P among White, but not Hispanic/Latinx, children. Among Hispanic/Latinx, girls and children born to older mothers and/or younger fathers were more likely to experience increases in BMI-P from 12 to 24 months than boys and children born to younger mothers and older fathers. Further research is needed to better understand the race- and ethnicity-specific mechanisms through which maternal and paternal social determinants influence disparities in children's growth and obesity risks in early life.
Data availability statement
The datasets for this article are not publicly available due to concerns regarding participant/patient anonymity. Requests to access the datasets should be directed to The Eunice Kennedy Shriver National Institute of Child Health and Human Development Data and Specimens Hub (NICHD/DASH).
Ethics statement
Ethics approval was sought from and given by the Institutional Review Boards at the respective institutions affiliated with each of the four study sites (Northshore University Hospital in Lake County, IL, Johns Hopkins University, Baltimore, MD, University of California, Los Angeles, and University of North Carolina, Chapel Hill).
Author contributions
LA and MS designed the study. LA drafted the manuscript. LA and CC conducted the data analyses. CC, LM, and MS revised it critically for important intellectual content. All authors contributed to the article and approved the submitted version.
Funding
This study is supported by the HRSA grant number R40MC26808. The CCHN is supported through cooperative agreements with the Eunice Kennedy Shriver National Institute of Child Health and Human Development (U HD44207, U HD44219, UHD44226, U HD44245, U HD44253, U HD54791, U HD54019, U HD44226-05S1, U HD44245-06S1, and R03HD59584) and the National Institute for Nursing Research (U NR008929). LA is supported by the American Heart Association (AHA Award Number: 938767), the National Institute of Diabetes and Digestive and Kidney Diseases (5R01DK115937-02), and the National Institute of Environmental Health Sciences (NIEHS K12ESO33593). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the HRSA or the AHA.
Acknowledgments
CCHN reflects joint endeavors of five local sites: Baltimore: Baltimore City Healthy Start and Johns Hopkins University: Community PI: M. Vance; Academic PI: C. S. Minkovitz; Co-Invs: P. O’Campo, and P. Schafer; Project Coordinators: N. Sankofa and K. Walton. Lake County, IL: Lake County Health Department and Community Health Center and the NorthShore University Health System: Community PI: K. Wagenaar; Academic PI: M. Shalowitz; Co-Invs: E. Adam, G. Duncan*, A. Schoua-Glusberg, C. McKinney, T. McDade, and C. Simon; Project Coordinators: B. Clark-Kauffman and Karen Reyes. Los Angeles: Healthy African-American Families, Cedars-Sinai Medical Center, University of California, Los Angeles: Community PI: L. Jones, Academic PI: C. Hobel, Co-PIs: C. Dunkel Schetter and M. C. Lu; Co-I: B. Chung; Project Coordinators: F. Jones, D. Serafin, and D. Young. North Carolina: East Carolina University, NC Division of Public Health, NC Eastern Baby Love Plus Consortium, and University of North Carolina, Chapel Hill: Community PIs: S. Evans, J. Ruffin, and R. Woolard; Academic PI: J. Thorp; Co-Invs: J. DeClerque, C. Dolbier, and C. Lorenz; Project Coordinators: L. S. Sahadeo and K. Salisbury. Washington, DC: Virginia Tech Carilion Research Institute, Virginia Tech, and Washington Hospital Center, and Developing Families Center: Community PI: L. Patchen, Academic PIs: S. L. Ramey and L. Klerman; Academic Co-PI: R. Lanzi; Co-Invs: M. Miodovnik, C. T. Ramey, and L. Randolph; Project Coordinator: N. Timraz; Community Coordinators: R. German and J. Bond*. Data Coordination and Analysis Center (Pennsylvania State University): PI: V. M. Chinchilli; Project Coordinator: G. Snyder; Co-Invs: R. Belue, G. Brown Faulkner*, M. Hillemeier, I. Paul, and M. L. Shaffer; Biostatisticians: E. Lehman and C. Stetter; Data Managers: J. Schmidt, K. Cerullo, and S. Whisler; Programmers: J. Fisher, J. Boyer, and M. Payton. NIH: Program Scientists: V. J. Evans and T. Raju, Eunice Kennedy Shriver National Institute of Child Health and Human Development; L. Weglicki, National Institute of Nursing Research. Program Officers: M. Spittel* and M. Willinger, NICHD; and Y. Bryan*, NINR. Steering Committee Chairs: E. Fuentes-Afflick* (University of California—San Francisco School of Medicine) and M. Phillippe (University of Vermont). * indicates those who participated in the planning phase of the CCHN.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1213534/full#supplementary-material
References
1. Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. J Am Med Assoc. (2018) 319(23):2410–8. doi: 10.1001/jama.2018.5158
2. Cunningham SA, Datar A, Narayan KMV, Kramer MR. Entrenched obesity in childhood: findings from a national cohort study. Ann Epidemiol. (2017) 27(7):435–41. doi: 10.1016/j.annepidem.2017.05.016
3. Perng W, Rifas-Shiman SL, Kramer MS, Haugaard LK, Oken E, Gillman MW, et al. Early weight gain, linear growth, and mid-childhood blood pressure: a prospective study in project viva. Hypertension. (2016) 67(2):301–8. doi: 10.1161/HYPERTENSIONAHA.115.06635
4. Aris IM, Rifas-Shiman SL, Li LJ, Yang S, Belfort MB, Thompson J, et al. Association of weight for length vs. body mass index during the first 2 years of life with cardiometabolic risk in early adolescence. JAMA Netw Open. (2018) 1(5):e182460. doi: 10.1001/jamanetworkopen.2018.2460
5. Innella N, Breitenstein S, Hamilton R, Reed M, McNaughton DB. Determinants of obesity in the Hispanic preschool population: an integrative review. Public Health Nurs. (2016) 33(3):189–99. doi: 10.1111/phn.12215
6. Jones A. Race, socioeconomic status, and health during childhood: a longitudinal examination of racial/ethnic differences in parental socioeconomic timing and child obesity risk. Int J Environ Res Public Health. (2018) 15(4):728. doi: 10.3390/ijerph15040728
7. Pineros-Leano M, Grafft N, Aguayo L. Childhood obesity risk factors by race and ethnicity. Obesity. (2022) 30(8):1670–80. doi: 10.1002/oby.23500
8. Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, et al. Early life risk factors for obesity in childhood: cohort study. Br Med J. (2005) 330(7504):1357. doi: 10.1136/bmj.38470.670903.E0
9. Pineros-Leano M. Association between early maternal depression and child growth: a group-based trajectory modeling analysis. Child Obes. (2019) 16(1):26–33. doi: 10.1089/chi.2019.0121
10. Ciciurkaite G. Race/ethnicity, gender and the SES gradient in BMI: the diminishing returns of SES for racial/ethnic minorities. Sociol Health Illn. (2021) 43(8):1754–73. doi: 10.1111/1467-9566.13267
11. Assari S, Bazargan M, Caldwell C. Parental educational attainment and chronic medical conditions among American youth; minorities’ diminished returns. Children. (2019) 6(9):96. doi: 10.3390/children6090096
12. Assari S, Boyce S, Bazargan M, Mincy R, Caldwell CH. Unequal protective effects of parental educational attainment on the body mass index of black and white youth. Int J Environ Res Public Health. (2019) 16(19):3641. doi: 10.3390/ijerph16193641
13. Assari S. College graduation and wealth accumulation: blacks’ diminished returns. World J Educ Res. (2020) 7(3):1–18. doi: 10.22158/wjer.v7n3p1
14. Guerrero AD, Mao C, Fuller B, Bridges M, Franke T, Kuo AA. Racial and ethnic disparities in early childhood obesity: growth trajectories in body mass index. J Racial Ethn Health Disparities. (2016) 3(1):129–37. doi: 10.1007/s40615-015-0122-y
15. Isong IA, Rao SR, Bind MA, Avendaño M, Kawachi I, Richmond TK. Racial and ethnic disparities in early childhood obesity. Pediatrics. (2018) 141(1):e20170865. doi: 10.1542/peds.2017-0865
16. Davison KK, Gicevic S, Aftosmes-Tobio A, Ganter C, Simon CL, Newlan S, et al. Fathers’ representation in observational studies on parenting and childhood obesity: a systematic review and content analysis. Am J Public Health. (2016) 106(11):e14–21. doi: 10.2105/AJPH.2016.303391
17. Rangel DE, Rauscher E. Paternal education and infant health: variation by race/ethnicity. J Racial Ethn Health Disparities. (2020) 1406–14. doi: 10.1007/s40615-020-00902-8
18. Slining M, Adair LS, Goldman BD, Borja JB, Bentley M. Infant overweight is associated with delayed motor development. J Pediatr. (2010) 157(1):20–5.e21. doi: 10.1016/j.jpeds.2009.12.054
19. Shoaibi A, Neelon B, Østbye T, Benjamin-Neelon SE. Longitudinal associations of gross motor development, motor milestone achievement and weight-for-length z score in a racially diverse cohort of US infants. BMJ Open. (2019) 9(1):e024440. doi: 10.1136/bmjopen-2018-024440
20. Zheng M, Lamb KE, Grimes C, et al. Rapid weight gain during infancy and subsequent adiposity: a systematic review and meta-analysis of evidence. Obes Rev. (2018) 19(3):321–32. doi: 10.1111/obr.12632
21. Pool LR, Aguayo L, Brzezinski M, Perak AM, Davis MM, Greenland P, et al. Childhood risk factors and adulthood cardiovascular disease: a systematic review. J Pediatr. (2021) 232:118–26.e23. doi: 10.1016/j.jpeds.2021.01.053
22. Goodell LS, Wakefield DB, Ferris AM. Rapid weight gain during the first year of life predicts obesity in 2-3 year olds from a low-income, minority population. J Community Health. (2009) 34(5):370–5. doi: 10.1007/s10900-009-9164-6
23. Victora CG, de Onis M, Hallal PC, Blössner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. (2010) 125(3):e473–80. doi: 10.1542/peds.2009-1519
24. Ramey SL, Schafer P, DeClerque JL, et al. The preconception stress and resiliency pathways model: a multi-level framework on maternal, paternal, and child health disparities derived by community-based participatory research. Matern Child Health J. (2015) 19(4):707–19. doi: 10.1007/s10995-014-1581-1
25. Cunningham SA, Hardy ST, Jones R, Ng C, Kramer MR, Narayan KMV. Changes in the incidence of childhood obesity. Pediatrics. (2022) 150(2):e2021053708. doi: 10.1542/peds.2021-053708
26. Barriuso L, Miqueleiz E, Albaladejo R, Villanueva R, Santos JM, Regidor E. Socioeconomic position and childhood-adolescent weight status in rich countries: a systematic review, 1990-2013. BMC Pediatr. (2015) 15:129. doi: 10.1186/s12887-015-0443-3
27. Patterson ML, Stern S, Crawford PB, et al. Sociodemographic factors and obesity in preadolescent black and white girls: NHLBI’s growth and health study. J Natl Med Assoc. (1997) 89(9):594–600. PMID: 9302856; PMCID: PMC2608268
28. Brophy S, Cooksey R, Gravenor MB, Mistry R, Thomas N, Lyons RA, et al. Risk factors for childhood obesity at age 5: analysis of the millennium cohort study. BMC Public Health. (2009) 9:467. doi: 10.1186/1471-2458-9-467
29. Manzoni A, Streib J. The equalizing power of a college degree for first-generation college students: disparities across institutions, majors, and achievement levels. Res High Educ. (2019) 60(5):577–605. doi: 10.1007/s11162-018-9523-1
30. Myrskylä M, Fenelon A. Maternal age and offspring adult health: evidence from the health and retirement study. Demography. (2012) 49(4):1231–57. doi: 10.1007/s13524-012-0132-x
31. Savage T, Derraik JGB, Miles HL, Mouat F, Hofman PL, Cutfield WS. Increasing maternal age is associated with taller stature and reduced abdominal fat in their children. PLoS One. (2013) 8(3):e58869. doi: 10.1371/journal.pone.0058869
32. Kitsantas P, Gaffney KF. Risk profiles for overweight/obesity among preschoolers. Early Hum Dev. (2010) 86(9):563–8. doi: 10.1016/j.earlhumdev.2010.07.006
33. Roy SM, Spivack JG, Faith MS, et al. Infant BMI or weight-for-length and obesity risk in early childhood. Pediatrics. (2016) 137(5):e20153492. doi: 10.1542/peds.2015-3492
34. Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. J Am Med Assoc. (2016) 315(21):2292–9. doi: 10.1001/jama.2016.6361
35. Lee JS, Jin MH, Lee HJ. Global relationship between parent and child obesity: a systematic review and meta-analysis. Clin Exp Pediatr. (2022) 65(1):35–46. doi: 10.3345/cep.2020.01620 33781054
36. Zhang Q, Lamichhane R, Chen HJ, Xue H, Wang Y. Does child-parent resemblance in body weight status vary by sociodemographic factors in the USA? J Epidemiol Community Health. (2014) 68(11):1034–42. doi: 10.1136/jech-2013-203476
37. Linabery AM, Nahhas RW, Johnson W, et al. Stronger influence of maternal than paternal obesity on infant and early childhood body mass index: the Fels longitudinal study. Pediatr Obes. (2013) 8(3):159–69. doi: 10.1111/j.2047-6310.2012.00100.x
38. Costa-Font J, Jofre-Bonet M. Is the intergenerational transmission of overweight ‘gender assortative’? Econ Hum Biol. (2020) 39:100907. doi: 10.1016/j.ehb.2020.100907
39. Dugas LR, Cao G, Luke AH, Durazo-Arvizu RA. Adiposity is not equal in a multi-race/ethnic adolescent population: NHANES 1999-2004. Obesity. (2011) 19(10):2099–101. doi: 10.1038/oby.2011.52
40. Martin CB, Stierman B, Yanovski JA, Hales CM, Sarafrazi N, Ogden CL. Body fat differences among US youth aged 8–19 by race and Hispanic origin, 2011–2018. Pediatr Obes. (2022) 17(7):e12898. doi: 10.1111/ijpo.12898
41. Min J, Goodale H, Xue H, Brey R, Wang Y. Racial-ethnic disparities in obesity and biological, behavioral, and sociocultural influences in the United States: a systematic review. Adv Nutr. (2021) 12(4):1137–48. doi: 10.1093/advances/nmaa162
42. Author A. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363(9403):157–63. doi: 10.1016/S0140-6736(03)15268-3
43. LeCroy MN, Kim RS, Stevens J, Hanna DB, Isasi CR. Ethnicity-specific BMI cutoffs for obesity based on type 2 diabetes risk in England: a population-based cohort study. Lancet Diabetes Endocrinol. (2021) 9(7):419–26. doi: 10.1016/S2213-8587(21)00088-7
44. LeCroy MN, Kim RS, Stevens J, Hanna DB, Isasi CR. Identifying key determinants of childhood obesity: a narrative review of machine learning studies. Child Obes. (2021) 17(3):153–9. doi: 10.1089/chi.2020.0324
Keywords: infant, obesity, childhood obesity, father, parental education, Hispanic/Latinx
Citation: Aguayo L, Chang C, McCormack LR and Shalowitz MU (2023) Parental determinants associated with early growth after the first year of life by race and ethnicity. Front. Pediatr. 11:1213534. doi: 10.3389/fped.2023.1213534
Received: 28 April 2023; Accepted: 27 June 2023;
Published: 25 July 2023.
Edited by:
Megan Gow, The University of Sydney, AustraliaReviewed by:
Lenycia De Cassya Lopes Neri, University of São Paulo, BrazilJ. Carolyn Graff, University of Tennessee Health Science Center (UTHSC), United States
© 2023 Aguayo, Chang, McCormack and Shalowitz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liliana Aguayo bGlsaWFuYS5hZ3VheW8tbWFya2VzQGVtb3J5LmVkdQ==
 Liliana Aguayo
Liliana Aguayo Cecilia Chang
Cecilia Chang Luke R. McCormack3
Luke R. McCormack3